Abstract
The foodborne pathogen Yersinia enterocolitica causes gastrointestinal infections worldwide. In the spring of 2019, the Swedish Public Health Agency and Statens Serum Institut in Denmark independently identified an outbreak caused by Yersinia enterocolitica 4/O:3 that after sequence comparison turned out to be a cross-border outbreak. A trace-back investigation suggested shipments of fresh prewashed spinach from Italy as a common source for the outbreak. Here, we determined the genome sequences of five Y. enterocolitica clinical isolates during the Swedish outbreak using a combination of Illumina HiSeq short-read and Nanopore Technologies’ MinION long-read whole-genome sequencing. WGS results showed that all clinical strains have a fully assembled chromosome of approximately 4.6 Mbp in size and a 72-kbp virulence plasmid; one of the strains was carrying an additional 5.7-kbp plasmid, pYE-tet. All strains showed a high pathogen probability score (87.5%) with associated genes for virulence, all of which are closely related to an earlier clinical strain Y11 from Germany. In addition, we identified a chromosomally encoded multidrug-resistance cassette carrying resistance genes against chloramphenicol (catA1), streptomycin (aadA1), sulfonamides (sul1), and a mercury resistance module. This chromosomally encoded Tn2670 transposon has previously been reported associated with IncFII plasmids in Enterobacteriaceae: a Shigella flexneri clinical isolate from Japan in 1950s, a Klebsiella pneumoniae outbreak from Australia in 1997, and Salmonella enterica serovar Typhimurium. Interestingly, we identified an additional 5.7-kbp plasmid with tetB (encoding an ABC transporter), Rep, and its own ORI and ORIt sites, sharing high homology with small tetB-Rep plasmids from Pasteurellaceae. This is the first time that Tn2670 and Pasteurellaceae plasmids have been reported in Y. enterocolitica. Taken together, our study showed that the Swedish Y. enterocolitica outbreak strains acquired multi-antibiotic and metal-resistance genes through horizontal gene transfer, suggesting a potential reservoir of intraspecies dissemination of multidrug-resistance genes among foodborne pathogens. This study also highlights the concern of food-chain contamination of prewashed vegetables as a perpetual hazard against public health.
Keywords: Yersinia enterocolitica, WGS, AMR, Tn2670, tetB
Introduction
Yersinia enterocolitica is a foodborne zoonotic bacterium of global importance, able to cause severe gastrointestinal infections among people of all ages (Scallan et al., 2011; Batz et al., 2012; Bancerz-Kisiel and Szweda, 2015). Yersinia is grouped under Yersiniaceae where Yersinia pestis, Yersinia pseudotuberculosis, and Y. enterocolitica are recognized as important human pathogens (Smego et al., 1999; Adeolu et al., 2016). Y. enterocolitica is divided into six biotypes (1A/B-5) depending on physio- and biochemical properties and additionally into approximately 50 serotypes depending on antigenic variation of the lipopolysaccharides (Jagielski et al., 2002).
While yersiniosis historically has been associated with consumption of undercooked pork products or un-pasteurized milk, the growing trend of ready-to-eat (RTE) vegetables in industrialized countries has been linked to sporadic outbreaks of Y. enterocolitica (Lee et al., 2004; Sakai et al., 2005; Much et al., 2009; Macdonald et al., 2011; Rahman et al., 2011). As discussed during the amplified implementation of the Hazard Analysis and Critical Control Point (HACCP) system in the 1990s, in the raw food industry, RTE products were highlighted as products without any pathogen elimination step (Motarjemi and Käferstein, 1999). Even without pathogen elimination, HACCP remains a good resource to reduce risks in food production, but intensification and mass distribution have nonetheless permitted quick nationwide spread of introduced contaminants. International trade has correspondingly introduced longer food-supply chains and countless wholesalers, increasing the risk of breaking the cold chain with consequential growth of foodborne pathogens (Motarjemi and Käferstein, 1999; Söderqvist et al., 2017a, b). Wholesalers in the European Union are required to regularly sample RTE vegetables for Escherichia, Listeria, and Salmonella, but Yersinia remains continuously absent from routine testing (EU commission 2073/2005) and its AMR surveillance occurs only through rare ad hoc reports (Fàbrega et al., 2015).
In the spring (February–April) of 2019, the Swedish Public Health Agency (PHAS) and Statens Serum Institut (SSI) in Denmark independently identified an outbreak with the same genotypic cluster of Y. enterocolitica 4/O:3. Whole-genome sequencing (WGS) comparisons were made using the respective outbreak sequences, resulting in a cross-border outbreak being declared. The outbreak reached 57 positive cases, mainly in a younger age group (15–39) (National Veterinary Institute (SVA), 2019). A Danish case–control study recognized fresh spinach as the cause behind the outbreak, and a traceback of common producers identified an Italian supplier behind shared market batches (Espenhain et al., 2019). Following the first outbreak, a second outbreak (April–May) occurred with an additional 30 cases. Y. enterocolitica in the second outbreak was of identical bioserotype and sequence type (ST) type but clustered separately on single nucleotide polymorphism (SNP) analysis. No food-related origin could be established for the latter outbreak (National Veterinary Institute (SVA), 2019).
Whole-genome sequencing is now routinely used in outbreak investigations to identify ST types, clusters, pathogenomics, and resistance genes, but typically this high-throughput resource is limited to short-read data (Lynch et al., 2016; Nutman and Marchaim, 2019; Adzitey et al., 2020). Short-read libraries are precise and cost-efficient but do rarely provide long enough contigs for molecular epidemiological identification of moveable genetic elements and small plasmids (Koren and Phillippy, 2015). Long-read sequencing technologies can now be used in combination with short-read data to provide high-quality full-genome assemblies (Jain et al., 2016; George et al., 2017; Lemon et al., 2017). To provide insight in resistance and adaptive traits in Y. enterocolitica causing foodborne outbreaks, we combined Illumina HiSeq and Oxford Nanopore technologies’ MinION to generate and close whole genomes for five clinical strains, isolated in Sweden during the time of the two consecutive outbreaks in 2019. This is the first report of multidrug-resistant Y. enterocolitica identified from imported fresh spinach, raising concerns on food-chain contamination.
Materials and Methods
Bacterial Isolation and Identification
A total of five clinical isolates from the spring of 2019 were characterized. PHAS received isolates from the Swedish clinical microbiological laboratories for epidemiological typing, and three of these were used in the study (Espenhain et al., 2019). Y30 was derived from the spinach-related outbreak (March), Y108 was isolated from the second outbreak (April), and Y72 was collected during the outbreak periods (April) but did not cluster with any of the outbreak strains (SNP analysis, PHAS). Two additional uncharacterized isolates were collected from the Clinical Microbiology Lab at Uppsala University Hospital from the same period, Y_Mar (March) and Y_May (May). All five isolates are in this study referred to as outbreak strains. One well-characterized strain Y11 (chromosome: FR729477, plasmid: FR745874) was received from the Leibniz Institute (DSM 13030) for comparative use. The Swedish strains were delivered in transport swabs with amies medium charcoal (SARSTEDT), streaked onto Cefsulodin Irgasan Novobiocin (CIN) agar with Yersinia supplement and incubated for 24 h at 26°C. A one-μl streak of confirmed Yersinia colonies was cultivated in Trypticase Soy Broth (TSB) for 24 h in shaking incubators at 26°C. Aliquots were saved in TSB-DMSO (10%) and stored in −80°C freezers until further use. Ethical approval was not required as the investigation was performed under a mandate of PHAS in its remit to undertake outbreak investigations regarding national communicable disease control in the interest of public health.
Whole-Genome Sequencing
Stocks were cultured on Trypticase Soy Agar (TSA) and in one ml TSB at 26°C overnight. Genomic DNA was extracted from overnight cultures with the MasterPure DNA purification kit (Epicentre, Lucigen) according to the manufacturer’s instructions. Purified DNA was analyzed and quantified with 2100 NanoDrop Spectrophotometer and Qubit 2.0 (Thermo Fisher Scientific). DNA short-read libraries were prepared and sequenced using an Illumina HiSeq 2500 platform (Illumina) by Novogene. Long-read libraries were prepared using an in-house MinION sequencer by Oxford Nanopore Technologies, run for 24+ hours with base calling in the MinKNOW software on standard settings. Assembly was performed in CLC Genomics Workbench 20.0.4 (Supplementary Table 1), and all Illumina data was deposited at PRJEB42815 (ENA). Obtained MinION raw reads from one strain (Y72) were fully de novo assembled into three separate contigs representing the chromosome, the virulence plasmid, and one additional plasmid. The Nanopore sequence from Y72 was corrected using the trimmed Illumina reads for the same strain. The corrected Y72 assembly was used as a reference for mapping of trimmed Illumina reads for the remaining four strains (Supplementary Table 2).
Preparing Reference Genomes
Illumina sequences were de novo assembled, and contigs were sorted by length. The five longest contigs (280--111 kbp) along with one additional 5.7-kb plasmid and a resistance cassette in Y72 were compared with genomic data available on NCBI using BLAST. As only a small set of WGS Y. enterocolitica genomes are available, the Yersinia EnteroBase V.1.1.21 was used to identify available sequence data for Y. enterocolitica biotype 4 (Zhou et al., 2020). A total of 24 scaffold sets for different Yersinia 4/O:3 chromosomes, mainly based on a previous assortment (PRJEB2116 and PRJEB2117) (Reuter et al., 2014), were collected to increase phylogenetic resolution of the outbreak strains and comparative power of the metadata (Supplementary Table 3). Metadata included biotype, serotype, collection year, isolation country, isolation host, McNally ST, Achtman ST, wgMLST, and cgMLST + HierCC V1 (Supplementary Table 3). Based on high-score BLAST hits, an additional 17 different sequences of chromosomal and plasmid origin were collected for cassette comparisons (Supplementary Table 4) along with a set of three different alignment matches for the 5.7-kb plasmid.
Functional Annotation
Molecular characterization for the outbreak strains and Y11 (six strains) were assessed with regard to pathogenicity potential, restriction--modification systems, and known virulence factors. Antimicrobial resistance genes were characterized in outbreak strains and the generated comparison platform (24 additional strains). Pathogenicity potential was assessed using PathogenFinder 1.12 with the automatic model selection for assembled genomes (Cosentino et al., 2013). Antimicrobial resistance was assessed using ResFinder 4.13 for acquired antimicrobial resistance genes among “other” species for assembled genomes (Zankari et al., 2017; Bortolaia et al., 2020). Restriction--modification systems were identified using Restriction-ModificationFinder 1.14 for type I–IV restriction enzymes including putative genes (Roer et al., 2016). Virulence was assessed using the Virulence Factor Database VFDB5 for Y. enterocolitica (Chen et al., 2005, 2016; Yang et al., 2008; Liu et al., 2019).
Phylogenetic Analysis
The 29 strains of Y. enterocolitica biotype 4 and one strain of biotype 2 (outgroup) were selected and analyzed on EnteroBase (Zhou et al., 2020). Enterobase’s cgMLST scheme was used to retrieve all SNPs from all strains. In total, 12,800 positions were polymorphic, of which about 3,600 were polymorphic in the ingroup. The alignment of all SNPs was used to infer a maximum-likelihood tree with IQ-TREE 2.1.2 (Minh et al., 2020). An extended range of substitution models was tested, and TVMe+ASC+R3, which had the lowest log likelihood according to Bayesian Information Criterion (BIC), was selected. This model assumes different rates for transitions and transversions, but with equal base frequencies (TVMe); it includes an ascertainment bias correction (ASC), which is appropriate in the case of SNP data (Lewis, 2001); it also includes a FreeRate model of rate heterogeneity across sites, with three categories (R3). A thousand ultrafast bootstraps (UFBoot) were drawn (Hoang et al., 2018).
All sequences matching the identified cassette were aligned to the known common ancestor Shigella flexneri R100 plasmid (Womble and Rownd, 1988), using the HOXD scoring-based Whole Genome Alignment plugin in CLC on standard settings (Chiaromonte et al., 2002). Only sequence regions overlapping with the Yersinia cassette were extracted (Extract Multiple Sequence Alignment tool) which corresponded to the R-det-Tn2670 region of the R100 plasmid. As the 22 sequences shared different percentages of R-det coverage and the purpose of the comparison was to see the overall relationship among the transposon modules, a pairwise comparison (Create Average Nucleotide Identity Comparison) was generated with Alignment Percentage (AP) on standard settings. Based on the AP pairwise comparison, an AP similarity tree was constructed using Neighbor Joining (NJ), which joins clusters close to each other and far from other clusters, suitable for sequences with differential rates of evolution (Saitou and Nei, 1987). The AP NJ tree was rooted in the Shigella flexneri R100 plasmid. Both trees were later combined with collected metadata in CLC, and figure segments for Figures 2, 3 were combined in Serif’s Affinity Designer 1.9.1.979.
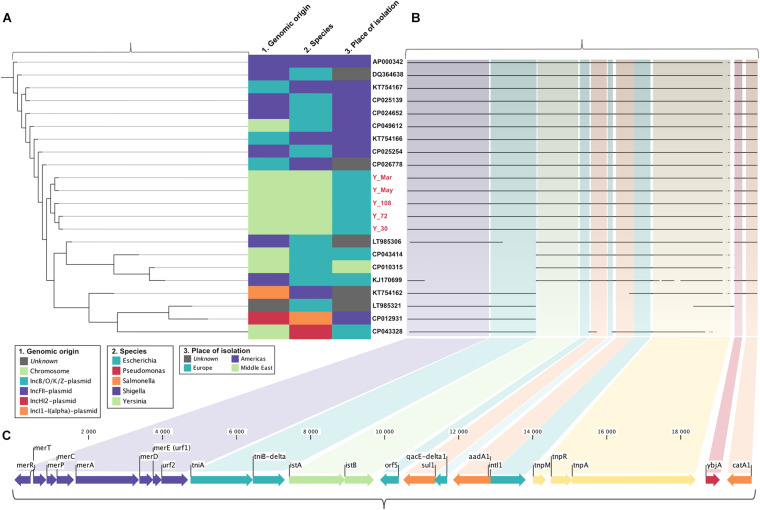
FIGURE 2.
Schematic representation of the multidrug-resistant Tn2670 transposon in clinical Y. enterocolitica and of similar mobile elements identified through BLAST. Segments were generated in CLC Genomics Workbench and combined in Affinity Designer. (A) Alignment Percentage Neighbor Joining relationship tree based on pairwise comparison of sequence alignments. (B) Sequence alignment of the Tn2670 transposon indicating missing segments. (C) The Tn2670 transposon depicted as situated in the chromosome of Y. enterocolitica Y72. Arrows indicate the orientation of the ORFs. Antibiotic resistance determinants are portrayed in orange and the mercury resistance operon in purple.
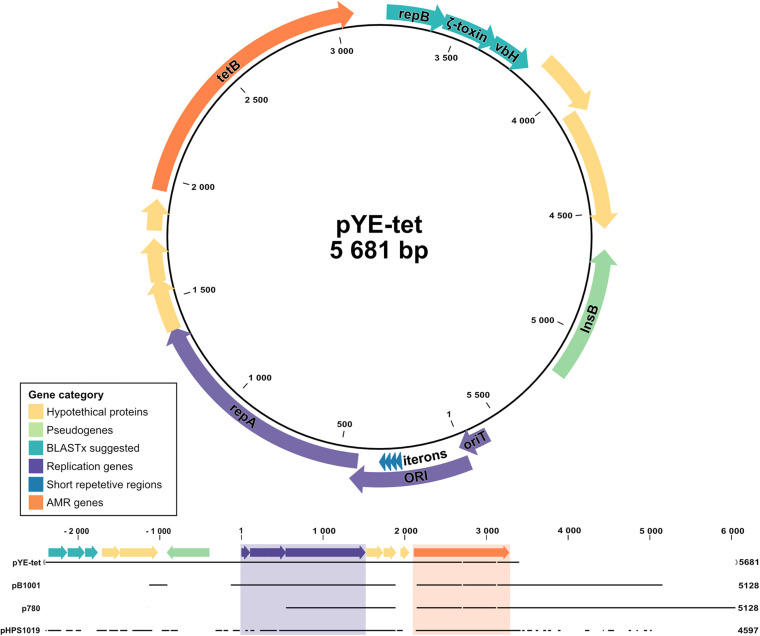
FIGURE 3.
Schematic illustration and sequence alignment of pYE-tet plasmid in Y. enterocolitica strain Y72. Colors indicate gene category with replication-related elements presented in purple, antibiotic resistance gene tetB in orange, pseudogene InsB in green, xBLAST-suggested proteins in turquoise, and hypothetical proteins in yellow. Segments were generated in CLC Genomics Workbench and combined in Affinity Designer.
Antimicrobial Susceptibility Testing
Minimum inhibitory concentration (MIC) tests were performed in biological duplicates with microdilutions in microtiter 96-well plates, where the antibiotic was added to the first well and diluted 1:2 per well in 10 consecutive wells. One column per plate was used as a positive control (no antibiotic), and one was used as a negative control (no bacteria). Bacterial concentrations of 0.5 McFarland standard units were added as 50 μl to each well. The starting concentrations were set to 2 × the clinical breakpoint (CB) for Enterobacterales (EUCAST). If no CB was available, E-tests were used as indicators for MIC and later adapted to broth microdilutions. All broth microdilutions were carried out in standardized EUCAST settings in Mueller Hinton media, incubated at 37°C for 16–20 h. Results were only accepted if controls were functional and the duplicates did not deviate more than one dilution.
Growth Rate Measurements
Growth rate was used as an indicator for bacterial fitness and measured using the Bioscreen C (Oy Growth Curves Ab Ltd.) turbidity monitoring system. The bioscreen was performed in 300 μl TSB (1:1,000 dilutions from overnight culture) in biological triplicates with technical duplicates. Experiments were run at 26°C, with continuous shaking at medium amplitude and 195 rpm for 24 h. Measurement was done using a 600-nm brown filter every 4 min and shaking stop 5 s prior to measurement. Generation time was derived from the slope of the exponential growth phase (0.02 < OD600 < 0.12) where R2 ≥ 0.98 per sample and SD ≤ 0.001 (slope) across replicates. Data were analyzed and presented using GraphPad Prism 9.
Results
Comparative Genomics
A total of five time-representative isolates were obtained from PHAS (Y30, Y72, Y108) and Uppsala University Hospital (Y_Mar, Y_May) during the time of the two outbreaks. A well-established clinical strain of the same bioserotype was used as a control (Y11).
Five strains were assembled to complete genomes, molecularly typed, and assessed together with Y11 with regard to pathogenicity and virulence. The genomes from the outbreaks had an average estimated probability score for human pathogenicity of 0.875 (chromosome) and were found matching 95–99 different families. Clinical strains carried similar known and putative Restriction-Modification systems (n = 4) as the Y11 strain, with two Type II restriction enzymes and two methyltransferases. Virulence factors were shared across the collected strains and included genes for adherence (psa, yap), invasion (ail, inv), proteases (pla), and chromosomal secretion systems. There were eight open reading frames (ORFs) for the O-antigen and 42 ORFs for the cluster I flagella (Supplementary Table 5). The Swedish outbreak strains differentiated from the Y11 strain by the presence of a chromosomal Type II Secretion System protein (yts1O) and genes for antimicrobial resistance (Table 1 and Figure 1).
TABLE 1.
Strain characterization.
| Outbreak | Biovar/serotype | Pathogenicity score (families) | Resistance genes | Chromosomal secretion systems | |
| Y11 | NA | 4/O:3 | 0.89 (96) | vat(F), blaA | T3SS (21 ORFs) |
| Y30 | First | 4/O:3 | 0.875 (98) | sul1, aadA1, catA1, vat(F), blaA | T2SS (yts1O), T3SS (21 ORFs) |
| Y72 | Unknown | 4/O:3 | 0.875 (99) | sul1, aadA1, catA1, vat(F), blaA, tetB | T2SS (yts1O), T3SS (21 ORFs) |
| Y108 | Second | 4/O:3 | 0.872 (95) | sul1, aadA1, catA1, vat(F), blaA | T2SS (yts1O), T3SS (21 ORFs) |
| Y_Mar | Firsta | 4/O:3 | 0.875 (98) | sul1, aadA1, catA1, vat(F), blaA | T2SS (yts1O), T3SS (21 ORFs) |
| Y_May | Unknown | 4/O:3 | 0.875 (98) | sul1, aadA1, catA1, vat(F), blaA | T2SS (yts1O), T3SS (21 ORFs) |
aAs identified by this study.
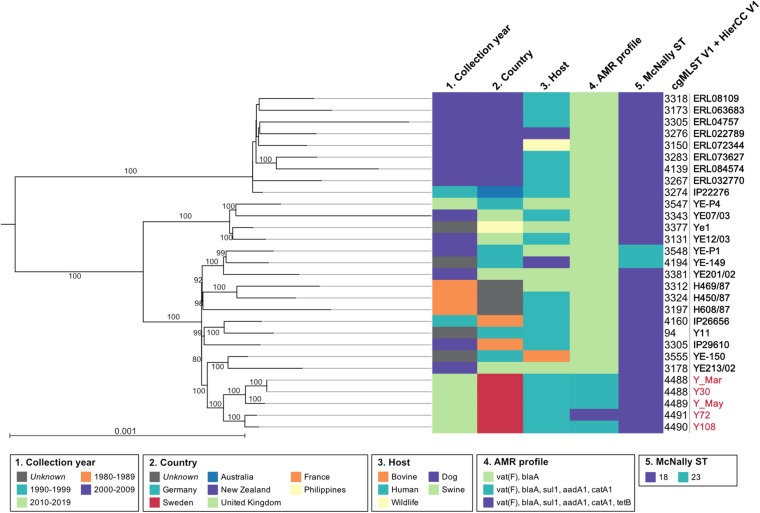
FIGURE 1.
Phylogeny of the 29 Y. enterocolitica 4/O:3. The maximum-likelihood tree is based on all polymorphic positions identified by cgMLST in 30 genomes, including and rooted in an isolate from biovar 2 used as an outgroup, and not shown in the tree. Numbers over branches are the percentage of ultrafast bootstraps supporting that branch; support values <80 are not represented. The scale represents the average number of substitutions per site. Metadata for collection year, country, host, AMR profile, McNally ST, and cgMLST V1 + HierCC V1 were presented using CLC Genomics Workbench.
Assembled genomes were phylogenetically analyzed based on maximum likelihood from all polymorphic positions identified by cgMLST in EnteroBase and rooted using an isolate from biovar 2/O:9 (IP26766, France, 2002) as an outgroup. The Swedish outbreak strains clustered together, having the closest shared node with a swine isolate from the UK (YE213/02, 2002) and a bovine isolate from Germany (YE-150, unknown collection year) (Figure 1). On a larger scale, the Swedish cluster grouped with European isolates from Germany, the UK, and France, including Y11. As inferred by McNally ST typing, the most common ST-type for 4/O:3 was ST18, but Hierarchical Clustering of cgMLST (HierCC) confirmed high similarity multilevel clustering for the Swedish outbreak strains. Results from ResFinder moreover demonstrated the global and time-independent presence of previously well-studied Y. enterocolitica vat(F) and blaA resistance genes, conferring resistance against streptogramin and β-lactam antibiotics (Pham et al., 1991; Stock et al., 1999; Seoane and García Lobo, 2000). The Swedish outbreak isolates also displayed a previously unreported multidrug resistance pattern (Figure 1).
Resistance Cassette
We report the fully sequenced genome of Y72, showing the presence of a chromosomal multidrug resistance cassette harboring determinants against quaternary ammonium compounds (qacE-delta1), heavy metal mercury (mer operon), phenicols (catA1), streptomycin (aadA1), and folate pathway antagonists (sul1) (PRJEB42815). This cassette was shown to be a known variant of the Tn2670 transposon, originally identified in the resistance segment (R-det) on a S. flexneri R100 plasmid in the 1950s (Nakaya et al., 1960). The average coverage of the transposon was approximately half of the chromosome in all strains but Y72 where it remained 100% (Supplementary Table 2). To investigate if carrying Tn2670 might come at a fitness cost, growth rates were measured to estimate generation time, but no difference could be observed when grown in TSB compared to Y11 at 26°C (Supplementary Figure 1). Tn2670 is a self-transmissible transposon flanked by direct repeats IS1a and IS1b with two overlapping open-reading frames (ORFs) that create a transposase after translational frameshifting (Hanni et al., 1982; Womble and Rownd, 1988; Escoubas et al., 1994; Partridge and Hall, 2004; Partridge, 2011). As demonstrated in Figure 2C, Tn2670 carries the identified catA1 (chloramphenicol acyltransferase) and ybjA (acyl-CoA acyltransferase) as well as the entire movable Tn21 transposon (Sun et al., 2016). Tn21 is an independent transposon lined with two indirect imperfect repeats, IRtnp (tnp genes for transposition) and IRmer (mer operon for mercury resistance) (De la Cruz and Grinsted, 1982; Liebert et al., 1999). Inside Tn21 lies the class I integron In2, bordered by the indirect imperfect repeats IRi and IRt, which on its own is not mobile due to a truncated tniB and lack of additionally required tni genes (Stokes and Hall, 1989; Brown et al., 1996). In2 can in turn be subdivided into three distinct regions: the integron as a unit, the “aadA1 cassette,” and an insertion sequence from a previous integron (IS1326). In2 can no longer transpose, but the integrase (intl1) can theoretically incorporate new genes at the attl1 site, the location for adenyl transferase (aadA1), and dihydropteroate synthase (sul1) for streptomycin and sulfonamide resistance, respectively (Collis et al., 1993, 1998). The variant of Tn2670 described here lacks IS1353, otherwise reported to locate inside IS1326 (Grinsted and Brown, 1984; Brown et al., 1996) (Figure 2C).
The Tn2670 transposon was compared with available sequences in NCBI using BLAST and analyzed using alignment percentage neighbor joining (Figures 2A,B). The transposon from Swedish strains clustered alone, but surrounded by Escherichia and Shigella carrying both plasmid-borne and chromosomally located sequence hits, mainly from plasmid types IncFII and IncB/O/K/Z. The cassette mainly matched sequences found in species of enteric bacteria, indicating interspecies spread and active dissemination of these determinants among Enterobacteriaceae.
TetB Plasmid
Along with the multidrug resistance cassette, our analysis revealed an additional plasmid carrying tetracycline resistance in strain Y72 with a coverage approximately 16 × that of the chromosome (Supplementary Table 2). The plasmid, hereafter termed pYE-tet (Figure 3), has a size of 5,681 bp and sporadically shares an approx. 5-kb segment with smaller plasmids identified in the family of Pasteurellaceae. The smaller plasmids have specifically been reported in Actinobacillus pleuropneumoniae (plasmid p780, MH457196.1), Haemophilus parasuis (plasmid pHPS1019, HQ622101.1), and Pasteurella multocida (plasmid pB1001, EU252517.1). These three plasmids were aligned with pYE-tet in Figure 3. The segment carries a suggested ORI transfer site (traJ-II), an ORI with four 21-bp iterons (4 × TTATACGACTAGAAATTTCCTG), a replication protein (repA), a tetracycline resistance gene (tetB), and five hypothetical proteins (San Millan et al., 2009; Li et al., 2018). The hypothetical protein nucleotide sequences were run through BLASTx and gave hits on another replication protein (repB) (qq: 100%, id: 100%, AXF94983.1), a vbH antitoxin (qq: 100%, id: 100%, WP_119774164.1), and a gene with partial agreement to the E. coli zeta toxin (qq: 94%, id: 36%, EFC6518787.1). An approx. 700-bp segment was identified as a pseudogene for an IS1ab InsB transposase shared with several families within the order Enterobacterales, including Morganella morganii (CP026651.1), Shigella dysenteriae (CP026778.1), Klebsiella pneumoniae (CP047701.1), S. enterica (CP049986.1), Proteus vulgaris (CP047346.1), Citrobacter freundii (CP047247.1), and Enterobacter hormaechei (LC590026.1). The tetB sequence was shared between both enteric bacteria and Pasteurellaceae.
Phenotypic Analysis of Y. enterocolitica Clinical Strains
Minimum inhibitory concentrations were assessed through broth microdilutions (Table 2). All outbreak strains were resistant to fusidic acid (>256 μg/ml), rifampicin (8 μg/ml), ampicillin (32 μg/ml), and erythromycin (64–128 μg/ml). Matching the characterized genotype was high-level resistance against chloramphenicol (>32 μg/ml), streptomycin (375–750 μg/ml), sulfamethoxazole (500 μg/ml), and tetracycline (32 μg/ml for Y72).
TABLE 2.
Minimum inhibitory concentrations (μg/ml) against routinely used antibiotics.
| FUS | RIF | AMP | CHL | STM | SMX | ERY | TET | CTX | CAZ | FOF | PIP | CIP | CST | GEN | |
| Y11 | >256 | 8 | 4 | <8 | <24 | <8 | 4 | <4 | <2 | <8 | <32 | <16 | <0.5 | <8 | <4 |
| Y30 | >256 | 8 | 32 | >32 | 375 | 500 | 64 | <4 | <2 | <8 | <32 | <16 | <0.5 | <8 | <4 |
| Y72 | >256 | 8 | 32 | >32 | 375 | 500 | 128 | 32 | <2 | <8 | <32 | <16 | <0.5 | <8 | <4 |
| Y108 | >256 | 8 | 32 | >32 | 375 | 500 | 64 | <4 | <2 | <8 | <32 | <16 | <0.5 | <8 | <4 |
| Y_Mar | >256 | 8 | 32 | >32 | 750 | 500 | 64 | <4 | <2 | <8 | <32 | <16 | <0.5 | <8 | <4 |
| Y_May | >256 | 8 | 32 | >32 | 375 | 500 | 64 | <4 | <2 | <8 | <32 | <16 | <0.5 | <8 | <4 |
FUS: fusidic acid, RIF: rifampicin, AMP: ampicillin, CHL: chloramphenicol, STM: streptomycin, SMX: sulfamethoxazole, ERY: erythromycin, TET: tetracycline, CTX: cefotaxime, CAZ: ceftazidime, FOF: fosfomycin, PIP: piperacillin, CIP: ciprofloxacin, CST: colistin, GEN: gentamicin.
Discussion
In the spring of 2019, the Swedish Public Health Agency and Statens Serum Institut in Denmark independently identified an outbreak caused by Y. enterocolitica 4/O:3. Sequence comparison and epidemiological investigation confirmed this cross-border outbreak, which was associated with imported fresh spinach. Here we determined the genome sequences, predicted virulence and pathogenicity factors, and charted the antimicrobial resistance profile of five Y. enterocolitica clinical isolates appearing during the time of the Swedish outbreaks. In comparison, we included a well-characterized clinical strain (Y11) isolated in Germany.
Of the five isolates, all expressed the virulence plasmid of Yersinia (pYV) along with genes commonly associated with infection, including the myf operon, yadA, ail, and invA (Bancerz-Kisiel et al., 2018). A predicted pathogenicity score averaged at 87.5% for chromosomally encoded genes when compared to 95–99 available families. All strains carried a Type II restriction enzyme (M.YenYEP1ORF12551P/M.YenY11ORF26101P) and a Type II methyltransferase (YenY11ORF26101P) along with a putative Type II restriction enzyme (M.SmaB3R3ORF2440P) and putative methyltransferase (Yen002ORF2900P). Our strains from 2019, but not Y11, carried a prepilin-like peptidase (aspartic hydrolase), Yts1O, from the Type II Secretion System Yts1 (occasionally termed as Yst). The Yts1 Type II Secretion cluster has previously been linked to increased pathogenicity in Y. enterocolitica, but interestingly our outbreak strains only carried yts1O, without any of the remaining operon coding units for the Yts secreton. The Yts1 and Yts2 clusters have only recently been studied, and little is known about the function and molecular mechanisms related to the operons (Iwobi et al., 2003; Shutinoski et al., 2010; von Tils et al., 2012; Rusak et al., 2017). Prepilin peptidases share high sequence homology among bacteria and are known transmembrane proteins allocated to a wide set of functions including pilus biogenesis and Type II Secretion (Schreiber and Donnenberg, 2002; Dupuy et al., 2013). The exact role of Yts1O in the Yts1 cluster, and specifically here as a single enzyme, remains a pressing question for further investigation.
All five strains showed antimicrobial resistance to chloramphenicol (>32 μg/ml), streptomycin (375–750 μg/ml), and sulfamethoxazole (500 μg/ml), and strain Y72 additionally carried clinically relevant resistance against tetracycline (32 μg/ml). All outbreak strains, but not Y11, showed resistance against ampicillin (32 μg/ml) and erythromycin (64–128 μg/ml). While there is resistance against ampicillin and erythromycin which are two of the more commonly reported AMR phenotypes in 4/O:3, tetracycline resistance is only rarely reported (Fàbrega et al., 2015; Gkouletsos et al., 2019). Resistance against chloramphenicol, streptomycin, and sulfamethoxazole correlated well with the presence of catA1, aadA1, and sul1 resistance genes situated on the chromosomally located Tn2670 transposon (Figure 2). Moreover, resistance genes other than vat(F) and blaA appear rare incidents among 4/O:3 Y. enterocolitica (Figure 1; Pham et al., 1991; Stock et al., 1999; Seoane and García Lobo, 2000). This transposon, originally derived from the S. flexneri R100 plasmid (belonging to IncFII incompatibility group), has been shown transferable between plasmids in vitro by P7 phages (Nakaya et al., 1960; Hanni et al., 1982; Partridge and Hall, 2004). The internal transposon Tn21 has been described widely spread among soil bacteria in both mercury-polluted and unpolluted sites and among clinically relevant Gram-negative bacteria, but to the best of our knowledge never before in Yersinia (Pearson et al., 1996; Liebert et al., 1999; Turner et al., 2003; Herrero et al., 2008; Partridge et al., 2018). Although both excision and loss rates are higher for composite transposons like Tn2670 compared to isolated insertion sequences, it remains intriguing that the transposon coverage is about half that of the chromosome for all strains but one (Wagner, 2006; Sun et al., 2016). The fact that this known resistance cassette has never been reported in Yersinia, while found in all five independent isolates in this study, may indicate a new trend of antimicrobial resistance genes in European foodborne Y. enterocolitica.
The tetracycline resistance observed in strain Y72 was accompanied by a small tetB plasmid, pYE-tet, sharing genes with small plasmids from Pasteurellaceae. This pattern of genes on a small tetB plasmid was first reported in multidrug-resistant P. multocida (pB1001) from diseased pigs in Spain 2002–2005 (San Millan et al., 2009), later in H. parasuis (pHPS1019) from Chinese pigs in 2010 (Liu and He, 2010), and most recently in A. pleuropneumoniae (p780) from Brazilian pigs collected between 2006 and 2011 (Pereira et al., 2016; Li et al., 2018). Except for the more diverse zoonotic P. multocida, the previous carriers of such plasmids have all been bacteria restricted to swine. All three species colonize the upper respiratory tract of pigs where they share the same environmental niche as Yersinia (Oliveira and Pijoan, 2004; Reiner et al., 2010; Wilson and Ho, 2013). The tetB gene found on pYE-tet, pB1001, pHPS1019, and p780 has previously been speculated to originate from Gram-negative enteric bacteria, strengthened by previous horizontal gene transfer events of AMR genes from enterobacteria to Pasteurellaceae plasmids (Li et al., 2018; Michael et al., 2018). Both pB1001 and p780 have been described to lack standard mobilization genes (mob), and even though non-selectively and stably replicated in Escherichia coli following electroporation, no actual conjugation has been observed (San Millan et al., 2009; Li et al., 2018). Detailed work on the p780 plasmids revealed a 22-bp iteron Rep protein-binding site in ORI; although slightly different and one nucleotide shorter, this was also identified in pYE-tet (4 × TTATACGACTAGAAATTTCCTG). Preceding the ORI is, similar to p780, an ORI transfer site with a speculated secondary sRNA traJ-II structure with a nic cleavage site, suggesting specificity to TraJ-RP4 relaxomes (Figure 3). None of the plasmids encode their own relaxomes, and RP4 was previously illustrated insufficient for conjugation of the Pasteurellaceae plasmid in E. coli, leaving the mechanistic accounts behind plasmid transfer unexplained (Li et al., 2018).
Y30, isolated from the spinach-related outbreak, shared the same cgMLST as Y_Mar, which might well be related to the same outbreak. These two strains are in turn more similar to Y_May than to the two strains Y108 and Y72, supporting the previous notion that these in fact do not share the same spinach-related origin (Figure 1; National Veterinary Institute (SVA), 2019). Y72 carries the additional pYE-tet plasmid with a strong phylogenetic tie to species naturally occurring in the upper respiratory tract of swine, suggesting that this strain might be derived from an animal source instead. This proposition remains speculative, but further investigations on the stability (losing rate) and fitness cost of pYE-tet could provide valuable insight on time since parting with the HGT niche. The Swedish isolates may be of different origins, but all carry the Tn2670 multidrug-resistant transposon, making it of even greater concern on food safety and public health. Although harboring an active large cassette (all strains) and the pYE-tet plasmid with a coverage approximately 16 × that of the chromosome (Y72), no growth rate differences could be observed as compared to Y11, which lacks all the mentioned elements. Our results suggest that these mobile elements do not come at a fitness cost at 26°C.
Neither the Tn2670 transposon nor the small tetB resistance plasmid has been reported in foodborne Yersinia or in isolates derived from RTE products. The results presented here suggest horizontal gene transfer events in environment, agriculture, or animal husbandry, permitting Y. enterocolitica to be an additional foodborne carrier of multi-antibiotic and metal-resistance determinants. Prospective studies are needed to elucidate the mechanistic conjugative properties of pYE-tet, the stability and potential mobility of the Tn2670 transposon, and the prevalence of these elements in clinical and food-related Yersinia. Our study highlights the concerns of food-chain contamination as potential reservoir for transmission and dissemination of AMR, raising concerns on food safety and public health.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Author Contributions
PK and HW: conceptualization and writing—original draft. CJ, ET, PK, and HW: data curation. PK, LG, and HW: formal analysis. HW: funding acquisition. PK, CJ, and HW: investigation. PK, RH, LG, and HW: methodology. HW: project administration. CJ, ET, LG, JJ, and HW: validation. ET, CJ, RH, LG, JJ, and HW: writing—review and editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. This work was supported by Swedish Research Council grant 2018-02376 and Swedish Society for Medical Research Stora Anslag to HW.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmicb.2021.664665/full#supplementary-material
References
- Adeolu M., Alnajar S., Naushad S., Gupta R. S. (2016). Genome-based phylogeny and taxonomy of the ‘Enterobacteriales’: Proposal for enterobacterales ord. nov. divided into the families Enterobacteriaceae, Erwiniaceae fam. nov., Pectobacteriaceae fam. nov., Yersiniaceae fam. nov., Hafniaceae fam. nov., Morganellaceae fam. nov., and Budviciaceae fam. nov. Int. J. Syst. Evol. Microbiol. 66 5575–5599. 10.1099/ijsem.0.001485 [DOI] [PubMed] [Google Scholar]
- Adzitey F., Asante J., Kumalo H. M., Khan R. B., Somboro A. M., Amoako D. G. (2020). Genomic Investigation into the Virulome, Pathogenicity, Stress Response Factors, Clonal Lineages, and Phylogenetic Relationship of Escherichia coli Strains Isolated from Meat Sources in Ghana. Genes 11:1504. 10.3390/genes11121504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bancerz-Kisiel A., Pieczywek M., Łada P., Szweda W. (2018). The most important virulence markers of yersinia enterocolitica and their role during infection. Genes 9:9050235. 10.3390/genes9050235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bancerz-Kisiel A., Szweda W. (2015). Yersiniosis - a zoonotic foodborne disease of relevance to public health. Ann. Agric. Env. Med. 22 397–402. 10.5604/12321966.1167700 [DOI] [PubMed] [Google Scholar]
- Batz M. B., Hoffmann S., Morris J. G., Jr. (2012). Ranking the disease burden of 14 pathogens in food sources in the United States using attribution data from outbreak investigations and expert elicitation. J. Food Prot. 75 1278–1291. 10.4315/0362-028x.jfp-11-418 [DOI] [PubMed] [Google Scholar]
- Bortolaia V., Kaas R. S., Ruppe E., Roberts M. C., Schwarz S., Cattoir V., et al. (2020). ResFinder 4.0 for predictions of phenotypes from genotypes. J. Antimicrob. Chemother. 75 3491–3500. 10.1093/jac/dkaa345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown H. J., Stokes H. W., Hall R. M. (1996). The integrons In0, In2, and In5 are defective transposon derivatives. J. Bacteriol. 178 4429–4437. 10.1128/jb.178.15.4429-4437.1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Yang J., Yu J., Yao Z., Sun L., Shen Y., et al. (2005). VFDB: A reference database for bacterial virulence factors. Nucleic Acids Res. 33:gki008. 10.1093/nar/gki008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Zheng D., Liu B., Yang J., Jin Q. (2016). VFDB 2016: Hierarchical and refined dataset for big data analysis - 10 years on. Nucleic Acids Res. 44 D694–D697. 10.1093/nar/gkv1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiaromonte F., Yap V. B., Miller W. (2002). Scoring pairwise genomic sequence alignments. Pac. Symp. Biocomput. 2002 115–126. 10.1142/9789812799623_0012 [DOI] [PubMed] [Google Scholar]
- Collis C. M., Grammaticopoulos G., Briton J., Stokes H. W., Hall R. M. (1993). Site-specific insertion of gene cassettes into integrons. Mol. Microbiol. 9 41–52. 10.1111/j.1365-2958.1993.tb01667.x [DOI] [PubMed] [Google Scholar]
- Collis C. M., Kim M. J., Stokes H. W., Hall R. M. (1998). Binding of the purified integron DNA integrase Intl1 to integron- and cassette-associated recombination sites. Mol. Microbiol. 29 477–490. 10.1046/j.1365-2958.1998.00936.x [DOI] [PubMed] [Google Scholar]
- Cosentino S., Voldby Larsen M., Møller Aarestrup F., Lund O. (2013). PathogenFinder - Distinguishing Friend from Foe Using Bacterial Whole Genome Sequence Data. PLoS One 8:0077302. 10.1371/journal.pone.0077302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De la Cruz F., Grinsted J. (1982). Genetic and molecular characterization of Tn21, a multiple resistance transposon from R100.1. J. Bacteriol. 151 222–228. 10.1128/jb.151.1.222-228.1982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuy B., Deghmane A. E., Taha M. K. (2013). Type IV Prepilin Peptidase in Handbook of Proteolytic Enzymes. Amsterdam: Elsevier Ltd, 261–265. 10.1016/B978-0-12-382219-2.00063-6 [DOI] [Google Scholar]
- Escoubas J. M., Lane D., Chandler M. (1994). Is the IS1 Transposase, InsAB, the Only IS1-Encoded Protein Required for Efficient Transposition? J. Bacteriol. 176 5864–5867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espenhain L., Riess M., Muller L., Colombe S., Ethelberg S., Litrup E., et al. (2019). Cross-border outbreak of Yersinia enterocolitica O3 associated with imported fresh spinach, Sweden and Denmark. Eur. Surveill. 24:1900368. 10.2807/1560-7917.es.2019.24.24.1900368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fàbrega A., Ballesté-Delpierre C., Vila J. (2015). Antimicrobial Resistance in Yersinia enterocolitica. Antimicrob. Resist. Food Safe. 2015 77–104. 10.1016/B978-0-12-801214-7.00005-3 [DOI] [Google Scholar]
- George S., Pankhurst L., Hubbard A., Votintseva A., Stoesser N., Sheppard A. E., et al. (2017). Resolving plasmid structures in enterobacteriaceae using the MinION nanopore sequencer: Assessment of MinION and MinION/illumina hybrid data assembly approaches. Microb. Genomics 3:e000118. 10.1099/mgen.0.000118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gkouletsos T., Patas K., Lambrinidis G., Neubauer H., Sprague L. D., Ioannidis A., et al. (2019). Antimicrobial resistance of Yersinia enterocolitica and presence of plasmid pYV virulence genes in human and animal isolates. N. Microb. N. Infect. 32:100604. 10.1016/j.nmni.2019.100604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinsted J., Brown N. L. (1984). A Tn 21 terminal sequence within Tn 501: complementation of tnpA gene function and transposon evolution. MGG Mol. Gen. Genet. 197 497–502. 10.1007/BF00329949 [DOI] [PubMed] [Google Scholar]
- Hanni C., Meyer J., Iida S., Arber W. (1982). Occurrence and properties of composite transposon Tn2672: Evolution of multiple drug resistance transposons. J. Bacteriol. 150 1266–1273. 10.1128/jb.150.3.1266-1273.1982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrero A., Mendoza M. C., Rodicio R., Rodicio M. R. (2008). Characterization of pUO-StVR2, a virulence-resistance plasmid evolved from the pSLT virulence plasmid of Salmonella enterica serovar Typhimurium. Antimicrob Agents Chemother 52 4514–4517. 10.1128/aac.00563-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoang D. T., Chernomor O., von Haeseler A., Minh B. Q., Vinh L. S. (2018). UFBoot2: Improving the Ultrafast Bootstrap Approximation. Mol. Biol. Evol. 35 518–522. 10.1093/molbev/msx281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwobi A., Heesemann J., Garcia E., Igwe E., Noelting C., Rakin A. (2003). Novel virulence-associated type II secretion system unique to high-pathogenicity Yersinia enterocolitica. Infect. Immun. 71 1872–1879. 10.1128/IAI.71.4.1872-1879.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagielski M., Rastawicki W., Kaluzewski S., Gierczynski R. (2002). [Yersiniosis–unappreciated infectious disease]. Przegl. Epidemiol. 56 57–64. [PubMed] [Google Scholar]
- Jain M., Olsen H. E., Paten B., Akeson M. (2016). The Oxford Nanopore MinION: delivery of nanopore sequencing to the genomics community. Genome Biol. 17:239. 10.1186/s13059-016-1103-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koren S., Phillippy A. M. (2015). One chromosome, one contig: Complete microbial genomes from long-read sequencing and assembly. Curr. Opin. Microbiol. 23 110–120. 10.1016/j.mib.2014.11.014 [DOI] [PubMed] [Google Scholar]
- Lee T. S., Lee S. W., Seok W. S., Yoo M. Y., Yoon J. W., Park B. K., et al. (2004). Prevalence, antibiotic susceptibility, and virulence factors of Yersinia enterocolitica and related species from ready-to-eat vegetables available in Korea. J Food Prot 67 1123–1127. 10.4315/0362-028x-67.6.1123 [DOI] [PubMed] [Google Scholar]
- Lemon J. K., Khil P. P., Frank K. M., Dekker J. P. (2017). Rapid nanopore sequencing of plasmids and resistance gene detection in clinical isolates. J. Clin. Microbiol. 55 3530–3543. 10.1128/JCM.01069-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis P. O. (2001). A Likelihood Approach to Estimating Phylogeny from Discrete Morphological Character Data. Syst. Biol. 50 913–925. 10.1080/106351501753462876 [DOI] [PubMed] [Google Scholar]
- Li Y., Da Silva G. C., Li Y., Rossi C. C., Crespo R. F., Williamson S. M., et al. (2018). Evidence of illegitimate recombination between two Pasteurellaceae plasmids resulting in a novel multi-resistance replicon, pM3362MDR, in Actinobacillus pleuropneumoniae. Front. Microbiol. 9:02489. 10.3389/fmicb.2018.02489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebert C. A., Hall R. M., Summers A. O. (1999). Transposon Tn21, Flagship of the Floating Genome. Microbiol. Mol. Biol. Rev. 63 507–522. 10.1128/mmbr.63.3.507-522.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B., Zheng D., Jin Q., Chen L., Yang J. (2019). VFDB 2019: A comparative pathogenomic platform with an interactive web interface. Nucleic Acids Res. 47 D687–D692. 10.1093/nar/gky1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y. Y., He Q. G. (2010). Haemophilus parasuis strain lung6591 plasmid pHPS1019 tetracycline resistance efflux pump (tetB), replication protein (rep), and hypothetical proteins genes - Nucleotide - NCBI. China: Wuhan. [Google Scholar]
- Lynch T., Petkau A., Knox N., Graham M., Van Domselaar G. (2016). Primer on infectious disease bacterial genomics. Clin. Microbiol. Rev. 29 881–913. 10.1128/CMR.00001-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdonald E., Heier B. T., Stalheim T., Cudjoe K. S., Skjerdal T., Wester A., et al. (2011). Yersinia enterocolitica o:9 infections associated with bagged salad mix in Norway. Eurosurveillance 16:19866. 10.2807/ese.16.19.19866-en [DOI] [PubMed] [Google Scholar]
- Michael G. B., Bossé J. T., Schwarz S. (2018). Antimicrobial Resistance in Pasteurellaceae of Veterinary Origin. Microbiol. Spectr. 6 331–363. 10.1128/microbiolspec.arba-0022-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minh B. Q., Schmidt H. A., Chernomor O., Schrempf D., Woodhams M. D., von Haeseler A., et al. (2020). IQ-TREE 2: New Models and Efficient Methods for Phylogenetic Inference in the Genomic Era. Mol. Biol. Evol. 37 1530–1534. 10.1093/molbev/msaa015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motarjemi Y., Käferstein F. (1999). Food safety, Hazard Analysis and Critical Control Point and the increase in foodborne diseases: A paradox? Food Control 10 325–333. 10.1016/s0956-7135(99)00008-0 [DOI] [Google Scholar]
- Much P., Pichler J., Kasper S. S., Allerberger F. (2009). Foodborne outbreaks, Austria 2007. Wien. Klin. Wochenschr. 121 77–85. 10.1007/s00508-008-1125-z [DOI] [PubMed] [Google Scholar]
- Nakaya R., Nakamura A., Murata Y. (1960). Resistance transfer agents in Shigella. Biochem. Biophys. Res. Commun. 3 654–659. 10.1016/0006-291X(60)90081-4 [DOI] [PubMed] [Google Scholar]
- National Veterinary Institute (SVA), (2019). Surveillance of infectious diseases in animals and humans in Sweden 2019. Uppsala: National Veterinary Institute, 1654–7098. [Google Scholar]
- Nutman A., Marchaim D. (2019). How to: molecular investigation of a hospital outbreak. Clin. Microbiol. Infect. 25 688–695. 10.1016/j.cmi.2018.09.017 [DOI] [PubMed] [Google Scholar]
- Oliveira S., Pijoan C. (2004). Haemophilus parasuis: New trends on diagnosis, epidemiology and control. Vet. Microbiol. 99 1–12. 10.1016/j.vetmic.2003.12.001 [DOI] [PubMed] [Google Scholar]
- Partridge S. R. (2011). Analysis of antibiotic resistance regions in Gram-negative bacteria. FEMS Microbiol. Rev. 35 820–855. 10.1111/j.1574-6976.2011.00277.x [DOI] [PubMed] [Google Scholar]
- Partridge S. R., Hall R. M. (2004). Complex multiple antibiotic and mercury resistance region derived from the r-det of NR1 (R100). Antimicrob. Agents Chemother. 48 4250–4255. 10.1128/AAC.48.11.4250-4255.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partridge S. R., Kwong S. M., Firth N., Jensen S. O. (2018). Mobile genetic elements associated with antimicrobial resistance. Clin. Microbiol. Rev. 31:17. 10.1128/CMR.00088-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson A. J., Bruce K. D., Osborn A. M., Ritchie D. A., Strike P. (1996). Distribution of class II transposase and resolvase genes in soil bacteria and their association with mer genes. Appl. Environ. Microbiol. 62 2961–2965. 10.1128/aem.62.8.2961-2965.1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira M. F., Rossi C. C., de Carvalho F. M., de Almeida L. G. P., Souza R. C., de Vasconcelos A. T. R., et al. (2016). Draft genome sequences of six Actinobacillus pleuropneumoniae serotype 8 Brazilian clinical isolates: Insight into new applications. Genome Announc. 3:14. 10.1128/genomeA.01585-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham J. N., Bell S. M., Lanzarone J. Y. M. (1991). A study of the β-lactamases of 100 clinical isolates of yersinia enterocolitica. J. Antimicrob. Chemother. 28 19–24. 10.1093/jac/28.1.19 [DOI] [PubMed] [Google Scholar]
- Rahman A., Bonny T. S., Stonsaovapak S., Ananchaipattana C. (2011). Yersinia enterocolitica: Epidemiological Studies and Outbreaks. J. Pathog. 2011:239391. 10.4061/2011/239391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiner G., Fresen C., Bronnert S., Haack I., Willems H. (2010). Prevalence of actinobacillus pleuropneumoniae infection in hunted wild boars (sus scrofa) in germany. J. Wildl. Dis. 46 551–555. 10.7589/0090-3558-46.2.551 [DOI] [PubMed] [Google Scholar]
- Reuter S., Connor T. R., Barquist L., Walker D., Feltwell T., Harris S. R., et al. (2014). Parallel independent evolution of pathogenicity within the genus Yersinia. Proc. Natl. Acad. Sci. 111 6768–6773. 10.1073/pnas.1317161111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roer L., Hendriksen R. S., Leekitcharoenphon P., Lukjancenko O., Kaas R. S., Hasman H., et al. (2016). Is the Evolution of Salmonella enterica subsp. enterica Linked to Restriction-Modification Systems? mSystems 1 9–16. 10.1128/msystems.00009-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusak L. A., Junqueira R. M., Hofer E., Vallim D. C., Asensi M. D. (2017). Next-generation sequencing virulome analysis of a Yersinia enterocolitica subsp. palearctica bioserotype 4/O:3 ST18 isolated from human blood in Brazil. Brazilian J. Infect. Dis. 21 550–553. 10.1016/j.bjid.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitou N., Nei M. (1987). The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol. Biol. Evol. 4 406–425. 10.1093/oxfordjournals.molbev.a040454 [DOI] [PubMed] [Google Scholar]
- Sakai T., Nakayama A., Hashida M., Yamamoto Y., Takebe H., Imai S. (2005). Laboratory and Epidemiology Communications Outbreak of Food Poisoning by Yersinia enterocolitica Serotype O8 in Nara Prefecture: the First Case Report in Japan. Jpn. J. Infect. Dis. 58 257–258. [PubMed] [Google Scholar]
- San Millan A., Escudero J. A., Gutierrez B., Hidalgo L., Garcia N., Llagostera M., et al. (2009). Multiresistance in Pasteurella multocida is mediated by coexistence of small plasmids. Antimicrob. Agents Chemother. 53 3399–3404. 10.1128/AAC.01522-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scallan E., Hoekstra R. M., Angulo F. J., Tauxe R. V., Widdowson M.-A., Roy S. L., et al. (2011). Foodborne illness acquired in the United States–major pathogens. Emerg. Infect. Dis. 17 7–15. 10.3201/eid1701.P11101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiber W., Donnenberg M. S. (2002). Type IV Pili in Escherichia Coli. Amsterdam: Elsevier, 307–336. 10.1016/b978-012220751-8/50012-4 [DOI] [Google Scholar]
- Seoane A., García Lobo J. M. (2000). Identification of a streptogramin a acetyltransferase gene in the chromosome of Yersinia enterocolitica. Antimicrob. Agents Chemother. 44 905–909. 10.1128/AAC.44.4.905-909.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shutinoski B., Schmidt M. A., Heusipp G. (2010). Transcriptional regulation of the Yts1 type II secretion system of Yersinia enterocolitica and identification of secretion substrates. Mol. Microbiol. 75 676–691. 10.1111/j.1365-2958.2009.06998.x [DOI] [PubMed] [Google Scholar]
- Smego R. A., Frean J., Koornhof H. J. (1999). Yersiniosis I: Microbiological and Clinicoepidemiological Aspects of Plague and Non-Plague Yersinia Infections - ProQuest. Eur. J. Clin. Microbiol. Infect. Dis. 18 1–15. 10.1007/s100960050219 [DOI] [PubMed] [Google Scholar]
- Söderqvist K., Ahmed Osman O., Wolff C., Bertilsson S., Vågsholm I., Boqvist S. (2017a). Emerging microbiota during cold storage and temperature abuse of ready-to-eat salad?. Infect. Ecol. Epidemiol. 7:1328963. 10.1080/20008686.2017.1328963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Söderqvist K., Lambertz S. T., Vågsholm I., Fernström L. L., Alsanius B., Mogren L., et al. (2017b). Fate of listeria monocytogenes, pathogenic yersinia enterocolitica, and Escherichia coli O157:H7 gfp+ in ready-to-eat salad during cold storage: What is the risk to consumers? J. Food Prot. 80 204–212. 10.4315/0362-028X.JFP-16-308 [DOI] [PubMed] [Google Scholar]
- Stock I., Heisig P., Wiedemann B. (1999). Expression of β-lactamases in Yersinia enterocolitica strains of biovars 2, 4 and 5. J. Med. Microbiol. 48 1023–1027. 10.1099/00222615-48-11-1023 [DOI] [PubMed] [Google Scholar]
- Stokes H. W., Hall R. M. (1989). A novel family of potentially mobile DNA elements encoding site−specific gene−integration functions: integrons. Mol. Microbiol. 3 1669–1683. 10.1111/j.1365-2958.1989.tb00153.x [DOI] [PubMed] [Google Scholar]
- Sun F., Zhou D., Sun Q., Luo W., Tong Y., Zhang D., et al. (2016). Genetic characterization of two fully sequenced multi-drug resistant plasmids pP10164-2 and pP10164-3 from Leclercia adecarboxylata. Sci. Rep. 6 33982. 10.1038/srep33982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner S. A., Luck S. N., Sakellaris H., Rajakumar K., Adler B. (2003). Molecular epidemiology of the SRL pathogenicity island. Antimicrob. Agents Chemother. 47 727–734. 10.1128/AAC.47.2.727-734.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Tils D., Blädel I., Schmidt M. A., Heusipp G. (2012). Type II secretion in Yersinia-a secretion system for pathogenicity and environmental fitness. Front. Cell. Infect. Microbiol. 2:160. 10.3389/fcimb.2012.00160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner A. (2006). Cooperation is Fleeting in the World of Transposable Elements. PLoS Comput. Biol. 2:e162. 10.1371/journal.pcbi.0020162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson B. A., Ho M. (2013). Pasteurella multocida: From Zoonosis to cellular microbiology. Clin. Microbiol. Rev. 26 631–655. 10.1128/CMR.00024-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Womble D. D., Rownd R. H. (1988). Genetic and physical map of plasmid NR1: Comparison with other IncFII antibiotic resistance plasmids. Microbiol. Rev. 52 433–451. 10.1128/mmbr.52.4.433-451.1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Chen L., Sun L., Yu J., Jin Q. (2008). VFDB 2008 release: An enhanced web-based resource for comparative pathogenomics. Nucleic Acids Res. 36:951. 10.1093/nar/gkm951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zankari E., Allesøe R., Joensen K. G., Cavaco L. M., Lund O., Aarestrup F. M. (2017). PointFinder: A novel web tool for WGS-based detection of antimicrobial resistance associated with chromosomal point mutations in bacterial pathogens. J. Antimicrob. Chemother. 72 2764–2768. 10.1093/jac/dkx217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z., Alikhan N. F., Mohamed K., Fan Y., Achtman M. (2020). The EnteroBase user’s guide, with case studies on Salmonella transmissions, Yersinia pestis phylogeny, and Escherichia core genomic diversity. Genome Res. 30 138–152. 10.1101/gr.251678.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.