Abstract
Background
Nazartinib is considered a new, permanent, and mutant-selective epidermal growth factor receptor-tyrosine kinase inhibitor (EGFR-TKI). It has a demonstrated efficacy to treat patients experiencing EGFR-mutated non-small cell cancer (NSCLC). The present study aims to explore the clinical efficacy and safety of nazartinib in patients experiencing EGFR-mutated NSCLC.
Materials and Methods
The present study is a prospective, multicentre, open-label experiment seeking to assess the clinical safety as well as efficacy of nazartinib in patients suffering from EGFR-mutated NSCLC. The study will randomly divide 78 patients into experimental and control groups using a ratio of 1:1. Additionally, the study will treat the experimental group with nazartinib, and the control group with other chemotherapeutic agents. Besides, the study will treat both the experimental and control groups with standard treatment for a period of 14 days and will be followed up at least 24 weeks. Overall response rate is the major endpoint. Accordingly, the minor endpoints will include progression-free survival, response time, overall survival, and adverse events. Statistical analysis will be performed by SPSS 25.0 software.
Discussion
The study will investigate the clinical safety and efficacy of nazartinib in patients suffering from EGFR-mutated NSCLC. The anticipated results of the study are expected to provide clinical basis for nazartinib to treat patients suffering from EGFR-mutated NSCLC.
Keywords: efficacy, EFGR, nazartinib, non-small cell lung cancer, safety
1. Introduction
Generally, lung cancer is considered among the primary triggers of cancer-related deaths worldwide. It accounts for an estimated 2.1 million new cases of lung cancer and around 1.8 million deaths in 2018 alone.[1] Moreover, lung cancer is primarily made up of non-small cell lung cancer (NSCLC), distributed into various histological groups, among them lung adenocarcinoma, which has become one of the most prevalent subtypes.[2] Regardless of the multimodal treatment strategies, such as immunotherapy and radiotherapy, it appears that non-invasive surgical resection has great progressions over the recent past. At the same time, the consequences of lung cancer are still unsatisfactory, with an estimated five-year relative overall survival rate of about 18%.[3]
The first-line treatments suggested for NSCLC patients with sensitising EGFR mutations are epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs) gefitinib, erlotinib, and afatinib.[4,5] Despite the impressive responses with first- and second-generation EGFR-TKIs utilised in treating patients with sensitising EGFR mutations, most patients still develop resistance.[6–9] One of the expected resistance mechanisms to first- and second-generation EGFR-TKIs is the gatekeeper Thr790Met mutation found in an estimated 60% of resistant tumours.[10] Nazartinib is a third-generation, new, permanent, oral EGFR-TKIs that selectively impedes EGFR-TKIs sensitising mutations, and Thr790Met resistance mutations are suggested as the first-line treatment of NSCLC patients with Thr790Met-positive.[11–13] In some previous studies, nazartinib demonstrated clinical activity in patients suffering from Thr790Met-positive NSCLC.[13] However, the present study will examine the clinical safety and efficacy of nazartinib in patients with EGFR-mutated NSCLC.
2. Materials and methods
2.1. Study design and setting
The present study considers a prospective, randomised, multicentre, open-label trial. It aims to explore the clinical safety as well as efficacy of nazartinib in patients histologically diagnosed with EGFR-mutated NSCLC. For the present investigation, 78 patients will be registered from among the outpatients in the Wuhan Fourth Hospital; Puai Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei Province, China. In particular, the study will randomise eligible participants utilising a ratio of 1:1 into the experimental group (with nazartinib-containing chemotherapy) and control group (without nazartinib-containing chemotherapy). The two groups will be treated for 28 days and followed up at least 24 weeks. Records of the experimental and control groups will be written as per the 2013 Standard Protocol Items.[14] The flowchart of the study will be presented in Figure 1.
Figure 1.
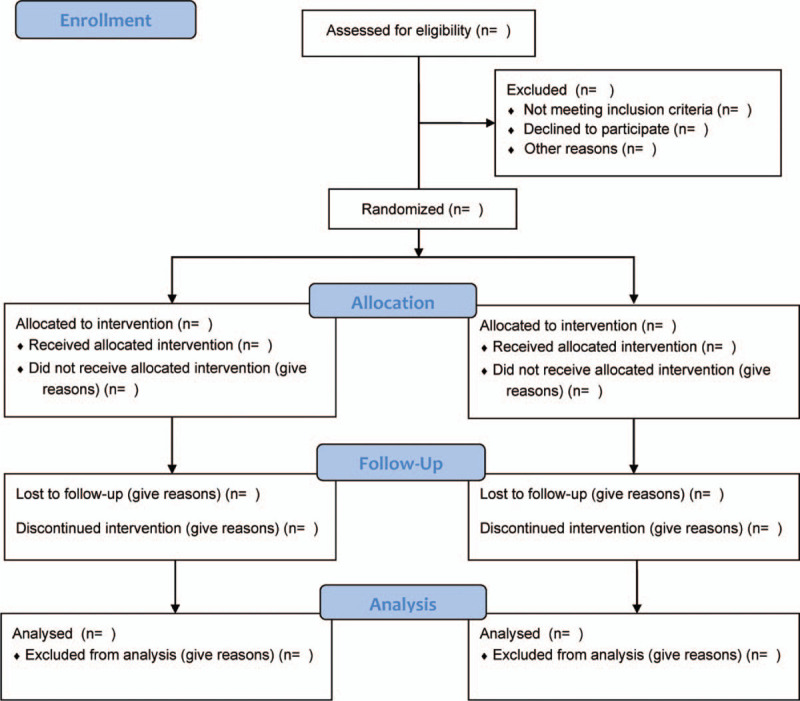
Flow diagram of the study.
2.2. Ethics and registration
The present study will be carried out as per the Helsinki Declaration and approved by the Ethics Committee of Wuhan Fourth Hospital; Puai Hospital, Tongji Medical College, Huazhong University of Science and Technology. Similarly, the study protocol has been enrolled on the Open Science Framework (OSF, registration number: 10.17605/OSF.IO/XWHJ2). Accordingly, all participants will need to sign a consent form before the onset of the study.
2.3. Participants
Participants or patients recruited in the study are those with histologically diagnosed EGFR-mutated NSCLC. The following criteria of inclusion and exclusion are being used:
-
1.
Inclusion criteria
-
1)
The study will consider histologically or cytologically established locally advanced/metastatic NSCLC;
-
2)
Eastern Cooperative Oncology Group performance status score from 0 to 2;[15]
-
3)
Occurrence of a minimum of a quantifiable lesion as per the Response Criteria for Clinical Trials of Cancer (RECIST) 1.1;[16]
-
4)
Mutated EGFR and requiring nazartinib therapy;
-
5)
Patients’ readiness to consent before the onset of the study.
-
1)
-
2.
Exclusion criteria
-
1)
Presence or history of another malignancy;
-
2)
Patients with a history or incidences of interstitial lung ailment or those with interstitial pneumonitis will be considered unsuitable for the present study by the researchers, including clinically significant radiation pneumonitis;
-
3)
Patients with clinically significant, uncontrolled heart disease;
-
4)
Severe hepatopathy (Child-Pugh C);
-
5)
Severe nephropathy (eGFR <15 ml/minute) or those in need of dialysis;
-
6)
Those with a history of Hepatitis B or C, and those with favourable outcomes in compulsory testing for acute or chronic hepatitis B or hepatitis C;
-
7)
Patients with known HIV infection or those with past HIV infections independent from the cellular immune status;
-
8)
Those unwilling to sign the written informed consent form.
-
1)
2.4. Interventions
Overall, participants in the experimental group will be given nazartinib chemotherapy (150 mg/day, orally). However, participants in the control group will be given erlotinib chemotherapy (150 mg/day, orally) or gefitinib chemotherapy (250 mg/day, orally). This might be adjusted as per the researcher's medical judgment.
2.5. Outcomes
The present study's primary outcome will be a comparison of the overall response rate between nazartinib chemotherapy and other chemotherapeutic agents for patients suffering from EGFR-mutated NSCLC (overall response rate denotes the number of participants with the best general response of complete responses and partial responses as determined by the Blinded Independent Review Committee assessment in accordance to RECIST 1.1). Therefore, the primary outcomes are comparisons of the progression-free survival, response time, overall survival, as well as adversative outcomes or events.
2.6. Randomisation and blinding
The study will conduct random assignment in a 1:1 ratio based on the computer-generated, blocked, random-allocation order. This study will also consider a total of 78 participants divided into a group based on a pre-generated randomisation table and an allocated randomised number. The participant will be divided into the experimental or control group on the basis of the codes of allocation of the randomised assignment technique. The arrangement will be done beforehand. However, the study did not carry out blinding.
2.7. Statistical methods
The present study carries the analyses of all the data using IBM SPSS Statistics for Windows, version 24.0. The statistical testing is two-tailed, and P < .05 will be regarded as statistically significant. A non-paired test will assess the numerical data of normal distribution. Accordingly, the study will evaluate categorical variables using a Pearson Chi-square test. The study will analyse the variations between the experimental and control groups using the Kaplan–Meier method from the evaluation.
3. Discussion
Overall, lung cancer is a common malignant tumour and is considered one of the leading causes of cancer-related mortalities globally. In particular, non-small cell lung carcinoma accounting for an estimated 80% of all lung cancer patients.[17–19] Nonetheless, there have been significant developments in immunotherapy, chemotherapy, radiotherapy, and non-invasive surgery to treat human tumour. The five-year relative survival rate for patients with advanced NSCLC is about 18%.[17] Therefore, the present study considers a prospective, randomised, multicentre, open-label trial that intends to investigate the clinical safety and efficacy of nazartinib in patients experiencing histologically diagnosed EGFR-mutated NSCLC. Generally, we also hope that this study will open a new direction to treat patients with EGFR-mutated NSCLC.
Author contributions
Conceptualization: Jun Cui, Lu-Lu Zhang.
Data curation: Zheng Xiao.
Formal analysis: Jun Cui.
Funding acquisition: Zheng Xiao.
Investigation: Jun Cui.
Methodology: Jun Cui, Lu-Lu Zhang.
Project administration: Zheng Xiao.
Resources: Zheng Xiao, Lu-Lu Zhang.
Software: Jun Cui.
Supervision: Zheng Xiao.
Validation: Jun Cui, Lu-Lu Zhang.
Visualization: Jun Cui, Zheng Xiao.
Writing – original draft: Jun Cui, Lu-Lu Zhang.
Writing – review & editing: Zheng Xiao, Lu-Lu Zhang.
Footnotes
Abbreviations: EGFR-TKIs = Epidermal growth factor receptor-tyrosine kinase inhibitors, NSCLC = Non-small cell lung cancer, RECIST = Response Criteria for Clinical Trials of Cancer.
How to cite this article: Cui J, Xiao Z, Zhang LL. Clinical efficacy and safety of nazartinib for epidermal growth factor receptor mutated non-small cell lung cancer: Study protocol for a prospective, multicenter, open-label. Medicine. 2021;100:21(e25992).
This study supported by the Scientific Research Projects of Medical and Health of Health and Family Planning Commission of Wuhan (Grant number: WX16C27). The sponsors had no role in the present protocol.
The authors have no conflicts of interest.
Trial registration: DOI 10.17605/OSF.IO/XWHJ2.
The datasets generated during and/or analyzed during the present study are available from the corresponding author on reasonable request.
References
- [1].Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- [2].Hirsch FR, Scagliotti GV, Mulshine JL, et al. Lung cancer: current therapies and new targeted treatments. Lancet 2017;389:299–311. [DOI] [PubMed] [Google Scholar]
- [3].Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. Cancer J Clin 2018;68:07–30. [DOI] [PubMed] [Google Scholar]
- [4].Planchard D, Popat S, Kerr K, et al. Metastatic non-small cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2018;29:iv192–237. [DOI] [PubMed] [Google Scholar]
- [5].Keedy VL, Temin S, Somerfield MR, et al. American Society of Clinical Oncology provisional clinical opinion: epidermal growth factor receptor (EGFR) mutation testing for patients with advanced non-small-cell lung cancer considering first-line EGFR tyrosine kinase inhibitor therapy. J Clin Oncol 2011;29:2121–7. [DOI] [PubMed] [Google Scholar]
- [6].Miura S, Yamanaka T, Kato T, et al. Treatment rationale and design of a phase III study of afatinib or chemotherapy in patients with non-small-cell lung cancer harboring sensitizing uncommon epidermal growth factor receptor mutations (ACHILLES/TORG1834). Clin Lung Cancer 2020;21:e592–6. [DOI] [PubMed] [Google Scholar]
- [7].Santos ES, Hart L. Advanced squamous cell carcinoma of the lung: current treatment approaches and the role of afatinib. Onco Targets Ther 2020;13:9305–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327–34. [DOI] [PubMed] [Google Scholar]
- [9].Santoni-Rugiu E, Melchior LC, Urbanska EM, et al. Intrinsic resistance to EGFR-tyrosine kinase inhibitors in EGFR-mutant non-small cell lung cancer: differences and similarities with acquired resistance. Cancers 2019;11: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Westover D, Zugazagoitia J, Cho BC, Cho BC, Lovly CM, Paz-Ares L. Mechanisms of acquired resistance to first- and second-generation EGFR tyrosine kinase inhibitors. Ann Oncol 2018;29: suppl_1: i10–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Andrews Wright NM, Goss GD. Third-generation epidermal growth factor receptor tyrosine kinase inhibitors for the treatment of non-small cell lung cancer. Transl Lung Cancer Res 2019;8: Suppl 3: S247–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jia Y, Juarez J, Li J, et al. EGF816 exerts anticancer effects in non-small cell lung cancer by irreversibly and selectively targeting primary and acquired activating mutations in the EGF receptor. Cancer Res 2016;76:1591–602. [DOI] [PubMed] [Google Scholar]
- [13].Tan DS, Leighl NB, Riely GJ, et al. Safety and efficacy of nazartinib (EGF816) in adults with EGFR-mutant non-small-cell lung carcinoma: a multicentre, open-label, phase 1 study. Lancet Respir Med 2020;8:561–72. [DOI] [PubMed] [Google Scholar]
- [14].Chan AW, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Zubrod CG, Schneiderman M, Frei E, et al. Appraisal of methods for the study of chemotherapy of cancer in man: comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. J Chronic Dis 1960;11:07–33. [Google Scholar]
- [16].Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. [DOI] [PubMed] [Google Scholar]
- [17].Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67:07–30. [DOI] [PubMed] [Google Scholar]
- [18].Wood SL, Pernemalm M, Crosbie PA, Whetton AD. The role of the tumor-microenvironment in lung cancer-metastasis and its relationship to potential therapeutic targets. Cancer Treat Rev 2014;40:558–66. [DOI] [PubMed] [Google Scholar]
- [19].Bray F, Ren J-S, Masuyer E, Ferlay J. Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int J Cancer 2013;132:1133–45. [DOI] [PubMed] [Google Scholar]


