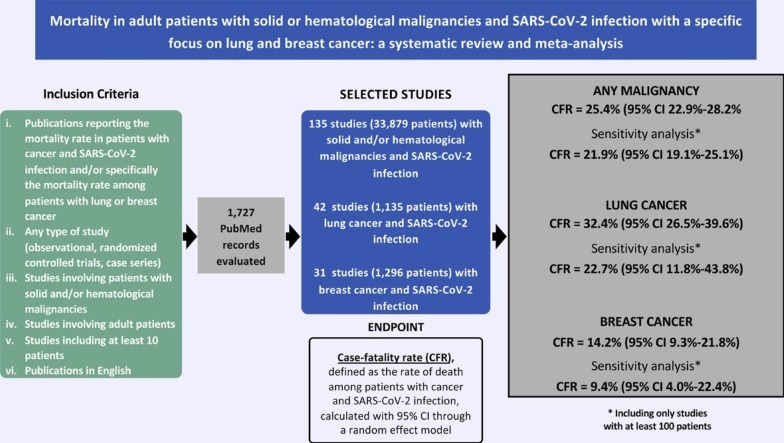
Graphical abstract
Keywords: SARS-CoV-2, COVID-19, Cancer, Tumor, Mortality, Lung cancer, Breast cancer
Abstract
Background
A systematic review and meta-analysis was performed to estimate mortality in adult patients with solid or hematological malignancies and SARS-CoV-2 infection.
Methods
A systematic search of PubMed, up to 31 January 2021, identified publications reporting the case-fatality rate (CFR) among adult patients with solid or hematological malignancies and SARS-CoV-2 infection. The CFR, defined as the rate of death in this population, was assessed with a random effect model; 95% confidence intervals (CI) were calculated.
Results
Among 135 selected studies (N = 33,879 patients), the CFR was 25.4% (95% CI 22.9%–28.2%). At a sensitivity analysis including studies with at least 100 patients, the CFR was 21.9% (95% CI 19.1%–25.1%). Among COVID-19 patients with lung (N = 1,135) and breast (N = 1,296) cancers, CFR were 32.4% (95% CI 26.5%–39.6%) and 14.2% (95% CI 9.3%–21.8%), respectively.
Conclusions
Patients with solid or hematological malignancies and SARS-CoV-2 infection have a high probability of mortality, with comparatively higher and lower CFRs in patients with lung and breast cancers, respectively.
1. Background
Since the start of the coronavirus disease 2019 (COVID-19) pandemic, the global cumulative number of cases all over the world has reached more than 108 million, with over 2.6 million cases of deaths as of March 2, 2021 (World Health Organization, 2021).
Patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and a diagnosis of cancer are at high risk of severe symptomatic disease and death (Xia et al., 2020). Several efforts have been made to prevent SARS-CoV-2 infection among patients with cancer, as well as to ensure continuity of cancer care during the pandemic (Lambertini et al., 2020; Tagliamento et al., 2020a).
Cancer has been shown to be an independent adverse prognostic factor on COVID-19-related mortality (de Azambuja et al., 2020; Saini et al., 2020). However, its effect across different patient subgroups is uncertain, and wide variability seems to exist according to different tumor types. In particular, patients with lung cancer have been reported to have disproportionally higher mortality rates from COVID-19, while those with breast cancer showed relatively lower mortality rates (Luo et al., 2020; Garassino et al., 2020; Vuagnat et al., 2020).
Since the outbreak of the pandemic, several case-series and cohort studies describing the clinical outcomes and mortality of SARS-CoV-2 infection in patients with cancer have been published. However, the relatively small sample size of most reports, their retrospective design and the restriction to hospitalized patients represent important limitations to interpret the reported mortality rates, and the extent to which they can be extrapolated to the wider population of patients with solid or hematological malignancies.
A systematic review and pooled analysis assessing the mortality rate of patients with SARS-CoV-2 infection and underlying cancer was published in 2020, but it included a relatively limited number of studies (n = 52) and did not provide pooled data on mortality according to tumor types (Saini et al., 2020). Moreover, to the best of our knowledge, no systematic review and meta-analyses focusing specifically on lung and breast malignancies are available to date.
To provide updated evidence on this important topic, we performed a systematic review and meta-analysis aiming to estimate the case-fatality rate (CFR) of patients with solid or hematological malignancies and SARS-CoV-2 infection. In addition, we also focused separately on patients with lung and breast cancers, in order to evaluate the CFR associated with these common tumors.
2. Materials and methods
2.1. Literature search
A systematic search of PubMed up to 31 January 2021 was performed by two authors (M.T. and F.P.); any disagreement was discussed among all authors and resolved. The search strategy included different combinations of terms: (covid OR coronavirus OR sars) AND (cancer OR tumor OR tumour OR tumors OR tumours OR malignancy OR malignancies OR neoplasia OR neoplasm) AND (mortality OR death). Duplicated results were not included. Only the most recent and updated version of a same study was considered.
2.2. Study selection
The following inclusion criteria were considered: i) publications reporting the mortality rate in patients with cancer and SARS-CoV-2 infection and/or specifically the mortality rate among patients with lung or breast cancers; ii) any type of study (observational, randomized controlled trials or case series); iii) studies involving patients with solid or hematological malignancies; iv) studies involving adult patients; v) studies including at least 10 patients; vi) publications in English.
2.3. Data extraction
Data extracted from every publication were: name of the first author, reported number of patients with cancer and SARS-CoV-2 infection, reported number of deaths among patients with cancer and SARS-CoV-2 infection, reported number of patients with lung cancer and SARS-CoV-2 infection, reported number of deaths among patients with lung cancer and SARS-CoV-2 infection, reported number of patients with breast cancer and SARS-CoV-2 infection, reported number of deaths among patients with breast cancer and SARS-CoV-2 infection. Data extraction was performed by two authors (M.T and E.A.).
2.4. Statistical analysis
A meta-analysis of selected studies was performed in order to assess the CRF among adult patients with solid or hematological malignancies and SARS-CoV-2 infection, defined as the cumulative rate of deaths among patients with history of malignancy and SARS-CoV-2-infection. Moreover, the mortality rates among patients with lung and breast cancers and SARS-CoV-2 infection were separately computed. A random effect model was used to assess the CFR, and 95% confidence intervals (CI) were calculated. The likelihood of publication bias was assessed by Egger’s test. The Higgins I2 index was used to assess the heterogeneity between studies. Sensitivity analyses were carried out after excluding studies including less than 100 patients.
3. Results
The systematic search of the literature returned 1,727 records. In total, 1,551 were excluded on the basis of the title and 34 based on the abstract not fulfilling the inclusion criteria, while 7 were duplicates. A total of 135 studies were selected, including 33,879 patients with solid or hematological malignancies and SARS-CoV-2 infection (Table 1 ) (Lundon et al., 2020; Liu et al., 2020; Fuentes‐Antrás et al., 2020; Wang et al., 2020a, 2021; Montopoli et al., 2020; Song et al., 2021; Huang et al., 2020; Sng et al., 2020; Li et al., 2020; Tagliamento et al., 2020a; de Melo et al., 2020; Bogani et al., 2020; Wang et al., 2020b; Cavanna et al., 2021; Rogado et al., 2020a; Mehta et al., 2020; Basse et al., 2021; Zhang et al., 2020a; Nakamura et al., 2021; Kalinsky et al., 2020; Jee et al., 2020; Engelhardt et al., 2020; Tian et al., 2020; Passamonti et al., 2020; Nie et al., 2021; Cattaneo et al., 2020; Zhang et al., 2020b; Sorouri et al., 2020; Yang et al., 2020a; Wu et al., 2020a; Sanchez‐Pina et al., 2020; Alpert et al., 2021; Deng et al., 2020; Özdemir et al., 2020; Chari et al., 2020; Rogiers et al., 2021; Aries et al., 2020; Fox et al., 2020; Wu et al., 2020b; Guan et al., 2020; Wang et al., 2020c; Piper-Vallillo et al., 2021; Stroppa et al., 2020; Rubio et al., 2020; Singh et al., 2020; Lattenist et al., 2021; Ramachandran et al., 2020; Rüthrich et al., 2021; Luo et al., 2020; Tsimafeyeu et al., 2020; Garassino et al., 2020; He et al., 2020; Breccia et al., 2020; Hultcrantz et al., 2020; Boilève et al., 2020; Lara Álvarez et al., 2020; Mehta et al., 2021; Kathuria-Prakash et al., 2021; Lee et al., 2020; Nichetti et al., 2020; Scarfò et al., 2020; Brar et al., 2020; Rogado et al., 2020b; Ali et al., 2020; Ramaswamy et al., 2020; Shoumariyeh et al., 2020; Infante et al., 2020; Angelis et al., 2020; Robilotti et al., 2020; Ferrari et al., 2021; Miyashita et al., 2020; Ciceri et al., 2020; Borah et al., 2021; Kabarriti et al., 2020; Russell et al., 2020; Gupta et al., 2020; Docherty et al., 2020; Bhogal et al., 2021; Elkrief et al., 2020; Assaad et al., 2020; Barbui et al., 2021; Hanna et al., 2021; Kvåle et al., 2020; Antrim et al., 2021; García-Suárez et al., 2020; de Azambuja et al., 2020; Caffo et al., 2020; Lee et al., 2021; Nepogodiev et al., 2020; Martínez-López et al., 2020; Lunski et al., 2021; Biernat et al., 2020; Cherri et al., 2020; COVIDSurg Collaborative et al., 2020; Ganatra et al., 2020; Mato et al., 2020; Calles et al., 2020; Duarte et al., 2020; Zhang et al., 2020c; Wood et al., 2020; Joharatnam-Hogan et al., 2020; de Oliveira et al., 2021; Thompson et al., 2020; Dai et al., 2020; Ayhan et al., 2021; Pinato et al., 2020a; Fillmore et al., 2020; Ramtohul et al., 2020; Lara et al., 2020; Sun et al., 2021; Cui et al., 2020; Cook et al., 2020; Booth et al., 2020; Grasselli et al., 2020; Lièvre et al., 2020; Yang et al., 2020b; Yarza et al., 2020; Reale et al., 2020; Laurenge et al., 2021; Pinto et al., 2020; Yu et al., 2020; Westblade et al., 2020; Glenthøj et al., 2021; Martín‐Moro et al., 2020; Wang et al., 2020d; Sadeghi et al., 2020; Morjaria et al., 2020; Erdal et al., 2021; Burn et al., 2021; Yigenoglu et al., 2021; Rivera et al., 2020; Rajasekaran et al., 2020; Wang et al., 2020e).
Table 1.
Details of reported number of patients and deaths in the studies selected for the meta-analysis.
| Author | Total patients with cancer and SARS-CoV-2 infection | Deaths in patients with cancer and SARS-CoV-2 infection | Total patients with lung cancer and SARS-CoV-2 infection | Deaths in patients with lung cancer and SARS-CoV-2 infection | Total patients with breast cancer and SARS-CoV-2 infection | Deaths in patients with breast cancer and SARS-CoV-2 infection |
|---|---|---|---|---|---|---|
| Ali et al. | 201 | 16 | ||||
| Alpert et al. | 421 | 129 | ||||
| Angelis et al. | 113 | 29 | ||||
| Antrim et al. | 50 | 5 | ||||
| Aries et al. | 35 | 14 | ||||
| Assaad et al. | 55 | 8 | 7 | 3 | ||
| Ayhan et al. | 46 | 0 | ||||
| Barbui et al. | 175 | 50 | ||||
| Basse et al. | 141 | 30 | 18 | 6 | ||
| Bhangu et al. | 78 | 15 | ||||
| Bhogal et al. | 179 | 66 | ||||
| Biernat et al. | 10 | 7 | ||||
| Bogani et al. | 19 | 3 | ||||
| Boilève et al. | 16 | 2 | ||||
| Booth et al. | 66 | 34 | ||||
| Borah et al. | 130 | 26 | ||||
| Brar et al. | 117 | 29 | ||||
| Breccia et al. | 36 | 8 | ||||
| Burn et al. | 5595 | 670 | ||||
| Caffo et al. | 34 | 13 | ||||
| Calles et al. | 23 | 8 | 23 | 8 | ||
| Cattaneo et al. | 102 | 40 | ||||
| Cavanna et al. | 51 | 25 | 12 | 7 | 4 | 2 |
| Chari et al. | 650 | 222 | ||||
| Cherri et al. | 53 | 16 | ||||
| Ciceri et al. | 22 | 11 | ||||
| Cook et al. | 75 | 41 | ||||
| COVIDSurg Collaborative | 189 | 43 | ||||
| Cui et al. | 32 | 9 | 26 | 7 | ||
| Dai et al. | 31 | 8 | 31 | 8 | ||
| Dai et al. | 105 | 12 | 22 | 4 | 11 | 0 |
| De Azambuja et al. | 832 | 283 | ||||
| de Melo et al. | 181 | 69 | 7 | 4 | 40 | 21 |
| de Oliveira et al. | 83 | 68 | 5 | 4 | 31 | 27 |
| Deng et al. | 107 | 6 | ||||
| Docherty et al. | 1743 | 617 | ||||
| Duarte et al. | 681 | 442 | 51 | 38 | 90 | 51 |
| Elkrief et al. | 249 | 71 | ||||
| Engelhardt et al. | 21 | 0 | ||||
| Erdal et al. | 77 | 17 | 7 | 1 | 11 | 1 |
| Ferrari et al. | 198 | 33 | 16 | 7 | 58 | 5 |
| Fillmore et al. | 1794 | 251 | 121 | |||
| Fox et al. | 52 | 18 | ||||
| Fuentes-Antras et al. | 73 | 18 | 14 | 5 | 10 | 4 |
| Ganatra et al. | 195 | 48 | ||||
| Garassino et al. | 200 | 66 | ||||
| García-Suárez et al. | 697 | 230 | ||||
| Glenthøj et al. | 66 | 16 | ||||
| Graselli et al. | 331 | 202 | ||||
| Guan et al. | 18 | 3 | ||||
| Gupta et al. | 112 | 60 | ||||
| Hanna et al | 32 | 7 | ||||
| He et al. | 13 | 8 | ||||
| Huang et al. | 16 | 3 | 2 | |||
| Hultcrantz et al. | 100 | 22 | ||||
| Infante et al. | 41 | 15 | ||||
| Jee et al. | 309 | 31 | ||||
| Joharatnam-Hogan et al. | 30 | 11 | 5 | 3 | 4 | 1 |
| Kabarriti et al. | 107 | 24 | ||||
| Kalinsky et al. | 27 | 1 | 27 | 1 | ||
| Kathuria-Prakash et al. | 21 | 2 | ||||
| Kvåle et al. | 372 | 36 | ||||
| Lara Álvarez et al. | 36 | 15 | ||||
| Lara et al. | 193 | 34 | ||||
| Lattenist et al. | 13 | 6 | ||||
| Laurenge et al. | 13 | 3 | ||||
| Lee L et al. | 1044 | 319 | 111 | 43 | 143 | 26 |
| Lee RJ et al. | 302 | 104 | ||||
| Li et al. | 65 | 18 | 5 | 2 | 8 | 1 |
| Lièvre et al. | 1289 | 370 | 173 | 26 | ||
| Liu et al. | 216 | 37 | 49 | 14 | 34 | 1 |
| Lundon et al. | 149 | 35 | ||||
| Lunski et al. | 312 | 66 | 26 | 8 | 70 | 8 |
| Luo et al. | 102 | 25 | 102 | 25 | ||
| Martinez-Lopez et al. | 167 | 56 | ||||
| Martín-Moro et al. | 34 | 11 | ||||
| Mato et al. | 198 | 66 | ||||
| Mehta A et al. | 218 | 61 | 11 | 6 | 28 | 4 |
| Mehta V et al. | 186 | 27 | 17 | 0 | 19 | 1 |
| Miyashita et al. | 334 | 37 | ||||
| Montopoli et al. | 430 | 75 | ||||
| Morjaria et al. | 304 | 53 | ||||
| Nakamura et al. | 32 | 11 | 2 | 1 | 2 | 0 |
| Nichetti et al. | 11 | 6 | 1 | 1 | 4 | 3 |
| Nie et al | 45 | 11 | 45 | 11 | ||
| Ozdemir et al. | 1523 | 77 | 157 | 18 | 302 | 2 |
| Passamonti et al. | 536 | 198 | ||||
| Pinato et al. | 204 | 59 | ||||
| Pinto et al. | 138 | 47 | ||||
| Piper-Valillo et al. | 24 | 7 | 24 | 7 | ||
| Rajasekeran et al. | 12 | 4 | ||||
| Ramachandran et al. | 53 | 32 | ||||
| Ramaswamy et al. | 198 | 23 | 30 | 3 | ||
| Ramtohul et al. | 70 | 17 | 11 | |||
| Reale et al. | 18 | 8 | 10 | 4 | ||
| Rivera et al. | 2186 | 357 | ||||
| Robilotti et al. | 423 | 51 | ||||
| Rogado et al. | 25 | 5 | 25 | 5 | ||
| Rogado et al. | 45 | 19 | 17 | 9 | ||
| Rogiers et al. | 110 | 18 | 17 | 4 | ||
| Rubio et al. | 28 | 9 | ||||
| Russell et al. | 156 | 34 | ||||
| Rutrich et al. | 435 | 114 | ||||
| Sadeghi et al. | 41 | 26 | ||||
| Sanchez‐Pina et al. | 39 | 14 | ||||
| Scarfò et al. | 190 | 56 | ||||
| Shoumariyeh et al. | 39 | 8 | ||||
| Singh et al. | 85 | 32 | ||||
| Sng et al. | 94 | 41 | 15 | 5 | 8 | 4 |
| Song et al. | 248 | 40 | 61 | 16 | 37 | 2 |
| Sorouri et al. | 53 | 27 | 5 | 0 | 4 | 2 |
| Stroppa et al. | 25 | 9 | 8 | 2 | 2 | 2 |
| Sun et al. | 67 | 9 | ||||
| Tagliamento et al. | 17 | 4 | ||||
| Thompson et al. | 87 | 47 | ||||
| Tian et al. | 232 | 46 | 23 | 9 | 31 | 5 |
| Tsimafeyeu et al. | 37 | 1 | ||||
| Wang QQ et al. | 670 | 100 | ||||
| Wang J et al. | 12 | 3 | 3 | 1 | 1 | 0 |
| Wang L et al. | 15 | 3 | ||||
| Wang J et al. | 283 | 50 | 51 | 13 | 38 | 2 |
| Wang B et al. | 58 | 14 | ||||
| Westblade et al. | 100 | 30 | ||||
| Wang Q et al. | 420 | 40 | ||||
| Wood et al. | 250 | 70 | ||||
| Wu Y et al. | 14 | 6 | ||||
| Wu Q et al. | 11 | 4 | ||||
| Yang B et al. | 37 | 7 | 37 | 7 | ||
| Yang K et al. | 205 | 40 | 24 | 6 | 40 | 3 |
| Yarza et al. | 63 | 16 | 17 | 6 | ||
| Yigenoglu et al. | 740 | 102 | ||||
| Yu et al. | 12 | 3 | 7 | 2 | 1 | 0 |
| Zhang B et al | 35 | 0 | 35 | 0 | ||
| Zhang H et al. | 107 | 23 | 21 | 5 | ||
| Zhang L et al. | 28 | 8 |
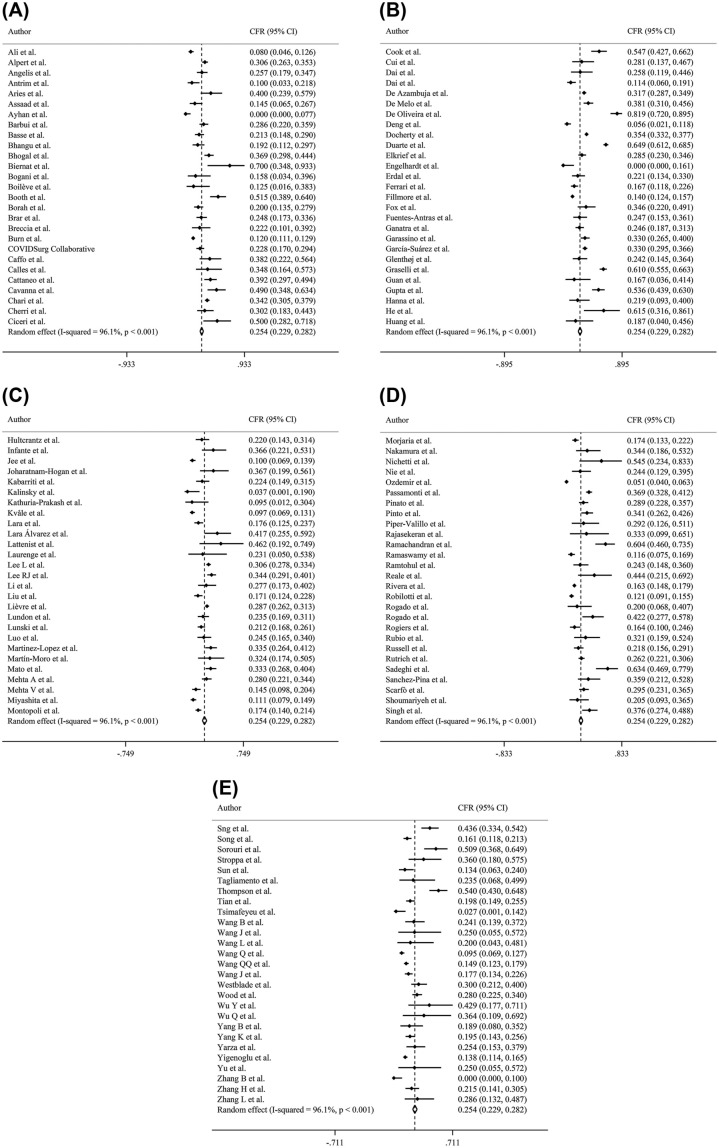
Overall, the CFR was 25.4% (95% CI 22.9%–28.2%; Egger’s test p = 0.001) (Fig. 1 ). A sensitivity analysis of the 66 studies (N = 31,184) including at least 100 patients showed a CFR of 21.9% (95% CI 19.1%–25.1%) (Fig. S1).
Fig. 1.
(A, B, C, D, E). Forest plot of studies reporting the CFR among patients with solid or hematological malignancies and SARS-CoV-2 infection. (A) Authors from A to C. (B) Authors from C to H. (C) Authors from H to M. (D) Authors from M to S. (E) Authors from S to Z.
Abbreviations. CFR: case-fatality rate; 95% CI: 95% confidence interval.
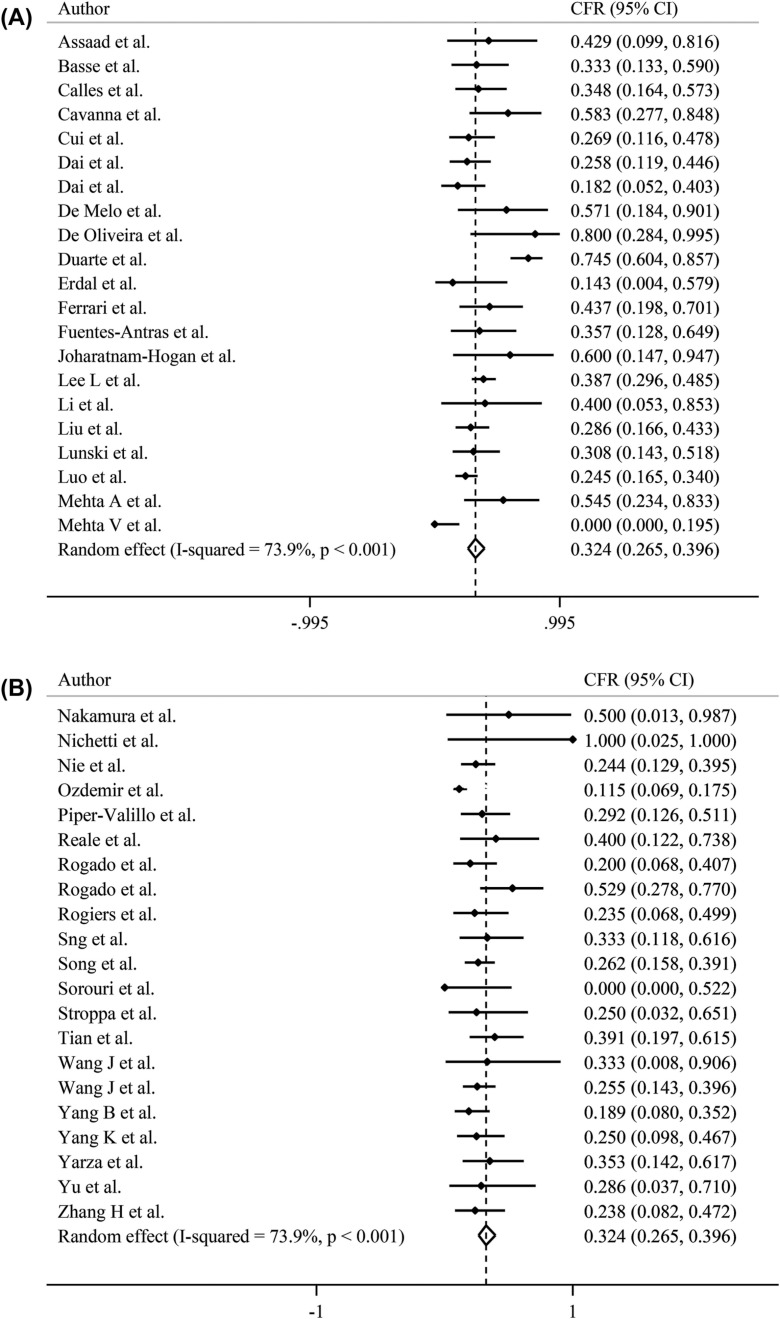
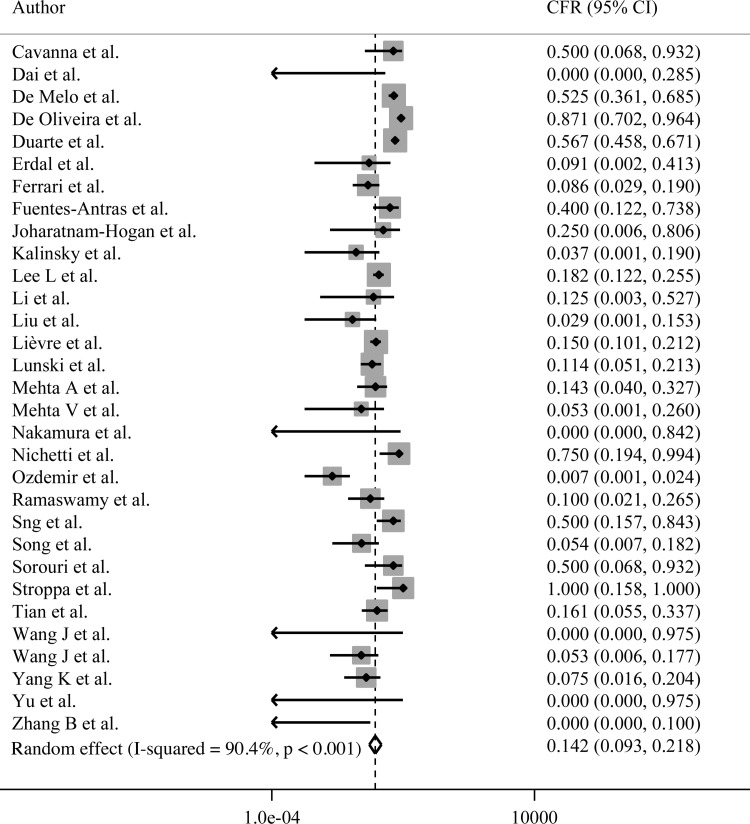
In total, 42 and 31 studies reported the mortality rate among COVID-19 patients with lung (N = 1,135) and breast (N = 1,296) cancers, respectively (Table 1). The CFR among patients with lung cancer and SARS-CoV2 infection was 32.4% (95% CI 26.5%–39.6%) when including all studies (Fig. 2 ) and 22.7% (95% CI 11.8%–43.8%) at the sensitivity analysis after excluding studies with less than 100 patients (Fig. S2). The CFR among patients with breast cancer and SARS-CoV2 infection was 14.2% (95% CI 9.3%–21.8%) when including all studies (Fig. 3 ) and 9.4% (95% CI 4.0%–22.4%) at the sensitivity analysis after excluding studies with less than 100 patients (Fig. S3).
Fig. 2.
(A, B). Forest plot of studies reporting the CFR among patients with lung cancer and SARS-CoV-2 infection. (A) Authors from A to M. (B) Authors from N to Z.
Abbreviations. CFR: case-fatality rate; 95% CI: 95% confidence interval.
Fig. 3.
Forest plot of studies reporting the CFR among patients with breast cancer and SARS-CoV-2 infection.
Abbreviations. CFR: case-fatality rate; 95% CI: 95% confidence interval.
4. Discussion
Over a year after the outbreak of the pandemic, this large meta-analysis reports the impact of COVID-19 in patients with solid or hematological malignancies. Overall, these patients were found to have a high probability of mortality (CFR = 25.4%); the absolute rate was particularly high among patients with lung cancer (32.4%), while it was lower in those with breast cancer (14.2%). These findings strongly highlight the need to dedicate special attention to patients with cancer during the ongoing pandemic.
Overall, there is a growing evidence that patients with a history of cancer have a higher mortality rate due to COVID-19 as compared with the general population. Several international registries, such as the International Severe Acute Respiratory and Emerging Infections Consortium (ISARIC) (Docherty et al., 2020), the OnCOVID (Pinato et al., 2020b), the Clinical impact of COVID-19 on patients with Cancer (CCC-19) (Kuderer et al., 2020), the GCO-002 CACOVID-19 (Lièvre et al., 2020), reported a mortality rate of oncological patients with SARS-CoV-2 infection up to 40% (Lee and Purshouse, 2021). The majority of these studies did not foresee a control group of patients with COVID-19 without cancer. Instead, a recent retrospective study, evaluating by a multivariate model the difference in mortality from COVID-19 between 312 patients with cancer and 4,833 patients without cancer in the U.S., found a higher death rate in the cancer group. Among patients with cancer, having an active or progressive disease was shown to increase the likelihood of mortality (p < 0.001) (Lunski et al., 2021). Our findings confirm a high mortality rate in patients with solid or hematological malignancies and SARS-CoV-2 infection.
Since the COVID-19 outbreak, major efforts have been implemented to protect most vulnerable patients from SARS-CoV-2 infection. Among them, the following measures have been suggested in cancer care: the rationalization of working practices, the adaptation of chemotherapy regimens as well as other systemic treatments, the deferral of procedures for diseases with favorable biology or not requiring urgent care, and additional measures related to specific subtypes of cancer (Poggio et al., 2020; Tagliamento et al., 2020b; Burki, 2020; Onesti et al., 2020, 2021). Aggressive preventive measures include preferential access to COVID-19 vaccination, which should be administered as early as possible (Garassino et al., 2021). Furthermore, ensuring cancer care continuity during the COVID-19 pandemic should represent a priority, considering treatment interruptions or discontinuations only on a case-by-case basis, taking into account patient and tumor characteristics (Lambertini et al., 2020; Tagliamento et al., 2020a).
In our meta-analysis, patients with lung cancer had a comparatively higher CFR than the overall population, consistent with the data reported in the Thoracic Cancers International COVID-19 Collaboration (TERAVOLT) registry (not included in our separate analysis of the CFR in lung cancer, since patients with non-lung thoracic malignancies were included as well, like in the study by Lièvre et al.) (Garassino et al., 2020; Lièvre et al., 2020), and with previous reports in patients from China (Yu et al., 2020; Liang et al., 2020; Zhang et al., 2020b). Whether this high mortality rate may be reduced with special management of such patients in intensive care is an open question (Garassino et al., 2020).
On the contrary, a comparatively lower CFR was observed in patients with breast cancer, suggesting that breast cancer per se does not seem to be a major determinant of COVID-19 mortality. One potential explanation might be that patients with lung cancer tend to be older than those with breast cancer. Furthermore, co-existing pulmonary conditions might further raise the risk for an unfavorable outcome in patients with lung cancer diagnosed with COVID-19, as well as the different spectrum of anticancer treatments received compared to breast cancer. Conversely, the delays in cancer diagnosis and treatment due to the COVID-19 pandemic may have an impact on outcomes, considering that a significant proportion of the important gain in disease-specific overall survival observed in the last 20–30 years are attributable to early detection and improved treatments (Gathani et al., 2021). The long-term effect on cancer-specific survival outcomes of the temporary suspension of routine screening during the peak of the pandemic will be only and fully revealed in the future (Gathani et al., 2021).
Our meta-analysis has some limitations that should be acknowledged. It included heterogeneous cohorts, involving hospitalized and non-hospitalized patients, with both solid or hematological malignancies currently receiving or not active anticancer treatments (and different types) at the time of SARS-CoV-2 infection. Some studies only reported on in-hospital mortality, and sometimes exclusively on 30-day rate. Moreover, we evaluated the mortality rate considering death from any cause, instead of focusing specifically on death due to COVID-19 or due to cancer progression (this specific information was frequently unavailable in the studies included in the meta-analysis). As expected, the heterogeneity in the analyses was significant (p < 0.001) probably due to the high number of evaluated studies characterized by different study design, population, sample size, and the geographical variability in the spread of the pandemic. Nevertheless, notably, more than 75% of CFRs reported in the individual studies ranged between 10% and 39%, so our pooled estimate (CFR = 25.4%) reflects this trend.
Our study has also several strengths. The present meta-analysis included a large number of studies (n = 135) and patients (n = 33,879). All studies published in the first year since the start of the pandemic were evaluated. The CFR computed among the overall population is consistent with a previous analysis (Saini et al., 2020). In addition, we also separately focused on patients with lung and breast cancers, in order to evaluate the CFRs associated with these two common malignancies.
5. Conclusions
Our systematic review and meta-analysis showed that patients with solid or hematological malignancies and SARS-CoV-2 infection have a high probability of mortality, with a comparatively higher CFR in patients with lung cancer, and a comparatively lower CFR in patients with breast cancer. Based on these results, patients with underlying cancer deserve special attention with aggressive preventive measures that should also include early access to COVID-19 vaccination.
Authors’ contribution
Conceptualization: Marco Tagliamento, Matteo Lambertini.
Data curation: Marco Tagliamento, Elisa Agostinetto, Marco Bruzzone, Marcello Ceppi, Francesca Poggio, Matteo Lambertini.
Formal analysis: Marco Bruzzone, Marcello Ceppi.
Methodology: Marco Tagliamento, Elisa Agostinetto, Marco Bruzzone, Marcello Ceppi, Francesca Poggio, Matteo Lambertini.
Project administration: Marco Tagliamento, Matteo Lambertini.
Validation: all authors.
Writing - original draft: Marco Tagliamento, Elisa Agostinetto, Matteo Lambertini
Writing - review & editing: all authors.
Disclosures
Dr. Tagliamento reported travel grants from Roche, Bristol-Myers Squibb, AstraZeneca, Takeda and Honoraria as medical writer from Novartis, Amgen outside the submitted work.
Dr. Lambertini acted as a consultant for Roche, Novartis, Lilly and AstraZeneca, and received honoraria from Novartis, Pfizer, Takeda, Roche, Sandoz and Lilly outside the submitted work.
Funding
This study received no funding.
Biographies
Marco Tagliamento is a Medical Oncology Resident and PhD Student in Translational Oncology at the University of Genova (Italy). His clinical and research activity is particularly focused on lung cancer. He is involved as researcher in clinical and translational trials in Oncology. He is member of the European Organization for Research and Treatmemt of Cancer (EORTC) Lung Cancer Group.
Elisa Agostinetto is a Clinical Research Fellow at Institut Jules Bordet in Brussels (Belgium) and a Medical Oncology Resident at Humanitas Research Hospital in Milan (Italy). In 2015, she received her degree in Medicine from the University of Udine (Italy), and she undertook her specialist training in Medical Oncology at Humanitas University. Her research activity focuses on her main fields of interest, namely breast cancer and immuno-oncology.
Marco Bruzzone is in Staff at the Clinical Epidemiology Unit of the IRCCS Ospedale Policlinico San Martino in Genova (Italy), where he works as biostatistician in the area of scientific research, mainly oncological. He is co-author of almost 50 scientific publications and of about 30 congress abstracts. The main topics of his research are the prognostic role of clinical, pathological and biological characteristics of patients with breast cancer in their survival and the relevance of genetic factors, lifestyle and occupational exposures as predictors of diseases, especially oncological. He took the bachelor’s degree in Mathematical Statistics at the University of Genova (Italy) in 2011 and the master’s degree in Biostatistics and Experimental Statistics at the University of Milano-Bicocca (Italy) in 2014.
Marcello Ceppi is a researcher at the Clinical Epidemiology Unit of the IRCCS Ospedale Policlinico San Martino in Genova (Italy). His area of expertise is the statistical analysis of epidemiological and clinical data in the field of oncology with particular reference to advanced statistical methods applied to cohort and case-control studies, clinical trials and meta-analysis. He was responsible for data analysis in several projects funded by Italian Association for Cancer Research (AIRC) and Italian Ministry of Health.
Kamal S. Saini, MBBS, MD, MRCP (UK), DM, is the Executive Medical Director at Covance Inc., and also works as a locum consultant medical oncologist at the NHS (UK). He has over 16 years of experience in drug development, which includes enrolling patients into cancer trials, helping design and execute studies, medical monitoring and data analysis of global trials, interfacing with regulatory bodies, and working with biotech and pharmaceutical companies to refine drug development strategies. His main areas of interest are breast and lung cancers, optimization of oncology trial design, intersection of COVID-19 and cancer, and adopting a precision medicine-based approach to the treatment of patients with cancer.
Evandro de Azambuja is a medical oncologist form the Institut Jules Bordet, Brussels (Belgium). He is a breast cancer specialist and the head of the Medical Support Team. He has been extensively involved in large phase III registration trials in breast cancer and had a special interest in cardiac toxicity cause by anticancer treatments. He is also the Chair of the ESMO Fellowship Committee.
Kevin Punie is a medical oncologist working as a staff member at the department of General Medical Oncology in the University Hospitals Leuven (Belgium). His main areas of interest are breast cancer and hereditary cancer syndromes. He is deeply involved in clinical cancer research as principal investigator for several phase I-III trials with a focus on triple negative breast cancer. He is currently working on a PhD investigating plasma and tissue single-cell multiomics in early triple negative breast breast cancer. He is involved in the EORTC Breast Cancer Group, board member of the Belgian Society of Medical Oncology and Committee member of ESMO Young Oncologists Committee and ESMO Resilience Task Force.
Benedikt Westphalen studied Medicine and Molecular Biology in Hamburg, Philadelphia, New York and Bern. After graduating from medical school, he started training in Internal Medicine at the University of Hamburg (Germany), in 2008. In 2010, Dr Westphalen joined the laboratory of Timothy C. Wang at Columbia University in New York City as a postdoctoral fellow. His studies were focused on cellular plasticity and the origins of gastrointestinal malignancies. After his postdoctoral training, he joined the department of haematology and oncology at the University of Munich (Germany), in 2013. In Munich, Dr Westphalen has focused on clinical and translational research in pancreatic cancer and early phase clinical trials. Since 2017 he heads the “Molecular Diagnostics and Therapy Programme” and the “Molecular Tumour Board” at the University of Munich (Germany). Furthermore, he serves as the medical lead for early phase clinical trials in medical oncology. He has received research support from the German Research Foundation, the Universities of Hamburg and Munich and young investigator awards from the AACR and GRG/AGA. Dr Westphalen has authored and co-authored more than seventy research papers. Dr Westphalen joined ESMO in 2017 and was a participant in the “ESMO Leaders Generation Programme” in 2018. He joined the ESMO Translational Research and Precision Medicine Working Group as well as the ESMO GI faculty Group in 2019.
Gilberto Morgan is an American oncologist with a background in molecular biology currently practicing in Lund (Sweden).
Paolo Pronzato is Head of the Medical Oncology Unit at the IRCCS Ospedale Policlinico San Martino in Genova (Italy). His clinical activity is dedicated to the care of different type of cancer, and particularly focused on patients with breast cancer. He has been extensively involved as PI or co-PI in phase II/III clinical trials in advanced and early breast cancer, as well as supportive care trials.
Lucia Del Mastro received his M.D. degree with full marks and honors from the University of Naples (Italy) in 1989. She took the specialty in Medical Oncology in 1993 at the University of Naples. She is the director of the Breast Unit at the IRCCS Ospedale Policlinico San Martino in Genova (Italy), and professor of oncology at the University of Genova. She is PI of phase II and III trials in metastatic and early breast cancer patients, and PI of toxicity and supportive care studies. She is PI of many research projects on breast cancer. She is reviewer of research projects for Cancer Research UK and EORTC. She is member of the Scientific Committee of GIM (Gruppo Italiano Mammella), secretary of the breast cancer working group of Alliance Against Cancer, chairperson of the steering committee of the AIOM (Associazione Italiana Oncologia Medica) recommendations for fertility preservation in cancer patients and she is a member of the steering committee of the AIOM recommendations for the management of breast cancer patients. She is author of more than 200 peer-reviewed publications in internationally recognized journals.
Francesca Poggio is a medical oncologist working in the Breast Unit at the IRCCS Ospedale Policlinico San Martino in Genova (Italy). Since the beginning of her career, she focused on the clinical management of early and advanced breast cancer, developing expertise and specific skills in breast cancer care. She is mainly involved as sub-investigator in several studies regarding breast cancer, including spontaneous, non-profit studies, as well as clinical trials.
Matteo Lambertini is adjunct professor and consultant in medical oncology at the IRCCS Ospedale Policlinico San Martino - University of Genova in Genova (Italy). He is mainly focused on the care of breast cancer patients and is deeply involved in cancer research. Above all, he has a particular expertise in the management of breast cancer in young women, with a specific attention to the fertility and pregnancy-related issues that they have to face after diagnosis. He is member of the guideline group on fertility preservation in cancer patients for the European Society for Medical Oncology (ESMO), the European Society of Human Reproduction and Embriology (ESHRE) and the Italian Association of Medical Oncology (AIOM).
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.critrevonc.2021.103365.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Ali J., Sajjad K., Farooqi A.R., Aziz M.T., Rahat A., Khan S. COVID-19-positive cancer patients undergoing active anticancer treatment: an analysis of clinical features and outcomes. Hematol. Stem Cell Ther. 2020 doi: 10.1016/j.hemonc.2020.12.001. Published online December:S1658387620301801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alpert N., Rapp J.L., Marcellino B., Lieberman-Cribbin W., Flores R., Taioli E. Clinical course of cancer patients with COVID-19: a retrospective cohort study. JNCI Cancer Spectr. 2021;5(1) doi: 10.1093/jncics/pkaa085. pkaa085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelis V., Tippu Z., Joshi K., et al. Defining the true impact of coronavirus disease 2019 in the at-risk population of patients with cancer. Eur. J. Cancer. 2020;136:99–106. doi: 10.1016/j.ejca.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antrim L., Capone S., Dong S., et al. Impact of COVID-19 infection among cancer patients treated at the Los Angeles County Medical Center. Cancer Treat. Res. Commun. 2021;26 doi: 10.1016/j.ctarc.2020.100273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aries J.A., Davies J.K., Auer R.L., et al. Clinical outcome of coronavirus disease 2019 in haemato‐oncology patients. Br. J. Haematol. 2020;190(2) doi: 10.1111/bjh.16852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assaad S., Avrillon V., Fournier M.-L., et al. High mortality rate in cancer patients with symptoms of COVID-19 with or without detectable SARS-COV-2 on RT-PCR. Eur. J. Cancer. 2020;135:251–259. doi: 10.1016/j.ejca.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayhan A., Oz M., Topfedaisi Ozkan N., et al. Perioperative SARS-CoV-2 infection among women undergoing major gynecologic cancer surgery in the COVID-19 era: a nationwide, cohort study from Turkey. Gynecol. Oncol. 2021;160(2):499–505. doi: 10.1016/j.ygyno.2020.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbui T., Vannucchi A.M., Alvarez-Larran A., et al. High mortality rate in COVID-19 patients with myeloproliferative neoplasms after abrupt withdrawal of ruxolitinib. Leukemia. 2021;35(2):485–493. doi: 10.1038/s41375-020-01107-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basse C., Diakite S., Servois V., et al. Characteristics and outcome of SARS-CoV-2 infection in cancer patients. JNCI Cancer Spectr. 2021;5(1) doi: 10.1093/jncics/pkaa090. pkaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhogal T., Khan U.T., Lee R., et al. Haematological malignancy and nosocomial transmission are associated with an increased risk of death from COVID-19: results of a multi-center UK cohort. Leuk. Lymphoma. 2021:1–16. doi: 10.1080/10428194.2021.1876865. Published online January 28. [DOI] [PubMed] [Google Scholar]
- Biernat M.M., Zińczuk A., Biernat P., et al. Nosocomial outbreak of SARS-CoV-2 infection in a haematological unit – high mortality rate in infected patients with haematologic malignancies. J. Clin. Virol. 2020;130 doi: 10.1016/j.jcv.2020.104574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogani G., Ditto A., Bosio S., Brusadelli C., Raspagliesi F. Cancer patients affected by COVID-19: experience from Milan, Lombardy. Gynecol. Oncol. 2020;158(2):262–265. doi: 10.1016/j.ygyno.2020.06.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boilève A., Stoclin A., Barlesi F., et al. COVID-19 management in a cancer center: the ICU storm. Support. Care Cancer. 2020;28(10):5037–5044. doi: 10.1007/s00520-020-05658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth S., Willan J., Wong H., et al. Regional outcomes of severe acute respiratory syndrome coronavirus 2 infection in hospitalised patients with haematological malignancy. Eur. J. Haematol. 2020;105(4):476–483. doi: 10.1111/ejh.13469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borah P., Mirgh S., Sharma S.K., et al. Effect of age, comorbidity and remission status on outcome of COVID-19 in patients with hematological malignancies. Blood Cells Mol. Dis. 2021;87 doi: 10.1016/j.bcmd.2020.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brar G., Pinheiro L.C., Shusterman M., et al. COVID-19 severity and outcomes in patients with cancer: a matched cohort study. J. Clin. Oncol. 2020;38(33):3914–3924. doi: 10.1200/JCO.20.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breccia M., Piciocchi A., De Stefano V., et al. COVID-19 in Philadelphia-negative myeloproliferative disorders: a GIMEMA survey. Leukemia. 2020;34(10):2813–2814. doi: 10.1038/s41375-020-01032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burki T.K. Cancer guidelines during the COVID-19 pandemic. Lancet Oncol. 2020;21(5):629–630. doi: 10.1016/S1470-2045(20)30217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burn E., Tebé C., Fernandez-Bertolin S., et al. The natural history of symptomatic COVID-19 during the first wave in Catalonia. Nat. Commun. 2021;12(1):777. doi: 10.1038/s41467-021-21100-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caffo O., Gasparro D., Di Lorenzo G., et al. Incidence and outcomes of severe acute respiratory syndrome coronavirus 2 infection in patients with metastatic castration-resistant prostate cancer. Eur. J. Cancer. 2020;140:140–146. doi: 10.1016/j.ejca.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calles A., Aparicio M.I., Alva M., et al. Outcomes of COVID-19 in patients with lung cancer treated in a tertiary hospital in Madrid. Front. Oncol. 2020;10:1777. doi: 10.3389/fonc.2020.01777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattaneo C., Daffini R., Pagani C., et al. Clinical characteristics and risk factors for mortality in hematologic patients affected by COVID‐19. Cancer. 2020;126(23):5069–5076. doi: 10.1002/cncr.33160. [DOI] [PubMed] [Google Scholar]
- Cavanna L., Citterio C., Toscani I., et al. Cancer patients with COVID-19: a retrospective study of 51 patients in the district of Piacenza, Northern Italy. Future Sci. OA. 2021;7(1) doi: 10.2144/fsoa-2020-0157. FSO645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chari A., Samur M.K., Martinez-Lopez J., et al. Clinical features associated with COVID-19 outcome in multiple myeloma: first results from the International Myeloma Society data set. Blood. 2020;136(26):3033–3040. doi: 10.1182/blood.2020008150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherri S., Lemmers D.H.L., Noventa S., Abu Hilal M., Zaniboni A. Outcome of oncological patients admitted with COVID-19: experience of a hospital center in northern Italy. Ther. Adv. Med. Oncol. 2020;12 doi: 10.1177/1758835920962370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciceri F., Castagna A., Rovere-Querini P., et al. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clin. Immunol. 2020;217 doi: 10.1016/j.clim.2020.108509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook G., John Ashcroft A., Pratt G., et al. Real‐world assessment of the clinical impact of symptomatic infection with severe acute respiratory syndrome coronavirus (COVID‐19 disease) in patients with multiple myeloma receiving systemic anti‐cancer therapy. Br. J. Haematol. 2020;190(2) doi: 10.1111/bjh.16874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVIDSurg Collaborative, Li E., Glasbey J.C., et al. Outcomes from elective colorectal cancer surgery during the SARS‐CoV‐2 pandemic. Colorectal Dis. 2020 doi: 10.1111/codi.15431. Published online December 17,:codi.15431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui W., Yousaf N., Bhosle J., et al. Real-world outcomes in thoracic cancer patients with severe acute respiratory syndrome Coronavirus 2 (COVID-19): single UK institution experience. Cancer Treat. Res. Commun. 2020;25 doi: 10.1016/j.ctarc.2020.100261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai M., Liu D., Liu M., et al. Patients with cancer appear more vulnerable to SARS-COV-2: a multi-center study during the COVID-19 outbreak. Cancer Discov. 2020:CD–0422. doi: 10.1158/2159-8290.CD-20-0422. Published online April 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Azambuja E., Brandão M., Wildiers H., et al. Impact of solid cancer on in-hospital mortality overall and among different subgroups of patients with COVID-19: a nationwide, population-based analysis. ESMO Open. 2020;5(5):e000947. doi: 10.1136/esmoopen-2020-000947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Melo A.C., Thuler L.C.S., da Silva J.L., et al. Cancer inpatients with COVID-19: a report from the Brazilian National Cancer Institute. Adrish M, ed. PLoS One. 2020;15(10):e0241261. doi: 10.1371/journal.pone.0241261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Oliveira L.C., da C Rosa K.S., Durante A.L., et al. Palliative care and COVID-19 pandemic: retrospective study of factors associated with infection and death at an Oncological Palliative Care Reference Center. Am. J. Hosp. Palliat. Med. 2021 doi: 10.1177/1049909120986962. Published online January 18,:104990912098696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng G., Yin M., Chen X., Zeng F. Clinical determinants for fatality of 44,672 patients with COVID-19. Crit. Care. 2020;24(1):179. doi: 10.1186/s13054-020-02902-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Docherty A.B., Harrison E.M., Green C.A., et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020 doi: 10.1136/bmj.m1985. Published online May 22,:m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duarte M.B.O., Leal F., Argenton J.L.P., Carvalheira J.B.C. Outcomes of COVID-19 patients under cytotoxic cancer chemotherapy in Brazil. Cancers. 2020;12(12):3490. doi: 10.3390/cancers12123490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkrief A., Desilets A., Papneja N., et al. High mortality among hospital-acquired COVID-19 infection in patients with cancer: a multicentre observational cohort study. Eur. J. Cancer. 2020;139:181–187. doi: 10.1016/j.ejca.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhardt Monika, Shoumariyeh Khalid, Rösner Amelie, et al. Clinical characteristics and outcome of multiple myeloma patients with concomitant COVID-19 at comprehensive cancer centers in Germany. Haematologica. 2020;105(12):2872–2878. doi: 10.3324/haematol.2020.262758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdal G.S., Polat O., Erdem G.U., et al. The mortality rate of COVID-19 was high in cancer patients: a retrospective single-center study. Int. J. Clin. Oncol. 2021 doi: 10.1007/s10147-021-01863-6. Published online January 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari B.L., Ferreira C.G., Menezes M., et al. Determinants of COVID-19 mortality in patients with cancer from a community oncology practice in Brazil. JCO Glob. Oncol. 2021;(7):46–55. doi: 10.1200/GO.20.00444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillmore N.R., La J., Szalat R.E., et al. Prevalence and outcome of COVID-19 infection in cancer patients: a national veterans affairs study. J. Natl. Cancer Inst. 2020 doi: 10.1093/jnci/djaa159. Published online October 8,:djaa159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox T.A., Troy‐Barnes E., Kirkwood A.A., et al. Clinical outcomes and risk factors for severe COVID‐19 in patients with haematological disorders receiving chemo‐ or immunotherapy. Br. J. Haematol. 2020;191(2):194–206. doi: 10.1111/bjh.17027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuentes‐Antrás J., Manzano A., Marquina G., et al. A snapshot of COVID ‐19 infection in patients with solid tumors. Int. J. Cancer. 2020 doi: 10.1002/ijc.33420. Published online December 19,:ijc.33420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganatra S., Dani S.S., Redd R., et al. Outcomes of COVID-19 in patients with a history of Cancer and comorbid cardiovascular disease. J. Natl. Compr. Cancer Netw. 2020:1–10. doi: 10.6004/jnccn.2020.7658. Published online November 3. [DOI] [PubMed] [Google Scholar]
- Garassino M.C., Whisenant J.G., Huang L.-C., et al. COVID-19 in patients with thoracic malignancies (TERAVOLT): first results of an international, registry-based, cohort study. Lancet Oncol. 2020;21(7):914–922. doi: 10.1016/S1470-2045(20)30314-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garassino M.C., Vyas M., de Vries E., Kanesvaran R., Giuliani R., Peters S. The ESMO call to action on COVID-19 vaccinations and patients with cancer: vaccinate. Monitor. Educate. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2021 doi: 10.1016/j.annonc.2021.01.068. Published online February. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Suárez J., de la Cruz J., Cedillo Á, et al. Impact of hematologic malignancy and type of cancer therapy on COVID-19 severity and mortality: lessons from a large population-based registry study. J. Hematol. Oncol. 2020;13(1):133. doi: 10.1186/s13045-020-00970-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gathani T., Clayton G., MacInnes E., Horgan K. The COVID-19 pandemic and impact on breast cancer diagnoses: what happened in England in the first half of 2020. Br. J. Cancer. 2021;124(4):710–712. doi: 10.1038/s41416-020-01182-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenthøj A., Jakobsen L.H., Sengeløv H., et al. SARS‐CoV‐2 infection among patients with haematological disorders: severity and one‐month outcome in 66 Danish patients in a nationwide cohort study. Eur. J. Haematol. 2021;106(1):72–81. doi: 10.1111/ejh.13519. [DOI] [PubMed] [Google Scholar]
- Grasselli G., Greco M., Zanella A., et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern. Med. 2020;180(10):1345. doi: 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W., Liang W., Zhao Y., et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur. Respir. J. 2020;55(5) doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Hayek S.S., Wang W., et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern. Med. 2020;180(11):1436. doi: 10.1001/jamainternmed.2020.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna G.J., Rettig E.M., Park J.C., et al. Hospitalization rates and 30-day all-cause mortality among head and neck cancer patients and survivors with COVID-19. Oral Oncol. 2021;112 doi: 10.1016/j.oraloncology.2020.105087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He W., Chen L., Chen L., et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34(6):1637–1645. doi: 10.1038/s41375-020-0836-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Q., Hu S., Ran F.-M., et al. Asymptomatic COVID-19 infection in patients with cancer at a cancer-specialized hospital in Wuhan, China – preliminary results. Eur. Rev. Med. Pharmacol. Sci. 2020;24(18):9760–9764. doi: 10.26355/eurrev_202009_23070. [DOI] [PubMed] [Google Scholar]
- Hultcrantz M., Richter J., Rosenbaum C.A., et al. COVID-19 infections and clinical outcomes in patients with multiple myeloma in New York City: a cohort study from five academic centers. Blood Cancer Discov. 2020;1(3):234–243. doi: 10.1158/2643-3230.BCD-20-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infante M., González‐Gascón y Marín, Muñoz‐Novas C., et al. COVID‐19 in patients with hematological malignancies: a retrospective case series. Int. J. Lab. Hematol. 2020;42(6) doi: 10.1111/ijlh.13301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jee J., Foote M.B., Lumish M., et al. Chemotherapy and COVID-19 outcomes in patients with Cancer. J. Clin. Oncol. 2020;38(30):3538–3546. doi: 10.1200/JCO.20.01307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joharatnam-Hogan N., Hochhauser D., Shiu K.-K., et al. Outcomes of the 2019 novel coronavirus in patients with or without a history of cancer: a multi-centre North London experience. Ther. Adv. Med. Oncol. 2020;12 doi: 10.1177/1758835920956803. 175883592095680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabarriti R., Brodin N.P., Maron M.I., et al. Extent of prior lung irradiation and mortality in COVID-19 patients with a cancer history. Adv. Radiat. Oncol. 2020;5(4):707–710. doi: 10.1016/j.adro.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalinsky K., Accordino M.K., Hosi K., et al. Characteristics and outcomes of patients with breast cancer diagnosed with SARS-Cov-2 infection at an academic center in New York City. Breast Cancer Res. Treat. 2020;182(1):239–242. doi: 10.1007/s10549-020-05667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kathuria-Prakash N., Mosaferi T., Xie M., et al. COVID-19 outcomes of patients with differentiated thyroid cancer: a multicenter los angeles cohort study. Endocr. Pract. 2021;27(2):90–94. doi: 10.1016/j.eprac.2020.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuderer N.M., Choueiri T.K., Shah D.P., et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31187-9. Published online May:S0140673620311879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvåle R., Bønaa K.H., Forster R., Gravningen K., Júlíusson P.B., Myklebust T.Å. Hva betyr tidligere hjerte- og karsykdom eller kreft for risiko for død etter påvist SARS-CoV-2? Tidsskr Den Nor Legeforening. 2020 doi: 10.4045/tidsskr.20.0956. Published online. [DOI] [PubMed] [Google Scholar]
- Lambertini M., Toss A., Passaro A., et al. Cancer care during the spread of coronavirus disease 2019 (COVID-19) in Italy: young oncologists’ perspective. ESMO Open. 2020;5(2) doi: 10.1136/esmoopen-2020-000759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara O.D., Smith M.J., Wang Y., et al. Racial disparities in patients with coronavirus disease 2019 infection and gynecologic malignancy. Cancer. 2020 doi: 10.1002/cncr.33335. Published online December 9,:cncr.33335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara Álvarez M.Á, Rogado Revuelta J., Obispo Portero B., Pangua Méndez C., Serrano Montero G., López Alfonso A. COVID-19 mortality in cancer patients in a Madrid hospital during the first 3 weeks of the epidemic. Med. Clín. Engl. Ed. 2020;155(5):202–204. doi: 10.1016/j.medcle.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattenist R., Yildiz H., De Greef J., Bailly S., Yombi J.C. COVID-19 in adult patients with hematological disease: analysis of clinical characteristics and outcomes. Indian J. Hematol. Blood Transfus. 2021;37(1):181–185. doi: 10.1007/s12288-020-01318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurenge A., Ursu R., Houillier C., et al. SARS-CoV-2 infection in patients with primary central nervous system lymphoma. J. Neurol. 2021 doi: 10.1007/s00415-020-10311-w. Published online January 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A.J.X., Purshouse K. COVID-19 and cancer registries: learning from the first peak of the SARS-CoV-2 pandemic. Br. J. Cancer. 2021 doi: 10.1038/s41416-021-01324-x. Published online March 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Lyw, Cazier J.-B., Starkey T., et al. COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol. 2020;21(10):1309–1316. doi: 10.1016/S1470-2045(20)30442-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R.J., Wysocki O., Bhogal T., et al. Longitudinal characterisation of haematological and biochemical parameters in cancer patients prior to and during COVID-19 reveals features associated with outcome. ESMO Open. 2021;6(1) doi: 10.1016/j.esmoop.2020.100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Chen L., Li Q., et al. Cancer increases risk of in-hospital death from COVID-19 in persons <65 years and those not in complete remission. Leukemia. 2020;34(9):2384–2391. doi: 10.1038/s41375-020-0986-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang W., Guan W., Chen R., et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lièvre A., Turpin A., Ray-Coquard I., et al. Risk factors for Coronavirus Disease 2019 (COVID-19) severity and mortality among solid cancer patients and impact of the disease on anticancer treatment: a French nationwide cohort study (GCO-002 CACOVID-19) Eur. J. Cancer. 2020;141:62–81. doi: 10.1016/j.ejca.2020.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Li L., Song K., et al. A nomogram for predicting mortality in patients with COVID-19 and solid tumors: a multicenter retrospective cohort study. J. Immunother. Cancer. 2020;8(2) doi: 10.1136/jitc-2020-001314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundon D.J., Kelly B.D., Shukla D., Bolton D.M., Wiklund P., Tewari A. A decision aide for the risk stratification of GU cancer patients at risk of SARS-CoV-2 infection, COVID-19 related hospitalization, intubation, and mortality. J. Clin. Med. 2020;9(9):2799. doi: 10.3390/jcm9092799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunski M.J., Burton J., Tawagi K., et al. Multivariate mortality analyses in COVID‐19: comparing patients with cancer and patients without cancer in Louisiana. Cancer. 2021;127(2):266–274. doi: 10.1002/cncr.33243. [DOI] [PubMed] [Google Scholar]
- Luo J., Rizvi H., Preeshagul I.R., et al. COVID-19 in patients with lung cancer. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2020;31(10):1386–1396. doi: 10.1016/j.annonc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-López J., Mateos M.-V., Encinas C., et al. Multiple myeloma and SARS-CoV-2 infection: clinical characteristics and prognostic factors of inpatient mortality. Blood Cancer J. 2020;10(10):103. doi: 10.1038/s41408-020-00372-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín‐Moro F., Marquet J., Piris M., et al. Survival study of hospitalised patients with concurrent COVID‐19 and haematological malignancies. Br. J. Haematol. 2020;190(1) doi: 10.1111/bjh.16801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mato A.R., Roeker L.E., Lamanna N., et al. Outcomes of COVID-19 in patients with CLL: a multicenter international experience. Blood. 2020;136(10):1134–1143. doi: 10.1182/blood.2020006965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta V., Goel S., Kabarriti R., et al. Case fatality rate of cancer patients with COVID-19 in a New York Hospital System. Cancer Discov. 2020;10(7):935–941. doi: 10.1158/2159-8290.CD-20-0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta A., Vasudevan S., Parkash A., Sharma A., Vashist T., Krishna V. COVID-19 mortality in cancer patients: a report from a tertiary cancer centre in India. PeerJ. 2021;9 doi: 10.7717/peerj.10599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyashita H., Mikami T., Chopra N., et al. Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City. Ann. Oncol. 2020;31(8):1088–1089. doi: 10.1016/j.annonc.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montopoli M., Zumerle S., Vettor R., et al. Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532) Ann. Oncol. 2020;31(8):1040–1045. doi: 10.1016/j.annonc.2020.04.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morjaria S., Zhang A.W., Kaltsas A., et al. The effect of neutropenia and filgrastim (G-CSF) in cancer patients with COVID-19 infection. Infect. Dis. (except HIV/AIDS) 2020 doi: 10.1101/2020.08.13.20174565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura S., Kanemasa Y., Atsuta Y., et al. Characteristics and outcomes of coronavirus disease 2019 (COVID-19) patients with cancer: a single-center retrospective observational study in Tokyo, Japan. Int. J. Clin. Oncol. 2021;26(3):485–493. doi: 10.1007/s10147-020-01837-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nepogodiev D., Bhangu A., Glasbey J.C., et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichetti F., Bini M., Ambrosini M., et al. COVID-19 risk for patients undergoing anticancer treatment at the outpatient clinic of the National Cancer institute of Milan: the COVINT study. ESMO Open. 2020;5(Suppl 3):e000883. doi: 10.1136/esmoopen-2020-000883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie L., Dai K., Wu J., et al. Clinical characteristics and risk factors for in‐hospital mortality of lung cancer patients with COVID ‐19: a multicenter, retrospective, cohort study. Thorac. Cancer. 2021;12(1):57–65. doi: 10.1111/1759-7714.13710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onesti C.E., Rugo H.S., Generali D., et al. Oncological care organisation during COVID-19 outbreak. ESMO Open. 2020;5(4):e000853. doi: 10.1136/esmoopen-2020-000853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onesti C.E., Tagliamento M., Curigliano G., et al. Expected medium- and long-term impact of the COVID-19 outbreak in oncology. JCO Glob. Oncol. 2021;(7):162–172. doi: 10.1200/GO.20.00589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özdemir N., Dizdar Ö, Yazıcı O., et al. Clinical features and outcomes of COVID ‐19 in patients with solid tumors: Turkish National Registry Data. Int. J. Cancer. 2020 doi: 10.1002/ijc.33426. Published online December 17,:ijc.33426. [DOI] [PubMed] [Google Scholar]
- Passamonti F., Cattaneo C., Arcaini L., et al. Clinical characteristics and risk factors associated with COVID-19 severity in patients with haematological malignancies in Italy: a retrospective, multicentre, cohort study. Lancet Haematol. 2020;7(10):e737–e745. doi: 10.1016/S2352-3026(20)30251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinato D.J., Lee A.J.X., Biello F., et al. Presenting features and early mortality from SARS-CoV-2 infection in cancer patients during the initial stage of the COVID-19 pandemic in Europe. Cancers. 2020;12(7):1841. doi: 10.3390/cancers12071841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinato D.J., Zambelli A., Aguilar-Company J., et al. Clinical portrait of the SARS-CoV-2 epidemic in European Patients with Cancer. Cancer Discov. 2020;10(10):1465–1474. doi: 10.1158/2159-8290.CD-20-0773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto C., Berselli A., Mangone L., et al. SARS-CoV-2 positive hospitalized cancer patients during the italian outbreak: the cohort study in Reggio Emilia. Biology. 2020;9(8):181. doi: 10.3390/biology9080181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper-Vallillo Aj, Mooradian Mj, Meador Cb, et al. Coronavirus disease 2019 infection in a patient population with lung cancer: incidence, presentation, and alternative diagnostic considerations. JTO Clin. Res. Rep. 2021;2(1) doi: 10.1016/j.jtocrr.2020.100124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poggio F., Tagliamento M., Di Maio M., et al. Assessing the impact of the COVID-19 outbreak on the attitudes and practice of Italian oncologists toward breast cancer care and related research activities. JCO Oncol. Pract. 2020;16(11):e1304–e1314. doi: 10.1200/OP.20.00297. [DOI] [PubMed] [Google Scholar]
- Rajasekaran R.B., Ashford R.U., Cosker T.D.A., et al. What proportion of patients with bone and soft-tissue tumors contracted coronavirus-19 and died from surgical procedures during the initial period of the COVID-19 pandemic? Results from the Multicenter British Orthopaedic Oncology Society Observational Study. Clin. Orthop. 2020 doi: 10.1097/CORR.0000000000001568. Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramachandran P., Kathirvelu B., Chakraborti A., et al. COVID-19 in Cancer patients from New York City: a comparative single center retrospective analysis. Cancer Control. 2020;27(1) doi: 10.1177/1073274820960457. 107327482096045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaswamy A., Nayak L., Roy Moulik N., et al. COVID‐19 in cancer patients on active systemic therapy – outcomes from LMIC scenario with an emphasis on need for active treatment. Cancer Med. 2020;9(23):8747–8753. doi: 10.1002/cam4.3423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramtohul T., Cabel L., Paoletti X., et al. Quantitative CT extent of lung damage in COVID-19 pneumonia is an independent risk factor for inpatient mortality in a population of cancer patients: a prospective study. Front. Oncol. 2020;10:1560. doi: 10.3389/fonc.2020.01560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reale M.L., Bironzo P., Bertaglia V., et al. SARS-CoV-2 Infection in cancer patients: a picture of an Italian onco-covid unitcancer patients: a picture of an Italian onco-covid unit. Front. Oncol. 2020;10:1722. doi: 10.3389/fonc.2020.01722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera D.R., Peters S., Panagiotou O.A., et al. Utilization of COVID-19 treatments and clinical outcomes among patients with cancer: a COVID-19 and cancer consortium (CCC19) cohort study. Cancer Discov. 2020;10(10):1514–1527. doi: 10.1158/2159-8290.CD-20-0941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robilotti E.V., Babady N.E., Mead P.A., et al. Determinants of COVID-19 disease severity in patients with cancer. Nat. Med. 2020;26(8):1218–1223. doi: 10.1038/s41591-020-0979-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogado J., Serrano-Montero G., Pangua C. Características y evolución de los pacientes con cáncer de pulmón e infección Covid-19 en un hospital de segundo nivel durante los 3 primeros meses de pandemia. Med. Clín. 2020;155(9):411–413. doi: 10.1016/j.medcli.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogado J., Obispo B., Pangua C., et al. Covid-19 transmission, outcome and associated risk factors in cancer patients at the first month of the pandemic in a Spanish hospital in Madrid. Clin. Transl. Oncol. 2020;22(12):2364–2368. doi: 10.1007/s12094-020-02381-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogiers A., Pires da Silva I., Tentori C., et al. Clinical impact of COVID-19 on patients with cancer treated with immune checkpoint inhibition. J. Immunother. Cancer. 2021;9(1) doi: 10.1136/jitc-2020-001931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio M.C., Sanchez L., Abreu-Ruíz G., Bermejo-Bencomo W., Crombet T., Lage A. COVID-19 and cancer in Cuba. Semin. Oncol. 2020;47(5):328–329. doi: 10.1053/j.seminoncol.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell B., Moss C., Papa S., et al. Factors affecting COVID-19 outcomes in cancer patients: a first report from guy’s cancer center in London. Front. Oncol. 2020;10:1279. doi: 10.3389/fonc.2020.01279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rüthrich M.M., Giessen-Jung C., Borgmann S., et al. COVID-19 in cancer patients: clinical characteristics and outcome-an analysis of the LEOSS registry. Ann. Hematol. 2021;100(2):383–393. doi: 10.1007/s00277-020-04328-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeghi A., Dooghaie Moghadam A., Eslami P., et al. The characteristics of cancerous patients infected with COVID-19 in hospital setting. Acta Bio Medica Atenei Parm. 2020;91(4) doi: 10.23750/abm.v91i4.10175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini K.S., Tagliamento M., Lambertini M., et al. Mortality in patients with cancer and coronavirus disease 2019: a systematic review and pooled analysis of 52 studies. Eur. J. Cancer. 2020;139:43–50. doi: 10.1016/j.ejca.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez‐Pina J.M., Rodríguez Rodriguez M., Castro Quismondo N., et al. Clinical course and risk factors for mortality from COVID‐19 in patients with haematological malignancies. Eur. J. Haematol. 2020;105(5):597–607. doi: 10.1111/ejh.13493. [DOI] [PubMed] [Google Scholar]
- Scarfò L., Chatzikonstantinou T., Rigolin G.M., et al. COVID-19 severity and mortality in patients with chronic lymphocytic leukemia: a joint study by ERIC, the European Research Initiative on CLL, and CLL Campus. Leukemia. 2020;34(9):2354–2363. doi: 10.1038/s41375-020-0959-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoumariyeh K., Biavasco F., Ihorst G., et al. Covid‐19 in patients with hematological and solid cancers at a comprehensive cancer center in Germany. Cancer Med. 2020;9(22):8412–8422. doi: 10.1002/cam4.3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S.R.K., Thanikachalam K., Jabbour-Aida H., Poisson L.M., Khan G. COVID-19 and cancer: lessons learnt from a Michigan Hotspot. Cancers. 2020;12(9):2377. doi: 10.3390/cancers12092377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sng C.C.T., Wong Y.N.S., Wu A., et al. Cancer history and systemic anti-cancer therapy independently predict COVID-19 mortality: a UK tertiary hospital experience. Front. Oncol. 2020;10 doi: 10.3389/fonc.2020.595804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song K., Gong H., Xu B., et al. Association between recent oncologic treatment and mortality among patients with carcinoma who are hospitalized with COVID‐19: a multicenter study. Cancer. 2021;127(3):437–448. doi: 10.1002/cncr.33240. [DOI] [PubMed] [Google Scholar]
- Sorouri M., Kasaeian A., Mojtabavi H., et al. Clinical characteristics, outcomes, and risk factors for mortality in hospitalized patients with COVID-19 and cancer history: a propensity score-matched study. Infect. Agent Cancer. 2020;15(1):74. doi: 10.1186/s13027-020-00339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroppa E.M., Toscani I., Citterio C., et al. Coronavirus disease-2019 in cancer patients. A report of the first 25 cancer patients in a western country (Italy) Future Oncol. 2020;16(20):1425–1432. doi: 10.2217/fon-2020-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun L., Surya S., Le A.N., et al. Rates of COVID-19–related outcomes in cancer compared with noncancer patients. JNCI Cancer Spectr. 2021;5(1) doi: 10.1093/jncics/pkaa120. pkaa120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tagliamento M., Lambertini M., Genova C., et al. Call for ensuring cancer care continuity during COVID-19 pandemic. ESMO Open. 2020;5(3) doi: 10.1136/esmoopen-2020-000783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tagliamento M., Spagnolo F., Poggio F., et al. Italian survey on managing immune checkpoint inhibitors in oncology during COVID‐19 outbreak. Eur. J. Clin. Invest. 2020;50(9) doi: 10.1111/eci.13315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson Jv, Meghani Nj, Powell Bm, et al. Patient characteristics and predictors of mortality in 470 adults admitted to a district general hospital in England with Covid-19. Epidemiol. Infect. 2020;148:e285. doi: 10.1017/S0950268820002873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian J., Yuan X., Xiao J., et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21(7):893–903. doi: 10.1016/S1470-2045(20)30309-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsimafeyeu I., Alekseeva G., Berkut M., et al. COVID-19 in patients with renal cell carcinoma in the Russian Federation. Clin. Genitourin. Cancer. 2020 doi: 10.1016/j.clgc.2020.07.007. Published online July:S1558767320301671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuagnat P., Frelaut M., Ramtohul T., et al. COVID-19 in breast cancer patients: a cohort at the Institut Curie hospitals in the Paris area. Breast Cancer Res. 2020;22(1):55. doi: 10.1186/s13058-020-01293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B., Van Oekelen O., Mouhieddine T.H., et al. A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward. J. Hematol. Oncol. 2020;13(1):94. doi: 10.1186/s13045-020-00934-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Zhang J., Tu Y., et al. Cancer patients in SARS-CoV-2 infection: a single-center experience from Wuhan. J. Cancer. 2020;11(21):6243–6247. doi: 10.7150/jca.47065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., He W., Yu X., et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J. Infect. 2020;80(6):639–645. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Song Q., Chen Y., et al. Systematic investigations of COVID-19 in 283 cancer patients. Oncology. 2020 doi: 10.1101/2020.04.28.20083246. [DOI] [Google Scholar]
- Wang Q., Berger N.A., Xu R. When hematologic malignancies meet COVID-19 in the United States: infections, death and disparities. Blood Rev. 2020 doi: 10.1016/j.blre.2020.100775. Published online November. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Berger N.A., Xu R. Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. JAMA Oncol. 2021;7(2):220. doi: 10.1001/jamaoncol.2020.6178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westblade L.F., Brar G., Pinheiro L.C., et al. SARS-CoV-2 viral load predicts mortality in patients with and without cancer who are hospitalized with COVID-19. Cancer Cell. 2020;38(5):661–671. doi: 10.1016/j.ccell.2020.09.007. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood W.A., Neuberg D.S., Thompson J.C., et al. Outcomes of patients with hematologic malignancies and COVID-19: a report from the ASH Research Collaborative Data Hub. Blood Adv. 2020;4(23):5966–5975. doi: 10.1182/bloodadvances.2020003170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2021. Coronavirus Disease (COVID-2019) Situation Reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Available at. [Google Scholar]
- Wu Y., Chen W., Li W., et al. Clinical characteristics, therapeutic management, and prognostic factors of adult COVID-19 inpatients with hematological malignancies. Leuk. Lymphoma. 2020;61(14):3440–3450. doi: 10.1080/10428194.2020.1808204. [DOI] [PubMed] [Google Scholar]
- Wu Q., Chu Q., Zhang H., et al. Clinical outcomes of coronavirus disease 2019 (COVID‐19) in cancer patients with prior exposure to immune checkpoint inhibitors. Cancer Commun. 2020;40(8):374–379. doi: 10.1002/cac2.12077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia Y., Jin R., Zhao J., Li W., Shen H. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020;21(4):e180. doi: 10.1016/S1470-2045(20)30150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang K., Sheng Y., Huang C., et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21(7):904–913. doi: 10.1016/S1470-2045(20)30310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang B., Choi H., Lee S.-K., et al. Risk of coronavirus disease incidence, severe presentation, and mortality in patients with lung cancer. Cancer Res. Treat. 2020 doi: 10.4143/crt.2020.1242. Published online December 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarza R., Bover M., Paredes D., et al. SARS-CoV-2 infection in cancer patients undergoing active treatment: analysis of clinical features and predictive factors for severe respiratory failure and death. Eur. J. Cancer. 2020;135:242–250. doi: 10.1016/j.ejca.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yigenoglu T.N., Ata N., Altuntas F., et al. The outcome of COVID‐19 in patients with hematological malignancy. J. Med. Virol. 2021;93(2):1099–1104. doi: 10.1002/jmv.26404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J., Ouyang W., Chua M.L.K., Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020;6(7):1108. doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B., Xie R., Hubert S.M., et al. Characteristics and outcomes of 35 breast cancer patients infected with COVID-19. Front. Oncol. 2020;10 doi: 10.3389/fonc.2020.570130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Zhu F., Xie L., et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann. Oncol. 2020;31(7):894–901. doi: 10.1016/j.annonc.2020.03.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Wang L., Chen Y., et al. Outcomes of novel coronavirus disease 2019 (COVID‐19) infection in 107 patients with cancer from Wuhan, China. Cancer. 2020;126(17):4023–4031. doi: 10.1002/cncr.33042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.