Abstract
Background
Pediatric obesity is one of the most important health challenges of the twenty-first century. Primary prevention of childhood obesity, can lessen its consequences. This study aims to assess childhood obesity prevention policies in Iran through a policy analysis of agenda-setting using Kingdon’s multiple streams.
Methods
A qualitative study was conducted using in-depth interviews with 39 key informants and document review from different stages of the policymaking process of childhood and adolescent obesity prevention programs in Iran. The analysis of documents and interviews were guided based on Kingdon’s multiple streams (problem, policy and political streams).
Results
The important factors of the problem stream were the high prevalence of childhood and adolescent obesity and its risk factors in Iran. In the policy stream, a focus on preventing non-communicable diseases in the health system, increasing the workforce in health centers, promoting health school programs, and creating healthy eating buffets in schools was identified. Under the political stream, the impact of the WHO ECHO program in 2015 and the implementation of the health system transformation plan in Iran in the new government took place after 2013, caused the Iran ECHO program entered the agenda and implemented from 2016.
Conclusions
Now that a window of opportunity for childhood and adolescent obesity prevention policymaking has been created, the problems such as the therapeutic approach in the health system, the existence of sanctions against Iran and outbreak of coronavirus disease-19 (COVID-19), have hindered the successful implementation of this policy and the opportunity window has not been well used. However, actors need political support from the high levels of government to keep this policy on the agenda.
Keywords: Childhood obesity, Prevention, Agenda-setting, Kingdon’s multiple streams
Background
Childhood and adolescent obesity (CAO) is one of the most serious risk factors for cardiovascular and metabolic diseases [1]. The world health organization (WHO) reports over 340 million children and adolescents aged 5–19 were overweight or obese in 2016 [2] and the rate of CAO in developing countries is 30% higher than in developed countries [3]. Although inactivity and intake of high energy foods are the main causes of CAO, studies show that nutritional transition, stunting, and intake of poor micronutrient foods in developing countries can be major challenges [4, 5]. It is noteworthy that the Asian race is more vulnerable to body mass index (BMI) increase than Western races, so, a slight increase in BMI compared to normal in the Asian race can show higher complication [6]. The results of CASPIAN-V (Childhood and Adolescence Surveillance and Prevention of Adult Non-Communicable Disease) study of 14,118 subjects aged 7 to 18 years of 30 provinces in Iran, showed that the prevalence of overweight and obesity were 9.4 and 11.4% respectively [7]. Heshmat et al. also, showed that 58% of children and adolescents in the CASPIAN-V study had low physical activity and adherence of healthy nutritional behaviors in 53.6% of them was low or moderate [8]. WHO, advise governments to implement population-based strategies to combat obesity [9]. Review studies show that different CAOP policies were adopted in each society based on their structure [10], however, in 2015, WHO, in collaboration with 100 member countries, launched a program called Ending Childhood Obesity (ECHO), and persuaded member countries to implement the program to prevent and treat CAO [11]. Based on this, we decided to examine how and when the CAO prevention policies were on the agenda, before and after the ECHO program. In this regard, we used the Kingdon’s multiple streams framework.
Conceptual framework
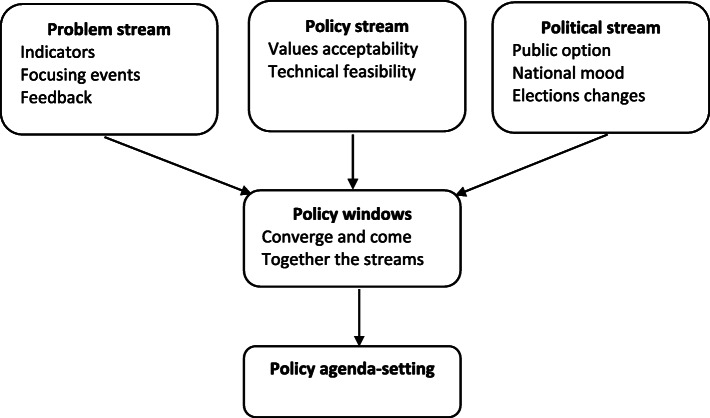
Agenda setting is part of the policy process proposed by Mirzoev [12] and Fafard [13] which is an important part of policy analysis. This approach allows researchers as well as policymakers to divide the policy-making process into specific stages, each of which has a distinct content and structural features, to better study the process. Kingdon was the first to suggest dividing policy-making into separate sets or streams [14]. The Kingdon model focuses on the role of key policy stakeholders inside and outside the government, which seizes streams to create opportunities called “policy windows”. This framework determines what were the problem streams? What were the policy streams? What was the politics stream at that time? And finally, what made the opportunity window open? The problem stream refers to policy reports, statistical indicators, and pressure from the advocacy groups which attract policymaker’s attention to that problem. The policy stream explains the solutions developed for a situation, and the political stream clarifies the political factors whether or not an issue emerges on the agenda. According to Kingdon’s model, these three streams operate separately and in independent channels, but, when all of the streams converged and come together the “window of opportunity,” will be created [14] Fig. 1.
Fig. 1.
The Kingdon’s multiple streams framework
Previous researchers have also used the Kingdon’s multiple streams framework to examine the inclusion of health policies on the agenda. Craig et al., used this framework to figure out how Arkansas’s Act 1220, school-based childhood obesity prevention policy, were put on the agenda and documented factors that produced a policy window and allowed entrepreneurs to enact comprehensive legislation [15]. Sainsbury et al. also, demonstrated that, despite significant evidence of the impact of the SSB tax on reducing the prevalence of obesity and existence of opportunities for policy reform in Australia over the past 30 years, an incomplete joining of the problem, policy and politics streams due to inadequate pressure for change from civil society, fragmented public health advocacy efforts, industry interference, and pragmatic political agendas has prevented a SSB tax policy window from opening [16].
Methods
Using Kingdon’s agenda-setting framework, this qualitative study explores the principal factors influencing the problem stream of CAO, the solutions to address CAO, and the political events affecting the emergence of childhood and adolescent obesity prevention (CAOP) policies on the agenda.
Document review and key informant interviews
This study was conducted adhering to a qualitative-descriptive research design which was part of large-scale research entitled “Future Studies and Analysis of Childhood and Adolescent Obesity Prevention Policies in Iran and Presenting Policy Options”. Accordingly, documents from the searching databases of Google Scholar, PubMed and SCOPUS as well as the websites were reviewed. Then, using a semi-structured interview and a snowball sampling method, after informing them of the objectives of the study, were interviewed until data saturation was reached.
The interviewer tried to avoid any bias or prejudice during the interview. Field notes were made during the interview and to complete the text of the interview, participants were asked to record their voices during the interview if they were satisfied. Transcripts returned to participants for comment and/or correction. The comments from the semi-structured interviews were coded by the researcher and the obtained codes were classified together according to their similarity to form themes and sub-themes. We tried to include stakeholders of different CAOP sectors in policymaking. The interviews took place between November 2019 and March 2020. Thirty-four interviews were conducted face-to-face and 5 of them by telephone, following informed consent. We used a topic guide that was designed based on Kingdon’s multiple streams theory. The topic guide was pre-tested in three interviews and based on the results from the analysis, some changes were made to the topic guide. The following questions were asked:
Problem stream: What are the unresolved issues in the field of CAOP in Iran?
Policy stream: So far, what solutions have been adopted by various organizations to address CAOP-related issues in Iran?
Political stream: What are the political factors that have an impact on CAOP prevention policies in Iran? Is there political support form the highest level of government for CAOP policymaking in Iran?
Data analysis
The conventional content analysis was used to analyze data through MAXQDA software (version, 2010). All collected materials were open-coded independently by two authors and categorized by the similarity of their content. The difficulties in coding and categorizing were discussed by the two authors (ShT and RK). After data analysis, 412 codes emerged related to the CAOP policies that after reviewing the similarities and merging of the codes, they were reduced to 125 codes and categories developed. After linking the underlying meanings of categories using inductive analysis, themes emerged
Rigor of the study
We tried to include stakeholders of different CAOP sectors of policymaking to increase the conformability of the study. Inter-observer reliability was used, and disagreements were resolved through discussion. Also, peer check was done by sharing extracted themes with other co-author (MAF). A member check was done after each interview, showing the notes and asking what was understood from interviewees. We collected and analyzed the data simultaneously.
Ethics and consent
This work was supported by Tabriz University of Medical Sciences (Grant number: 62918).
And was approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.840). Signed informed consent was obtained from the key informants at the beginning of the interview. Also, interviewees were free to withdraw from the study for any reason at any time. The present study aimed to evaluate the possibility of policy change opportunity regarding childhood and adolescent obesity prevention (CAOP) through Kingdon’s agenda-setting framework.
Results
Twenty policy documents (Table 1) were reviewed and 39 key informants, with an average age of 44.76 years old and 15.47 years of work experience, after informing them of the objectives of the study, were interviewed (Table 2). The average interviews time was about 1 h (59.6 min). The results of the review of documents as well as the interview are explained in the form of Kingdon streams.
Table 1.
List of analyzed policy documents
| No | Document | Publisher organization | Year of publication |
|---|---|---|---|
| 1 | Optimal food basket for Iranian society | MoHME | 2013 |
| 2 | WHO Ending Childhood Obesity | WHO | 2015 |
| 3 | Amendment of the executive instructions of the PHC expansion plan for the realization of UHC in urban areas for 2018 | MoHME | 2018 |
| 4 | Special nutrition education package for a health care provider in the health transformation plan in the field of health | MoHME | 2019 |
| 5 | Healthy instructions for healthy nutrition buffets in schools | MoHME | 2013 |
| 6 | assessing the micronutrient status in Iran in 2012 | MoHME | 2012 |
| 7 | Executive instructions of health-promoting schools in the Islamic Republic of Iran | MoE | 2010 |
| 8 | Executive instructions of the Health Ambassadors Program for the academic year 2017–2018 | MoE | 2018 |
| 9 | Instructions for a comprehensive program to prevent and control overweight and obesity in children and adolescents | MoHME | 2016 |
| 10 | Instructions for providing a hot meal in the rural kindergarten | Welfare Organization | 2007 |
| 11 | Executive instructions for in-school and out-of-school sports centers | MoE | 2015 |
| 12 | Guideline for caring for and managing the weight of children under 5 years of age, for health care providers in the country’s health system | MoHME | 2018 |
| 13 | Health culture promotion program document approved by the Public Culture Council of 2018 | Ministry of Culture and Islamic Guidance | 2018 |
| 14 | Fundamental Transformation Document of the Ministry of Education | MoE | 2011 |
| 15 | National Document for the Prevention and Control of Non-Communicable Diseases and Related Risk Factors in the Period 2015–2025 | MoHME | 2015 |
| 16 | A set of basic interventions for non-communicable diseases in the Iranian primary health care system “IRAPEN” | MoHME | 2017 |
| 17 | National Document on Nutrition and Food Safety 1399–1391 | MoHME | 2012 |
| 18 | Action plan for performing stretching exercises in the classroom, a solution to promote optimal physical activity in the community | MoE | 2014 |
| 19 | Care system for prevention of behaviors and risk factors for students’ health (CASPIAN Studies 1–5) | MoHME | 2003–2014 |
| 20 | Comprehensive scientific map of the country’s health | MoHME | 2010 |
MoHME Ministry of Health and Medical Education, MoE Ministry of Education, WHO World Health Organization
Table 2.
The characteristics of participations in the study
| Stakeholder’s name | Participant’s No | work experience (year) | Age (year) | Level | Sector | Related role |
|---|---|---|---|---|---|---|
| Department of education (Professor of the University of medical sciences of MoHME)a | P1 | 12 | 40 | Regional | Professional | Collaborate in developing policies to prevent childhood obesity by nutrition education in the university |
| Welfare Organization | P2 | 12 | 39 | National | Governmental | Policymaking for nutrition education to children and parents and adherence to the principles of healthy nutrition in kindergartens and childcare centers |
| Municipality | P3 | 8 | 49 | Regional | Non-Governmental | Providing sports equipment and spaces for children and adolescents |
| Ministry of Sports and Youth | P4 | 15 | 51 | Regional | Governmental | Providing appropriate facilities for exercise in childhood |
| Imam Khomeini Relief Committee | P5 | 10 | 58 | Regional | Non-Governmental | Providing healthy food items for financial trouble families as well as education healthy lifestyle in family training sessions |
| Islamic Development Organization | P6 | 15 | 41 | Regional | Governmental | Advertising of nutrition and PA in the community |
| Secretariat of the Health and Food Safety | P7 | 3 | 41 | Regional | Governmental | Establish better coordination and communication between stakeholders and organizations |
| Health care providers of MoHME | P8 | 20 | 52 | Regional | Governmental | Collaborate on primary health care, nutrition education and PA advice screening for overweight and obese children and adolescents in health centers |
| Student Organization | P9 | 2 | 40 | Regional | Non-Governmental | Collaborate on providing school buffet snakes |
| Food and Drug Office | P10 | 18 | 52 | Regional | Governmental | Increase the level of safety of food and beverages |
| School Health Department of the Province’s Health Center | P11 | 24 | 55 | Regional | Governmental | Coordinate with schools to provide nutrition and PA training and screening overweight and obese children and adolescents |
| Food and Drug Organization | P12 | 17 | 40 | National | Governmental | Policymaking to increase the level of safety of food and beverages |
| Children and Adolescents’ Intellectual Development | P13 | 20 | 49 | Regional | Governmental | Participation in healthy nutrition education for children and adolescents |
| Welfare Organization | P14 | 27 | 50 | Regional | Governmental | Collaborate on nutrition education for children and parents in kindergartens and observing the principles of healthy nutrition in kindergarten food and child care centers |
| Population and Family Health Department [1] | P15 | 9 | 53 | Regional | Governmental | Collaborate on primary health care and screening for overweight and obese children and adolescents in health centers |
| Ministry of Education | P16 | 12 | 39 | National | Governmental | Collaborate with the MoHME in develop or implement the nutrition education, school foods or PAa policies in schools |
| Department of education (Professor of the University of medical sciences of MoHME) | P17 | 6 | 59 | National | Governmental | Cooperation with the MoHME and WHO in promoting Iran ECHO, Responsible for implementing Iran ECHO pilot program in Isfahan (one of the cities in Iran) |
| The Office of Community Nutrition Improvement [1] | P18 | 10 | 48 | National | Governmental | Mainly responsible for the CAOPb: Policymaking, design and implementation of nutritional interventions |
| Islamic Republic of Iran Broadcasting (IRIB) | P19 | 12 | 45 | National | Media | Producing educational and informational programs as well as harmful food ads |
| Health Deputy of MoHME | P20 | 15 | 58 | National | Governmental | Policymaking for health service system in Iran |
| Executive manager in the Ministry of Education [1] | P21 | 25 | 52 | Regional | Governmental | Collaborate in implementation of the nutrition education, and PA policies in schools |
| The office of the Community Nutrition Improvement department of the Health Center | P22 | 15 | 40 | Regional | Governmental | Policymaking, design and implementation of nutritional interventions at the provincial level |
| School Health Department of MoHME | P23 | 30 | 50 | National | Governmental | Policymaking for nutrition education, providing healthy food, as well as training and doing PA in schools |
| Population and Family Health Department [2] | P25 | 15 | 40 | Regional | Governmental | Collaborate on primary health care and screening for overweight and obese children and adolescents in health centers |
| Non-communicable diseases Department of the Province’s Health Center | P26 | 12 | 39 | Regional | Governmental | Collaborate on the development of guidelines for non-communicable diseases prevention |
| Population and Family Health Department [3] | P27 | 23 | 45 | Regional | Governmental | Collaborate on primary health care and screening for overweight and obese children and adolescents in health centers |
| Boys’ high school physical education teacher | P28 | 16 | 42 | Regional | Governmental | Collaborate in implementation of the PA policies in schools |
| The headmaster of boys’ high school [1] | P29 | 25 | 48 | Regional | Governmental | Collaborate in implementing CAOP policies in schools |
| The headmaster of boys’ high school [2] | P30 | 28 | 47 | Regional | Governmental | Collaborate in implementing CAOP policies in schools |
| Girls’ high school physical education teacher [1] | P31 | 30 | 51 | Regional | Governmental | Collaborate in implementation of the PA policies in schools |
| Girls’ high school physical education teacher [2] | P32 | 15 | 37 | Regional | Governmental | Collaborate in implementation of the PA policies in schools |
| The headmaster of girls’ high school [1] | P33 | 27 | 48 | Regional | Governmental | Collaborate in implementing CAOP policies in schools |
| The headmaster of girls’ high school [2] | P34 | 13 | 37 | Regional | Governmental | Collaborate in implementing CAOP policies in schools |
| Executive manager in the Ministry of Education [2] | P35 | 24 | 47 | Regional | Governmental | Collaborate in implementation of the nutrition education, and PA policies in schools |
| The Office of Community Nutrition Improvement [2] | P36 | 18 | 44 | National | Governmental | Mainly responsible for the CAOP: Policymaking, design and implementation of nutritional interventions |
| Office of the Parents and Teachers Association of the Ministry of Education | P37 | 4 | 40 | Regional | Governmental | Collaborate on communication between parents and school officials |
| Executive manager in the Ministry of Education [3] | P38 | 8 | 48 | Regional | Governmental | Collaborate in implementation of the nutrition education, and PA policies in schools |
| Manager of food production and processing factory (cakes and cookies) | P39 | 5 | 43 | Regional | Private | Participation in the production of a variety of food products |
a MoHME Ministry of Health and Medical Education
b CAOP childhood and adolescent’s obesity prevention
Problem stream
High prevalence of childhood and adolescent obesity in Iran
Studies show an upward trend in the prevalence of CAO in Iran. These studies also show that obesity prevention activities in this age group have many gaps and barriers and have not been able to control this disease [17, 18]. It has been reported that the prevalence of obesity was 8% in children under 5 years in 2019 [19], 13.1% in boys and 9.8% in girls, in the age group of 5–9 years, and 9.3% in boys and 8.1% in girls in the age group of 10–19 years in 2016 [18].
High prevalence of childhood and adolescent obesity risk factors in Iran
The main causes of CAO (inactivity and high energy intake) and some of their risk factors such as knowledge and perception of weight, socioeconomic status, fast food advertising, family history of obesity, duration of exclusive breastfeeding, do not have a favorable situation in Iran [17, 20–22]. In 2016, WHO statistics related to Iran’s health profile showed that only 23% of infants under 6 months were exclusively breastfed [23], which indicates inappropriate nutrition in the first 6 months of life. One of the main reasons affecting food intake in infancy, childhood and adolescence is insufficient parental awareness of obesity and its consequences. One stakeholder states:
“Student control is not entirely in the authority of schools, therefore, our main problem and obstacle is parents who have low nutritional awareness" (p.21).
Also, one of the Welfare Organization stakeholders explains socioeconomic status as the reason for the problems in implementing CAOP policies in kindergartens” .... Even if there is a policy, due to lack of budget and economic problems in our organization, we cannot do any policy in this regard “(P.14).
Also, high access to fast food is an important problem in Iran. One of the stakeholders says in this regard: “Even if schools follow the rules because the stores near the school also sell unhealthy food, then the policies will be difficult” (p.33).
Policy stream
Attention to the prevention of CAO occurred after a national study of micronutrients in 2001 as “assessing the micronutrient status in Iran”. In that year, according to WHO criteria, 29.1% of 15–23 months’ children and 10% of 6 years old children were overweight and obese. So, the ephemeral CAOP practices emerged after that study. A review of texts, websites and the results of interviews showed that the following activities were performed as a solution to reduce obesity in children and adolescents: nutrition and physical activity (PA) education (in kindergartens, schools, health centers and in the community), improving the status of primary health care, controlling sugar and fat levels and use of food labels and lights on the produced foods, monitoring of healthy nutrition bases of school buffets, health-promoting schools plan and dynamic schools plan. The results of a study in 2012 showed that those interventions failed to control obesity among children and adolescents [24].
The interventions in this regard can be examined in two parts:
-
A.
Under 6 years old children:
Except for two studies cited in 2001 and 2012 that have checked 15–23 months’ children, no other nationwide study looked at the prevalence of obesity in children under 6 years of age, but, some strategies and interventions have been done in this regard.
The results of the present study showed that many factors are the main barriers to exclusive breastfeeding of neonates in Iran; such as the high availability of infant formula, the recommendation of pediatricians to use infant formulas, encouraging by relatives to use sugar water, cow’s milk, formula or start complementary feeding earlier.
“Parents often ask health workers to prescribe infant formula, and if our colleagues, pediatricians will easily prescribe that. If you can change the minds of pediatricians and gynecologist who do not prescribe infant formula indiscriminately, we can get good results in the long run” (P.25).
Among the solutions adopted in this section for children under 6 years of age, was the development of guidelines in education for nutrition, exclusive breastfeeding, proper complementary feeding, increase the PA for pregnant and lactating mothers and mothers with children under 6 years of age in health centers and children in the kindergartens. Due to a lack of manpower time, the implementation of nutritional education interventions faces many challenges.
"One of the stakeholders of the Welfare Organization in the policymaking level, says "Benefiting from the expertise of our organization and the participation of other agencies such as the Nutrition Improvement Office of the Ministry of Health, the target community is educated and informed about nutrition and PA (P.2).
Also, the establishment of child-friendly hospitals since 1992 in most hospitals with gynecology and obstetrics, NICU and pediatrics units, and the promotion of breastfeeding through this program, is one of the activities taken in this area.
-
B.
Children and adolescents 6–18 years:
With the beginning of the weekly iron supplementation program, for female students in middle and high school, since 2004, it was suggested that students should receive nutrition education simultaneously with supplementation programs. The result of this study showed that nutrition education was not successful in that program.
“Implementing nutrition education along with iron supplementation has many problems because there is not enough time and opportunity to do these training in schools and it takes time for classes” (P.32).
The next strategy was the increase of nutritionists staffing number in health centers since 2014, however, due to the interference of school time with the working hours of nutritionists in health centers, there are many problems in the implementation of nutritionists services for students in health centers.
one of the key informants in this regard says “... but because there is not enough opportunity for the health staff, so we have to be content with a few general recommendations and we cannot do all the training in detail based on the system.” (P.8).
Other programs included creating a dynamic schools plan in some schools to increase PA.
Political stream
The simultaneity of the first national food security survey in 2011, formation of a specialized working group on health and food safety in 2012, formation of a national document on health and food security, as well as a national document on prevention of non-communicable diseases and publication of CASPIAN- V study results in 2014, increased policymakers’ attention to CAO and government support with the launch of Iranian health care system reform plan, opened the policy windows to perform the proposed program by WHO (ECHO), with the responsibility of the Nutrition Improvement Office of the Ministry of Health. One interviewee working with MoHME explained that:
” after the health transformation plan, two important things happened that are unique: one is the use of nutrition experts and the other is that the programs were integrated with the view of preventing Noncommunicable diseases (NCD), obesity and overweight” (P.18).
Accordingly, the way was paved for political support for the actions of various stakeholders involved in the prevention of CAO. So, since 2016, with the implementation of the Iran ECHO (IRAN-Ending Childhood Obesity) program, this plan has been implemented in some provinces of Iran [25].
When deciding to adopt a solution, the prevention approach is often considered, but in the implementation phase, more attention is paid to treatment than prevention in the health system.
"In macro-level policies ... we have to move towards prevention. ... But this is something that most of our government officials do not have the right interest in and attitude towards," said one source (P.21).
Discussion
The key findings indicated that the major problems were the lack of cooperation and coordination between stakeholders, the priority of the treatment approach over prevention in the health system, economic problems and low awareness and attitude towards CAO as an obstacle to the agenda-setting of this policy or not implementing the policy optimally after it was put on the agenda.
For a health-related issue to appear on the agenda, the policymaker needs to provide a source of evidence to highlight this issue [26]. In our study, the impact of statistics on the problem of CAOP policies was also important because it was one of the important components of evidence that required action from stakeholders. A major concern in this area, is the high prevalence of CAO, despite numerous actions taken by the Ministry of Health and Medical Education (MoHME) and some other stakeholders, before and after the implementation of the Iran ECHO program [18, 19]. The studies in other countries, also, showed that despite some obesity prevention policies, the prevalence of obesity in this age group not controlled [27–29]. The switch in lifestyles from traditional to western type, which has exacerbated the problem of sedentary lifestyle and intake of high-energy, low-nutrient foods, is the second major indicator that highlights the issue of CAOP policies for policymakers [30].
The results of the studies in Iran, which are consistent with studies done in most other countries such as Vietnam and China [31, 32] showed that CAO is more prevalent in urban areas than in the rural areas and in boys higher than girls [17, 18]. In the urban areas processed and fast foods are more available, the game shops for children and adolescents are more common and spaces for play are more limited than in rural areas. So, the differences in obesity prevalence between the urban and rural areas were due to differences in community characteristics [32]. Studies demonstrated that girls and boys differ in environmental factors (hormones, ethnicity, weight gain patterns, susceptibility to social factors, and body composition) and genetic, which may lead to gender differences in the prevalence of obesity [33, 34]. Despite the high evidence of a higher prevalence of obesity in boys than girls, policies do not pay more attention to obesity in boys, and even nutrition education in schools, along with iron supplementation programs, is done only for female students, which requires revision in policymaking. The first CASPIAN study in 2003 showed that inactivity and unhealthy nutrition were prevalent among children and adolescents [35]. So that, Rahmanian et al. 7 years later, in a study showed that the policies in that period, has not improved the obesity prevalence problem, due to the nutrition transition and rapid lifestyle changes. They showed that the prevalence of obesity and overweight in children and adolescents aged 7–18 years reached from 4.5% and 8.2 in 2003 to 7.5 and 9.1% in 2010, respectively [30].
Children and adolescents, were exposed to widespread marketing of unhealthy foods in Iran [22]. Considering that more than 60% of TV commercials are related to food in Iran [36] and most of these commercials are related to unhealthy foods [37].
Other factors which affecting CAO, were the misperception of weight by children, adolescents, parents or even school officials. So that, the national study in 2014 among 14,440 children and adolescents aged 18–7 years showed that misperception of weight is very common among Iranian children and adolescents and its rate among children and adolescents was 59.1% which, 30.8% of the participants reported underestimated weight [20]. Most of the interventions and solutions adopted in Iran are in the form of nutrition education and less intervention is done to increase physical activity. As the results of the interviews with stakeholders showed that due to the high workload of teachers and insufficient manpower of the health care sector in schools, nutrition education and PA training are not fully done. Although the guidelines developed by the Ministry of Education emphasize the increase of physical activity, the results of studies showed that PA in schools is less than the recommended values [38]. A study in 2018 by Wang et al. found that implementing a policy of increasing 1 h of PA per week more than routine time, combined with 24 theory sessions for 1 year, could control the prevalence of CAO. In that study, the prevalence of obesity at the beginning of the intervention was 16.6%, which after 1 year reached 16.9% in the intervention group and 18.6% in the control group [39]. Also, nutrition education without changing the structure of society will not lead to effective results. High access of children and adolescents to unhealthy food in stores near the schools and sometimes in the schools at low prices, can be one of the important structural factors in this area in Iran. In 2017, the MoHME developed IraPEN (Package of Essential Non-Communicable (PEN) Disease Interventions for Primary Health Care in Iran) program to control NCDs [26], but unfortunately, this program does not pay much attention to children and adolescents.
In the CAOP related programs in Iran, before and after the Iran ECHO, despite considering both treatment and prevention in the formulation and development level, in the implementation level, the prevention aspect is neglected. More focus on curative care than prevention in this age group in the health care system is one of the issues to be considered in the policies adopted by the stakeholders of the health system. Doshmangir et al., also, demonstrated that the Iranian government was more focused on curative care, while, less attention was given to public health and preventive interventions [40]. Except for reducing the sugar of carbonated beverages and fats of some food products and use of food labels and lights on the produced foods, that benefit all age groups in society [41], other community-based policies, such as, increasing sports equipment in the cities, increasing community based educational programs by the media, and municipalities education centers pays more attention to adult obesity.
Our study highlights the impact of international support and national political content in shaping the agenda for CAOP policies. In 2015, WHO formed a committee to end the childhood obesity in the world (ECHO) program. The program includes strategies that should be implemented with the participation of all sectors and stakeholders to develop the policy. The implementation of the health system transformation plan in Iran in the new government took place after 2013 and more attention was paid to NCD control in this plan [40]. Therefore, the change of government in 2013 was another important political factor that caused the Iran ECHO program entered the agenda and implemented in 2016. The effects of change of government and its effect on health system policies in the Kabiri et al. study are similar to our study [26].
It was expected that by opening this window of opportunity, the policy flow would be strengthened and the solutions and practical initiatives would be used in this field, but, as the results of the current study showed, the stakeholders other than the health system didn’t show much motivation to participate in the policy. as Haghi et al. stated, CAO is described as very worrying and requires immediate action in Iran [42]. Despite the confluence of three streams at a specific point in 2016, this confluence again distances over time. Numerous factors such as the centralized health policy and the existence of a top-down approach can be effective in not achieving the goals of this policy, which was also observed in the study of Hendriks et al. [43] in top-down policies that are organized at three levels of country, province and city in Iran [44], there is not much consultation of executive stakeholders in the policymaking. When top policymakers do not engage with down executive and local stakeholders, the desired result is often not achieved and may lead to the destruction of initiatives and policies [45]. However, the centralized health system cannot be explicitly described as an inefficient approach in the health system. For example, Cuba has one of the most effective and efficient health systems in the world. Cuba is one of the countries where the health system is central. The characteristics of free public access and the integration of health services as well as the emphasis on prevention services in Cuba are among the most prominent features of Cuban health policies [46, 47].
Another noteworthy point is that economic sanctions against Iran have jeopardized food security, which, by reducing access to healthier food at a higher price, does not move the policy in line with policies adopted to prevent CAO [48]. As mentioned, the launch of the Iran ECHO program could be an important turning point in preventing CAO. Although, the beginning of the activities of this policy, coincided with the economic sanctions and with the outbreak of coronavirus disease-19 (COVID-19) in 2020 [49], it was not possible to implement the policy actively. Studies show that there are conflicts of interest among stakeholders in the health care system and that health priorities are not prioritized properly in Iran [40]. Instability in the MoHME programs as the main stakeholder of CAOP policies, ineffective use of the power of multiple stakeholders and insufficient coordination between them, has led to inadequate development and implementation of CAOP policies in Iran [50]. Although it was thought that the launch of the Iran ECHO program could be effective in CAOP, the policymakers’ attention to barriers of CAOP policies, with priority at the structural level and examining the factors involved in the agenda-setting which led the upward trend of prevalence of overweight and obesity in this age group after 5 years, requires a comprehensive review.
In our opinion, our study is the first study that seeks to identify leverage points to advance the implementation of CAOP policies in Iran, examines all its related policies and describes the barriers and facilitators of their entry into the policy window in Iran. One of the main limitations of the present study was the lack of cooperation of some stakeholders due to the COVID-19 pandemic, which is expected to be overcome in future studies by other researchers.
Conclusion
This paper provides insights into the positive and negative impact drivers behind the political process of CAOP agenda setting, which can lead to the introduction of a policy package in this issue. Now that a window of opportunity for childhood and adolescent obesity prevention policymaking has been created, the problems such as the therapeutic approach in the health system, the existence of sanctions against Iran and outbreak of coronavirus disease-19 (COVID-19), have hindered the successful implementation of this policy and the opportunity window has not been well used. However, actors need support from the high levels of government to keep this policy on the agenda. Policymakers need to know that the strengthening intra-sectoral cooperation and create advocacy for inter-sectoral cooperation is essential to implementing such policies. The existence of health indicators and the active presence of actors in this period can put pressure on policy change. However, actors need political support to put this issue on the agenda. This support can go beyond organizations such as the MoHME as well as the Ministry of Education to overcome not only political opposition but also actors who were crucial in the implementation phase. It is certain that the findings of this study alone cannot stop the increase in the prevalence of obesity in Iran, but they can be used by decision makers and policymakers in policy decisions by recognizing the facilitators of flows into the opportunity window and the obstacles that prevent better use of this opportunities.
Acknowledgements
We thank the all of stakeholder. The current work has been financially supported by a grant from Research Underseceretary of Tabriz University of Medical Sciences (Identifier: IR.TBZMED.REC.1398.840 and grant number: 62918).
Abbreviations
- BMI
Body Mass Index
- COVID-19
Coronavirus disease-19
- CAO
Childhood and adolescent obesity
- CASPIAN-V
Childhood and Adolescence Surveillance and Prevention of Adult Non-Communicable Disease
- CAOP
Childhood and adolescent obesity prevention
- ECHO
Ending Childhood Obesity
- IraPEN
Package of Essential Non-Communicable (PEN) Disease Interventions for Primary Health Care in Iran
- MoHME
Ministry of Health and Medical Education
- MoE
Ministry of Education
- NCD
Noncommunicable diseases
- WHO
World Health Organization
Authors’ contributions
ShT participated in data collection, in the statistical analysis and in the writing of the manuscript. ShT, RKh, and MAF, designed the study. ShT and RKh, wrote the first draft. All authors contributed to writing, revising, and approved the final manuscript.
Funding
This work was supported by Tabriz University of Medical Sciences (Grant number: 62918).
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
All the methods were carried out in accordance with relevant guidelines and regulations. This study was approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.840). Participants were provided information about the study and written informed consent to participation in the study.
Consent for publication
Written informed consent for publication was obtained from participants. The consent form will be available to the editor if requested.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shahnaz Taghizadeh, Email: sh.taghizadeh54@gmail.com.
Rahim Khodayari-Zarnaq, Email: Rahimzarnagh@gmail.com.
Mahdieh Abbasalizad Farhangi, Email: abbasalizad_m@yahoo.com.
References
- 1.Daniels S. Complications of obesity in children and adolescents. Int J Obes. 2009;33(1):S60–SS5. doi: 10.1038/ijo.2009.20. [DOI] [PubMed] [Google Scholar]
- 2.Kuczmarski R, Ogden C, Grummer-Strawn L, Flegal K, Guo S, Wei R, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]
- 3.Hammersley ML, Okely AD, Batterham MJ, Jones RA. An internet-based childhood obesity prevention program (Time2bHealthy) for parents of preschool-aged children: randomized controlled trial. J Med Internet Res. 2019;21(2):e11964. doi: 10.2196/11964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Payab M, Kelishadi R, Qorbani M, Motlagh ME, Ranjbar SH, Ardalan G, Zahedi H, Chinian M, Asayesh H, Larijani B, Heshmat R. Association of junk food consumption with high blood pressure and obesity in Iranian children and adolescents: the Caspian-IV study. Jornal de Pediatria (Versão em Português) 2015;91(2):196–205. doi: 10.1016/j.jpedp.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Kelishadi R, Haghdoost A-A, Sadeghirad B, Khajehkazemi R. Trend in the prevalence of obesity and overweight among Iranian children and adolescents: a systematic review and meta-analysis. Nutrition. 2014;30(4):393–400. doi: 10.1016/j.nut.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Nubé M. The Asian enigma: predisposition for low adult BMI among people of south Asian descent. Public Health Nutr. 2009;12(4):507–516. doi: 10.1017/S1368980008002826. [DOI] [PubMed] [Google Scholar]
- 7.Motlagh M, Ziaodini H, Qorbani M, Taheri M, Aminaei T, Goodarzi A, et al. Methodology and early findings of the fifth survey of childhood and adolescence surveillance and prevention of adult noncommunicable disease: The caspian-v study. Int J Prev Med. 2017;8(1):4. doi: 10.4103/2008-7802.198915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heshmat R, Hemati Z, Qorbani M, Asl LN, Motlagh ME, Ziaodini H, et al. Metabolic syndrome and associated factors in Iranian children and adolescents: the CASPIAN-V study. J Cardiovasc Thorac Res. 2018;10(4):214–220. doi: 10.15171/jcvtr.2018.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization . Population-based prevention strategies for childhood obesity: report of a WHO forum and technical meeting, Geneva, 15–17 December 2009. 2010. [Google Scholar]
- 10.Taghizadeh S, Farhangi MA. The effectiveness of pediatric obesity prevention policies: a comprehensive systematic review and dose–response meta-analysis of controlled clinical trials. J Transl Med. 2020;18(1):1–21. doi: 10.1186/s12967-020-02640-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishtar S, Gluckman P, Armstrong T. Ending childhood obesity: a time for action. Lancet. 2016;387(10021):825–827. doi: 10.1016/S0140-6736(16)00140-9. [DOI] [PubMed] [Google Scholar]
- 12.Mirzoev T. Assessment of capacity of the Ministry of Health to conduct health policy processes in the Republic of Tajikistan. Tajikistan: University of Leeds; 2010. pp. 34–39. [Google Scholar]
- 13.Fafard P. Evidence and healthy public policy: insights from health and political sciences: Canadian policy research networks Quebec (CAN) 2008. [Google Scholar]
- 14.Kingdon J. Agendas, alternatives and public policies 2nd edition chapter 8: the policy window, and joining the streams. Agendas, alternatives and public policies 2nd edition. 1995. p. 165. [Google Scholar]
- 15.Craig RL, Felix HC, Walker JF, Phillips MM. Public health professionals as policy entrepreneurs: Arkansas's childhood obesity policy experience. Am J Public Health. 2010;100(11):2047–2052. doi: 10.2105/AJPH.2009.183939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sainsbury E, Magnusson R, Thow A-M, Colagiuri S. Explaining resistance to regulatory interventions to prevent obesity and improve nutrition: a case-study of a sugar-sweetened beverages tax in Australia. Food Policy. 2020;93:101904. doi: 10.1016/j.foodpol.2020.101904. [DOI] [Google Scholar]
- 17.Motlagh ME, Ziaodini H, Qorbani M, Taheri M, Aminaei T, Goodarzi A, et al. Methodology and early findings of the fifth survey of childhood and adolescence surveillance and prevention of adult noncommunicable disease: The CASPIAN-V Study. Int J Prev Med. 2017;8:4–14. [DOI] [PMC free article] [PubMed]
- 18.Jenabi E, Khazaei S. Trends in obesity among iranian children and adolescents: 2000–2016. J Tehran Univ Heart Center. 2020;15(1):41–2. [PMC free article] [PubMed]
- 19.Khateri S, Moradi Y, Khazaei Z, Mirzaei H, Hanis SM, Aliabadi MA, et al. Prevalence of obesity and overweight in Iranian children aged less than 5 years: a systematic review and meta-analysis. Korean J Pediatr. 2019;62(6):206. doi: 10.3345/kjp.2018.07255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riahi R, Motlagh ME, Heshmat R, Qorbani M, Daniali SS, Kelishadi R. Body weight misperception and psychological distress among children and adolescents: the CASPIAN-V study. Osong Public Health Res Perspect. 2019;10(5):315–324. doi: 10.24171/j.phrp.2019.10.5.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Behzadifar M, Saki M, Behzadifar M, Mardani M, Yari F, Ebrahimzadeh F, et al. Prevalence of exclusive breastfeeding practice in the first six months of life and its determinants in Iran: a systematic review and meta-analysis. BMC Pediatr. 2019;19(1):1–10. doi: 10.1186/s12887-019-1776-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amini M, Omidvar N, Yeatman H, Shariat-Jafari S, Eslami-Amirabadi M, Zahedirad M. Content analysis of food advertising in Iranian children's television programs. Int J Prev Med. 2014;5(10):1337–1342. [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization, WHO Library Cataloguing in Publication Data. cited 10/1/2020. Available from: https://rho.emro.who.int/sites/default/files/Profiles-briefs-files/EMROPUB_EN_19265-IRN.pdf.
- 24.Siassi F, Mohammad K, Djazayery A, Djalali M, Abdollahi Z, Dorosty A, et al. National Integrated Micronutrient Survey 2012 (NIMS II) Tehran: Ministry Health Med Educ. 2015;141:108–109. [Google Scholar]
- 25.Ezzeddin N, Eini-Zinab H, Ajami M, Kalantari N, Sheikhi M. WHO ending childhood obesity and Iran-ending childhood obesity programs based on urban health equity indicators: a qualitative content analysis. Arch Iranian Med. 2019;22(11):646–652. [PubMed] [Google Scholar]
- 26.Kabiri N, Khodayari-zarnaq R, Khoshbaten M, Arab-Zozani M, Janati A. Gastrointestinal cancer prevention policies in Iran: a policy analysis of agenda-setting using Kingdon’s multiple streams. J Cancer Policy. 2021;27:100265. doi: 10.1016/j.jcpo.2020.100265. [DOI] [PubMed] [Google Scholar]
- 27.Lubans DR, Smith JJ, Plotnikoff RC, Dally KA, Okely AD, Salmon J, et al. Assessing the sustained impact of a school-based obesity prevention program for adolescent boys: The ATLAS cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2016;13(1):1. doi: 10.1186/s12966-016-0420-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lubans DR, Morgan PJ, Okely AD, Dewar D, Collins CE, Batterham M, Callister R, Plotnikoff RC. Preventing obesity among adolescent girls: one-year outcomes of the nutrition and enjoyable activity for teen girls (NEAT girls) cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2012;166(9):821–827. doi: 10.1001/archpediatrics.2012.41. [DOI] [PubMed] [Google Scholar]
- 29.Leme ACB, Baranowski T, Thompson D, Nicklas T, Philippi ST. Sustained impact of the “healthy habits, healthy girls – Brazil” school-based randomized controlled trial for adolescents living in low-income communities. Prev Med Rep. 2018;10:346–352. doi: 10.1016/j.pmedr.2018.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rahmanian M, Kelishadi R, Qorbani M, Motlagh ME, Shafiee G, Aminaee T, Ardalan G, Taslimi M, Poursafa P, Asayesh H, Larijani B, Heshmat R. Dual burden of body weight among Iranian children and adolescents in 2003 and 2010: the CASPIAN-III study. Arch Med Sci AMS. 2014;10(1):96–103. doi: 10.5114/aoms.2014.40735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhai L, Dong Y, Bai Y, Wei W, Jia L. Trends in obesity, overweight, and malnutrition among children and adolescents in Shenyang, China in 2010 and 2014: a multiple cross-sectional study. BMC Public Health. 2017;17(1):1–7. doi: 10.1186/s12889-017-4072-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Do LM, Tran TK, Eriksson B, Petzold M, Ascher H. Prevalence and incidence of overweight and obesity among Vietnamese preschool children: a longitudinal cohort study. BMC Pediatr. 2017;17(1):1–10. doi: 10.1186/s12887-017-0904-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu Z, Han S, Chu J, Xu Z, Zhu C, Guo X. Trends in overweight and obesity among children and adolescents in China from 1981 to 2010: a meta-analysis. PLoS One. 2012;7(12):e51949. doi: 10.1371/journal.pone.0051949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wisniewski AB, Chernausek SD. Gender in childhood obesity: family environment, hormones, and genes. Gender Med. 2009;6:76–85. doi: 10.1016/j.genm.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 35.Kelishadi R, Razaghi EM, Gouya MM, Ardalan G, Gheiratmand R, Delavari A, Motaghian M, Ziaee V, Siadat ZD, Majdzadeh R, Heshmat R, Barekati H, Arabi MSM, Heidarzadeh A, Shariatinejad K. Association of physical activity and the metabolic syndrome in children and adolescents: CASPIAN study. Hormone Res Paediatr. 2007;67(1):46–52. doi: 10.1159/000096121. [DOI] [PubMed] [Google Scholar]
- 36.Hajizadehoghaz M, Amini M, Abdollahi A. Iranian television advertisement and Children's food preferences. Int J Prev Med. 2016;7:128. doi: 10.4103/2008-7802.195825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Etemad K, Ebrahimi P, Azimi H, Lotfi M, Nojomi M. A content analysis of health-related advertisements in Islamic Republic of Iran broadcasting (IRIB) Med J Islam Repub Iran. 2016;30:353. [PMC free article] [PubMed] [Google Scholar]
- 38.Mortazavi S, Motlagh M, Qorbani M, Mozafarian N, Heshmat R, Kelishadi R. Association of Screen Time with sleep duration in school-aged children; a Nationwide propensity score-matched analysis: the CASPIAN-V study. J Res Health Sci. 2019;19(2):e00443. [PMC free article] [PubMed] [Google Scholar]
- 39.Wang Z, Xu F. Childhood obesity prevention through a community-based cluster randomized controlled physical activity intervention among schools in china: the health legacy project of the 2nd world summer youth olympic Games (YOG-Obesity study) Int J Obes (Lond) 2018;42(4):625–633. doi: 10.1038/ijo.2017.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doshmangir L, Moshiri E, Mostafavi H, Sakha MA, Assan A. Policy analysis of the Iranian health transformation plan in primary healthcare. BMC Health Serv Res. 2019;19(1):1–8. doi: 10.1186/s12913-019-4505-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Food and Drug Administration, Tehran.Iran . Criterion of health and hygienic properties of edible seeds and fruits, edible oils and fats (Persian) 2018. [Google Scholar]
- 42.Asar ME, Haghi M. Obesity in Iran: challenges arising and policy options. Iran J Public Health. 2019;48(11):2112. [PMC free article] [PubMed] [Google Scholar]
- 43.Hendriks AM, Habraken JM, Kremers SPJ, Jansen MWJ, Oers HV, Schuit AJ. Obstacles and enablers on the way towards integrated physical activity policies for childhood obesity prevention: an exploration of local policy Officials’ views. Biomed Res Int. 2016;2016:7–8. doi: 10.1155/2016/5739025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khodayari-Zarnaq R. Analysis of the HIV/AIDS policy-making in Iran: University of medical sciences, Iran. 2014. p. 189. [Google Scholar]
- 45.Leach M. Pathways to sustainability in the forest? Misunderstood dynamics and the negotiation of knowledge, power, and policy. Environ Plan A. 2008;40(8):1783–1795. doi: 10.1068/a40215. [DOI] [Google Scholar]
- 46.Hauge S. Primary care in Cuba. Einstein J Biol Med. 2016;23(1):37–42. doi: 10.23861/EJBM20072369. [DOI] [Google Scholar]
- 47.World Health Organization . World health statistics 2016: monitoring health for the SDGs sustainable development goals: WHO. 2016. pp. 7–111. [Google Scholar]
- 48.Hejazi J, Emamgholipour S. The effects of the re-imposition of US sanctions on food security in Iran. Int J Health Policy Manag. 2020. 10.34172/ijhpm.2020.207. [DOI] [PMC free article] [PubMed]
- 49.Buonsenso D, Piano A, Raffaelli F, Bonadia N, Donati KDG, Franceschi F. Novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24(5):2776–2780. doi: 10.26355/eurrev_202003_20549. [DOI] [PubMed] [Google Scholar]
- 50.Taghizadeh S, Zarnag RK, Farhangi MA. Stakeholder analysis of childhood obesity prevention policies in Iran. Arch Public Health. 2021;79(1):1–12. doi: 10.1186/s13690-021-00557-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.