Abstract
Purpose:
To assess whether routine fundus photography (RFP) to screen for posterior segment disease at community eye clinics in South India increases referral to the urban hospital for ophthalmology care.
Design:
Stepped-wedge, cluster-randomized trial.
Participants:
Patients aged 40–75 and those aged 20–40 with a known history of hypertension or diabetes mellitus presenting to four technician-run, community eye care centers (vision centers) associated with the Aravind Eye Hospital, Pondicherry, India.
Methods:
Vision centers (clusters) were randomized to standard care or RFP across five 2-week study periods (steps). Patients in each cluster received standard care in the first step. At the start of each subsequent step, a randomly chosen cluster crossed over to providing RFP to eligible patients. Patients in all clusters took part in RFP during the last step. Standard care involved technician eye exams, optional fundus photography, and teleconsultation with an ophthalmologist. RFP involved technician eye exams, mandatory dilation and 40-degree fundus photography, and teleconsultation with an ophthalmologist.
Main outcome measures:
Standard care and RFP clusters were compared by the proportion of patients referred for in-person evaluation by an ophthalmologist due to fundus photography findings as well as urgency of referral (urgently in ≤2 weeks vs. non-urgently in >2 weeks). Generalized linear mixed models adjusting for cluster and step were used to estimate the odds of referral due to fundus photography findings compared to standard care.
Results:
1447 patients were enrolled across the vision centers, including 737 in the standard care group and 710 in the RFP group. Compared to standard care, the RFP group had a higher proportion of referrals due to fundus photography findings (11.3% vs. 4.4%), non-urgent referrals due to fundus photography (9.3% vs. 3.3%), and urgent referrals due to fundus photography (1.8% vs. 1.1%). The RFP intervention was associated with a two-fold increased odds of being referred due to photography findings compared to standard care (odds ratio=2.07, 95% confidence interval=0.98–4.40, p=0.058).
Conclusion:
Adding RFP to community eye clinics was associated with an increased odds of referral compared to standard care. This increase in referral was mostly attributed to non-urgent posterior segment disease.
Keywords: ophthalmology, telemedicine, diabetic retinopathy, epidemiology
In this large community-based randomized trial, adding mandatory fundus photography to routine eye examinations doubled detection of referral-warranted posterior segment diseases such as glaucoma and diabetic retinopathy, primarily due to detection of early stage pathology.
The major causes of global visual impairment and blindness are in transition due to greater numbers of elderly patients, widespread adoption of Western diets and lifestyles, and elimination of infectious diseases such as trachoma and onchocerciasis.1,2 Posterior segment diseases such as diabetic retinopathy, glaucoma, and age-related macular degeneration are accounting for a greater proportion of the global eye disease burden. From 1990 to 2015, the number of people with blindness due to diabetic retinopathy worldwide doubled from 0.2 million to 0.4 million while the number of people with visual impairment due to diabetic retinopathy nearly doubled from 1.4 million to 2.6 million.2 Glaucoma-related blindness increased from 2.5 million in 1990 to 3.0 million in 2015 while visual impairment due to glaucoma increased from 3.0 million to 4.0 million over the same time period.2 Patients living in rural or resource-limited settings in low and middle-income countries are at greater risk of visual impairment and blindness from posterior segment diseases, often due to lack of timely diagnosis and treatment,3 geographic clustering of fully-trained eye care providers in urban rather than rural locations,4 and substantial logistical and economic barriers to obtaining eye care far from home.5–7 Similar health disparities are evident in developed countries, where patients with diabetic retinopathy are less likely to undergo annual dilated eye examinations when residing in remote locations with limited geographic access to eye care professionals.8
Telemedicine is increasingly viewed as a potential solution to these challenges. Several fundus photography devices have shown high sensitivity and specificity for detection of posterior segment diseases such as diabetic retinopathy9 and glaucoma10 when compared to the gold standard of in-person slit lamp ophthalmoscopy.11 However, many studies of fundus photography screening published to date have been retrospective, non-randomized, inadequately powered, or focused on metrics of diagnostic validity such as sensitivity and specificity. Few prospective, randomized studies have rigorously compared the real-world effectiveness of fundus photography screening to preexisting standards of care in community settings. As telemedicine technology matures, demonstrating the practical utility of telemedicine approaches will be essential to justifying its widespread integration into routine eye care, particularly in low-resource settings where logistical and financial barriers to implementation are greatest.
The southern India state of Tamil Nadu has a substantial and increasing burden of posterior segment disease among its low-resource population, making it an appropriate setting to evaluate the effectiveness of telemedicine approaches. Population-based surveys from 2003 and 2006 revealed a 10.4% prevalence of vitreoretinal pathology12 and 2.6% prevalence of glaucoma.13 Prevalence likely has risen due to an aging population and a dramatic increase in diabetes mellitus prevalence over the past decade.14 As of 2016, diabetes mellitus affected one-fifth (20%) of the rural population and one-eighth (13%) of the semi-urban population in this region.14 At least 10% of examined patients with diabetes have retinopathy, but only 6.5% of patients have ever received an eye examination.12 As of 2006, 90% of Tamil Nadu patients diagnosed with primary open angle glaucoma had never undergone a prior eye examination; 5% of those patients were blind in one or both eyes.15 In 2016, a quality review at the Aravind Eye Care System showed that 10% of patients seen in community eye clinics underwent fundus photography, while the proportion of patients diagnosed with posterior segment disease was far lower than known local prevalence measured in previous population-based surveys.12,13 The need for screening to aid early diagnosis and treatment is evident. The purpose of this study was to evaluate the effectiveness of ancillary testing with fundus photography screening in a clinical setting. The goal is to improve early detection and referral for posterior segment eye diseases for patients presenting to rural primary eye care centers.
METHODS
Study population and setting
The Aravind Eye Care System in Tamil Nadu, India is a large eye health system that conducts over 4 million patient visits and performs over 450,000 surgeries annually. Over half of patients receive free or subsidized eye care.16 Aravind provides eye care to smaller communities through 76 vision centers (VC) located between 45 minutes and three hours away from the nearest main eye hospital. Patients presenting to VCs are examined by trained non-physician ophthalmic technicians who are adept at basic vision examination, refraction, and anterior segment slit lamp examination.17 Examinations traditionally focused on identifying refractive error and signs of anterior segment disease, such as cataract and conjunctivitis. Technicians have less resources and training to evaluate the posterior segment of the eye. In a routine evaluation, the technicians perform an examination and then connect via live video teleconferencing to convey examination findings and obtain advice from an ophthalmologist at the nearest base hospital. The ophthalmologist finalizes each patient’s management plan. Patients with non-vision threatening conditions, such as refractive error, dry eye syndrome, conjunctivitis, and corneal abrasion, are prescribed treatment locally and asked to follow up at the VC. Patients with unclear diagnoses or potentially vision-threatening pathology are referred to the base hospital at the discretion of the ophthalmologist in a time urgency related to the assessment.
If the teleconsulting ophthalmologist suspects posterior segment disease, the technician can attempt fundus photography if the camera is available and upload the photo for immediate interpretation as part of teleconsultation. This option has been infrequently utilized due to training and resource limitations.
Stepped-wedge clinical trial design
A stepped-wedge, cluster-randomized, clinical trial design18 was used to evaluate the effectiveness of routine fundus photography for early detection and referral due to signs of posterior segment disease among patients presenting to four VCs associated with Aravind base hospital in Pondicherry, India. Four VCs were selected as study sites that had been operational for multiple years and were staffed by experienced technicians. Under the stepped-wedge design, allocation to control and intervention groups occurred at the VC (cluster) level. The four VC clusters were randomized to receive the intervention at one of the four predefined, two-week steps over ten total weeks from August 14, 2017 to October 23, 2017. During the first two-week step, participants presenting to all four VC clusters were allocated to the control group (standard practice of optional fundus photography at the teleconsulting ophthalmologist’s request). At the beginning of each subsequent two-week step, one additional randomly selected VC crossed over to the intervention group (routine fundus photography). This sequential rollout of the intervention resulted in all four VCs participating in the intervention group during the final two-week step. A fifth VC was originally selected to participate, but ultimately did not take part in stepped-wedge randomization and instead provided the intervention at all steps. As a result, this VC was excluded from the stepped-wedge study’s final main analysis. A supplemental analysis was performed including data from this VC and is briefly presented with details included in an online appendix. This study protocol was approved by the Institutional Review Board at the Aravind Eye Care System and adhered to the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants prior to participation in the study.
Eligibility criteria
Upon patient arrival to the VC, technicians verified eligibility criteria for study participation and recorded participants’ informed consent in the electronic medical record. Eligible participants included anyone 40 to 75 years old, as well as those who were 20 to 40 years old with a reported history of hypertension, diabetes mellitus, or a family history of glaucoma. To limit the study to participants without a prior diagnosis of chronic eye disease, participants who had previously been seen at one of the urban, base eye hospitals for any reason were excluded. Technicians also collected participants’ baseline sociodemographic information such as sex, occupation, education level, type of housing, and annual household income.
Intervention
Participants in control clusters underwent a technician-performed eye examination followed by teleconsultation with an ophthalmologist at the base hospital. Evaluations typically focused on refractive error and anterior segment disease. In keeping with standard practice, fundus photography was optional and was only obtained if specifically requested by the ophthalmologist during teleconsultation.
Participants in intervention clusters underwent a similar technician-performed eye examination as well as pupillary dilation and fundus photography prior to teleconsultation. Participants with shallow anterior chambers preventing safe dilation, significant media opacities preventing photography, active ocular trauma or inflammation preventing dilation or photography, or lack of desire to participate in the intervention were not required to undergo dilation and photography. All participants in the intervention cluster who underwent fundus photography were shown their own fundus photographs to assist with counseling during teleconsultation.
Fundus photographs were taken using the Bosch handheld non-mydriatic fundus camera (Bosch, Inc., Germany). In undilated patients with clear media, this fundus camera can reliably obtain high quality 40-degree color photos of the macula and optic disc.19 Upon viewing the fundus photograph, the teleconsultation ophthalmologist graded each fundus photograph in terms of quality (clear, centered, both, or neither). During a pilot period occurring several months prior to the study, each technician was trained to perform fundus photography using the camera and was required to obtain clear and centered fundus photographs for >90% of a convenience sample of 20 consecutive patients. At the time of teleconsultation, the ophthalmologist also assigned clinical diagnoses to each photograph. Diagnostic choices included normal fundus, diabetic retinopathy, diabetic macular edema, hypertensive retinopathy, retinal vein occlusion, retinal arterial occlusion, age-related macular degeneration, disc/glaucoma suspect, glaucoma, or a free text field in which the ophthalmologist could enter any other diagnosis.
Outcomes
The primary outcome was participant referral to the base hospital for evaluation by an ophthalmologist specifically due to findings on fundus photography. Participant referral due to findings on regular clinical examination performed by the technician was also assessed. The teleconsultation ophthalmologist noted his/her reason for referral (fundus photography findings vs. findings from technician’s usual examination) at the time of teleconsultation. A secondary outcome was participants urgently referred versus non-urgently referred. Urgency was also determined by the ophthalmologist at the time of teleconsultation. “Urgent” referral was defined as recommended follow-up within 2 weeks of teleconsultation. “Non-urgent” referral was defined as follow-up more than 2 weeks after the teleconsultation. Lastly, we evaluated the proportion of participants diagnosed with normal fundi or specific posterior segment diseases at the time of teleconsultation. Participants were labeled as having normal fundi if both eyes’ fundus photographs were interpreted as “normal.” Participants were diagnosed with a posterior segment disease if either eye’s fundus photograph was assigned that diagnosis.
Statistical analysis
Demographic variables were summarized for control and intervention groups using means and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables. Differences between groups were tested with t-tests and chi-squared tests. Rates of referral to the base hospital were summarized with proportions by VC and step and displayed using line plots. Consistent with prior analyses of studies using the stepped wedge design,18 generalized linear mixed models (GLMM) were used to evaluate the association of the intervention with probability of referral to the base hospital due to fundus photography. These models analyzed data at the subject level but including a random effect for cluster (VC) and a fixed effect for step (time). GLMMs used the binomial distribution and logit link, and results are reported with odds ratios (OR) and 95% confidence intervals (CI). Analyses are presented for the 4 VCs that adhered to the stepped-wedge study design, but a separate analysis including the fifth VC is briefly presented with details provided in supplemental material. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Participants
Out of 1650 participants assessed for study eligibility, 3 were excluded due to age or comorbidity status and 200 were excluded because of prior receipt of care at a base eye hospital. A total of 1447 eligible participants were enrolled across four VCs over five two-week steps, with 737 participants in the control group and 710 participants in the intervention group (Figure 1). The first vision center enrolled 238 participants, of which 47 (20%) were controls from step 1 and 191 (80%) received the intervention over steps 2–5. Similarly, the second vision center enrolled 526 participants (46% control from steps 1–2, 54% intervention from steps 3–5), the third vision center enrolled 426 participants (58% control from steps 1–3, 42% intervention from steps 4–5), and the fourth vision center enrolled 257 participants (80% control from steps 1–4, 20% intervention from step 5). Baseline sociodemographic characteristics for participants in the control and intervention groups are presented in Table 1. The two groups were similar with respect to age (control mean ± SD, 51.9 ± 9.3 years; intervention, 52.3 ± 9.1 years), prevalence of self-reported hypertension (control, 15.3%; intervention, 12.8%) and diabetes mellitus (control, 16.0%; intervention, 17.2%). Compared to the intervention group, the control group had a higher proportion of females (57.1% versus 50.9%, p=0.0166), low-wage laborers (11.3% vs. 8.2%, p=0.0455), and participants reporting an annual income of less than 20,000 Indian rupee (INR) per year (28.5% versus 6.1%, p<0.0001).
Figure 1.
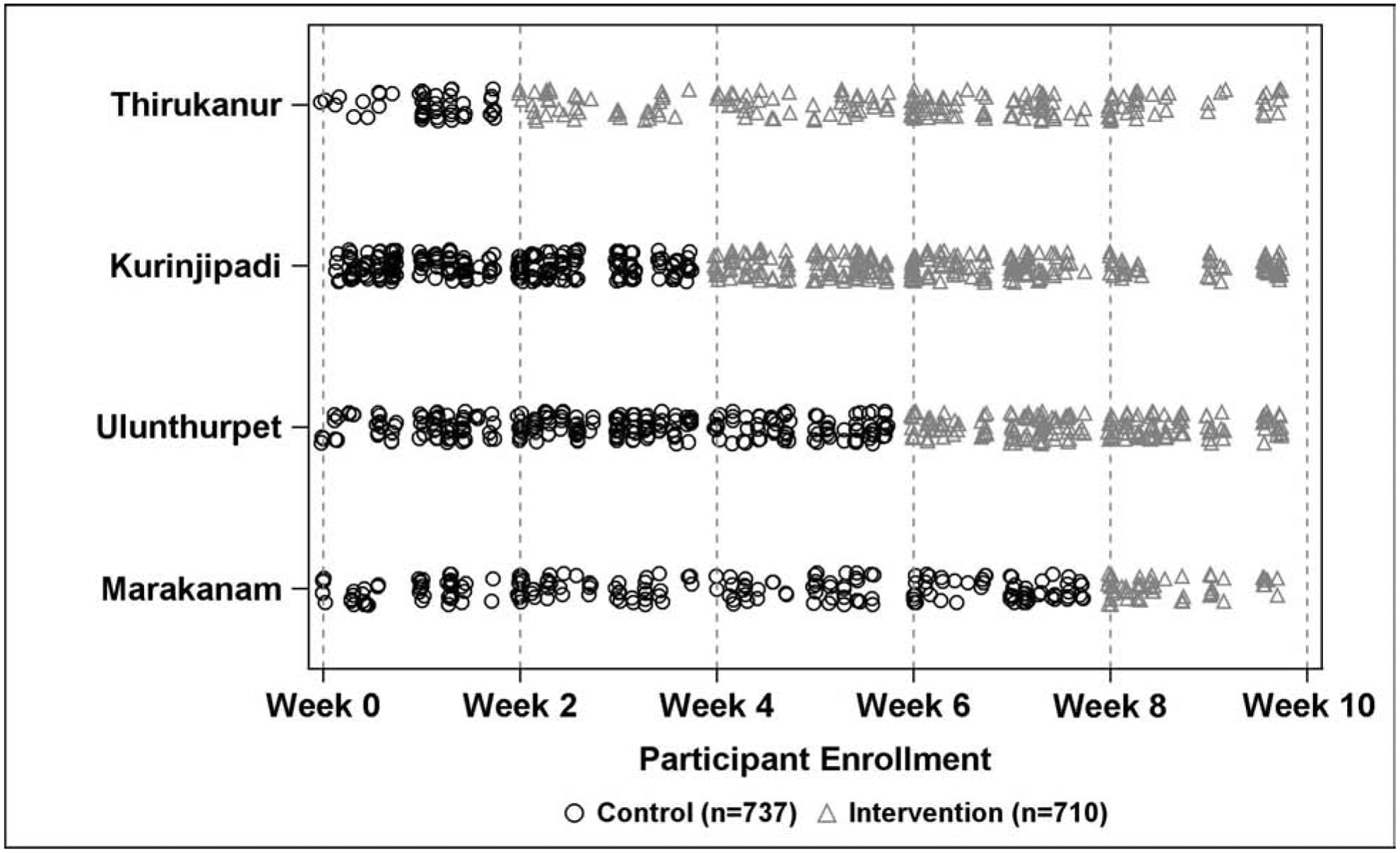
Scatterplot showing the stepped-wedge study design across four vision centers (clusters) and five 2-week steps. Each plotted symbol represents a patient who received either the control standard of care (circles) or the routine fundus photography intervention (triangles).
Table 1.
Demographic characteristics of enrolled patientsa
| Variable | Control N=737 (51%) |
Intervention N=710 (49%) |
Total N=1447 |
p valuea |
|---|---|---|---|---|
| Age (years) | mean ± SD | mean ± SD | mean ± SD | 0.3268 |
| 51.9 ± 9.3 | 52.3 ± 9.1 | 52.1 ± 9.2 | ||
| N (%) | N (%) | N (%) | ||
| Gender | ||||
| Male | 316 (42.9) | 349 (49.2) | 665 (46.0) | 0.0166 |
| Female | 421 (57.1) | 361 (50.9) | 782 (54.0) | |
| House Type | ||||
| Cement | 566 (77.2) | 599 (84.6) | 1165 (80.9) | 0.0004 |
| Non-cement | 167 (22.8) | 109 (15.4) | 276 (19.1) | |
| Occupation | ||||
| Laborer | 83 (11.3) | 58 (8.2) | 141 (9.7) | 0.0455 |
| Farmer | 188 (25.5) | 188 (26.5) | 376 (26.0) | |
| Housewife | 166 (22.5) | 164 (23.1) | 330 (22.8) | |
| None | 190 (25.8) | 161 (22.7) | 351 (24.3) | |
| Other | 110 (14.9) | 139 (19.6) | 249 (17.2) | |
| Education | ||||
| None | 317 (43.0) | 286 (40.3) | 603 (41.7) | 0.2514 |
| Primary school | 149 (20.2) | 130 (18.3) | 279 (19.3) | |
| Secondary school | 213 (28.9) | 222 (31.3) | 435 (30.1) | |
| Higher secondary | 25 (3.4) | 24 (3.4) | 49 (3.4) | |
| Undergraduate or higher | 33 (4.5) | 48 (6.8) | 81 (5.6) | |
| Income (INR) | ||||
| <20000 | 191 (28.5) | 43 (6.1) | 234 (17.1) | <0.0001 |
| 20000 to 50000 | 433 (64.5) | 542 (77.3) | 975 (71.1) | |
| >50000 | 47 (7.0) | 116 (16.6) | 163 (11.9) | |
| Diabetes | ||||
| Yes | 118 (16.0) | 122 (17.2) | 240 (16.6) | 0.5490 |
| No | 619 (84.0) | 588 (82.8) | 1207 (83.4) | |
| Hypertension | ||||
| Yes | 113 (15.3) | 91 (12.8) | 204 (14.1) | 0.1693 |
| No | 624 (84.7) | 619 (87.2) | 1243 (85.9) | |
SD, standard deviation; INR, Indian Rupee
P values calculated using t test for age and chi square test for all other variables.
Fundus photograph utilization and quality
Fundus photography utilization in the control group was 9.2% overall (N=68) and ranged from 4.9% to 21.7% over the steps of the study. Fundus photography utilization in the intervention group was high at 97% (N=689) and remained consistently high across all intervention steps (range: 93%−99%). The proportion of photographs graded “clear and centered” was 73% among the control group compared to 94% among the intervention group, and 92.5% overall. Although 65% of fundus photographs taken during step 1 were graded clear and centered, as technicians within VCs assigned to the intervention gained experience with fundus photography, this proportion increased over time (88% in step 2, 92% in step 3, 96% in step 4, 95% in step 5).
Referral for in-person examination
Out of 1447 patients in the study, 1435 had information on referral status (708 intervention patients; 727 control patients). A total of 485 patients (33.8%) were referred to the base hospital for in-person ophthalmology care, of which 112 were referred due to fundus photography findings and 373 were referred due to standard examination. Overall, the intervention group referred a higher proportion of subjects due to fundus photography findings than the control group (11.3% [80 of 708] versus 4.4% [32 of 727], respectively). Based on this increase in proportion of referrals, we calculated that for every 14.5 patients screened with routine fundus photography in the VC setting, one additional patient would be referred to the base hospital due to fundus photography findings. The proportions of participants who were referred to the base hospital for examination by an ophthalmologist due to fundus photography findings, stratified by VC and step, are displayed in Table 2 and Figure 2. After adjustment for VC and step in the model to account for study design, the intervention was associated with an increased odds of being referred to the base hospital due to photography findings compared to controls (OR=2.07, 95% CI: 0.98–4.40, p=0.0581). The proportion referred due to regular technician examination findings, as well as the overall proportion referred, are also reported in Table 2.
Table 2.
Proportion of patients referreda to the base hospital for examination by an ophthalmologist, overall and due to fundus photography findings or due to technician examination, stratified by vision center and step.
| Time | Treatment | N | Nnonmissing | Referral Due to Fundus Photography | Referral Due to Regular Examination | All Referred | |||
|---|---|---|---|---|---|---|---|---|---|
| Nreferred | Preferred | Nreferred | Preferred | Preferred | Preferred | ||||
| Thirukanur (n=238) | |||||||||
| Step 1 | Control | 47 | 43 | 2 | 0.05 | 15 | 0.35 | 17 | 0.40 |
| Step 2 | Intervention | 41 | 41 | 0 | 0.00 | 16 | 0.39 | 16 | 0.39 |
| Step 3 | Intervention | 43 | 43 | 5 | 0.12 | 11 | 0.26 | 16 | 0.37 |
| Step 4 | Intervention | 65 | 65 | 4 | 0.06 | 18 | 0.28 | 22 | 0.34 |
| Step 5 | Intervention | 42 | 42 | 6 | 0.14 | 11 | 0.26 | 17 | 0.40 |
| Kurinjipadi (n=526) | |||||||||
| Step 1 | Control | 121 | 118 | 5 | 0.04 | 26 | 0.22 | 31 | 0.26 |
| Step 2 | Control | 119 | 119 | 0 | 0.00 | 22 | 0.18 | 22 | 0.18 |
| Step 3 | Intervention | 110 | 109 | 9 | 0.08 | 23 | 0.21 | 32 | 0.29 |
| Step 4 | Intervention | 119 | 119 | 9 | 0.08 | 31 | 0.26 | 40 | 0.34 |
| Step 5 | Intervention | 57 | 57 | 4 | 0.07 | 23 | 0.40 | 27 | 0.47 |
| Ulunthurpet (n=426) | |||||||||
| Step 1 | Control | 71 | 69 | 3 | 0.04 | 18 | 0.26 | 21 | 0.30 |
| Step 2 | Control | 98 | 98 | 5 | 0.05 | 28 | 0.29 | 33 | 0.34 |
| Step 3 | Control | 77 | 77 | 1 | 0.01 | 28 | 0.36 | 29 | 0.38 |
| Step 4 | Intervention | 97 | 96 | 11 | 0.11 | 24 | 0.25 | 35 | 0.36 |
| Step 5 | Intervention | 83 | 83 | 20 | 0.24 | 20 | 0.24 | 40 | 0.48 |
| Marakanam (n=257) | |||||||||
| Step 1 | Control | 49 | 48 | 4 | 0.08 | 13 | 0.27 | 17 | 0.35 |
| Step 2 | Control | 50 | 50 | 2 | 0.04 | 7 | 0.14 | 9 | 0.18 |
| Step 3 | Control | 45 | 45 | 4 | 0.09 | 18 | 0.40 | 22 | 0.49 |
| Step 4 | Control | 60 | 60 | 6 | 0.10 | 8 | 0.13 | 14 | 0.23 |
| Step 5 | Intervention | 53 | 53 | 12 | 0.23 | 13 | 0.25 | 25 | 0.47 |
Referral data available for 727 of 737 control group participants (Nmissing=10) and 708 of 710 intervention group participants (Nmissing=2).
Figure 2.
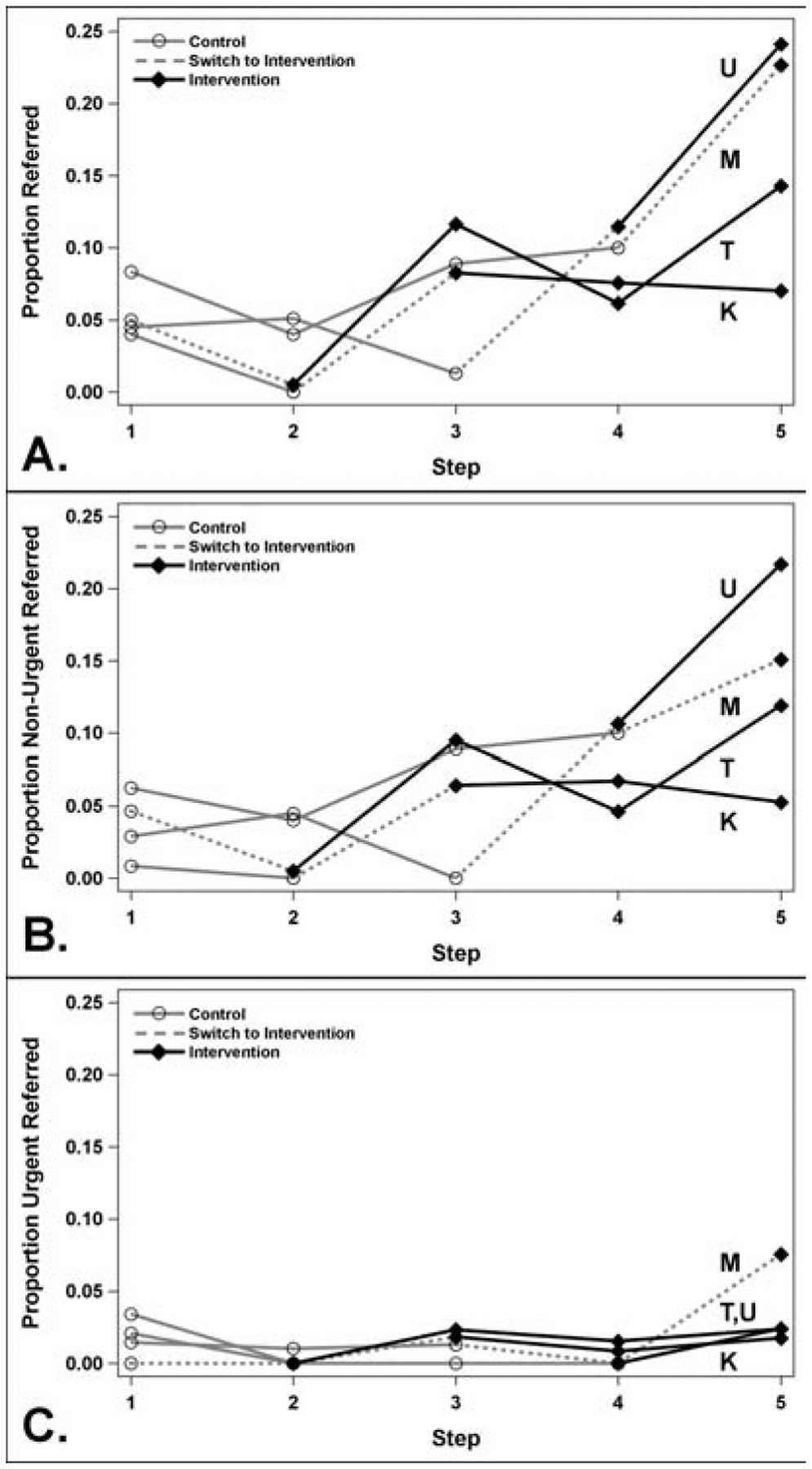
Line plot showing the proportion of patients referred to the base hospital due to fundus photography findings, by vision center and step. Proportions are plotted, A. overall, B. non-urgently, and C. urgently. Each line represents a different vision center (T, Thirukanur; K, Kurinjipadi; U, Ulunthurpet; M, Marakanam). Note: some proportions were offset slightly for better visualization of lines.
Out of the 1435 patients in the study who had information on referral status, 1432 also had information on urgency of referral (706 intervention patients; 726 control patients). The majority of the 112 patients referred to the base hospital for ophthalmology care due to fundus photography findings were non-urgently referred (n=90), with a minority urgently referred (n=21), and one patient was missing data on urgency status. Overall, patients in the intervention group were non-urgently referred following fundus photography findings at a higher rate than those in the control group (9.3% [66 of 706 with non-missing urgency status] versus 3.3% [24 of 726], respectively). Similarly, intervention patients were urgently referred at a higher rate than controls (1.8% [13 of 706] versus 1.1% [8 of 726], respectively). Proportions non-urgently referred and urgently referred, stratified by VC and step, are displayed in eTables 1–2 and Figure 2. After adjustment for VC and step in the model accounting for study design, the intervention was associated with a non-significant increase in the odds of being non-urgently referred to the base hospital following fundus photography findings compared to controls (OR=1.93, 95% CI: 0.86–4.37, p=0.1130; Table 3). A similar result was observed for urgent referral following fundus photography findings (OR=2.21, 95% CI: 0.35–14.03, p=0.4002; Table 3).
Table 3.
Model results for the effect of intervention on the probability of referral to the base hospital. Models are adjusted for step effects and contain a random effect for vision center (cluster). N=1447 total patients.
| Outcome | Overall | Urgent | Non-Urgent | |||
|---|---|---|---|---|---|---|
| # referred | OR (95% Cl) p-value |
# referred | OR (95% Cl) p-value |
# referred | OR (95% Cl) p-value |
|
| Referral Due to Fundus Photography | 112 | 2.07 (0.98, 4.40) p=0.0581 |
21 | 2.21* (0.35, 14.03) p=0.4002 |
90 | 1.93 (0.86, 4.37) p=0.1130 |
| Referral Due to Technician Exam | 373 | 1.05 (0.71, 1.56) p=0.7924 |
28 | 1.44 (0.41, 5.05) p=0.5681 |
343 | 1.00 (0.67, 1.48) p=0.9855 |
| Referral for Any Reason | 485 | 1.21 (0.83, 1.77) p=0.3198 |
49 | 1.97 (0.71, 5.48) p=0.1920 |
433 | 1.10 (0.75, 1.62) p=0.6339 |
OR, Odds Ratio; CI, Confidence Interval
due to the small number of referral events, the generalized linear mixed model would not converge as parameterized, simple logistic regression results reported; note: sample sizes do not sum to overall number referred due to missing data on urgency of referral.
The fifth VC provided the intervention to eligible patients (n=123) at all steps of the study, with referral rates due to fundus photography at each step of 0.15, 0.10, 0.13, 0.16, and 0.06 (eFigures 1–2, eTable 3). As observed with the other VCs, the majority of patients referred due to fundus photography were non-urgent (0.15, 0.10, 0.09, 0.16, and 0.06, respectively). Including data from this VC in the model adjusting for VC and step, the intervention was significantly associated with increased odds of being referred to the base hospital due to fundus photography findings (both non-urgent and urgent) compared to controls (OR=2.54, 95% CI: 1.32–4.90, p=0.0055; eTable 4). This result was driven by non-urgent referrals due to fundus photography (OR=2.66, 95% CI: 1.29–5.48, p=0.0082) and not by urgent referrals due to fundus photography (OR=1.47, 95% CI: 0.36–5.89, p=0.5899).
Diseases detected on fundus photography
eTable 5 shows fundus photography diagnoses in control and intervention patients. Among the 68 controls that underwent fundus photography, 23 (34%) had normal fundus photographs for both eyes, while most others were diagnosed in at least one eye with diabetic retinopathy (N=7 or 10%), disc/glaucoma suspect (N=16 or 24%), glaucoma (N=2 or 3%), and/or other posterior segment pathology (N=13 or 19%). Since an eye can have more than one diagnosis, sample sizes do not sum to totals. Out of 689 participants in the intervention group that underwent routine fundus photography, 515 (75%) had normal fundi while the remainder had diagnoses of disc/glaucoma suspect (N=38 or 6%), diabetic retinopathy (N=12 or 2%), diabetic macular edema (N=5 or 1%), hypertensive retinopathy (N=5 or 1%), age-related macular degeneration (N=11 or 2%), or other pathology (N=40, 6%) in one or both eyes. Among the 66 participants in the intervention group who were referred for non-urgent ophthalmologist evaluation due to fundus photography findings, 33 (50%) were diagnosed as disc/glaucoma suspects, 6 (9%) with diabetic retinopathy, 2 (3%) with diabetic macular edema, and 21 (33%) with other posterior segment pathologies.
DISCUSSION
This is the first large stepped-wedge, cluster-randomized trial assessing the value of fundus photography in screening for posterior segment pathology. Among 1447 subjects presenting to community eye clinics in Tamil Nadu, India, adding routine fundus photography to regular technician-performed eye examinations increased the proportion of participants referred for evaluation of posterior segment disease by an ophthalmologist, particularly for non-urgent posterior segment disease. The proportion of participants referred for urgent pathology showed little change. Although further studies should seek to replicate these findings in different populations and health care settings, our findings may be of interest to eye care and public health practitioners as they seek to integrate teleophthalmology and fundus photography into routine eye care in both developed and developing country settings.
Urgent versus non-urgent pathology
Routine fundus photography was associated with an increase in the proportion of participants referred specifically due to fundus photograph findings (11.3% for intervention group versus 4.4% for control group). The proportion of participants referred due to non-urgent fundus photograph findings increased nearly three-fold (9.3% vs. 3.3%). Even after adjusting for differences across four study clusters and five time periods, our model showed a two-fold increase in odds of referral due to fundus photography findings (p=0.0581). These findings indicate a practical use of fundus photography to influence screening diagnosis and referral at earlier stages of posterior segment disease. Consistent with known estimates of local disease prevalence, participants in this study who had diabetic retinopathy, suspected glaucoma, and age-related macular degeneration comprised the majority of those referred.
Even in a population with a known high prevalence of blindness from glaucoma13,20 and an increasing burden of diabetic retinopathy,12 routine fundus photography in community eye clinics was not associated with any substantial increase in referral for urgent reasons (1.8% vs. 1.1%) or for overall referrals. Our findings suggest that in individuals with acute and/or severe vision loss, fundus photography may not be the critical tool that aids patients in receiving care, perhaps because the patient is already symptomatic and may self-present for evaluation. Fundus photography may instead be better utilized as a screening tool for occult, potentially blinding chronic eye diseases such as glaucoma or earlier stages of diabetic retinopathy. Timely, effective community-based counseling about the disease process, preventive measures, and the importance of regular follow-up could prevent disease progression and reduce the human, financial, and health system burden of severe vision loss from later stage diseases.
Photograph quality and utilization over time
The quality of fundus photographs increased with use during the study period. Although 67% of photographs in the first (control) step were graded clear and centered, among the VC randomized to routine fundus photography this proportion increased to 88% by the second step and remained in the 92–96% range for the remainder of the study. The proportion of participants referred non-urgently due to fundus photography also increased across the clusters and time periods. Taken together, these results indicate that the diagnostic utility of fundus photography increases with frequent use; the ophthalmic technicians became more facile with the technology. Consistent with our findings, a prior study noted progressive increases in the proportion of gradable photographs taken by ancillary staff using a non-mydriatic fundus camera over a 13 month period.21 Short-term evaluations of telemedicine modalities may therefore fail to fully capture the clinical impact of technology integration over a longer time period. We hypothesize the quality of images would continue to rise before an eventual plateau for each user. These results also emphasize the importance of training staff and of workforce stability.
Strengths and limitations
To our knowledge, this is the first ophthalmology trial to use a stepped-wedge, cluster-randomized design. While traditional clinical trials measure an intervention’s efficacy under ideal testing conditions, stepped-wedge trials enable measurement of an intervention’s effectiveness in real-world settings. By using a staged rollout of a healthcare intervention, the design permits close observation of the intervention’s effects across multiple clusters and time points while ensuring that all clusters eventually implement the potentially beneficial intervention. This design is increasingly used to evaluate the effectiveness of healthcare delivery innovations in settings such as nursing homes,22 hospital wards,23 and community clinics where randomization and implementation at the cluster level are more logistically feasible than at the individual participant level. In keeping with cluster randomized trials, stepped-wedge trials require larger sample sizes than trials that randomize individuals.24 Furthermore, their results can be influenced by temporal trends across steps as well as differences in subject characteristics and intervention effects across clusters. The “borderline statistical significance” of our model’s findings after adjusting for differences across four study clusters and five time periods (p=0.0581) may represent limitations in the number of referrals (n=112) rather than a lack of strength of association. The stepped-wedge trial design may be well-suited for rigorous comparative evaluation of eye care delivery approaches in communities and merits further consideration in ophthalmology.
This study also has several limitations due to the particular intervention, health care setting, and population examined. Changes to any of these factors could well have yielded different results. The study only evaluated the benefits of fundus photography as an adjunct to refractive and anterior segment slit lamp examinations in a community eye clinic, not as a replacement for eye examinations altogether. However, the eye care delivery model used in this study’s intervention group may be considered similar to examinations provided by many non-ophthalmic providers. Requiring dilation before fundus photography increased the ease and quality of photography but limited generalizability of findings to populations undergoing non-mydriatic fundus photography. Future studies should evaluate utility of non-mydriatic fundus photography which can still obtain high-quality images without the inconvenience of patient dilation. Patients presenting to eye clinics may have been more likely to have posterior segment disease than the general population, although the proportion of participants diagnosed with suspected glaucoma (6%) and diabetic retinopathy (2%) in the routine fundus photography group was similar to prevalence estimates from population-based surveys. Different results may be expected in primary care clinics, diabetes clinics, and regions with different disease burdens. The Aravind Eye Care System’s strong technician training, adherence to fundus photography recommendations, and human resources availability may also limit generalizability of this study’s findings to other eye care delivery settings.
Several factors may bias this study’s findings toward the null. The handheld non-mydriatic camera used in this study was developed in 2015, but newer fundus cameras developed since that time may offer improved photo quality, wider field of view than 40 degrees, and greater ease of adoption, all of which may further increase disease detection and referral rates in the future as technology continues to advance. In low-resource rural settings patients typically need to overcome substantial logistical and financial challenges before receiving subspecialty care at an urban eye hospital located up to three hours away. The teleconsultation ophthalmologist’s clinical threshold for referral based on fundus photography findings may therefore have been higher that it would be in developed countries, where patients with even the earliest stages of disease on photography are more likely to get referred for a confirmatory in-person examination by an ophthalmologist. Despite being non-physicians, the VC technicians of Aravind Eye Hospital are highly trained and often remarkably adept at skills typically considered within the province of the ophthalmologist. Although individual technicians’ ability to examine the posterior segment varied substantially, during the study’s pilot phase several technicians demonstrated impressive competence at dilated fundus examinations and were able to accurately diagnose conditions such as glaucoma, macular degeneration, and central serous chorioretinopathy without the help of fundus photography. The benefits of routine fundus photography may therefore be greater in settings with less skilled staff.
This study’s results should also be viewed in the context of ongoing advances in artificial intelligence (AI) approaches for detection of posterior segment diseases. Recent studies have demonstrated the ability for deep learning approaches to detect mild diabetic retinopathy,25 referral-warranted diabetic retinopathy,26,27 sight-threatening diabetic retinopathy,27 age-related macular degeneration,27 glaucomatous-appearing optic disc changes,27,28 and referable glaucomatous optic neuropathy with a greater than 0.7 cup:disc ratio29 with most studies consistently demonstrating sensitivity over 90% and specificity over 85% across multiple programs and datasets. Offline AI analysis of fundus photographs taken using a smartphone-based camera showed 100% sensitivity and 88% specificity for detecting referral-warranted diabetic retinopathy compared to the gold standard of photograph interpretation by an ophthalmologist.30 Automated grading of diabetic retinopathy using 40 to 45 degree fundus photographs achieved 92% sensitivity and 95% specificity compared to grading performed by ophthalmologists.26 Although our study assessed the impact of live fundus photograph interpretation by an ophthalmologist, the substantial changes in diagnosis and referral patterns from adding this single new imaging modality may indicate the potential of AI-based fundus photograph interpretation to influence preventive care at the community level without live reliance on ophthalmologists. More research on the real-world effects of integrating AI into regular clinical care is needed.
In this pragmatic trial, all referral decisions were made by the tele-consultation ophthalmologist at the point of care after weighing several clinical factors such as visual acuity, patient complaints, anterior segment examination findings, and fundus photography findings. Although this study only assessed whether fundus photography findings prompted referral irrespective of specific diagnosis, future research should also examine whether specific fundus photography diagnoses, such as proliferative diabetic retinopathy or end-stage glaucoma, are more likely to trigger referral decisions. This study only examined the effect of fundus photography on referral patterns in the primary eye care setting, but future studies should assess agreement between remote diagnoses made using fundus photography and diagnoses made via ophthalmologists’ in-person examination. Future studies should assess patient satisfaction with remote fundus photography as well as patients’ adherence to follow-up recommendations.
In conclusion, adding routine fundus photography to technician-performed eye examinations and teleconsultation services at vision centers in Tamil Nadu was associated with an increase in patient referrals for in-person evaluation of posterior segment disease by an ophthalmologist. Although non-urgent referrals increased, urgent referrals remained similar. Fundus photograph quality increased over time.
Supplementary Material
eFigure 1. Scatterplot showing the stepped-wedge study design across five vision centers (clusters) and five 2-week steps. Each plotted symbol represents a patient who received either the control standard of care (circles) or the routine fundus photography intervention (triangles).
eFigure 2. Line plot showing the proportion of patients referred to the base hospital due to fundus photography findings, by vision center and step. Proportions are plotted, A. overall, B. non-urgently, and C. urgently. Each line represents a different vision center (T, Thirukanur; K, Kurinjipadi; U, Ulunthurpet; M, Marakanam; Th, Thiruvennainalur). Note: some proportions were offset slightly for better visualization of lines.
Conflict of Interest/Funding:
Dr. Woodward reported receiving grants from National Institutes of Health (NIH- 1R01EY031033)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Bourne RRA, Stevens GA, White RA, et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1(6):e339–349. doi: 10.1016/S2214-109X(13)70113-X [DOI] [PubMed] [Google Scholar]
- 2.Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221–e1234. doi: 10.1016/S2214-109X(17)30393-5 [DOI] [PubMed] [Google Scholar]
- 3.Olatunji VA, Adepoju FG, Owoeye JFA. Perception and Attitude of a Rural Community Regarding Adult Blindness in North Central Nigeria. Middle East Afr J Ophthalmol. 2015;22(4):508–513. doi: 10.4103/0974-9233.167826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Estopinal CB, Ausayakhun S, Ausayakhun S, et al. Access to ophthalmologic care in Thailand: a regional analysis. Ophthalmic Epidemiol. 2013;20(5):267–273. doi: 10.3109/09286586.2013.821498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olusanya BA, Ashaye AO, Owoaje ET, Baiyeroju AM, Ajayi BG. Determinants of Utilization of Eye Care Services in a Rural Adult Population of a Developing Country. Middle East Afr J Ophthalmol. 2016;23(1):96–103. doi: 10.4103/0974-9233.164621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marmamula S, Khanna RC, Shekhar K, Rao GN. A population-based cross-sectional study of barriers to uptake of eye care services in South India: the Rapid Assessment of Visual Impairment (RAVI) project. BMJ Open. 2014;4(6):e005125. doi: 10.1136/bmjopen-2014-005125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kovai V, Krishnaiah S, Shamanna BR, Thomas R, Rao GN. Barriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh, South India. Indian J Ophthalmol. 2007;55(5):365–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chou C-F, Zhang X, Crews JE, Barker LE, Lee PP, Saaddine JB. Impact of geographic density of eye care professionals on eye care among adults with diabetes. Ophthalmic Epidemiol. 2012;19(6):340–349. doi: 10.3109/09286586.2012.722244 [DOI] [PubMed] [Google Scholar]
- 9.Williams GA, Scott IU, Haller JA, Maguire AM, Marcus D, McDonald HR. Single-field fundus photography for diabetic retinopathy screening: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111(5):1055–1062. doi: 10.1016/j.ophtha.2004.02.004 [DOI] [PubMed] [Google Scholar]
- 10.Myers JS, Fudemberg SJ, Lee D. Evolution of optic nerve photography for glaucoma screening: a review. Clinical & Experimental Ophthalmology. 2018;46(2):169–176. doi: 10.1111/ceo.13138 [DOI] [PubMed] [Google Scholar]
- 11.Gupta A, Cavallerano J, Sun JK, Silva PS. Evidence for Telemedicine for Diabetic Retinal Disease. Semin Ophthalmol. 2017;32(1):22–28. doi: 10.1080/08820538.2016.1228403 [DOI] [PubMed] [Google Scholar]
- 12.Nirmalan PK, Katz J, Robin AL, et al. Prevalence of vitreoretinal disorders in a rural population of southern India: the Aravind Comprehensive Eye Study. Arch Ophthalmol. 2004;122(4):581–586. doi: 10.1001/archopht.122.4.581 [DOI] [PubMed] [Google Scholar]
- 13.Ramakrishnan R, Nirmalan PK, Krishnadas R, et al. Glaucoma in a rural population of southern India: the Aravind comprehensive eye survey. Ophthalmology. 2003;110(8):1484–1490. doi: 10.1016/S0161-6420(03)00564-5 [DOI] [PubMed] [Google Scholar]
- 14.Nanditha A, Snehalatha C, Satheesh K, et al. Secular TRends in DiabEtes in India (STRiDE-I): Change in Prevalence in 10 Years Among Urban and Rural Populations in Tamil Nadu. Diabetes Care. 2019;42(3):476–485. doi: 10.2337/dc18-1559 [DOI] [PubMed] [Google Scholar]
- 15.Vijaya L, George R, Baskaran M, et al. Prevalence of Primary Open-angle Glaucoma in an Urban South Indian Population and Comparison with a Rural Population. Ophthalmology. 2008;115(4):648–654.e1. doi: 10.1016/j.ophtha.2007.04.062 [DOI] [PubMed] [Google Scholar]
- 16.Aravind Eye Care System: Activity Report 2017–18. Aravind Eye Care System, Chenai, India; 2011. :1–96; http://online.pubhtml5.com/idml/copn/. :1–72. [Google Scholar]
- 17.Khanna RC, Sabherwal S, Sil A, et al. Primary eye care in India - The vision center model. Indian J Ophthalmol. 2020;68(2):333–339. doi: 10.4103/ijo.IJO_118_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemporary Clinical Trials. 2007;28(2):182–191. doi: 10.1016/j.cct.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 19.Zhang W, Nicholas P, Schuman SG, et al. Screening for Diabetic Retinopathy Using a Portable, Noncontact, Nonmydriatic Handheld Retinal Camera: Journal of Diabetes Science and Technology. Published online January 1, 2017. doi: 10.1177/1932296816658902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thulasiraj RD, Nirmalan PK, Ramakrishnan R, et al. Blindness and vision impairment in a rural south Indian population: the Aravind Comprehensive Eye Survey. Ophthalmology. 2003;110(8):1491–1498. doi: 10.1016/S0161-6420(03)00565-7 [DOI] [PubMed] [Google Scholar]
- 21.Davila JR, Sengupta SS, Niziol LM, et al. Predictors of Photographic Quality with a Handheld Nonmydriatic Fundus Camera Used for Screening of Vision-Threatening Diabetic Retinopathy. Ophthalmologica. 2017;238(1–2):89–99. doi: 10.1159/000475773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jordan S, Gabe-Walters ME, Watkins A, et al. Nurse-Led Medicines’ Monitoring for Patients with Dementia in Care Homes: A Pragmatic Cohort Stepped Wedge Cluster Randomised Trial. PLOS ONE. 2015;10(10):e0140203. doi: 10.1371/journal.pone.0140203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White DB, Angus DC, Shields A-M, et al. A Randomized Trial of a Family-Support Intervention in Intensive Care Units. New England Journal of Medicine. 2018;378(25):2365–2375. doi: 10.1056/NEJMoa1802637 [DOI] [PubMed] [Google Scholar]
- 24.Ellenberg SS. The Stepped-Wedge Clinical Trial: Evaluation by Rolling Deployment. JAMA. 2018;319(6):607–608. doi: 10.1001/jama.2017.21993 [DOI] [PubMed] [Google Scholar]
- 25.Gargeya R, Leng T. Automated Identification of Diabetic Retinopathy Using Deep Learning. Ophthalmology. 2017;124(7):962–969. doi: 10.1016/j.ophtha.2017.02.008 [DOI] [PubMed] [Google Scholar]
- 26.Gulshan V, Rajan RP, Widner K, et al. Performance of a Deep-Learning Algorithm vs Manual Grading for Detecting Diabetic Retinopathy in India. JAMA Ophthalmol. 2019;137(9):987–993. doi: 10.1001/jamaophthalmol.2019.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ting DSW, Cheung CY-L, Lim G, et al. Development and Validation of a Deep Learning System for Diabetic Retinopathy and Related Eye Diseases Using Retinal Images From Multiethnic Populations With Diabetes. JAMA. 2017;318(22):2211–2223. doi: 10.1001/jama.2017.18152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu H, Li L, Wormstone IM, et al. Development and Validation of a Deep Learning System to Detect Glaucomatous Optic Neuropathy Using Fundus Photographs. JAMA Ophthalmol. Published online September 12, 2019. doi: 10.1001/jamaophthalmol.2019.3501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li Z, He Y, Keel S, Meng W, Chang RT, He M. Efficacy of a Deep Learning System for Detecting Glaucomatous Optic Neuropathy Based on Color Fundus Photographs. Ophthalmology. 2018;125(8):1199–1206. doi: 10.1016/j.ophtha.2018.01.023 [DOI] [PubMed] [Google Scholar]
- 30.Natarajan S, Jain A, Krishnan R, Rogye A, Sivaprasad S. Diagnostic Accuracy of Community-Based Diabetic Retinopathy Screening With an Offline Artificial Intelligence System on a Smartphone. JAMA Ophthalmol. Published online August 8, 2019. doi: 10.1001/jamaophthalmol.2019.2923 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Scatterplot showing the stepped-wedge study design across five vision centers (clusters) and five 2-week steps. Each plotted symbol represents a patient who received either the control standard of care (circles) or the routine fundus photography intervention (triangles).
eFigure 2. Line plot showing the proportion of patients referred to the base hospital due to fundus photography findings, by vision center and step. Proportions are plotted, A. overall, B. non-urgently, and C. urgently. Each line represents a different vision center (T, Thirukanur; K, Kurinjipadi; U, Ulunthurpet; M, Marakanam; Th, Thiruvennainalur). Note: some proportions were offset slightly for better visualization of lines.


