Abstract
Background:
The glenohumeral joint is one of the most frequently dislocated joints in the body, particularly in young, active adults.
Purpose:
To conduct a systematic review and meta-analysis to evaluate and compare outcomes between anterior versus posterior shoulder instability.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was performed using the PubMed, Cochrane Library, and MEDLINE databases (from inception to September 2019) according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Studies were included if they were published in the English language, contained outcomes after anterior or posterior shoulder instability, had at least 1 year of follow-up, and included arthroscopic soft tissue labral repair of either anterior or posterior instability. Outcomes including return-to-sport (RTS) rate, postoperative instability rate, and pre- and postoperative American Shoulder and Elbow Surgeons (ASES) scores were recorded and analyzed.
Results:
Overall, 39 studies were included (2077 patients; 1716 male patients and 361 female patients). Patients with anterior instability had a mean age of 23.45 ± 5.40 years (range, 11-72 years), while patients with posterior instability had a mean age of 23.08 ± 8.41 years (range, 13-61 years). The percentage of male patients with anterior instability was significantly higher than that of female patients (odds ratio [OR], 1.36; 95% CI, 1.04-1.77; P = .021). Compared with patients with posterior instability, those with anterior instability were significantly more likely to RTS (OR, 2.31; 95% CI, 1.76-3.04; P < .001), and they were significantly more likely to have postoperative instability (OR, 1.53; 95% CI, 1.07-2.23; P = .018). Patients with anterior instability also had significantly higher ASES scores than those with posterior instability (difference in means, 6.74; 95% CI, 4.71-8.77; P < .001). There were no significant differences found in postoperative complications between the anterior group (11 complications; 1.8%) and the posterior group (3 complications; 1.6%) (OR, 1.12; 95% CI, 0.29-6.30; P = .999).
Conclusion:
Patients with anterior shoulder instability had higher RTS rates but were more likely to have postoperative instability compared with posterior instability patients. Overall, male patients were significantly more likely to have anterior shoulder instability, while female patients were significantly more likely to have posterior shoulder instability.
Keywords: anterior shoulder instability, anterior shoulder dislocation, posterior shoulder instability, posterior shoulder dislocation, Bankart repair, anterior labral tear, posterior labral tear
The glenohumeral joint is exceedingly unstable and therefore is one of the most frequently dislocated joints in the body, particularly in young, active adults.4,16,18,33 A study on shoulder instability performed by the Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Instability Group37 concluded that most patients who undergo shoulder stabilization are in their early 20s or younger and that anterior instability is more prevalent than posterior instability. These findings have also been found by numerous other studies.4,33,46 Although posterior instability is not as common, there are certain subgroups that have a high prevalence, including weightlifters, football players, and rugby players.26,38
The presenting symptoms of anterior instability are very different from posterior instability. A cohort study by Bernhardson et al4 comparing outcomes of anterior versus posterior instability between 200 patients determined that patients with anterior instability typically present after an identifiable mechanism of injury (requiring reduction by a medical provider) and complaints of instability. On the other hand, patients with posterior instability primarily presented with pain, but no mechanism of injury nor complaints of instability. This frequently occurs in the setting of repetitive microtrauma, such as long-term bench press, incline bench, or push-ups. Thus, weightlifters, football players, and rugby players are found to have a higher prevalence of posterior shoulder instability.26,38
Finally, the decision of whether to treat shoulder instability operatively or nonoperatively is of considerable debate. With regard to anterior instability, patients traditionally have initially been managed nonoperatively with a period of immobilization and rehabilitation, but this can lead to an unacceptably high recurrence rate, which has increased the prevalence of early operative stabilization.5,34,45,54 On the other hand, treatment for posterior instability is largely controversial, owing to the overall low prevalence of patients with posterior instability and the even lower number of patients undergoing surgical stabilization.26
Thus, numerous studies have observed outcomes after arthroscopic labral repair for anterior and posterior shoulder instability. The purpose of this study was to conduct a systematic review and meta-analysis to evaluate and compare outcomes between anterior versus posterior shoulder instability. We hypothesized that patients suffering from posterior shoulder instability would have superior outcomes after operative treatment.
Methods
Search Strategy and Study Selection
This study was reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.60 Two authors (R.G.C., N.E.G.) performed a manual study selection using the PubMed, Cochrane Library, and MEDLINE databases with any discrepancies being resolved through discussion with a third author (M.L.V.). The following search terms were utilized: “anterior shoulder instability,” “anterior shoulder dislocation,” “posterior shoulder instability,” “posterior shoulder dislocation,” “anterior labral tear,” “anterior labral repair,” “posterior labral tear,” “posterior labral repair,” “Bankart repair,” and “Reverse Bankart repair.” These databases were searched from inception to September 2019. All selected articles were then screened for additional studies using the reference lists provided in each article. After duplicates were removed, the titles and abstracts were screened for relevance. The full text was reviewed for the remaining articles to assess for eligibility using the criteria stated below.
Eligibility Criteria
Studies that met the following criteria were included: published in the English language, contained outcomes (defined below) after anterior or posterior shoulder instability, only included patients with at least 1 year of follow-up, and treated with arthroscopic soft tissue labral repair of either anterior or posterior instability. Studies were excluded if any of the following were present: published in a non-English language, no mention made of anterior or posterior instability, no stated data on outcomes, contained or used nonhuman subjects, included any other shoulder pathologies at the time of treatment, utilized open soft tissue labral repair, or utilized open and/or arthroscopic bony repair or reconstruction for shoulder instability. Patients from the included studies were separated into an anterior instability group and a posterior instability group based on their demographics, injury history, and postoperative outcomes and complications.
Outcomes
Patient demographics included sex, age, and whether the study reported on anterior or posterior instability. Outcomes that were used for a study to meet inclusion criteria required 1 of the following: pre- and postoperative functional scores specified by the American Shoulder and Elbow Surgeons (ASES) shoulder score, percentage of patients who returned to sport (RTS), recurrence of instability postoperatively, and postoperative complications. Recurrence of instability was defined as 1 or more of the following parameters: postoperative traumatic instability/dislocation, instability preventing return to full activity or sport, or necessity for postoperative surgical intervention. RTS was defined as percentage of patients who returned to sport at or above their preinjury level without any episodes of recurrence/instability.
Statistical Analysis and Meta-analyses
When comparing the RTS percentage, instability recurrence, and postoperative complications, the Fisher exact test was used to estimate odds ratios (ORs) between the anterior and posterior instability groups. The ASES scores from reporting studies were used to assess the difference between preoperative and postoperative outcomes, and the Z test was used to estimate the difference in means between the anterior and posterior instability groups. The odds of the different sexes experiencing an anterior versus posterior instability was calculated using a Fisher exact test. Finally, age of experiencing anterior and posterior instabilities was compared using a Z test. P ≤ .05 and confidence intervals that did not contain the null value (zero) were considered significant.
Results
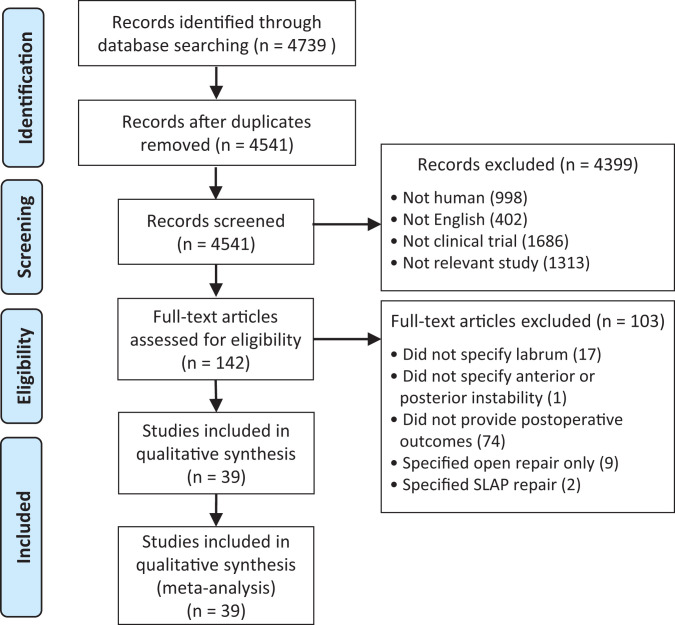
After identifying 4739 studies that matched our search criteria, this was narrowed to 4541 studies after duplicate removal. We then excluded 4399 studies based on the criteria mentioned previously. Only 142 full-text articles remained, which was further reduced to the final 39 studies that met criteria for the meta-analysis. Figure 1 denotes the flow diagram used for the study. Only 1 study was found to directly compare anterior versus posterior instability.4 The included studies were then assessed based upon the following components: patient demographics, RTS rate, postoperative instability, and functional outcomes.
Figure 1.
Flow diagram used for the study. SLAP, superior labral from anterior to posterior.
Patient Demographics
Table 1 summarizes the patient demographics in the included studies.
Table 1.
Patient Demographics in the 39 Included Studiesa
| Lead Author (year) | Patients, n | Male Patients, n | Female Patients, n | Follow-up, mo | Age, y | LOE |
|---|---|---|---|---|---|---|
| Anterior Instability (n = 28) | ||||||
| Bernhardson4 (2019)b | 103 | 96 | 15 | 40.4 | 23.5 (18-36) | 2 |
| Arciero3 (1994) | 21 | — | — | 32 (15-45) | 20.5 (18-21) | 2 |
| Jones32 (2007) | 30 | 17 | 13 | 25.2 | 15.4 (11-18) | 3 |
| Ee22 (2011) | 74 | 74 | 1 | 24 | 24.9 (13-44) | 2 |
| Alentorn-Geli1 (2016) | 57 | 57 | — | 96 (60-120) | 22 (16-28) | 4 |
| Plath49 (2015) | 66 | 46 | 20 | 42 (25-56) | 29.3 (14-72) | 4 |
| Carreira13 (2006) | 69 | 57 | 12 | 46 (24-108) | 27 (13-49) | 4 |
| Kim35 (2003) | 167 | 149 | 18 | 44 (24-76) | 25.2 (15-46) | 4 |
| O’Neill44 (1999) | 41 | 31 | 10 | 52 (25-84) | F = 27 (17-49); M = 18 (14-43) | 2 |
| Hantes28 (2009) | 38 | 30 | 8 | 38.4 (25-66) | 26.2 (15-48) | 2 |
| Larrain39 (2001) | 28 | 34 | 2 | 67.4 (28-120) | 21 (17-27) | 2 |
| Cho15 (2006) | 29 | — | — | 62.1 (25-117) | 21.1 (16-29) | 4 |
| Bottoni9 (2002) | 10 | 10 | — | 35 (17-56) | 21.6 (18-26) | 2 |
| Flinkkilä24 (2018) | 182 | 132 | 59 | 146.4 (120-192) | 26 (15-58) | 2 |
| Kirkley36 (2005) | 16 | 13 | 3 | 79 (51-102) | (23.3) | 2 |
| Robinson55 (2008) | 88 | 82 | 6 | 24 | 24.8 | 1 |
| Flint25 (2018) | 59 | 56 | 3 | 48 | 19.1 | 4 |
| Park48 (2019) | 51 | 51 | — | 24+ | 20.9 (19-27) | 3 |
| Sperber58 (2001) | 30 | 21 | 9 | 24 | 25 (18-51) | 1 |
| Stein59 (2011) | 47 | 39 | 8 | 32 | 26.9 | 4 |
| Szyluk61 (2015) | 92 | 74 | 18 | 98.4 (72-150) | 22.5 (15-37) | 2 |
| Rhee52 (2006) | 16 | 16 | — | 66.8 (30-136) | 20.4 (16-29) | 4 |
| Chapus14 (2015) | 21 | 20 | 1 | 116.4 (96-132) | 20.5 (15-25) | 4 |
| Bock6 (2018) | 21 | 17 | 4 | 105.6 (60-151.2) | 25.3 (15-41) | 4 |
| Law40 (2008) | 38 | 35 | 3 | 28 (24-48) | 21 (16-30) | 3 |
| Uhring62 (2014) | 14 | 11 | 3 | 19 | 20.6 (15-28) | 2 |
| Voos63 (2010) | 73 | 61 | 12 | 33 (24-49) | 32.6 (15-55) | 4 |
| Yamamoto66 (2015) | 40 | 36 | 13 | 12+ | 24.1 (14-54) | 4 |
| Overall | n = 1521 | n = 1265 | n = 241 | 23.45 ± 5.40 | ||
| Posterior Instability (n = 12) | ||||||
| Bernhardson4 (2019)b | 97 | 86 | 15 | 38.9 | 24.5 (18-36) | 2 |
| Provencher50 (2005) | 33 | 32 | 1 | 39.1 (22-60) | 25 (19-34) | 4 |
| Garret27 (2017) | 25 | 16 | 9 | 24 | 30 (16-45) | 2 |
| Radkowski51 (2008) | 98 | 75 | 23 | T = 28; NT = 26.7 | 22.3 | 2 |
| Lenart41 (2012) | 32 | 26 | 6 | 35.5 (12-67) | 21.4 (15-33) | 4 |
| Bottoni8 (2005) | 31 | 29 | 1 | 40 | 23 (15-39) | 4 |
| Bradley10 (2006) | 91 | 77 | 23 | 27.7 (12-77) | 23.3 (15-61) | 2 |
| Engelsma23 (2010) | 18 | 8 | 10 | 50 | 26 | 4 |
| Hurley30 (1992) | 25 | — | — | 60 (24-132) | 18.3 (13-30) | 3 |
| McClincy42 (2015) | 96 | 48 | 28 | T = 37 (12-97); NT = 37 (12-79) | 17.7 | 2 |
| Cruz-Ferreira17 (2017) | 32 | 28 | 4 | 12 | 29 (16-48) | 3 |
| Williams64 (2003) | 26 | 26 | — | 61.2 (24-140.4) | 28.7 (15-55) | 3 |
| Overall | n = 604 | n = 451 | n = 120 | 23.08 ± 8.41 | ||
aData are reported as mean (range) or mean ± SD unless otherwise indicated. Dashes indicate the study did not include this value. LOE, level of evidence; NT, nonthrowing athletes; T, throwing athletes.
bBernhardson et al4 was included in both anterior and posterior instability.
For the analysis of patient sex, 36 studies (92.3%) were included, with 1716 male and 322 female patients.∥ The percentage of male patients with anterior instability was significantly higher than that of female patients (OR, 1.36; 95% CI, 1.04-1.77; P = .021, Fisher exact test), and the percentage of female patients with posterior instability was significantly higher than that of male patients (OR, 1.36; 95% CI, 1.04-1.77; P = .021, Fisher exact test) (Table 2).
Table 2.
Overall Prevalence of Instability Between Sexesa
| Male | Female | Odds Ratio (95% CI) | P | |
|---|---|---|---|---|
| Anterior instability | 1265 (73.7) | 217 (67.4) | 1.36 (1.04-1.77) | .02b |
| Posterior instability | 451 (26.3) | 105 (32.6) | 1.36 (1.04-1.77) | .02b |
aData are reported as n (%) unless otherwise indicated.
bStatistically significant (P ≤ .05).
For the age analysis, 9 studies (23.8%) were used.6,10,14,25,51,53–55,59 Of the 425 patients included, 236 (55.5%) had anterior instability6,14,25,53–55,59 while 189 (44.5%) had posterior instability.10,51 There was no significant difference between the groups (difference in means, 0.37; 95% CI, –1.02 to 1.75; P = .302, Z test) (Table 3).
Table 3.
Difference in Age Between Anterior and Posterior Instability Patientsa
| Age, y | |
|---|---|
| Anterior instability (n = 236) | 23.45 ± 5.40 |
| Posterior instability (n = 189) | 23.08 ± 8.41 |
| Difference in means (95% CI) | 0.37 (–1.02 to 1.75) |
| P | .3 |
aData are reported as mean ± SD unless otherwise indicated.
Return to Sport
For the comparison of RTS between anterior and posterior instability, 25 studies (64.1%) with a total of 1257 patients were included.¶ The range of follow-up time varied between the 2 groups. The anterior instability subset ranged from 15 months (1.25 years) to 132 months (11 years), while the posterior instability subset ranged from 12 months (1 year) to 132 months (11 years). There were 874 patients (69.5%) with anterior instability, of which 695 (79.5%) returned to sport,# and 383 patients (30.5%) with posterior instability, of which 240 (62.7%) returned to sport.10,27,30,41,42,51,66 Patients with anterior instability were significantly more likely to RTS (OR, 2.31; 95% CI, 1.76-3.04; P < .001, Fisher exact test) (Table 4).
Table 4.
Difference in Return to Sport Between Anterior and Posterior Instability Patientsa
| Returned to Sport | |
|---|---|
| Anterior instability (n = 874) | 695 (79.52) |
| Posterior instability (n = 283) | 240 (84.81) |
| Odds ratio (95% CI) | 2.31 (1.76-3.04) |
| P | <.001b |
aData are reported as n (%).
bStatistically significant (P ≤ .05).
Postoperative Instability
There were 35 studies (89.7%) included in the analysis of postoperative instability, with a total of 1846 patients.** The range of follow-up time varied between the 2 groups. The anterior instability subgroup ranged from 15 months (1.25 years) to 192 months (16 years), while the posterior instability subgroup ranged from 12 months (1 year) to 140.4 months (11.7 years). There were 1406 patients (76.2%) with anterior instability, of which 195 (13.9%) had postoperative instability,†† and 440 patients (23.8%) with posterior instability, of which 42 (9.5%) had postoperative instability.8,10,23,27,41,50,51,64 Patients with anterior instability were significantly more likely to have postoperative instability (OR, 1.53; 95% CI, 1.07-2.23; P = .018, Fisher exact test) (Table 5).
Table 5.
Difference in Postoperative Instability Between Anterior and Posterior Instability Patientsa
| Postoperative Instability | |
|---|---|
| Anterior instability (n = 1406) | 195 (13.87) |
| Posterior instability (n = 440) | 42 (9.54) |
| Odds ratio (95% CI) | 1.53 (1.07-2.23) |
| P | .02b |
aData are reported as n (%).
bStatistically significant (P ≤ .05).
Functional Scores
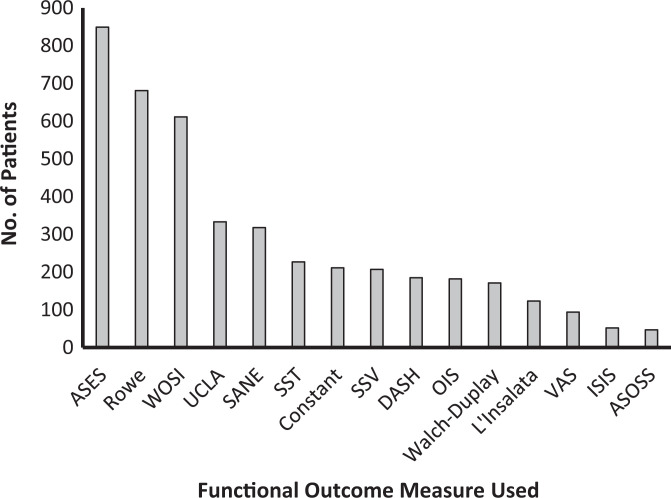
Figure 2 provides a breakdown of functional outcome measures reported by the included studies. The ASES score was used as the primary functional outcome of interest, as it provided the most comparable data between studies. There were 6 studies (15.4%), with a total of 547 patients, that reported ASES scores.10,35,41,42,51,63 The difference between preoperative and postoperative scores was used to analyze the data. The follow-up time for anterior instability studies that reported ASES scores ranged from 24 months (2 years) to 76 months (6.3 years), while posterior instability studies ranged from 12 months (1 year) to 97 months (8.1 years). There were 240 patients with anterior instability (43.9%)35,63 with a mean difference of 35.71 ± 19.91 between preoperative and postoperative scores, and 307 patients with posterior instability (56.1%)10,41,42,51 with a mean difference of 35.71 ± 33.73 between preoperative and postoperative scores. The functional scores in patients with anterior instability were not significantly different than in patients with posterior instability (difference in means, 0.001; 95% CI, –4.54 to 4.54; P = .999, Z test). However, when looking at just postoperative ASES scores, patients with anterior instability scored significantly higher (difference in means, 6.74; 95% CI, 4.71-8.77; P < .001, Z test). These results are shown in Table 6.
Figure 2.
Breakdown of the various shoulder functional outcome scores used in the included studies. ASES, American Shoulder and Elbow Surgeons; ASOSS, Athletic Shoulder Outcome Scoring System; DASH, Disabilities of the Arm, Shoulder and Hand; ISIS, Instability Severity Index Score; OIS, Oxford Instability Score; SANE, Single Assessment Numeric Evaluation; SST, Simple Shoulder Test; SSV, Subjective Shoulder Value; UCLA, University of California Los Angeles Shoulder Score; VAS, visual analog scale; WOSI, Western Ontario Shoulder Instability Index.
Table 6.
Difference in ASES Scores Between Anterior and Posterior Instability Patientsa
| Preoperative ASES | Postoperative ASES | Mean Difference | Difference in Means (95% CI) | P | |
|---|---|---|---|---|---|
| ASES score | 0.00 (–4.54 to 4.54) | .9996 | |||
| Anterior instability (n = 240) | 57.10 ± 16.98 | 92.81 ± 8.0 | 35.71 ± 19.91 | ||
| Posterior instability (n = 287) | 50.36 ± 18.62 | 86.07 ± 15.71 | 35.71 ± 33.73 | ||
| Difference in means (95% CI) | 6.74 (4.71-8.77) | ||||
| P | <.001b |
aData are reported as mean ± SD unless otherwise indicated. ASES, American Shoulder and Elbow Surgeons.
bStatistically significant (P ≤ .05).
Postoperative Complications Other Than Recurrence
Table 7 outlines the various complications listed among our subgroups of interest. Among the 39 included studies, only 19‡‡ (48.7%) indicated whether or not there were postoperative complications, and only 6 of these studies3, 10, 44, 55, 61, 63 (15.4%) actually had complications listed.There was no significant difference found between the anterior group (11 complications; 1.8%) and the posterior group (3 complications; 1.6%) (OR, 1.12; 95% CI, 0.29-6.30; P = .999). Of note, 1 study (Arciero et al3) had 3 postoperative complications but did not delineate whether the complications fell in the anterior operative or anterior nonoperative subgroups. Therefore, these complications were not included in the data analysis but were included in Table 7 to be more all-inclusive.
Table 7.
Postoperative Complications Between Subgroupsa
| Postoperative Complications | |
|---|---|
| Anterior instability | Posterior suture abscess (n = 1) Posterior sterile foreign-body granulomas (n = 1) Erythema and swelling over portal sites (n = 2) Adhesive capsulitis (n = 3) Axillary nerve praxia (n = 1) Anchor loosening (n = 1) Revisions for shoulder stiffness (n = 2) |
| Posterior instability | Infection of superficial portal (n = 1) Development of subacromial impingement (n = 2) |
| Othera | Subcutaneous suture abscess posteriorly (n = 1)
Transient hypesthesia of the median nerve distribution (n = 2) |
aArciero et al3 included both anterior operative and anterior nonoperative but did not specify which complications were attributed to each group.
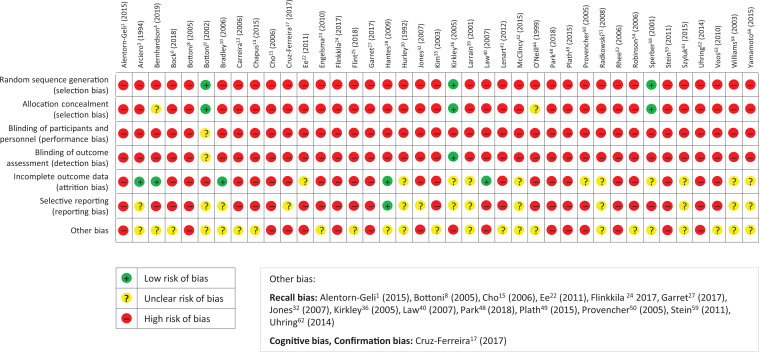
Quantitative Bias Analysis
The results of the quantitative bias analysis can be found in Appendix Figure A1. We were only able to find 2 studies55,58 in our literature review that were level 1 evidence; however, none of these studies directly compared anterior versus posterior shoulder instability. While only 4 included studies were randomized controlled trials,9,36,55,58 there were also 13 prospective cohort and 9 retrospective cohort studies that carried a somewhat low risk of bias. However, the fact that 13 included studies were case series may partially skew our results due to their heightened risk of bias. Furthermore, only 1 level 3 study4 directly looked at anterior versus posterior instability, thus putting the overall results of this study at high risk of compounding bias.
Discussion
To our knowledge, this is the first systematic review that has shed light on the differences in outcomes after anterior versus posterior shoulder instability. The most noteworthy conclusion was that overall, patients with anterior shoulder instability were 2.31 times more likely to RTS than patients with posterior instability. Even though patients with anterior instability were more likely to RTS, they still had a 1.53 times greater risk of suffering from postoperative instability. Our study also found that patients with anterior instability may have statistically significant higher ASES scores postoperatively, although this 7-point difference may not be clinically significant. Thus, our hypothesis was partially true because patients with posterior shoulder instability had less postoperative instability; however, they were also less likely to RTS. Finally, our results showed that there was no significant difference in postoperative complications when comparing anterior and posterior instability.
Our finding that patients with anterior shoulder instability have significantly better outcomes if they undergo surgery is widely supported throughout the published literature.3,12,20,21 However, one of the limitations of our study was the lack of published studies that directly compared anterior and posterior shoulder instability. As this is the first systematic review and meta-analysis to do so, we were limited in our ability to relate some of our major results to other published literature.
The only included study that directly compared anterior versus posterior instability outcomes was the cohort study by Bernhardson et al,4 which found that functional outcomes for 103 patients with anterior instability were statistically superior in all domains (ASES, Single Assessment Numeric Evaluation, Western Ontario Shoulder Instability Index) compared with the 97 patients with posterior instability. This was also found to be true in our results, where we found statistically significant higher postoperative ASES functional scores in patients with anterior instability. It should also be noted that the overall preoperative and postoperative ASES scores in their study were remarkably close to those in our study. Our preoperative and postoperative ASES scores for anterior instability were 57.1 and 92.8, respectively, while they found 58.0 and 94.2, respectively. For posterior stability, we found preoperative and postoperative ASES scores of 50.4 and 86.1, respectively, while they found 60.0 and 87.7, respectively. The only major difference noted here is that our study found much lower preoperative ASES scores in patients with posterior instability. This could be attributed to our larger sample size of 307 patients compared with their 97 patients.
Although the goal of our study was to find outcomes after anterior and posterior instability to effectively compare with studies such as Bernhardson et al,4 we were limited by the fact that no other included studies directly compared anterior versus posterior instability. Further data comparing outcomes of anterior versus posterior instability are needed to better clarify this comparison.
Another topic of discussion is the wide variety of functional scores used throughout the studies included in this systematic review. There was a total of 17 different functional scores used throughout the 39 included studies, as noted in Figure 2. This wide variety made it very difficult to directly compare functional outcomes between the studies. We chose to compare ASES functional scores, as they provided the most comparable data between studies and are also accepted as a good measure of shoulder function.2,56 The wide variation in functional tests used throughout the papers in our study certainly limited our ability to compare them in a meta-analysis. This problem of overabundance in functional tests is a commonality among other studies as well, including a meta-analysis by DeLong et al19 looking at posterior instability. They discussed the same inability to effectively compare shoulder instability studies via meta-analysis due to the overabundance of functional tests prevalent throughout the literature and cited other studies that had the same dilemma.57,65 This raises the need for a more well-rounded functional test that can be used throughout shoulder studies, allowing for proper comparison via meta-analysis. Additionally, although functional tests may be a good measure of postoperative outcomes, one may want to consider recurrence of instability as the best measure to delineate good versus poor outcomes in shoulder instability. However, what is considered the best measure of instability is certainly up for debate.
Limitations
We understand that our study comes with several limitations. Our study did not differentiate whether patients who underwent surgical intervention were treated nonoperatively before surgery. We also did not differentiate whether patients presented after their first traumatic event or if they had a history of multiple episodes of instability. These discrepancies could have altered patients’ postoperative outcomes from further compounding bias.
Regarding RTS, because of the limited reporting of sport type and level of competition in the current literature, we were unable to analyze how the type of sport (contact vs noncontact) or level of competition (high school, college, recreational, and professional) affected patient RTS. As the current literature has proven, these variables can largely affect a patient’s RTS prognosis.11,43,47 This limits our overall RTS conclusion between anterior versus posterior shoulder instability. Also, because of the limited reported time to RTS, we were unable to comment on how fast patients should expect to RTS. More randomized controlled studies looking at time to RTS for patients experiencing either anterior or posterior instability would be beneficial.
Another limitation is that even though we tried to standardize our results by only including studies that treated patients with arthroscopic soft tissue repair, we still understand there can be heterogenicity in both these treatment modalities. Nonoperative treatment can differ concerning time in sling, type of sling, and type of physical therapy. Similarly, another confounding factor is that previous studies have shown that surgeons’ experience, type of fixation, and amount of fixation used can alter patients’ surgical outcomes after shoulder instability.7 Thus, even though we tried to standardize the treatment methods, we were limited by variability within each study. We also tried to limit our review to studies that only included patients with at least 1 year of follow-up. However, there was still a wide range in time to follow-up in all variables measured. Thus, we understand there is a higher risk of rate of instability the longer the follow-up, and this can overall skew our results and weaken our conclusion.
The most notable limitation involves the small quantity of published literature regarding outcomes after posterior instability. As the main goal was to compare anterior versus posterior outcomes, the small sample size in posterior instability may be poorly representative of the entire population. However, since posterior instability is already less prevalent than anterior instability, this may not be a substantial limitation. Finally, we included many studies with a high risk of bias, likely due to the fact that only a few were randomized controlled trials. Although this may have skewed the results, we believe the large number of included studies and large cohort could correct for this issue.
Conclusion
In the current review, patients with anterior shoulder instability were associated with better outcomes with regard to RTS but were more likely to have postoperative instability compared with patients with posterior instability. Overall, men were significantly more likely to have anterior shoulder instability while women were significantly more likely to have posterior shoulder instability.
Appendix
Figure A1.
Risk of bias regarding the included studies.
∥References 1, 4, 6, 8 –10, 13, 14, 17, 22 –25, 27 –29, 31, 32, 35, 36, 39 –42, 44, 48, 49, 50 –55, 58, 59, 61 –64, 66, 67.
¶References 1, 3, 9, 10, 13 –15, 22, 27, 28, 30, 32, 35, 36, 41, 42, 44, 48, 49, 51, 55, 62, 63, 66, 67.
**References 1, 3, 8 –10, 13 –15, 22 –25, 27 –28, 32, 35, 36, 39 –42, 44, 48 –52, 55, 58, 59, 61 –64, 66.
Footnotes
Final revision submitted January 6, 2021; accepted February 18, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: The article processing charges related to the publication of this article were supported by the University of Kansas (KU) One University Open Access Author Fund, sponsored jointly by the KU Provost, KU Vice Chancellor for Research & Graduate Studies, and KUMC Vice Chancellor for Research and managed jointly by the Libraries at the Medical Center and KU-Lawrence. M.L.V. has received education payments from Titan Surgical Group and hospitality payments from DePuy and Zimmer Biomet. J.P.S. has received education payments from Arthrex and consulting fees from Vericel. M.T.P. has received consulting fees from Arthrex and JRF, nonconsulting fees from Arthrex and Arthrosurface, honoraria from Flexion and JRF, and royalties from Arthrex and Arthrosurface. B.G.V. has received education payments from Titan Surgical Group, consulting fees from DePuy, and hospitality payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Alentorn-Geli E, Alvarez-Diaz P, Doblas J, et al. Return to sports after arthroscopic capsulolabral repair using knotless suture anchors for anterior shoulder instability in soccer players: minimum 5-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):440–446. [DOI] [PubMed] [Google Scholar]
- 2. Angst F, Schwyzer HK, Aeschlimann A, et al. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society Standardized Shoulder Assessment Form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis Care Res (Hoboken). 2011;63(suppl_11):S174–S188. [DOI] [PubMed] [Google Scholar]
- 3. Arciero RA, Wheeler JH, Ryan JB, et al. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22(5):589–594. [DOI] [PubMed] [Google Scholar]
- 4. Bernhardson AS, Murphy CP, Aman ZS, et al. A prospective analysis of patients with anterior versus posterior shoulder instability: a matched cohort examination and surgical outcome analysis of 200 patients. Am J Sports Med. 2019;47(3):682–687. [DOI] [PubMed] [Google Scholar]
- 5. Bishop JA, Crall TS, Kocher MS. Operative versus nonoperative treatment after primary traumatic anterior glenohumeral dislocation: expected-value decision analysis. J Shoulder Elbow Surg. 2011;20(7):1087–1094. [DOI] [PubMed] [Google Scholar]
- 6. Bock J, Buckup J, Reinig Y, et al. The arthroscopic Bankart repair procedure enables complete quantitative labrum restoration in long-term assessments. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3788–3796. [DOI] [PubMed] [Google Scholar]
- 7. Bonacci J, Manson B, Bowe SJ, et al. Operative shoulder instability injury management in Australian Football League players: a case series. J Sci Med Sport. 2018;21(8):760–764. [DOI] [PubMed] [Google Scholar]
- 8. Bottoni CR, Franks BR, Moore JH, et al. Operative stabilization of posterior shoulder instability. Am J Sports Med. 2005;33(7):996–1002. [DOI] [PubMed] [Google Scholar]
- 9. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30(4):576–580. [DOI] [PubMed] [Google Scholar]
- 10. Bradley JP, Baker CL, Kline AJ, et al. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34(7):1061–1071. [DOI] [PubMed] [Google Scholar]
- 11. Brophy RH, Lyman S, Chehab EL, et al. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37(4):768–775. [DOI] [PubMed] [Google Scholar]
- 12. Brophy RH, Marx RG. The treatment of traumatic anterior instability of the shoulder: nonoperative and surgical treatment. Arthroscopy. 2009;25(3):298–304. [DOI] [PubMed] [Google Scholar]
- 13. Carreira DS, Mazzocca AD, Oryhon J, et al. A prospective outcome evaluation of arthroscopic Bankart repairs: minimum 2-year follow-up. Am J Sports Med. 2006;34(5):771–777. [DOI] [PubMed] [Google Scholar]
- 14. Chapus V, Rochcongar G, Pineau V, et al. Ten-year follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocation in young patients. Orthop Traumatol Surg Res. 2015;101(8):889–893. [DOI] [PubMed] [Google Scholar]
- 15. Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy. 2006;22(9):947–953. [DOI] [PubMed] [Google Scholar]
- 16. Coyner KJ, Arciero RA. Shoulder instability: anterior, posterior, multidirectional, arthroscopic versus open, bone block procedures. Sports Med Arthrosc Rev. 2018;26(4):168–170. [DOI] [PubMed] [Google Scholar]
- 17. Cruz-Ferreira E, Abadie P, Godeneche A, et al. Posterior shoulder instability: prospective non-randomised comparison of operative and non-operative treatment in 51 patients. Orthop Traumatol Surg Res. 2017;103(8_suppl):S185–S188. [DOI] [PubMed] [Google Scholar]
- 18. Danzinger V, Schulz E, Moroder P. Epidemiology of functional shoulder instability: an online survey. BMC Musculoskelet Disord. 2019;20(1):281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. DeLong JM, Jiang K, Bradley JP. Posterior instability of the shoulder: a systematic review and meta-analysis of clinical outcomes. Am J Sports Med. 2015;43(7):1805–1817. [DOI] [PubMed] [Google Scholar]
- 20. Dickens JF, Rue JP, Cameron KL, et al. Successful return to sport after arthroscopic shoulder stabilization versus nonoperative management in contact athletes with anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2017;45(11):2540–2546. [DOI] [PubMed] [Google Scholar]
- 21. Donohue MA, Mauntel TC, Dickens JF. Recurrent shoulder instability after primary Bankart repair. Sports Med Arthrosc Rev. 2017;25(3):123–130. [DOI] [PubMed] [Google Scholar]
- 22. Ee GW, Mohamed S, Tan AH. Long term results of arthroscopic Bankart repair for traumatic anterior shoulder instability. J Orthop Surg Res. 2011;6:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Engelsma Y, Willems WJ. Arthroscopic stabilization of posterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1762–1766. [DOI] [PubMed] [Google Scholar]
- 24. Flinkkilä T, Knape R, Sirniö K, et al. Long-term results of arthroscopic Bankart repair: minimum 10 years of follow-up. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):94–99. [DOI] [PubMed] [Google Scholar]
- 25. Flint JH, Pickett A, Owens BD, et al. Recurrent shoulder instability in a young, active, military population and its professional implications. Sports Health. 2018;10(1):54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Frank RM, Romeo AA, Provencher MT. Posterior glenohumeral instability: evidence-based treatment. J Am Acad Orthop Surg. 2017;25(9):610–623. [DOI] [PubMed] [Google Scholar]
- 27. Garret J, Nourissat G, Hardy MB, et al. Painful posterior shoulder instability: anticipating and preventing failure. A study in 25 patients. Orthop Traumatol Surg Res. 2017;103(8_suppl):S199–S202. [DOI] [PubMed] [Google Scholar]
- 28. Hantes ME, Venouziou AI, Liantsis AK, et al. Arthroscopic repair for chronic anterior shoulder instability: a comparative study between patients with Bankart lesions and patients with combined Bankart and superior labral anterior posterior lesions. Am J Sports Med. 2009;37(6):1093–1098. [DOI] [PubMed] [Google Scholar]
- 29. Hovelius L, Augustini BG, Fredin H, et al. Primary anterior dislocation of the shoulder in young patients: a ten-year prospective study. J Bone Joint Surg Am. 1996;78(11):1677–1684. [DOI] [PubMed] [Google Scholar]
- 30. Hurley JA, Anderson TE, Dear W, et al. Posterior shoulder instability: surgical versus conservative results with evaluation of glenoid version. Am J Sports Med. 1992;20(4):396–400. [DOI] [PubMed] [Google Scholar]
- 31. Jakobsen BW, Johannsen HV, Suder P, et al. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow up. Arthroscopy. 2007;23(2):118–123. [DOI] [PubMed] [Google Scholar]
- 32. Jones KJ, Wiesel B, Ganley TJ, et al. Functional outcomes of early arthroscopic Bankart repair in adolescents aged 11 to 18 years. J Pediatr Orthop. 2007;27(2):209–213. [DOI] [PubMed] [Google Scholar]
- 33. Kane P, Bifano SM, Dodson CC, et al. Approach to the treatment of primary anterior shoulder dislocation: a review. Phys Sportsmed. 2015;43(1):54–64. [DOI] [PubMed] [Google Scholar]
- 34. Khiami F, Gerometta A, Loriaut P. Management of recent first-time anterior shoulder dislocations. Orthop Traumatol Surg Res. 2015;101(1_suppl):S51–S57. [DOI] [PubMed] [Google Scholar]
- 35. Kim SH, Ha KI, Cho YB, et al. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am. 2003;85(8):1511–1518. [PubMed] [Google Scholar]
- 36. Kirkley A, Werstine R, Ratjek A, et al. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21(1):55–63. [DOI] [PubMed] [Google Scholar]
- 37. Kraeutler MJ, McCarty EC, Belk JW, et al. Descriptive epidemiology of the MOON Shoulder Instability Cohort. Am J Sports Med. 2018;46(5):1064–1069. [DOI] [PubMed] [Google Scholar]
- 38. Lanzi JT, Chandler PJ, Cameron KL, et al. Epidemiology of posterior glenohumeral instability in a young athletic population. Am J Sports Med. 2017;45(14):3315–3321. [DOI] [PubMed] [Google Scholar]
- 39. Larrain MV, Botto GJ, Montenegro HJ, et al. Arthroscopic repair of acute traumatic anterior shoulder dislocation in young athletes. Arthroscopy. 2001;17(4):373–377. [DOI] [PubMed] [Google Scholar]
- 40. Law BK, Yung PS, Ho EP, et al. The surgical outcome of immediate arthroscopic Bankart repair for first time anterior shoulder dislocation in young active patients. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):188–193. [DOI] [PubMed] [Google Scholar]
- 41. Lenart BA, Sherman SL, Mall NA, et al. Arthroscopic repair for posterior shoulder instability. Arthroscopy. 2012;28(10):1337–1343. [DOI] [PubMed] [Google Scholar]
- 42. McClincy MP, Arner JW, Bradley JP. Posterior shoulder instability in throwing athletes: a case-matched comparison of throwers and non-throwers. Arthroscopy. 2015;31(6):1041–1051. [DOI] [PubMed] [Google Scholar]
- 43. Okoroha KR, Taylor KA, Marshall NE, et al. Return to play after shoulder instability in national football athletes. J Shoulder Elbow Surg. 2018;27(1):17–22. [DOI] [PubMed] [Google Scholar]
- 44. O’Neill DB. Arthroscopic Bankart repair of anterior detachments of the glenoid labrum: a prospective study. J Bone Joint Surg Am. 1999;81(10):1357–1366. [PubMed] [Google Scholar]
- 45. Owens BD, Agel J, Mountcastle SB, et al. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37(9):1750–1754. [DOI] [PubMed] [Google Scholar]
- 46. Owens BD, Duffey ML, Nelson BJ, et al. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35(7):1168–1173. [DOI] [PubMed] [Google Scholar]
- 47. Pantalone A, Vanni D, Guelfi M, et al. Arthroscopic treatment of shoulder instability in professional athletes. Muscles Ligaments Tendons J. 2016;6(4):440–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Park JY, Lee JH, Oh KS, et al. Return to play after arthroscopic treatment for shoulder instability in elite and professional baseball players. J Shoulder Elbow Surg. 2019;28(1):77–81. [DOI] [PubMed] [Google Scholar]
- 49. Plath JE, Feucht MJ, Saier T, et al. Sporting activity after arthroscopic Bankart repair for chronic glenohumeral instability. Arthroscopy. 2015;31(10):1996–2003. [DOI] [PubMed] [Google Scholar]
- 50. Provencher MT, Bell SJ, Menzel KA, et al. Arthroscopic treatment of posterior shoulder instability: results in 33 patients. Am J Sports Med. 2005;33(10):1463–1471. [DOI] [PubMed] [Google Scholar]
- 51. Radkowski CA, Chhabra A, Baker CL, et al. Arthroscopic capsulolabral repair for posterior shoulder instability in throwing athletes compared with nonthrowing athletes. Am J Sports Med. 2008;36(4):693–699. [DOI] [PubMed] [Google Scholar]
- 52. Rhee YG, Ha JH, Cho NS. Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. Am J Sports Med. 2006;34(6):979–985. [DOI] [PubMed] [Google Scholar]
- 53. Riccio I, de Sire A, Latte C, et al. Conservative treatment of traumatic shoulder instability: a case series study. Musculoskelet Surg. 2015;99(2):133–137. [DOI] [PubMed] [Google Scholar]
- 54. Robinson CM, Howes J, Murdoch H, et al. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88(11):2326–2336. [DOI] [PubMed] [Google Scholar]
- 55. Robinson CM, Jenkins PJ, White TO, et al. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: a randomized, double-blind trial. J Bone Joint Surg Am. 2008;90(4):708–721. [DOI] [PubMed] [Google Scholar]
- 56. Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum. 2009;61(5):623–632. [DOI] [PubMed] [Google Scholar]
- 57. Savoie FH, Holt MS, Field LD, et al. Arthroscopic management of posterior instability: evolution of technique and results. Arthroscopy. 2008;24(4):389–396. [DOI] [PubMed] [Google Scholar]
- 58. Sperber A, Hamberg P, Karlsson J, et al. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. J Shoulder Elbow Surg. 2001;10(2):105–108. [DOI] [PubMed] [Google Scholar]
- 59. Stein T, Linke RD, Buckup J, et al. Shoulder sport-specific impairments after arthroscopic Bankart repair: a prospective longitudinal assessment. Am J Sports Med. 2011;39(11):2404–2414. [DOI] [PubMed] [Google Scholar]
- 60. Stewart LA, Clarke M, Rovers M, et al. Preferred Reporting Items for Systematic Review and Meta-Analyses of Individual Participant Data: The PRISMA-IPD Statement. JAMA. 2015;313(16):1657–1665. [DOI] [PubMed] [Google Scholar]
- 61. Szyluk K, Jasinski A, Widuchowski W, et al. Results of arthroscopic Bankart lesion repair in patients with post-traumatic anterior instability of the shoulder and a non-engaging Hill-Sachs lesion with a suture anchor after a minimum of 6-year follow-up. Med Sci Monit. 2015;21:2331–2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Uhring J, Rey PB, Rochet S, et al. Interest of emergency arthroscopic stabilization in primary shoulder dislocation in young athletes. Orthop Traumatol Surg Res. 2014;100(8_suppl):S401–S408. [DOI] [PubMed] [Google Scholar]
- 63. Voos JE, Livermore RW, Feeley BT, et al. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38(2):302–307. [DOI] [PubMed] [Google Scholar]
- 64. Williams RJ, 3rd, Strickland S, Cohen M, et al. Arthroscopic repair for traumatic posterior shoulder instability. Am J Sports Med. 2003;31(2):203–209. [DOI] [PubMed] [Google Scholar]
- 65. Wolf EM, Eakin CL. Arthroscopic capsular plication for posterior shoulder instability. Arthroscopy. 1998;14(2):153–163. [DOI] [PubMed] [Google Scholar]
- 66. Yamamoto N, Kijima H, Nagamoto H, et al. Outcome of Bankart repair in contact versus non-contact athletes. Orthop Traumatol Surg Res. 2015;101(4):415–419. [DOI] [PubMed] [Google Scholar]
- 67. Yanmis I, Tunay S, Komurcu M, et al. Outcomes of acute arthroscopic repair and conservative treatment following first traumatic dislocation of the shoulder joint in young patients. Ann Acad Med Singapore. 2003;32(6):824–827. [PubMed] [Google Scholar]