Abstract
Introduction:
Diltiazem is a preferred agent for rate control in atrial fibrillation due to its quick onset, minimal side effects, and low cost. Due to its intermittent national shortage since February 2018, the utilization of intravenous metoprolol and verapamil has increased. This study investigated the effect of intravenous diltiazem, metoprolol, and verapamil on rate control in patients with atrial fibrillation with rapid ventricular rate.
Methods:
This study was a retrospective, single-center, cohort study conducted in patients with acute atrial fibrillation receiving intravenous diltiazem, metoprolol, or verapamil for rapid ventricular rate between 1 January 2012 and 31 August 2018. The primary outcome was the incidence of patients who achieved a rate less than 100 bpm within 1 h of treatment. Secondary outcomes included time to achieve rate control, heart rate at 30 min and 1 h after administration, bradycardia and hypotension incidence, the requirement of other rate control agent(s), inpatient admission, length of stay, and mortality.
Results:
A total of 73 patients were included in the study. At 1 h after receiving the initial rate control drug, there was no statistically significant difference between diltiazem, metoprolol, and verapamil in achieving rate control. Median time to ventricular rate control was 166 min in the diltiazem group, 297 min in the metoprolol group, and 100.5 min in the verapamil group.
Conclusion:
There was no difference in achieving rate control when using intravenous diltiazem, metoprolol, or verapamil. Any of the three rate control agents may be used for rate control. However, further studies are needed to determine which agent is superior for rate control.
Keywords: Arrhythmias, beta-adrenergic blockers, calcium-channel blockers, emergency medicine, antiarrhythmics
Introduction
Atrial fibrillation is a supraventricular tachyarrhythmia with irregularly irregular rhythm caused by structural or electrical abnormalities of the heart. Patients with atrial fibrillation are at a higher risk of being hospitalized and having multiple admissions due to inadequate control of heart rate or rhythm.1 According to the Centers for Disease Control and Prevention (CDC), approximately 6 million Americans have atrial fibrillation, with more than 454,000 hospitalizations and 158,000 deaths each year related to the disease, costing the United States more than 6 billion dollars each year.2 Atrial fibrillation is associated with an increased risk of stroke and myocardial infarction, progression of left ventricular systolic dysfunction, and increased mortality.3–5
The American Heart Association/American College of Cardiology/Heart Rhythm Society Guideline for the Management of Patients With Atrial Fibrillation recommends administration of an intravenous beta-blocker or nondihydropyridine calcium channel blocker to decrease ventricular heart rate in acute settings.1 Among the beta-blockers that may be used are metoprolol tartrate, esmolol, and propranolol. Nondihydropyridine calcium channel blockers include diltiazem and verapamil. Current literature includes various studies investigating the effects of beta-blockers and nondihydropyridine calcium channel blockers in patients with acute atrial fibrillation.6–10
A study by Phillips et al.6 investigated the efficacy and safety of intravenous diltiazem and verapamil in controlling ventricular rate in patients with atrial fibrillation, as well as the effects on left ventricular systolic function. There were no statistically significant differences in mean ventricular response after an initial bolus of both agents.
Platia et al.7 studied the efficacy and safety of esmolol and verapamil in patients with atrial fibrillation or flutter with a rapid ventricular rate of at least 120 bpm. The authors found that heart rate decreased by 28% in the esmolol group compared to 30% in the verapamil group. Fifty percent of esmolol patients and 12% of verapamil patients converted to normal sinus rhythm. Results also showed conversion to normal sinus rhythm after 29 min in patients who received esmolol versus 24–26 min in patients who received verapamil.
Numerous studies have compared intravenous diltiazem and metoprolol for rate reduction in acute atrial fibrillation.8–10 In 2005, Demircan et al. concluded that there was a significantly higher decrease in the ventricular rate at 2 min in the diltiazem group compared to the metoprolol group. In 2015, Fromm et al. compared the effectiveness of diltiazem and metoprolol for rate control in atrial fibrillation or flutter in the emergency department (ED).10 Fromm et al. concluded that the mean decrease in heart rate for diltiazem was more rapid and substantial than in the metoprolol group. Hirschy et al.10 found no difference between diltiazem and metoprolol in achieving successful ventricular rate control.
Although diltiazem and metoprolol have been compared for rate control in patients with acute atrial fibrillation, results have been variable. Furthermore, current literature includes very few studies looking at the effectiveness of verapamil in achieving rate control in patients with acute atrial fibrillation.6,7 Intravenous diltiazem has been intermittently on the United States Food and Drug Administration (FDA) National Drug Shortage list since 21 February 2018, resulting in providers at our institution prescribing either intravenous metoprolol or verapamil in place of diltiazem for rate control in patients with atrial fibrillation with rapid ventricular rate. This study investigated the effectiveness between intravenous diltiazem, verapamil, and metoprolol in achieving ventricular rate control in atrial fibrillation with a rapid ventricular response.
Methods
Study design
A retrospective, single-center, cohort study was conducted in patients who received intravenous diltiazem, metoprolol, or verapamil for rate control in atrial fibrillation with the rapid ventricular response. The Investigational Review Board granted approval before the data collection of this study.
This study was conducted at a 500-bed community hospital with a Level III Trauma Center in West Texas. Eligible patients were 18 years and older, had a diagnosis of acute atrial fibrillation (symptom onset within less than 48 h) with rapid ventricular rate (defined as heart rate > 100 bpm) coming through the ED, and received one of the studied rate control agents as the initial rate control drug (intravenous diltiazem, metoprolol, or verapamil) between 1 January 2012 and 31 August 2018. Patients were excluded if they were 90 years and older, were prisoners, were pregnant, or had incomplete medical records.
Patients with atrial fibrillation with rapid ventricular rate were identified by International Classification of Diseases (ICD) 10 diagnosis codes, “I48.0: Paroxysmal atrial fibrillation,” “I48.1: Persistant atrial fibrillation,” “I48.2: Chronic atrial fibrillation,” “I48.9: Unspecific atrial fibrillation and atrial flutter,” “I48.91: Unspecific atrial fibrillation,” and “I48.92: Unspecified atrial flutter.” Patients were assigned to either the control group (diltiazem) or intervention group one (metoprolol) or intervention group two (verapamil) based on the initial rate control agent.
The primary outcome was incidence of patients who achieved ventricular rate less than 100 bpm within 1 h of treatment. Secondary outcomes included time to achieve ventricular rate less than 100 bpm, heart rate at 30 min and 1 h after administration, bradycardia and hypotension after administration, requirement of other rate control agent(s), inpatient admission, length of stay, and mortality.
Statistical analyses
Descriptive statistics for baseline characteristics and study outcomes were conducted and summarized as mean (standard deviation), median (interquartile range), and frequency (percentage) in Tables 1 and 2, respectively. Chi-square tests were conducted to determine the statistically significant associations between the categorical variables and rate control agents (diltiazem, metoprolol, and verapamil). For normally distributed continuous outcomes, one-way analysis of variance (ANOVA) test was conducted to determine if the differences were statistically significant between the groups with different rate control agents. For nonnormally distributed continuous outcomes, a nonparametric alternative, Kruskal–Wallis tests were conducted to determine if there were statistically significant differences between groups that differed in rate control agents. The p value < 0.05 was set as statistically significant. All the analyses were conducted using IBM SPSS software, version 25.
Table 1.
Baseline characteristics.
| Total (N = 78) | Diltiazem (n = 51) | Metoprolol (n = 15) | Verapamil (n = 12) | p value | |
|---|---|---|---|---|---|
| Age, yearsa | 71.0 ± 26.0 | 71.0 ± 12.1 | 76.0 ± 16.1 | 70.5 ± 10.3 | 0.331 |
| Male sex, no (%) | 35 (44.9%) | 22 (43.2%) | 8 (53.3%) | 5 (41.7%) | 0.752 |
| Weight, kga | 87.0 ± 23.0 | 84.0 ± 20.3 | 86.0 ± 21.2 | 106.5 ± 28.4 | 0.033 |
| Height, cma | 170.0 ± 10.7 | 168.0 ± 11.5 | 173.0 ± 8.3 | 170.0 ± 9.7 | 0.381 |
| Heart rate, bpma | 139.0 ± 18.3 | 138.0 ± 19.0 | 132.0 ± 13.1 | 146.0 ± 18.4 | 0.112 |
| Systolic blood pressure, mmHga | 132.0 ± 23.6 | 134.0 ± 22.2 | 118.0 ± 25.4 | 151.5 ± 23.6 | 0.020 |
| Diastolic blood pressure, mmHga | 87.0 ± 19.7 | 88.0 ± 18.8 | 74.0 ± 13.9 | 97.0 ± 23.0 | 0.015 |
| Alcohol use, no (%) | 12 (15.4%) | 7 (13.7%) | 2 (12.2%) | 3 (25.0%) | 0.604 |
| Tobacco use, no (%) | 19 (24.4%) | 11 (21.6%) | 4 (26.7%) | 4 (33.3%) | 0.676 |
| Illicit drug use, no (%) | 1 (1.3%) | 1 (2.0%) | 0 (0.0%) | 0 (0.0%) | 0.765 |
| Heart valve replacement, no (%) | 2 (2.6%) | 1 (2.0%) | 0 (0.0%) | 1 (8.3%) | 0.356 |
| Pacemaker, no (%) | 15 (19.2%) | 13 (25.5%) | 1 (6.7%) | 1 (8.3%) | 0.155 |
| Beta blocker, no (%) | 40 (51.3%) | 21 (41.2%) | 11 (73.3%) | 8 (66.7%) | 0.917 |
| Nondihydropyridine calcium channel blocker, no (%) | 10 (7.8%) | 7 (13.7%) | 2 (13.3%) | 1 (8.3%) | 0.084 |
| Digoxin, no (%) | 3 (3.8%) | 3 (5.9%) | 0 (0.0%) | 0 (0.0%) | 0.055 |
| Age-adjusted Charlson comorbidity index score, no. Median (IQR) | 5 (3.3-7.0) | 5 (4.0-7.0) | 6 (4.5-6.4) | 4 (2.8-6.3) | 0.801 |
| ED no (%) | 73 (93.6%) | 48 (94.1%) | 13 (86.7%) | 12 (100.0%) | 0.360 |
| Inpatient, no (%) | 5 (6.4%) | 3 (5.9%) | 2 (13.3%) | 0 (0.0%) | 0.360 |
| Received rate control agent from EMS, no (%) | 5 (6.4%) | 3 (5.9%) | 1 (6.7%) | 1 (8.3%) | 0.952 |
| First dose, mga | – | 15.0 ± 6.5 | 5.0 ± 0.9 | 7.5 ± 2.6 | – |
| Second dose, mga | – | 0.0 ± 8.0 | 0.0 ± 2.4 | 0.0 ± 3.3 | – |
| Third dose, mga | – | 0.0 ± 0.8 | 0.0 ± 1.8 | 0.0 + 0.0 | – |
| Total dose from continuous infusion, mga | – | 1.0 ± 31.0 | n/a | 0.0 + 25 | – |
| Total dose, mga | – | 22.5 ± 33.8 | 5.0 ± 4.0 | 10.0 ± 25.9 | – |
ED: emergency department; EMS: emergency medical services; IQR: interquartile range.
Mean ± standard deviation.
Table 2.
Study outcomes.
| Total (N = 78) | Diltiazem (n = 51) | Metoprolol (n = 15) | Verapamil (n = 12) | p value | |
|---|---|---|---|---|---|
| Primary outcome | |||||
| Achieved ventricular rate less than 100 bpm within 1 h of treatment, no (%) | 24 (30.8%) | 16 (31.4%) | 3 (20.0%) | 5 (41.7%) | 0.474 |
| Secondary outcomes | |||||
| Time to achieve ventricular rate less than 100 bpm, min (median (IQR)) | 153.5 (55.0–326.3) | 166.0 (41.5–305.0) | 297.0 (72.5–387.5) | 100.5 (32.0–154.5) | 0.190 |
| Heart rate at 30 min after administration of rate control agent, bpma | 115.0 ± 22.8 | 117.0 ± 25.8 | 124.5 ± 14.7 | 0.196 | |
| Heart rate at 1 h after administration of rate control agent, bpma | 109.5 ± 22.0 | 112.5 ± 22.9 | 115.0 ± 22.7 | 104.0 ± 15.3 | 0.267 |
| Incidence of bradycardia after administration of rate control agent, no (%) | 2 (2.6%) | 1 (2.0%) | 0 (0.0%) | 1 (8.3%) | 0.356 |
| Incidence of hypotension after administration of rate control agent, no (%) | 11 (14.1%) | 7 (13.7%) | 3 (20.0%) | 1 (8.3%) | 0.682 |
| Required rate control agent other than initial rate control agent used, no (%) | 18 (23.1%) | 10 (19.6%) | 8 (53.3%) | 0 (0.0%) | 0.003 |
| Required inpatient admission, no (%) | 78 (100.0%) | 51 (100.0%) | 15 (100.0%) | 12 (100.0%) | — |
| Telemetry admission, no (%) | 72 (92.3%) | 50 (98.0%) | 10 (66.7%) | 12 (100.0%) | <0.001 |
| ICU admission, no (%) | 11 (14.1%) | 4 (7.8%) | 6 (40.0%) | 1 (8.3%) | 0.006 |
| Duration of hospital stay, daysa | 4.5 ± 4.9 | 4.0 ± 4.8 | 9.0 ± 5.1 | 3.0 ± 4.2 | 0.035 |
| ICU mortality, no (%) | 1 (1.28%) | 1 (2.0%) | 0 (0.0%) | 0 (0.0%) | 0.765 |
| Hospital mortality, no (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | – |
IQR: interquartile range; ICU: intensive care unit.
Mean ± standard deviation.
Results
Baseline characteristics
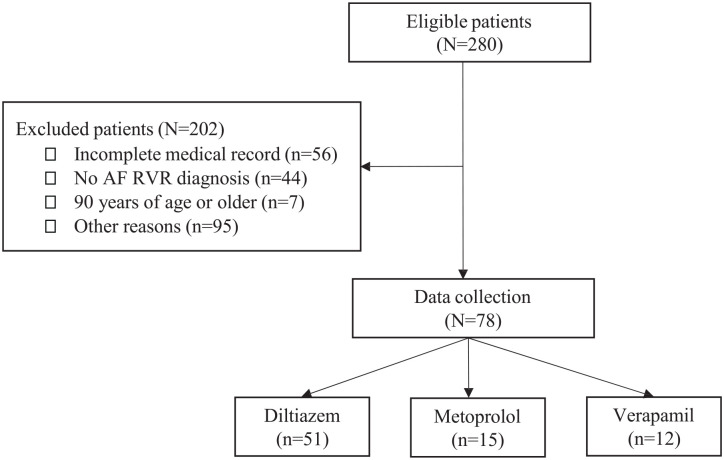
A total of 73 patients were included in the study, out of the 280 patients evaluated (Figure 1). Baseline characteristics are shown in Table 1. The baseline characteristics between the diltiazem (n = 51), metoprolol (n = 15), and verapamil (n = 12) groups were similar, although patients in the verapamil group weighed more (84 vs. 86 vs. 106.5 kg, p = 0.033) and had a higher systolic (134 vs. 118 vs. 152 mmHg, p = 0.02) and diastolic blood pressure (88 vs. 74 vs. 97 mmHg, p = 0.015). The mean total doses of diltiazem, metoprolol, and verapamil required for achieving rate control were 22.5, 5, and 10 mg, respectively.
Figure 1.
Patient enrollment.
AF: atrial fibrillation; RVR: rapid ventricular rate.
Study outcomes
At 1 h after receiving the initial rate control drug, there was no statistical difference between diltiazem, metoprolol, and verapamil in achieving ventricular rate less than 100 bpm (15.7% vs. 5% vs. 3.7%, p = 0.474).
There was no significant difference in median time to ventricular rate control was 166 min in the diltiazem group, 297 min in the metoprolol group, and 100.5 min in the verapamil group (p = 0.190). The mean heart rates at 30 min (117 vs. 125 vs. 105 bpm, respectively, p = 0.196) and at 1 h (113 vs. 115 vs. 104 bpm, respectively, p = 0.267) were similar between groups. Incidence of bradycardia (2.0% vs. 0.0% vs. 8.3%, respectively, p = 0.356) and hypotension (13.7% vs. 20.0% vs. 8.3%, respectively, p = 0.682) were similar between groups. Patients who received metoprolol required additional rate control agents (53.5%) when compared to diltiazem (19.6%) and verapamil (0.0%) (p = 0.003). All patients included in the study required inpatient admission, with more patients who received metoprolol being admitted to the intensive care unit (ICU) (p < 0.006) and consequently having a longer duration of hospital stay (p = 0.035). Only one patient died during admission. This patient who was admitted to the ICU had multiple comorbidities and complications. All study outcomes are available in Table 2.
Discussion
The variability and a lack of conclusive studies comparing multiple rate control agents against each other have led to providers administering intravenous diltiazem as the initial rate control agent in atrial fibrillation with rapid ventricular rate. Furthermore, there is an uncertainty of reliability of other rate control agents in achieving successful rate control, which has ultimately led to the common practice of prescribing intravenous diltiazem.
Our study, which aimed at investigating the difference between intravenous diltiazem, metoprolol, and verapamil, found that there was no statistically significant difference between the three rate control agents for successful rate control after 1 h of administration. Although not statistically significant, there was a trend toward better outcomes with diltiazem and verapamil in achieving rate control. When compared to diltiazem and verapamil, patients who received metoprolol experienced more hypotension, had a higher requirement for an additional rate control agent, and had a longer time to achieve rate control. These results are similar to results from several previous studies.8,9,11 Demircan et al.8 concluded that diltiazem had a significantly larger decrease in ventricular rate. Fromm et al.9 and Feeney et al.11 found a higher success rate with diltiazem compared to metoprolol. Hines et al.12 found no difference in heart rate control between diltiazem and metoprolol after 1 and 2 h. Ulimoen et al.13 concluded that diltiazem and verapamil were equally effective in reducing heart rate, similar to our results. Although our investigation shared similar results, all of these studies excluded many comorbidities including heart failure, unstable angina, myocardial infarction, hyperthyroidism, asthma, chronic pulmonary obstructive disorder, diabetes, and peripheral vascular disease. Our study included all comorbidities for better applicability to the general population.
There were also a few studies differing from our study that favored a beta-blocker for rate control. Hirschy et al.10 included patients with heart failure and found higher success rates with rate control within 30 min of administration of metoprolol when compared to diltiazem. Vinson et al.14 found higher success rates in reducing ventricular rate with beta-blockers compared to calcium channel blockers. Moskowitz et al.15 investigated rate control agents in the ICU and found that metoprolol was superior to diltiazem in achieving rate control at 4 h and diltiazem had a higher in-hospital mortality rate. Although these results differ from our study, they suggest that patients in the ICU and patients with heart failure who are in atrial fibrillation with rapid ventricular rate may benefit from receiving a beta-blocker for rate control. Our study included all comorbidities but did not investigate heart failure independently. In addition, our study did not specifically look at ICU patients requiring rate control agents. Further studies need to be performed to investigate rate control in heart failure and rate control in the ICU. To our knowledge, this is the first study comparing these three rate control agents against each other. Our study is also one of the few that does not exclude various comorbidities and uses the Charlson age comorbidity index score (CACI) score. Although this makes our results more relatable to the general population, we cannot make specific conclusions about a rate control agent for individual comorbidities, such as heart failure.
Since our study is a retrospective chart review, it has some limitations. The metoprolol group has only 15 patients, and the verapamil group has 12 patients. A difference of 66% between the time needed to achieve rate control in verapamil versus diltiazem and roughly 180% difference for the metoprolol was not different. This result is more likely due to the small sample size. This study was not powered to answer this question and type II error cannot be ruled out. Physicians may have had preference of a specific rate control agent over another. Most physicians favored diltiazem as the first-choice agent despite the diltiazem shortage, leading to a lack of patients in the metoprolol and verapamil groups and a small sample size. Documentation in the ED may not be accurate due to the retrospective nature of charting. Many charts were excluded from the study due to inconsistent charting on heart rate. Administration and timing of rate control agents may not have been charted if administered by first responders which could be a confounding factor in the primary outcome of this study. Also, our study included 41 patients who received a beta-blocker at home. Among them, only 27.5% of patients received a beta-blocker as a rate control with Atrial fibrillation. This could be a confounder.
Conclusion
Based on the results of our study, there is no difference in achieving rate control when using intravenous diltiazem, metoprolol, or verapamil. Therefore, any of the three rate control agents may be considered for rate control in atrial fibrillation with rapid ventricular rate. Although not significant, our study revealed slightly better outcomes with nondihydropyridine calcium channel blockers compared to a beta-blocker for rate control. Further and larger studies are needed to investigate the comparative effectiveness of beta-blockers and nondihydropyridine calcium channel blockers for rate control in atrial fibrillation with rapid ventricular rate.
Acknowledgments
The authors wish to acknowledge the contribution of the Texas Tech University Health Sciences Center Clinical Research Institute for their assistance with this research. This work was presented earlier as a poster presentation—Medeiros T, et al. Rate control with Intravenous Diltiazem, Verapamil, and Metoprolol in Atrial Fibrillation with Rapid Ventricular Rate. Poster presentation at 2018 American Society of Health-System Pharmacists Midyear Clinical Meeting, Anaheim, CA, December 2018—and platform presentation: Rate control with Intravenous Diltiazem, Verapamil, and Metoprolol in Atrial Fibrillation with Rapid Ventricular Rate. Texas State Hospital Pharmacists ALCALDE XXXVIII, Frisco, TX, April 2019.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Texas Tech University Health Sciences Center Institutional Review Board (#A19-4056).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was waived by Texas Tech University Health Sciences Center IRB: The Texas Tech University Health Sciences Center IRB review finds this project meets the following criteria and in accordance with 45 CFR 45.116 (d) waives the requirement for documentation of consent. The research involves no more than minimal risk to the subjects. The waiver will not adversely affect the rights and welfare of the subjects. The research could not practicably be carried out without the waiver. When appropriate, the subjects will be provided with pertinent information after participation.
ORCID iD: Young R Lee  https://orcid.org/0000-0002-7677-2125
https://orcid.org/0000-0002-7677-2125
Trial registration: This study was not registered because this study was conducted based on the retrospective chart review.
References
- 1. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. J Am Coll Cardiol 2014; 64(21): 2246–2280. [DOI] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. Atrial fibrillation fact sheet, https://www.cdc.gov/heartdisease/atrial_fibrillation.htm (accessed 18 May 2021).
- 3. Walkey AJ, Greiner MA, Heckbert SR, et al. Atrial fibrillation among Medicare beneficiaries hospitalized with sepsis: incidence and risk factors. Am Heart J 2013; 165(6): 949–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dries DL, Exner DV, Gersh BJ, et al. Atrial fibrillation is associated with an increased risk for mortality and heart failure progression in patients with asymptomatic and symptomatic left ventricular systolic dysfunction: a retrospective analysis of the SOLVD trials. J Am Coll Cardiol 1998; 32(3): 695–703. [DOI] [PubMed] [Google Scholar]
- 5. Soliman EZ, Safford MM, Muntner P, et al. Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med 2014; 174(1): 107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Phillips BG, Gandhi AJ, Sanoski CA, et al. Comparison of intravenous diltiazem and verapamil for the acute treatment of atrial fibrillation and atrial flutter. Pharmacotherapy 1997; 17(6): 1238–1245. [PubMed] [Google Scholar]
- 7. Platia EV, Michelson EL, Porterfield JK, et al. Esmolol versus verapamil in the acute treatment of atrial fibrillation or atrial flutter. Am J Cardiol 1989; 63: 925–929. [DOI] [PubMed] [Google Scholar]
- 8. Demircan C, Cikriklar H, Engindeniz Z, et al. Comparison of the effectiveness of intravenous diltiazem and metoprolol in the management of rapid ventricular rate in atrial fibrillation. Emerg Med J 2005; 22(6): 411–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fromm C, Suau SJ, Cohen V, et al. Diltiazem vs. metoprolol in the management of atrial fibrillation or flutter with rapid ventricular rate in the emergency department. J Emerg Med 2015; 49(2): 175–182. [DOI] [PubMed] [Google Scholar]
- 10. Hirschy R, Ackerbauer KA, Peksa GD, et al. Metoprolol vs. diltiazem in the acute management of atrial fibrillation in patients with heart failure with reduced ejection fraction. Am J Emerg Med 2018; 37(1): 80–84. [DOI] [PubMed] [Google Scholar]
- 11. Feeney ME, Rowe SLB, Mah ND, et al. Achieving ventricular rate control in patients taking chronic beta-blocker therapy. Am J Emerg Med 2018; 36(1): 110–113. [DOI] [PubMed] [Google Scholar]
- 12. Hines MC, Reed BN, Ivaturi V, et al. Diltiazem versus metoprolol for rate control in atrial fibrillation with rapid ventricular response in the emergency department. Am J Health Syst Pharm 2016; 73(24): 2068–2076. [DOI] [PubMed] [Google Scholar]
- 13. Ulimoen SR, Enger S, Carlson J, et al. Comparison of four single-drug regimens on ventricular rate and arrhythmia-related symptoms in patients with permanent atrial fibrillation. Am J Cardiol 2013; 111: 225–230. [DOI] [PubMed] [Google Scholar]
- 14. Vinson DR, Hoehn T, Graber DJ, et al. Managing emergency department with recent-onset atrial fibrillation. J Emerg Med 2012; 42(2): 139–148. [DOI] [PubMed] [Google Scholar]
- 15. Moskowitz A, Chen KP, Cooper AZ, et al. Management of atrial fibrillation with rapid ventricular response in the intensive care unit: a secondary analysis of electronic health record data. Shock 2017; 48(4): 436–440. [DOI] [PMC free article] [PubMed] [Google Scholar]