Abstract
Despite clinical observations of cardiotoxicity among cancer patients treated with tyrosine kinase inhibitors (TKIs), the molecular mechanisms by which these drugs affect the heart remain largely unknown. Mechanistic understanding of TKI-induced cardiotoxicity has been limited in part due to the complexity of tyrosine kinase signaling pathways and the multi-targeted nature of many of these drugs. TKI treatment has been associated with reactive oxygen species generation, mitochondrial dysfunction, and apoptosis in cardiomyocytes. To gain insight into the mechanisms mediating TKI-induced cardiotoxicity, this study constructs and validates a computational model of cardiomyocyte apoptosis, integrating intrinsic apoptotic and tyrosine kinase signaling pathways. The model predicts high levels of apoptosis in response to sorafenib, sunitinib, ponatinib, trastuzumab, and gefitinib, and lower levels of apoptosis in response to nilotinib and erlotinib, with the highest level of apoptosis induced by sorafenib. Knockdown simulations identified AP1, ASK1, JNK, MEK47, p53, and ROS as positive functional regulators of sorafenib-induced apoptosis of cardiomyocytes. Overexpression simulations identified Akt, IGF1, PDK1, and PI3K among the negative functional regulators of sorafenib-induced cardiomyocyte apoptosis. A combinatorial screen of the positive and negative regulators of sorafenib-induced apoptosis revealed ROS knockdown coupled with overexpression of FLT3, FGFR, PDGFR, VEGFR, or KIT as a particularly potent combination in reducing sorafenib-induced apoptosis Network simulations of combinatorial treatment with sorafenib and the antioxidant N-acetyl cysteine (NAC) suggest that NAC may protect cardiomyocytes from sorafenib-induced apoptosis.
Keywords: cardiotoxicity, tyrosine kinase inhibitor, cardiomyocyte, apoptosis, computational model, systems biology
Introduction
Cardiovascular disease is the leading cause of death among long-term cancer survivors (1). Several chemotherapeutic agents, including small molecule tyrosine kinase inhibitors (TKIs), may predispose cancer patients to cardiomyopathies. TKIs, which inhibit oncogenic tyrosine kinases, were developed as targeted therapies to minimize damage to healthy cells compared to broadly cytotoxic chemotherapies. However, the use of TKIs in cancer therapy has still been associated with certain adverse effects, one of which is cardiotoxicity (2). This cardiotoxicity can manifest itself in several ways, including hypertrophy, infarction, and heart failure (2,3).
Cardiotoxicities of TKIs fall into on-target and off-target categories (4). In on-target toxicity, the primary kinase target of the TKI is involved in signaling pathways important in the growth and survival of cardiomyocytes. However, many TKIs non-specifically inhibit multiple other kinases in addition to the primary target, resulting in off-target toxicity. Observations of drug-induced adverse events made by healthcare professionals, consumers, and manufacturers are currently recorded in the United States Food and Drug Administration Adverse Event Reporting System (FAERS) database (5). While these reports may indicate which drugs are cardiotoxic (6), they do not offer explanatory insight into the mechanisms of drug-induced cardiotoxicity. Due to the complexity of tyrosine kinase signaling pathways and the multitude of kinases targeted by these drugs both directly and indirectly, the molecular mechanisms underlying their cardiotoxicity remain largely unknown (7). This study applies a computational modeling approach to conduct a systematic, network-based investigation of the mechanisms mediating TKI-induced cardiotoxicity.
Previous studies have observed decreased cell viability, reactive oxygen species (ROS) generation, changes in morphology, and apoptosis in cardiomyocytes in response to TKI treatment (2,8), suggesting connections between tyrosine kinase signaling pathways and intrinsic apoptotic signaling pathways. By developing a computational model of cardiomyocyte apoptosis, the present study aimed to identify the specific interactions between these pathways that may be responsible for TKI-induced cardiotoxicity. The mechanistic insights gained from this model suggest new drug targets and therapeutic approaches to minimize and mitigate the cardiotoxicity associated with TKIs, which may result in better outcomes for cancer patients.
Results
A predictive computational model of cardiomyocyte apoptosis
The signaling intermediates (“species”) and reactions in the constructed cardiomyocyte apoptosis network were based on experimental results extracted from 97 published studies referencing tyrosine kinase signaling pathways and apoptotic signaling pathways. Studies investigating cardiomyocyte responses to relevant perturbations, such as the effects of ROS or TKI treatment on the activity of downstream species such as caspases 3 and 9, anti-apoptotic proteins such as Bcl-2, and pro-apoptotic proteins such as Bax and Bad, were set aside for later use in model validation. The network was then converted into a predictive computational model using a logic-based differential equation (LDE) approach, where activating and inhibiting reactions in the network are modeled using normalized Hill functions combined with AND and OR logic gates (see Methods) (9).
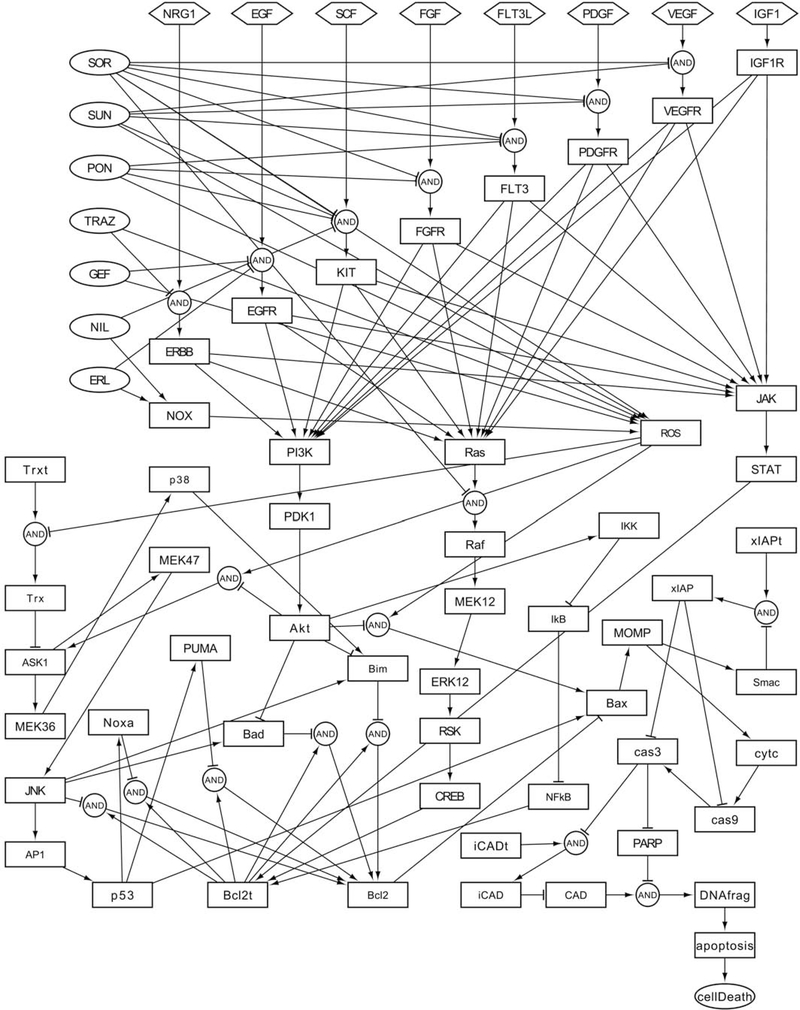
The model consists of 69 species involved in 112 reactions (Fig. 1), integrating the signaling pathways of eight receptor tyrosine kinases (EGFR, ERBB, FGFR, FLT3, IGF1R, KIT, PDGFR, and VEGFR) with intrinsic apoptotic signaling pathways, ultimately leading from receptor inputs (i.e. EGF, FGF, FLT3L, IGF1, NRG1, PDGF, SCF, and VEGF) to an output of apoptosis and cell death (Table S1). In intrinsic apoptosis, the pro-apoptotic proteins Bax, Bad, Bim, Noxa, and Puma induce mitochondrial outer membrane permeabilization (MOMP), either by directly puncturing the mitochondrial outer membrane, as in the case of Bax, or by inhibiting anti-apoptotic proteins such as Bcl-2, allowing for Bax-induced membrane permeabilization (10). After Bax forms pores in the membrane, cytochrome c is released into the cytosol, stimulating caspase activation and resulting in cell death and apoptosis. Seven TKIs known to be cardiotoxic are modeled in the network: erlotinib (ERL), gefitinib (GEF), nilotinib (NIL), ponatinib (PON), sorafenib (SOR), sunitinib (SUN), and trastuzumab (TRAZ). The targets of these drugs are listed in Table 1. Modeled targets were selected based on the availability of experimental data linking targets to apoptotic signaling pathways. The BCR and ABL1 kinases were not incorporated into the network as they are primarily targeted as parts of the oncogenic fusion protein BCR-ABL1 (11), which would not be expected under normal physiological conditions.
Fig. 1. Cardiomyocyte apoptosis network.
The network consists of 69 signaling intermediates (“species”) involved in 112 activating and inhibiting reactions joined by logical AND and OR gates. Network species and reactions are defined in Table S1.
Table 1. Tyrosine kinase inhibitors (TKIs) modeled in the network and their targets.
Targets incorporated into the network shown in bold. Data on TKI targets was obtained from the DrugBank database.
| TKI | Targets |
|---|---|
| Erlotinib (ERL) | EGFR |
| Gefitinib (GEF) | EGFR |
| Nilotinib (NIL) | ABL1, KIT |
| Ponatinib (PON) | ABL1, BCR, KIT, RET, TEK, FLT3, FGFR1, FGFR2, FGFR3, FGFR4 |
| Sorafenib (SOR) | BRAF, RAF1, VEGFR3, VEGFR2, FLT3, PDGFRB, KIT, FGFR1, RET, VEGFR1 |
| Sunitinib (SUN) | PDGFRB, VEGFR1, KIT, VEGFR2, VEGFR3, FLT3 |
| Trastuzumab (TRAZ) | ERBB2 |
Network parameters were set as in previously described models (weight = 1, n = 1.4, T = 1, and EC50 = 0.5) (9,12–14). The baseline condition was defined by an input value of 0.175 for all tyrosine kinase receptor inputs (growth factors) and a 0.05 ROS input, representing normal physiological signaling activity. These input values were chosen to induce mid-level activation of the pro-survival protein Akt and a low level of caspase 3 activity at baseline. All simulations were run to steady-state. Network simulations showed no apoptosis under the baseline condition.
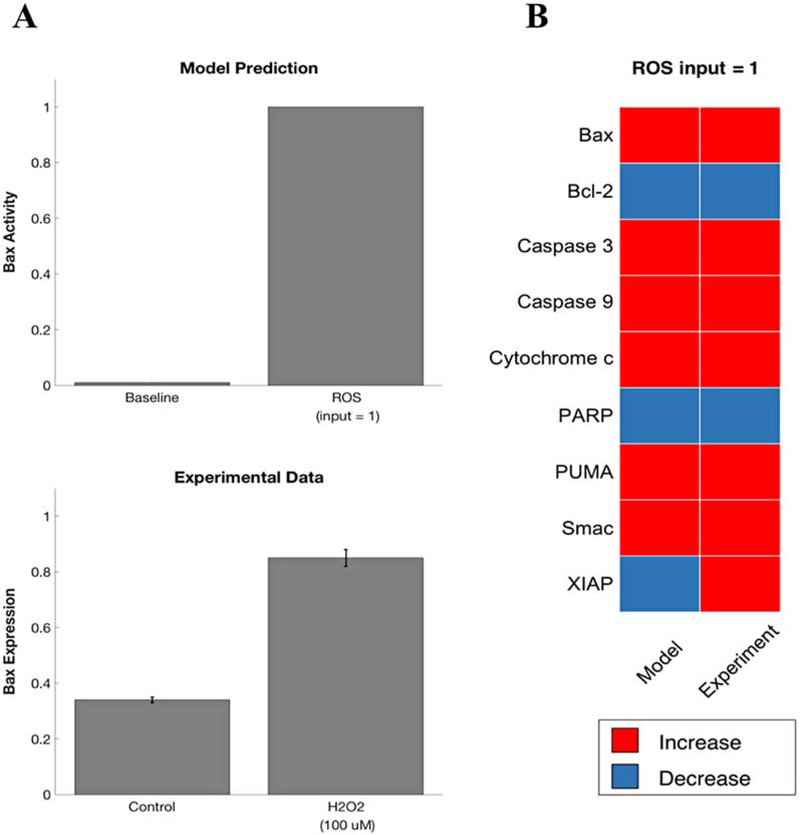
Prior to examining network responses to TKI treatments, validation of model predictions against experimental data not used in defining the model structure was performed to ensure that the network could predict ROS-induced apoptosis, consistent with experimental studies. Experimental observations from published literature were qualitatively coded as “increase,” “decrease,” or “no change” relative to the control condition, and then compared with model predictions for change in activity of relevant species relative to baseline. A 0.5% threshold was used to define change for model predictions. For example, the effect of a ROS input of 1 (100% activity) on the network protein Bax was simulated and compared to experimental data obtained by Hu et al. (Fig. 2A). The model predicts that a ROS input of 1 will markedly increase Bax activity; similarly, Hu et al. observed an increase in Bax protein expression in H9c2 cardiomyoblasts exposed to H2O2 (15). For a ROS input value of 1, the model correctly predicts 89% (8/9) of experimental observations (Fig. 2B) (15–17).
Fig. 2. Model validation for ROS input.
A) Comparing model predictions for a ROS input of 1 to experimental data from Hu et al. (13) showing an increase in Bax protein expression following exposure to H2O2. B) Validation of model predictions against experimental results (13–15). Increase/decrease compared to the baseline condition. For model predictions, no change defined as <0.5% change in fractional activation compared to baseline.
Predicting network responses to TKIs
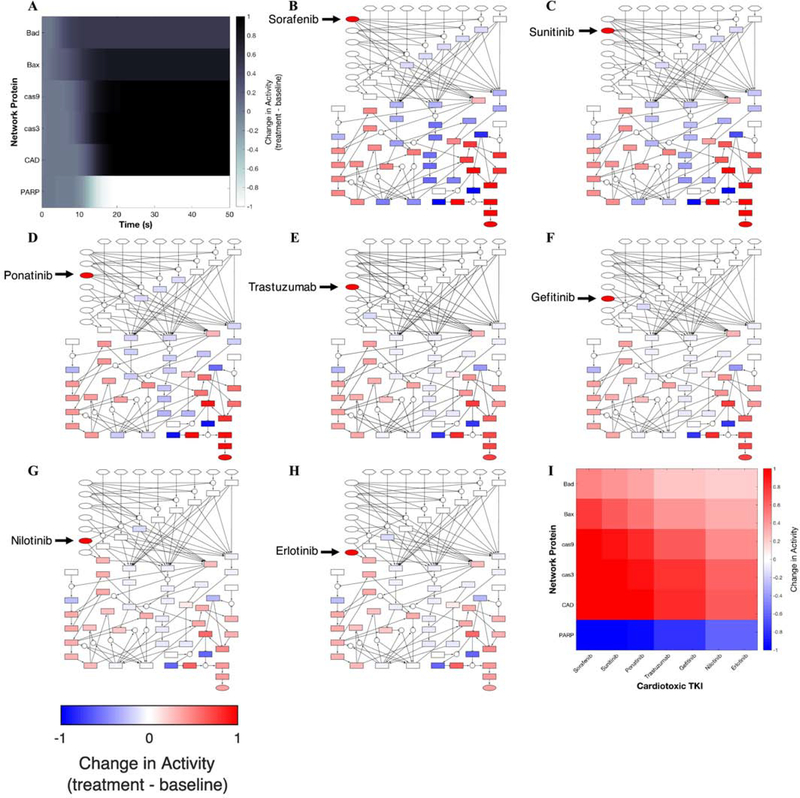
After validating that the model could accurately predict ROS-induced apoptosis, perturbation simulations were run for the TKI sorafenib to identify how this drug may be enacting cardiotoxic responses in cardiomyocytes. Dynamics of network proteins Bad, Bax, caspases 3 and 9, CAD, and PARP in response to sorafenib treatment are shown in Fig. 3A. Activity of several proteins associated with apoptosis, Bad, Bax, caspase 3, and caspase 9, increases relative to baseline over time, whereas activity of PARP, an enzyme involved in DNA repair, decreases over time. The model predicts high levels of apoptosis following treatment with sorafenib, as evidenced by upregulated pro-apoptotic species compared to the baseline condition, including caspases 3 and 9, Bax, and Bad (Fig. 3B). Network simulations were also run for treatment of the TKIs erlotinib, gefitinib, nilotinib, ponatinib, sunitinib, and trastuzumab. The model predicts high levels of apoptosis following treatment with sunitinib, ponatinib, trastuzumab, and gefitinib (Fig. 3C-F), and lower levels of apoptosis for nilotinib and erlotinib (Fig. 3G-H). The differential effects of the simulated TKIs on several network proteins are summarized in Fig. 3I. Out of the seven simulated TKIs, sorafenib exerted the strongest apoptotic response, followed by sunitinib, then ponatinib. Nilotinib and erlotinib exerted the weakest apoptotic responses.
Fig. 3. Cardiotoxic drug perturbation simulations.
A) Predicted dynamics of selected network proteins in response to sorafenib. Change in cardiomyocyte apoptosis network activity following treatment with B) Sorafenib, C) Sunitinib, D) Ponatinib, E) Trastuzumab, F) Gefitinib, G) Nilotinib, and H) Erlotinib. Caspases 3 and 9 are upregulated in response to all treatment conditions, confirming that the model predicts apoptosis for these seven TKIs. I) Change in activity of network proteins Bad, Bax, caspase 9, caspase 3, CAD, and PARP in response to the seven simulated TKI treatments.
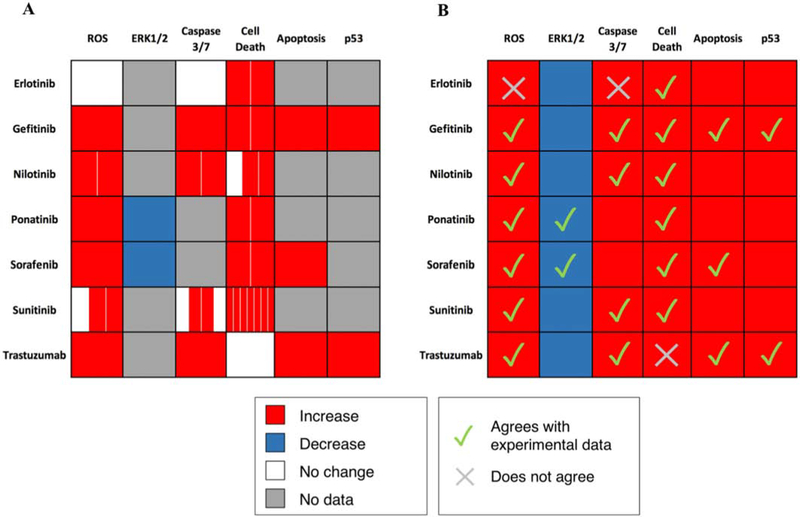
Model predictions of TKI-induced apoptosis were then validated against the results of 51 experimental studies examining the effects of TKI treatments on cardiomyocytes in vitro. Again, published experimental observations were coded as “increase,” “decrease,” or “no change” relative to the control condition, and compared with model predictions for change in activity of relevant species relative to baseline, using a 0.5% threshold to define change for model predictions, consistent with the thresholds used by previously published network validations, which have ranged from 0.1% to 5% (12–14). The model correctly predicts 82.5% (66/80) of experimental observations. Papers used in model validation are documented in Table S2, which are distinct from those used to define the model (Table S1). A subset of the validation results is shown in Fig. 4 (18–36). Some model predictions could not be validated due to a lack of experimental data, as seen in Fig. 4B.
Fig. 4. Validation of model predictions against manually-curated experimental data from the literature.
A) Results of experimental studies examining the effects of TKI treatments on cardiomyocytes in vitro (16–34). Each subcell represents a separate study in the literature. B) Model predictions of effects of TKI treatments. For model predictions, no change defined as <0.5% change in activity compared to baseline.
Model robustness in response to parameter variation was evaluated by examining changes in validation accuracy upon generation of new parameter sets sampled from uniform random distributions. Validation accuracy was robust (>70%) to variation in model parameters using a uniform random distribution of ±25% for ymax, and using a distribution range of ±50% for w, n, and EC50 (Fig. S1), consistent with other studies using an LDE approach (12,13). No changes in validation accuracy occurred when τ or yinit were varied. High validation accuracy (>70%) was observed in response to ±50% changes in baseline input reaction weights when TKI inputs were held at their original level of 1. Validation accuracy remained high when TKI inputs were decreased up to 30% of their original values for baseline input weights between -50% and +20% of their original values (Fig. S2). Overall, preservation of validation accuracy over a wide range of parameters demonstrates the robustness of the model to variation in parameters.
Model predictions were further compared to RNA sequencing data from Wang et al. (37), examining gene expression changes in human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) after treatment with one of four cardiotoxic TKIs: erlotinib, lapatinib, sorafenib, and sunitinib. Performing 6 different treatments for each drug, varying both dose and time: 1 μM for 24 hours, 3.16 μM for 6, 24, 72 and 168 hours, and 10 μM for 24 hours, with three replicates per treatment per drug, Wang et al. identified 8,567 transcripts that were significantly regulated by any one treatment condition. The list of differentially expressed genes included several species in the cardiomyocyte apoptosis network that were likely to be transcriptionally regulated: AP1, Bax, Noxa, PUMA, p53, Bcl2, and Bim, prompting comparison of the log2 fold changes in expression between the drug-treated condition and the control determined by RNA sequencing and the log2 fold changes in activity between the drug-treated (50 second sorafenib treatment) and baseline conditions predicted by the model. In agreement with model predictions, the RNA sequencing data for sorafenib treatment shows that sorafenib treatment increased expression of pro-apoptotic species Noxa, PUMA, and p53 (Fig. 5). Model predictions also agree with experimental results for Bax and Bim in the 3.16 μM 72-hour treatment condition; however, this agreement varies with other times and doses. While the nodes shown in Fig. 5 are all regulated transcriptionally, the model nodes represent protein activity, which is due to a combination of transcriptional and post-transcriptional regulation. For example, AP1 and Bcl2 are predicted to be regulated in directions opposite to that measured by mRNA, suggesting potential negative feedbacks that are missing in the model. Further, dose- and time-related differences in gene expression limit the ability to draw additional conclusions about the model’s predictive capabilities using this data.
Fig. 5. Comparison of model predictions and RNA sequencing data from Wang et al. (35) for sorafenib treatment.
Both model predictions and experimental results show an increase in Noxa, PUMA, and p53 activity in response to sorafenib.
Identifying functional regulators of TKI-induced apoptosis
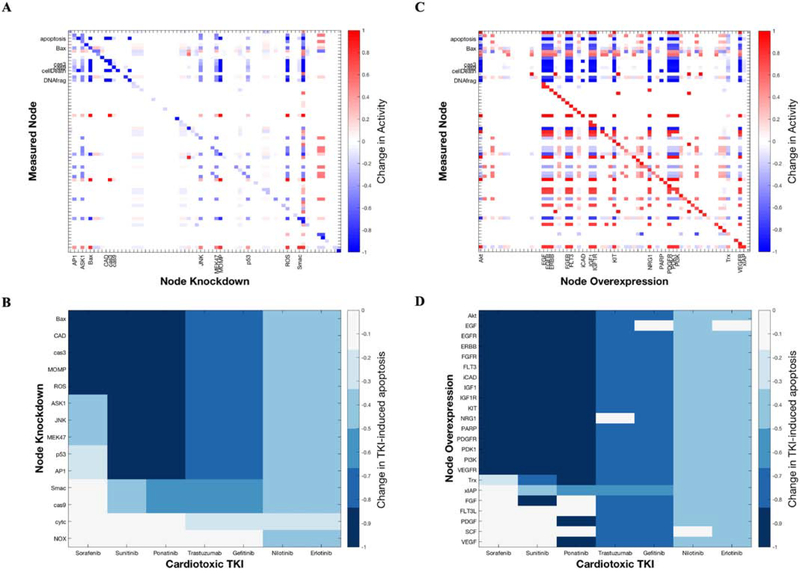
Since sorafenib induced the greatest apoptotic response among the seven drugs simulated, functional regulators of sorafenib-induced apoptosis were examined by sensitivity analysis. A knockdown of each species in the network was simulated by setting its maximum activity value to 0. Change in activity was calculated for each species by subtracting the activity at steady-state with sorafenib treatment from the activity at steady-state under each knockdown condition with sorafenib treatment. A decrease in apoptosis was observed with knockdown of AP1, ASK1, Bax, CAD, cas3, JNK, MEK47, MOMP, p53, and ROS, suggesting that these species positively regulate sorafenib-induced apoptosis (Fig. 6A) – while knockdown of Bax, CAD, cas3, and MOMP is expected to decrease apoptosis, as these nodes are traditionally considered pro-apoptotic, AP1, ASK1, JNK, MEK47, p53, and ROS present interesting therapeutic targets to mitigate sorafenib-induced apoptosis. The sensitivities of the top 14 positive regulators of apoptosis (i.e. network species that produced the greatest decrease in apoptosis when knocked down) among the seven TKIs are shown in Fig. 6B. This shows that while a number of positive regulator nodes are conserved across TKIs (e.g. Bax, cas3, and ROS), other nodes had more TKI-specific effects (e.g. p53 knockdown being less effective for sorafenib).
Fig. 6. Functional regulators of TKI-induced apoptosis.
A) Knockdown of network species AP1, ASK1, JNK, MEK47, p53, and ROS decreases in sorafenib-induced apoptosis, indicating that these species are positive regulators of apoptosis. B) Top positive regulators of sorafenib-, sunitinib-, ponatinib-, trastuzumab-, gefitinib-, nilotinib-, and erlotinib-induced apoptosis. C) Overexpression of network species Akt, IGF1, PDK1, and PI3K reduces sorafenib-induced apoptosis. D) Top negative regulators (mitigators) of TKI-induced apoptosis.
Overexpression simulations were used to identify negative functional regulators, or mitigators of sorafenib-induced apoptosis. Overexpression was simulated by setting the initial activity of a node to 1 and its time constant to 1000 (38). Change in activity for each node was calculated by subtracting the fractional activation at steady-state with sorafenib treatment from the fractional activation at steady-state under each overexpression condition with sorafenib treatment. A decrease in apoptosis was observed with overexpression of Akt, EGF, EGFR, ERBB, FGFR, FLT3, iCAD, IGF1, IGF1R, KIT, NRG1, PARP, PDGFR, PDK1, PI3K, and VEGFR, suggesting that increasing the activity of these nodes may mitigate the extent of apoptosis induced by sorafenib (Fig. 6C). The sensitivities of the top 23 negative regulators of apoptosis (i.e. network nodes that produced the greatest decrease in apoptosis when overexpressed) for the seven TKIs are shown in Fig. 6D. Again, some nodes acted as mitigators of apoptosis regardless of TKI (e.g. Akt, IGF1), while others mitigated apoptosis only when treated with specific TKIs. For example, VEGF overexpression mitigates apoptosis due to ponatinib but not sunitinib.
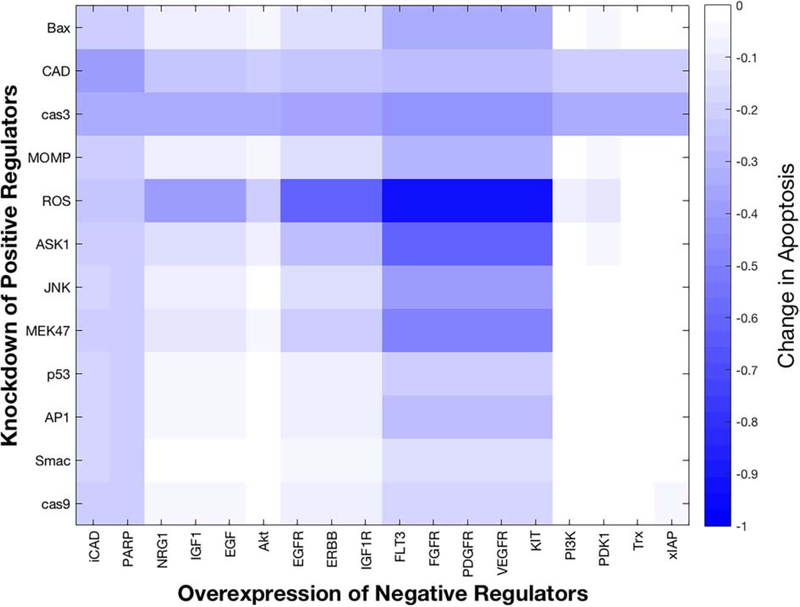
A combinatorial screen was performed using the functional regulators of sorafenib-induced apoptosis to determine whether there exist certain combinations of positive and negative functional regulators that most effectively reduce sorafenib-induced apoptosis (Fig. 7). Simulations involving complete knockdown of positive regulators (ymax = 0) and complete overexpression of negative regulators (yinit = 0, = 1000) did not reveal a differential effect as most combinations decreased sorafenib-induced apoptosis to 0, thus partial knockdown and partial overexpression simulations were used. Partial knockdown of a positive regulator was simulated by setting its ymax to 0.75, while partial overexpression of a negative regulator was simulated by setting its yinit to 0.25 and τ to 1000. Change in apoptosis for each combination of partial knockdown of a positive regulator coupled with partial overexpression of a negative regulator was calculated by subtracting the steady-state activity of the apoptosis node with sorafenib treatment from the steady-state apoptosis activity with the combination treatment and sorafenib. Knockdown of ROS accompanied by overexpression of FLT3, FGFR, PDGFR, VEGFR, or KIT most markedly and synergistically reduced sorafenib-induced apoptosis (Fig. 7). In contrast, caspase 3 knockdown was predicted to decrease apoptosis regardless of the paired negative regulator.
Fig. 7. Combinatorial screen using positive and negative regulators of sorafenib-induced apoptosis to identify pairwise combinations that may most effectively mitigate apoptosis.
Knockdown of positive regulator ROS coupled with overexpression of negative regulators FLT3, FGFR, PDGFR, VEGFR, or KIT results in the largest decrease in sorafenib-induced apoptosis.
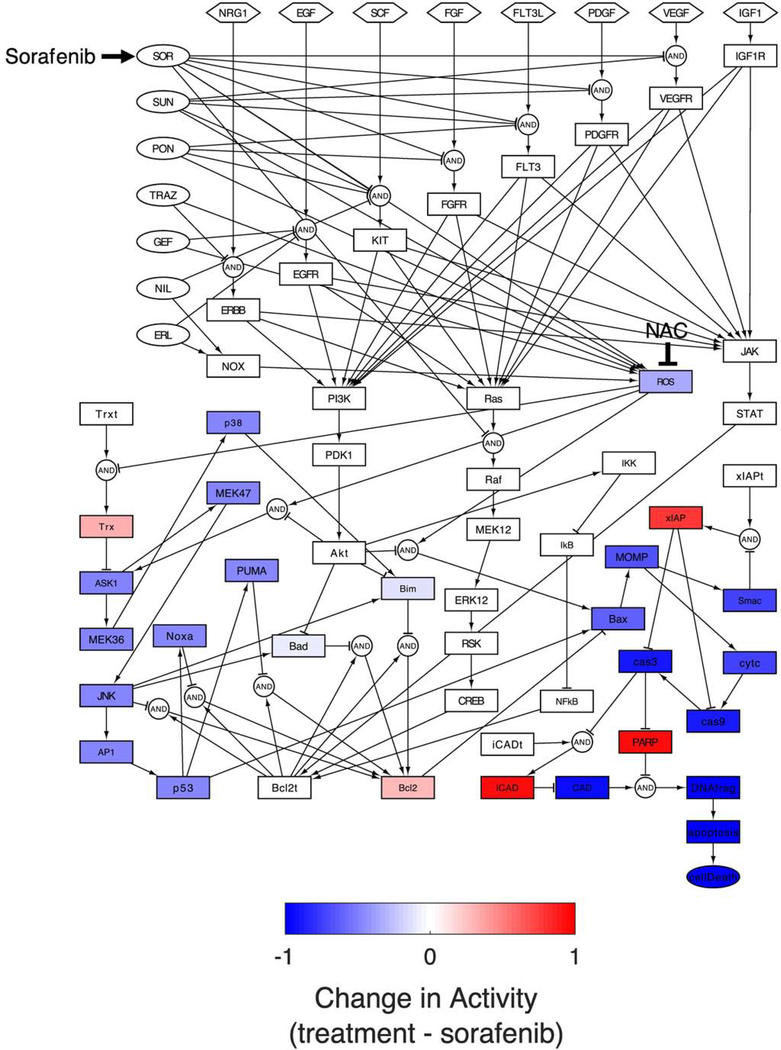
Among the functional regulators of sorafenib identified by sensitivity analysis, the positive regulator ROS stands out as one with prominent therapeutic potential, given the widespread availability of antioxidant products. Thus network simulations were performed using N-acetyl cysteine (NAC), a commonly used antioxidant, in combination with sorafenib to examine how inhibition of ROS would affect the level of sorafenib-induced apoptosis. As expected from sensitivity analysis, simultaneous treatment with sorafenib and NAC resulted in the reduction of apoptosis to baseline levels, suggesting that NAC and other antioxidants may mitigate TKI-induced apoptosis. Network visualization further illustrated how NAC mitigated the effect of sorafenib (Fig. 8). In comparison to the sorafenib-treated network in Fig. 3B, the model predicts that NAC suppresses the actions of ROS by two main routes: 1) a short path from oxidation of Bax, to MOMP, and caspase 3; 2) a longer path of ROS oxidation of ASK1, JNK, and p53 which again activates Bax. Thus, NAC is predicted to suppress multiple routes to sorafenib-induced apoptosis that appear to work together. Furthermore, as shown Fig. 6B, knockdown of ROS results in a decrease in apoptosis for all seven simulated TKIs. As such, inhibition of ROS via NAC or another antioxidant may also be expected to reduce apoptosis induced by sunitinib, ponatinib, trastuzumab, gefitinib, nilotinib, and erlotinib.
Fig. 8. Change in cardiomyocyte apoptosis network activity following simultaneous sorafenib and NAC inputs.
Combinatorial treatment with sorafenib and NAC protects against sorafenib-induced apoptosis.
Discussion
We manually reconstructed the cardiomyocyte apoptosis signaling network, which was converted into a predictive computational model using a logic-based differential equation approach. The model predicts apoptosis in response to all seven simulated TKIs, with the highest level of apoptosis in response to sorafenib and lower levels of apoptosis following nilotinib and erlotinib treatment. Model predictions were validated against experimental observations in literature studies, with a validation rate of 82.5% (66/80) for effects of TKI treatments on cardiomyocytes. Simulated knockdown and overexpression screens were performed to identify functional regulators of TKI-induced apoptosis. AP1, ASK1, JNK, MEK47, p53, and ROS were identified as negative functional regulators of sorafenib-induced apoptosis, while Akt, IGF1, PDK1, and PI3K were identified as positive functional regulators of sorafenib-induced apoptosis. A combinatorial screen revealed ROS knockdown together with overexpression of FLT3, FGFR, PDGFR, VEGFR, or KIT as combinations especially effective in reducing sorafenib-induced apoptosis. Network simulations revealed the antioxidant NAC as a mitigator of sorafenib-induced apoptosis and the mechanisms by which this reduction in apoptosis occurred.
Model validation
While the model correctly predicts over 80% of experimental observations, some of its predictions for erlotinib and trastuzumab disagree with published experimental studies. The model predicts an increase in ROS and caspase 3 activity for erlotinib treatment, whereas no change has been found in experimental studies (18). The model also predicts an increase in cell death for trastuzumab, although experimental findings indicate no change (35). A lack of cell death in response to trastuzumab treatment in an experimental study does not necessarily indicate that trastuzumab is not cytotoxic in cardiomyocytes in vitro, particularly if the dose tested was relatively low, as the cardiotoxic effects of TKIs have been found to be dose-dependent (39). Other input-output pairs in the model that do not align with experimental findings involve crosstalk between ROS and nodes in pro-survival pathways including Akt, CREB, and ERK12, which are not currently reflected in the model, but suggest areas for model improvement.
Differential cardiotoxicity in response to tyrosine kinase inhibitors
Not all TKIs are equally cardiotoxic. Previous studies have attempted to determine an index or ranking of TKI toxicity (39,40). While these metrics of TKI toxicity have varied substantially, most studies agree that sorafenib and sunitinib are highly cardiotoxic, whereas erlotinib is generally considered cardiosafe (39,41). Model predictions support the results of these studies, as erlotinib simulations show lower levels of apoptosis than sorafenib and sunitinib. Hasinoff et al. have found that the toxicity of TKIs may be related to a lack of target specificity (19). This is supported by model predictions. The simulated TKIs with the lowest effect on apoptosis, erlotinib and nilotinib, are modeled as selective TKIs with a single target (EGFR and KIT, respectively, as shown in Table 1). Sorafenib and sunitinib, however, have multiple targets in the model. These results may suggest that sorafenib and sunitinib produce a stronger apoptotic response than erlotinib due to a greater number of tyrosine kinase targets.
Drug mitigator combinations
To our knowledge, prior experimental studies have not examined the effects of combinatorial tyrosine kinase inhibitor-antioxidant treatments in cardiomyocytes. However, Damiano et al. found that 5 mM NAC treatment significantly decreased intracellular ROS and apoptosis induced by 20 μM nilotinib treatment in cancer cells (42). These results support model predictions of NAC’s potential use as a mitigator of sorafenib-induced apoptosis. In the context of sorafenib, ROS inhibition acted through parallel pathways that then converge to inhibit apoptosis, including Bax, Trx, and ASK1. Sharma et al. found that stimulation of cardiomyocytes with IGF1 and insulin can rescue TKI-induced toxicity in cardiomyocytes (39), lending strength to model predictions of IGF1 as a mitigator of sorafenib-induced apoptosis.
The combinatorial screen of the functional regulators of sorafenib-induced apoptosis suggested pairing an antioxidant with growth factor stimulation to reduce TKI toxicity, although further experimental investigation is needed. The development of modified mRNAs encoding for growth factors may hold therapeutic potential in this area.
Limitations
Although the computational model of cardiomyocyte apoptosis uses default parameters, the model predictions are rather robust to variation in model parameters (Fig. S1 and S2). This robustness is similar to that seen with prior large network models, and it seems to be a property of larger network structures (9,12,43). We chose not to perform parameter estimation, because it would decrease the amount of data we could use for validation. Availability of quantitative signaling data would allow parameter estimation, which may allow for dynamic and more quantitative predictions. TKI simulations involve complete inhibition of a drug’s identified targets, yet inhibition may be incomplete for certain targets, requiring adjustment of reaction weights. Furthermore, as the off-target effects of TKIs are still far from being well understood, the model in its current state may not encompass all of a particular TKI’s off-targets. We expect that the model may need to be adjusted and improved based on new experimental data in the future. In particular, one interesting area of model improvement would be the incorporation of feedback loops between ROS and tyrosine kinase receptors (44); however, this has not been thoroughly investigated in cardiomyocytes.
While studies used for model validation were limited to those using rat or human cardiomyocytes, studies used for model construction were not limited to papers from cardiac systems in order to expand the data available for model construction. We assumed that signaling pathways identified in another cell line would be conserved in cardiomyocytes, with the rationale that findings contrary to this assumption would be identified during the model validation process. However, there is the possibility that some signaling pathways are not conserved across cell lines, which may impact the specificity of our results to cardiomyocytes. Recently reported methods for uncertainty and sensitivity analyses for logic-based networks could aid identification of incorrect or poorly parameterized elements of the model (45,46)..
Conclusions
The development of a computational model of cardiomyocyte apoptosis presents a new way of investigating TKI-induced cardiotoxicity at the systems level. This model predicts apoptosis in response to seven TKIs: sorafenib, sunitinib, ponatinib, trastuzumab, gefitinib, nilotinib, and erlotinib, with the most pronounced apoptotic response following sorafenib treatment. The model also yields rational and mechanistic insight into drugs and drug combinations that may mitigate TKI-induced cardiotoxicity, notably antioxidants, used alone or in concert with growth factor stimulation.
Materials and Methods
Model construction
A cardiomyocyte apoptosis signaling network was manually reconstructed from published experimental studies. Literature search identified 97 papers describing tyrosine kinase signaling pathways, intrinsic apoptotic signaling pathways, and pathway crosstalk, which were then used to define the signaling intermediates (“nodes”) and reactions in the network, determining the network structure (Table S1). A pathway reaction was only incorporated into the network if it had at least two supporting studies. Information about TKI targets was obtained from the DrugBank database. TKI network nodes were connected to their corresponding targets via inhibitory reactions. During the literature search, some studies were set aside for model validation, particularly if the cell type used was human or rat cardiomyocyte and the study examined the relationship between a network input (i.e. ROS or tyrosine kinase inhibitor treatment) and some downstream network nodes (e.g. caspase 3).
A logic-based differential equation (LDE) approach was used to convert the network into a predictive computational model, as previously described (9,12–14). In this approach, the fractional activation of each node in the network is modeled using a differential equation. Network reactions are represented using normalized Hill functions, with logical AND and OR gates describing pathway crosstalk. Default network node parameters include initial activation (yinit = 0), maximal activation (ymax = 1), and time constant (τ = 1); default reaction parameters include weight (w = 1), Hill coefficient (n = 1.4), and half-maximal effective concentration (EC50 = 0.5). These default parameter values are chosen in part because they are intuitive for a normalized activation scale, but also because they have been successfully applied to a number of large network models(12–14,38). The baseline condition was defined by an input value of 0.175 for all tyrosine kinase receptor inputs (growth factors) and a 0.05 ROS input, representing normal physiological signaling activity. The network was converted into a system of LDEs implemented in MATLAB using Netflux software (available at https://github.com/saucermanlab/Netflux).
Model validation
As described above in Model Construction, studies for model validation were identified using manual literature search. Validation literature for TKI simulations was identified searching the PubMed database using MeSH search tags (e.g. sunitinib and “Myocytes, Cardiac/drug effects”[MAJR]) for each of the seven TKIs in the model. These searches identified 51 papers examining the effects of TKIs on cardiomyocytes (Table S2). Studies used for validation were limited to those using rat or human cardiomyocytes. Importantly, experimental studies used for model validation did not include any of the studies used in network construction. Network nodes’ change in activity following a particular perturbation was classified as “increase”, “decrease,” or “no change” relative to baseline (for model predictions) or control conditions (for experimental results). No change was defined as less than 0.5% change in activity compared to baseline. This threshold value for model validation was chosen to be consistent with thresholds ranging from 0.1 to 5% used by previously published logic-based network models (12–14). A small threshold is sensitive to small changes in node activity despite the use of default parameters that may predispose nodes to saturation or inactivation. Additionally, prediction accuracy is stable for thresholds between 0.1 and 2% (Fig. S3). Prediction accuracy remains high (>70%) for thresholds of up to 10% (Fig. S3). Model accuracy was calculated based on the percentage concordance between published experimental observations and model predictions. If multiple validation studies were available, we used “majority rules”. In a tie (e.g. 2 increase 2 no change), we assumed it was an increase.
Parameter robustness
Robustness of model predictions to variation in model parameters (ymax, w, n, EC50, τ, and yinit) was evaluated by generating new parameter sets for each parameter by sampling from a uniform random distribution with a half-width of up to 50% of the original parameter value. For the parameters w and n, the new parameter sets also met the constraints 0 ≤ w ≤ 1 and n > 1, protecting against negative values in the normalized Hill functions (9). For each distribution range for each parameter, 100 new parameter sets were generated, and model predictions were compared with experimental observations using a ±0.5% validation threshold as described in Model Validation. Validation accuracy was also assessed in response to the indicated changes in baseline input reaction weights and TKI inputs using a ±0.5% threshold.
Sensitivity analysis
Knockdown simulations
Knockdown simulations were used to identify negative functional regulators of TKI-induced apoptosis. A simulated knockdown of each node in the network was performed by setting its maximal activation value (ymax) to 0. The change in activity of each node was then calculated by subtracting the fractional activation at steady-state under TKI treatment from the fractional activation at steady-state under each knockdown condition with TKI treatment. In the sensitivity matrix, each column represents the response of all nodes in the network to knockdown of a particular node. Each row shows the response of a particular node in the network to knockdown of each node.
Nodes whose knockdown produced the greatest decrease in activity of the apoptosis node were identified as the top negative regulators of TKI-induced apoptosis.
Overexpression simulations
Overexpression simulations were used to identify positive functional regulators of TKI-induced apoptosis. Overexpression of each node in the network was modeled by setting its initial activation (yinit) to 1 and its time constant (τ) to 1000 (38). The change in activity of each node was then calculated by subtracting the fractional activation at steady-state under TKI treatment from the fractional activation at steady-state under each overexpression condition with TKI treatment. Again, in the sensitivity matrix, each column represents all network nodes’ responses to one particular node’s knockdown, while each row indicates the response of one particular node in the network to each node’s knockdown.
Nodes whose overexpression produced the greatest decrease in activity of the apoptosis node were identified as the top positive regulators of TKI-induced apoptosis.
Combinatorial screen
A combinatorial screen was performed to identify combinations of positive and negative regulators of sorafenib-induced apoptosis that most effectively decrease sorafenib-induced apoptosis. Positive regulators were partially knocked down by setting ymax to 0.75, while negative regulators were partially overexpressed by setting yinit to 0.25 and to 1000. The change in apoptosis for each combinatorial treatment consisting of a positive regulator partial knockdown and a negative regulator partial overexpression was calculated by subtracting the fractional activation of the apoptosis node at steady-state with sorafenib treatment from the fractional activation of apoptosis at steady-state with the combinatorial treatment and sorafenib.
Combined TKI and antioxidant simulation
Simulations with TKIs were performed by setting their input reaction weight to 1. Simulation of the ROS scavenger NAC was performed by setting the ROS input reaction weight to 0 (vs. its baseline level of 0.05) and the ymax parameter for ROS to 0.
Supplementary Material
Highlights.
Computational model of cardiomyocyte apoptosis signaling network
The model is validated against a wide range of experimental data
Virtual screen predicts regulators of tyrosine kinase inhibitor-induced apoptosis
Inhibition of ROS is predicted to block apoptosis from tyrosine kinase inhibitors
Acknowledgements
This study was funded by a Beckman Scholar Fellowship and the National Institutes of Health (HL137755, HL137100, HL127624).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
None
References
- 1.Daher IN, Daigle TR, Bhatia N, Durand J-B. The Prevention of Cardiovascular Disease in Cancer Survivors. Tex Heart Inst J. 2012;39(2):190–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Chen MH, Kerkela R, Force T. Mechanisms of cardiomyopathy associated with tyrosine kinase inhibitor cancer therapeutics. Circulation. 2008. July 1;118(1):84–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Florescu M, Cinteza M, Vinereanu D. Chemotherapy-induced Cardiotoxicity. Mædica. 2013. March;8(1):59–67. [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Z, Ai D. Cardiotoxicity associated with targeted cancer therapies. Mol Clin Oncol. 2016. May;4(5):675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Research. Questions and Answers on FDA’s Adverse Event Reporting System (FAERS). FDA. FDA; 2019. [Google Scholar]
- 6.Wittayanukorn S, Qian J, Johnson BS, Hansen RA. Cardiotoxicity in targeted therapy for breast cancer: A study of the FDA adverse event reporting system (FAERS). J Oncol Pharm Pract. 2017. March 1;23(2):93–102. [DOI] [PubMed] [Google Scholar]
- 7.Shim JV, Chun B, van Hasselt JGC, Birtwistle MR, Saucerman JJ, Sobie EA. Mechanistic Systems Modeling to Improve Understanding and Prediction of Cardiotoxicity Caused by Targeted Cancer Therapeutics. Front Physiol. 2017;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teppo H-R, Soini Y, Karihtala P. Reactive Oxygen Species-Mediated Mechanisms of Action of Targeted Cancer Therapy. Oxid Med Cell Longev. 2017;2017:1485283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kraeutler MJ, Soltis AR, Saucerman JJ. Modeling cardiac β-adrenergic signaling with normalized-Hill differential equations: comparison with a biochemical model. BMC Syst Biol. 2010. November 18;4(1):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalkavan H, Green DR. MOMP, cell suicide as a BCL-2 family business. Cell Death Differ. 2018. January;25(1):46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pophali PA, Patnaik MM. The Role of New Tyrosine Kinase Inhibitors in Chronic Myeloid Leukemia. Cancer J Sudbury Mass. 2016;22(1):40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryall KA, Holland DO, Delaney KA, Kraeutler MJ, Parker AJ, Saucerman JJ. Network Reconstruction and Systems Analysis of Cardiac Myocyte Hypertrophy Signaling. J Biol Chem. 2012. December 7;287(50):42259–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zeigler AC, Richardson WJ, Holmes JW, Saucerman JJ. A computational model of cardiac fibroblast signaling predicts context-dependent drivers of myofibroblast differentiation. J Mol Cell Cardiol. 2016. May;94:72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tan PM, Buchholz KS, Omens JH, McCulloch AD, Saucerman JJ. Predictive model identifies key network regulators of cardiomyocyte mechano-signaling. PLoS Comput Biol. 2017. November;13(11):e1005854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu L, Sun Y, Zhang H, Zhang J, Hu J. Catalpol inhibits apoptosis in hydrogen peroxide-induced cardiac myocytes through a mitochondrial-dependent caspase pathway. Biosci Rep. 2016. June 30;36(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang B, Shravah J, Luo H, Raedschelders K, Chen DDY, Ansley DM. Propofol protects against hydrogen peroxide-induced injury in cardiac H9c2 cells via Akt activation and Bcl-2 up-regulation. Biochem Biophys Res Commun. 2009. November 6;389(1):105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yaniv G, Shilkrut M, Larisch S, Binah O. Hydrogen peroxide predisposes neonatal rat ventricular myocytes to Fas-mediated apoptosis. Biochem Biophys Res Commun. 2005. October 28;336(3):740–6. [DOI] [PubMed] [Google Scholar]
- 18.Doherty KR, Wappel RL, Talbert DR, Trusk PB, Moran DM, Kramer JW, et al. Multi-parameter in vitro toxicity testing of crizotinib, sunitinib, erlotinib, and nilotinib in human cardiomyocytes. Toxicol Appl Pharmacol. 2013. October 1;272(1):245–55. [DOI] [PubMed] [Google Scholar]
- 19.Hasinoff BB, Patel D. The lack of target specificity of small molecule anticancer kinase inhibitors is correlated with their ability to damage myocytes in vitro. Toxicol Appl Pharmacol. 2010. December 1;249(2):132–9. [DOI] [PubMed] [Google Scholar]
- 20.Korashy HM, Attafi IM, Ansari MA, Assiri MA, Belali OM, Ahmad SF, et al. Molecular mechanisms of cardiotoxicity of gefitinib in vivo and in vitro rat cardiomyocyte: Role of apoptosis and oxidative stress. Toxicol Lett. 2016. June 11;252:50–61. [DOI] [PubMed] [Google Scholar]
- 21.Lekes D, Szadvari I, Krizanova O, Lopusna K, Rezuchova I, Novakova M, et al. Nilotinib induces ER stress and cell death in H9c2 cells. Physiol Res. 2016. 21;65(Suppl 4):S505–14. [DOI] [PubMed] [Google Scholar]
- 22.Hasinoff BB, Patel D, Wu X. The Myocyte-Damaging Effects of the BCR-ABL1-Targeted Tyrosine Kinase Inhibitors Increase with Potency and Decrease with Specificity. Cardiovasc Toxicol. 2017. July 1;17(3):297–306. [DOI] [PubMed] [Google Scholar]
- 23.Talbert DR, Doherty KR, Trusk PB, Moran DM, Shell SA, Bacus S. A multi-parameter in vitro screen in human stem cell-derived cardiomyocytes identifies ponatinib-induced structural and functional cardiac toxicity. Toxicol Sci Off J Soc Toxicol. 2015. January;143(1):147–55. [DOI] [PubMed] [Google Scholar]
- 24.Kawabata M, Umemoto N, Shimada Y, Nishimura Y, Zhang B, Kuroyanagi J, et al. Downregulation of stanniocalcin 1 is responsible for sorafenib-induced cardiotoxicity. Toxicol Sci Off J Soc Toxicol. 2015. February;143(2):374–84. [DOI] [PubMed] [Google Scholar]
- 25.Hui Cheng, Gabor Kari, Dicker Adam P, Ulrich Rodeck, Koch Walter J, Thomas Force. A Novel Preclinical Strategy for Identifying Cardiotoxic Kinase Inhibitors and Mechanisms of Cardiotoxicity. Circ Res. 2011. December 9;109(12):1401–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rainer PP, Doleschal B, Kirk JA, Sivakumaran V, Saad Z, Groschner K, et al. Sunitinib causes dose-dependent negative functional effects on myocardium and cardiomyocytes. BJU Int. 2012. November;110(10):1455–62. [DOI] [PubMed] [Google Scholar]
- 27.Cohen JD, Babiarz JE, Abrams RM, Guo L, Kameoka S, Chiao E, et al. Use of human stem cell derived cardiomyocytes to examine sunitinib mediated cardiotoxicity and electrophysiological alterations. Toxicol Appl Pharmacol. 2011. November 15;257(1):74–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harvey PA, Leinwand LA. Oestrogen enhances cardiotoxicity induced by Sunitinib by regulation of drug transport and metabolism. Cardiovasc Res. 2015. July 1;107(1):66–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Z Y, X T, Y X, Z H, D X, L L, et al. Autophagy plays an important role in sunitinib-mediated cell death in H9c2 cardiac muscle cells. Toxicol Appl Pharmacol. 2010. July 15;248(1):20–7. [DOI] [PubMed] [Google Scholar]
- 30.Chiusa M, Hool S-L, Truetsch P, Djafarzadeh S, Jakob SM, Seifriz F, et al. Cancer therapy modulates VEGF signaling and viability in adult rat cardiac microvascular endothelial cells and cardiomyocytes. J Mol Cell Cardiol. 2012. May;52(5):1164–75. [DOI] [PubMed] [Google Scholar]
- 31.Maayah ZH, Ansari MA, El Gendy MA, Al-Arifi MN, Korashy HM. Development of cardiac hypertrophy by sunitinib in vivo and in vitro rat cardiomyocytes is influenced by the aryl hydrocarbon receptor signaling pathway. Arch Toxicol. 2014. March;88(3):725–38. [DOI] [PubMed] [Google Scholar]
- 32.Clements M, Millar V, Williams AS, Kalinka S. Bridging Functional and Structural Cardiotoxicity Assays Using Human Embryonic Stem Cell-Derived Cardiomyocytes for a More Comprehensive Risk Assessment. Toxicol Sci Off J Soc Toxicol. 2015. November;148(1):241–60. [DOI] [PubMed] [Google Scholar]
- 33.Mohan N, Shen Y, Endo Y, ElZarrad MK, Wu WJ. Trastuzumab, but Not Pertuzumab, Dysregulates HER2 Signaling to Mediate Inhibition of Autophagy and Increase in Reactive Oxygen Species Production in Human Cardiomyocytes. Mol Cancer Ther. 2016;15(6):1321–31. [DOI] [PubMed] [Google Scholar]
- 34.ElZarrad MK, Mukhopadhyay P, Mohan N, Hao E, Dokmanovic M, Hirsch DS, et al. Trastuzumab Alters the Expression of Genes Essential for Cardiac Function and Induces Ultrastructural Changes of Cardiomyocytes in Mice. PLoS ONE. 2013. November 8;8(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kurokawa YK, Shang MR, Yin RT, George SC. Modeling trastuzumab-related cardiotoxicity in vitro using human stem cell-derived cardiomyocytes. Toxicol Lett. 2018. March 15;285:74–80. [DOI] [PubMed] [Google Scholar]
- 36.Singh KK, Shukla PC, Quan A, Lovren F, Pan Y, Wolfstadt JI, et al. Herceptin, a recombinant humanized anti-ERBB2 monoclonal antibody, induces cardiomyocyte death. Biochem Biophys Res Commun. 2011. July 29;411(2):421–6. [DOI] [PubMed] [Google Scholar]
- 37.Wang H, Sheehan RP, Palmer AC, Everley RA, Boswell SA, Ron-Harel N, et al. Adaptation of Human iPSC-Derived Cardiomyocytes to Tyrosine Kinase Inhibitors Reduces Acute Cardiotoxicity via Metabolic Reprogramming. Cell Syst. 2019. 22;8(5):412–426.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frank DU, Sutcliffe MD, Saucerman JJ. Network-based Predictions of in vivo Cardiac Hypertrophy. J Mol Cell Cardiol. 2018. August;121:180–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sharma A, Burridge PW, McKeithan WL, Serrano R, Shukla P, Sayed N, et al. High-Throughput Screening of Tyrosine Kinase Inhibitor Cardiotoxicity with Human Induced Pluripotent Stem Cells. Sci Transl Med. 2017. February 15;9(377). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rana P, Anson B, Engle S, Will Y. Characterization of human-induced pluripotent stem cell-derived cardiomyocytes: bioenergetics and utilization in safety screening. Toxicol Sci Off J Soc Toxicol. 2012. November;130(1):117–31. [DOI] [PubMed] [Google Scholar]
- 41.Stuhlmiller TJ, Zawistowski JS, Chen X, Sciaky N, Angus SP, Hicks ST, et al. Kinome and Transcriptome Profiling Reveal Broad and Distinct Activities of Erlotinib, Sunitinib, and Sorafenib in the Mouse Heart and Suggest Cardiotoxicity From Combined Signal Transducer and Activator of Transcription and Epidermal Growth Factor Receptor Inhibition. J Am Heart Assoc. 2017. October 19;6(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Damiano S, Montagnaro S, Puzio MV, Severino L, Pagnini U, Barbarino M, et al. Effects of antioxidants on apoptosis induced by dasatinib and nilotinib in K562 cells. J Cell Biochem. 2018;119(6):4845–54. [DOI] [PubMed] [Google Scholar]
- 43.Soltis A, Saucerman J. Robustness portraits of diverse biological networks conserved despite order-of-magnitude parameter uncertainty. Bioinforma Oxf Engl. 2011. October 15;27(20):2888–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weng M-S, Chang J-H, Hung W-Y, Yang Y-C, Chien M-H. The interplay of reactive oxygen species and the epidermal growth factor receptor in tumor progression and drug resistance. J Exp Clin Cancer Res CR [Internet]. 2018. March 16 [cited 2021 Jan 7];37. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5857086/ [DOI] [PMC free article] [PubMed]
- 45.Khalilimeybodi A, Paap AM, Christiansen SLM, Saucerman JJ. Context-specific network modeling identifies new crosstalk in β-adrenergic cardiac hypertrophy. PLoS Comput Biol. 2020. December;16(12):e1008490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cao S, Aboelkassem Y, Wang A, Valdez-Jasso D, Saucerman JJ, Omens JH, et al. Quantification of model and data uncertainty in a network analysis of cardiac myocyte mechanosignalling. Philos Transact A Math Phys Eng Sci. 2020. June 12;378(2173):20190336. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.