Abstract
Hospital readmission of stroke elderly remains a need for detecting preventable risks. This study aims to develop a Readmission Stroke Screening Tool or RRST. The mixed research design was employed, phase1; systematic reviews from 193 articles extracting to be 14 articles, 9 experts’ consensus, and try out the RRST Internal consistency; IOC = .93, ICC = between .93 and .56, phase 2; Data collecting 150 of strokes patients in the stroke units during 2019 to 2020; 30 nurses employed the RRST to screen stroke elderly before discharge. Statistical analysis, Exploring Principal Factor Analysis to test the best predictor factor, and Confirmatory Factor Analysis to test the model identity were employed. Results: The multi-domain RRST; 4 factors: Intra, inter, and external factors of patients can predict the hospital readmission of Stroke elderly at a high level in 28 days. The ADL: Activities in the Daily life domain was the highest level of predicting (Eigen Value = 6.76, 1.15, Variances = 79.19%) significantly. 53.3% of user nurses reflected; the RRST tool’s effectiveness was achievable in usefulness, benefit, accuracy, and easy to use; however, the rest users identified to improve the RRST easier and quicker. Conclusion; The new RRST; can predict the high-risk readmission effectively = 92.5%. User nurses satisfied the RRST predicted quality. the multi-domain RRST could be detecting the Thai Stroke’s high-risk group for reducing avoidable risks, suggestion; more effort will be investigated prospectively in readmission by expanded volume of the Asian’ Stroke elderly for increasing accuracy predicting and extended tool quality utilized standard scored correctly
Keywords: prediction of readmission, Asian’ Stroke elderly, risk screening, tool quality, tool development
Introduction
Stroke is a significant cause of morbidity and mortality and of which the second leading cause of death worldwide in both developing and developed countries. As a result, the leading cause of long-term disability worldwide. Stroke survivors are often left with permanent physical and mental disabilities and losing health care costs.1 More than 4.5 million strokes have a significant residual disability.2,3 The costs of stroke are rising payments to acute care facilities with high readmission rates within 30 days of discharge, partly due to an aging population.4,5 Stroke patients must be well prepared before hospital discharge to perform medical adherence effectively management at home. Since lacking prepare sufficiently for a routine discharge plan for the preventable readmission, the Stroke patient leaves the hospital then returns to the hospital in 28 days, critically or unplanned, is still occurring incontinent. Moreover; truly represent real avoidable patient readmissions is unclear; routine preventability assessment may require observation and information outside the scope of health records.6,7
Most of the older stroke patients also suffered from at least one other chronic condition compounding their various treatment regimen and recovery in the rehabilitation process.8 Many studies in stroke readmission presented that; multicenter study, 9% of the discharged patients with ischemic stroke were readmitted within a 1 month9; Thai’s 70 years old or more were 17.5%.10 A prediction of the readmission model was 15.5% in an Asian Population from proxy markers of hospitalization severity.11 Some studies reported that nurses’ screening devices for hospital discharge home among the stroke-patients having some limitations or a single domain or unclear, uncovered aspects,12 there is a lack of studies and instruments that evaluate the evaluation in various covered domains, including a standard for identifying and defining what is considered preventable readmission does not exist.12 A preventable hospital readmission rates as a quality metric and domains of Hospital Accreditation quality measures; the tool prediction’s reliability and feasibility are necessary.5
Within 28 days in the same condition, readmission stroke patients are more than a standard guideline; identified should not exceed 1.5%. However, in Thai, 10%; repeated stroke readmission in hospitals occurred among people aged 65 years and over.13,14 To detect crucial warning signs of post-stroke patients, screening with a clinician-friendly tool is necessary for surveillance. The gaps in post-discharge care coordination are increasing potential readmission risks. This study aims to develop and validate a predictive screening tool, Readmission Stroke Screening Tools (RRST), for constructing and confirming factors or domains determining hospital readmission for an older adult with a stroke and evaluating the quality of the tool by user nurses.
Material and Method
The RRST Clinical screening tool was developed to predict accuracy, used systematic reviews for initial construct mapping.15 Then following by 9 experts’ opinions, validate the screening framework, as has been done by others in health care clinics,16 to obtain the consensus of content validity of a panel of experts. The consistency of standardizing criteria, practicability, and measurement appraisal properties of the tool is achieved.16 Comprehensively mastering relevant knowledge and implementing usability in tool development processing are essential requirements for correctly assessing tool development’s methodological quality.16 To judge the quality of performance from the expert opinion into fit the RRST tool on the Thai’s context and time appropriately, based on decision-making rules, and screening administration recording and reporting requirements. Therefore, the design was composed of 2 sequential phases.
The first phase used a systematic review searching from 5 data-based. Five databases; (CINAHL Plus with Full Text (Ebsco); MEDLINE/PubMed (Ebsco); Ovid UML Journals@Ovid (University of Massachusetts, Lowell Subscribed content, and Cochrane Library (Wiley), Broad 5 important keywords were search items included keywords for readmission, risk assessment, tools and the terms “hospital settings” and “older adults.” Reliability, validity, and predictors of readmission tools were extracted independently by 2 authors and categorized by the authors’ classification tool to explore and investigate 194 topics related to RRST to be analyzed. The relevant titles and abstracts were screened as to eligibility based on the inclusion criteria. In doubtful cases, a decision was made by 2 reviewers. Differences in judgment were resolved through a consensus procedure.
The completed report articles were deducted to be 14 articles related to RRST. Assessing manuscripts from the corpus was conducted using the online systematic review software DistillerSR1. A pool of items or components was developed for the initial prototype version of the First draft RRST.
Nine experts included 4 medical doctors, 3 instructor nurses, and 2 head nurses who studied and work with stroke patients and older adults. The procedure of the tool formation refinement consisted of 5 steps: (1) define the concept, (2) generate the itemized pool, (3) determine the format of scored scaling, (4) itemized reviews, (5) pilot testing, Indexing Objective-itemized Correlation (IOC) of the RRST was calculated and improved to be an RRST in the Second draft RRST (48 items), They were tried out among 30 stroke patients before hospital discharge home. The new RRST (39 items) was implemented in phase 2 among 150 stroke patients before discharged home by 30 user nurses’ in screening and evaluating the RRST. This study’s setting was a Neurological service institute in Bangkok and Hospital in Pathum-Thani Province, Thailand.
Research Instrument Development
Phase 2; evidence gathering tools contain both the instrument and the instructions for gathering and interpreting evidence in an assessment process. An assessment tool is made up of the following components: (1) the context and conditions for the assessment, (2) the tasks to be administered to the population, (3) an outline of the evidence to be gathered from the population, (4) the evidence criteria used to judge the quality of performance, for instance, the decision-making rules, and (5) the administration recording and reporting requirements.
The RRST consisted of 5 domains/factors were affecting readmission; ADL domain applied the originality source from Barthel Index.17 All items were rated on a 3-points (10 items, full scored = 100); 10 = able to do, 5 = do some, 0 = don’t do, the summative response scale with ADL interpretation; 0-20 scored = high risk, 25-90 scored = moderate risk, 95-100 scored = low risk. IADL domain (modified originality source from Instrumental Activities of Daily Living Scale).18 All items were rated a 3-points (8 items, full scored = 24; 100); 3 = able to do, 2 = do some, 1 = can’t do, the summative response scale with IADL interpretation; 1%-20% = high risk, 21%-79% = moderate risk, 80%+ = low-risk for hospital readmission, Health Risk Behavior (HRB); all items were rated a 2-points (12 items full scored = 24; 100); 2 = able to do, can’t do = 1 (applied originality source from chronic care model).19 Summative response scale with the HRB scored interpretation ≥20% = low risk, ≤20 ± 79% = moderate risk, ≤80 = high risk. The ISAR (applied to originating source from Identification of Seniors at Risk Screening Tool)20 (7 items, full scored = 14:100). Moreover, TRST (applied originality source from Triage Risk Stratification Tool)21 (9 items, full scored = 18:100), the ISAR & TRST all items were rated a 2-points summative response scale scored on rating, and the interpretation used the same values scored scaling of HRB. Intraclass Correlation Coefficient: (ICC), Cranach’s Alpha Coefficient of ADL, IADL, HRB, ISAR, and TRST ranged = .95, .88, .71, .71, & .57 respectively, internal consistency IOC value = .936, 885, .710, .710 and 566, mean = 49, and SD = 13.360.
The sample was Thai stroke patients aged 60 years and older in the selected health care institute and hospital. The sample size can calculate from the table of estimating a population with specific relative precision.22 They admitted that from 2017 to 2018, 150 first stroke patients diagnosed by the physician who meets the inclusion criteria were selected. The acceptable sample size was 10 subjects per item,23 and 30 professional nurses as trained researchers’ assistants in the stroke units, who employed the RRST.
Data Collecting
Recruitment and consent of the first stroke patients were consent. They would be asked to participate by his /her treating health care professional before discharge home. All patients are free to choose whether or not to participate in the project. If they agree to engage in the study, the informed consent form will be signed before discharged home, continue into follow-up at the stroke clinic at the end of 2, 4 weeks after discharge home. A total of 3 times data gathering, users’ nurses assessed the patient’s level of consciousness and readiness to respond; before discharge home at the 1st screening using RRST (39 items). The screening through direct observation, interview, and patient’s profile recording.
Ethical considerations; there were necessary for participants to receive the harm’s protection while participating in this study. The participants received respect, no liability, and equality in this study as a whole. Before the implementation of the study protocol, approval was obtained by the Human Research Ethics Committee COA. No. MUPH 2016-19, 61039, and 091/2561. The committee approved, including the consent forms on the 2 Institute of the Stroke units’ human rights.
Data Analysis
Descriptive statistics of each item/component were used to delineate the scored distribution. Initially, the data were screened by examining descriptive statistics and potential univariate and multivariate assumption violations. The RRST quality criterion level for those metric correlation coefficients in each item of the RRST was 0.30 or greater (P-value <.05) were considered statistically significant and accepted.24 Then Exploratory Factor Analysis (EFA), principal components analysis, and rotation with Varimax method were applied. To test the tool quality, construct, and content validity, was the best factors, subfactors, and items/components of readmission of the stroke elderly. Indexing base on reliability, item quality, and predictivity of the new RRST; While as Confirmatory Factor Analysis (CFA)was used for RRSTModel identity testing the excellent fitting between the observed variables from the selected sample, and the theoretical framework underlying this framework.25,26 This process resulted in a 30-item RRST prototype scale as the latest model.
Qualitative Data Collecting and Analysis
Thirty nurse user responses were screening and recorded the 150 first stroke patients. It is observational and narrative in the stroke patient screening before discharge home; the narrative was verbatim and integrated thematically by 2 co-authors to form 4 declarative statements that followed Flick’s thematic coding procedures.27
Results
The participants’ characteristics; the 150 older adults with the first stroke; ranged in age from 60 to 89 years, 93 males, and 57 females. They were finished primary school and secondary school, respectively, living with spouses, and unemployed. Having 2 to 4 family members, and mostly live with spouse and children. Most of them can help themselves and have no caregivers; 6.7% were severity cases depend on the caregivers at home. Most treatment rights were the medical right of an official and gold card 30 baht. The final sample characteristics are presented in Table 1.
Table 1.
Demographic Characteristics of Older Adults with the First Stroke (n = 150).
| General characteristics | Values | |
|---|---|---|
| Frequency | % | |
| Gender | ||
| Male | 93 | 62.0 |
| Female | 57 | 38.0 |
| Age (years) | ||
| 60-69 | 78 | 51.9 |
| 70-79 | 47 | 31.4 |
| 80-89 | 25 | 16.7 |
| Financial status (person) | ||
| Insufficient | 21 | 36.0 |
| Sufficient | 110 | 60.0 |
| Sufficient and savings | 19 | 4.0 |
| Living style | ||
| Alone | 10 | 6.7 |
| Living with husband/wife | 28 | 18.7 |
| Living with husband/wife and children | 60 | 40.0 |
| Living with husband/wife and grandchildren | 8 | 5.3 |
| Living with husband/wife grandchildren and relatives | 44 | 29.4 |
| Self-care demand | ||
| No need caregiver | 100 | 73.3 |
| Need caregiver sometimes | 27 | 18.0 |
| Need caregiver totally | 13 | 6.7 |
| Underlying diseases | ||
| No | 4 | 2.7 |
| DM | 23 | 15.3 |
| HT | 32 | 21.3 |
| DM with HT | 85 | 56.7 |
| Other chronic diseases | 6 | 4 |
The RRST comprises 5 factors correlated to readmission for the older adult with a stroke. After data extraction from 48 components to be 4 crucial factors (39 components) influencing the stroke readmission in hospital as the following Table 2.
Table 2.
The Multi-Domain RRST; 4 Factors Attributed Influencing Hospital Readmission of an Older Adult with a Stroke.
| Attributes/statistical values | RRST domains | ||||
|---|---|---|---|---|---|
| ADL | IADL | Health risk behavior | ISAR | TRST | |
| Sub factor/component | 2 sub-factors; 10 component; factor loading ranged 0.925 to 0.689 | 1 sub-factors 8 components; factor loading ranged 0.921 to 0.599 | 5 sub-factors; 14 components; factor loading ranged 0.873 to 0.394 | 3 sub-factors; 7 components | 3 sub-factors; 9 components; factor loading ranged 0.957 to 0.477 |
| Eigen values | 6.764, 1.155 | 5.729 | 2.891, 1.903, 1.615, 1.323, 1.119 | 1.984, 1.312, 1.165 | 2.625, 1.495, 1.069 |
| % Of variance | 67.639, 11.548 | 71.613 | 20.825, 13.292, 11.903, 9.505, 7.669 | 28.341, 18.749, 16.639 | 29.465, 16.615, 13.019, 11.883 |
| Kaiser-Meyer-Olkin | 0.886 | 0.922 | 0.642 | 0.515** non-corresponding | 0.618 |
| Total % of variance | 79.187 | 71.613 | 62.714 | 63.924 | 70.982 |
| Total RRST 39 components | KMO = 0.843, approx. χ2 = 4.391, df = 0.741, sig = .000, Eigenvalue = 12.310, total % of variance = 72.678 | ||||
Note. EFA; Kaiser-Meyer-Olkin (KMO) scored value ≥0.60 = be accepted, ISAR was excluded the RRST (39 items) were obtained, accounting for 72.68% of the variance. *= N/A.
The Minimal Criterion
Firstly, the best predictor of the 4 factors of the Readmission screening tool passed the criteria (The Keiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett tests of sphericity indicated that the EFA was possible, as shown in Table 2. When the correlation is high, the factor analysis can be carried out. This scale of RRST (KMO value is 0.918, which is greater than 0.8) indicates that these data from 4 factors are very suitable for the Explanatory Factor Analysis and are accepted28 (The significance probability of Bartlett’s sphere test is 0.000, it is less than 0.01. The eigenvalue is approximately greater than or equal to 1). Accordingly, the results in Table 3; illustrated the words itemized and meaning counted of the components on each factor passed all significant criteria; Iteratively eliminated items from the item-pool were 39 items. Of course, the ADL factors are divided into 2 sub-factors: sub-factor 1, referred to the patients’ movement with 8 components; sub-factor 2, referred to patients’ urinary function, consisted of 2 components. While as the IADL factor has shown, only 1 factor consisted of 8 components. Likely HRB divided to be 4 subfactors: Including the TRST was divided into 3 sub-factors:
Table 3.
The Illustrated 4-Factors Pattern Matrix Showing the Factor Loadings of Each Component on EFA of RRST Model (39 Components) Compared with CFA of the New RRST Model (30 Components).
| EFA of RRST (39 items) | CFA of RRST (30 items) | Observed, interviewed | |||||
| EFA; ADL factor | CFA; ADL factor | ||||||
| Items ranking | Components | Sub-factors | Factor loading | Items ranking | Components | Sub-factors | |
| 1 | B6 | Movement | 0.925 | 1 | B6 | Movement | Body movement |
| 2 | B2 | Movement | 0.915 | 2 | B2 | Movement | Go to the toilet |
| 3 | B4 | Movement | 0.877 | 3 | B4 | Movement | Take a bath |
| 4 | B5 | Movement | 0.868 | 4 | B5 | Movement | Dress |
| 5 | B7 | Movement | 0.846 | 5 | B7 | Movement | Up the stairs |
| 6 | B1 | Movement | 0.844 | 6 | B1 | Movement | Up-down on the bed |
| 7 | B3 | Movement | 0.787 | 7 | B3 | Movement | Cleanse, wash the body |
| 8 | B8 | Movement | 0.685 | 8 | B8 | Movement | Dining |
| 9 | B9 | Toilet | 0.878 | 9 | B9 | Toilet | Urination |
| 10 | B10 | Toilet | 0.831 | 10 | B10 | Toilet | Defecation |
| EFA; IADL factor | CFA; IADL factor | ||||||
| 1 | D2 | Self-management | 0.921 | 11 | D2 | Self-management | Shopping |
| 2 | D5 | Self-management | 0.894 | 12 | D5 | Self-management | Homecare |
| 3 | D4 | Self-management | 0.880 | 13 | D4 | Self-management | Laundry |
| 4 | D8 | Self-management | 0.875 | 14 | D8 | Self-management | Traveling |
| 5 | D6 | Self-management | 0.861 | 15 | D6 | Self-management | Self-medication |
| 6 | D7 | Self-management | 0.855 | 16 | D7 | Self-management | Financial management |
| 7 | D3 | Self-management | 0.841 | 17 | D3 | Self-management | Self-food preparation |
| 8 | D1 | Self-management | 0.599 | 18 | D1 | Self-management | Taking advantage of the phone |
| EFA; HRB factor | CFA; HRB factor | ||||||
| 1 | C5 | Addictive substance | 0.873 | * | * | * | Having drunk alcohol or beverage drinks containing alcohol or not |
| 2 | C3 | Food consumption | 0.812 | * | * | * | Taking still eating the lipid food |
| 3 | C9 | Pattern of sleeping | 0.806 | 19 | C9 | Pattern of sleeping | Getting sleep behavior pattern problems |
| 4 | C6 | Addictive substance | 0.800 | * | * | * | Still smoking? (smoking) |
| 5 | C10 | Pattern of sleeping | 0.742 | 20 | C10 | Pattern of sleeping | Feeling confused/unfresh when waking up in the morning (wakeup) |
| 6 | C14 | Problem of sleeping | 0.734 | * | * | * | Having an unsolved coping with stress problem (solve stress problem) |
| 7 | C13 | Problem of sleeping | 0.729 | 21 | C13 | Problem of sleeping | Stressful or not comfortable to sleep |
| 8 | C11 | Pattern of sleeping | 0.722 | 22 | C11 | Pattern of sleeping | The number of hours of sleep can sleep per day? |
| 9 | C4 | Food consumption | 0.581 | 23 | C4 | Food consumption | Cooking food, add up the seasoning or salty food |
| 10 | C12 | Problem of sleeping | 0.569 | * | * | * | Need to take a drug for rest or sleep frequently |
| 11 | C2 | Food consumption | 0.511 | * | * | * | Eating sweets, soft drinks, beverages, and sweet food often |
| 12 | C7 | Exercise behavior | 0.394 | 24 | C7 | Exercise behavior | Getting exercise frequently |
| EFA; TRST factor | CFA; TRST; factor | ||||||
| 1 | G6_1 | Being pretended | 0.957 | 25 | G6_1 | Being pretended | Violence to the rights |
| 2 | G6_3 | Being pretended | 0.944 | 26 | G6_3 | Being pretended | Seeking the benefits |
| 3 | G4 | History of falls | 0.860 | * | * | * | History of accidentally falling |
| 4 | G6_2 | Being pretended | 0.857 | 27 | G6_2 | Being pretended | Neglected own self |
| 5 | G2 | History of illness | 0.828 | 28 | G2 | History of illness | History of dementia or forgetfulness |
| 6 | G3 | Authority | 0.772 | 29 | G3 | Authority | Walking or limb movement difficult |
| 7 | G5 | Authority | 0.528 | * | * | * | Additive drug using |
| 8 | G6_4 | Authority | 0.477 | * | * | * | Within one month, receive readmission |
| 9 | G1 | History of illness | 0.419 | 30 | G1 | History of illness | Having a sign/symptom of confusion, calculating the number, and thinking slowly |
Note. EFA: all domains has Eigenvalues >1, all of the RRST component significant level at .05 to .00 and pass the criterion measured. *= N/A.
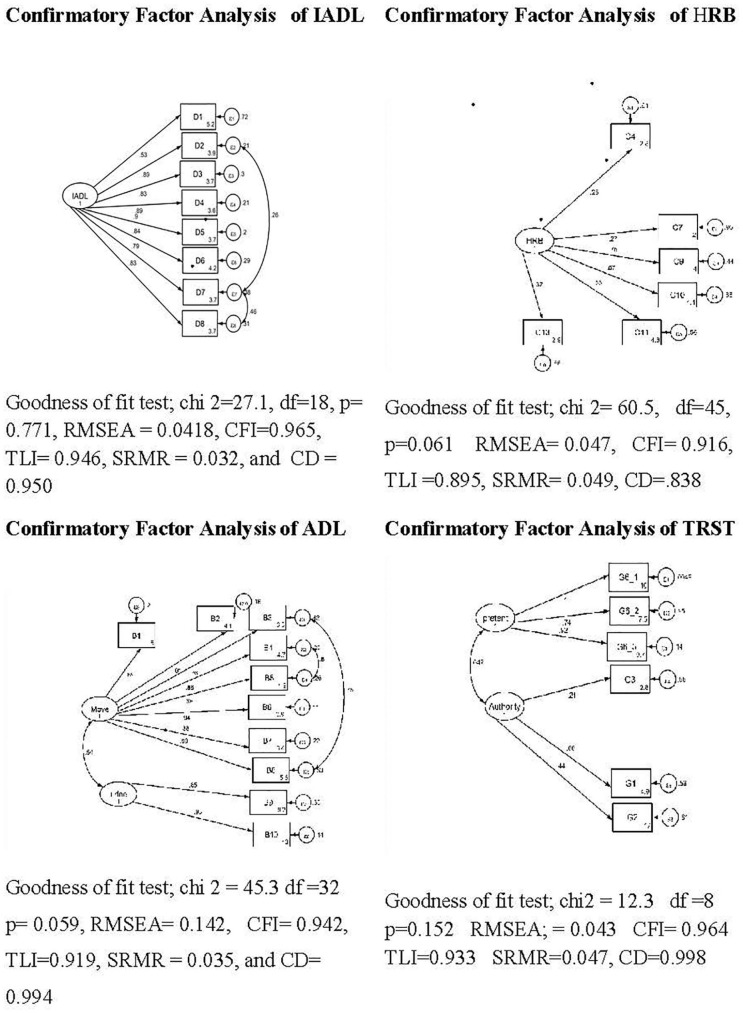
Further perform a confirmatory factor analysis (CFA) on the 39 components, verifying and replicating a new structure’s solution, the 9 items loss to be 30 items as the latest multi-domain RRST, (30 components); (due to 4 domains passed criteria of the goodness of fit) except ADL (factor had RMSEA = 0.142 higher than 0.08 cut off point, do not pass the criteria)29 as the following Table 3.
The latest multi-domains RRST
ADL domain: 10 components, IADL domain: 8 components, HRB domain: 6 components, and TRST domain: 6 components. The coefficient of a determinant of ADL, IADL, HRB, and TRST factors was 0.994, 0.950, 0.838, and 0.998. The multi-domain RRST Latent constructs in each domain are shown in elliptical line, and observed variables in rectangle line as Figures 1 and 2 as follows;
Figure 1.
The model fit indices of the new RRST of 4 factors: 30 components influencing the readmission of the older adult with stroke.
Figure 2.
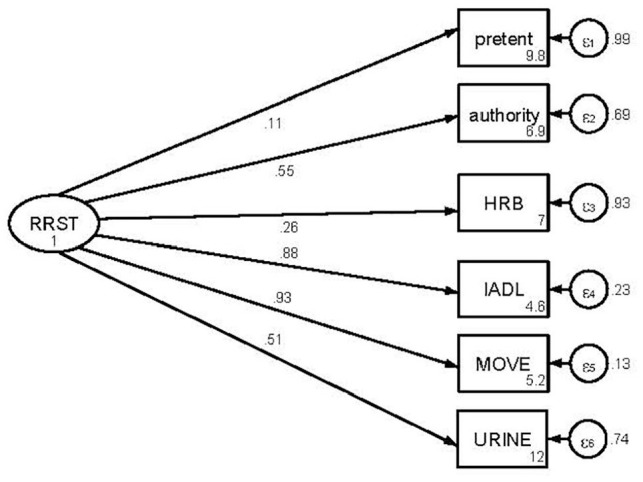
The multi-factors RRST model influencing the hospital readmission of the older adult with first stroke.
Note. The multi-domain RRST (30 components) model was the Goodness of fit found that χ2 = 7.572, df = 9, P = .578. RMSEA (root mean squared error of approximate) = 0.002, CFI = 0.99, TLI = 0.99, SRMR = 0.023, CD (coefficient of determination) = .916.
The latest multi domain RRST (30 components) was the Goodness of fit test; χ2 = 7.572, df = 9, P = .578, RMSEA = 0.002, CFI = 0.99, TLI = 0.99, SRMR = 0.023, and CD = 0.916, therefore the factor influencing hospital readmion of the stroke elderly as Figure 2 as follows:
The tool quality of prediction: The multi-domain RRST model had a cutoff point of the best predictor: ADL factor; ranged = 0-20, 25-90, and 95-100 scored: = high risk, moderate risk, and low-risk of stroke elderly readmission, respectively. Hence the researcher and user nurses followed the patients after discharge home, found that; the first time visited the stroke clinic; 2.7% of patients in the high-risk group (the ADL scored ≤ 20) were hospital readmitted in 28 days all, the second times of follow-up in 45 days; 6.16% of patients in the middle high-risk group( ADL scored = 20-25) had unplanned readmission in 6 weeks all.Therefore, the positive predictive value quality of the RRST in 28 days = 1, Negative Predictive Value = 0% Confidence Interval ( 95% CI = 1.00-1.00), In 45 days Negative Predictive Value = 92.5% (95% CI) = .883-.968.
The practicability of the new RRST found that 53.3% of the users’ nurses like to use the tools. The new RRST screening quality to be classified into 4 themes (1) usefulness, (2) fast and easy to use, (3) practical of the tools, and (4) total satisfaction of the tools. The overall general thought and feeling were that the tools could detect the Stroke elderly readmission. Moreover, 36.7% of them identified that the screening checklist was easy to understand, clear, and comprehensive in practicality, 43.3% presented that the RRST could help decrease working of hospital readmission rate of the stroke elderly; however, half of them commented to reviews the new RRST be shorter and quicker, including difficult to use because of the increased workload. Some user nurses identified that:
“Very satisfied; its useful, and easy to use” (H1N1, 2, 3, 5, H2 N8, 10, 12, H2 N 18, 19, 20, 23, 25, 26, 27, 28, 29, and H2N30).
They favor using the tools. The overall general feeling was that
“The tools should be used to prevent in-practice nursing from detecting readmission of older adults with Stroke.”
“It covers many aspects and updates new knowledge” (H1 N6, 7, & H2 N11)
However, 6 people identified “Moderate satisfaction” (N13, 15, H2N16, N21, 22, 24),
4 of them said, “Quite a lot of tool details and take much time to do” (H2N9, H1N14, 17).
“It takes a long time because there are many questions” (H1N4, H1N14)
The overall user nurse’s satisfaction was in the high middle level (X– = 8.78, SD = 0.552).
Discussion
The selected first stroke elderly subjects were representative, covering the mild,moderate-severity, and a high-risk cohort of the elderly with the first-time stroke; 73.3, 18.0, and 6.7%.30 New multi- domains RRST was designed from multiple perspectives to enhance this screening tool development quality. The solid empirical support from the systematic reviews shown; systematically developed statements informed of hard and soft evidence are trusted on the benefits and harms of stroke patient’s condition before discharge, multiple risks to be gathered from the previous stroke population; however, readmission models for the ischemic stroke in older adult populations, especially in Asian population based on administrative data, clinical data, or both generally performed inadequately.13,30 However; The systematic reviews had some limitations; hence, the data were not granular enough to allow for a systematic review compared to the other studies, even in the same design. Data were unavailable for several countries. Hospital-based studies are prone to selection bias, with a significant flaw in their representativeness; Therefore, experts’ consensus confirmed that the clustering structure and components of the first draft of the RRST are necessary, especially in potential risks hospital’s repeated admission. That is the best reconstructive technique for Tool development.29-31
The quality of the tool in content validity and reliability as a primary role in developing any new instrument by assessing the degree to which the instrument measures the targeted construct. The expert opinions come across a high correlation in IOC = .93 in accepted quality of IOC.32 The best sensitivity (95% confidence interval = ≥.90) of this new RRST was achieved; a comprehensive quality assessment tool for screening a broad range is a practical tool approved by the user.32,33
Reliability or coefficients Cornbrash’s alpha of the RRST as internal consistency each factor had the α coefficient of more than .7 passed the criteria, except the TRST had been improved before used,34,35 Probably of the scored might not represent the actual action/activities or congruent meaning with the stroke patient’s action; besides this, the scale narrowly ratings ranged from 1 to 2. In actual screening, the result prediction correctly indicated the gap of post-care readiness at home would be avoided or prepared further. The user nurses satisfied the new RRST is sufficiently flexible to be applied in the stroke clinic in holistic domains beyond one purely dimension tool measured ever used before,
However, the current study sufficiency reflected that 4 domains influencing stroke readmission in 28 days, primarily the ADL domain, the high scored level (0-20) contribute to clustering variance of RRST = 79.187%. This result is consistent with previous factor analysis studies.36,37 Moreover, IADL, HRB, and TRST tool these domains are considered as new stroke markers in a clinical stroke screening on the other studies.38 It is consistent with the Asian population study on stroke readmission; Several factors are essential for the risk of 30-day readmissions,12,13 including proxy markers of hospitalization severity30; the factors analyzed in the current study showed the determining variance in the new RRST = 71.613%.
ADL domain is the highest value of factor influencing the new RRST; However, significant body organ functions should be recorded, explicitly focusing on each specific malfunction of eyes, ears, arms, and balance movement are sufficiency condition among elderly. Moreover, sleep apnea36 dysphagia as a biomarker of deficit ADL39 and appropriate exercise activities in everyday life requires conscious assessment.38 Previously studies found that a critical condition needs to be solved or take special care at home, referral system to have a home visit case by case are necessary.40
The effectiveness of the newest RRST from sensitivity, specificity, and predictivity in 28 days = 100% correctly prediction typically has advantages such as placing fewer demands on health resources; being more accessible, less invasive, less expensive, and less physically and psychologically discomforting for elderly clients. Moreover, the screening resulted from feedback or counseling on the patient’s discharge plan for taking self-care at home. This study’s limitation; the new RRST did not integrate any clinical lab documents. Moreover, the cutoff point scored as an accurate predictor would be verified by extending the sample size in various Asien populations and settings. A detailed history of medication did not include in this study. The possibility of selection bias cannot be excluded from the inclusion criteria of a one-group study.
Conclusion and Suggestion
The new multi-domain RRST extends understanding to a comprehensive screening tool and tool quality assessment. The ADL domain combined with other domains, accuracy increasing 100% detection virtually in a high-risk older adult with the first stroke; base on the Intra, Inter, and External factors,41 influencing their hospital readmission in 28 days, might impact the patient’s recovery time frame management at home. A new knowledge resource for sharing would be applied for clinical screening by user nurses with better quality improvement of the stroke elderly in today’s healthcare property. More extensive studies, drive into follow-up 45 to 90 days, are still needed to investigate whether our findings could be applied to others in the Asian population.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received National Research Council of Thailand no. 46/2560; Faculty of Medicine Ramathibodi Hospital/Ramathibodi School of Nursing no.818/2557 financial support for the research, authorship, and/or publication of this article.
ORCID iD: Pimpan Silpasuwan  https://orcid.org/0000-0002-2969-0497
https://orcid.org/0000-0002-2969-0497
References
- 1. Lindsay MP, Norrving B, Sacco RL, et al. World stroke organization (WSO): global stroke fact sheet. Int J Stroke. 2019;14:806-817. doi: 10.1177/1747493019881353 [DOI] [PubMed] [Google Scholar]
- 2. Ingall T. Stroke: incidence, mortality, morbidity, and risk. J Insur Med. 2004;36:143-152. [PubMed] [Google Scholar]
- 3. Feigin VL, Forouzanfar MH, Krishnamurthi R, et al. The global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383:245-255. doi: 10.1016/s0140-6736(13)61953-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Luengo-Fernandez R, Violato M, Candio P, Leal J. Economic burden of stroke across Europe: a population-based cost analysis. Eur J Stroke. 2020;5:17-25. doi: 10.1177/2396987319883160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Healthcare Accreditation Institute. Criteria Evaluation and Certification Primary Stroke Center. Public Organization, Ministry of Public Health; 2015. (in Thai) [Google Scholar]
- 6. White CL, Brady TL, Saucedo LL, Motz D, Sharp J, Birnbaum LA. Towards a better understanding of readmissions after stroke: partnering with stroke survivors and caregivers. J Clin Nurs. 2015;24:1091-1100. doi: 10.1111/jocn.12739 [DOI] [PubMed] [Google Scholar]
- 7. Tsai TY, Hsu PF, Lin CC, et al. Factor analysis for the clustering of cardiometabolic risk factors and sedentary behavior, a cross-sectional study. PLoS One. 2020;15:e0242365. doi: 10.1371/journal.pone.0242365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mennella HDA-B. Hospital readmissions: United States Centers for Medicare and Medicaid Services (CMS). Pravikoff D RPF, editor. CINAHL Nursing Guide [Internet]. June 22, 2018. Accessed January 16, 2021. https://search-ebscohostcom.ejournal.mahidol.ac.th/login
- 9. Suri MF, Qureshi AI. Readmission within 1 month of discharge among patients with acute ischemic stroke: results of the University HealthSystem Consortium Stroke Benchmarking study. J Vasc Interv Neurol. 2013;6(2):47-51. [PMC free article] [PubMed] [Google Scholar]
- 10. Singkham N, Denwannakul W, Oa-sot J, Talodthaisong M. Predictors of hospital readmission among stroke patients. Naresuan Phayao J. 2017;10(3):87-89. [Google Scholar]
- 11. LL, Liu N, Wang S, Thumboo J, Ong ME, Lee KH. Predicting 30-day readmissions in an Asian population: building a predictive model by incorporating markers of hospitalization severity. PLoS One. 2016;11(12):e0167413. doi: 10.1371/journal.pone.0167413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vluggen TPMM, van Haastregt JCM, Tan FES, Kempen GIJM, Schols JMGA, Verbunt JA. Factors associated with successful home discharge after inpatient rehabilitation in frail older stroke patients. BMC Geriatr. 2020;20:25. doi: 10.1186/s12877-020-1422-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Prasat Neurological Institute, Department of Medical Service, Ministry of Public Health. Clinical Guideline for Standard Stroke Center Certify; 2015. (in Thai) [Google Scholar]
- 14. Hanchaiphiboolkul S, Poungvarin N, Nidhinandana S, et al. Prevalence of stroke and stroke risk factors in Thailand: Thai epidemiologic stroke (TES) study. J Med Assoc Thai. 2011;94:427-436. [PubMed] [Google Scholar]
- 15. Taylor-Rowan M, Nafisi S, Patel A, Burton JK, Quinn TJ. Informant-based screening tools for diagnosis of dementia, an overview of systematic reviews of test accuracy studies protocol. Syst Rev. 2020;9(1):271. doi: 10.1186/s13643-020-01530-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and better? Mil Med Res. 2020;7:7. doi: 10.1186/s40779-020-00238-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Quinn TJ, Langhorne P, Stott DJ. Barthel index for stroke trials: development, properties, and application. Stroke. 2011;42:1146-1151. doi: 10.1161/STROKEAHA.110.598540 [DOI] [PubMed] [Google Scholar]
- 18. Graf C. The Lawton instrumental activities of daily living scale. AJN. 2008;108:52-62. doi: 10.1097/01.NAJ.0000314810.46029.74 [DOI] [PubMed] [Google Scholar]
- 19. Wen T, Liu B, Wan X, et al. Risk factors associated with 31-day unplanned readmission in 50,912 discharged patients after Stroke in China. BMC Neurol. 2018;18:218. doi:10.1155 /2018/9853837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yao JL, Fang J, Lou QQ, Anderson RM. A systematic review of the identification of seniors at risk (ISAR) tool for the prediction of adverse outcomes in elderly patients seen in the emergency department. Int J Clin Exp Med. 2015;8:4778-4786. [PMC free article] [PubMed] [Google Scholar]
- 21. Naglie G. Validation of the triage risk stratification tool to identify older persons at risk for hospital admission and returning to the emergency department. J Am Geriatr Soc. 2008;56:2112-2117. doi:10.1111/j.1532-5415.2008. 01959.x [DOI] [PubMed] [Google Scholar]
- 22. Lwanga SK, Leamshow S. Sample size determination in health studies: instrumental activities of daily living. Gerontologist. 1969;9:179-186. [PubMed] [Google Scholar]
- 23. Mishel MH. Methodological studies: instrument development. In: Brink PJ, Wood MJ, eds. Advanced Design in Nursing Research. 2nd ed. SAGE Publications; 1998:238-284. [Google Scholar]
- 24. Mukaka MM, Nyirongo VB, Mukaka MM, Kalilani-Phiri LV. A guide to the appropriate use of correlation coefficient in medical research. Malawi Med J. 2008;20:15-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mueller RO, Hancock GR. Factor analysis and latent structure, confirmatory in an international encyclopedia of the social & behavioral sciences. 2001. www.ScienceDirect.com
- 26. Newsom JT, Shaw BA, August KJ, Strath SJ. Physical activity-related social control and social support in older adults: cognitive and emotional pathways to physical activity. J Health Psychol. 2018;23:1389-1404. doi: 10.1177/1359105316656768 [DOI] [PubMed] [Google Scholar]
- 27. Flick U. An Introduction to Qualitative Research. 6th ed. SAGE; 2018. [Google Scholar]
- 28. Glen S. “Kaiser-Meyer-Olkin (KMO) test for sampling adequacy” from StatisticsHowTo.com: elementary statistics for the rest of us. doi: 10.1159/000492820 https://www.statisticshowto.com/kaiser-meyer-olkin/ [DOI]
- 29. Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA test statistic in structural equation models. Sociol Methods Res. 2008;36:462-494. doi: 10.1177/0049124108314720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Béjot Y, Bailly H, Graber M, et al.·Impact of the ageing population on the burden of stroke: the Dijon stroke registry. Neuroepidemiology. 2019;52:78-85. [DOI] [PubMed] [Google Scholar]
- 31. Hung L-C, Sung S-F, Hu Y-H. A machine learning approach to predicting readmission or mortality in patients hospitalized for stroke or transient ischemic attack. Appl Sci. 2020;10(18):6337. doi: 10.3390/app10186337 [DOI] [Google Scholar]
- 32. Nye CD, Drasgow F. Assessing goodness of fit: simple rules of thumb simply do not work. Org Res Methods. 2011;14:548-570. doi: 10.1177/1094428110368562 [DOI] [Google Scholar]
- 33. Kilkenny MK, Longworth M, Pollack M, et al. Factors associated with 28-day hospital readmission after Stroke in Australia. Stroke. 2013;44:2260-2268. doi: 10.1161/STROKEAHA.111.000531 [DOI] [PubMed] [Google Scholar]
- 34. Braes T, Moons P, Lipkens P, et al. Screening for risk of unplanned readmission in older patients admitted to hospital: predictive accuracy of three instruments. Aging Clin Exp Res. 2010;22:345-351. doi: 10.1007/BF03324938 [DOI] [PubMed] [Google Scholar]
- 35. Zijlmans EO, Tijmstra J, Ark LA. Item-score reliability in empirical data sets and its relationship with other item indices. Educ Psychol Meas. 2018;78:998-1020. doi: 10.1177/0013164417728358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bajpai RC, Bajpai S. Goodness of measurement: reliability and validity. J Med Sci Public Health. 2014;3:112-115. [Google Scholar]
- 37. Shebeshi DS, Dolja-Gore X, Byles J. Unplanned readmission within 28 days of hospital discharge in a longitudinal population-based cohort of older Australian women. Int J Environ Res Public Health. 2020;17:3136. doi: 10.3390/ijerph17093136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Andersson E, Bohlin L, Herlitz J, Sundler AJ, Fekete Z, Hagiwara MA. Prehospital identification of patients with a final hospital diagnosis of stroke. Prehosp Disaster Med. 2018;33:63-70. doi: 10.1017/S1049023X17007178 [DOI] [PubMed] [Google Scholar]
- 39. Moons P, De Ridder K, Geyskens K. Screening for risk of readmission of patients aged 65 years and above after discharge from the emergency department: predictive value of four instruments. Eur J Emerg Med. 2007;14:315-323. doi:10.1097/MEJ.0b013 e3282aa3e45 [DOI] [PubMed] [Google Scholar]
- 40. Kumar S, Selim M, Caplan LR. Medical complications after stroke. Lancet Neurol. 2010;9:105-118. doi: 10.1016/S1474-4422(09)70266-2 [DOI] [PubMed] [Google Scholar]
- 41. Zingg W, Castro-Sanchez E, Secci FV. Innovative tools for quality assessment: integrated quality criteria for review of multiple study designs (ICROMS). Public Health. 2016;133:19-37. doi: 10.1016/j.puhe.2015.10.012 [DOI] [PubMed] [Google Scholar]