Abstract
BRAF inhibitors (BRAFi) selectively target oncogenic BRAFV600E/K and are effective in 80% of advanced cutaneous malignant melanoma cases carrying the V600 mutation. However, the development of drug resistance limits their clinical efficacy. Better characterization of the underlying molecular processes is needed to further improve treatments. We previously demonstrated that transcription of PTEN is negatively regulated by the PTEN pseudogene antisense RNA, PTENP1-AS, and here we investigated the impact of this transcript on clinical outcome and BRAFi resistance in melanoma. We observed that increased expression levels of PTENP1-AS in BRAFi resistant cells associated with enrichment of EZH2 and H3K27me3 at the PTEN promoter, consequently reducing the expression levels of PTEN. Further, we showed that targeting of the PTENP1-AS transcript sensitized resistant cells to BRAFi treatment and that high expression of PTENP1-AS in stage III melanoma correlated with poor survival. Collectively, the data presented here show that PTENP1-AS is a promising target for re-sensitizing cells to BRAFi and also a possible prognostic marker for clinical outcome in stage III melanoma.
Subject terms: Cancer, Molecular biology
Introduction
Although cutaneous malignant melanoma is a molecularly diverse disease, approximately 50% carry activating mutations in the serine/threonine protein kinase BRAF. The majority of BRAF mutations are represented by a valine (V) to glutamic acid (E) or lysine (K) substitution at position 600 (BRAFV600E/K)1. These missense mutations occur in the BRAF kinase domain, which results in constitutively active BRAF and subsequently activated MAPK signaling. Drug development efforts using a targeted approach have successfully led to the development of small inhibitory molecules (BRAFi, i.e. vemurafenib, dabrafenib, encorafenib), which specifically target the oncogenic BRAFV600E/K. While 80% of patients with advanced melanoma carrying a BRAFV600E/K mutation initially respond well to this treatment, resistance emerges within a median of 6–7 months of treatment2. Although the time to emergence of resistance can be prolonged to 11 months when combined with MEK inhibitors, the 5-year overall survival rate is only 34% for the combined treatment3. In recent years there has been a growing understanding of the underlying molecular mechanisms involved in acquired BRAFi resistance4,5 and activation of the PI3K/AKT pathway due to loss of PTEN has been found to contribute to this process6. Therefore, better molecular understanding of the mechanisms that contribute to suppression of PTEN is desired and might help to identify novel approaches that could circumvent or delay the onset of resistance.
Approximately 14,000 pseudogenes have been identified in the human genome and roughly 900 of these have been reported to be transcribed into non-coding RNAs (ncRNAs)7. Molecular functions have been characterized for only a handful of these pseudogenes8–11, for instance through microRNA (miRNA) sponging10 and trans acting antisense RNAs (asRNA)8. One of these, the PTEN pseudogene, PTENP1 (also known as PTENpg1 and PTENΨ), is divergently transcribed into sense (PTENP1-S) and asRNA (PTENP1-AS) transcripts. While PTENP1-S promote expression of PTEN by functioning as a miRNA sponge for PTEN related miRNAs10, PTENP1-AS acts as a transcriptional suppressor by inducing epigenetic alterations at the PTEN promoter8,12. Interestingly, loss of PTEN expression has been found during the development of resistance to BRAFi6 and melanoma metastasis13,14, but the involvement of PTENP1-AS remains unknown.
In this study, our aim was to characterize the impact of PTENP1-AS on clinical outcome in stage III melanoma and BRAFi treatment efficacy. We observe that the expression of PTENP1-AS is induced in BRAFi resistant sublines in relation to the parental sensitive cell line. This coincides with transcriptional suppression of PTEN, likely through the recruitment of EZH2 and subsequent formation of H3K27me3 at the PTEN promoter. Finally, we also demonstrate that expression of PTENP1-AS is increased in tumor samples from stage III melanoma patients with poor survival. In summary, our study provides insights into the involvement of PTENP1-AS in resistance to BRAFi treatment.
Results
Inverse correlation of PTEN and PTENP1-AS in BRAFi resistant A375 sublines
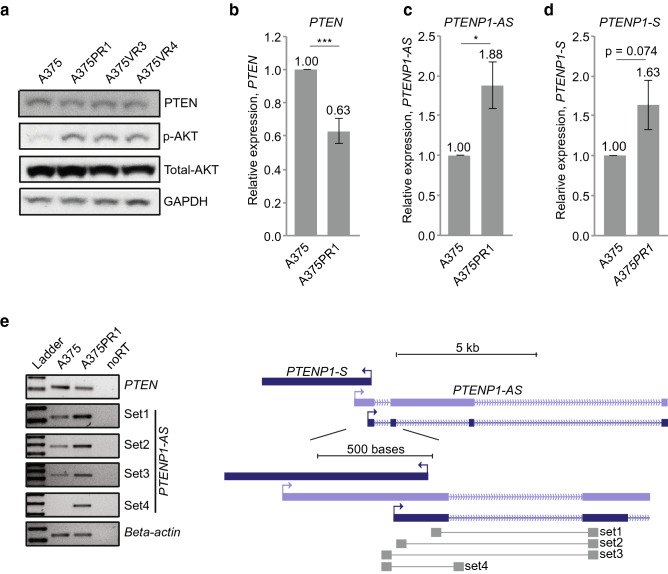
Previous studies suggested downregulation of PTEN to be important upon the development of resistance to BRAFi6,13. Based on these reports, we set out to investigate if PTENP1-AS was involved in this process through transcriptional suppression of PTEN. To do this, a series of BRAFi resistant melanoma sublines were obtained by culturing the BRAFi sensitive A375 cell line in increasing doses of BRAFi (A375PR1 (resistant to PLX4720), A375VR3 and A375VR4 (both resistant to vemurafenib))15. Compared to the parental A375 cells, IC50 measurements for the A375PR1 and A375VR4 cell lines confirmed roughly six- to eight-fold increased tolerance to vemurafenib (Supplementary Fig. S1), thus in agreement with a previous study15. We next measured PTEN expression using Western blot and qRTPCR and observed downregulation of PTEN at the protein (Fig. 1a, Supplementary Fig. S2a) as well as mRNA (Fig. 1b, Supplementary Fig. S2b) levels. Importantly, the negatively regulated downstream target of PTEN, p-AKT, showed a corresponding increase in phosphorylation compared to the parental A375 cell line (Fig. 1a, Supplementary Fig. S2a).
Figure 1.
Expression levels of PTEN and PTENP1-lncRNAs in BRAFi sensitive and resistant cell lines. (a) Western blot analysis presenting the expression of PTEN, total AKT and p-AKT in A375 and the BRAFi resistant sublines. (b–d) qRTPCR analysis of (b) PTEN, (c) PTENP1-AS and (d) PTENP1-S in A375 and the BRAFi resistant A375PR1 subline (n = 3, p-values represent a two-tailed student’s t-test). (e) Semi-qRTPCR assay showing different isoforms of the PTENP1-AS transcripts with a scheme showing primer binding sites.
We next measured levels of PTENP1-encoded transcripts and identified a significant upregulation of PTENP1-AS in all three resistant sublines (Fig. 1c, Supplementary Fig. S2c) and also a modest, although non-significant, induction of PTENP1-S (Fig. 1d, Supplementary Fig. S2d). Since previous studies had identified multiple isoforms of PTENP1-AS with distinct regulatory functions8, we carefully investigated different isoforms in one of the sublines (A375PR1). Multiple primer sets for the different variants of PTENP1-AS were assessed on semi-qRTPCR and revealed increased expression of all isoforms (Fig. 1e, Supplementary Fig. S3). Notably, unspliced RNA levels of PTENP1-AS was also found to be induced, indicating that PTENP1-AS is activated at the transcriptional level. Collectively, these initial observations motivated us to further elucidate the role of PTENP1-AS in resistance to BRAFi.
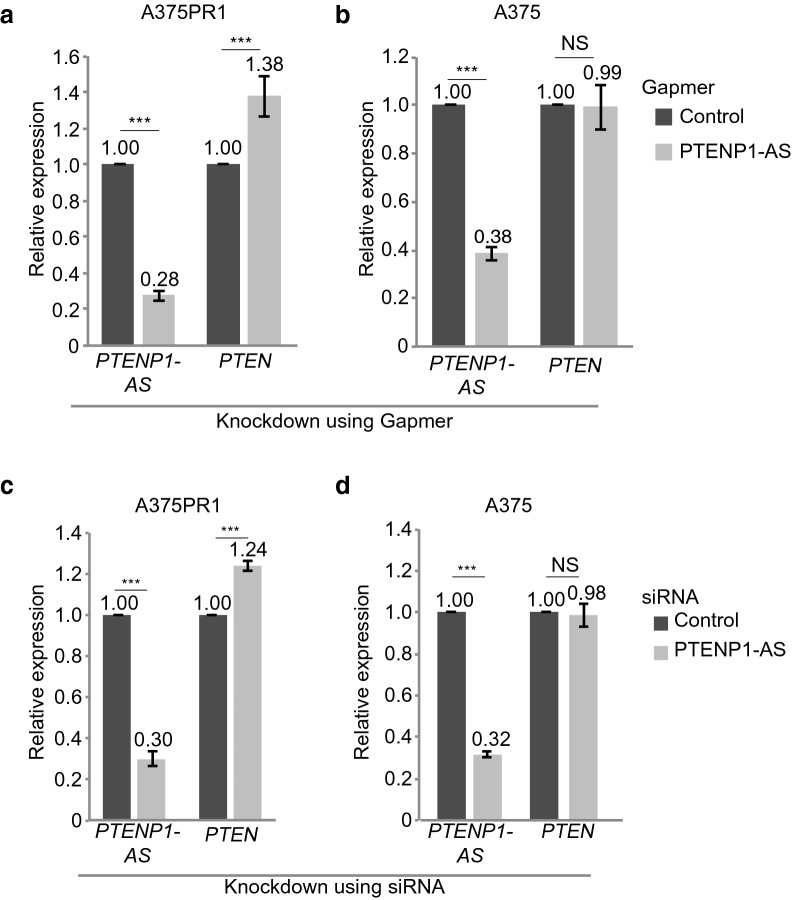
PTENP1-AS suppresses PTEN in BRAFi resistant cells through chromatin remodeling
To investigate the molecular interplay between PTENP1-AS and PTEN in greater detail, we focused, from here, on the A375PR1 subline. We designed a gapmer antisense oligonucleotide (ASO) (Fig. 2a,b) and also an siRNA targeting the PTENP1-AS transcript (Fig. 2c,d) and confirmed knockdown in A375 as well as in A375PR1 cells using qRTPCR. Intriguingly, knockdown of PTENP1-AS only induced the expression of PTEN in the A375PR1 cells, while PTEN remained unaffected in the vemurafenib sensitive A375 cells (Fig. 2a–d), suggesting that PTENP1-AS is predominantly active in the resistant subline. In contrast, no effect on PTENP1-S expression levels was observed in either cell line upon knockdown of PTENP1-AS (Supplementary Fig. S4).
Figure 2.
Effect on PTEN expression upon knockdown of PTENP1-AS. (a,b) qRTPCR measuring the expression levels of PTENP1-AS and PTEN in (a) A375PR1 or (b) A375 cells upon knockdown of PTENP1-AS using gapmer ASO. (c,d) qRTPCR measuring the expression levels of PTENP1-AS and PTEN in (c) A375PR1 or (d) A375 cells upon knockdown of PTENP1-AS using siRNA. (a–d) n = 3, p-values represent two-tailed student’s t-tests.
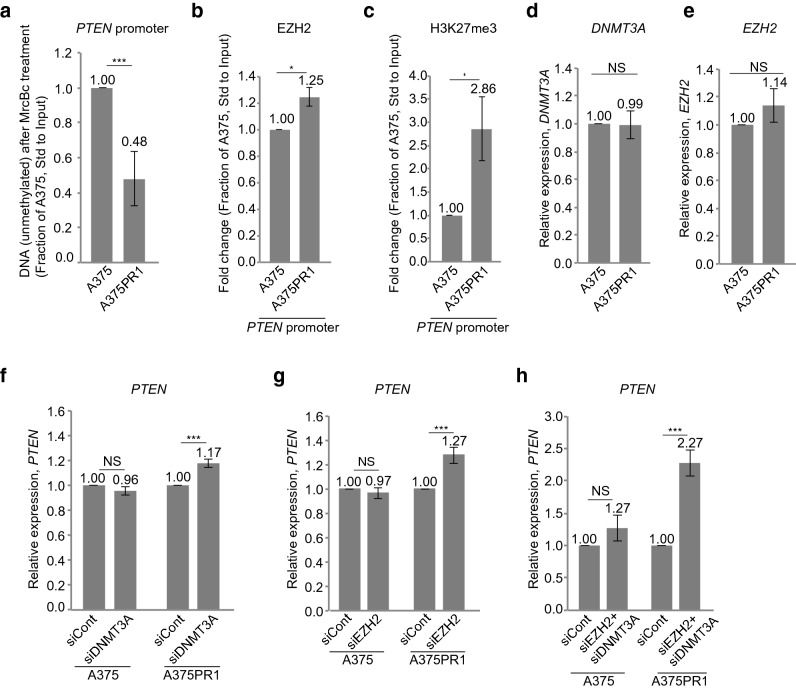
We next asked if suppression of PTEN in the A375R1 subline was due to epigenetic changes at the PTEN promoter since high promoter methylation has been commonly observed in melanoma and is associated with poor clinical outcome16. PTEN promoter CpG methylation was assessed by the methyl-cytosine-specific McrBc restriction enzyme. qRTPCR showed increased enzymatic cleavage in the A375PR1 subline, compared to the parental A375 cells (Fig. 3a), thus suggesting increased PTEN promoter CpG methylation in the resistant subline. Since we have previously reported PTENP1-AS to modulate transcription of PTEN through the recruitment of EZH2 and DNMT3A8,12, we next measured levels of EZH2 and H3K27me3 at the PTEN promoter. Chromatin immunoprecipitation (ChIP) followed by qRTPCR revealed increased levels of EZH2 and H3K27me3 at the PTEN promoter in the A375PR1 subline (Fig. 3b,c), while the baseline expression levels of DNMT3A and EZH2 were similar in the resistant and parental cell lines as measured by qRTPCR (Fig. 3d,e). To further interrogate their role in suppression of PTEN, EZH2 and DNMT3A were depleted using siRNAs. Although individual siRNA-mediated knockdown only resulted in a modest induction of PTEN (Fig. 3f,g, Supplementary Fig. S5a,b), simultaneous knockdown generated over a twofold induction of PTEN in the A375PR1 cells, in contrast to the parental A375 cells, where the expression of PTEN was largely unchanged (Fig. 3h, Supplementary Fig. S5c,d). Altogether, these data suggest that suppression of PTEN is mediated by PTENP1-AS likely through the recruitment of EZH2 by a mechanism that may be exclusively active in the vemurafenib resistant cells.
Figure 3.
Characterization of the PTEN promoter in A375 and A375PR1 cell lines. (a) qRTPCR measuring PTEN promoter CpG methylation, as determined by the remaining (unmethylated) DNA upon treatment with the methyl-cytosine-specific restriction enzyme McrBc (n = 3). (b–c) ChIP followed by qRTPCR analysis measuring the levels of (b) EZH2 and (c) H3K27me3 at the PTEN promoter in A375 and A375PR1 cell lines (n = 3). (d–e) qRTPCR measuring baseline expression levels of (d) DNMT3A and (e) EZH2 in A375 and A375PR1 cell lines (n = 3). (f–g) qRTPCR measuring the expression levels of PTEN following siRNA induced knockdown of (f) DNMT3A and (g) EZH2 in A375 and A375PR1 cell lines (n > 3). (h) qRTPCR measuring the expression levels of PTEN following simultaneous siRNA-induced knockdown of EZH2 and DNMT3A in A375 and A375PR1 cell lines (n = 3). (a–h; p-values represent a two-tailed student’s t-test).
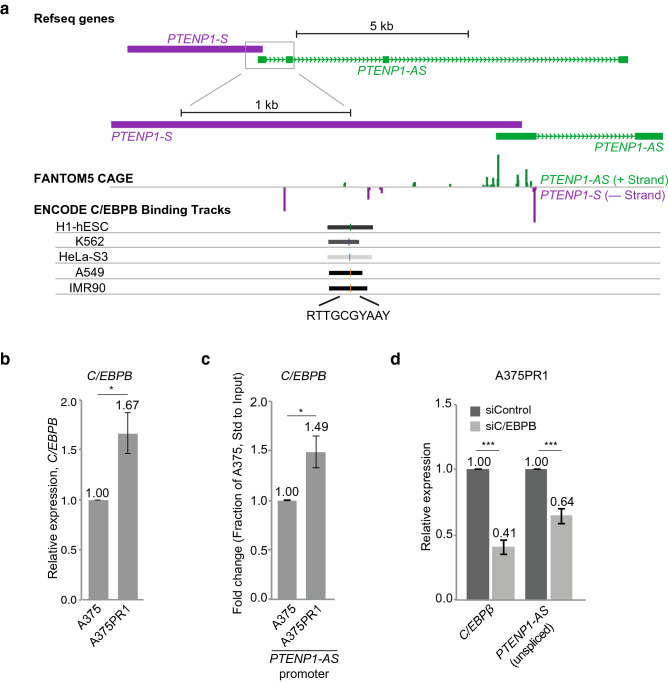
C/EBPB is a transcriptional regulator of PTENP1-AS
To explore mechanisms underlying transcriptional induction of PTENP1-AS (Fig. 1c), we took advantage of FANTOM5 CAGE data and ChIP-sequencing data from the UCSC Genome Browser and identified a binding site for the transcription factor (TF) C/EBPB close to the PTENP1-AS transcriptional start site (TSS) (Fig. 4a). Comparing A375PR1 to A375 cells, revealed an increased RNA expression of C/EBPB by qRTPCR (Fig. 4b), and ChIP further identified increased levels of C/EBPB at the PTENP1-AS promoter (Fig. 4c) in A375PR1 cells. Targeting C/EBPB with dsiRNA reduced the expression of unspliced PTENP1-AS in the A375PR1 cells (Fig. 4d), while no significant change was identified for PTENP1-S (Supplementary Fig. S6), thus suggesting that C/EBPB functions as a transcriptional activator of PTENP1-AS.
Figure 4.
Transcriptional regulation of PTENP1-AS by C/EBPB. (a) A scheme showing binding of C/EBPB at the PTENP1 locus (data retrieved from the Zenbu FANTOM5 CAGE and the UCSC genome browser) and the predicted DNA binding site for C/EBPB (R is an A/G, Y is C/T). (b) qRTPCR measuring the expression levels of C/EBPB (n > 3). (c) ChIP followed by qRTPCR analysis measuring the levels of C/EBPB at the PTENP1-AS promoter (n = 3). (d) qRTPCR measuring expression levels of C/EBPB and unspliced PTENP1-AS in A375PR1 cells upon siRNA-induced knockdown of C/EBPB (n = 3).
PTENP1-AS is a clinically relevant target and a prognostic marker in melanoma
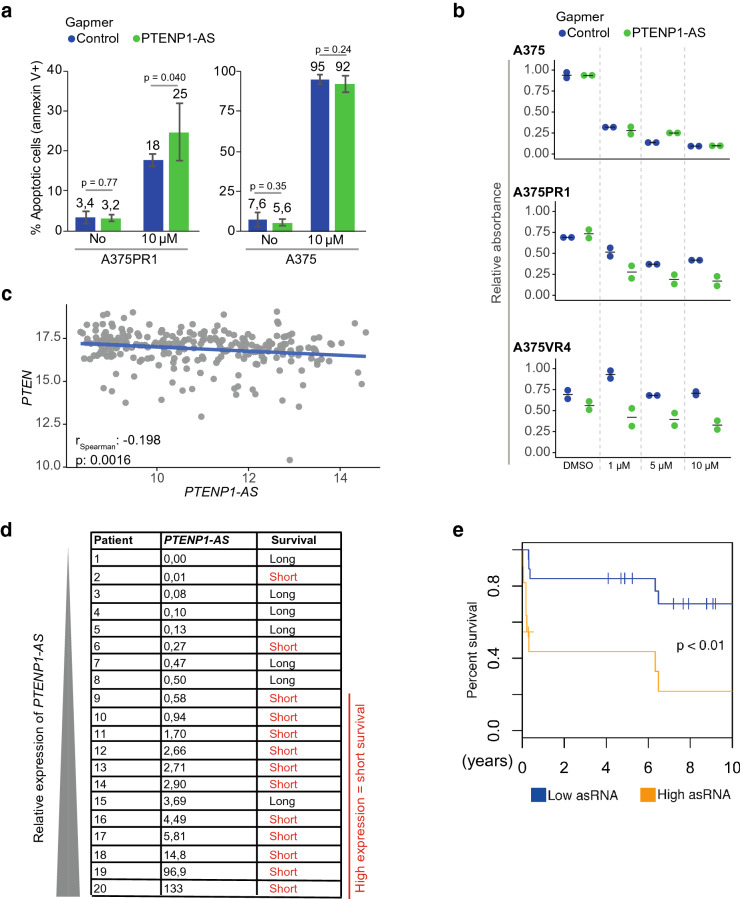
We next explored if the resistant A375PR1 cells could be sensitized to BRAFi by targeting the PTENP1-AS transcript. Gapmer ASO-mediated suppression did not have an effect on the basal levels of cell death but sensitized resistant cells to treatment with 10 μM of vemurafenib (Fig. 5a), as measured by annexin V and propidium iodide staining. To further validate this effect, we performed a colony formation assay and also included a second resistant subline, A375VR4. While gapmer ASO-mediated knockdown of PTENP1-AS had minor effect on colony formation in parental A375, both resistant sublines were clearly sensitized to vemurafenib, in particular at lower concentrations (1 μM) (Fig. 5b, Supplementary Fig. S7).
Figure 5.
Manipulation of PTENP1-AS in BRAFi resistant sublines and evaluation of PTENP1-AS in metastatic melanoma samples. (a) Cell-death analysis by annexin V and propidium iodide staining upon knockdown of PTENP1-AS and vemurafenib treatment (n = 6). (b) Colony formation assays for A375, A375PR1 and A375VR4 cell lines measuring relative absorbance of crystal violet solution stained colonies upon gapmer ASO-induced knockdown of PTENP1-AS co-treated with various concentrations of vemurafenib. (c) Expression data (TCGA) for PTEN and PTENP1-AS from melanoma samples. (d) qRTPCR measuring expression levels of PTENP1-AS in a set of 20 first regional lymph node metastases from stage III melanoma patients. Based on clinical follow up data, the patients were categorized as long- or short-term survivors, > 60 months or ≤ 13 months, respectively. (e) Kaplan–Meier plot showing overall survival for patients with high (n = 12) or low (n = 17) expression levels of PTENP1-AS. Expression levels of PTENP1-AS was measured in first regional lymph node metastases from an independent set of 29 stage III melanoma patients using qRTPCR. The p-value represents a log-rank test.
We finally set out to investigate the relevance of PTENP1-AS in tumors from melanoma patients. The expression levels of PTEN and PTENP1-AS were first assessed in melanoma samples from the TCGA (The Cancer Genome Atlas program) where although weak but a significant negative correlation was observed (r = − 0.20, p = 1.6e−3, Fig. 5c). The expression of PTENP1-AS was next determined in lymph node metastases from a cohort of 20 stage III melanoma patients. The samples were initially chosen to include two groups of patients, with either long (≥ 60 months) or short (≤ 13 months) overall survival17, and the expression of PTENP1-AS was determined by qRTPCR. Notably, 9/10 (90%) patients having tumors with high expression of PTENP1-AS (median cut-off) had poor survival, while low expression of PTENP1-AS seemed to be indicative of prolonged survival, although not reaching significance (p = 0.06) (Fig. 5d). This motivated us to evaluate the expression of PTENP1-AS in an independent second cohort of stage III melanoma metastasis samples. Lymph node metastases from 29 stage III melanoma patients were analyzed for the expression of PTENP1-AS. The patient samples from the second cohort were divided in high (n = 12) or low (n = 17) expression of PTENP1-AS, as determined by qRTPCR, and a survival plot was generated (Fig. 5e). A significant difference in overall survival was observed between patients with high and low expression of PTENP1-AS. In summary, the expression of PTENP1-AS appears to be a promising prognostic marker for clinical outcome, where increased expression of PTENP1-AS correlates with poor overall survival.
Discussion
The data presented in this study suggest a role for PTENP1-AS in the development of resistance to BRAFi. On the basis of our data, we suggest that expression of PTENP1-AS is induced by the TF C/EBPB in BRAFi resistant melanoma cell lines, which results in transcriptional suppression of PTEN through the recruitment of EZH2 with subsequent formation of H3K27me3 (Fig. 3b,c) and DNA methylation of the PTEN promoter (Fig. 3a). Moreover, we find that expression of PTENP1-AS predicts clinical outcome in stage III melanoma patients, where high expression of PTENP1-AS in first regional lymph node metastases correlates with poor overall survival. In summary, our findings bring important information about molecular functions of PTENP1-AS upon development of BRAFi resistance and better understanding of this pathway could reveal novel approaches to re-sensitize drug resistant cells.
Our data are consistent with our previous findings demonstrating that PTENP1-AS is a negative regulator of PTEN through chromatin remodeling of the PTEN promoter8. Targeting the PTENP1-AS transcript using gapmer ASOs and siRNAs generate a moderate induction of PTEN exclusively in the resistant subline (Fig. 2), thus demonstrating that the PTENP1-AS transcript does not act as an on/off switch for PTEN expression, but rather causes subtle variations of transcription in a phenotype-dependent manner8. These variations of PTEN expression are within physiological relevant levels where a modest decrease of 20% have been shown to increase cancer susceptibility18.
Our data is also consistent with previous RNA-sequencing studies showing induction of C/EBPB in BRAFi resistant cells19. However, these previous studies did not report PTEN or PTENP1-AS as candidate genes involved in BRAFi resistance, possibly due to the applied thresholds since the cut-off was set to a fold change ≥ 2. Based on our study, both PTEN and PTEN1-AS are likely to be excluded from such an analysis when these thresholds are applied.
Several PTENP1-encoded lncRNAs with opposing functions have been described. While the miRNA sponge model suggests concordant expression of PTEN and PTENP1-S10, we have not observed this phenomenon in the present study, despite a modest induction of PTENP1-S (Fig. 1d, Supplementary Fig. S2d). Instead, the PTENP1-AS transcript appears to be the dominant regulator of PTEN expression under these conditions. However, this does not exclude that miRNA sponging could take place as well. A regulatory mechanism, where translation as well as transcription of PTEN is regulated through lncRNAs encoded by the PTENP1 locus is still a plausible scenario. Subtle variations of PTEN expression have previously been reported to be associated with cancer susceptibility18, suggesting that strict and highly ordered regulation of PTEN expression is crucial for evading carcinogenesis. It is therefore likely that PTEN is regulated at several different levels. Deletions of PTENP1 have been reported in melanoma cell lines and tissues, supporting that suppression of PTEN also occurs at the post-transcriptional level through miRNA-mediated regulation20. It is also likely that tissue and cell type specific expression levels of i.e. DNMT3A, EZH2 and miRNAs dictate the regulatory outcome of PTENP1-encoded lncRNAs, and PTENP1-S may also be involved in sponging of miRNAs related to other mRNAs beyond PTEN21.
Notably, this study also shows that the suppression of PTEN in BRAFi resistant cells may be reversible through targeting of EZH2, DNMT3A as well as PTENP1-AS. The individual knockdown of EZH2 or DNMT3A did not re-activate the expression of PTEN to the same extent as a simultaneous knockdown of these proteins (Fig. 3f–h). We speculate that this is due to incomplete knockdown of DNMT3A and EZH2 where some active protein complexes may still be present under these circumstances (Supplementary Fig. S5). An interaction between EZH2 and DNMT3A have been demonstrated22 and the combined knockdown of EZH2 and DNMT3A may in this case be more efficient in reducing these protein complexes. Importantly, the induction of PTEN is more prominent in the A375PR1 cells than in the parental cells, indicative of a therapeutic window for re-activation of PTEN in BRAFi resistant melanoma cells. In support of this, we show that manipulation of the PTENP1-AS pathway re-sensitized the A375PR1 and A375VR4 resistant cells to treatment with vemurafenib (Fig. 5a,b and Supplementary Fig. S7).
We evaluated the expression of PTENP1-AS in regional lymph node metastases of stage III melanoma and found that high expression correlated with poor survival (Fig. 5d,e). This indicates that PTENP1-AS may be involved in melanoma tumor progression and is not only important during the development of resistance to BRAFi. Also, development of a particular type of resistance to vemurafenib may depend on the pre-existing factors/pathways in the tumors. High expression of PTENP1-AS could, for example, indicate that the tumor is less likely to respond to treatment and loss of PTEN expression has previously been linked to metastasis13. Therefore, one may speculate that PTENP1-AS is involved in such inactivation and consequently enhance initiation of distant metastasis. Additional studies will be required to better understand the functional role and importance of PTENP1-AS in melanoma progression and drug resistance i.e. by taking patient samples pre- and post- treatment with BRAFi.
In summary, we have identified PTENP1-AS to be involved both in melanoma tumor progression and in development of resistance to vemurafenib. The data presented here show that PTENP1-AS is not only a promising target for re-activation of PTEN, but also a possible prognostic marker for clinical outcome in stage III melanoma.
Materials and methods
Cell cultures
A375 cells were purchased from ATCC (CRL-1619). A375, A375PR1, A375VR3 and A375VR4 cell lines were cultured in 5% CO2 at 37 °C in MEM supplemented with 10% heat-inactivated FBS, 2 mM glutamine, 0.1 mM non-essential amino acids, 1 mM sodium pyruvate, 50 μg/ml of streptomycin and 50 μg/ml of penicillin. As previously described15, resistant A375 cell lines had been generated by repeated exposures to increasing concentrations of vemurafenib (A375VR3 and A375VR4) or its analog PLX4720 (A375PR1).
RNA extraction and cDNA
RNA was extracted using the RNA NucleoSpin II kit (Macherey–Nagel) and treated with DNase (Ambion Turbo DNA-free, Life Technologies). DNase treated RNA (~ 500 ng) was used for the generation of cDNAs using M-MLV (Life Technologies) and a mixture of oligo(dT)15 with nanomers.
Semi-qRTPCR
PCR was performed by using the KAPA2G FAST mix (Kapa Biosystems) according to the manufacturer’s recommendations and by using the corresponding oligos in Supplementary Table 1.
qRTPCR
qRTPCR was performed by using the KAPA 2G SYBR Green (Kapa Biosystems) on the Applied Biosystems 7900HT or the BioRad CFX96 Touch platform with the following cycling conditions: 95 °C for 3 min, 95 °C for 3 s, 60 °C for 30 s. The corresponding oligos for each gene is specified in Supplementary Table 1.
siRNAs and gapmers
siRNAs and gapmer antisense oligonucleotides, ASOs, were ordered from the respective manufacturers (Supplementary Table 1) and transfected using lipofectamine 2000 (Life Technologies) according to the manufacturer’s recommendations. A final concentration of 10–40 nM was used for the siRNAs and gapmer ASOs and PLUS Reagent (Life Technologies), which was added for transfections of gapmers ASOs.
Protein analysis
Samples were lysed in 50 mM Tris–HCl, pH 7.4, 1% NP-40, 150 mM NaCl, 1 mM EDTA, 1% glycerol, 100 μM vanadate, protease inhibitor cocktail and PhosSTOP (Roche Diagnostics GmbH). Lysates were subjected to SDS-PAGE using 4–12% acrylamide gels (Life Technologies) and transferred to PVDF membranes using the iBlot system (Life Technologies). The proteins were detected by western blot analysis by using an enhanced chemiluminescence system (Western Lightning–ECL, PerkinElmer). Antibodies used were specific for PTEN (Cell Signaling, cat. no. 9552, 1:1000), AKT (Cell Signaling, cat. no. 9272, 1:1000), phospho-AKT (Cell signaling, cat. no. 4060S, 1:1000) and β-actin (Sigma-Aldrich, cat. no. A5441, 1:5000). Membranes were first incubated for p-AKT followed by reprobing the same membranes for total AKT and PTEN.
ChIP of EZH2, H3K27me3 and C/EBPB
ChIP assays were performed as previously described8. Briefly, the ChIP assay Kit (Upstate/Millipore) was used by crosslinking the cells in 1% formaldehyde for 10 min, quenched in 0.125 M Glycine for 5 min and lysed according to the manufacturer's recommendations. The samples/nuclei were sonicated with a Bioruptor Sonicator (Diagenode) at 30 s ON, 30 s OFF (setting = high) for a total of 18 cycles. The water was replaced with ice-cold water after every sixth cycle. The samples were diluted 1:10 in ChIP dilution buffer, pre-cleared and incubated overnight with the appropriate antibody. Salmon sperm DNA/Protein A-agarose (Upstate/Millipore) was used to pull down the antibody. The DNA was eluted in elution buffer (1% SDS, 100 mM NaHCO3), followed by reverse cross-linking at 65 °C overnight. The samples were RNase-A and protease-K treated and finally eluted using the Qiagen PCR purification kit (Qiagen). The following antibodies were used (4 μg/sample): H3K27me3 (Upstate/Millipore, cat. no. 17-622), EZH2 (Upstate/Millipore, cat. no. 07-689) and C/EBPB (Santa Cruz Biotechnology cat. no. sc-150).
Assessment of methylated DNA
The methyl-cytosine-specific McrBc restriction enzyme McrBc (New England Biolabs) was used to cleave methylated DNA. Briefly, 200 ng DNA was digested with McrBc at 37 °C overnight and heat inactivated the next day at 65 °C for 1 h. Samples were run on a qPCR machine and standardized to uncut input. Delta CT values were converted to fold-change values and the ratio between A375PR1/A375 was calculated.
PI-annexin V staining
The cells were harvested, washed twice in PBS and resuspended in 100 μL annexin V incubation buffer (10 mM HEPES/NaOH, pH 7.4, 140 mM NaCl, 5 mM CaCl2) containing 1% annexin V FLOUS (Roche Molecular Biochemicals) and 500 μg/μL PI stain. The samples were incubated for 15 min at room temperature followed by adding 400 μL of ice-cold annexin V incubation buffer and subsequently analyzed on a cytometry machine.
IC50 measurements
4,000 cells per well were plated in 96 well plate format. The following day, cells were treated with the BRAFi vemurafenib (Selleckchem) at the indicated doses and further incubated for 72 h. The cell viability was then analyzed by MTS assay (Promega, Madison, WI, USA) according to manufacturer’s protocol followed by absorbance read at 490 nM using Tecan Spark 10 M plate reader (Tecan Trading AG, Switzerland). IC50 was analyzed using Graphpad Prism 8.0.
Colony formation assay
1000 cells per well were plated in 6 well plates and transfected 24 h later by using lipofectamine RNAiMax (Life Technologies), at a final concentration of 20 nM of gapmer ASO (Control or PTENP1-AS). Vemurafib treatment (or DMSO control) was initiated the day after transfection, cells were let grown for another 8–10 days before being fixed in 4% buffered formaldehyde and stained with 0.05% crystal violet. To estimate number of colonies, crystal violet staining was dissolved in 100% methanol, diluted to 1:10 in PBS and absorbance was measured at 540 nM using a Tecan Spark 10 M plate reader.
TCGA analysis
Gene expression profiles from GDC-TCGA (Genomic Data Commons—Cancer Genome Atlas) were utilized to correlate the expression of PTENP1-AS and PTEN in skin cutaneous melanoma (SKCM). We used the Xena browser (https://xenabrowser.net) to extract the RNA expression data for each gene, excluded samples with no expression of PTENP1-AS and PTEN, and correlated their expression using Spearman correlation (n = 251).
Patient samples
First regional lymph node metastases from stage III melanoma patients that had not received any systemic treatment were collected. The RNA was extracted using the Qiagen RNeasy mini kit (Qiagen). The RNA was DNase treated on column according to the manufacturer’s recommendations. The expression of PTENP1-AS was analyzed using qRTPCR and standardized to Beta-actin (dCt) by using the corresponding oligos in Supplementary Table 1. ddCt was calculated by using the mean Ct value of all samples. High expression of PTENP1-AS (Fig. 5e) was defined as Ct < 30.
Statistics
Two tailed Student’s T-test was used to determine statistical significance. Error bars represent the standard error of the mean. Statistical significance of the melanoma patient samples in Fig. 5e is evaluated using log-rank test. Throughout the paper, *P < 0.05; **P < 0.01; ***P < 0.005.
Ethical approval and consent to participate
This study has been approved by the Research Ethics Committee of Karolinska Institutet (Dnr: 2006/1373-31/3) and the Regional Ethics Committee in Lund (Dnr 2013/101). All involved individuals have provided informed consent to be included in the study. All the study procedures were carried out in accordance with relevant guidelines.
Supplementary Information
Acknowledgements
Professor Dan Grandér, who was the grant holder and the senior author of this project at the Department of Oncology & Pathology, passed away in October 2017. The authors are deeply sorrowed by his tragic death and dedicate this study to his memory.
Author contributions
L.V., A.A., I.D., I.S., and P.J. performed experiments. A.S.R. and O.S. provided general laboratory support for the research project. A.P and S.K designed gapmer antisense oligonucleotide. J.H., S.E.B., C.I., G.J., H.O., M.F.S. and R.T. provided and prepared clinical samples. L.V., D.G. and P.J. wrote the manuscript with the support from A.A., S.E.B., J.H. and K.P.T. D.G., S.E.B. and P.J. supervised the project.
Funding
Open access funding provided by Karolinska Institute. The project was supported by the Swedish Childhood Cancer Foundation under Grant [PR2015-0009; [PR2017-0078]; and The Swedish Cancer Society under Grants [CAN2017/326]; [CAN2015/698]; [CAN2014/851]; and Radiumhemmets Forskningsfonder under Grants [144063]; [171183], [144073] and the Karolinska Institutet’s PhD support program.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Suzanne Egyházi Brage, Email: suzanne.egyhazi.brage@ki.se.
Per Johnsson, Email: per.a.johnsson@ki.se.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-89389-9.
References
- 1.Davies H, et al. Mutations of the BRAF gene in human cancer. Nature. 2002 doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 2.Flaherty KT, et al. Inhibition of mutated, activated BRAF in metastatic melanoma. N. Engl. J. Med. 2010 doi: 10.1056/NEJMoa1002011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robert C, et al. Five-year outcomes with dabrafenib plus trametinib in metastatic melanoma. N. Engl. J. Med. 2019 doi: 10.1056/NEJMoa1904059. [DOI] [PubMed] [Google Scholar]
- 4.Liu D, Liu X, Xing M. Activities of multiple cancer-related pathways are associated with BRAF mutation and predict the resistance to BRAF/MEK inhibitors in melanoma cells. Cell Cycle. 2014 doi: 10.4161/cc.26971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roller DG, et al. Combinatorial drug screening and molecular profiling reveal diverse mechanisms of intrinsic and adaptive resistance to BRAF inhibition in V600E BRAF mutant melanomas. Oncotarget. 2016 doi: 10.18632/oncotarget.6548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paraiso KHT, et al. PTEN loss confers BRAF inhibitor resistance to melanoma cells through the suppression of BIM expression. Cancer Res. 2011 doi: 10.1158/0008-5472.CAN-10-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pei B, et al. The GENCODE pseudogene resource. Genome Biol. 2012 doi: 10.1186/gb-2012-13-9-r51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnsson P, et al. A pseudogene long-noncoding-RNA network regulates PTEN transcription and translation in human cells. Nat. Struct. Mol. Biol. 2013 doi: 10.1038/nsmb.2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawkins PG, Morris KV. Transcriptional regulation of Oct4 by a long non-coding RNA antisense to Oct4-pseudogene 5. Transcription. 2010 doi: 10.4161/trns.1.3.13332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poliseno L, et al. A coding-independent function of gene and pseudogene mRNAs regulates tumour biology. Nature. 2010 doi: 10.1038/nature09144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnsson P, Morris KV, Grandér D. Pseudogenes: A novel source of trans-acting antisense RNAs. Methods Mol. Biol. 2014 doi: 10.1007/978-1-4939-0835-6_14. [DOI] [PubMed] [Google Scholar]
- 12.Lister N, et al. The molecular dynamics of long noncoding RNA control of transcription in PTEN and its pseudogene. Proc. Natl. Acad. Sci. U. S. A. 2017 doi: 10.1073/pnas.1621490114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dankort D, et al. BrafV600E cooperates with Pten loss to induce metastatic melanoma. Nat. Genet. 2009 doi: 10.1038/ng.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Michaloglou C, et al. BRAFE600-associated senescence-like cell cycle arrest of human naevi. Nature. 2005 doi: 10.1038/nature03890. [DOI] [PubMed] [Google Scholar]
- 15.Azimi A, et al. Silencing FLI or targeting CD13/ANPEP lead to dephosphorylation of EPHA2, a mediator of BRAF inhibitor resistance, and induce growth arrest or apoptosis in melanoma cells. Cell Death Dis. 2017 doi: 10.1038/cddis.2017.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roh MR, et al. Promoter methylation of PTEN is a significant prognostic factor in melanoma survival. J. Investig. Dermatol. 2016 doi: 10.1016/j.jid.2016.01.024. [DOI] [PubMed] [Google Scholar]
- 17.Falkenius J, et al. High expression of glycolytic and pigment proteins is associated with worse clinical outcome in stage III melanoma. Melanoma Res. 2013 doi: 10.1097/CMR.0000000000000027. [DOI] [PubMed] [Google Scholar]
- 18.Alimonti A, et al. Subtle variations in Pten dose determine cancer susceptibility. Nat. Genet. 2010 doi: 10.1038/ng.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahn JH, Hwang SH, Cho HS, Lee M. Differential gene expression common to acquired and intrinsic resistance to BRAF inhibitor revealed by RNA-seq analysis. Biomol. Ther. 2019 doi: 10.4062/biomolther.2018.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Poliseno L, et al. Deletion of PTENP1 pseudogene in human melanoma. J. Investig. Dermatol. 2011 doi: 10.1038/jid.2011.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karreth FA, et al. In vivo identification of tumor-suppressive PTEN ceRNAs in an oncogenic BRAF-induced mouse model of melanoma. Cell. 2011 doi: 10.1016/j.cell.2011.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Viré E, et al. The Polycomb group protein EZH2 directly controls DNA methylation. Nature. 2006 doi: 10.1038/nature04431. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.