Abstract
Introduction
In early 2020, our hospital responded with high alertness when novel coronavirus SARS-CoV-2 appeared. A hospital-based training programme was rapidly arranged to prepare staff for the imminent threat.
Objective
We developed a hospital-wide multidisciplinary infection control training programme on endotracheal intubation for healthcare workers to minimise nosocomial spread of COVID-19 during this high-stress and time-sensitive risky procedure.
Methodology
Major stakeholders (Quality & Safety Department, Infection Control Team, Central Nursing Division, high-risk clinical departments and hospital training centre) formed a training programme task group. This group was tasked with developing high-fidelity scenario-based simulation training curriculum for COVID-19 endotracheal intubation with standard workflow and infection control practice. This group then implemented and evaluated the training programme for its effectiveness.
Results
101 training classes of 2-hour session were conducted from 5 February to 18 March 2020, involving 1415 hospital staff (~81% of target participants with training needs) either inside the hospital training centre or as in situ simulation training (intensive care unit or accident and emergency department). Learners’ satisfaction was reflected by overall positive response percentage at 90%. Opinions of participating staff were incorporated into the standard airway management and infection control practice for endotracheal intubation of adult patients with COVID-19. Thirty-five patients with COVID-19 were intubated with the current workflow and guideline without any nosocomial transmission.
Conclusion
An early planned and well-structured multidisciplinary hospital-wide simulation training programme was organised expeditiously to provide extensive staff coverage. The insight and experience gained from this project is valuable for future infectious disease challenges.
Keywords: simulation in healthcare, anaesthesia, endotracheal intubation
What is already known on this subject.
COVID-19 poses a major threat for healthcare system and there are high causalities in healthcare workers (HCWs) which can cripple the system.
Endotracheal intubation is the most consistently high-risk aerosol-generating procedure that causes the nosocomial spread of COVID-19 and other contagious acute respiratory diseases to HCWs.
Simulation training can bridge the knowledge gap, enhance skill competency and alleviate anxiety of HCWs.
What this study adds.
Hospital-wide training programme for contagious disease like COVID-19 can still be implemented early in outbreak with coordinated effort.
With limited resources and time, the focus of COVID-19 training should be on three areas: individual infection control practice optimisation, team work designation to minimise exposure and workflow reorganisation to contain contamination.
Frontline HCWs opinions can be effectively and efficiently incorporated into hospital workflow through training for COVID-19 preparedness.
Introduction
Hospital Authority, a statutory body established under the Hospital Authority Ordinance of Hong Kong Special Administrative Region in 1990, has been managing 43 public hospitals and 122 outpatient clinics with over 84 000 staff members and 29 000 beds for the 8 million population. After Hong Kong suffered a great loss from severe acute respiratory syndrome (SARS) outbreak in 2003,1 the Hong Kong Centre for Health Protection was established and policy was set up to face any similarly drastic and swift challenge because history repeats itself.2
After the first reported cases of pneumonia of unknown aetiology (SARS-CoV-2) detected in Wuhan City, the Government and Hospital Authority Head Office of Hong Kong SAR raised the response level to ‘serious’ on 4 January 2020. Queen Elizabeth Hospital (QEH) received the first confirmed case on 23 January 2020, and the region raised to the highest emergency response level on 25 January 2020. Without hesitation, our hospital chief executive and senior management proactively launched a preparatory plan that included a comprehensive hospital-based training programme as part of it before WHO declared Public Health Emergency of International Concern for this disease. The training programme was aimed to be organised as soon as possible with extensive coverage at all frontline staff level within a short period in anticipation of COVID-19 patient surge. Hospital Quality & Safety Department convened a multidisciplinary training programme task group composed of relevant stakeholders.
High-fidelity scenario-based simulation training has been used as an educational tool to improve individual and team performances through deliberate practice.3–8 It can enhance staff preparedness, improve systems and protocols and ultimately patient safety.9 Simulation is an excellent method to prepare healthcare workers (HCWs) and systems for disaster response.10
Close airway contact of critical patients during aerosol generating procedures with failure of infection control practice was proven to increase risk of SARS transmission to HCWs.11 Bag mask ventilation and endotracheal intubation are deemed as aerosol-generating procedure. The evidence suggests that performing or exposure to endotracheal intubation, either by itself or combined with other procedures (eg, cardiopulmonary resuscitation or bronchoscopy), is the most consistently associated risk factor of nosocomial transmission of acute respiratory infections.12 13 Viral load of the patient with COVID-19, contaminated environment together with aerosol generating nature of the procedure account for its high infectivity to HCWs. Christian et al 14 recommended in addition to provision of proper personal protective equipment (PPE) for staff performing this ‘high-risk’ procedure, the administrative controls and environmental controls should also be included in the systematic approach to this problem. Caputo et al 15 also suggested that protection guidelines alone failed to prevent SARS transmission to HCWs. Mission of this training programme task group was to prepare the simulation training scenario for COVID-19 endotracheal intubation, define the role of different teams, modify the guidelines and workflow logistics and integrate feedback and opinions of trained staff into the hospital standard of practice.
The desired outcome was a critical mass of hospital HCWs to go through the training programme. They would be trained with endotracheal intubation practice with proper infection control measures for critical patients with COVID-19 to provide safe, timely and quality patient care. Moreover, the proper and up-to-date infection control principles, measures and skills in general practice could also be promoted and conveyed in the training programme. This paper records the preparation, arrangement, process, impact and the outcome of the hospital training programme in face of COVID-19 disease.
Methods
The training programme task group for critical COVID-19 endotracheal intubation was convened by the Quality & Safety Department. Members included representatives from Accident & Emergency Department, Central Nursing Division, Infection Control Teams, Department of Anaesthesiology & Operation Theatre Services, Intensive Care Unit, Multi-disciplinary Simulation and Skills Centre and Resuscitation Committee. These departments were either involved in the treatment of critical patients with COVID-19 or responsible for hospital staff training. The training programme was subsequently coordinated, prepared and implemented by Central Nursing Division and training centre, as well as supported by Infection Control Teams.
Emergency airway management outside the operating theatre involves multidisciplinary collaboration in an unfavourable physical environment under great time stress. After the training, the learners were expected to perform proper donning and doffing of PPE, to practice the procedure under standard guidelines and to work as a team with clear role delineation defined by protocol. The task group reviewed the WHO guideline on respiratory infections,16 Hospital Authority Head Office infection control guideline,17 expert opinion of hospital Infection Control Teams and literature on nosocomial SARS transmission and its related training.
WHO clinical management of 2019-nCoV infection is suspected
In the table of ‘How to implement infection prevention and control measures for patients with suspected or confirmed 2019-nCoV’ and section on ‘Management of hypoxemic respiratory failure and acute respiratory distress syndrome’,16 recommendations are:
-
Contact precaution for protection against transmission from contact with contaminated surfaces or equipment in contaminated environment like airborne infection isolation room.
Use PPE when entering and remove it when leaving the room.
Use either disposable or dedicated equipment (eg, stethoscopes, blood pressure cuffs, and monitors).
Avoid patient movement or transport.
-
Airborne precaution against infective aerosol generated during procedures like endotracheal intubation
All HCWs performing aerosol-generating procedures use PPE, including gloves, long-sleeved gowns, eye protection, fit-tested N95 or higher level of protection respirators.
Avoid the presence of unnecessary individuals in the room.
Endotracheal intubation should be performed by a trained and experienced provider using airborne precautions.
Hospital Authority Head Office infection control guideline and toolkit
According to Hospital Authority,17 recommendations are:
N95 respirators, face shield/goggles for eye protection, disposable isolation gown (Association for the Advancement of Medical Instrumentation, Level 3), gloves with proper hand hygiene for aerosol-generating procedures in both high-risk patient areas and other patient areas (recommended PPE under serious response (S2) and emergency level, 81 of 126 slides).
Assign trained staff with full PPE for the procedure and limit the number of staff in the room during the procedure (management of aerosol-generating procedures in general ward).
Development of scenario design
COVID-19 training scenario prototype was prepared by nurse educators with input of simulation training experts and other clinical specialists. It was set as a deteriorating patient with COVID-19 requiring endotracheal intubation. Details of role delineation, responsibility and collaboration of Parent Team and Central Resuscitation Team, clean and non-clean zone segregation to minimise staff and environmental contamination were included. Learners were required to work as a team to manage this patient under proper infection control measures against infectious respiratory droplets and fomites in a relatively closed environment. Airway management workflow was based on the ‘Measures for Intubation in General Ward/ Air-borne Infection Isolation Room) during nCoV (Novel Coronavirus which was subsequently named as COVID-19 by World Health Organisation on 11 February 2020) Period’ for emergency endotracheal intubation formulated by Department of Anaesthesiology & Operation Theatre Services. At the same time, the department had also promulgated the ‘Recommended safety measures for emergency intubation in General/ Isolation Wards during COVID-19’ (online supplemental appendix A) to all hospital medical and nursing staff in early February. By the time the learners joined the training courses, they already had some ideas of the latest arrangement and this recommendation. The scenario prototype was then vetted by the task group and finalised after a trial run observed by major stakeholders (online supplemental appendix B, scenarios of COVID-19 simulation training for isolation ward).
bmjstel-2020-000766supp001.pdf (78.7KB, pdf)
bmjstel-2020-000766supp002.pdf (295.1KB, pdf)
The training goals were to enhance the knowledge and skills of learners and different teams to help them protect themselves, work more collaboratively and use valuable resources rationally. Cognitive, procedural, communication and team work domains were covered in the training courses. The simulation instructors ensured that every step of donning and doffing of appropriate PPEs for airborne/droplet protection including test-fit N95, face shield±goggle, cap, gloves and water-proof gown were properly practiced in the training. Mistakes in infection control practice by HCWs were noted and corrected.
Just before the activation of the emergency response level, Hospital Authority Head Office announced cancellation of corporate training courses up to June 2020. This move gave the training centre maximal flexibility for training resources allocation to prepare and organise COVID-19 training classes instantly. The curriculum was designed with the aim to enhance staff protection, minimise staff exposure and environmental contamination with patient safety secured. The training class titled ‘Infectious Disease Practice Drill and Refresher Training (Novel Coronavirus)’ rolled out from 5 February to 18 March 2020. A standardised and unified workflow was developed in the training programme and adopted for subsequent clinical practice.
Considerations in procedures and setting of simulation training
Supported by experienced simulation educators with professional certificate in train-the-trainer programme accredited by Monash University, simulation training was conducted either in simulation lab for isolation ward and general ward staff or in the real clinical environment as in situ simulation inside accident and emergency (A&E) department and intensive care unit (ICU) for respective teams. The duration of each training session was 2 hours, covering: (1) briefing/familiarisation, (2) scenario-based simulation, (3) skills practice on doffing (and return demo), (4) debriefing, (5) discussion and sharing of common pitfall in caring of patient during aerosol generating procedures, as well as (6) evaluation/questionnaire (as in online supplemental appendix B, P.2 duration).
For each session, there were three to four trained instructors observing and recording notes in real time. After each training session, instructors held a debriefing with the participating team members and observers. Instructors led the discussion and reflection of participants on infection control performance, team work, compliance to protocol and other observed issues. Concerns and great ideas of the trained staff were shared during debriefing. These were collected and communicated with relevant stakeholders, including hospital senior management. Simulation was thus used both for training and process modification.
Training in the simulation lab, A&E and ICU proceeded simultaneously so that more staff could be trained within a limited period of time with minimal disturbance to service. Priority of training in simulation lab was given to staff working in isolation ward who took care of confirmed patients with COVID-19. Training of general ward staff who took care of asymptomatic patients commenced after training of isolation ward staff had accomplished. As different types of HCWs were infected in SARS, training was not limited to one profession but to all HCWs in close proximity to patients with COVID-19 in the ‘high-risk’ procedure (see figure 1).
Figure 1.
Training in proper personal protective equipment gear.
In order to conserve the PPE, which was in shortage for frontline clinical use, the genuine PPE was replaced by simulated PPE for training purpose. Examples included the use of industrial N95 masks, training centre three-dimensional printed visors and house-made face shields by centre simulation technicians, with the considerations of scientific evidence and cost-effectiveness.
Target participants and coverage
With the support of more than 700 doctors and 2500 nurses, QEH is one of the major hospitals providing acute and tertiary referral services for the community. Between financial year of 2019/2020, the amount of annual patient uptake in QEH was more than 113 thousand (table 1). According to a snapshot of hospital statistics (as of 31 March 2020) provided by statistical officer of QEH, 119 and 171 medical and nursing staff were hired in the ICU and A&E Department, respectively. Target participants for training of ‘general wards’ and ‘isolation wards’ (kept rotating staff from a department/ward to another one) were recruited from department of medicine (N=680, 39%), surgery (N=247, 14%), specialist outpatient (N = 83, 5%) and others (N=454, 26%). Of the 3200 doctors and nurses in QEH, 1754 (55%) from departments stated above were all our potential target participants. Coordinated by the Central Nursing Division, all participants were recruited through nomination received from department heads, department operation managers, nurse consultants and ward managers. Our aim of training coverage for potential target participants was 1400 (about 80%) within 6 weeks.
Table 1.
Hospital size and potential target participants in Queen Elizabeth Hospital (QEH)
| Potential target for COVID-19 sessions |
Target departments | Medical staff, n (%) | Nursing staff, n (%) | Annual patient uptake (1 April 2019 to 31 March 2020) |
| (as of 31 March 2020) | ||||
| In situ – ICU | Intensive Care Unit | 14 (4) | 105 (7) | 162 |
| In situ – A&E | Accident & Emergency | 46 (14) | 125 (9) | 172 435 |
| Simulation lab-based - ’Isolation Ward’ or ‘General Ward’ |
Medicine | 116 (34) | 564 (40) | 39 916 |
| Surgery | 59 (18) | 188 (13) | 17 260 | |
| Specialist Outpatient* | / | 83 (6) | 619 131 | |
| Others | 98 (30) | 356 (25) | 56 326 | |
| QEH inpatients (n=1754) |
333 (19) | 1421 (81) | 113 664 | |
‘Others’ included anaesthesiology and operation theatre service, orthopaedics and traumatology, obstetrics and gynaecology and clinical departments otherwise not specified.
*Unlike nurses, doctors who worked for Specialist Outpatient Department were those actually working in other relevant clinical departments (eg, consultants from specific department would spend time on outpatients session according to their clinical schedule). Patient intake from Accident & Emergency and Specialist Outpatient will be excluded from Annual Patient Uptake of QEH Inpatients between 1 April 2019 and 31 March 2020.
Ethical considerations
Ethical approval of the Research Ethics Committee of Hospital Authority was not necessary for medical and nursing education program initiated by high management of Hospital Authority. All participants were asked to complete a written informed consent on confidentiality issues and use of data from course evaluation, questionnaire, formal and informal feedback in written or verbal format, formative or summative assessment approved by respective steering committee, as well as audio-visual recording for internal audit, education and research purposes prior to commencement of each simulation training session.
Procedures and measurements
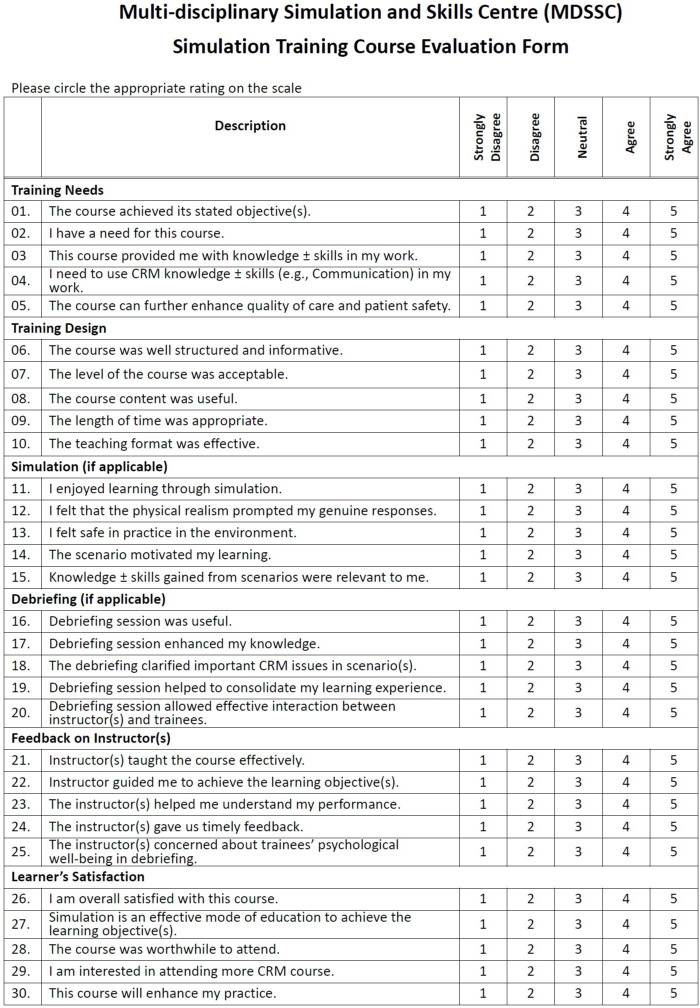
In line with quality assurance measures for accreditation standards of the Society of Simulation in Healthcare,18 all simulation training courses organised by the Multi-disciplinary Simulation and Skills Centre required participants and instructors completing standardised course evaluation forms. By the end of each training session, one set of questionnaires with 35 items (30 rating scales and 5 open-ended follow-up questions) and another set with 13 items (related to training quality of simulation session) were distributed to participants and instructors, respectively. Each item was measured on a 5-point Likert scale ranging from 1 ‘strongly disagree’ to 5 ‘strongly agree’. Positive response percentage is operationally defined as the proportion in counts for rating 4 ‘agree’ or 5 ‘extremely agree’ (figure 2).
Figure 2.
Questionnaire for participants in COVID-19 simulation training in Queen Elizabeth Hospital. CRM, Crew Resources Management.
With excellent interitem reliability (Cronbach’s alpha=0.92), average of summary content validity index (S-CVI/Ave=0.96) and scale content validity index with universal agreement (S-CVI/UA=0.87) reviewed by multidisciplinary committee members, participants’ questionnaire can be categorised into six domains: (1) training needs, (2) training design, (3) simulation, (4) debriefing, (5) feedback on instructor and (6) satisfaction.
Statistical and data analysis
Training deliverables and their distributions were covered with a demographic table prior to inferential statistical analysis. Participants were stratified by two groups with respective mode of simulation: (1) in situ and (2) lab based. Independent sample t-tests were used for between-group comparison of their population means of six domains, including: (1) training needs, (2) training design, (3) simulation, (4) debriefing, (5) feedback on instructor and (6) satisfaction. All significant levels of alpha were set at 0.05 (two tailed), if not otherwise indicated. The data were analysed using IBM SPSS Statistics (V.25.0, IBM Corp, 2017).
If there were no significant between-group differences, positive response percentage of different domains would be presented as basic descriptive statistics. On top of that, quantitative and qualitative feedback from instructors was roughly addressed in order to monitor the quality of simulation training in the lens of professional members in the field. Furthermore, qualitative contents drawn from feedback and opinions from stakeholders throughout the simulation training and debriefing sessions would be included as supplementary information to evoke further discussion.
Results
Training deliverables
Of 101 sessions carried out between 5 February and 18 March 2020, about one-third of simulation classes (A&E=20%; ICU=14%) was in situ in respective departments and two-thirds (isolation ward=30%; general ward=36%) was lab based in the training centre. Within this period under intense time and resources constraint, 1415 hospital staff members, including 1167 nurses, 163 doctors and 85 other professionals, were trained (see table 2 for ‘demographic table’). As a result, the number of trained potential target in crash courses, in either in situ or simulation lab-based mode was 1415 out of 1754 (81%). Total 1186 evaluation forms were collected from participants (response rate=84%).
Table 2.
Demographics table of COVID-19 simulation training course
| Based on attendance record | Number of session | Number of attendance | Simulation setting | |||
| Trained groups | Counts | (%) | Counts | (%) | In situ | Lab based |
| Accident & Emergency | 20 | (20) | 129 | (9) | ✓ | ✗ |
| Intensive Care Unit | 15 | (14) | 116 | (8) | ✓ | ✗ |
| Isolation Ward | 30 | (30) | 544 | (38) | ✗ | ✓ |
| General Ward | 36 | (36) | 626 | (45) | ✗ | ✓ |
| Based on attendance record | In situ | Lab-based | ||||
| Counts | (%) | Counts | (%) | |||
| Type of HCWs | Doctors | 59 | (24) | 104 | (9) | |
| Nurses | 176 | (72) | 991 | (85) | ||
| Others | 10 | (4) | 75 | (6) | ||
| Based on evaluation forms returned | In situ | Lab-based | ||||
| Counts | (%) | Counts | (%) | |||
| Gender | Female | 108 | (66) | 725 | (70) | |
| Male | 56 | (34) | 311 | (30) | ||
| Year(s) of clinical experience | <3 | 32 | (20) | 322 | (31) | |
| 3–6 | 50 | (30) | 186 | (18) | ||
| 7–10 | 54 | (33) | 318 | (31) | ||
| 11–15 | 18 | (11) | 85 | (8) | ||
| >15 | 10 | (6) | 124 | (12) | ||
| Department of participants | Accident & Emergency | 73 | (45) | / | / | |
| Intensive Care Unit | 91 | (55) | / | / | ||
| Anaesthesiology & Operation Theatre Service | / | / | 87 | (8) | ||
| Medicine | / | / | 454 | (44) | ||
| Surgery/Neurosurgery | / | / | 245 | (24) | ||
| Others | / | / | 250 | (24) | ||
‘Others’ included Orthopaedics & Traumatology, Obstetrics & Gynaecology and otherwise not specified.
HCW, healthcare worker.
Quantitative feedback
Regarding modes of simulation training, no significant mean differences between in situ and lab-based mode of simulation training were found (p>0.05) for all components in the questionnaire, in terms of training needs, training design, simulation, debriefing, instructor feedback and satisfaction. For participants, mean scores of positive response percentage ranged from 88% to 91% for all domains (table 3). For instructors, 74 evaluation forms were received from training of isolation ward (31%) and general ward (69%). Mean scores of positve response percentage ranged from 96% to 100% for all items (table 4).
Table 3.
Learners positive response percentage on COVID-19 simulation training for all trained groups
| Trained group: | A&E | ICU | Isolation ward | General ward | Overall |
| Domains | PR% | PR% | PR% | PR% | PR% |
| Training needs | 95 | 86 | 90 | 92 | 91 |
| Training design | 98 | 84 | 88 | 91 | 90 |
| Simulation | 96 | 83 | 85 | 91 | 88 |
| Debriefing | 97 | 89 | 90 | 92 | 91 |
| Feedback on instructor | 97 | 84 | 87 | 97 | 89 |
| Satisfaction | 96 | 83 | 88 | 91 | 89 |
| Overall | 97 | 85 | 88 | 91 | 90 |
A&E, Accident & Emergency Department; ICU, Intensive Care Unit; PR%, Positive Response Percentage.
Table 4.
Instructors positive response percentage on COVID-19 simulation training for isolation and general wards
| Trained groups: | Isolation ward | General ward | Overall |
| Items of questionnaire | PR% | PR% | PR% |
| 1) The objectives of the course are clearly stated. | 100 | 100 | 100 |
| 2) The course content is appropriate. | 100 | 100 | 100 |
| 3) The course manuals or materials are clear and useful. | 96 | 100 | 99 |
| 4) The amount of course material is sufficient. | 100 | 100 | 100 |
| 5) The scenarios are properly set. | 100 | 100 | 100 |
| 6) The modalities used in the scenario are appropriate. | 100 | 100 | 100 |
| 7) Learners performed well and actively involved in the scenarios. | 100 | 94 | 96 |
| 8) Learners performed well and actively involved in the debriefing session. | 100 | 94 | 96 |
| 9) The level of course to the learners is about right. | 100 | 100 | 100 |
| 10) The course length is appropriate. | 100 | 100 | 100 |
| 11) The venue is appropriate and well organised. | 100 | 100 | 100 |
| 12) Overall quality of the course is good and recommended. | 100 | 100 | 100 |
| 13) You are willing to teach next time. | 96 | 100 | 99 |
| Overall | 99 | 99 | 99 |
PR%, positive response percentage.
Qualitative feedback
On top of rating scores, instructors from both isolation and general ward expressed their appreciation of teamwork, communication and support from all involved departments. They reflected on observations and correction of learners’ non-adherence to hospital recommendation on doffing of PPE just in time before actual outcome. Learners and instructors recognised the importance of on-site support from Infection Control Teams to respond with professional advice, especially on standard procedures of donning and doffing of PPE and proper case transfer management. Under evolving conditions of the pandemic, learners unanimously agreed that their knowledge, skills and confidence were greatly enhanced by the training.
Insight from debriefing sessions
Post-training debriefing session served as an open discussion platform to incorporate bidirectional opinions into the standard airway management and infection control practice for endotracheal intubation in adult patients with COVID-19. Examples of reflection included: (1) proper hairdressing to avoid breaching infection control principles in doffing of PPE, (2) clarification of handling clinical waste for patients with COVID-19 in different clinical areas, (3) minimised circuit disconnection by preconnecting the bag-mask device or ventilator circuit with necessary components like viral/bacterial filter and closed circuit suction set; (4) putting prepacked resuscitation items on top of emergency-trolley in general ward and keeping one defibrillator in non-clean zone; and (5) raised staff awareness of how proper donning and doffing of PPE could build up patient safety climate from personal level to community level. Some of these opinions and feedbacks were conveyed to stakeholders, which were adopted and integrated into the standards of clinical practice.
Discussion
COVID-19 pandemic has struck almost every part of the world with heavy casualties. The impact is colossal with faster, wider and deeper spread compared with SARS. It has also imposed tremendous burden on healthcare system in different countries. Millions of people have been infected and thousands have succumbed. Hong Kong is one of the first batches of affected regions. Up to 12 August 2020, Hong Kong has recorded more than 4200 confirmed cases with 58 deaths after 6 months. HCWs are the highest risk profession due to nosocomial transmission. In the USA, over 130 000 HCWs are infected with reported death over 600.19 Over 600 nurses died from COVID-19 worldwide.20 Every single HCW occupationally acquired COVID-19 was demoralising and was a dangerous source of nosocomial spread to other hospital patients and staff. SARS-CoV-2 was transmitted in hospitals through contact, respiratory droplet spread as well as certain aerosol-generating procedures. With the agonising SARS experience and the initial inconspicuous nature of this COVID-19, our hospital decided to prepare early for the anticipation of COVID-19 disease. Training was one of the best approaches to engage and mobilise staff, to standardise our practice and to effectively use our resources within the tight time constraint. Our hospital adopted the just-in-time simulation training, enabling healthcare workers to rehearse infection control measures and entire workflow in teams prior to performing aerosol-generating procedures with confirmed or suspended COVID-19 patients in designated wards.21
We decided to strengthen our staff preparedness and process through high-fidelity simulation training. Simulation provides an opportunity for deliberate practice in a safe environment.18 It can rapidly facilitate hospital preparation and education of large number of HCWs with proven values.3 13 A ‘relatively small’ amount of education with the correct and well-chosen objectives was believed to be associated with a significant increase in adherence to infection control practice and provide safety benefits.11 22 The workforce capacity, workflow logistics and processes can be optimised through simulation training even in healthcare organisation under pressure.13. In 6 weeks’ time, a large group of staff from both high risk and general ward areas were trained up with standard infection control and endotracheal intubation practice guidelines under clear role delineation to scale up the workforce. American Heart Association recently complied and published an interim guidance to address the gap in its cardiopulmonary resuscitation guidelines for providing resuscitation of patients with COVID-19.23 Most, if not all, of its recommended new measures echo our hospital intubation protocol for patients with COVID-19 released in February.
Policy and guidelines that were well planned and well written must combine with appropriate training to achieve optimal effect. A study of questionnaires from HCWs who performed endotracheal intubation in SARS revealed that staff concerns changed over time.15 Staff concerns gradually shift from the need for PPE to the need for better training and patient care protocols. HCWs also perceived that their experiences were ineffectively integrated into guidelines and protocols. The participating HCWs in our training programme were encouraged to provide feedback to policy makers on the protocols and treatment guidelines in the debriefing. In this way, their valuable experience and input were rapidly incorporated into treatment guidelines for endotracheal intubation of patients with COVID-19. As a result, learners showed high positive rating percentage in the post-training evaluation.
Three training objectives were met: first, reinforce proper infection control practice; second, contain contamination of staff, environment and equipment; and third, minimise HCWs exposure to highly infectious SARS-CoV-2 during endotracheal intubation for patients with COVID-19. Patients were cared by Parent and Central Resuscitation Teams with close communication for this emergency procedure. Up to early Aug 2020, of the 377 patients with COVID-19 admitted into QEH, 35 were intubated due to critical conditions from collected data of A&E, ICU and Anaesthesiology & Operation Threatre Services department. All intubation adopted the workflow and practice being taught in the training programme. The feedback from the Parent Team staff, Central Resuscitation Team members and ICU colleagues were positive, and they had great confidence in adopting the protocol that gave them great sense of safety. According to compilation of hospital statistics from the ICU as of 10 August 2020, there were no adverse events reported on intubation procedures after training. So far, no single HCW in our hospital has acquired COVID-19 through nosocomial transmission.
The arts of scenario design: how different context affects the way the scenario is set up?
There are discrepancies between airway management in isolation ward in different contexts when a standard workflow and protocol is applied as indicated in online supplemental appendix A (see 3. Indications and location of intubation). For example, intubation procedures (and application of high-flow oxygen therapy) is not recommended in general ward for patient with suspected nCoV infection. Subsequent arrangement and preparative procedures for patient transfer from general ward to isolation ward would specifically apply to simulation training for ‘general wards’. Such procedures have been included in the set-up of simulation scenarios (see online supplemental appendix B, P.2 scenarios and P.3 checklist remarks).
Any differences in staff perception on simulation training, in terms of ‘mode’ and ‘role’?
Our study found that there was no significant difference in staff perception between modes of in situ and lab-based simulation. Regardless of mode of simulation training and clinical backgrounds, most participants felt satisfied with the simulation training, in terms of training needs (91%), training design (90%), simulation (88%), debriefing (91%) and instructor feedback (89%).
In order to facilitate learning and reflective process in relatively passive role, staff proficiency checklists were distributed to all observers in advance (see online supplemental appendix C). Observers involved in scenario-based simulation and subsequent debriefing session could gain insights from the scenario and enhanced knowledge as much as their counterparts by reflecting on their observation and enhance personal experience in clinical setting.
bmjstel-2020-000766supp003.pdf (46.3KB, pdf)
Distribution of in situ and lab-based simulation: golden ratio or by chance?
The distribution of 2/3 in simulation lab and 1/3 in real workplace resulted from maximum capacities in operating simulation training within 6-week duration. To take all factors, such as operation needs, manpower issues, availability of training venues and clinical safety into considerations, the training programme task group decided to implement some management strategies:
Use parallel mode of simulation (lab-based and in situ).
Accept quotas for observers.
At the time of planning phase of simulation training, A&E and ICU staff have already been occupied with clinical duties, whereas staff from other departments were awaiting rotation to isolation ward and/or change of ward setting to suspected cases of COVID-19. For A&E and ICU training, in situ simulation could achieve the highest degree of environmental fidelity and provide optimal flexibility for instructors and trainees based on their availability. For training of general ward and isolation ward, simulation lab was considered as an appropriate venue that could balance the risk of infection and occupancy of clinical operation.
Training effect of healthcare simulation on organisation sustainability
Our simulation training centre and Central Nursing Division were able to rapidly mobilise and conduct appropriate hospital-based training courses to cover a large proportion of relevant hospital staff within a 6-week period. This type of response is not possible without an investment in simulation educators, technicians and robust simulation infrastructure. The training outcome speaks to the value and benefits of the simulation training centre to the organisation. Healthcare simulation had also been used in several healthcare organisations and training centres to evaluate the preparedness in their institutions during the Ebola crisis.10 It can be one of the organisational factors, which may improve safety climate in healthcare setting and help the hospital management advance service quality by sharpening the focus on patient and system outcomes.
Based on our experience of using simulation for training and modification of the process, we summarise a recommendation list to be considered when faced with an acute need for simulation in a disaster preparedness situation (box 1). ‘Box 1. 4. Implementation of Post-training measures’ served as sustainable measures following the simulation training, including balance between needs/manpower issues and demonstration videos accessible by staff. On top of captioned measures, Central Nursing Division used regular cardiopulmonary resuscitation drills (with checklist regarding PPE proficiency, N95 and hand hygiene) to remind staff of skills related to patients with COVID-19. The retaining intervals for infection control related refreshing course were 2 years.
Box 1. Summary of change in strengthening of existing procedures and preparedness plan for COVID-19 pandemic after simulation training.
-
Reinforce Infection control practice to improve staff personal protection knowledge and skills
Correct personal protective equipment (PPE) donning and choose right equipment (like video-laryngoscope) before procedure.
Proper PPE doffing sequence of contaminated PPE after procedure.
Understand the importance of buddy system and mutual protection during the procedure.
Unify the minor variations of different practice for high-risk aerosol-generating procedures in different clinical areas into one standard infection control practice.
-
Contain contamination by reorganising workflow process
Formulate guidelines ‘Measures for Intubation in General Ward/AIIR during nCoV Period’ for emergency endotracheal intubation by Department of Anaesthesiology & Operation Theatre Services.
Consolidate workflow for intensive care unit (ICU) transfer of intubated patients to minimise transit time and contamination.
Minimise circuit disconnection by preconnection of the bag-mask device or ventilator circuit with necessary components like viral/bacterial filter and closed circuit suction set.
Segregate equipment from clean and non-clean zones to reduce environmental contamination.
-
Minimise staff exposure by designation of team work
Familiarise designated roles and responsibilities of Parent Team and Central Resuscitation Team in the procedure.
Early recognition of deteriorating patient with COVID-19 by Parent Team to alert Central Resuscitation Team and ICU of potential endotracheal intubation for more preparatory time and lower the risk of transmission.15
Central Resuscitation Team led by an experienced anaesthesiologist specialist for intubation to minimise the number of attempts and exposure time.
Active and backup team assigned to limit the number of healthcare workers and avoid unnecessary exposure.
-
Implementation of post-training measures
Follow up with feedback from frontline staff during debriefing session.
Organise additional COVID-19 related in situ multipurpose simulation training coordinated by senior nurse management.
Arrange in situ simulation drills for newly converted isolation ward following the increasing service needs, supported by hospital Quality & Safety Department and Central Resuscitation Team.
Prepare video clips on COVID-19 proper doffing procedures and endotracheal intubation on hospital intranet accessible to all hospital staff for review and refreshment.
Strengthen accountability of clinical staff in general practice by promoting the culture that ‘Proper donning and doffing of PPE is every staff responsibility to protect themselves, to protect colleagues, to protect patients, to protect family and community’.
-
Practical tips for effective COVID-19 simulation training
Summon relevant stakeholders and experts of the field early to form a multidisciplinary task group.
Initiate planning of high-fidelity simulation training of infectious disease protocol and practice as an invaluable asset for staff and patient safety in early phase of the outbreak.
Identify gap of existing practice based on empirical evidence from literature search, expert opinions and/or root-cause analysis (if applicable).
Stay focus on limited number of well-defined dangerous procedure(s) and its associated workflow(s).
Take individual and team work, knowledge and skills, complex and context-specific system issues,24 safety issues of the patients and healthcare professionals into accounts.
Anticipate a number of days needed to train enough staff for a critical mass to achieve a reasonable impact on staff empowerment.
Listen to the learners as they usually have the solutions for their issues. Collective wisdom is important in this kind of challenge.
Allow over time for debriefing session to address learners’ level of anxiety, concerns for their own safety and direct relevant questions to Infection Control Team.
Mitigate HCWs’ pressure and emotional stress by acknowledging their concerns and building sense of being supported and protected in work environment.
Act as a bridge to bring the learners’ feedback to senior management for consideration, follow-up and incorporate into protocol if appropriate.
Engage staff into the preparation and implementation phase of new measures or protocols if possible.
Limitations
Under frequent staff rotation and heavy clinical duty of HCWs handling patients with COVID-19, obtaining post-training feedback from participants through structured interview and focus group became unfeasible. With restrictive time for planning of simulation training in 1 week and clinical duty of both participants and instructors, no formal qualitative analysis with anecdotes or themes were conducted, not to mention structural debriefing models. There was no specific model of debriefing considered in the planning phase, given all instructors are quite experienced in healthcare simulation education.
Without formal structured interview or focus group for content analysis, we have only drawn meaningful feedback from open-ended questions, shared opinions during debriefing sessions and informal responses from trained staff who had performed intubation with patients with COVID-19 by the authors under limited time, resources and infection control measures. In addition, post-training feedback from the Parent Team staff, Central Resuscitation Team members and ICU colleagues were collected informally via Department Operation Manager Meeting and Quality & Safety forum with staff at all levels and added to summary table at the back of this paper.
Regarding quantitative analysis on simulation training, results were based on self-report questionnaire from participants, which may be subjective at certain time point. They could neither evaluate the degree of change in knowledge and skills just after the training nor track the translational effect of clinical effectiveness on high-risk procedures in real clinical practice. Owing to anonymity in rating for all active participants and observers, we could no longer be possible to differentiate their identity in data analysis. Therefore, we have no way to verify whether two populations were homogeneous through subgroup analysis.
Fourthly, healthcare simulation training is only one of all aspects in strengthening preparedness yet connecting frontline worker with up-to-date knowledge and closing gap of knowledge and skills. Ongoing monitoring by proficiency assessment of infection control teams is not feasible when hospital service retained normalcy on and off among waves of COVID-19 pandemic. Accountability for monitoring clinical outcomes and safety issues were shouldered by respective departments, not by coordinators of simulation training.
Lastly, the service flow or procedure change of COVID-19 management could not be evaluated through our training because the main purpose of our simulation was for education, not for ‘stress test’. Other research questions beyond service workflow, such as gadgets for airway intervention using florescence stain to visualise spread of virus, could not be examined through this study as well.
Conclusions
Under the COVID-19 pandemic threat, we have demonstrated how simulation-based training contributed significantly to prepare the hospital staff, strengthen the protocols and workflow for endotracheal intubation as part of our hospital response plan. The programme has trained 1415 hospital HCWs (~81% of target participants with training needs) with overall positive feedback within limited time frame. There was zero nosocomial transmission to HCWs during subsequent endotracheal intubation of patients with COVID-19. The insight and experience gained from this training programme is valuable for future infectious disease challenges.
bmjstel-2020-000766supp004.pdf (98.7KB, pdf)
Acknowledgments
We would like to express our gratitude to the Hospital Authority Head Office and Queen Elizabeth Hospital top management for their operational support to simulation training: Quality & Safety Department for their initiation for workforce establishment; Infection Control Teams, especially Ms S Y Lee, Mr W K Lo and Ms Naomi Yeung, for their knowledge in up-to-date infection control standards; Central Nursing Division for overall coordination and scenario proposal; Resuscitation Committee, especially Dr K C Lui, for formulation of standard algorithm of aerosol-generating procedures and other high-risk procedures; and all administrative and technical staff members in Multi-disciplinary Simulation and Skills Centre for their active involvement and intellectual input in converting conceptual ideas into feasible plan throughout the training and data management processes.
Footnotes
Collaborators: Eric H K So, N H Chia, George W Y Ng, Osburga P K Chan, S L Yuen, David C Lung, W C Li, S S So and Victor K L Cheung.
Contributors: Conceptualisation: all authors. Methodology: EHKS, NHC, GWYN, SLY, SSS and VC. Software: EHKS, SLY, SSS and VC. Validation: all authors. Formal analysis: EHKS, SLY, SSS and VC. Investigation: EHKS, SLY, SSS and VC. Resources: SLY, SSS and VC. Data curation: EHKS, SLY, SSS and VC. Writing – original draft preparation: EHKS, SLY, SSS and VC. Writing – review and editing: all authors. Visualisation: VC. Supervision: EHKS, NHC and GWYN. Project administration: SSS and VC. Funding acquisition: EHKS, NHC, GWYN and SSS. All authors have read and agreed to the published version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
The data of this study are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
For review on training on education purpose, ethical approval from institutional research ethics committee is not required.
References
- 1. World Health Organisation . Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. Available: https://www.who.int/csr/sars/country/table2004_04_21/en/ [Accessed 08 Apr 2020].
- 2. Yuen KY. The SARS attack on Hong Kong. Hong Kong Med J 2003;9:302–3. [PubMed] [Google Scholar]
- 3. Abrahamson SD, Canzian S, Brunet F. Using simulation for training and to change protocol during the outbreak of severe acute respiratory syndrome. Crit Care 2006;10:R3. 10.1186/cc3916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chopra V, Gesink BJ, de Jong J, et al. Does training on an anaesthesia simulator lead to improvement in performance? Br J Anaesth 1994;73:293–7. 10.1093/bja/73.3.293 [DOI] [PubMed] [Google Scholar]
- 5. Holcomb JB, Dumire RD, Crommett JW, et al. Evaluation of trauma team performance using an advanced human patient simulator for resuscitation training. J Trauma 2002;52:1078–86. 10.1097/00005373-200206000-00009 [DOI] [PubMed] [Google Scholar]
- 6. Howard SK, Gaba DM, Fish KJ, et al. Anesthesia crisis resource management training: teaching anesthesiologists to handle critical incidents. Aviat Space Environ Med 1992;63:763–70. [PubMed] [Google Scholar]
- 7. Larbuisson R, Pendeville P, Nyssen AS, et al. Use of anaesthesia simulator: initial impressions of its use in two Belgian university centers. Acta Anaesthesiol Belg 1999;50:87–93. [PubMed] [Google Scholar]
- 8. Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev 1993;100:363–406. 10.1037/0033-295X.100.3.363 [DOI] [Google Scholar]
- 9. Dieckmann P, Torgeirsen K, Qvindesland SA, et al. The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: practical tips and resources from Norway, Denmark, and the UK. Adv Simul 2020;5:3. 10.1186/s41077-020-00121-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Biddell EA, Vandersall BL, Bailes SA, et al. Use of simulation to gauge preparedness for Ebola at a free-standing children's Hospital. Simul Healthc 2016;11:94–9. 10.1097/SIH.0000000000000134 [DOI] [PubMed] [Google Scholar]
- 11. Raboud J, Shigayeva A, McGeer A, et al. Risk factors for SARS transmission from patients requiring intubation: a multicentre investigation in Toronto, Canada. PLoS One 2010;5:e10717. 10.1371/journal.pone.0010717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tran K, Cimon K, Severn M, et al. Aerosol-generating procedures and risk of transmission of acute respiratory infections: a systematic review. CADTH Technol Overv 2013;3:e3101. [PMC free article] [PubMed] [Google Scholar]
- 13. World Health Organisation . Infection prevention and control of Epidemic- and Pandemic-Prone acute respiratory infections in health care. Available: https://www.who.int/csr/bioriskreduction/infection_control/publication/en/ [Accessed 08 May 2020]. [PubMed]
- 14. Christian MD, Loutfy M, McDonald LC, et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect Dis 2004;10:287–93. 10.3201/eid1002.030700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Caputo KM, Byrick R, Chapman MG, et al. Intubation of SARS patients: infection and perspectives of healthcare workers. Can J Anaesth 2006;53:122–9. 10.1007/BF03021815 [DOI] [PubMed] [Google Scholar]
- 16. World Health Organisation . Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance, 28 January 2020, 2020. Available: https://apps.who.int/iris/handle/10665/330893 [Accessed 01 Jun 2020].
- 17. Hospital Authority . HAHO infection control guideline and toolkit, 2020. Available: https://www.ha.org.hk/haho/ho/pad/Comkit.pdf [Accessed 08 May 2020].
- 18. Society for Simulation in Healthcare . Accreditation standards, 2016. Available: https://www.ssih.org/Credentialing/Accreditation/Full-Accreditation [Accessed 11 Mar 2021].
- 19. Centers for Disease Control and Prevention (CDC) . Cases in the US. Available: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html [Accessed 12 Aug 2020].
- 20. International Council of Nurses (ICN) . More than 600 nurses die from COVID-19 worldwide. Available: https://www.icn.ch/news/more-600-nurses-die-covid-19-worldwide [Accessed 01 Jun 2020].
- 21. Agency for the Healthcare Research and Quality . Healthcare simulation dictionary, 2020. Available: https://www.ahrq.gov/news/second-edition-healthcare-simulation-dictionary.html [Accessed 11 Mar 2021].
- 22. Shigayeva A, Green K, Raboud JM, et al. Factors associated with critical-care healthcare workers' adherence to recommended barrier precautions during the Toronto severe acute respiratory syndrome outbreak. Infect Control Hosp Epidemiol 2007;28:1275–83. 10.1086/521661 [DOI] [PubMed] [Google Scholar]
- 23. Edelson DP, Sasson C, Chan PS, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care Committee and get with the Guidelines-Resuscitation adult and pediatric task forces of the American heart association. Circulation 2020;141:e933–43. 10.1161/CIRCULATIONAHA.120.047463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brazil V. Translational simulation: not 'where?' but 'why?' A functional view of in situ simulation. Adv Simul 2017;2:20. 10.1186/s41077-017-0052-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjstel-2020-000766supp001.pdf (78.7KB, pdf)
bmjstel-2020-000766supp002.pdf (295.1KB, pdf)
bmjstel-2020-000766supp003.pdf (46.3KB, pdf)
bmjstel-2020-000766supp004.pdf (98.7KB, pdf)
Data Availability Statement
The data of this study are available from the corresponding author on reasonable request.