Abstract
This study is aimed to compare whole-spine lateral radiograph (WLR) and cervical lateral radiograph (CLR) in terms of T1 slope visibility and cervical sagittal parameters and to identify the superior imaging modality for assessment of cervical sagittal parameters.
We retrospectively reviewed the radiographic data of 60 consecutive adult patients (male-to-female ratio, 38:22; mean age, 55.6 ± 1.3 years) who presented with only neck pain (without radiculopathy or myelopathy). All the patients underwent standing CLR and WLR. The following parameters were measured and analyzed:
-
1.
T1 slope visibility,
-
2.
T1 slope,
-
3.
C7 slope,
-
4.
C0–C2 Cobb angle (CAC0–C2),
-
5.
C2–C7 Cobb angle (CAC2–C7), and
-
6.
cervical sagittal vertical axis (cSVA).
The visibility of the T1 slope was significantly lower with WLR than with CLR (28.3% vs 83.3%, P = .049). The mean CAC2–C7 on WLR was significantly less lordotic than that on CLR (11.2 ± 9.2° vs 14.3 ± 11.3°; P = .01). The mean cSVA was translated more posteriorly on WLR than on CLR (9.9 ± 18.9 mm vs 15.0 ± 13.4 mm, P = .04). However, no significant differences in T1 slope, C7 slope, and CAC0–C2 were found between CLR and WLR.
This study shows that standing CLR could provide better visualization of the upper endplate of T1. Furthermore, WLR taken in hands on clavicle position distorted radiographic measurements such as CAC2-C7 and cSVA. Therefore, CLR performed in the standing position seems to allow more-accurate measurements of cervical sagittal parameters.
Keywords: cervical lateral radiograph, cervical sagittal alignment, T1 slope, whole spine lateral radiograph
1. Introduction
Standing whole-spine lateral radiograph (WLR) is an essential imaging modality for evaluating global spine sagittal alignment. It is also commonly used to evaluate cervical sagittal parameters.[1–5] Among the many arm positions used during WLR imaging, the hands-on-clavicle position is the most widely applied position, as it provides the best visualization of thoracolumbar spine and can minimize position-related distortion of the thoracolumbar sagittal parameters. However, WLR in the hands-on-clavicle position has limitations for evaluating cervical sagittal alignment. The T1 slope, a key influencing factor of cervical sagittal balance, is frequently obscured by the shoulder and thoracic trunk in the hands-on-clavicle position.[6] The hands-on-clavicle position has been reported to distort the T1 slope, head position, or cervical lordosis, which limits its capacity to measure accurate cervical sagittal parameters.[7]
Besides WLR, cervical lateral radiograph (CLR) with arms in the neutral position (hands-on-thigh position) is another commonly used imaging modality to assess cervical sagittal parameters.[7] Although a few studies have evaluated the differences in cervical sagittal parameters between WLR and CLR, no consensus has been reached regarding the optimal position during imaging for cervical sagittal parameter measurement.[7–9] Moreover, visibility of T1 which is an important factor in operative planning, has not been compared between the two imaging methods.
Whether CLR can replace WLR completely for cervical sagittal parameter assessment with regard to visibility and accuracy or WLR would provide additional information has not been clarified. Therefore, the present study aimed to evaluate differences in T1 upper endplate visibility and various cervical sagittal parameters measured on WLR and CLR and to clarify which imaging modality provides better information in the assessment of cervical sagittal alignment.
2. Materials and methods
2.1. Patient characteristics and study design
Sixty consecutive patients who visited the outpatient clinic between July 2017 and March 2018 for axial neck pain alone without radiculopathy or myelopathy were retrospectively evaluated. The study protocol was approved by institutional review board of Asan Medical Center (2018-0942). Informed consent was waived owing to the retrospective nature of the study. Patients who had undergone previous spine operations or diagnosed with spine deformities have been excluded. All the patients underwent both standing CLR and WLR for evaluating regional and global spinal balance. T1 visibility, sagittal parameters measured in WLR were compared with those measured in CLR.
2.2. Data collection
CLR was performed with the patient standing in a comfortable position with horizontal gaze and arms extended to the sides. The radiation tube was centered at the disc space between C4 and C5. WLR was performed in the hand-on-clavicle position with flexed elbows and wrists, and relaxed fists and fingers placed in the supraclavicular fossa. The radiation tube was centered at the xyphoid process during WLR (Figure 1).
Figure 1.
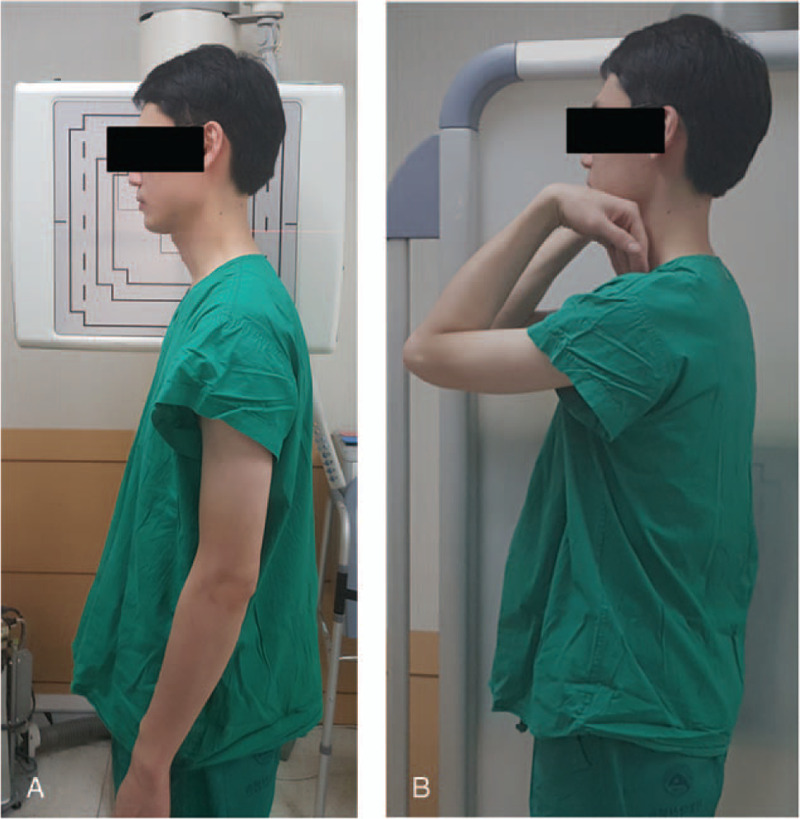
Cervical lateral radiograph obtained in a comfortable standing position with horizontal gaze and arms extended to the sides (A) and whole-spine lateral radiograph obtained in the hand-on-clavicle position with the elbows and wrist flexed, the fist relaxed, and the fingers placed into the supraclavicular fossa. Adopted from Society 20 Suppl 5:602–608. doi:10.1007/s00586-011-1927-y.
The following parameters were measured on CLR and WLR:
-
1.
T1 slope visibility,
-
2.
T1 slope,
-
3.
C7 slope,
-
4.
C0–C2 Cobb angle (CAC0–C2),
-
5.
C2–C7 Cobb angle (CAC2–C7), and
-
6.
cervical sagittal vertical axis (cSVA).
The radiographic measurements were performed by two spine fellowship-trained orthopedic surgeons.
The visibility of the T1 slope was determined according to the visibility of the T1 superior endplate. Visibility was defined as a clearly visible T1 superior endplate or sufficient visibility of part of the endplate for drawing a line. Non-visibility was defined as a T1 superior endplate obscured by surrounding structures (Figure 2). T1 slope was defined as the angle between a horizontal line and a line parallel to the superior endplate of T1. C7 slope was defined as the angle between a horizontal line and the C7 superior endplate. CAC0–C2 was defined as the angle between two lines on the inferior endplates of C0 and C2 that are extended until they intersect. CAC2–C7 was defined as the angle between two lines on the inferior endplates of C2 and C7 that are extended until they intersect. cSVA was defined as the horizontal distance between the centers of C2 and the C7 vertebral body (Figure 3).
Figure 2.
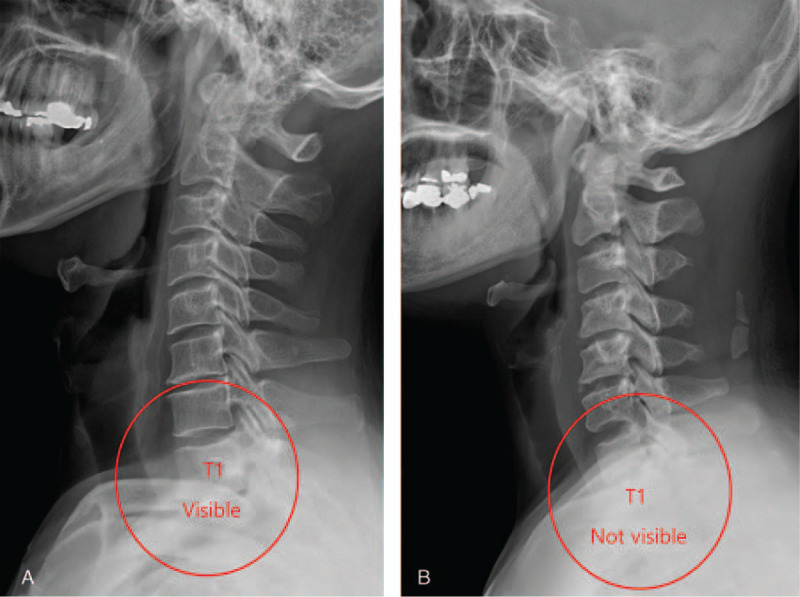
(A) T1 slope visible on the cervical spine lateral radiograph. (B) T1 slope not visible on the whole-spine lateral radiograph.
Figure 3.
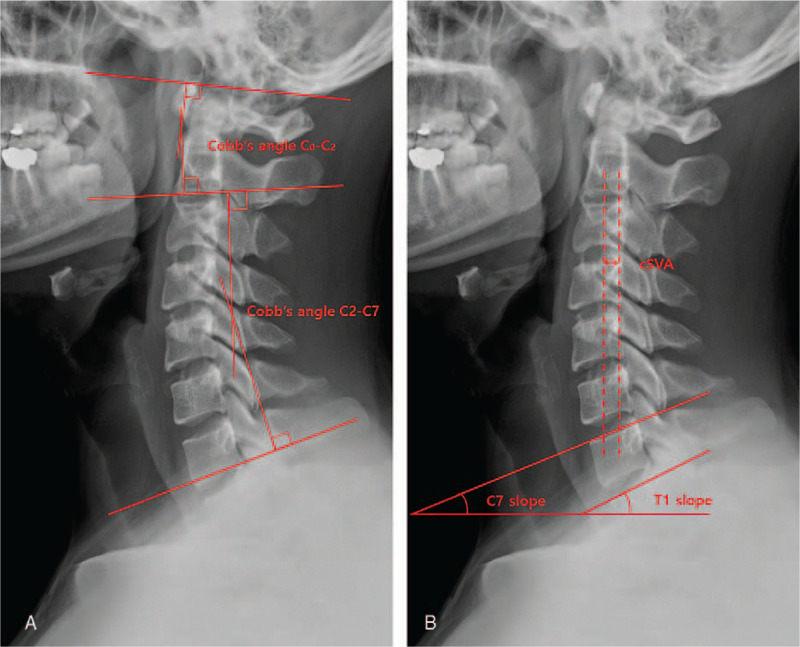
Schematic drawing of the parameters. Radiograph showing several sagittal parameters measured in this study: CAC0–C2: angle between two lines on the inferior endplates of C0 and C2 that are extended until they intersect. CAC2–C7: angle between two lines on the inferior endplates of C2 and C7 that are extended until they intersect (A). T1-slope: angle between a horizontal line and a line parallel to the superior endplate of T1. C7 slope: angle between a horizontal line and the C7 upper endplate. cSVA: horizontal distance between the centers of C2 and C7 vertebral body (B).
2.3. Statistical analyses
Data management and statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 18.0; SPSS Inc., Chicago, IL, USA). The visibility of the T1 slope was analyzed using a chi-square test, while the T1 slope, C7 slope, CAC0–C2, and CAC2–C7 were analyzed using a Student t test. The interobserver reliability was calculated using the intraclass correlation coefficient (ICC) for the cervical sagittal parameters and the kappa test for T1 upper endplate visibility. A P-value of < .05 was considered statistically significant.
3. Results
The study included 38 men (63.3%) and 22 women (36.7%). The mean age of the patients was 55.6 years (range, 36–75 years). The interobserver reliability for sagittal parameter measurement based on the ICC was 0.836. The kappa coefficient for the interobserver reliability of the T1 upper endplate visibility was 0.825.
On CLR, the T1 endplate was visible in 83.3% (50/60) of the patients but not clearly identifiable in 17.6% (10/60). On WLR, the T1 endplate was visible in only 28.3% (17/60) of the patients but not identifiable in 71.7% (43/60). The visibility rate of the T1 slope was significantly higher with CLR than with WLR (28.3% vs 83.3%, P = .049; Table 1).
Table 1.
Visibility rates of the T1 endplate on radiography.
| Visible | Invisible | P value | |
| Cervical spine lateral radiography | 83.3% (50/60) | 16.7% (10/60) | .049∗ |
| Whole-spine lateral radiography | 28.3% (17/60) | 71.7% (43/60) |
The T1 slopes on CLR and WLR were 22.82 ± 6.37o and 21.29 ± 5.01o, respectively (P = .161). The C7 slopes on CLR and WLR were 18.79 ± 6.84o and 18.35 ± 7.63o, respectively (P = .681). No significant differences in T1 and C7 slopes were found between the measurements using CLR and WLR. Furthermore, there were no significant difference in CAC0–C2 measured on CLR (15.58 ± 9.31o) and WLR (16.14 ± 9.65o) (P = .580). The CAC2–C7 on CLR and WLR were 14.73 ± 11.31o and 11.20 ± 9.24o, respectively. The CAC2–C7 on WLR in the hands-on-clavicle position was significantly less lordotic than that on CLR with the arms extended (P = .01). The cSVA on CLR and WLR were 14.96 ± 13.44 mm and 9.92 ± 18.86 mm, respectively. The sagittal balance of the cervical spine measured using cSVA was more translated posteriorly on WLR than on CLR (P = .040, Table 2).
Table 2.
Comparison of the parameters measured on cervical spine lateral radiography and whole-spine lateral radiography.
| CLR | WLR | P values | |
| T1 slope (°) | 22.82 ± 6.37 | 21.29 ± 5.01 | .161 |
| C7 slope (°) | 18.79 ± 6.84 | 18.35 ± 7.63 | .681 |
| C0–C2 Cobb angle (°) | 15.58 ± 9.31 | 16.14 ± 9.65 | .580 |
| C2–C7 Cobb angle (°) | 14.73 ± 11.31 | 11.20 ± 9.24 | <.001∗ |
| Cervical sagittal vertical axis (mm) | 14.96 ± 13.44 | 9.92 ± 18.86 | .040∗ |
4. Discussion
Spine sagittal global imbalance is associated with pain, disability, and deterioration of health-related quality of life.[10,11] Moreover, increasing evidence suggests that cervical sagittal malalignment can lead to increased neck pain and poor neurological recovery after decompressive operations.[6,12] Many parameters have been studied, including T1 slope, C7 slope, cSVA, and Cobb's angle, that can aid in operation planning and predicting prognosis and accurate assessment of these parameters would lead to appropriate clinical decision. However, although CLR and WLR are the two most common radiographic modalities utilized to assess cervical sagittal alignment, the optimal radiological protocol for accurate assessment has not been clarified.
Among the parameters, the T1 slope suggested by Knot et al is one of the most commonly assessed sagittal parameters of the cervical spine during preoperative planning.[2,13] However, assessment of the T1 slope has some drawbacks. First, it can be distorted depending on the arm position. Several studies have evaluated whether the hands-on-clavicle or arm-clearing position is better for visualizing the thoracic and lumbar spine and reflecting the actual spine global balance on WLR.[14–16] However, the T1 slope has often differed between the two positions.[7,9] Park et al reported that the hands-on-clavicle position on WLR caused the T1 slope to decrease and the head position to translate posteriorly, which resulted in cervical sagittal alignment distortion into a hypo-lordotic or kyphotic alignment to compensate for the gravity line and sustain the horizontal gaze.[9] Furthermore, in WLR, the tube center is usually at the xiphoid process, which is more distant from T1 and the cervical spine than in CLR, in which the tube is at the C4–C5 level; this results in a distortion of the cervical spine area because of beam divergence.[17] Previous studies reported that the T1 slope was smaller on WLR than on CLR owing to the above-mentioned reasons.[7,9] The results of the present study also demonstrated decreases in the T1 and C7 slopes on WLR as compared with CLR, although the difference was not statistically significant.
Second, the T1 upper endplate is frequently obscured by the shoulder and thoracic trunk, which limits its measurement.[8,18] Therefore, research data using the T1 slope commonly depend on the poorly visible T1 upper endplate on lateral radiographs.[19,20] The passive flexion of the shoulder required in the hands-on-clavicle position for WLR often causes the shoulder to migrate upward, which would further obscure the T1 upper endplate.[16,21,22] Although Nunez et al proposed the use of the C7 slope to overcome the limitations of the T1 slope,[23] whether the C7 slope is more likely to be visible than the T1 slope is unclear, and few studies have examined the relationship between the C7 slope and other cervical parameters.[24–26] In the present study, the T1 visibility reached 83.3% when assessed on CLR and 28.3% when assessed using WLR, signifying that the T1 slope would be more accurately measured using CLR. Koji et al reported 37% T1 slope visibility on CLR in the sitting position, which is rather low when compared with the results of the present study.[24] The difference could have been caused by the difference in position between the two studies. Hwee et al reported that gravity applied to the center of the head in sitting CLR results in a more forward translation of the head and that increased cervical lordosis is needed to maintain the horizontal gaze.[27] Increased cervical lordosis would also increase the T1 slope, and a more vertically positioned T1 upper endplate would be easily obscured by surrounding structures. Therefore, during lateral radiography, the standing position with arms extended would be a better position to assess the T1 slope compared to sitting position.
CAC2–C7 and cSVA measured on WLR were significantly different from those measured on CLR, signifying a hypolordotic change and posterior migration of the cervical alignment in the hands-on-clavicle position in WLR. These findings were also demonstrated in the study by Park et al.[9] It seems that true cervical sagittal alignment should be assessed using CLR since hands on clavicle position utilized for WLR causes significant distortion in sagittal parameter measurements.
To summarize, CLR seems to have several advantages over WLR in the assessment of cervical sagittal alignment parameters. CLR is performed with the patient's arm extended to the sides. This would minimize the change in the cervical sagittal parameters such as decrease in lordosis and posterior translation of sagittal balance caused by the hands-on-clavicle position required in WLR. Furthermore, the radiation beam is centered at the cervical spine to limit the distortion caused by divergence.[17] Moreover, CLR performed while the patient is in the standing position with arm extended provides the best T1 upper endplate visibility as demonstrated in the present study, thereby allowing accurate assessment of the T1 slope. These findings suggest that CLR in the standing position with arms extended to the sides would be the single best imaging modality when cervical sagittal alignments are the measurements of interest. WLR would provide additional information regarding thoracolumbar alignment and its relationship to cervical spine. However, WLR does not add to the assessment of cervical sagittal parameters because of position- and beam divergence-related distortion and invisibility of the T1 slope.
Our study has several limitations. First, it was not conducted with healthy, symptom-free patients. Although the patients did not have an underlying deformity or myeloradiculopathy, neck pain would have possibly affected the cervical sagittal parameters. Second, the present study was conducted with a relatively small sample size. Third, we did not consider the sagittal parameters of the thoracic and lumbar spine and their relationships to cervical sagittal parameters.
In conclusion, T1 visibility was significantly higher on CLR than on WLR. Furthermore, CAC2–C7 and cSVA were significantly greater when measured using CLR, signifying the position- and radiation divergence-related distortions in WLR. CLR performed in the standing position with arms extended seems to allow more-accurate measurements of cervical sagittal parameters. Therefore, CLR would be a better radiographic modality than WLR to assess cervical sagittal alignment in terms of accuracy and visibility. Repeated WLR would not be necessary for evaluation unless accompanying thoracolumbar spine lesions are found in the initial examination.
Acknowledgments
We thank to Mi Young Lee and So Jeong Yoon for their assistance in data collection.
Author contributions
Conceptualization: Dong-Ho Lee.
Data curation: Dong-Ho Lee, Sehan Park, Dong Gyun Kim, Choon Sung Lee, Eui Seung Hwang.
Investigation: Dong-Ho Lee, Sehan Park, Dong Gyun Kim.
Methodology: Dong-Ho Lee, Dong Gyun Kim, Chang Ju Hwang, Jae Hwan Cho.
Project administration: Dong-Ho Lee.
Formal analysis: Sehan Park.
Software: Sehan Park.
Footnotes
Abbreviations: CAC0–C2 = C0–C2 Cobb angle, CAC2–C7 = C2–C7 Cobb angle, cSVA = cervical sagittal vertical axis, CLR = Cervical lateral radiograph, WLR = whole-spine lateral radiograph.
How to cite this article: Lee DH, Park S, Kim DG, Hwang CJ, Lee CS, Hwang ES, Cho JH. Cervical spine lateral radiograph versus whole spine lateral radiograph: A retrospective comparative study to identify a better modality to assess cervical sagittal alignment. Medicine. 2021;100:21(e25987).
This study was not supported by external funding.
All authors do not have any conflicts of interest to declare,
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Statistical analysis was performed using a chi-square test.
P value < .05
CLR, cervical lateral radiography; WLR, whole spine lateral radiography. Statistical analysis was performed using the Student t test.
P value < .05
References
- [1].Hardacker JW, Shuford RF, Capicotto PN, Pryor PW. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976) 1997;22:1472–80. discussion 1480. [DOI] [PubMed] [Google Scholar]
- [2].Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J 2010;10:994–8. [DOI] [PubMed] [Google Scholar]
- [3].Kuntz Ct, Levin LS, Ondra SL, Shaffrey CI, Morgan CJ. Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: a review and resynthesis of the literature. J Neurosurg Spine 2007;6:104–12. [DOI] [PubMed] [Google Scholar]
- [4].Harrison DE, Harrison DD, Janik TJ, Holland B, Siskin LA. Slight head extension: does it change the sagittal cervical curve? Eur Spine J 2001;10:149–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Dvorak J, Froehlich D, Penning L, Baumgartner H, Panjabi MM. Functional radiographic diagnosis of the cervical spine: flexion/extension. Spine (Phila Pa 1976) 1988;13:748–55. [DOI] [PubMed] [Google Scholar]
- [6].Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38:S149–60. [DOI] [PubMed] [Google Scholar]
- [7].Park MS, Moon SH, Kim TH, Oh JK, Kang HJ, Riew KD. Radiographic comparison between cervical spine lateral and whole-spine lateral standing radiographs. Global Spine J 2016;6:118–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Singhatanadgige W, Kang DG, Luksanapruksa P, Peters C, Riew KD. Correlation and reliability of cervical sagittal alignment parameters between lateral cervical radiograph and lateral whole-body EOS stereoradiograph. Global Spine J 2016;6:548–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Park SM, Song KS, Park SH, Kang H, Daniel Riew K. Does whole-spine lateral radiograph with clavicle positioning reflect the correct cervical sagittal alignment? Eur Spine J 2015;24:57–62. [DOI] [PubMed] [Google Scholar]
- [10].Mac-Thiong JM, Transfeldt EE, Mehbod AA, et al. Can c7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine (Phila Pa 1976) 2009;34:E519–27. [DOI] [PubMed] [Google Scholar]
- [11].Kim TH, Lee SY, Kim YC, Park MS, Kim SW. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976) 2013;38:E992–7. [DOI] [PubMed] [Google Scholar]
- [12].Smith JS, Lafage V, Ryan DJ, et al. Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the AOSpine North America Myelopathy study. Spine (Phila Pa 1976) 2013;38:S161–70. [DOI] [PubMed] [Google Scholar]
- [13].Park MS, Moon SH, Lee HM, et al. The effect of age on cervical sagittal alignment: normative data on 100 asymptomatic subjects. Spine (Phila Pa 1976) 2013;38:E458–63. [DOI] [PubMed] [Google Scholar]
- [14].Aota Y, Saito T, Uesugi M, Ishida K, Shinoda K, Mizuma K. Does the fists-on-clavicles position represent a functional standing position? Spine (Phila Pa 1976) 2009;34:808–12. [DOI] [PubMed] [Google Scholar]
- [15].Marks MC, Stanford CF, Mahar AT, Newton PO. Standing lateral radiographic positioning does not represent customary standing balance. Spine (Phila Pa 1976) 2003;28:1176–82. [DOI] [PubMed] [Google Scholar]
- [16].Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there an optimal patient stance for obtaining a lateral 36" radiograph?. A critical comparison of three techniques. Spine (Phila Pa 1976) 2005;30:427–33. [DOI] [PubMed] [Google Scholar]
- [17].Morvan G, Mathieu P, Vuillemin V, et al. Standardized way for imaging of the sagittal spinal balance. Eur Spine J 2011;20:602–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Park JH, Cho CB, Song JH, Kim SW, Ha Y, Oh JK. T1 Slope and cervical sagittal alignment on cervical CT radiographs of asymptomatic persons. J Korean Neurosurg Soc 2013;53:356–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976) 1995;20:1351–8. [PubMed] [Google Scholar]
- [20].Jang JS, Lee SH, Min JH, Kim SK, Han KM, Maeng DH, et al. Surgical treatment of failed back surgery syndrome due to sagittal imbalance. Spine (Phila Pa 1976) 2007;32:3081–7. [DOI] [PubMed] [Google Scholar]
- [21].Faro FD, Marks MC, Pawelek J, Newton PO. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:2284–9. [DOI] [PubMed] [Google Scholar]
- [22].Vedantam R, Lenke LG, Bridwell KH, Linville DL, Blanke K. The effect of variation in arm position on sagittal spinal alignment. Spine (Phila Pa 1976) 2000;25:2204–9. [DOI] [PubMed] [Google Scholar]
- [23].Nunez-Pereira S, Hitzl W, Bullmann V, Meier O, Koller H, et al. Sagittal balance of the cervical spine: an analysis of occipitocervical and spinopelvic interdependence, with C-7 slope as a marker of cervical and spinopelvic alignment. J Neurosurg Spine 2015;23:16–23. [DOI] [PubMed] [Google Scholar]
- [24].Tamai K, Buser Z, Paholpak P, Sessumpun K, Nakamura H, Wang JC. Can C7 slope substitute the T1 slope?.: an analysis using cervical radiographs and kinematic MRIs. Spine (Phila Pa 1976) 2018;43:520–5. [DOI] [PubMed] [Google Scholar]
- [25].Boissiere L, Bernard J, Vital JM. Cervical spine balance: postoperative radiologic changes in adult scoliosis surgery. Eur Spine J 2015;24:1356–61. [DOI] [PubMed] [Google Scholar]
- [26].Sakai K, Yoshii T, Hirai T, Arai Y, Shinomiya K, Okawa A. Impact of the surgical treatment for degenerative cervical myelopathy on the preoperative cervical sagittal balance: a review of prospective comparative cohort between anterior decompression with fusion and laminoplasty. Eur Spine J 2017;26:104–12. [DOI] [PubMed] [Google Scholar]
- [27].Hey HWD, Teo AQA, Tan KA, et al. How the spine differs in standing and in sitting-important considerations for correction of spinal deformity. Spine J 2017;17:799–806. [DOI] [PubMed] [Google Scholar]


