Abstract
Simple Summary
Prostate tumors are heterogeneous with unpredictable outcomes, ranging from harmless to aggressive, metastatic and deadly disease. Current diagnostic methods have limited ability to predict disease aggressiveness. New biomarkers are urgently needed to improve risk stratification, preferably involving non-invasive procedures. The aim of this prospective study was to assess the prognostic value of the inflammation markers S100A9 and S100A12 together with the monocyte count in blood samples from a cohort of 121 prostate cancer patients. We show that high monocyte count and high mRNA levels of S100A9, S100A12 are associated with poor outcome in patients with metastases at diagnosis. Our results suggest that analysis of these factors in blood could identify patients who are in direct need of additional treatment to conventional androgen deprivation therapy (ADT).
Abstract
Increasing evidence indicates calcium-binding S100 protein involvement in inflammation and tumor progression. In this prospective study, we evaluated the mRNA levels of two members of this family, S100A9 and S100A12, in peripheral blood mononuclear cells (PBMCs) in a cohort of 121 prostate cancer patients using RT-PCR. Furthermore, monocyte count was determined by flow cytometry. By stratifying patients into different risk groups, according to TNM stage, Gleason score and PSA concentration at diagnosis, expression of S100A9 and S100A12 was found to be significantly higher in patients with metastases compared to patients without clinically detectable metastases. In line with this, we observed that the protein levels of S100A9 and S100A12 in plasma were higher in patients with advanced disease. Importantly, in patients with metastases at diagnosis, high monocyte count and high levels of S100A9 and S100A12 were significantly associated with short progression free survival (PFS) after androgen deprivation therapy (ADT). High monocyte count and S100A9 levels were also associated with short cancer-specific survival, with monocyte count providing independent prognostic information. These findings indicate that circulating levels of monocytes, as well as S100A9 and S100A12, could be biomarkers for metastatic prostate cancer associated with particularly poor prognosis.
Keywords: prostate cancer, metastases, monocytes, S100A9, S100A12, peripheral blood mononuclear cells
1. Introduction
Prostate tumors are heterogeneous and with an unpredictable outcome, ranging from tumors causing no symptoms to aggressive, metastatic and deadly disease. Today, serum levels of prostate specific antigen (PSA), Gleason score of prostate cancer biopsies, and TNM stage are all used for prostate cancer diagnosis and prognosis [1,2]. However, in many patients these methods have limited ability to predict disease aggressiveness. New biomarkers are therefore urgently needed to improve risk stratification, preferably involving non-invasive procedures.
Several studies show presence of inflammatory cells in prostate cancer and suggest that macrophages potentiate prostate cancer progression [3,4,5,6]. In addition, high levels of macrophages in prostate biopsies are associated with prostate cancer progression after hormonal therapy [7]. Previous studies have also shown that systemic inflammation, measured by combining C-reactive protein and albumin, is associated with excess risk of death from prostate cancer [8]. This suggests that inflammatory cells and inflammatory markers in the circulation could have prognostic value.
S100A9 and S100A12 are calcium binding proteins that belong to a subgroup of S100 proteins called calgranulins or myeloid related protein, having several extra- and intracellular functions [9,10]. S100A9 and S100A12 are mainly expressed by neutrophils, monocytes, and activated macrophages and are thus linked to innate immune functions and inflammation [9,11,12,13]. S100A12 mainly acts as a functional homodimer in contrast to S100A9 that can be present as a homodimer or in a complex with S100A8 [11,13]. S100A9 and S100A12 mediate their effect by interacting with cell surface molecules such as Toll-like receptor 4 (TLR4) and receptor for advanced glycation end-product (RAGE) [14,15,16].
In addition to inflammatory cells, S100 proteins have also been detected in tumor cells in many types of cancers, such as breast, lung, bladder, kidney, thyroid, gastric, colorectal and oral, suggesting a possible role in inflammation-associated carcinogenesis [11,17].
There is sparse information regarding S100A12 and cancer, with no studies on S100A12 and prostate cancer to our knowledge. However, high stromal expression of S100A12 in hepatocellular cancer is associated with poor patient outcome [18], and a recent study shows that S100A12 expression in tissues of glioma patients is correlated to tumor grade and size [19]. Upregulation of S100A9, on the other hand, seems associated with tumor progression and metastasis in most cancer forms [11,17,20]. In line with this, we have previously shown that high density of S100A9 positive inflammatory cells in prostate cancer stroma is associated with poor outcome [21]. High S100A9 in prostate tumors is also associated with biochemical recurrence [22]. High protein and mRNA expression of S100A9 are also reported for prostate cancer tissue compared to surrounding benign tissue, and in high-grade compared to low-grade cancers [23].
In this study, we were interested to see if similar information could be gained from blood sample analysis. A previous study analyzing circulating S100A9 protein levels in serum showed higher levels of S100A9 in prostate cancer patients compared to healthy men [23]. Another study showed contradictive results and could not detect any difference in plasma levels of S100A9 between prostate cancer patients with different risk profiles and controls [24], thus confirming the need for further evaluation. Moreover, studies of mRNA expression signatures in whole blood from patients with castration resistant prostate cancer (CRPC) have indicated that a dysfunctional immune system might be a key factor in determining poor prognosis [25,26,27].
In this prospective study, the aim was to evaluate the level distribution of S100A9 and S100A12 in peripheral blood mononuclear cells (PBMCs) and its prognostic value in prostate cancer patients. As monocytes could be a source of S100 proteins in PBMCs, we also analyzed the prognostic value of the monocyte count by themselves and in relation to S100A9 and S100A12.
Here we show that high expression of S100A9 and S100A12 and a high monocyte count are associated with poor outcome in patients with metastases at diagnosis.
2. Materials and Methods
2.1. Patient Samples
Within Uppsala-Umea Comprehensive Cancer Consortium (U-CAN) [28], patients diagnosed with prostate cancer were recruited and a written consent was signed. The study was approved by the Ethical Committee (Dnr 2013-57-31M), Umeå University, Sweden.
Blood samples were prospectively collected at time for diagnosis between the years 2013–2016, and before any treatment. In total, 121 patients representing different stages of the disease were included in the study. Two patients were excluded due to low RNA concentration, leaving a total of 119 patient samples for inclusion in the mRNA analysis together with 15 samples voluntarily donated from un-matched healthy men. Patients were defined to have low risk (LR), intermediate risk (IR), high risk (HR) or metastatic disease (M1) at diagnosis, according to Gleason score, TNM stage and serum PSA levels [29], as specified in Table 1. Bone scan was performed to evaluate M1 stage.
Table 1.
Clinical characteristics of prostate cancer patients.
| Clinical Parameter | Low Risk (LR) | Intermediate Risk (IR) | High Risk (HR) | Metastasis (M1) |
|---|---|---|---|---|
| Number of patients | 15 | 32 | 42 | 30 |
| Age at first sample, median (quartiles) years | 66 (59–69) | 68 (62–72) | 70 (67–73) | 67 (63–79) |
| Initial PSA, median (quartiles) µg/L | 6.2 (4.7–6.8) | 5.3 (4.3–9.5) | 28.5 (21–51) | 193 (98–372) |
| Risk group * | ||||
| 1: T 1–2 and GS < 7 and PSA < 10 µg/L | 15 | |||
| 2: T 1–2 and/or GS 7 and/or 10 ≤ PSA < 20 µg/L | 32 | |||
| 3a: T 1–2 and/or GS 8–10 and/or 20 ≤ PSA < 50 µg/L | 17 | |||
| 3b: T 3 and/or PSA < 50 µg/L | 10 | |||
| 4: T 4 and/or N1 and/or 50 ≤ PSA < 100 µg/L and M0 | 10 | |||
| 4b: PSA ≥ 100 µg/L and M0 | 5 | |||
| 5: Metastasis # | 30 |
* Risk groups were defined according to Gleason score (GS), TNM stage and serum prostate specific antigen (PSA) levels [29]. # Positive scintigraphy or bone scan at diagnosis.
M1 patients (n = 30) were subjected to androgen deprivation therapy (ADT) and followed over time with time for PSA progression and death noted until last follow up in January 2020. PSA progression was determined according to the PCWG2 criteria [30] with PSA ≥ 2 ng/mL and a 25% increase from nadir. At first routine clinical follow-up within approximately 3 months (median: 98 days, quartiles: 70–124 days), new blood samples were collected in 24 cases.
2.2. Sample Preparation
Whole blood was collected in EDTA tubes and centrifuged within two hours as previously described [31]. The plasma was frozen in −80 degrees Celsius and saved for later analysis. Peripheral blood mononuclear cells (PBMCs) were isolated from the remaining blood sample by Lymphoprep density gradient centrifugation (Nycomed). The PBMCs were washed in PBS and 7 × 106 cells were used for flow cytometry analyses (BD LSRII, BD Biosciences, Franklin Lakes, NJ, USA) and the remaining PBMCs were frozen in RNA-later (Qiagen) for RT-PCR analysis.
2.3. RNA Preparation
Isolation of total RNA from PBMCs was performed using RNeasy plus mini kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions and quantified with Nanodrop spectrophotometer (Thermo Scientific, Waltham, MA, USA). The RNA integrity was determined using Agilent 2100 BioAnalyzer (Agilent, Santa Clara, CA, USA).
2.4. qRT-PCR Analyses
The Superscript VILO cDNA Synthesis kit (Invitrogen, Carlsbad, CA, USA) was used for converting 420 ng total RNA to cDNA. In this initial study we analyzed the expression of S100A9 (QT00018739) and S100A12 (QT00005635) by using Quantitec Primer Assays (Qiagen, Hilden, Germany). The primers were evaluated with melting curves to ensure one PCR-product. RT-PCR reactions were performed on a TaqMan 7900HT (Applied Biosystems, Life Technologies, Carlsbad, CA, USA). Samples were analyzed in duplicate and coefficient of variance (CV) between the samples was calculated, with a mean of 3.51%. Relative gene expression was determined using the comparative Ct method, with RPL13 (QT00067963) and GAPDH (QT00079247) (Qiagen) as standard reference genes, as described in the Applied Biosystems user bulletin [32]. On every plate a standard sample from the laboratory was used for interplate calibration.
2.5. Flow Cytometry Analysis
Flow cytometry was used to analyze CD14 positive monocytes. In total, 112 samples before treatment together with 15 samples from healthy men were analyzed. Extracted PBMCs were washed in FACS medium (PBS containing 3% bovine calf serum and 0.05% sodium azide) and incubated with Human TruStain FcXTM (BioLegend, San Diego, CA, USA) for 10 min at room temperature to block Fc receptors. PBMCs were then stained with anti-CD14-fluorescein isothiocyanate (FITC) (clone M5E2, BD Biosciences) on ice for 30 min in round-bottom 96-well plates. Isotype-matched irrelevant Ab was used as a negative control. After washing in FACS medium, staining was determined by flow cytometry (BD LSRII; BD Biosciences). Data was analyzed with FACSDiva software (BD Biosciences) after gating on the monocyte and lymphocyte population in the FSC/SSC window, followed by elimination of the doublets based on FSC-W/FSC-H and SSC-W/SSC-H parameters and then examine CD14 positive cells in the FL1/FSC window. Data from 100,000 gated events was collected and are represented as the percentage of positive cells. To calculate monocytes per ml blood, percent CD14 positive cells were multiplied with total number of PBMCs per mL.
2.6. Plasma Analyses
Protein profiling of plasma samples from 96 patients (Table S1) and ten healthy controls had been previously performed by 384-plex antibody bead array analysis (Plasma Profiling Facility, SciLifeLab, Stockholm, Sweden) and panels of proximity extension assays (Olink Proteomics, Uppsala, Sweden). Here, data for S100A9 (HPA004193 on bead array) and S100A12 (EN-RAGE on Olink Inflammation panel) were retrieved and expressed as relative levels, while the comprehensive data will be presented elsewhere.
2.7. Statistical Analyses
Statistical analyses were performed using SPSS Statistics 27 (SPSS Inc., Chicago, IL, USA). The non-parametric Kruskal–Wallis H test was used for multiple comparisons. The non-parametric Mann–Whitney U test (continuous variables) and Fisher’s exact test (categorical variables) were used to compare differences between groups. Bivariate correlations were calculated using Spearman’s rank correlation test. The pairwise Wilcoxon rank sum test was used when comparing samples at diagnosis with samples 3 months after ADT treatment. Kaplan–Meier survival analysis was used to estimate cancer-specific survival and progression-free survival (PFS) after ADT treatment with the log-rank test for univariate comparison and Cox proportional hazard model for multivariate analysis. Survival was defined as the time in months between the date of diagnosis to the date of last follow-up (January 2020) or to the date of an event (PSA progression or prostate cancer specific death). Median S100A9 (0.935) and S100A12 (0.940) values were used as cutoff values to define high and low mRNA expression and median monocyte count (22.1 × 104/mL blood) was used as cutoff to define high and low monocyte count. All statistical analyses were two-sided and p-values ≤ 0.05 were considered statistically significant.
3. Results
3.1. Prostate Cancer Patients with Metastases Show High Levels of S100A9 and S100A12
This prospective study included a total of 121 prostate cancer patients that were defined to have low risk (LR), intermediate risk (IR), high risk (HR) or metastatic (M1) disease, according to Gleason score, TNM stage and serum PSA levels (Table 1) [29].
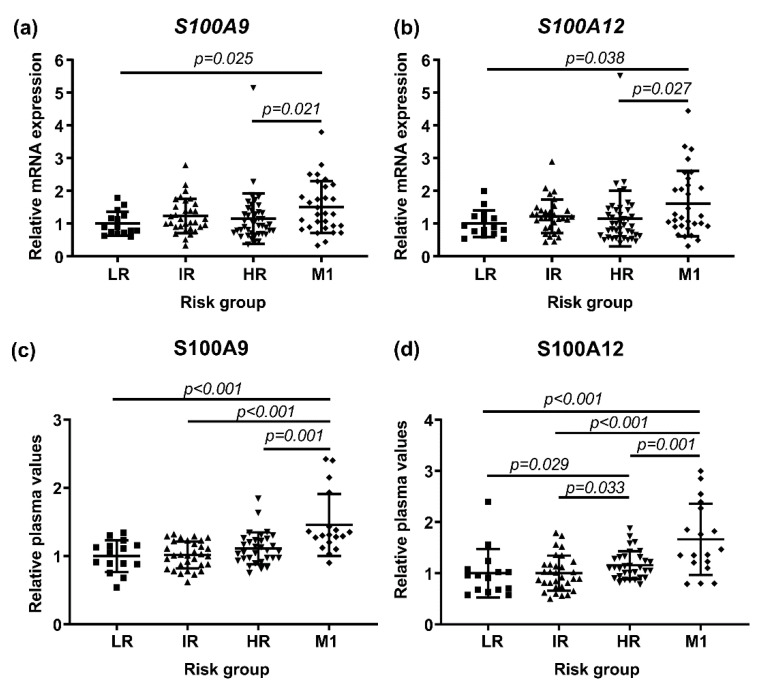
PBMCs were isolated from peripheral blood sampled at diagnosis of untreated patients and were characterized by RT-PCR for the expression of S100A9 and S100A12 in relation to patient risk group. Patients with diagnosed metastases had higher mRNA levels of S100A9 and S100A12 compared to the other risk groups (Figure 1a,b). Interestingly, these M1 patients had significantly higher expression of S100A9 and S100A12 compared to high risk patients without clinically detectable metastases (Figure 1a,b). Of note, S100A9 and S100A12 levels in LR, IR or HR patients were not significantly different compared to healthy men (n = 15) (Kruskal–Wallis; p = 0.063).
Figure 1.
Evaluation of S100A9 and S100A12 according to patient risk group at diagnosis, stratified as low risk (LR), intermediate risk (IR), high risk (HR) and metastasis (M1). Shown are the relative mRNA levels of S100A9 (a) and S100A12 (b) in PBMCs; LR (n = 15), IR (n = 32), HR (n = 42), M1 (n = 30) and relative plasma protein levels of S100A9 (c) and S100A12 (d); LR (n = 15), IR (n = 31), HR (n = 32) and M1 (n = 18). Each dot represents one individual and horizontal bars indicate mean values with standard deviation. Group comparisons were performed using Kruskal–Wallis followed by the Mann–Whitney U test. Significant p-values from the Mann–Whitney U tests are indicated.
Plasma samples from a majority of the patients (Table S1) had been previously analyzed for broad protein profiling (unpublished), and data was now retrieved for S100A9 and S100A12. The plasma protein analyses showed similar results as the RNA analyses with significantly higher levels of S100A9 and S100A12 in patients with metastases compared to high risk patients without metastases (Figure 1c,d). The mRNA expression of S100A9 and S100A12 in PBMCs were correlated to each other and to their corresponding plasma protein levels (Table 2). However, the S100A9 and S100A12 levels were not correlated with age, Gleason score or PSA at diagnosis (Table 2).
Table 2.
Bivariate correlations.
| Variable | S100A9 mRNA | S100A12 mRNA | ||||
|---|---|---|---|---|---|---|
| r | n | r | n | |||
| mRNA S100A12 | 0.879 | ** | 119 | |||
| Gleason score | 0.031 | 119 | 0.063 | 119 | ||
| Initial PSA | 0.101 | 119 | 0.055 | 119 | ||
| Age | −0.097 | 119 | −0.087 | 119 | ||
| Plasma S100A9 | 0.307 | ** | 94 | 0.322 | ** | 94 |
| Plasma S100A12 | 0.162 | 94 | 0.222 | * | 94 | |
| Monocyte count | 0.239 | * | 112 | 0.258 | ** | 112 |
Spearman’s rank correlation test. Data used in the correlation analyses was collected at the time of blood sampling before any treatment. Abbreviations: r, correlation coefficient; n, numbers; PSA, prostate specific antigen. * p < 0.05 (2-tailed). ** p < 0.01 (2-tailed).
The percentage of CD14 positive cells was analyzed by flow cytometry and calculated as monocytes per ml blood (monocyte count). The S100A9 and S100A12 mRNA levels were positively correlated with monocyte count, suggesting that monocytes could be a source of these factors (Table 2). No significant correlations were found between monocyte count and plasma protein levels of S100A9 (r = 0.125, p = 0.245) or S100A12 (r = 0.195, p = 0.067). Furthermore, no significant difference in monocyte count was found between the prostate cancer risk groups (LR, 14.3–34.0; IR, 10.6–31.0; HR, 10.3–25.8; M1, 12.1–34.0, 25–75 percentiles, Kruskal–Wallis; p = 0.658), although all prostate cancer patient risk groups had significantly higher monocyte count compared to healthy men (2.8–11.1, 25–75 percentiles, Mann–Whitney U; p < 0.001 compared to each respective group).
Taken together this suggests that S100A9 and S100A12 levels in blood could be markers of metastatic disease.
3.2. High Expression of S100A9 and S100A12 and a High Monocyte Count Are Associated with Poor Outcome in Patients with Metastases
We further examined S100A9 and S100A12 mRNA levels and monocyte count in relation to outcome in patients with metastases at diagnosis (n = 30). Outcome was analyzed based on two clinical endpoints; PSA progression after treatment with ADT or prostate cancer-specific death, with 22 patients having PSA progression and 11 patients dying from prostate cancer during the study period. Due to the low number of metastatic patients (n = 18, Table S1) we did not analyze the plasma protein levels of S100A9 and S100A12 in relation to outcome.
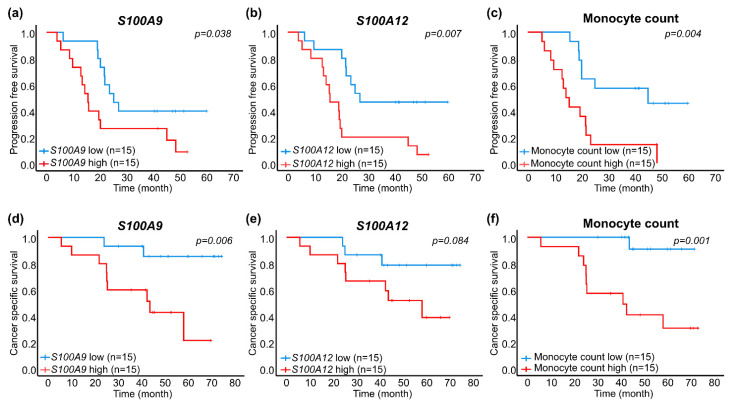
Kaplan–Meier survival analysis with the log-rank test showed that patients with high mRNA expression (>median value) of S100A9, S100A12 or a high monocyte count (>median value) had significantly shorter progression free survival than patients with low expression or low count (≤median value) (Figure 2a–c). Importantly, patients with high S100A9 expression or a high monocyte count had significantly reduced cancer-specific survival compared to patients with low expression or low count (Figure 2d,f). A trend for reduced cancer-specific survival was also seen in patients of S100A12 (Figure 2e).
Figure 2.
Kaplan–Meier survival analysis of patients in the metastatic group based on low (blue line) and high (red line) S100A mRNA expression and monocyte count, grouped by median values as cut off. Shown is PSA progression-free survival for S100A9 (a), S100A12 (b) and monocyte count (c), and prostate cancer-specific survival for S100A9 (d), S100A12 (e) and monocyte count (f).
In univariate Cox regression analysis, a high mRNA expression of S100A12 was associated with increased relative risk for PSA progression (Table 3). S100A9 and a high monocyte count were associated with increased relative risk for both PSA progression and prostate cancer-specific death (Table 3). Age, PSA at diagnosis or Gleason score were not significantly associated with progression free or cancer-specific survival in the M1 patients (Table 3).
Table 3.
Cox regression analysis of specified markers in relation to PSA progression-free survival and prostate cancer-specific survival after androgen deprivation therapy of patients with metastases.
| PSA Progression | PC Specific Death | |||||
|---|---|---|---|---|---|---|
| Variable | HR | 95% CI | p-Value | HR | 95% CI | p-Value |
| (A) Univariate analyses | ||||||
| S100A9 mRNA | 2.4 | 1.0–5.7 | 0.045 | 6.7 | 1.4–32 | 0.016 |
| S100A12 mRNA | 3.2 | 1.3–7.9 | 0.010 | 3.1 | 0.8–12 | 0.100 |
| Monocyte count | 3.6 | 1.4–9.2 | 0.007 | 14 | 1.8–110 | 0.013 |
| Age | 1.0 | 1.0–1.1 | 0.186 | 1.1 | 1.0–1.1 | 0.059 |
| Gleason Score | 1.2 | 0.7–2.0 | 0.548 | 1.5 | 0.7–3.2 | 0.293 |
| PSA | 1.0 | 1.0–1.0 | 0.537 | 1.0 | 1.0–1.0 | 0.438 |
| (B) Multivariate analysis | ||||||
| S100A9 mRNA | 2.2 | 0.9–5.4 | 0.103 | 3.8 | 0.8–18 | 0.099 |
| Monocyte count | 3.4 | 1.3–8.7 | 0.011 | 10 | 1.2–82 | 0.031 |
| (C) Multivariate analysis | ||||||
| S100A12 mRNA | 2.9 | 1.1–7.6 | 0.027 | |||
| Monocyte count | 3.3 | 1.3–8.5 | 0.012 | |||
The S100A9, S100A12 mRNA levels and monocyte count were dichotomized by their median values and analyzed as categorical variables. Age, Gleason score and PSA were analyzed as continuous variables. Abbreviations: HR, hazard ratio; CI, confidence interval; PC, prostate cancer; PSA, prostate specific antigen.
In multivariate Cox regression analyses, only monocyte count remained significantly associated with increased risk of dying from prostate cancer in men with metastatic disease (Table 3). However, due to the small number of patients/events, all three factors could be important prognostic markers for metastatic prostate cancer and deserve to be further validated in larger patient’s cohorts.
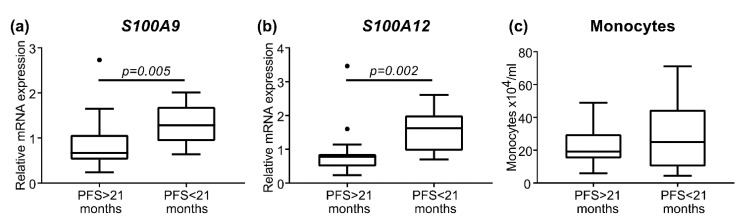
The median time to PSA progression in the metastatic group was 21 months. Using 21 months as a cut off value, the patients were subdivided in short progression free survival (PFS < 21 months) and long progression free survival (PFS > 21 months), with 15 patients in each group (Table 4). There was a significant difference in S100A9 and S100A12 mRNA expression between the groups of short respective long progression free survival (Figure 3). In contrast, monocyte count was not significantly different between the groups (Figure 3). Moreover, the patients with long or short progression free survival differed in relation to overall survival, but not age, PSA, Gleason score or if patients had received early complementary chemotherapy (Table 4). This further indicates S100A9 and S100A12 mRNA expression as therapy-predictive factors for metastatic patients treated with ADT.
Table 4.
Detailed clinical characteristics of metastatic prostate cancer patients treated with androgen deprivation therapy.
| Clinical Parameter | Long PFS | Short PFS | p-Value |
|---|---|---|---|
| Number of patients | 15 | 15 | |
| PSA progression at last follow-up, n | 7/15 (47%) | 15/15 (100%) | |
| Age, median (quartiles) years | 67 (65–76) | 66 (61–80) | 0.678 * |
| PSA at baseline, median (quartiles) µg/L | 233 (91–330) | 144 (115–391) | 0.917 * |
| Gleason Score (Min-Max) | 7–10 | 7–10 | 0.466 # |
| Median time to PSA progression, (quartiles) months | 42 (25–49) | 14 (8.7–19) | <0.0001 * |
| Median time to death, (quartiles) months | 53 (42–71) | 41 (25–45) | 0.011 * |
| Docetaxel prior to PSA progression, n | 3 | 2 | 1.000 # |
| Treatment post PSA progression | |||
| Docetaxel, n | 2 | 3 | |
| Abiraterone, n | 2 | 2 | |
| Bicalutamide or Enzalutamide, n | 3 | 7 | |
| Radium-223, n | 1 | ||
| No treatment, n | 2 |
Abbreviations: PFS, PSA progression-free survival after androgen deprivation therapy; n, numbers. Data are divided according to median time to PSA progression, long PFS > 21 months and short PFS < 21 months. * p-value obtained using Mann–Whitney test. # p-value obtained using Fisher test.
Figure 3.
Short progression free survival (PFS < 21 months, n = 15) compared to long progression free survival (PFS > 21 months, n = 15) for patients with metastases at diagnosis. The relative gene expression levels of S100A9 (a) and S100A12 (b), and monocyte count (c) are illustrated by box plots. Outlier values (o) and significant p-values from the Mann–Whitney U tests are indicated.
Taken together, this shows that high levels of S100A9, S100A12 and high monocyte count in blood are associated with a particularly bad outcome in patients with prostate cancer metastases.
3.3. Expression of S100A9 Decreases after Treatment
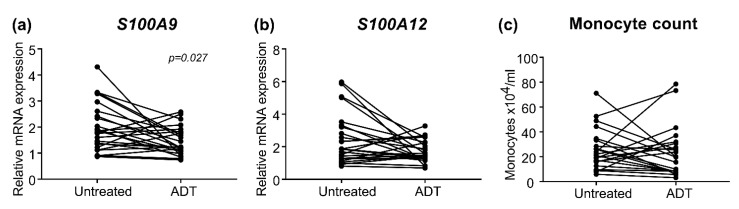
To evaluate if ADT affected the mRNA expression levels of S100A9 and S100A12 or monocyte count, we analyzed blood samples collected from M1 patients (n = 24) approximately three months (median: 98 days, quartiles: 70–124 days) after treatment.
Significantly reduced S100A9 levels were seen in M1 patients treated with ADT (Figure 4a). However, the decrease in S100A9 levels after ADT treatment was not correlated with PFS (r = −0.099, p = 0.646) or prostate cancer-specific death (r = −0.082, p = 0.704). Similar trends were seen for S100A12 and monocyte levels, although not reaching significance (Figure 4b,c).
Figure 4.
Evaluation in patients with metastases of (a) S100A9 and (b) S100A12 relative mRNA levels and (c) monocyte count in paired samples at diagnosis (untreated) and after approximately 3 months of androgen deprivation therapy (ADT). Wilcoxon rank sum test was used to compare samples from untreated metastatic patients at diagnosis with paired samples after ADT treatment. Significant p-values are shown.
4. Discussion
In this prospective study, we have examined monocyte count and mRNA expression of S100A9 and S100A12 in PBMCs as well as corresponding circulating protein levels in blood samples from prostate cancer patients, and report higher levels in patients with metastases compared to high-risk patients without metastases. Importantly, in patients with metastases at diagnosis, high monocyte count and high mRNA levels of S100A9 and S100A12 are associated with short PSA progression-free time after ADT. Monocyte count and S100A9 levels are also associated with short prostate cancer-specific survival, with monocyte count providing independent prognostic information. Furthermore, we show that metastatic patients that had early PSA progression (<21 months) had higher expression of both S100A9 and S100A12 compared to patients that progressed later (>21 months). These findings should be validated in a larger cohort of metastatic prostate cancer patients.
We show that mRNA expression of both S100A9 and S100A12 was positively correlated with monocyte count, suggesting that a population of monocytes could be one source of these proteins in PBMCs. In line with S100A9 and S100A12, high blood monocyte count was shown to be associated with shorter PFS and cancer-specific survival in patients with metastases. Consistent with this, peripheral monocyte count has previously been shown as an independent prognostic biomarker for prostate cancer [33]. The absolute number of monocytes in peripheral blood has also been associated with survival in patients with B cell lymphoma [34] and locally advanced cervical cancer [35]. Furthermore, it was recently shown that monocyte subpopulation distribution and transcriptomes are significantly changed by the presence of endometrial or breast cancers and could reflect patient outcomes [36].
Taken together, our results suggest that analysis of monocytes or expression levels of S100A9 or S10012 in a blood sample could provide additive prognostic information for prostate cancer patients with metastases at diagnosis. In this group of patients, baseline PSA levels did not show any significant relation to patient outcome. Metastatic patients are in urgent need of novel treatments and high levels of S100A9, S100A12 and monocytes in blood may not only identify patients in need of complementary therapies to ADT, but possibly also identify patients who would benefit from therapies affecting monocytes/macrophages and/or therapies targeting S100A9 or S10012 directly. Further studies to test these hypotheses are warranted.
The S100A9 inhibitor tasquinimod showed promising results in a phase 2 randomized controlled trial (n = 201), by improving both PFS and overall survival (OS) for metastatic CRPC (mCRPC) patients [37]. Inconsistent with these findings, a phase 3 randomized controlled trial (n = 1245) in men with chemotherapy-naïve mCRPC demonstrated that tasquinimod significantly improved radiographic PFS but did not improve OS [38]. In both these studies, tasquinimod was administrated to mCRPC patients blindly without selection of patients based on their S100A9 expression. Here we identified a group of patients with metastases that had high expression of S100A9, S100A12 and monocytes in blood, suggesting that this group of patients would likely respond better to tasquinimod or other treatments targeting this system. In relation to this, recent studies demonstrated that the frequency of peripheral blood monocytes in patients with melanoma, was associated with response to anti-CTLA-4 immune checkpoint blockade (ipilimumab) [39] and anti-PD-1 treatment [40].
We did not confirm if the levels of S100A9, S100A12 and monocytes in blood reflected an inflammatory profile in the prostate cancer tissue, but this is not unlikely. We have previously shown that S100A9 expression is detected in CD68 positive macrophages in the prostate tumor stroma and in the non-malignant prostate stroma adjacent to prostate tumors, suggesting monocytes/macrophages as a plausible source of S100A9 also in tumors [21]. Moreover, peripheral blood monocyte count has previously been correlated with the number of tumor-infiltrating macrophages [41]. However, prostate cancer cells and other cells, such as neutrophils and mast cells, have also been shown to express S100A9 [11,23,42,43]. Contribution of S100A9 and S100A12 from other cell types than PBMCs to the blood is therefore also likely and could explain the relatively low correlations between protein and mRNA levels for S100A9 and S100A12.
Moreover, we have previously shown that both S100A9 and CD68 positive macrophages are associated to poor outcome in PC patients [6,21]. We have also demonstrated that macrophages infiltrating PC are mainly of an M2 type (CD163+) and correlates with a more aggressive tumor and poor patient prognosis [3]. In experimental models, depletion of extratumoral macrophages/monocytes [44] and decreased S100A9 expression [45,46] inhibited prostate tumor growth. Taken together this shows the importance of macrophages in prostate tumor progression.
In this study, high monocyte count was associated with poor outcome in patients with metastases at diagnosis, suggesting that macrophages may be important for metastatic growth. We have previously shown that heme oxygenase-1 (HO-1)-positive macrophages are abundant in prostate bone metastases and at higher levels than in primary tumors [47]. Moreover, we have shown that infiltration of CD68 positive monocytes is higher in non-androgen receptor (AR)-driven CRPC bone metastases than in AR-driven, suggesting subgroups of metastases with a higher immune infiltration than others [48]. A recent study also demonstrated a progressive increase in mannose receptor-positive macrophages from normal prostate tissue to mCRPC [49]. Collectively, this indicates that monocyte count in blood could reflect the inflammatory profile in prostate cancer metastases.
Nevertheless, the inflammatory changes detected in blood in this study could also be due to systemic effects induced by metastatic disease that are unrelated to the levels within the tumors. More studies are needed to understand the mechanisms behind as well as the effects of the increased levels seen for circulating monocytes and expression of S100A9 and S100A12 in PBMCs in prostate cancer patients with particularly poor prognosis.
Furthermore, we show that S100A9 expression in PBMCs was significantly decreased in M1 patients after ADT. The mechanism for this is unknown but indicate that ADT could directly or indirectly lower the inflammatory activity. However, no significant effect on the levels of S100A12 or monocytes were found and the decrease in S100A9 levels after ADT treatment was small and not correlated with outcome, hence not associated with response to treatment at the measured time-point. If S100A9 expression change when prostate metastases become castration resistant needs to be further examined.
5. Conclusions
This is the first study showing that high blood monocyte count and high mRNA expression of S100A9 or S100A12 in PBMCs are associated with particularly poor outcome in patients with prostate cancer metastases, with monocytes providing independent prognostic information. Our results suggest that monocytes or the circulating levels of S100A9 or S10012 could be analyzed to give prognostic information for prostate cancer patients diagnosed with metastases, and possibly also to identify patients in need of complementary treatment to the conventional androgen-deprivation therapy. However, the study is limited by the low number of patients included, and further studies to test these hypotheses are warranted.
Acknowledgments
The authors are grateful to all the patients who participated in the study. We thank Lars Rönnlund and Kerstin Almroth for their work with patient and sample inclusion.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/cancers13102424/s1, Table S1: Clinical characteristics of prostate cancer patients analyzed for plasma protein levels of S100A9 and S100A12.
Author Contributions
Conceptualization, P.W. and M.L.; methodology, A.-M.Å., E.T., P.W. and M.L.; formal analysis, A.-M.Å., S.H.B., P.W. and M.L.; investigation, A.-M.Å., E.T., L.-A.T.-K.-F. and M.L.; data curation, A.-M.Å., E.T., C.T.-K., A.B., P.W. and M.L.; writing—original draft preparation, A.-M.Å., S.H.B. and M.L.; writing—review and editing, A.-M.Å., S.H.B., E.T., L.-A.T.-K.-F., J.A.N., A.W., C.T.-K., A.B., P.W. and M.L.; visualization, A.-M.Å., S.H.B. and M.L.; project administration, M.L.; funding acquisition, P.W. and M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from U-CAN; Prostate Cancer Foundation; the Swedish Foundation for Strategic Research, RB13-0119; the Swedish Cancer Society, CAN 2018/863; the Swedish Research Council, 2018-02594; and the Cancer Research Foundation in Northern Sweden, CFF AMP 16-834. The funders had no role in study design, data collection, analysis and interpretation of the data.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Umeå University (approval number 2013-57-31 M).
Informed Consent Statement
Written informed consent has been obtained from the patients involved in the study.
Data Availability Statement
Data are not publically availble due to Swedish law, GDPR restrictions for clinical data.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Damber J.E., Aus G. Prostate cancer. Lancet. 2008;371:1710–1721. doi: 10.1016/S0140-6736(08)60729-1. [DOI] [PubMed] [Google Scholar]
- 2.Gleason D.F., Mellinger G.T. Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J. Urol. 1974;111:58–64. doi: 10.1016/S0022-5347(17)59889-4. [DOI] [PubMed] [Google Scholar]
- 3.Lundholm M., Hagglof C., Wikberg M.L., Stattin P., Egevad L., Bergh A., Wikstrom P., Palmqvist R., Edin S. Secreted Factors from Colorectal and Prostate Cancer Cells Skew the Immune Response in Opposite Directions. Sci. Rep. 2015;5:15651. doi: 10.1038/srep15651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strasner A., Karin M. Immune Infiltration and Prostate Cancer. Front. Oncol. 2015;5:128. doi: 10.3389/fonc.2015.00128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Velasco M.A., Uemura H. Prostate cancer immunotherapy: Where are we and where are we going? Curr. Opin. Urol. 2018;28:15–24. doi: 10.1097/MOU.0000000000000462. [DOI] [PubMed] [Google Scholar]
- 6.Lissbrant I.F., Stattin P., Wikstrom P., Damber J.E., Egevad L., Bergh A. Tumor associated macrophages in human prostate cancer: Relation to clinicopathological variables and survival. Int. J. Oncol. 2000;17:445–451. doi: 10.3892/ijo.17.3.445. [DOI] [PubMed] [Google Scholar]
- 7.Nonomura N., Takayama H., Nakayama M., Nakai Y., Kawashima A., Mukai M., Nagahara A., Aozasa K., Tsujimura A. Infiltration of tumour-associated macrophages in prostate biopsy specimens is predictive of disease progression after hormonal therapy for prostate cancer. BJU Int. 2011;107:1918–1922. doi: 10.1111/j.1464-410X.2010.09804.x. [DOI] [PubMed] [Google Scholar]
- 8.Shafique K., Proctor M.J., McMillan D.C., Qureshi K., Leung H., Morrison D.S. Systemic inflammation and survival of patients with prostate cancer: Evidence from the Glasgow Inflammation Outcome Study. Prostate Cancer Prostatic Dis. 2012;15:195–201. doi: 10.1038/pcan.2011.60. [DOI] [PubMed] [Google Scholar]
- 9.Donato R., Cannon B.R., Sorci G., Riuzzi F., Hsu K., Weber D.J., Geczy C.L. Functions of S100 proteins. Curr. Mol. Med. 2013;13:24–57. doi: 10.2174/156652413804486214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marenholz I., Heizmann C.W., Fritz G. S100 proteins in mouse and man: From evolution to function and pathology (including an update of the nomenclature) Biochem. Biophys. Res. Commun. 2004;322:1111–1122. doi: 10.1016/j.bbrc.2004.07.096. [DOI] [PubMed] [Google Scholar]
- 11.Gebhardt C., Nemeth J., Angel P., Hess J. S100A8 and S100A9 in inflammation and cancer. Biochem. Pharm. 2006;72:1622–1631. doi: 10.1016/j.bcp.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 12.Goyette J., Geczy C.L. Inflammation-associated S100 proteins: New mechanisms that regulate function. Amino. Acids. 2011;41:821–842. doi: 10.1007/s00726-010-0528-0. [DOI] [PubMed] [Google Scholar]
- 13.Perera C., McNeil H.P., Geczy C.L. S100 Calgranulins in inflammatory arthritis. Immunol. Cell Biol. 2010;88:41–49. doi: 10.1038/icb.2009.88. [DOI] [PubMed] [Google Scholar]
- 14.Bjork P., Bjork A., Vogl T., Stenstrom M., Liberg D., Olsson A., Roth J., Ivars F., Leanderson T. Identification of human S100A9 as a novel target for treatment of autoimmune disease via binding to quinoline-3-carboxamides. PLoS Biol. 2009;7:e97. doi: 10.1371/journal.pbio.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vogl T., Tenbrock K., Ludwig S., Leukert N., Ehrhardt C., van Zoelen M.A., Nacken W., Foell D., van der Poll T., Sorg C., et al. Mrp8 and Mrp14 are endogenous activators of Toll-like receptor 4, promoting lethal, endotoxin-induced shock. Nat. Med. 2007;13:1042–1049. doi: 10.1038/nm1638. [DOI] [PubMed] [Google Scholar]
- 16.Hofmann M.A., Drury S., Fu C., Qu W., Taguchi A., Lu Y., Avila C., Kambham N., Bierhaus A., Nawroth P., et al. RAGE mediates a novel proinflammatory axis: A central cell surface receptor for S100/calgranulin polypeptides. Cell. 1999;97:889–901. doi: 10.1016/S0092-8674(00)80801-6. [DOI] [PubMed] [Google Scholar]
- 17.Salama I., Malone P.S., Mihaimeed F., Jones J.L. A review of the S100 proteins in cancer. Eur J. Surg. Oncol. 2008;34:357–364. doi: 10.1016/j.ejso.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 18.Cai H., Ye B.G., Ao J.Y., Zhu X.D., Zhang Y.Y., Chai Z.T., Wang C.H., Sun H.C. High expression of S100A12 on intratumoral stroma cells indicates poor prognosis following surgical resection of hepatocellular carcinoma. Oncol. Lett. 2018;16:5398–5404. doi: 10.3892/ol.2018.9270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu C., Liu J., Yao M., Li L., Li G. Downregulation of S100 calcium binding protein A12 inhibits the growth of glioma cells. BMC Cancer. 2020;20:261. doi: 10.1186/s12885-020-06768-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ichikawa M., Williams R., Wang L., Vogl T., Srikrishna G. S100A8/A9 activate key genes and pathways in colon tumor progression. Mol. Cancer Res. 2011;9:133–148. doi: 10.1158/1541-7786.MCR-10-0394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tidehag V., Hammarsten P., Egevad L., Granfors T., Stattin P., Leanderson T., Wikstrom P., Josefsson A., Hagglof C., Bergh A. High density of S100A9 positive inflammatory cells in prostate cancer stroma is associated with poor outcome. Eur. J. Cancer. 2014;50:1829–1835. doi: 10.1016/j.ejca.2014.03.278. [DOI] [PubMed] [Google Scholar]
- 22.Grebhardt S., Veltkamp C., Strobel P., Mayer D. Hypoxia and HIF-1 increase S100A8 and S100A9 expression in prostate cancer. Int. J. Cancer. 2012;131:2785–2794. doi: 10.1002/ijc.27591. [DOI] [PubMed] [Google Scholar]
- 23.Hermani A., Hess J., De Servi B., Medunjanin S., Grobholz R., Trojan L., Angel P., Mayer D. Calcium-binding proteins S100A8 and S100A9 as novel diagnostic markers in human prostate cancer. Clin. Cancer Res. 2005;11:5146–5152. doi: 10.1158/1078-0432.CCR-05-0352. [DOI] [PubMed] [Google Scholar]
- 24.Ludwig S., Stephan C., Lein M., Loening S.A., Jung K. S100A8, S100A9, and the S100A8/A9 complex in circulating blood are not associated with prostate cancer risk-A re-evaluation study. Prostate. 2007;67:1301–1307. doi: 10.1002/pros.20619. [DOI] [PubMed] [Google Scholar]
- 25.Olmos D., Brewer D., Clark J., Danila D.C., Parker C., Attard G., Fleisher M., Reid A.H., Castro E., Sandhu S.K., et al. Prognostic value of blood mRNA expression signatures in castration-resistant prostate cancer: A prospective, two-stage study. Lancet Oncol. 2012;13:1114–1124. doi: 10.1016/S1470-2045(12)70372-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ross R.W., Galsky M.D., Scher H.I., Magidson J., Wassmann K., Lee G.S., Katz L., Subudhi S.K., Anand A., Fleisher M., et al. A whole-blood RNA transcript-based prognostic model in men with castration-resistant prostate cancer: A prospective study. Lancet Oncol. 2012;13:1105–1113. doi: 10.1016/S1470-2045(12)70263-2. [DOI] [PubMed] [Google Scholar]
- 27.Wang L., Gong Y., Chippada-Venkata U., Heck M.M., Retz M., Nawroth R., Galsky M., Tsao C.K., Schadt E., de Bono J., et al. A robust blood gene expression-based prognostic model for castration-resistant prostate cancer. BMC Med. 2015;13:201. doi: 10.1186/s12916-015-0442-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glimelius B., Melin B., Enblad G., Alafuzoff I., Beskow A., Ahlstrom H., Bill-Axelson A., Birgisson H., Bjor O., Edqvist P.H., et al. U-CAN: A prospective longitudinal collection of biomaterials and clinical information from adult cancer patients in Sweden. Acta Oncol. 2018;57:187–194. doi: 10.1080/0284186X.2017.1337926. [DOI] [PubMed] [Google Scholar]
- 29.Van Hemelrijck M., Wigertz A., Sandin F., Garmo H., Hellstrom K., Fransson P., Widmark A., Lambe M., Adolfsson J., Varenhorst E., et al. Cohort Profile: The National Prostate Cancer Register of Sweden and Prostate Cancer data Base Sweden 2.0. Int. J. Epidemiol. 2013;42:956–967. doi: 10.1093/ije/dys068. [DOI] [PubMed] [Google Scholar]
- 30.Scher H.I., Halabi S., Tannock I., Morris M., Sternberg C.N., Carducci M.A., Eisenberger M.A., Higano C., Bubley G.J., Dreicer R., et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: Recommendations of the Prostate Cancer Clinical Trials Working Group. J. Clin. Oncol. 2008;26:1148–1159. doi: 10.1200/JCO.2007.12.4487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nilsson R.J., Balaj L., Hulleman E., van Rijn S., Pegtel D.M., Walraven M., Widmark A., Gerritsen W.R., Verheul H.M., Vandertop W.P., et al. Blood platelets contain tumor-derived RNA biomarkers. Blood. 2011;118:3680–3683. doi: 10.1182/blood-2011-03-344408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pfaffl M.W., Horgan G.W., Dempfle L. Relative expression software tool (REST) for group-wise comparison and statistical analysis of relative expression results in real-time PCR. Nucleic Acids Res. 2002;30:e36. doi: 10.1093/nar/30.9.e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Y.Q., Zhu Y.J., Pan J.H., Xu F., Shao X.G., Sha J.J., Liu Q., Huang Y.R., Dong B.J., Xue W. Peripheral monocyte count: An independent diagnostic and prognostic biomarker for prostate cancer—A large Chinese cohort study. Asian J. Androl. 2017;19:579–585. doi: 10.4103/1008-682X.186185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilcox R.A., Ristow K., Habermann T.M., Inwards D.J., Micallef I.N., Johnston P.B., Colgan J.P., Nowakowski G.S., Ansell S.M., Witzig T.E., et al. The absolute monocyte and lymphocyte prognostic score predicts survival and identifies high-risk patients in diffuse large-B-cell lymphoma. Leukemia. 2011;25:1502–1509. doi: 10.1038/leu.2011.112. [DOI] [PubMed] [Google Scholar]
- 35.Lee Y.Y., Choi C.H., Sung C.O., Do I.G., Huh S., Song T., Kim M.K., Kim H.J., Kim T.J., Lee J.W., et al. Prognostic value of pre-treatment circulating monocyte count in patients with cervical cancer: Comparison with SCC-Ag level. Gynecol. Oncol. 2012;124:92–97. doi: 10.1016/j.ygyno.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 36.Cassetta L., Fragkogianni S., Sims A.H., Swierczak A., Forrester L.M., Zhang H., Soong D.Y.H., Cotechini T., Anur P., Lin E.Y., et al. Human Tumor-Associated Macrophage and Monocyte Transcriptional Landscapes Reveal Cancer-Specific Reprogramming, Biomarkers, and Therapeutic Targets. Cancer Cell. 2019;35:588–602.e10. doi: 10.1016/j.ccell.2019.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Armstrong A.J., Haggman M., Stadler W.M., Gingrich J.R., Assikis V., Polikoff J., Damber J.E., Belkoff L., Nordle O., Forsberg G., et al. Long-term survival and biomarker correlates of tasquinimod efficacy in a multicenter randomized study of men with minimally symptomatic metastatic castration-resistant prostate cancer. Clin. Cancer Res. 2013;19:6891–6901. doi: 10.1158/1078-0432.CCR-13-1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sternberg C., Armstrong A., Pili R., Ng S., Huddart R., Agarwal N., Khvorostenko D., Lyulko O., Brize A., Vogelzang N., et al. Randomized, Double-Blind, Placebo-Controlled Phase III Study of Tasquinimod in Men with Metastatic Castration-Resistant Prostate Cancer. J. Clin. Oncol. 2016;34:2636–2643. doi: 10.1200/JCO.2016.66.9697. [DOI] [PubMed] [Google Scholar]
- 39.Romano E., Kusio-Kobialka M., Foukas P.G., Baumgaertner P., Meyer C., Ballabeni P., Michielin O., Weide B., Romero P., Speiser D.E. Ipilimumab-dependent cell-mediated cytotoxicity of regulatory T cells ex vivo by nonclassical monocytes in melanoma patients. Proc. Natl. Acad. Sci. USA. 2015;112:6140–6145. doi: 10.1073/pnas.1417320112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krieg C., Nowicka M., Guglietta S., Schindler S., Hartmann F.J., Weber L.M., Dummer R., Robinson M.D., Levesque M.P., Becher B. High-dimensional single-cell analysis predicts response to anti-PD-1 immunotherapy. Nat. Med. 2018;24:144–153. doi: 10.1038/nm.4466. [DOI] [PubMed] [Google Scholar]
- 41.Hayashi T., Fujita K., Nojima S., Hayashi Y., Nakano K., Ishizuya Y., Wang C., Yamamoto Y., Kinouchi T., Matsuzaki K., et al. Peripheral blood monocyte count reflecting tumor-infiltrating macrophages is a predictive factor of adverse pathology in radical prostatectomy specimens. Prostate. 2017;77:1383–1388. doi: 10.1002/pros.23398. [DOI] [PubMed] [Google Scholar]
- 42.Foell D., Wittkowski H., Vogl T., Roth J. S100 proteins expressed in phagocytes: A novel group of damage-associated molecular pattern molecules. J. Leukoc. Biol. 2007;81:28–37. doi: 10.1189/jlb.0306170. [DOI] [PubMed] [Google Scholar]
- 43.McCormick M.M., Rahimi F., Bobryshev Y.V., Gaus K., Zreiqat H., Cai H., Lord R.S., Geczy C.L. S100A8 and S100A9 in human arterial wall. Implications for atherogenesis. J. Biol. Chem. 2005;280:41521–41529. doi: 10.1074/jbc.M509442200. [DOI] [PubMed] [Google Scholar]
- 44.Halin S., Rudolfsson S.H., Van Rooijen N., Bergh A. Extratumoral macrophages promote tumor and vascular growth in an orthotopic rat prostate tumor model. Neoplasia. 2009;11:177–186. doi: 10.1593/neo.81338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jennbacken K., Welen K., Olsson A., Axelsson B., Torngren M., Damber J.E., Leanderson T. Inhibition of metastasis in a castration resistant prostate cancer model by the quinoline-3-carboxamide tasquinimod (ABR-215050) Prostate. 2012;72:913–924. doi: 10.1002/pros.21495. [DOI] [PubMed] [Google Scholar]
- 46.Kallberg E., Vogl T., Liberg D., Olsson A., Bjork P., Wikstrom P., Bergh A., Roth J., Ivars F., Leanderson T. S100A9 interaction with TLR4 promotes tumor growth. PLoS ONE. 2012;7:e34207. doi: 10.1371/journal.pone.0034207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Halin Bergstrom S., Nilsson M., Adamo H., Thysell E., Jernberg E., Stattin P., Widmark A., Wikstrom P., Bergh A. Extratumoral Heme Oxygenase-1 (HO-1) Expressing Macrophages Likely Promote Primary and Metastatic Prostate Tumor Growth. PLoS ONE. 2016;11:e0157280. doi: 10.1371/journal.pone.0157280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ylitalo E.B., Thysell E., Jernberg E., Lundholm M., Crnalic S., Egevad L., Stattin P., Widmark A., Bergh A., Wikstrom P. Subgroups of Castration-resistant Prostate Cancer Bone Metastases Defined Through an Inverse Relationship Between Androgen Receptor Activity and Immune Response. Eur. Urol. 2017;71:776–787. doi: 10.1016/j.eururo.2016.07.033. [DOI] [PubMed] [Google Scholar]
- 49.Zarif J.C., Baena-Del Valle J.A., Hicks J.L., Heaphy C.M., Vidal I., Luo J., Lotan T.L., Hooper J.E., Isaacs W.B., Pienta K.J., et al. Mannose Receptor-positive Macrophage Infiltration Correlates with Prostate Cancer Onset and Metastatic Castration-resistant Disease. Eur. Urol. Oncol. 2019;2:429–436. doi: 10.1016/j.euo.2018.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are not publically availble due to Swedish law, GDPR restrictions for clinical data.