Abstract
Rationale & Objective:
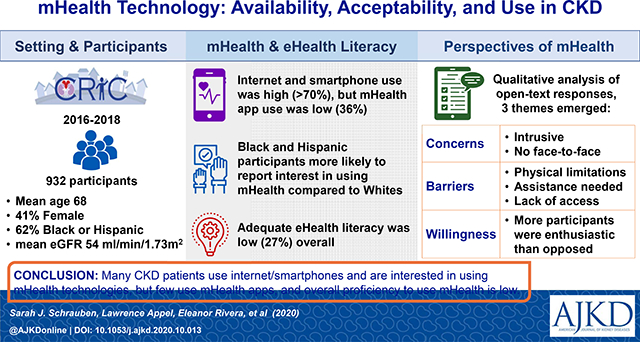
Digital and mobile health (mHealth) technologies improve patient-provider communication and increase information accessibility. We assessed technology use, attitudes toward using mHealth technologies, and the proficiency in using mHealth technologies among individuals with chronic kidney disease (CKD).
Study Design:
Cross-sectional survey with open text responses
Setting & Participants:
Chronic Renal Insufficiency Cohort Study participants who completed current use and interest in using mHealth technologies questionnaires, and the eHealth literacy Survey (eHEALS).
Exposures:
Participant characteristics
Outcomes:
Technology use (internet/email/smartphone/mHealth applications [apps]), interest in future mHealth use, and proficiency in using digital and mHealth technologies, or eHealth literacy, determined by eHEALS score.
Analytic Approach:
Poisson regression and a qualitative content analysis of open-ended responses
Results:
Study participants (N=932) had a mean age of 68 years, eGFR 54 ml/min/1.73m2, and 59% were male. Approximately 70% reported current use of internet/email/smartphones, and 35% used mHealth apps; only 27% had adequate eHealth literacy (eHEALS score ≥32). Participants <65 years (vs. ≥65), with more education, higher income, better cognition, and adequate health literacy reported more technology use, and greater interest in using technologies. Participants of white (vs. non-white) race reported more internet/email use, but less interest in future mHealth use. Younger age, higher annual income, and greater disease self-efficacy were associated with adequate eHealth literacy. Three themes regarding interest in using digital and mHealth technologies emerged: willingness, concerns, and barriers.
Limitations:
Residual confounding, ascertainment bias
Conclusions:
Many individuals with CKD currently use the internet and smartphones, and are interested in using mHealth in the future, but few use mHealth apps or have adequate eHealth literacy. mHealth technologies present an opportunity to engage individuals with CKD, especially members of racial or ethnic minority groups since they reported greater interest in using mHealth technology, compared to the non-minority population. Further research is needed to identify strategies to overcome inadequate eHealth literacy.
Keywords: mobile health, mHealth, chronic kidney disease, eHealth literacy
Plain Language Summary
Mobile health (mHealth) technology improves patient-provider communication and increases access to information. We wanted to explore how extensively patients are using mHealth technology, what they think about using it, and how proficient they are using it. Our study focused on a group of 932 individuals with chronic kidney disease (CKD). We found that 70% currently used internet/email/smartphones, and 35% used health-specific apps. Less than a third of our patients reported proficient use of mHealth technology. Individuals who were under 65, had more education, and higher income were more likely to use mHealth technology and had a greater interest in it. Black and Hispanic individuals had less technology use overall but were more interested in using mHealth technology. mHealth technology presents an opportunity to engage individuals with CKD.
Graphical Abstract
INTRODUCTION
Mobile health (mHealth) technology pertains to the use of mobile and wireless digital technologies to support health and wellness by extending education, communication, health interventions, and research beyond the reach of traditional clinical care.1 In chronic disease populations, mHealth has been shown to improve overall patient-provider communication, strengthen patient autonomy, and empower patients to become active participants in their own care,2,3 each of which increases the patient-centeredness of care.
Individuals with chronic conditions such as chronic kidney disease (CKD) often need to participate in complicated disease management strategies, but have low levels of participation in self-management behaviors, a characteristic that links to poor outcomes.4 mHealth technology has the potential to improve the management of CKD by facilitating patient education, supporting behavior engagement (such as medication adherence and dietary modification), and aiding in patient-provider communication.5 mHealth is also an attractive option to supplement the taxed resources of health care providers, resulting, in part, from the increasing prevalence of CKD. In addition, the global coronavirus pandemic has necessitated that nephrology care be delivered remotely to improve social distancing and thus, has created the need to harness the potential of using mHealth technologies.
Despite the potential of mHealth to support CKD management, few mHealth strategies have been used to assist individuals with this condition.5,6 To date, little is known about the availability and use of mHealth technologies, attitudes about their use, or level of proficiency in using digital and mHealth technologies for health purposes (i.e., eHealth literacy) among people with CKD.7 In this mixed methods study, we describe the use of mHealth technologies, as well as willingness to use mHealth technologies and the level of eHealth literacy among individuals with mild-to-moderate CKD in the Chronic Renal Insufficiency Cohort (CRIC) Study.
METHODS
Study Design and Study Population
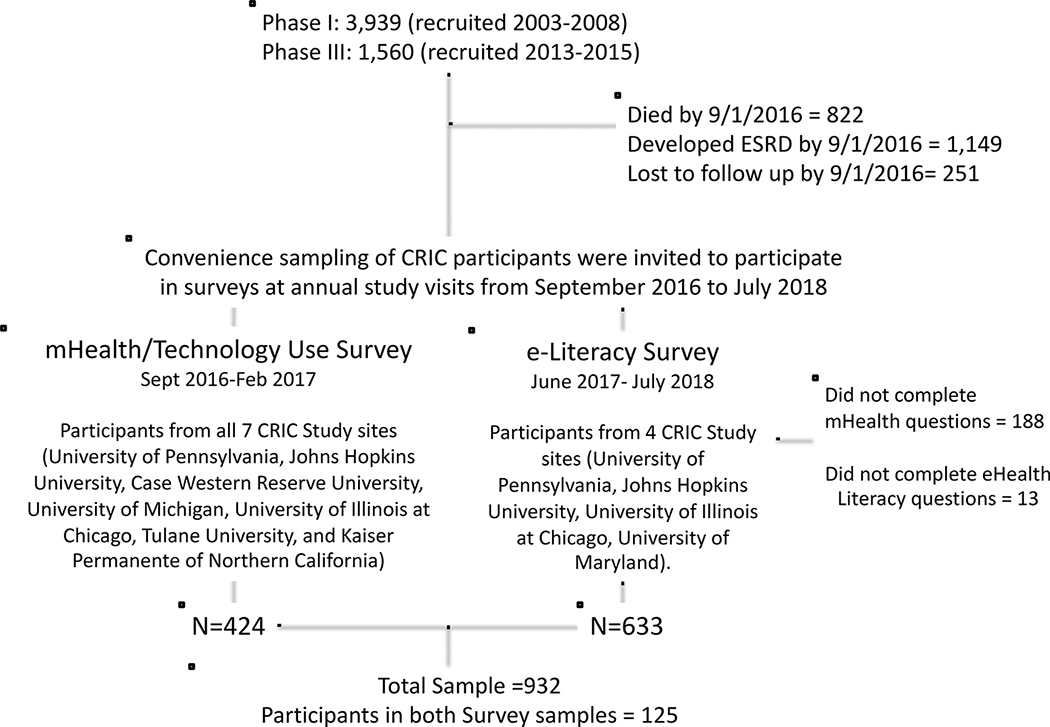
This study used data from the CRIC Study, a multi-center, prospective observational cohort of persons with mild-moderate CKD in the US.8,9 CRIC participants were recruited from seven clinical centers (University of Pennsylvania, Johns Hopkins University, Case Western Reserve University, University of Michigan, University of Illinois at Chicago, Tulane University, and Kaiser Permanent of Northern California) during two phases: 1) Phase I, from 2003 to 2008 (3,939 participants), and 2) Phase III, from 2013 to 2015 (1,560 participants), and prospectively followed annually. The full inclusion and exclusion criteria have been previously reported.8,9 In brief, Phase I included adults 21–74 years with age-based estimated glomerular filtration rate (eGFR) 20–70 ml/min/1.73m2, and entry into Phase III required eGFR 45–70 ml/min/1.73m2 and age 45–79 years. Exclusion criteria included inability to consent and certain severe conditions. For this study, we used data from participants who completed at least one of two surveys (mHealth/Technology Use Survey or e-Literacy Survey), which contained questions related to the use of internet, email, smartphones, or mHealth applications (apps), future interest in using mHealth technologies, and eHealth literacy. Potential survey participants consisted of a convenience sample of CRIC participants who attended annual study visits between late 2016 and mid-2018. Research coordinators offered the mHealth/Technology Use Survey to the first 60 participants at their annual visit at all seven clinical centers, and the e-Literacy Survey was offered at four of the seven clinical centers (see Figure 1). The surveys were self-administered at in-person visits or administered by the research coordinator if the visit was conducted over the phone. The CRIC Study protocol was approved by the Institutional Review Board of all participating centers and is in accordance with the Declaration of Helsinki. All participants provided written informed consent.
Figure 1:
Flow diagram of study sample selection.
Measurements
The mHealth/Technology Use Survey and e-Literacy Survey were developed within the CRIC Study in parallel for distinct, but complimentary reasons (please see Supplementary Methods for more information). In brief, the mHealth/Technology Use Survey consisted of 12 questions that were developed to collect information from participants about their willingness to use mHealth technologies, along with their current availability and use in the effort to plan for future research in the CRIC Study. The survey questions were drafted and vetted by CRIC investigators, and then piloted among CRIC research staff. The e-Literacy Survey was developed for use in a CRIC ancillary study to learn about participants’ current use of and proficiency of using digital and mHealth technology, and consisted of 19 questions, 11 of which were developed de novo by CRIC ancillary investigators, and eight composed the validated eHealth Literacy Scale (eHEALS).10,11
Study Outcomes
The primary study outcome was technology use, with secondary outcomes of interest in future use of mHealth technologies, and level of eHealth literacy (Table S1). Technology use was categorized as current or not current use of three types of technology: internet or email, smartphones, and mHealth apps. Internet or email use was collapsed into one category, since email requires the internet. Internet use was assessed by “do you use the internet?” or by confirming internet use of at least once per month. Email use was assessed by “do you use and read email?” or by confirming the use of email when using the internet or a smartphone. Smartphone use was assessed by “do you use a smartphone (a cell phone that can access the internet such as an iPhone)?” or by selecting ‘smartphone’ when asked “What type of cell/mobile phone do you primarily use?” mHealth app use was determined by endorsing a response to “which of the following types of health apps have you used on your cell/mobile phone?” Interest in future use of mHealth technologies was assessed by answering “are you willing to answer study questionnaires using: the internet, email, or smartphone?” since these study questions focus on the participants’ willingness to use mHealth to report on their health status, or by an affirmative response to at least one statement related to the development of a new internet or mHealth tool for the following purposes: “I’d like more help remembering to take my medications”, “I’d like more help learning about what my medications are for”, or “I’d like more help learning about possible side effects from my medications”.
eHealth literacy is the skill set needed to effectively find, appraise, and use health information from electronic or digital materials, including mHealth technology. eHealth literacy was assessed with eHEALS to measure the level of an individual’s knowledge and perceived skills at finding, evaluating, and applying digital health information to their health problems.10,11 eHEALS consists of eight questions with 5 response options on a Likert-scale, and scored as a cumulative score of the eight questions (range 8–40, with a score of ≥32 considered to be adequate) or individually (range 1–5).10,11 In our analysis, we used a dichotomous cumulative score of <32 or ≥32 for adequate eHealth literacy.
Covariates
Covariates were chosen for their potential influence on technology use, interest in digital and mHealth technologies, and eHealth literacy.12–14 Age was determined by the year of survey completion. Sex, race/ethnicity, education, income, and co-morbidity history were collected through self-report during the CRIC baseline assessment, co-morbidities reported were used to construct a Charlson comorbidity index.15 Health literacy, depressive symptoms, and cognitive function were also collected at baseline with validated questionnaires, the short version of the Test of Functional Health Literacy in Adults (S-TOFHLA), Beck’s Depression Inventory (BDI), and Modified Mini-Mental State Exam, respectively.16–18 Measures of disease management self-efficacy (Self-Efficacy for Management of Chronic Disease) and social network (Lubben Social Network Score) were available only at baseline in Phase III Cohort participants.19,20 Blood samples collected at the study visit closest to survey completion were used to determine an eGFR with a CRIC-specific equation using serum creatinine and cystatin C.21 Location of recruitment site was included in the models to account for potential geographic differences.
Statistical Analysis
We describe the study population using mean and standard deviation, or median and interquartile range for continuous variables, and frequency and proportion for categorical variables. The Pearson’s chi-square and Kruskal-Wallis test were used to compare categorical and continuous variables, respectively. We report the prevalence of current technology use and interest in future use of digital and mHealth technologies in the total study sample and by age group (<65 and ≥65 years) since age has been shown to be an important influence on digital technology.22–26
We examined the association of sociodemographic and clinical factors with current technology use, interest in mHealth, and eHealth literacy in multivariable adjusted Poisson (log-link) regression models with robust error variance to model rate ratios to approximate prevalence ratios (PR).27,28 Poisson regression was preferred over logistic regression since the odds ratio is known to overstate the risk ratio versus the PR in cross-sectional studies with common outcomes.29 Analyses were performed with STATA 14.2. Adjusted PRs with 95% confidence intervals are reported. Significance level was 0.05 for two-sided test.
We also conducted a qualitative content analysis of responses to the open-ended question included in the mHealth/Technology Use Survey, “Do you have any comments about what we’ve asked you in this questionnaire?” Given the lack of prior literature on this topic, we did not begin with preconceived codes, but developed them inductively through examination of the data.30 Coding was conducted independently by two members of the author team with qualitative research training (SJS, ER) using Microsoft Excel for Mac, version 16.32. They each examined all of the open question responses and created their own list of codes to categorize the responses with no predetermined structure. They then shared those codes and resolved any coding differences through iterative discussion, finally arriving at a common final coding scheme.
RESULTS
Among the total sample of 932 CRIC participants who reported their technology use, 633 completed the e-Literacy Survey and 424 responded to the mHealth/Technology Use Survey. Please see Table S2 for details of participants who did and did not respond to the surveys. There were 125 participants (13.4%) who completed both sets of questions. The participants who completed either survey were similar, except that the e-Literacy Survey group had more participants from a racial or ethnic minority group, with hypertension, diabetes, lower education, as well as more categorized as having inadequate health literacy, and less representation from the South and West Coast than the mHealth/Technology Use Survey group (Table 1). Younger participants (<65 years) reported more current use of internet/email, smartphones, and mHealth apps, as well as more interest in the future use of digital and mHealth technologies, compared to older participants. The reasons for using an mHealth app were similar across age categories (Table 2).
Table 1:
Demographic and Clinical Characteristics of Study Sample, and by Survey type.
| Total Sample (N=932) | e-Literacy Survey Sub-sample (N=633) | mHealth/Technology Use Survey Sub-sample (N=424) | P-value | |
|---|---|---|---|---|
| Age, mean (SD) | 67.9 (9.3) | 67.6 (9.2) | 68.5 (9.2) | 0.06 |
| Male gender, % | 58.5 | 60.5 | 56.1 | 0.08 |
| Race/Ethnicity, % | <0.001 | |||
| Non-Hispanic White | 37.9 | 31.9 | 42.9 | |
| Non-Hispanic Black | 51.4 | 54.8 | 49.8 | |
| Hispanic | 7.6 | 10.7 | 3.5 | |
| Other | 3.1 | 2.5 | 3.8 | |
| Annual Household Income, % | 0.18 | |||
| <$20,000 | 25.4 | 26.2 | 25.5 | |
| $20–50,000 | 25.1 | 26.9 | 23.6 | |
| >$50,000 | 34.2 | 31.4 | 35.9 | |
| Prefer not to answer | 15.2 | 15.5 | 15.1 | |
| Education, % | <0.001 | |||
| <High school | 15.2 | 18.5 | 12.7 | |
| High school/some college | 47.0 | 47.6 | 47.2 | |
| College or higher | 37.8 | 33.9 | 40.1 | |
| Clinical Recruitment Site*, % | <0.001 | |||
| East Coast | 50.6 | 67.3 | 28.5 | |
| Midwest | 35.9 | 32.4 | 42.2 | |
| South | 6.4 | 0 | 14.2 | |
| West Coast | 7.0 | 0.3 | 15.1 | |
| Adequate Health Literacy1, % | 89.0 | 87.4 | 90.8 | 0.04 |
| Cognition score2, mean (SD) | 91.7 (8.0) | 91.1 (8.5) | 92.2 (6.9) | 0.02 |
| Depressive symptom score3, mean (SD) | 7.6 (8.0) | 7.8 (8.3) | 7.3 (7.3) | 0.69 |
| eGFR, ml/min/1.73m2, mean (SD) | 54.4 (15.3) | 53.6 (15.7) | 54.4 (14.6) | 0.06 |
| Prevalent cardiovascular disease, % | 25.5 | 25.6 | 26.4 | 0.85 |
| Diabetes, % | 46.6 | 49.3 | 44.3 | 0.04 |
| Hypertension, % | 85.2 | 88.2 | 81.6 | <0.001 |
| Charlson Comorbidity score, mean (SD) | 5.1 (2.0) | 5.2 (2.0) | 5.1 (2.0) | 0.05 |
| Disease self-efficacy4, mean (SD) | 41.3 (8.7) | 41.3 (9.1) | 41.2 (7.9) | 0.25 |
| Social support score5, mean (SD)^ | 16.0 (5.9) | 15.7 (6.0) | 16.4 (5.9) | 0.33 |
| Adequate eHealth Literacy6, % | -- | 27.2 | -- | -- |
eGFR – estimated glomerular filtration rate
East coast (Philadelphia, PA, Baltimore, MA), Midwest (Ann Arbor, MI; Cleveland, OH; Chicago, IL), South (New Orleans, LA); West Coast (San Francisco, CA; Oakland, CA)
Assessed with S-TOFHLA instrument (adequate score >16, out of 36)16
Assessed with modified mini-Mental State Exam (score range 0–100)18
Assessed with Becks depression inventory (score range 0–63)17
Assessed with disease self-efficacy20 (score range 5–50); only assessed in Phase III cohort participants (N=462)
Assessed with Lubben social network scale, score range (0–30)19; only assessed in Phase III cohort participants ≥65 years of age (N=235)
X2 testing of difference across survey type sub-samples for categorical variables and Kruskal-Wallis for continuous variables
Table 2:
Current Technology Use and Future Interest in Use of mHealth Technologies.
| All Ages | <65 years | ≥65 years | p-value* | |
|---|---|---|---|---|
| Current technology use1, Yes % (N) | ||||
| Internet or email | 75 (690) | 87 (265) | 68 (425) | <0.001 |
| Smartphone | 70 (648) | 88 (267) | 61 (381) | <0.001 |
| mHealth apps2 | 36 (226) | 50 (107) | 29 (119) | <0.001 |
| If yes, reported purpose of mHealth app: | ||||
| Access personal medical record | 51 (116) | 56 (60) | 47 (56) | |
| Look up nutrition or diet information | 49 (110) | 54 (58) | 44 (52) | |
| Learn about health conditions | 48 (109) | 57 (61) | 40 (48) | |
| Track exercise activity or weight | 46 (103) | 48 (51) | 44 (52) | |
| Keep track of medications | 26 (59) | 28 (30) | 24 (29) | |
| Track eating | 18 (40) | 22 (23) | 14 (17) | |
| Record blood pressure | 11 (24) | 13 (14) | 8 (10) | |
| Record blood sugars | 10 (22) | 10 (11) | 9 (11) | |
| Interest in Future Use of Digital and mHealth Technologies, Yes % (N) | ||||
| Internet/email/smartphone for kidney research purposes3 | 77 (328) | 89 (114) | 75 (215) | 0.001 |
| mHealth apps for medication knowledge and management2 | 80 (501) | 82 (177) | 78 (324) | 0.21 |
X2 testing of difference between age groups (<65 vs. ≥65 years)
Sample sizes: All Ages (N=922), <65 years (N=302), ≥65 years (N=620)
Available only in the e-Literacy Survey sub-sample: All Ages, N=630 (N=215 <65 years, N=415 ≥65 years)
Available only in the mHealth/Technology Use Survey sub-sample: All Ages, N=424 (N=128 <65 years, N=296 ≥65 years)
Associations with Technology Use and Interest in Using Digital and mHealth Technologies
Younger age (per 10 years), high school education or higher (vs. less), and higher annual household income (≥$20,000 vs. <$20,000) were associated with more current use of technology (Table 3). Adequate health literacy was also associated with more internet/email and smartphone use, with a similar trend observed for mHealth app use. Non-Hispanic Black participants reported less internet/email use than Non-Hispanic white participants, and non-white (Non-Hispanic Black and Hispanic) participants reported more interest in future use of digital and mHealth technologies. Younger age was the only other characteristic associated with more interest in future use of digital and mHealth technologies.
Table 3:
Associations of participant characteristics with current use and interest in future use of mHealth technologies, and adequate eHealth Literacy. Prevalence ratios (PR), and 95% Confidence Intervals (CI) reported.
| Characteristic | Internet/Email Use1 | Smartphone Use1 | mHealth app Use2 | Interest in mHealth Technology Use1 | Adequate eHealth Literacy2 |
|---|---|---|---|---|---|
| Age (per 10 years) | 0.87 (0.84–0.91) | 0.84 (0.80–0.88) | 0.71 (0.63–0.80) | 0.92 (0.88–0.95) | 0.74 (0.63–0.85) |
| Race/Ethnicity Groups | |||||
| Non-Hispanic White | REF | REF | REF | REF | REF |
| Non-Hispanic Black | 0.88 (0.81–0.95) | 1.08 (0.98–1.19) | 0.89 (0.71–1.10) | 1.17 (1.08–1.27) | 1.01 (0.75–1.36) |
| Hispanic | 0.87 (0.71–1.07) | 1.16 (0.97–1.38) | 1.02 (0.64–1.63) | 1.20 (1.03–1.41) | 1.27 (0.76–2.12) |
| Other | 0.90 (0.72–1.11) | 1.00 (0.77–1.31) | 1.09 (0.59–2.02) | 1.01 (0.81–1.26) | 1.04 (0.44–2.46) |
| Education level | |||||
| <High school | REF | REF | REF | REF | REF |
| ≥High school | 1.56 (1.20–2.04) | 1.27 (1.04–1.56) | 2.62 (1.32–5.17) | 1.05 (0.93–1.19) | 1.90 (1.01–3.61) |
| Annual Income | |||||
| <$20,000 | REF | REF | REF | REF | REF |
| ≥$20,000 | 1.32 (1.16–1.49) | 1.13 (1.00–1.28) | 1.46 (1.07–2.00) | 1.06 (0.97–1.16) | 1.90 (1.28–2.83) |
| No answer | 1.22 (1.05–1.41) | 1.20 (1.03–1.38) | 1.31 (0.90–1.90) | 1.05 (0.93–1.18) | 1.78 (1.12–2.84) |
| Health Literacy | |||||
| Inadequate Health Literacy | REF | REF | REF | REF | REF |
| Adequate Health Literacy | 1.61 (1.21–2.13) | 1.25 (1.00–1.57) | 1.92 (0.98–3.77) | 1.05 (0.93–1.20) | 2.07 (0.95–4.52) |
| Cognition score (per SD) | 1.09 (1.01–1.17) | 1.05 (0.98–1.13) | 1.04 (0.87–1.25) | 1.00 (0.95–1.05) | 1.10 (0.87–1.38) |
| eGFR (per ml/min/1.732) | 1.00 (0.99–1.00) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) | 1.00 (0.99–1.00) | 1.00 (1.00–1.01) |
| Comorbidity score | |||||
| <4 | REF | REF | REF | REF | REF |
| 4–6 | 1.05 (0.97–1.13) | 1.00 (0.91–1.10) | 1.15 (0.90–1.48) | 1.08 (0.99–1.18) | 1.32(0.95–1.82) |
| >6 | 1.01 (0.90–1.14) | 0.96 (0.84–1.10) | 0.98 (0.69–1.39) | 1.09 (0.98–1.22) | 1.01 (0.64–1.61) |
| Depression symptom score (per SD) | 0.99 (0.96–1.03) | 1.01 (0.98–1.05) | 1.09 (1.00–1.19) | 1.03 (0.93–1.20) | 1.01 (0.89–1.14) |
| Only assessed in Phase III cohort: | |||||
| Disease self-efficacy*(per SD) | 1.05 (0.9–1.13) | 1.03 (0.96–1.11) | 1.11 (0.93–1.32) | 1.01 (0.96–1.06) | 1.26 (1.01–1.58) |
| Social support^ (per SD) | 0.99 (0.92–1.07) | 1.10 (0.99–1.22) | 1.11 (0.90–1.37) | 0.99 (0.92–1.07) | 1.04 (0.77–1.39) |
Total study sample without missing variables (N=827)
e-Literacy Survey sub-sample without missing variables (N=567)
Models adjusted for age, sex, race, income, education, clinical recruitment site, health literacy, cognition, depression, baseline eGFR, baseline comorbidity score
Model above + self-efficacy: assessed only in Phase III participants (N=403 for all models except eHealth literacy; N=291 for eHealth Literacy)
Model above + social support: assessed only in Phase III participants ≥65 years of age (N=207 for all models except eHealth Literacy; N=146 for eHealth Literacy)
Associations with eHealth Literacy
Younger age (per 10 years), an annual income of ≥$20,000 (vs. <20,000), and a higher disease self-efficacy score associated with adequate eHealth literacy (Table 3). There was no apparent association of education or race/ethnicity with eHealth literacy. Individual eHEALS question scores were associated with participant characteristics in a similar manner as the cumulative eHEALS score (Table S3).
Patient Perspectives regarding mHealth Technologies
Of the 424 participants who completed the mHealth/Technology Use Survey, 66 provided open text responses. Three themes emerged from the coding of the participant perspectives regarding mHealth technologies: concerns, barriers, and willingness (Table 4). Reported concerns generally related to apprehensions about the level of intrusiveness of monitoring and losing face-to-face interactions with clinic staff as illustrated by an 80-year-old female participant that said “I love coming to the clinic and the interaction between the personal contact with all of the staff”, as well as needing more details about the technologies. Concerns were predominantly reported by those older than 65 years. Barriers to technology use were mainly related to physical limitations, as highlighted by a 76-year-old female participant who shared “I had a stroke three years ago and now have problems trying to read on the internet”. Some participants reported they would require assistance from others, or they lacked technology access. Of the participants who reported barriers to technology use, less than half reported current use of smartphone technology and only half used internet/email. In regard to the willingness to use digital and mHealth technologies, more participants were enthusiastic compared to those who opposed it. Those opposed reported slightly lower use of internet/email than those who were enthusiastic and were more likely to be older than 65 years.
Table 4:
Themes of participant perspectives of future use of digital and mHealth technologies with exemplar quotations.
| Major Themes | Minor themes | Exemplar quotations |
|---|---|---|
| Concerns about use | Intrusiveness | “I work full time, so answers are contingent on devices being unobtrusive in a work environment” (Female, Age 55, Record 310) “Do not want any kind of constant monitoring” (Female, Age 61, Record 9) |
| Losing face-to-face interaction | “I love coming to the clinic and the interaction between the personal contact with all of the staff” (Female, Age 80, Record 44) “I like coming here. Less I have to do at home; the better I like it” (Male, Age 74, Record 40) |
|
| Needs more details | “More details needed” (Female, Age 79, Record 294) “What are the side effects?” (Male, Age 68, Record 161) |
|
| Barriers to use | Physical limitations | “Had stroke 3 years ago and now have problems trying to read on the internet” (Female, Age 76, Record 326) “I am blind, but willing to use talking instruments” (Female, Age 58, Record 184) |
| Requires assistance | “Would need assistance from spouse for email/internet” (Male, Age 69, Record 68) “Good instruction, including video would be important for me to make sure I was doing it correctly” (Male, Age 51, Record 291) |
|
| Lack of technology access | “Do not own a smartphone but is willing to learn” (Female, Age 66, Record 22) “Do not have internet access” (Female, Age 59, Record 1) |
|
| Willingness to use | Enthusiasm | “It would be easier for me at home” (Female, Age 74, Record 269) “Great idea!” (Male, Age 57, Record 29) |
| Opposition | “I am old school and would rather write” (Male, Age 64, Record 91) “Do not use smartphone and have no desire to do so” (Male, Age 68, Record 222) |
DISCUSSION
Among a cohort of individuals with non-dialysis dependent CKD, we identified patient characteristics that likely impact the current uptake of and future interest in using digital and mHealth technologies, including age, health literacy, annual income, and education level. Interestingly, members of racial or ethnic minority groups reported less internet/email use, but more interest in future use of mHealth technologies than white individuals. Another important finding was that approximately three-quarters of our sample did not report an adequate level of eHealth literacy. Prior to this study, mHealth and digital technology use among individuals with kidney diseases in the United States (US) had not been well described, nor had the level of interest in using mHealth technologies or the level of eHealth literacy in this population, despite the growing interest and need to use mHealth technologies for chronic disease management.
Estimates of technology use among those with kidney disease have been reported to be lower than the general US population24,31,32, but they were based largely on individuals with end-stage kidney disease (ESKD). In the current study of individuals with non-dialysis dependent CKD, we found a higher use of the internet or email and smartphones than these prior reports. Greater technology use could be due to more recent timing of data collection and potentially due to the exclusion of individuals with ESKD, who tend to be older and have more co-morbidities, which has been associated with decreased technology use.23,25,33
Despite the substantial use of digital and mHealth technologies in the US, a “digital divide” remains, with an uneven distribution in the access to, use of, and potential benefits of these technologies34, which is driven by socioeconomic status, age and racial minority status.26,35,25,33,36 We also found that a digital divide is present in the population with CKD, observing that older age, membership in a racial or ethnic minority group, and lower socio-economic status (as measured by education level and yearly income) had strong negative relationships with use of all forms of technology. However, smartphone technology may offer an opportunity to bridge the digital divide since smartphones provide more Internet access to underserved communities than in-home internet.36–38 Additionally, we observed that that Black and Hispanic individuals reported more interest in using mHealth technologies than White participants, and that this interest was not linked to education level and yearly income, further supporting that smartphone technology may help overcome the digital divide to facilitate remote health management.
As of 2014, more than half (62%) of smartphone users in the US reported using their phones to look up information about a health condition39, and 32% specifically used medical-related apps.39–42 We also found that about one-third of participants (35.9%) reported use of an mHealth app, primarily for learning about health conditions, looking up nutrition or diet information, or accessing their medical record, which is likely driven by the types mHealth apps available for those with kidney disease that focus mainly on patient education rather than tracking health information.43 mHealth apps that focus on tracking health parameters, facilitating remote monitoring and supporting self-management behaviors could represent a major opportunity to improve management of CKD, which are particularly relevant to the remotely delivered nephrology care that has exponentially grown during the coronavirus pandemic.44 Importantly, a recent systematic review found that mHealth self-management interventions were highly feasible, usable and acceptable, and have the potential to improve CKD patients’ management and health outcomes.45 However, the effectiveness of the interventions is still inconclusive and warrants further research.
Among this cohort of individuals with non-dialysis CKD, several participants opposed the future use of mHealth technologies. Those opposed tended to be older and not currently use the internet or email, and therefore might have a low level of ‘digital readiness’, which is the willingness to use technology to navigate one’s environment, solve problems, or make decisions. A recent report has shown that many US adults have low digital readiness.46 This willingness, or ‘digital readiness’, highlights that in order for mHealth technologies to be effective, one must not only have access to technology, but also be willing to use it. More research is needed to assess the readiness of using mHealth technology among those with CKD.
A major concern reported by CRIC participants about using digital and mHealth technologies included the fear of losing face-to-face interaction with clinic staff. In prior reports, individuals with chronic disease have reported an overwhelming preference to receive health-related education and advice from a professional47 and most patients prefer mHealth in conjunction with visits to the doctors.48 Therefore, mHealth is likely an accessory to, rather than a replacement for the perceived quality of patient provider interactions in the management of chronic diseases.
Reported barriers to using mHealth technologies closely linked to physical limitations, which likely relates to the advancing age and growing number of comorbidities among individuals with CKD. In general, internet and mHealth use has been shown to be inversely related to age and number of medical conditions,25,33 with many older adults reporting comorbid conditions, disabilities, or other types of physical limitations that might prevent them from fully utilizing health related digital technologies.23 More research is needed to more clearly identify the reasons why certain populations such as older adults do not use mHealth technologies, and if supporting the use of mHealth technologies for CKD management can improve outcomes.
It is important to target a population’s eHealth literacy level to successfully leverage the capabilities of digital and mHealth technologies for disease management. Assessing eHealth literacy is especially vital for the CKD population since many are already at risk for low technology use due to older age, lower socioeconomic status, and inadequate health literacy. To date, eHealth literacy has not been well characterized among individuals with CKD. In our study, approximately three-quarters of the individuals had inadequate eHealth literacy, suggesting that lack of adequate eHealth literacy will likely serve as a barrier to fully leveraging the benefits of mHealth technologies in this population. Older age and less technology use were associated with inadequate eHealth literacy; both of which likely relate to the level of familiarity and confidence in utilizing technology to carry out tasks, as demonstrated by findings from a 2017 Pew Research Survey in which 34% of internet users aged 65 and older reported they had little-to-no confidence in their ability to use electronic devices to perform online tasks23 and our observation that confidence in managing one’s chronic disease was associated with adequate eHealth literacy. In combination, these findings support the potential role for perceived confidence and adequate eHealth literacy in the CKD population.
This study’s strengths include representation of a large number of well-characterized individuals from multiple locations across the US and inclusion of a wide range of ages, including older adults, as well as several racial and ethnic groups. Additionally, this is the largest study to date to describe technology use and eHealth literacy in the population with CKD in the US. However, there are several limitations. Due to the observational study design, we are not able to assess causality and are susceptible to residual confounding, particularly by socio-economic status, since we were only able to adjust for education and household income, and by location (urban vs. rural), which has been shown to influence technology access in other studies.24 To best account for location, we adjusted for recruitment site. Additionally, not all survey questions were validated, and we had incomplete data on response rates, which both limit the external validity of our findings. Questions assessing the interest in future use of mHealth specifically focused on medication management or participation in a research study, and this interest may not apply to other mHealth applications. Furthermore, our qualitative data collection did not give the opportunity to expand on identified themes due to lack of follow up or formal interview, which limits the depth of exploration of individual experiences. Lastly, ascertainment bias is a concern since the study utilized a convenience sampling strategy and healthier and more engaged individuals may have decided to complete the surveys and participate in the CRIC Study in general.
In summary, many individuals with non-dialysis CKD currently use the internet/email and smartphones, and are interested in using mHealth in the future, but few use mHealth apps or have adequate eHealth literacy. mHealth technologies have the potential to allow for greater digital equity, given that internet accessibility is more available via smartphones among underserved communities, racial minorities, adults with less education, and lower incomes, and since minorities reported more interest in using mHealth and digital technologies. Leveraging mHealth represents a potential opportunity to engage individuals with CKD, but further research needs to be conducted regarding barriers to use, inadequate eHealth literacy, and low digital readiness.
Supplementary Material
Supplemental Methods
Table S1: Survey questions used to determine study outcomes.
Table S2: Characteristics of CRIC participants who did and did not respond to the e-Literacy Survey, by question type.
Table S3: Associations of Baseline Characteristics with eHealth Literacy Domains.
Acknowledgments
Support: This work was supported by grant K23-DK099385-01A1 (CJD), K23DK118198-01A1 (SJS) from the National Institute of Diabetes and Digestive and Kidney Diseases. RRT reports NIH grant support. Funding for the CRIC Study was obtained under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (U01DK060990, U01DK060984, U01DK061022, U01DK061021, U01DK061028, U01DK060980, U01DK060963, U01DK060902 and U24DK060990). In addition, this work was supported in part by: the Perelman School of Medicine at the University of Pennsylvania Clinical and Translational Science Award NIH/NCATS UL1TR000003, Johns Hopkins University UL1 TR-000424, University of Maryland GCRC M01 RR-16500, Clinical and Translational Science Collaborative of Cleveland, UL1TR000439 from the National Center for Advancing Translational Sciences (NCATS) component of the National Institutes of Health and NIH roadmap for Medical Research, Michigan Institute for Clinical and Health Research (MICHR) UL1TR000433, University of Illinois at Chicago CTSA UL1RR029879, Tulane COBRE for Clinical and Translational Research in Cardiometabolic Diseases P20 GM109036, Kaiser Permanente NIH/NCRR UCSF-CTSI UL1 RR-024131, Department of Internal Medicine, University of New Mexico School of Medicine Albuquerque, NM R01DK119199. The funders had no a role in study design, data collection, analysis, reporting, or the decision to submit for publication.
Footnotes
Financial Disclosure: The authors declare that they have no relevant financial interests.
Peer Review: Received March 1, 2020. Evaluated by 3 external peer reviewers and a statistician, with editorial input from an Acting Editor-in-Chief (Editorial Board Member Allison Tong, PhD). Accepted in revised form October 8, 2020. The involvement of an Acting Editor-in-Chief to handle the peer-review and decision-making processes was to comply with AJKD’s procedures for potential conflicts of interest for editors, described in the Information for Authors & Journal Policies.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kay M, Santos J, Takane M. mHealth: New horizons for health through mobile technologies. World Health Organization, Global Observatory for e-Health. 2011;64(7):66–71. [Google Scholar]
- 2.Fjeldsoe BSMA, Miller YD. Behavior change interventions delivered by mobile telephone short-messaging service. Am J Prev Med. 2009;36(2):165–173. [DOI] [PubMed] [Google Scholar]
- 3.Hurling RCM, Boni MD, Fairley BW, Hurst T, Murray P, Richardson A, Sodhi JS. Using internet and mobile phone technology to deliver an automated physical activity program: randomized controlled trial. J Med Internet Res. 2007;9(e7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schrauben S, Hsu J, Rosas S, et al. CKD Self-management: Phenotypes and Associations With Clinical Outcomes. Am J Kidney Dis. 2018;72:360–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ong S, Jassal S, Miller J, et al. Integrating a Smartphone-Based Self-Management System into Usual Care of Advanced CKD. CJASN. 2016;11:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Becker S, Kribben A, Mesiter S, Diamantidis C, Unger N, Mitchell A. User profiles of a smartphone application to support drug adherence-experiences from the iNephro project. PLoS One. 2013;8(e78547). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tuot D, Diamantidis C, Corbett C, et al. The last mile: Translational research to improve CKD outcomes. Clin J Am Soc Nephrol. 2014;9:1802–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feldman HI, Appel LJ, Chertow GM, et al. The Chronic Renal Insufficiency Cohort (CRIC) Study: Design and methods.. J Am Soc Nephrol. 2003;14(Suppl 2):S148–S153. [DOI] [PubMed] [Google Scholar]
- 9.Lash JP, Go AS, Appel LJ, et al. Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol. 2009;4:1302–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nguyen J, Moorhouse M, Curbow B, Christie J, Walsh-Childers K, Islam S. Construct Validity of the eHealth Literacy Scale (eHEALS) Among Two Adult Populations: A Rasch Analysis. JMIR Public Health Surveill. 2016;2:e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Norman C, Skinner H. eHEALS: The eHealth Literacy Scale. J Med Internet Res. 2006;8:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vart P, Gansevoort R, Joosten M, Bultmann U, Reijneveld S. Socioeconomic disparities in chronic kidney disease: A systematic review and meta-analysis. Am J Prev Med. 2015;48:580–592. [DOI] [PubMed] [Google Scholar]
- 13.Butler J, Carter M, Hayden C, et al. Understanding adoption of a personal health record in rural health clinics: Revealing barriers and facilitators of adoption including attributions about potential patient portal users and self-reported characteristics of early adopting users. AMAI Annu Symp Proc. 2013;2013:152–161. [PMC free article] [PubMed] [Google Scholar]
- 14.Berkman N, Seridan S, Donahue E, Halpern D, Crotty K. Low health literacy and health outcomes: an updated systemic review. Ann Intern Med. 2011;155(2):97–107. [DOI] [PubMed] [Google Scholar]
- 15.Charlson M, Pompei P, Ales K, MacKenzie C. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 16.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- 17.Craven JL, Rodin GM, Littlefield C. The Beck Depression Inventory as a screening device for major depression in renal dialysis patients. Int J Psychiatry Med. 1988;18:365–374. [DOI] [PubMed] [Google Scholar]
- 18.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48(8):314–318. [PubMed] [Google Scholar]
- 19.Lubben J, Blozik E, Gillmann G, et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European Community-dwelling older adult populations. Gerontologist. 2006;46(4):503–513. [DOI] [PubMed] [Google Scholar]
- 20.Lorig K, Sobel D, Ritter P, Laurent D, Hobbs M. Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program for patients with chronic disease. Effective Clinical Practice, 4, 2001,pp. 256–262. Effective Clinical Practice. 2001;4:256–262. [PubMed] [Google Scholar]
- 21.Anderson A, Yang W, Hsu C, et al. Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2012;60:250–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pew Research Center. Record shares of Americans now own smartphones, have home broadband. www.pewresearch.org/fact-tank/2017/01/12/evolution-of-technology/. Published 2017. Accessed May 17, 2019.
- 23.Anderson M, Perrin A. Tech Adoption Climbs Among Older Adults. Pew Research Center;2017. [Google Scholar]
- 24.Pew Research Center: Internet & Technology. 2018.
- 25.Kontos E, Blake K, Chou W, Prestin A. Predictors of eHealth usage: Insights of the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res. 2014;16:e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sarkar U, Karter A, Liu J, et al. Social disparities in internet patient portal use in diabetes: Evidence that the digial divide extends beyond access.. J Am Med Inform Assoc. 2011;18:318–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zou G A modified poisson regression approach to prospective studies with binary data.. Am J Epidemiol. 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 28.Greenland S Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–305. [DOI] [PubMed] [Google Scholar]
- 29.Behrens T, Taeger D, Wellmann J, Keil U. Different methods to calculate effect estimates in cross-sectional studies. A comparison between prevalence odds ratio and prevalence ratio. Methods Inf Med. 2004;43:505–509. [PubMed] [Google Scholar]
- 30.Bryant A, Charmaz K. The SAGE Handbook of Grounded Theory. Thousand Oaks, CA: Sage; 2007. [Google Scholar]
- 31.McGillicuddy J, Weiland A, Frenzel R, et al. Patient Attitudes Toward Mobile Phone-Based Health Monitoring: Questionnaire Study Among Kidney Transplant Recipients. J Med Internet Res. 2013;15(1):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bonner A, Gillespie K, Campbell K, et al. Evaluating the prevalence and opportunity for technology use in chronic kidney disease patients: a cross-sectional study. BMC Nephrology. 2018;19:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choi N, Dinnito D. The digital divide among low-income homebound older adults: internet use patterns, eHealth literacy, and attitudes toward computer/Internet use. J Med Internet Res. 2013;15(5):e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lorence D, Park H, Fox S. Racial disparities in health information access: resilience of the digital divide. J Med Syst. 2006;30(4):241–249. [DOI] [PubMed] [Google Scholar]
- 35.Yamin C, Emani S, Williams D, et al. The digital divide in adoption and use of a personal health record.. Arch Intern Med. 2011;171:568–574. [DOI] [PubMed] [Google Scholar]
- 36.Smith A A Portrait of Smartphone Ownership. Pew Research Institute;2015. [Google Scholar]
- 37.Zickuhr K, Smith A. Digital Differences. Pew Research Center;2012. [Google Scholar]
- 38.Pew Research Center: Mobile Access. http://www.pewinternet.org/Reports/2010/Mobile-Access-2010.aspx. Published 2010. Accessed June 5, 2019.
- 39.Smith A Smartphone Use in 2015. Pew Research Center;2015. [Google Scholar]
- 40.Lella A The U.S. Mobile App Report. https://www.comscore.com/Insights/Presentations-and-Whitepapers/2014/The-US-Mobile-App-Report. Published 2014. Accessed June 5, 2019. [Google Scholar]
- 41.Japsen B Health App Usage Soars as Consumers Take Charge. 2015.
- 42.Tracking for Health, 2013. Pew Research Center; 2013. [Google Scholar]
- 43.Singh K, Diamantidis C, Ramani S, et al. Patients’ and Nephrologists’ Evaluation of Patient-Facing Smartphone Apps for CKD. Clin J Am Soc Nephrol. 2019;14:523–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jain G, Ahamd M, Wallace E. Technology, telehealth and nephrology: The time is now. Kidney360. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shen H, van der Kleij R, van der Boog P, Chang X, Chavannes N. Electronic Health Self-Management Interventions for Patients with Chronic Kidney Disease: Systematic Review of Quantitative and Qualitative Evidence.. J Med Internet Res. 2019;21(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Center PR. Digital Readiness Gaps. September 20, 2016. 2016.
- 47.Kuehn B Patients on online seeking support, practical advice on health conditions. JAMA. 2011;305(16):1664–1665. [DOI] [PubMed] [Google Scholar]
- 48.Rai A, Chen L, Pye J, Baird A. Understanding determinants of consumer mobile health usage intentions, assimilaion, and channel preferences. J Med Internet Res. 2013;15(8):e149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Methods
Table S1: Survey questions used to determine study outcomes.
Table S2: Characteristics of CRIC participants who did and did not respond to the e-Literacy Survey, by question type.
Table S3: Associations of Baseline Characteristics with eHealth Literacy Domains.