Abstract
Background:
The treatment of Rockwood Grade-III acromioclavicular (AC) joint separation has been widely disputed since the introduction of the classification system. The present literature does not reach consensus on whether operative or nonoperative management is more advantageous, nor does it effectively distinguish between operative measures. We hypothesized that nonoperative treatment of Rockwood Grade-III AC joint separation would be more cost-effective when compared with surgical options.
Methods:
We created a decision-tree model outlining the treatment of Rockwood Grade-III separations using nonoperative management or hook-plate, suture-button, or allograft fixation. After nonoperative intervention, the possible outcomes predicted by the model were uneventful healing, delayed operative management, a second round of sling use and physical therapy, or no reduction and no action; and after operative intervention, the possible outcomes were uneventful healing, loss of reduction and revision, and depending on the implant, loss of reduction and no action, or removal of the implant. A systematic review was conducted, and probabilities of each model state were averaged. A cost-effectiveness analysis was conducted both through rollback analysis yielding net monetary benefit and through incremental cost-effectiveness ratios (ICERs). Thresholds of $50,000/quality-adjusted life-year (QALY) and $100,000/QALY were used for ICER analysis. Furthermore, a sensitivity analysis was utilized to determine whether differential probabilities could impact the model.
Results:
Forty-five papers were selected from a potential 768 papers identified through our literature review. Nonoperative treatment was used as our reference case and showed dominance over all 3 of the operative measures at both the $50,000 and $100,000 ICER thresholds. Nonoperative treatment also showed the greatest net monetary benefit. Nonoperative management yielded the lowest total cost ($6,060) and greatest utility (0.95 QALY). Sensitivity analysis showed that allograft fixation became the favored technique at a willingness-to-pay threshold of $50,000 if the rate of failure of nonoperative treatment rose to 14.6%. Similarly, at the $100,000 threshold, allograft became dominant if the probability of failure of nonoperative treatment rose to 22.8%.
Conclusions:
The cost-effectiveness of nonoperative treatment is fueled by its notably lower costs and overall high rates of success in Grade-III separations. It is important to note that, in our analysis, the societal cost (measured in lost productivity) of nonoperative treatment neared that of surgical treatment, but the cost from the health-care system perspective was minimal. Physicians should bear in mind the sensitivity of these conclusions and should consider cost-effectiveness analyses in their decision-making guidelines.
Level of Evidence:
Economic and Decision Analysis Level IV. See Instructions for Authors for a complete description of levels of evidence.
The choice to treat Rockwood Grade-III acromioclavicular (AC) joint separation nonsurgically or surgically remains controversial. A Grade-III injury is a distal clavicular injury involving a rupture of both the AC and coracoclavicular (CC) ligaments, accompanied by a CC distance increase of 25% to 100%1. This injury typically occurs in young male athletes through direct force to the acromion with the shoulder adducted or indirect force from falling on an outstretched arm2,3. Grade III is 1 of 6 types of distal AC joint injuries. Rockwood Grade-I and II injuries are minor and treated nonoperatively with a shoulder sling, while Rockwood Grade-IV through VI injuries are more serious and treated surgically.
As for treating Grade-III dislocations, patients and surgeons are left to choose on the basis of preference, level of activity, and age2. Nonoperative approaches reduce complications, but some patients are left with a cosmetic deformity, residual pain, or chronic subluxation, as the distal part of the clavicle is typically not reduced to an anatomic distance2,4. Surgical approaches have much higher rates of complications, necessitating revision, and have not been shown to produce significantly better shoulder function4. There are many AC joint fixation techniques, including the use of hook plates, suture buttons, and allograft implants. Suture buttons have gained much attention in recent years because of lower rates of complications and revision surgeries when compared with the use of hook plates5,6.
The concept of value-based care may provide a solution in guiding a physician’s and patient’s decision to pursue operative or nonoperative treatment of Rockwood Grade-III AC joint separations. In the U.S., Medicare, Medicaid, and some private providers are already rewarding better outcomes for lower costs in bundled packages, including total hip and knee replacements7,8. The purpose of the present study was to develop a decision-tree model to analyze nonoperative, hook-plate, suture-button, and allograft intervention costs, outcomes, and complications. We conducted a cost-effectiveness analysis of treatment options and aggregated total costs for comparison. Our hypothesis was that nonoperative treatment of Rockwood Grade-III AC joint separation would be more cost-effective when compared with surgical options: hook-plate fixation, suture-button fixation, or repair with allograft.
Materials and Methods
Study Design
This study was exempt from institutional review board approval. All analyses were conducted in accordance with Second Panel on Cost-Effectiveness in Health and Medicine guidelines9. The reference case consisted of healthy patients between the ages of 20 and 39 years, as determined through epidemiological studies10, who underwent operative repair of Rockwood Grade-III AC joint separations.
Decision Model
We created a decision-tree model detailing the treatment of Rockwood Grade-III AC joint separation. We evaluated nonoperative treatment, which consisted of immobilization (sling therapy) and physical therapy, as well as the following operative measures: hook-plate fixation, suture-button fixation, and repair with allograft. All operative measures are assumed to also have had similar physical therapy components. Each node of the model is associated with a specific cost, in U.S. dollars, and a utility adjustment (quality-adjusted life-years [QALYs]).
Event Probabilities
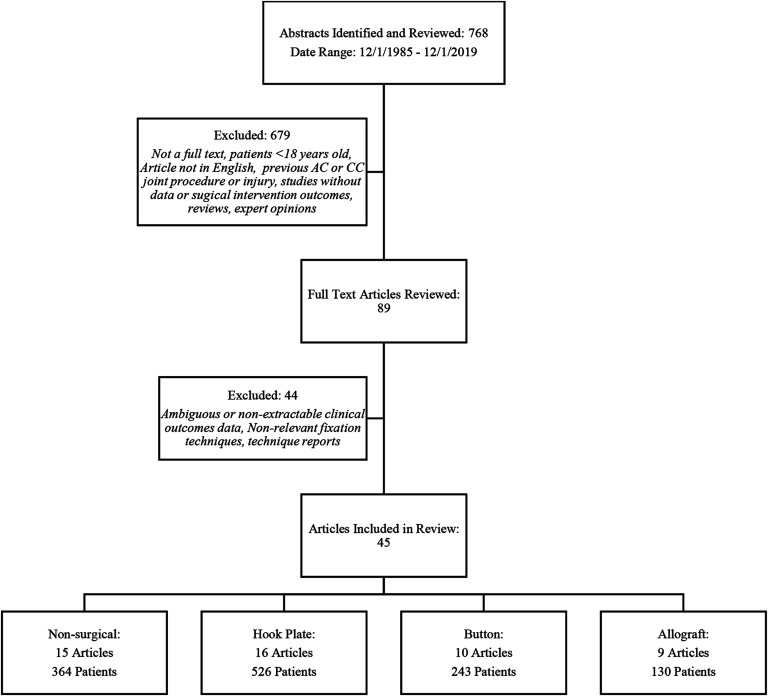
After nonoperative intervention, our model predicts the following possible outcomes: uneventful healing, delayed operative management, a second round of sling use and physical therapy, or no reduction and no action. After operative intervention, the possible outcomes include uneventful healing, loss of reduction and revision, and depending on the implant, loss of reduction and no action, or removal of the implant. Outcome probabilities were calculated for each technique using previous literature (Table I). Using a systematic review process, we queried PubMed (see Appendix 1) utilizing general terms to capture the widest range of Rockwood Grade-III-related articles from December 1, 1985, to December 1, 2019. This search identified 768 abstracts. After inputting exclusion criteria, 89 full-text articles remained for review. After further screening of the full-text articles, 45 articles meeting the criteria for calculating outcome probabilities remained (see Appendix 2). Figure 1 presents a flow diagram of the study’s literature review with inclusion and exclusion criteria. Our model used weighted averages to account for study-size variation when calculating outcome probabilities for each group (Table I).
Fig. 1.
Flowchart of the selection and elimination of studies from the literature review.
TABLE I.
Decision Model Transition-State Probability Inputs*
| Event | Transition State | References | |
| Mean Probability (%) | Probability Range (%) | ||
| Sling and physical therapy (PT) | 24,26-39 | ||
| Uneventful healing | 92.1 | 58.8-100 | |
| Delayed operative management | 1.8 | 0-25 | |
| Second-round sling and PT | 4.3 | 0-41.2 | |
| No reduction and no action | 1.8 | 0-4.0 | |
| Hook-plate fixation | 6,31,40-53 | ||
| Uneventful healing | 98.3 | 83.3-100 | |
| Loss of reduction and revision | 1.7 | 0-16.7 | |
| Removal of implant | 99.1 | 89.5-100 | |
| Suture-button fixation | 6,19,28,54-60 | ||
| Uneventful healing | 92.7 | 62.5-100 | |
| Loss of reduction and revision | 6.6 | 0-25.0 | |
| Loss of reduction and no action | 0.7 | 0-12.5 | |
| Allograft | 18,52,53,61-66 | ||
| Uneventful healing | 98.4 | 80.0-100 | |
| Loss of reduction and revision | 0.8 | 0-5.9 | |
| Loss of reduction and no action | 0.8 | 0-25.0 | |
Transition-state probabilities utilized in the decision-tree model. The mean probability is derived from the weighted average of the individual event probabilities from each of the included references. The probability range reflects the range of individual probabilities encountered in the included literature.
Costs
We calculated total allowable reimbursement by using Current Procedural Terminology (CPT) codes to search the U.S. Centers for Medicare & Medicaid Services (CMS) Physician Fee Schedule and Ambulatory Surgical Center Payment System11,12. For uneventful healing of hook-plate and suture-button fixation, CPT code 23550 was used, while 23552 was used for allograft treatment and 23540 was used for nonoperative treatment. Furthermore, 20680 was used for implant removal. Anesthesia fees were calculated using operative-time data gleaned from the previously detailed literature search. To do this, operative minutes were divided by 15 to provide base time units, and then these time units were added to the anesthesia base units and multiplied by the 2020 national anesthesia conversion factor to provide the total allowable anesthesia reimbursement13.
By adding anesthesia fees, surgeon fees, and CMS surgical center reimbursement, we arrived at the total procedure cost, as shown in Table II. We excluded postoperative care (physical therapy, occupational therapy, etc.) from our cost inputs because of the similarities among treatment modalities. Suture-button, allograft, and nonoperative interventions, along with revision surgery, were assigned 6 weeks of disutility due to lost productivity. One week was assigned for implant removal, and 12 weeks were assigned to hook-plate intervention because of the nature of healing after implant removal. Lost-productivity time intervals were estimated on the basis of return to work not necessitating labor-intensive duties. Median income values sourced from the U.S. Bureau of Labor Statistics were used in conjunction with these time intervals to estimate societal costs (Table II)14.
TABLE II.
Decision Model Cost Inputs*
| Cost Item | Initial Fixation | Complications | ||||
| Hook Plate | Suture Button | Allograft | Nonoperative | Revision for Loss of Reduction | Removal of Implant | |
| Health-care management ($) | ||||||
| Surgical center costs | 2,803 | 2,803 | 3,822 | 108 | 2,803 | 994 |
| Surgeon fees | 598 | 598 | 688 | 227 | 598 | 649 |
| Anesthesia fees | 158 | 158 | 203 | 0 | 221 | 155 |
| Total surgical costs | 3,559 | 3,559 | 4,713 | 335 | 3,622 | 1,798 |
| Societal | ||||||
| No. of wk of disutility | 12 | 6 | 6 | 6 | 6 | 1 |
| Cost of disutility/wk ($) | 957 | 957 | 957 | 957 | 957 | 957 |
| Total societal cost ($) | 11,484 | 5,742 | 5,742 | 5,742 | 5,742 | 957 |
| Total cost, baseline and societal ($) | 15,043 | 9,301 | 10,455 | 6,077 | 9,364 | 2,755 |
Costs are rounded to the nearest dollar. Cost inputs were calculated for each node of the decision model. In the decision-tree model, total costs for secondary surgical procedures were added to the total costs already incurred by the index procedure.
Utility and Effectiveness Estimation
Because of the scarcity of utility estimation in AC joint injury research, we sought data on similarly treated injuries of the clavicle for comparison. Open reduction and internal fixation (ORIF) of midshaft clavicular fractures was analyzed using the randomized clinical trial Short Form Six-Dimension (SF-6D) question set, which resulted in an estimated loss of 0.078 QALY from a disutility over 3 months15. Similarly, another study investigated QALY loss for a host of injuries using both the standard QALY/DALY (disability-adjusted life-year) model (SQM) and the annual profile model (APM)16. Under “fracture clavicula/scapula,” Haagsma et al. reported values of 0.054 and 0.050 for the 2 models16. We elected to use 0.078 as our value for disutility after operative intervention and 0.052 (an average of 0.054 and 0.050) as our disutility value for nonoperative management. Revision surgery was assigned a QALY of the index surgery (0.078) plus a loss of 0.04 to account for the interim time between surgeries in which the patient experienced disutility from the loss of reduction. Implant removal conferred a loss of QALY equal to 0.01, reflective of the minimal impact on weeks of disutility.
We decided to assign all 4 interventions equivalent long-term health states because of the scarcity of data supporting one mode of management of Rockwood Grade-III AC joint separation over another.
Cost-Effectiveness Analysis
The incremental cost-effectiveness ratio (ICER) is the ratio of the difference in cost (dollars) to the difference in effectiveness (QALY) of a particular treatment modality when compared with another. Typically, after an ICER is generated, thresholds are implemented to evaluate whether the gain in utility is worth the added cost. These ICER thresholds are most commonly set at $50,000 and $100,000. For example, a hypothetical modality may present with a substantially higher QALY than traditional intervention (+0.10) but also substantially increased cost (+$15,000). While this hypothetical treatment may be far more effective, it confers an ICER of $150,000/QALY, which would be deemed too expensive by society at both the $50,000 and $100,000 thresholds. For the purpose of this study, both the $50,000 and $100,000 thresholds were evaluated in the ICER analysis, with nonoperative management as the reference strategy. Furthermore, rollback analysis was also used to quantify the net monetary benefit. Net monetary benefit (NMB) calculations are a combination of willingness-to-pay (WTP), cost, and effectiveness (measured as NMB = effectiveness × WTP – cost)17.
To effectively estimate the total cost, we used societal and health-care system perspectives. The health-care system perspective included all surgeon fees, surgical center costs, and anesthesia fees. The societal perspective was primarily a measure of the cost of lost productivity. After the model was created, we used a sensitivity analysis to evaluate the stability throughout a range of values identified in the literature search. The sensitivity analysis was carried out using the societal and health-care perspectives separately as well as combined. All analyses were performed using TreeAge Pro (TreeAge Software).
Results
Rollback Analysis
To achieve a baseline understanding of the cost and utility of each modality, a rollback analysis was conducted to yield a net monetary benefit, measured in dollars. Nonoperative management displayed the greatest net monetary benefit from the societal perspective ($41,578), the health-care system perspective ($46,798), and the total combined perspective ($41,157). Table III outlines the net monetary benefit for each treatment modality, by perspective.
TABLE III.
Net Monetary Benefit (NMB) for Each Intervention Modality, by Perspective*
| Societal Perspective | Health-Care System Perspective | Total Combined Perspective | |
| Nonoperative | 41,578 | 46,798 | 41,157 |
| Hook plate | 31,572 | 37,720 | 26,159 |
| Suture button | 40,333 | 42,170 | 36,535 |
| Allograft | 40,755 | 41,342 | 36,013 |
Values are represented in dollars. Costs are rounded to the nearest dollar. Results were derived from the following NMB equation: effectiveness × willingness-to-pay – cost.
ICER Analysis
Using nonoperative treatment as our reference case, we saw negative ICER values for all 3 operative interventions for both the health-care and total combined perspectives. Negative ICER values are a result of the treatment modality being both costlier and less effective than the reference strategy. Thus, in all 3 cases, the WTP thresholds of $50,000 and $100,000 for hook-plate and suture-button fixation were not considered. In the societal perspective, allograft treatment was used as the reference modality as it yielded the lowest total cost. Here we saw nonoperative treatment as being slightly costlier but also slightly more effective (ICER value of 13,751), and thus, nonoperative management was still preferred at both WTP thresholds. Nonoperative management was once again dominant to both hook-plate and suture-button interventions. All comparisons of procedure costs, effectiveness, and ICER values are presented in Table IV.
TABLE IV.
Results of Cost-Effectiveness Analysis for Baseline Models*
| Net Cost ($) | Difference in Cost ($) | Effectiveness (QALY) | Difference in QALY | ICER | |
| Health-care perspective | |||||
| Hook plate | 5,372 | +4,952 | 0.86 | –0.09 | Dominated by NO |
| Suture button | 3,798 | +3,378 | 0.91 | –0.04 | Dominated by NO |
| Allograft | 4,742 | +4,322 | 0.92 | –0.03 | Dominated by NO |
| Nonoperative | 420 | Ref. | 0.95 | Ref. | Ref. |
| Societal perspective | |||||
| Hook plate | 11,520 | +6,192 | 0.86 | –0.06 | Dominated by AG |
| Suture button | 5,635 | +307 | 0.91 | –0.01 | Dominated by AG |
| Allograft | 5,328 | Ref. | 0.92 | Ref. | Ref. |
| Nonoperative | 5,640 | +312 | 0.95 | +0.03 | $13,751/QALY gained |
| Combined perspective | |||||
| Hook plate | 16,892 | +10,832 | 0.86 | –0.09 | Dominated by NO |
| Suture button | 9,433 | +3,373 | 0.91 | –0.04 | Dominated by NO |
| Allograft | 10,070 | +4,010 | 0.92 | –0.03 | Dominated by NO |
| Nonoperative | 6,060 | Ref. | 0.95 | Ref. | Ref. |
QALY = quality-adjusted life-year, ICER = incremental cost-effectiveness ratio, NO = nonoperative, and AG = allograft.
Sensitivity Analysis
In order to determine whether our model was sensitive to changes in event probabilities reported in the literature, a sensitivity analysis was conducted. Nonoperative management largely remained the favored treatment modality over the other 3 perspectives, except for 2 circumstances: if the rate at which patients experienced unsuccessful nonoperative treatment but then achieved successful healing after a second round of physical therapy was increased, or if the rate at which patients experienced unsuccessful nonoperative treatment and proceeded to surgical intervention was increased. In both circumstances, operative management using an allograft became the favored intervention.
For the WTP threshold of $50,000, the rate of unsuccessful physical therapy followed by a second round of physical therapy would have had to increase from 4.3% (average) to 14.6%. Similarly, the rate of unsuccessful physical therapy followed by operative management would have had to increase from a rate of 1.8% (average) to 9.3%.
For the WTP threshold of $100,000, the rate of unsuccessful physical therapy followed by a second round of physical therapy would have had to increase from a rate of 4.3% (average) to 22.8%. Similarly, the rate of unsuccessful physical therapy followed by operative management would have had to increase from a rate of 1.8% (average) to 15.0%.
Discussion
When comparing nonoperative and operative interventions for Rockwood Grade-III AC joint separation, nonoperative management dominated in cost-effectiveness terms. Nonoperative treatment was the least expensive modality because of minimal health-care system costs. Similarly, nonoperative treatment was the most effective because of a larger decrease in health utility after surgery, yet with relatively similar success rates.
Hook-plate intervention was, by far, the costliest of the 4 modalities because of the lengthened recovery time associated with the temporary implant. The societal cost was double that of the 3 other modalities, but there was not substantial utility gain to offset this cost. In fact, hook-plate fixation was associated with the lowest assigned QALY by a margin of at least 0.05 units, and these assessments are echoed by clinical data comparing the modalities18,19. Suture buttons were similarly not cost-effective, but this was because of the high rates of revision rather than their societal cost. Allograft was the closest competitor to nonoperative management. Allograft treatment demonstrated both the highest index surgery success rate and the lowest revision rate. While similar to nonoperative treatment in societal cost, allograft treatment was much costlier to the health-care system.
Because of disparities in event probabilities reported in the literature, there are situations in which allograft treatment was superior to nonoperative treatment, in a cost-effectiveness sense. When the rates of nonoperative treatment failure increased, yet remained well within the ranges reported in literature, allograft treatment was shown to be more cost-effective. This is an important finding to note, as a clinician may want to consider which patient-centric details may alter the probability of nonoperative success for a particular patient. Guidelines suggesting which patients are deemed more suitable for nonoperative management are currently lacking, but clinicians may want to consider the patient’s previous experiences and successes with a physical therapy protocol before suggesting nonoperative management. Similarly, as suggested by Smith et al.20, physicians may have to weigh the cost-effectiveness of nonoperative treatment with the chance of anatomic deformities that may hinder a patient’s profession, if said profession involves carrying heavy weight on the shoulder.
While other studies have investigated cost-effectiveness strategies in areas of the upper extremity, such as clavicular and humeral fractures15,16,21-23, this is the first study, to our knowledge, to investigate the cost-effectiveness of the treatment of AC joint separation. Furthermore, our study went further to investigate the most controversial grade of separation, Rockwood Grade III20,24, in order to provide a guideline for clinicians when deciding whether to proceed with operative or nonoperative management. The present study included a sizable amount of literature detailing the outcomes of Rockwood Grade-III treatment. The large bank of patients and studies provides validity to the accuracy of the values used in our analysis. Furthermore, because of the sample size, we were able to test our model with a range of event probabilities, which we believe lends further support to the strength of our findings.
Despite an extensive review of the literature, our study had notable limitations. First, the difficulty of defining subjective utility scores such as QALYs is a limitation common to cost-effective studies across the board. While acknowledging that limitation, we emphasize that the QALY estimates presented here were sourced from multiple external sources that all produced reliably similar values15,16,21. Second, there is a noticeable lack of literature reporting Rockwood Grade-III outcomes when compared with other Rockwood grades. This limitation cannot be remedied by anything other than time and commitment from the orthopaedic community to better investigate the proper treatment modality for this controversial topic. Last, our model was based on averages at every junction (health system costs, societal costs, QALYs), and thus it is entirely reasonable for a patient or clinician to elect treatment against the suggestions presented here. Our model was not all-inclusive and should not be taken as doctrine at the level of individual patients but may be better used as an overarching guideline.
Treatment of Rockwood Grade-III AC joint separation has been the center of controversy since the adoption of Rockwood grading25. Operative and nonoperative measures have proven effective20, on average, at treating this injury, but to date, we are not aware of any study that has provided a cost-effectiveness analysis on the treatment modalities. In the present study, we found that nonoperative treatment dominated operative management for nearly every perspective. Clinicians should consider both the cost benefit and the utility benefit of electing to proceed with nonoperative management when counseling patients with Rockwood Grade-III AC joint separation.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A272).
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Henry Ford Hospital, Detroit, Michigan
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A271).
References
- 1.Guy DK, Wirth MA, Griffin JL, Rockwood CA, Jr. Reconstruction of chronic and complete dislocations of the acromioclavicular joint. Clin Orthop Relat Res. 1998. February;347:138-49. [PubMed] [Google Scholar]
- 2.Gowd AK, Liu JN, Cabarcas BC, Cvetanovich GL, Garcia GH, Manderle BJ, Verma NN. Current concepts in the operative management of acromioclavicular dislocations: a systematic review and meta-analysis of operative techniques. Am J Sports Med. 2019. September;47(11):2745-58. Epub 2018 Oct 1. [DOI] [PubMed] [Google Scholar]
- 3.Simovitch R, Sanders B, Ozbaydar M, Lavery K, Warner JJP. Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg. 2009. April;17(4):207-19. [DOI] [PubMed] [Google Scholar]
- 4.Li X, Ma R, Bedi A, Dines DM, Altchek DW, Dines JS. Management of acromioclavicular joint injuries. J Bone Joint Surg Am. 2014. January 1;96(1):73-84. [DOI] [PubMed] [Google Scholar]
- 5.Cisneros LN, Reiriz JS. Management of chronic unstable acromioclavicular joint injuries. J Orthop Traumatol. 2017. December;18(4):305-18. Epub 2017 Mar 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang YC. M A Y y U WZ, Wang H. Surgical treatment of acute Rockwood III acromioclavicular dislocations-comparative study between two flip-button techniques. Sci Rep. 2020. March 10;10(1):4447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Porter ME, Lee TH. From volume to value in health care: the work begins. JAMA. 2016. September 13;316(10):1047-8. [DOI] [PubMed] [Google Scholar]
- 8.Tsevat J, Moriates C. Value-based health care meets cost-effectiveness analysis. Ann Intern Med. 2018. September 4;169(5):329-32. Epub 2018 Aug 7. [DOI] [PubMed] [Google Scholar]
- 9.Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, Kuntz KM, Meltzer DO, Owens DK, Prosser LA, Salomon JA, Sculpher MJ, Trikalinos TA, Russell LB, Siegel JE, Ganiats TG. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016. September 13;316(10):1093-103. [DOI] [PubMed] [Google Scholar]
- 10.Chillemi C, Franceschini V, Dei Giudici L, Alibardi A, Salate Santone F, Ramos Alday LJ, Osimani M. Epidemiology of isolated acromioclavicular joint dislocation. Emerg Med Int. 2013;2013:171609. Epub 2013 Jan 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services. Ambulatory Surgical Center (ASC) Payment. Accessed 2020 Apr 2. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/index
- 12.Centers for Medicare & Medicaid Services. Physician Fee Schedule. Accessed 2021 March 25. https://www.cms.gov/medicare/physician-fee-schedule/search
- 13.Centers for Medicare & Medicaid Services. Anesthesiologists center. Accessed 2020 Apr 2. https://www.cms.gov/Center/Provider-Type/Anesthesiologists-Center
- 14.Bureau of Labor Statistics. Usual weekly earnings of wage and salary workers news release. Published 2020. January 17. Accessed 2020 Apr 2. https://www.bls.gov/news.release/archives/wkyeng_01172020.htm [Google Scholar]
- 15.Pearson AM, Tosteson ANA, Koval KJ, McKee MD, Cantu RV, Bell JE, Vicente M. Is surgery for displaced, midshaft clavicle fractures in adults cost-effective? Results based on a multicenter randomized, controlled trial. J Orthop Trauma. 2010. July;24(7):426-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haagsma JA, Polinder S, van Beeck EF, Mulder S, Bonsel GJ. Alternative approaches to derive disability weights in injuries: do they make a difference? Qual Life Res. 2009. June;18(5):657-65. Epub 2009 May 7. [DOI] [PubMed] [Google Scholar]
- 17.TreeAge Software. TreeAge Pro 2018 user’s manual. 2018. Accessed 2021 Feb 11. http://files.treeage.com/treeagepro/18.1.0/20180118/TP-Manual-2018R1.pdf [Google Scholar]
- 18.Ye G, Peng CA, Sun HB, Xiao J, Zhu K. Treatment of Rockwood type III acromioclavicular joint dislocation using autogenous semitendinosus tendon graft and EndoButton technique. Ther Clin Risk Manag. 2016. January 11;12:47-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang L, Zhou X, Qi J, Zeng Y, Zhang S, Liu G, Ping R, Li Y, Fu S. Modified closed-loop double-EndoButton technique for repair of Rockwood type III acromioclavicular dislocation. Exp Ther Med. 2018. January;15(1):940-8. Epub 2017 Nov 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith TO, Chester R, Pearse EO, Hing CB. Operative versus non-operative management following Rockwood grade III acromioclavicular separation: a meta-analysis of the current evidence base. J Orthop Traumatol. 2011. March;12(1):19-27. Epub 2011 Feb 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fox HM, Ramsey DC, Thompson AR, Hoekstra CJ, Mirarchi AJ, Nazir OF. Neer type-II distal clavicle fractures: a cost-effectiveness analysis of fixation techniques. J Bone Joint Surg Am. 2020. February 5;102(3):254-61. [DOI] [PubMed] [Google Scholar]
- 22.Nwachukwu BU, Schairer WW, McCormick F, Dines DM, Craig EV, Gulotta LV. Arthroplasty for the surgical management of complex proximal humerus fractures in the elderly: a cost-utility analysis. J Shoulder Elbow Surg. 2016. May;25(5):704-13. Epub 2016 Mar 8. [DOI] [PubMed] [Google Scholar]
- 23.Osterhoff G, O’Hara NN, D’Cruz J, Sprague SA, Bansback N, Evaniew N, Slobogean GP. A cost-effectiveness analysis of reverse total shoulder arthroplasty versus hemiarthroplasty for the management of complex proximal humeral fractures in the elderly. Value Health. 2017. March;20(3):404-11. Epub 2016 Dec 12. [DOI] [PubMed] [Google Scholar]
- 24.Phillips AM, Smart C, Groom AF. Acromioclavicular dislocation. Conservative or surgical therapy. Clin Orthop Relat Res. 1998. August;353:10-7. [PubMed] [Google Scholar]
- 25.Deans CF, Gentile JM, Tao MA. Acromioclavicular joint injuries in overhead athletes: a concise review of injury mechanisms, treatment options, and outcomes. Curr Rev Musculoskelet Med. 2019. June;12(2):80-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calvo E, López-Franco M, Arribas IM. Clinical and radiologic outcomes of surgical and conservative treatment of type III acromioclavicular joint injury. J Shoulder Elbow Surg. 2006. May-Jun;15(3):300-5. [DOI] [PubMed] [Google Scholar]
- 27.Cardone D, Brown JN, Roberts SNJ, Saies AD, Hayes MG. Grade III acromioclavicular joint injury in Australian rules football. J Sci Med Sport. 2002. June;5(2):143-8. [DOI] [PubMed] [Google Scholar]
- 28.De Carli A, Lanzetti RM, Ciompi A, Lupariello D, Rota P, Ferretti A. Acromioclavicular third degree dislocation: surgical treatment in acute cases. J Orthop Surg Res. 2015. January 28;10(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dias JJ, Steingold RF, Richardson RA, Tesfayohannes B, Gregg PJ. The conservative treatment of acromioclavicular dislocation. Review after five years. J Bone Joint Surg Br. 1987. November;69(5):719-22. [DOI] [PubMed] [Google Scholar]
- 30.Glick JM, Milburn LJ, Haggerty JF, Nishimoto D. Dislocated acromioclavicular joint: follow-up study of 35 unreduced acromioclavicular dislocations. Am J Sports Med. 1977. Nov-Dec;5(6):264-70. [DOI] [PubMed] [Google Scholar]
- 31.Gstettner C, Tauber M, Hitzl W, Resch H. Rockwood type III acromioclavicular dislocation: surgical versus conservative treatment. J Shoulder Elbow Surg. 2008. Mar-Apr;17(2):220-5. Epub 2008 Feb 4. [DOI] [PubMed] [Google Scholar]
- 32.Joukainen A, Kröger H, Niemitukia L, Mäkelä EA, Väätäinen U. Results of operative and nonoperative treatment of Rockwood types III and V acromioclavicular joint dislocation: a prospective, randomized trial with an 18- to 20-year follow-up. Orthop J Sports Med. 2014. December 11;2(12):2325967114560130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacDonald PB, Alexander MJ, Frejuk J, Johnson GE. Comprehensive functional analysis of shoulders following complete acromioclavicular separation. Am J Sports Med. 1988. Sep-Oct;16(5):475-80. [DOI] [PubMed] [Google Scholar]
- 34.Petri M, Warth RJ, Greenspoon JA, Horan MP, Abrams RF, Kokmeyer D, Millett PJ. Clinical results after conservative management for grade III acromioclavicular joint injuries: does eventual surgery affect overall outcomes? Arthroscopy. 2016. May;32(5):740-6. Epub 2016 Feb 4. [DOI] [PubMed] [Google Scholar]
- 35.Prokop A, Helling HJ, Andermahr J, Mönig S, Rehm KE. [Tossy III injuries of the acromioclavicular joint. In what circumstances is surgery still justified? Personal results and literature review]. Orthopade. 2003. May;32(5):432-6. German. [DOI] [PubMed] [Google Scholar]
- 36.Rawes ML, Dias JJ. Long-term results of conservative treatment for acromioclavicular dislocation. J Bone Joint Surg Br. 1996. May;78(3):410-2. [PubMed] [Google Scholar]
- 37.Schlegel TF, Burks RT, Marcus RL, Dunn HK. A prospective evaluation of untreated acute grade III acromioclavicular separations. Am J Sports Med. 2001. Nov-Dec;29(6):699-703. [DOI] [PubMed] [Google Scholar]
- 38.Taft TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint. An end-result study. J Bone Joint Surg Am. 1987. September;69(7):1045-51. [PubMed] [Google Scholar]
- 39.Tang G, Zhang Y, Liu Y, Qin X, Hu J, Li X. Comparison of surgical and conservative treatment of Rockwood type-III acromioclavicular dislocation: a meta-analysis. Medicine (Baltimore). 2018. January;97(4):e9690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cai L, Wang T, Lu D, Hu W, Hong J, Chen H. Comparison of the tight rope technique and clavicular hook plate for the treatment of Rockwood type III acromioclavicular joint dislocation. J Invest Surg. 2018. June;31(3):226-33. Epub 2017 Apr 12. [DOI] [PubMed] [Google Scholar]
- 41.Chang HM, Hong CK, Su WR, Wang TH, Chang CW, Tai TW. Comparison of clavicular hook plate with and without coracoclavicular suture fixation for acute acromioclavicular joint dislocation. Acta Orthop Traumatol Turc. 2019. November;53(6):408-13. Epub 2019 Sep 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen CH, Dong QR, Zhou RK, Zhen HQ, Jiao YJ. Effects of hook plate on shoulder function after treatment of acromioclavicular joint dislocation. Int J Clin Exp Med. 2014. September 15;7(9):2564-70. [PMC free article] [PubMed] [Google Scholar]
- 43.Wang DL, Ruan DK, Yin Q, Li HF, Wang PJ, He Q, Li W. [Clinical application of hook plate for the treatment of distal clavicular trauma and analysis on its complications]. Zhongguo Gu Shang. 2009. September;22(9):655-7. Chinese. [PubMed] [Google Scholar]
- 44.Di Francesco A, Zoccali C, Colafarina O, Pizzoferrato R, Flamini S. The use of hook plate in type III and V acromio-clavicular Rockwood dislocations: clinical and radiological midterm results and MRI evaluation in 42 patients. Injury. 2012. February;43(2):147-52. Epub 2011 May 17. [DOI] [PubMed] [Google Scholar]
- 45.Kienast B, Thietje R, Queitsch C, Gille J, Schulz AP, Meiners J. Mid-term results after operative treatment of Rockwood grade III-V acromioclavicular joint dislocations with an AC-hook-plate. Eur J Med Res. 2011. February 24;16(2):52-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kumar N, Sharma V. Hook plate fixation for acute acromioclavicular dislocations without coracoclavicular ligament reconstruction: a functional outcome study in military personnel. Strateg Trauma Limb Reconstr. 2015. August;10(2):79-85. Epub 2015 Jul 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Łazarski A, Sarzyńska S, Struzik S, Jędral T, Łęgosz P, Małdyk P. Results of treatment of type 3 acromioclavicular joint dislocation with three methods. Ortop Traumatol Rehabil. 2019. June 30;21(3):167-79. [DOI] [PubMed] [Google Scholar]
- 48.Metzlaff S, Rosslenbroich S, Forkel PH, Schliemann B, Arshad H, Raschke M, Petersen W. Surgical treatment of acute acromioclavicular joint dislocations: hook plate versus minimally invasive reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016. June;24(6):1972-8. Epub 2014 Sep 11. [DOI] [PubMed] [Google Scholar]
- 49.Pereira-Graterol E, Álvarez-Díaz P, Seijas R, Ares O, Cuscó X, Cugat R. Treatment and evolution of grade III acromioclavicular dislocations in soccer players. Knee Surg Sports Traumatol Arthrosc. 2013. July;21(7):1633-5. Epub 2012 Aug 29. [DOI] [PubMed] [Google Scholar]
- 50.Salem KH, Schmelz A. Treatment of Tossy III acromioclavicular joint injuries using hook plates and ligament suture. J Orthop Trauma. 2009. September;23(8):565-9. [DOI] [PubMed] [Google Scholar]
- 51.Steinbacher G, Sallent A, Seijas R, Boffa JM, Espinosa W, Cugat R. Clavicular hook plate for grade-III acromioclavicular dislocation. J Orthop Surg (Hong Kong). 2014. December;22(3):329-32. [DOI] [PubMed] [Google Scholar]
- 52.Ye JK, Yu BJ, Ye FS, Hong JY, Wang W, Tong PJ. [Case-control study on therapeutic effects between modified Weaver-Dunn surgery and clavicular hook plate fixation in the treatment of acromioclavicular joint dislocation]. Zhongguo Gu Shang. 2014. January;27(1):4-8. Chinese. [PubMed] [Google Scholar]
- 53.Wang G, Xie R, Mao T, Xing S. Treatment of AC dislocation by reconstructing CC and AC ligaments with allogenic tendons compared with hook plates. J Orthop Surg Res. 2018. July 11;13(1):175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Acar MA, Güleç A, Erkoçak ÖF, Yılmaz G, Durgut F, Elmadağ M. Percutaneous double-button fixation method for treatment of acute type III acromioclavicular joint dislocation. Acta Orthop Traumatol Turc. 2015;49(3):241-8. [DOI] [PubMed] [Google Scholar]
- 55.Beris A, Lykissas M, Kostas-Agnantis I, Vekris M, Mitsionis G, Korompilias A. Management of acute acromioclavicular joint dislocation with a double-button fixation system. Injury. 2013. March;44(3):288-92. Epub 2013 Jan 24. [DOI] [PubMed] [Google Scholar]
- 56.Faggiani M, Vasario GP, Mattei L, Calò MJ, Castoldi F. Comparing mini-open and arthroscopic acromioclavicular joint repair: functional results and return to sport. Musculoskelet Surg. 2016. December;100(3):187-91. Epub 2016 Jun 10. [DOI] [PubMed] [Google Scholar]
- 57.Glanzmann MC, Buchmann S, Audigé L, Kolling C, Flury M. Clinical and radiographical results after double flip button stabilization of acute grade III and IV acromioclavicular joint separations. Arch Orthop Trauma Surg. 2013. December;133(12):1699-707. [DOI] [PubMed] [Google Scholar]
- 58.Loriaut P, Casabianca L, Alkhaili J, Dallaudière B, Desportes E, Rousseau R, Massin P, Boyer P. Arthroscopic treatment of acute acromioclavicular dislocations using a double button device: clinical and MRI results. Orthop Traumatol Surg Res. 2015. December;101(8):895-901. Epub 2015 Nov 3. [DOI] [PubMed] [Google Scholar]
- 59.Sun LJ, Lu D, Tao ZY, Yu XB, Hu W, Ma YF, Yu B. Analysis of risk factors for loss of reduction after acromioclavicular joint dislocation treated with the suture-button. J Orthop Sci. 2019. September;24(5):817-21. Epub 2019 Feb 16. [DOI] [PubMed] [Google Scholar]
- 60.Torkaman A, Bagherifard A, Mokhatri T, Haghighi MH, Monshizadeh S, Taraz H, Hasanvand A. Double-button fixation system for management of acute acromioclavicular joint dislocation. Arch Bone Jt Surg. 2016. January;4(1):41-6. [PMC free article] [PubMed] [Google Scholar]
- 61.Huang JL, Mo HP. [Reconstructing coracoclavicular ligament in treating Rockwood - III acromioclavicular dislocation by palmaris longus muscle with polyester suture]. Zhongguo Gu Shang. 2015. June;28(6):538-41. Chinese. [PubMed] [Google Scholar]
- 62.Kibler WB, Sciascia AD, Morris BJ, Dome DC. Treatment of symptomatic acromioclavicular joint instability by a docking technique: clinical indications, surgical technique, and outcomes. Arthroscopy. 2017. April;33(4):696-708.e2. Epub 2016 Nov 17. [DOI] [PubMed] [Google Scholar]
- 63.Kocaoglu B, Ulku TK, Gereli A, Karahan M, Türkmen M. Palmaris longus tendon graft versus modified Weaver-Dunn procedure via dynamic button system for acromioclavicular joint reconstruction in chronic cases. J Shoulder Elbow Surg. 2017. September;26(9):1546-52. Epub 2017 Mar 31. [DOI] [PubMed] [Google Scholar]
- 64.Millett PJ, Braun S, Gobezie R, Pacheco IH. Acromioclavicular joint reconstruction with coracoacromial ligament transfer using the docking technique. BMC Musculoskelet Disord. 2009. January 14;10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tauber M, Gordon K, Koller H, Fox M, Resch H. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med. 2009. January;37(1):181-90. Epub 2008 Sep 25. [DOI] [PubMed] [Google Scholar]
- 66.Yoo JC, Ahn JH, Yoon JR, Yang JH. Clinical results of single-tunnel coracoclavicular ligament reconstruction using autogenous semitendinosus tendon. Am J Sports Med. 2010. May;38(5):950-7. Epub 2010 Mar 12. [DOI] [PubMed] [Google Scholar]