Abstract
Background:
The collagen meniscal implant (CMI) is a biologic scaffold aimed at replacing partial meniscal defects. The long-term results of lateral meniscal replacement have never been investigated.
Purpose:
To document the clinical outcomes and failures of lateral CMI implantation for partial lateral meniscal defect at a minimum 10-year follow-up.
Study Design:
Case series; Level of evidence, 4,
Methods:
This study included 24 consecutive patients who underwent lateral CMI implantation for partial lateral meniscal defects between April 2006 and September 2009 and who were part of a previous study with a 2-year follow-up. Outcome measures at the latest follow-up included the Lysholm score, Knee injury and Osteoarthritis Outcome Score, visual analog scale (VAS) for pain, Tegner activity level, and EuroQol 5-Dimensions score. Data regarding complications and failures were collected, and patients were asked about their satisfaction with the procedure.
Results:
Included in the final analysis were 19 patients (16 male, 3 female) with a mean age at surgery of 37.1 ± 12.6 years and a mean follow-up of 12.4 ± 1.5 years (range, 10-14 years). Five failures (26%) were reported: 1 CMI removal because of implant breakage and 4 joint replacements (2 unicompartmental knee arthroplasties and 2 total knee arthroplasties). The implant survival rate was 96% at 2 years, 85% at 5 years, 85% at 10 years, 77% at 12 years, and 64% at 14 years. Lysholm scores at the final follow-up were rated as “excellent” in 36% (5 of 14 nonfailures), “good” in 43% (6 of 14), and “fair” in 21% (3 of 14). The VAS score was 3.1 ± 3.1, with only 16% (3 of 19 patients) reporting that they were pain-free; the median Tegner score was 3 (interquartile range, 2-5). All clinical scores decreased from the 2-year follow-up; however, with the exception of the Tegner score, they remained significantly higher compared with the preoperative status. Overall, 79% of patients were willing to undergo the same procedure.
Conclusion:
Lateral CMI implantation for partial lateral meniscal defects provided good long-term results, with a 10-year survival rate of 85% and a 14-year survival rate of 64%. At the final follow-up, 58% of the patients had “good” or “excellent” Lysholm scores. However, there was a general decrease in outcome scores between the short- and the long-term follow-up.
Keywords: meniscal scaffold, lateral meniscus, collagen meniscal implant, long-term follow-up
The number of meniscal surgeries performed in Europe and the United States is increasing every year because of their more active and older populations.10,12,13 While the percentages of meniscal repair procedures are increasing, meniscectomy is still the most performed surgery. In fact, most of the meniscal lesions are in the white-white zone or, especially in older patients, involve degenerated tissue, making them unsuitable for suture.11 A subset of the patients treated using meniscectomy will experience a worsening of symptoms and pain and increased contact stress, which is referred to as postmeniscectomy syndrome.2 Meniscal replacement is considered the optimal and desired approach for these patients6: in cases of total or subtotal meniscectomy, a meniscal allograft transplantation (MAT) is indicated, while meniscal scaffolds should be considered in cases of partial meniscectomy.3
Regarding the scaffolds, there are 3 main options: the collagen meniscal implant (CMI) derived from a bovine collagen; the ACTIfit, a polyurethane scaffold; and 3-dimensional printed scaffolds.4,7 While the last option has been recently proposed as an experimental treatment and only a few case reports are available, CMI and ACTIfit have been widely studied in large multicenter trials. However, most of them have been limited to a midterm follow-up. The only 2 studies18,26 that have presented long-term, 10-year results were limited exclusively to the medial CMI.
The present study aimed to investigate the long-term outcome of lateral CMI implantation for partial lateral meniscal defects at a minimum 10-year follow-up, and to report failures. The hypothesis was that beneficial results would decrease over time in terms of clinical scores and failure rate 10 years after CMI implantation.
Methods
The study was conducted according to the principles of the Declaration of Helsinki. Study approval was obtained from the institutional review board of both institutions where the study was developed. Informed consent complied with European Union laws and was signed by patients before enrollment.
Patient Cohort
We investigated the long-term clinical outcomes of 24 consecutive patients who underwent lateral CMI implantation for partial lateral meniscal defects between April 2006 and September 2009 at 2 institutions (Istituto Ortopedico Rizzoli and Ospedale di Circolo).25 The included patients represented a prospective, multicenter European cohort from which 6-month and 2-year outcomes had already been published.25 According to the original study protocol,25 the inclusion criteria for CMI implantation were (1) irreparable acute lateral meniscal tears requiring partial meniscectomy (acute pattern) or previous traumatic or degenerative loss of lateral meniscal tissue (chronic pattern) greater than 25%, (2) intact anterior and posterior horn attachments of the lateral meniscus, (3) intact rim (≥1 mm) over the entire circumference of the involved meniscus (a deficient popliteal hiatus was allowed because here the native meniscal rim has low vascularization and, consequently, less healing ability), (4) anterior cruciate ligament deficiency stabilized at the time of the index surgery, (5) age between 15 and 60 years, (6) a contralateral healthy knee, and (7) diagnosis of Outerbridge grades 1 to 3. Exclusion criteria were (1) concomitant posterior cruciate ligament insufficiency of the involved knee; (2) diagnosis of Outerbridge grade 4 degenerative cartilage disease in the affected joint; (3) uncorrected malformations or axial misalignment in the involved lower extremity greater than 5°; (4) documented allergy to collagen or chondroitin sulfate of animal origin; (5) systemic or local infection; (6) history of anaphylactic reaction; (7) systemic administration of corticosteroid or immunosuppressive agents within 30 days of surgery; (8) evidence of osteonecrosis in the involved knee; (9) history of rheumatoid arthritis, inflammatory arthritis, or autoimmune diseases; (10) neurologic abnormalities or conditions that would preclude the patient’s requirements for the rehabilitation program; and (11) pregnancy.
Patients were reviewed in May 2020 with a minimum of 10 years of follow-up. One patient had a knee injury during a car accident 3 years after CMI implantation and was excluded from the long-term analysis. Four of the remaining 23 patients (17%) were lost to follow-up after the 2-year evaluation; therefore, 19 patients were available for the long-term assessment.
Surgical Technique and Rehabilitation
The technique for arthroscopic lateral CMI implantation has already been described in previous publications.25 Briefly, after arthroscopic confirmation of CMI implantation indication, the damaged meniscus was debrided according to the presence of an acute tear or a chronic defect. The anterior and posterior meniscal attachment points were trimmed square to accept the scaffold, and the blood supply was enhanced by making puncture holes in the peripheral rim using a Steadman awl. After measuring the defect size and opportune trimming of the scaffold, the CMI was positioned inside the joint and sutured to the host meniscal remnant using “all-inside” stitches (nonabsorbable ULTRABRAID No. 0 wire and poly-l-lactide bioabsorbable ULTRA FAST-FIX implants; Smith & Nephew).
A knee brace locked in full extension was applied and maintained for 6 weeks. Continuous passive motion exercises were performed 4 times per day, up to 60° for the first 2 weeks and 90° for the second to fourth weeks, and complete range of motion was achieved at the sixth week. Progressive weightbearing was allowed 2 weeks after surgery. Muscle strengthening started on the second postoperative day via isometric exercises, and cycling was allowed during the second postoperative week. Full unrestricted activity as tolerated was permitted 6 months after surgery.
Patient Evaluation
Patient-reported outcome measures (PROMs) included the Lysholm score, visual analog scale (VAS) for pain (0-10 [worst pain]), Tegner activity level, and EuroQol 5-Dimensions (EQ-5D) score. The preoperative, 6-month, and 2-year scores were retrieved from another study previously published by our team.25 At the final follow-up, patients were contacted, and the same PROMs were obtained; in addition, the Knee injury and Osteoarthritis Outcome Score (KOOS) was administered, and the value for each patient was interpreted according to the Patient Acceptable Symptom State (PASS) determined for MAT.14 Patients were also queried regarding complications and reoperations during the considered follow-up time, and they were asked about their satisfaction with the procedure. Patients with partial or total scaffold removal, unicompartmental knee arthroplasty (UKA), and total knee arthroplasty (TKA) were considered to have experienced failure. Patients with failures were rated as “poor” according to the Lysholm score and were considered not to have achieved the PASS for any of the KOOS subscales (Quality of Life [QoL], Symptoms, Activities of Daily Living [ADL], Sport, and Pain).
We also compared the results of the present study with those of another study our team conducted on 17 patients who underwent medial CMI implantation with a similar follow-up period.26 Data regarding clinical scores and surgical characteristics of patients who underwent medial scaffold implantation were retrieved and compared.
Data regarding the modified Yulish score for cartilage status23,24 in the preoperative evaluation and at the 2-year follow-up were retrieved from the original short-term study25; the Genovese score for the scaffold size and signal5 measured at the 2-year follow-up was also obtained. No magnetic resonance imaging (MRI) was performed at the last follow-up. Briefly, MRI scans were obtained via a 1.5-T unit using the same sequences (gradient echo T2, spin echo T1, fat-saturated fast-spin echo proton density, and T2-weighted) and techniques.
Statistical Analysis
Statistical analysis was performed using MedCalc software. Continuous variables were reported as mean ± SD, while categorical variables were reported as absolute number and proportion of the total sample. Only the Tegner score was reported as median value with interquartile range. The Mann-Whitney U test was used to compare the Tegner level at the different follow-ups, while the paired-samples t test was used to compare the Lysholm, VAS, and EQ-5D scores. To avoid overestimation of PROM average values, in the case of failure, a value of 1 was used for the Tegner score20; 64, for the Lysholm score (“poor”)17; 8, for the VAS1 (severe pain); and 0.383, for the EQ-5D9 (preoperative values of patients undergoing knee joint replacement). A Kaplan-Meier survival curve was created to analyze the survival rates at 2, 5, 10, 12, and 14 years, using failures (scaffold removal, UKA, or TKA) as the endpoint. For the survival rate at 2 years, all 24 patients from the original study25 were included. Statistical significance was set at P < .05.
Results
Failures and Reoperations
Nineteen patients (16 male, 3 female) with a mean age at surgery of 37.1 ± 12.6 years were included in the final analysis at an average follow-up of 12.4 ± 1.5 years (range, 10-14 years) (Table 1).
Table 1.
Patient and Surgical Characteristics (N = 19)a
| Variable | Value |
|---|---|
| Age at surgery, y | 37.1 ± 12.6 |
| Age at final follow-up, y | 49.5 ± 12.4 |
| Final follow-up, y | 12.4 ± 1.5 |
| Sex, male/female | 16 (84)/3 (16) |
| BMI | 23.7 ± 2.8 |
| Indication, acute/chronic | 4 (21)/15 (79) |
| Time from meniscectomy, y | 8.3 ± 9.5 |
| Tear zone, RR/RW | 14 (74)/5 (26) |
| Defect length, mm | 45 ± 8 |
| No. of sutures | 5 ± 1 |
| Combined ACL, yes/no | 4 (21)/15 (79) |
aValues are presented as mean ± SD or n (%). ACL, anterior cruciate ligament; BMI, body mass index; RR, red-red; RW, red-white.
Overall, 5 patients (26%) experienced failure (Table 2): 1 had the CMI removed after 6 months because of a rupture, and 4 underwent joint replacement (2 UKA and 2 TKA) because of increased pain in the context of already-existing osteoarthritis (Figure 1). In fact, the patients who underwent joint replacement were evaluated with the highest Yulish score at preoperative MRI (grades 3 and 4 for lateral femoral condyle or tibial plateau) and had partial or total CMI resorption at postoperative MRI at the 2-year follow-up. The implant overall survival was 96% at 2 years, 85% at 5 years, 85% at 10 years, 77% at 12 years, and 64% at 14 years (Figure 2). Another patient underwent anterior cruciate ligament reconstruction 9 years after CMI implantation but was not considered to have experienced failure.
Table 2.
Characteristics and Surgical Details of the Patients with Implant Failure (n = 5)a
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | |
|---|---|---|---|---|---|
| Age at surgery, y | 16.5 | 52.6 | 48.2 | 53.4 | 33.9 |
| Sex | Male | Female | Male | Female | Male |
| Indication | Chronic | Chronic | Chronic | Acute | Chronic |
| Time from meniscectomy, y | 0.5 | 7 | 29.5 | 0 | 1.7 |
| Defect size, mm | 40 | 50 | 60 | 65 | 45 |
| MRI Youlish score | 1 LFC, 1 LTP | 1 LFC, 3 LTP | 4 LFC, 4 LTP | 3 LFC, 3 LTP | 3 LFC, 1 LTP |
| Concomitant procedures | ACL-R | None | None | None | None |
| Type of failure | CMI removal | TKA | UKA | TKA | UKA |
| Cause of failure | CMI rupture | Increasing pain | Increasing pain | Increasing pain | Increasing pain |
| Time of failure, y postop | 0.5 | 2.1 | 2.3 | 12.2 | 13.5 |
| Age at failure, y | 17.1 | 54.7 | 50.5 | 65.6 | 47.4 |
aACL-R, anterior cruciate ligament reconstruction; CMI, collagen meniscal implant; LFC, lateral femoral condyle; LTP, lateral tibial plateau; MRI, magnetic resonance imaging; postop, postoperatively; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Figure 1.
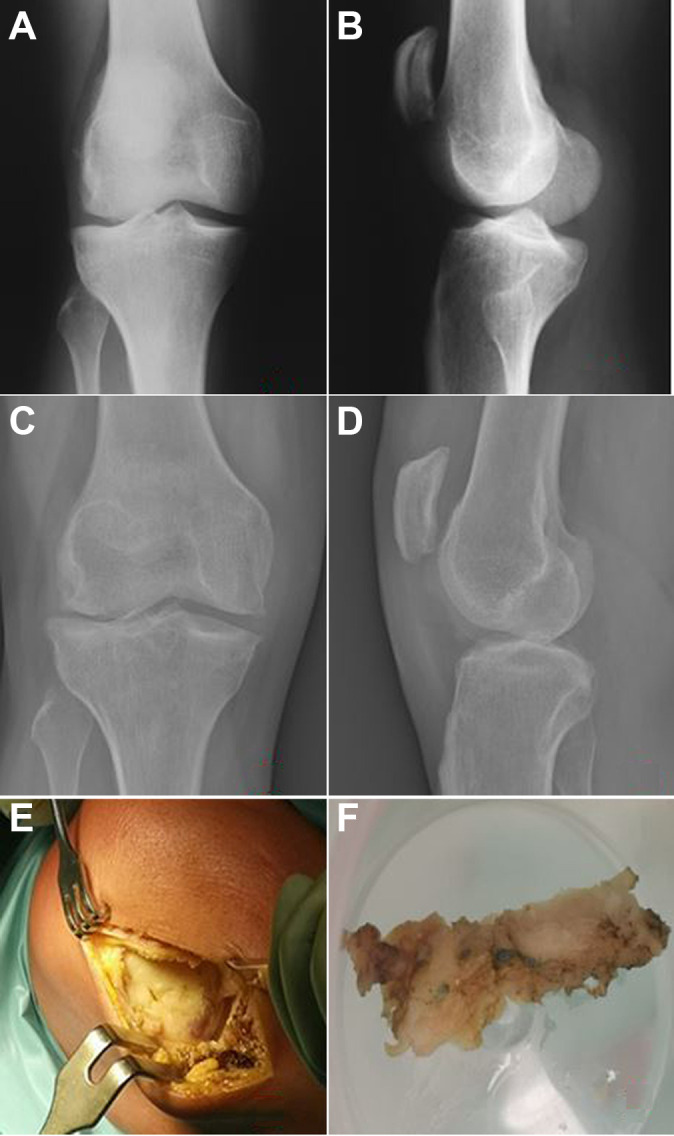
Clinical case of 1 patient with failure. Anteroposterior and lateral radiographs under weightbearing (A, B) at the time of the collagen meniscal implant (CMI) implantation and (C, D) before the implantation of a unicompartmental knee arthroplasty. (E, F) Intraoperative pictures showing the appearance of the CMI at the 14-year follow-up.
Figure 2.
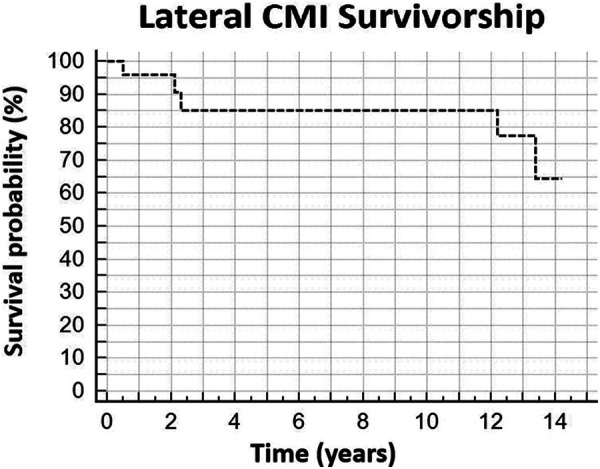
Kaplan-Meier curve of survivorship using collagen meniscal implant (CMI) removal, unicompartmental knee arthroplasty, or total knee arthroplasty as failure criteria.
Subjective PROM Evaluations
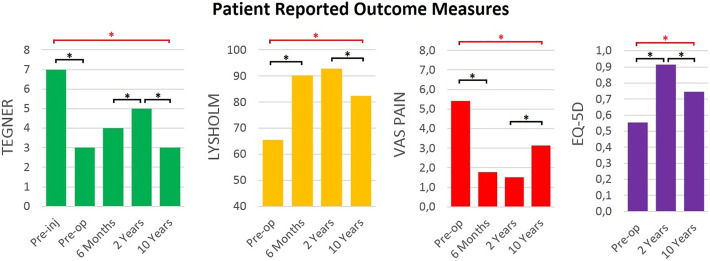
With respect to the earlier 2-year follow-up,25 the average Lysholm score significantly decreased to 82 ± 14 at the final follow-up (P = .0098), with the scores of 5 of 14 patients (36%) rated as “excellent”; 6 of 14 (43%), as “good”; and 3 of 14 (21%), as “fair.” Considering the 5 patients who experienced failure (scores rated as “poor”), a total of 58% had an excellent/good Lysholm score, while 42% had a fair/poor result. The VAS score significantly increased to 3.1 ± 3.1 at the final follow-up (P = .0136) (Figure 3), with only 3 of 19 patients (16%) reporting that they were totally pain-free. The EQ-5D score significantly decreased to 0.7 ± 0.3 (P = .0056), while the Tegner activity score decreased to a median value of 3 (interquartile range, 2-5; P = .0052) (Figure 3). All of the clinical scores were significantly higher than were their preoperative status, with the exception of the Tegner score.
Figure 3.
Mean Tegner activity level, Lysholm, visual analog scale (VAS) pain, and EuroQol 5-Dimensions (EQ-5D) scores at various study time points. A black asterisk indicates a statistically significant difference compared with the previously measured value (P < .05); a red asterisk indicates a statistically significant difference compared with a preoperative (Pre-op) value (P < .05). Pre-inj, preinjury.
The average KOOS subscale scores were 61 ± 36 for QoL, 67 ± 38 for Symptoms, 75 ± 41 for ADL, 60 ± 36 for Sport, and 73 ± 40 for Pain; 14 of 19 patients (74%) achieved the PASS14 for the QoL (>53 points), Sport (>22.5 points), ADL (>74.5 points), and Pain (>43 points) subscales, while 11 of 19 (58%) achieved it for the Symptoms subscale (>73 points). Overall, 79% reported that they would undergo the same procedure, if required, and the mean satisfaction score was 3.5 ± 1.3 out of 5.
The results from comparing this study with the previous study on medial CMI26 are shown in Table 3. According to the results, the lateral scaffold had inferior outcomes in terms of failure rate, pain score, and activity level compared with the medial scaffold.
Table 3.
Comparison of Characteristics and Long-Term Outcomes Between Lateral and Medial CMIa
| Lateral CMI (n = 19) | Medial CMI (n = 17) | P Value | |
|---|---|---|---|
| Characteristics | |||
| Age at surgery, y, mean (range) | 37.1 (16-54) | 38.0 (24-60) | .8305 |
| Sex, male/female, n (%) | 16 (84)/3 (16) | 17 (100)/0 (0) | .3163 |
| Indication, acute/chronic, n (%) | 4 (21)/15 (79) | 7 (41)/10 (59) | .2814 |
| Combined ACL, yes/no, n (%) | 4 (21)/15 (79) | 2 (12)/15 (88) | .6617 |
| Final follow-up, y, mean (range) | 12.4 (10.10-14.2) | 11.3 (10.0-12.6) | .0623 |
| Outcomes | |||
| Failures, n (%) | 5 (26) | 0 (0) | .0473 |
| Lysholm score, mean ± SD | 82 ± 14 | 92 ± 23 | .1200 |
| VAS pain score, mean ± SD | 3.1 ± 3.1 | 1.2 ± 1.9 | .0359 |
| Tegner score, median (IQR) | 3 (2-5) | 4 (3-5) | .0402 |
aThe medial collagen meniscal implant (CMI) outcomes are from a previously published study.26 The raw data for patient characteristics and outcomes of medial CMI were obtained and directly compared with the lateral CMI data according to the methods described in the Statistical Analysis section. Boldface P values indicate statistically significant differences between the groups (P < .05). ACL, anterior cruciate ligament; IQR, interquartile range; VAS, visual analog scale.
Discussion
The most important finding of the present study was that the implantation of lateral CMI for partial lateral meniscal defects provided good long-term results, with 74% of patients still having the implant in situ after a minimum of 10 years of follow-up and 58% of them rating their knee status as “good” or “excellent” according to the Lysholm score. However, a general decrease of all PROMs was reported from the short- to the long-term follow-up.
The present study provides novel insights regarding the outcome and performance of meniscal scaffolds for 2 main reasons: (1) the treatment of partial lateral meniscal defects and (2) the long-term follow-up of a minimum of 10 years. In fact, the current literature is lacking in studies with such features. Despite several multicenter clinical studies conducted worldwide analyzing the performance of meniscal scaffolds, such treatment is not widespread, and the current evidence on the clinical outcomes in humans is derived from fewer than 20 clinical studies published mostly from the same authors and from multicenter studies.8 Moreover, considering that a study on polyurethane scaffolds suggested a higher failure rate of lateral implants with respect to the medial ones at 2-year follow-up,22 a deeper and continual analysis of all aspects and long-term prognostic factors of meniscal substitution using scaffolds is worth investigation. In fact, the data for lateral meniscal replacement using lateral CMI implantation are limited to a short follow-up of 2 years.25 In that study,25 24 patients had good outcomes, with 1 (4%) experiencing failure because of scaffold removal, thus resulting in a 2-year survival rate of 96%. The long-term review of the same patients allowed us to determine the natural history of lateral CMI implantation and its survivorship. Two further failures occurred between the second and third postoperative years, accounting for a total survival rate at 3 years of 85%, which was maintained up to 10 to 12 years. After this time point, another 2 joint replacements were performed, decreasing the overall survival rate to 64% at 14 years. Based on this trend, the first 3 postoperative years could be identified as a critical time period in which 10% to 15% of patients could have suboptimal results and require further treatment. In contrast, the patients with successful early results tended to maintain a good clinical status for more than 10 years after the implantation. After this time point, patients could have consistent worsening of results and require joint replacement. As expected, a significant decrease of PROMs with lower function and greater pain occurred from 2 years to the long-term assessment. However, taking into account patients who experienced failure within the PROM evaluation, nearly 60% had good or excellent outcomes according to the Lysholm score, and 74% maintained the PASS for all KOOS subscales except for KOOS Symptoms. Moreover, 79% were satisfied with the procedure, despite only 3 patients remaining pain-free at the final follow-up. Therefore, based on the analysis of failures and PROMs of this small series, it can be affirmed that lateral CMI implantation is an effective procedure with acceptable long-term results.
In the literature, the long-term results of scaffolds at a minimum of 10 years have been reported only for medial meniscal replacement using CMI18,26; these studies have highlighted a significant improvement of pain, activity level, and radiologic outcomes with respect to partial meniscectomy. When comparing the results of the present study with those from a similar group of patients who underwent medial CMI implantation with a similar follow-up,26 a significantly higher failure rate and pain score and a lower activity level were present in the lateral scaffold group compared with the medial group. This could be due to the inherent anatomy biomechanics of the lateral compartment. In fact, a higher shear has been observed on the lateral tibial plateau,16 and the lateral meniscus has been shown to carry 70% of the load in the lateral compartment compared with the medial meniscus that carries only 50% of the load in the medial compartment. Moreover, the increased mobility of the lateral meniscus and the whole compartment could contribute to early wear and failure.16
A comparison with the results of other scaffolds for lateral meniscus is possible only for the polyurethane scaffold (ACTIfit) at 5 years of follow-up21; the reported survival rate (86.9%) is similar to the 85% rate reported during the same time frame in the present study. In contrast, the mean KOOS and VAS values of ACTIfit at 5 years appear to be slightly higher than the values reported for the CMI at 10 years. This seems logical considering the possible decrease of beneficial outcomes over time. Thus, based on this evidence, it could be speculated that no substantial differences in clinical outcomes are present between the 2 types of scaffolds.
The comparison between the outcomes of meniscal replacement and scaffold represents another critical aspect because the 2 treatments are not alternatives for the same indication but rather are complementary. In fact, allografts are indicated for total or subtotal meniscal defects,6 while scaffolds are indicated for partial defects with intact horns.3 Keeping in mind this difference, the overall long-term results of lateral CMI described in the present study seem comparable with the nearly 80% survival15 and the average Lysholm score of 77 points19 of lateral MAT.
Although this represents the first study to assess the long-term outcome of lateral meniscal replacement using a scaffold, several limitations are present. Four patients were lost to follow-up, thus creating a possible selection bias. However, a follow-up rate of 83% could be considered satisfactory, especially taking into account that the final assessment was performed at least 10 years postoperatively. Another limitation is represented by the limited number of patients, which did not allow us to perform sophisticated statistical subanalyses to identify outcomes and failure predictors; additional factors such as a surgical learning curve, the time from meniscectomy to scaffold implantation and the cartilage status, and the time of the index surgery could be relevant and should be investigated in studies with a larger sample size.
However, these patients represent the very first ones to be operatively treated using this device within the first multicenter European trial. It is hoped that more patients can be evaluated in future years. Finally, the lack of objective results and MRI assessment of the scaffold could leave some questions unanswered regarding the status of the scaffold and cartilage at the long-term follow-up. In particular, it is not possible to draw a conclusion regarding the rate of articular cartilage wear in the presence of a CMI and the potential chondroprotective effect of the scaffold. Moreover, the lower limb alignment could play an important role in terms of cartilage degeneration and was assessed only at the time of the index surgery as an inclusion criterion; it was not investigated at the final follow-up. However, the study aimed to investigate the clinical implications of meniscal replacement, how patients perceived pain, their knee function, and how many needed joint replacements at a minimum of 10 years after surgery, all important information for physicians and patients considering CMI implantation for lateral meniscal defects.
Conclusion
Lateral CMI implantation for partial lateral meniscal defects provided good long-term results, with a 10-year survival rate of 85% and a 14-year survival rate of 64%. Moreover, 58% of patients rated their knee status as “good” or “excellent” according to the Lysholm score, and 78% were satisfied by the procedure, although a general decrease of PROMs was reported from the short- to the long-term follow-up.
Footnotes
Final revision submitted November 23, 2020; accepted January 5, 2021.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from IRCCS Istituto Ortopedico Rizzoli, Bologna.
References
- 1. Boonstra AM, Schiphorst Preuper HR, Balk GA, Stewart RE. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain. 2014;155(12):2545–2550. [DOI] [PubMed] [Google Scholar]
- 2. Drobnič M, Ercin E, Gamelas J, et al. Treatment options for the symptomatic post-meniscectomy knee. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1817–1824. [DOI] [PubMed] [Google Scholar]
- 3. Filardo G, Andriolo L, Kon E, de Caro F, Marcacci M. Meniscal scaffolds: results and indications. A systematic literature review. Int Orthop. 2015;39(1):35–46. [DOI] [PubMed] [Google Scholar]
- 4. Filardo G, Petretta M, Cavallo C, et al. Patient-specific meniscus prototype based on 3D bioprinting of human cell-laden scaffold. Bone Joint Res. 2019;8(2):101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Genovese E, Angeretti MG, Ronga M, et al. Follow-up of collagen meniscus implants by MRI. Radiol Med. 2007;112(7):1036–1048. [DOI] [PubMed] [Google Scholar]
- 6. Getgood A, LaPrade RF, Verdonk P, et al. International Meniscus Reconstruction Experts Forum (IMREF) 2015 consensus statement on the practice of meniscal allograft transplantation. Am J Sports Med. 2017;45(5):1195–1205. [DOI] [PubMed] [Google Scholar]
- 7. Ghodbane SA, Brzezinski A, Patel JM, et al. Partial meniscus replacement with a collagen-hyaluronan infused three-dimensional printed polymeric scaffold. Tissue Eng Part A. 2019;25(5-6):379–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grassi A, Zaffagnini S, Marcheggiani Muccioli GM, Benzi A, Marcacci M. Clinical outcomes and complications of a collagen meniscus implant: a systematic review. Int Orthop. 2014;38(9):1945–1953. [DOI] [PubMed] [Google Scholar]
- 9. Gwynne-Jones DP, Sullivan T, Wilson R, Abbott JH. The relationship between preoperative Oxford hip and knee score and change in health-related quality of life after total hip and total knee arthroplasty: can it help inform rationing decisions? Arthroplasty Today. 2020;6(3):585–589.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002-2014. Sports Health. 2018;10(6):523–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hulet C, Helder P, Peretti G, Denti M. Surgery of the Meniscus. Springer-Verlag; 2016. [Google Scholar]
- 12. Jacquet C, Pujol N, Pauly V, Beaufils P, Ollivier M. Analysis of the trends in arthroscopic meniscectomy and meniscus repair procedures in France from 2005 to 2017. Orthop Traumatol Surg Res. 2019;105(4):677–682. [DOI] [PubMed] [Google Scholar]
- 13. Kawata M, Sasabuchi Y, Taketomi S, et al. Annual trends in arthroscopic meniscus surgery: analysis of a national database in Japan. PloS One. 2018;13(4):e0194854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu JN, Gowd AK, Redondo ML, et al. Establishing clinically significant outcomes after meniscal allograft transplantation. Orthop J Sports Med. 2019;7(1):2325967118818462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McCormick F, Harris JD, Abrams GD, et al. Survival and reoperation rates after meniscal allograft transplantation: analysis of failures for 172 consecutive transplants at a minimum 2-year follow-up. Am J Sports Med. 2014;42(4):892–897. [DOI] [PubMed] [Google Scholar]
- 16. McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88(12):1549–1556. [DOI] [PubMed] [Google Scholar]
- 17. Mitsou A, Vallianatos P, Piskopakis N, Maheras S. Anterior cruciate ligament reconstruction by over-the-top repair combined with popliteus tendon plasty. J Bone Joint Surg Br. 1990;72(3):398–404. [DOI] [PubMed] [Google Scholar]
- 18. Monllau JC, Gelber PE, Abat F, et al. Outcome after partial medial meniscus substitution with the collagen meniscal implant at a minimum of 10 years’ follow-up. Arthroscopy. 2011;27(7):933–943. [DOI] [PubMed] [Google Scholar]
- 19. Saltzman BM, Bajaj S, Salata M, et al. Prospective long-term evaluation of meniscal allograft transplantation procedure: a minimum of 7-year follow-up. J Knee Surg. 2012;25(2):165–175. [DOI] [PubMed] [Google Scholar]
- 20. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 21. Toanen C, Dhollander A, Bulgheroni P, et al. Polyurethane meniscal scaffold for the treatment of partial meniscal deficiency: 5-year follow-up outcomes. A European multicentric study. Am J Sports Med. 2020;48(6):1347–1355. [DOI] [PubMed] [Google Scholar]
- 22. Verdonk P, Beaufils P, Bellemans J, et al. Successful treatment of painful irreparable partial meniscal defects with a polyurethane scaffold: two-year safety and clinical outcomes. Am J Sports Med. 2012;40(4):844–853. [DOI] [PubMed] [Google Scholar]
- 23. Verdonk PCM, Verstraete KL, Almqvist KF, et al. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):694–706. [DOI] [PubMed] [Google Scholar]
- 24. Yulish BS, Montanez J, Goodfellow DB, Bryan PJ, Mulopulos GP, Modic MT. Chondromalacia patellae: assessment with MR imaging. Radiology. 1987;164(3):763–766. [DOI] [PubMed] [Google Scholar]
- 25. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Two-year clinical results of lateral collagen meniscus implant: a multicenter study. Arthroscopy. 2015;31(7):1269–1278. [DOI] [PubMed] [Google Scholar]
- 26. Zaffagnini S, Marcheggiani Muccioli GM, Lopomo N, et al. Prospective long-term outcomes of the medial collagen meniscus implant versus partial medial meniscectomy: a minimum 10-year follow-up study. Am J Sports Med. 2011;39(5):977–985. [DOI] [PubMed] [Google Scholar]