Abstract
Background
Service learning (SL) is an educational methodology presumed to help medical students be more empathetic and compassionate. We longitudinally investigated the level of empathy in medical students and how preclinical SL experience was related to their level of empathy in their clinical clerkships.
Methods
Our cohort comprised fifth-year medical students engaged in clerkships as part of a 7-year medical programme at one medical school in Taiwan. Surveys were conducted at the beginning of the clerkship in September 2015 (T1) to collect data on the medical students’ preclinical SL experience in curriculum-based service teams (CBSTs) and extracurricular service teams (ECSTs) and their SL self-efficacy, demographic characteristics, and empathy level. Subsequently, three follow-up surveys were conducted once every 3 months to determine the empathy level of the students during their clinical clerkships (T2–T4). Seventy students who returned the written informed consent and completed the baseline (T1) and two or more follow-up surveys (T2–T4) were included in our analysis with the response rate of 34%. In total, 247 responses across the 1-year clerkship were analysed. Descriptive statistics, paired t tests, and generalised estimating equations were employed.
Results
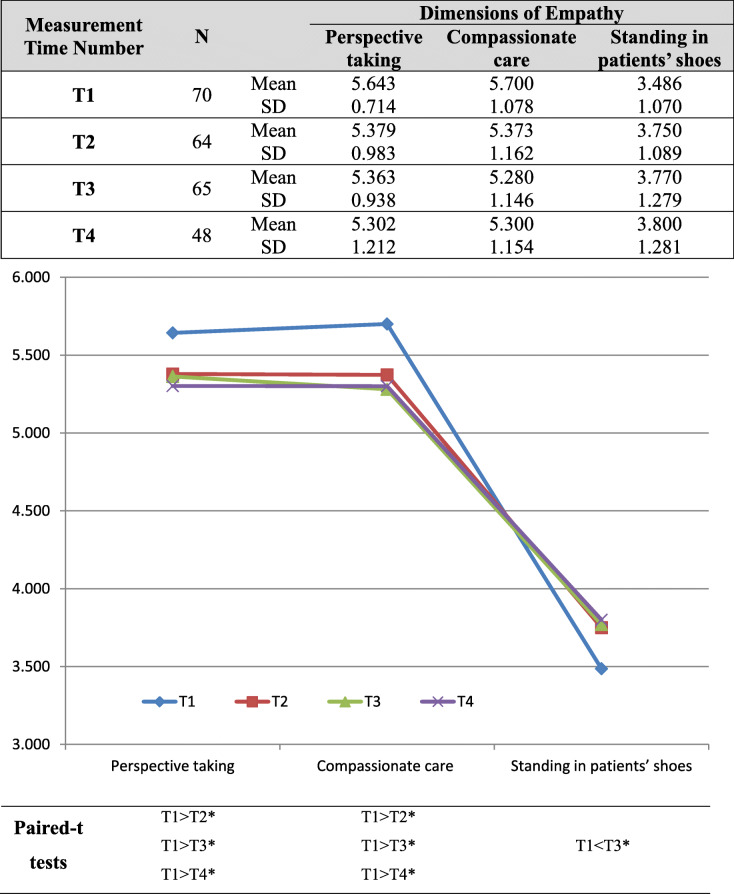
Our study revealed that changes in empathy level in the dimensions of perspective taking, compassionate care, and standing in patients’ shoes in their clinical clerkships. Relative to that at T1, their empathy decreased in perspective taking and compassionate care at T2–T4 but increased in standing in patients’ shoes at T3. Additionally, our study verified the positive effect of medical students’ preclinical SL experience in CBSTs and ECSTs on empathy in terms of compassionate care and perspective taking, respectively, but not on that of standing in patients’ shoes.
Conclusions
Separate investigations into subconstructs of empathy, such as perspective taking, compassionate care, and standing in patients’ shoes, in medical students may be necessary for exploring the various driving forces or barriers to developing empathy in medical students. Moreover, SL experience through both CBSTs and ECSTs at medical academies may have positive effects on medical students’ empathy in their clinical clerkships and should be promoted at medical schools.
Keywords: Service learning, Curriculum-based service team, Extracurricular service team, Empathy, Clinical training, Clerkships
Background
In medicine, empathy is defined as a practitioner’s ability to perceive and understand a patient’s emotional state and clearly articulate the patient’s feelings [1]. The Association for Medical Education in Europe recommended that empathy be included as a key criterion in the evaluation of academic performance and professionalism [2]. Studies have indicated a correlation between empathy and good clinical performance [3], specifically in communicative ability [4], low burnout rates [5], and improved well-being [6]. Moreover, empathy has been associated with high patient satisfaction [7–13], high medical compliance [11, 14–17], and favourable treatment results [8, 10, 14, 18–20] and reduced medical costs [21], medical errors [22], and medical malpractice [23–26]. Because of the critical role of empathy in medical training, the cultivation of empathy in medical students has been a recent topic of interest. Medical educators have endeavoured to propose methods for improving empathy in medical students; for example, by improving students’ communication skills, incorporating perspectives of medical humanities, and reforming medical curricula [1, 27]. A study in Singapore reported that community service and socialisation may be key factors affecting the demonstration of empathy in medical students [28].
Service learning (SL) is a pedagogical process that enriches conventional coursework through the inclusion of activities outside the classroom that meet the needs of the community [29]. Implementing SL early in medical training as a form of community-based learning may provide a formative experience that influences the perspectives of medical students as they enter clinical clerkships [30]. SL can be traced back to 1938, when John Dewey first argued that education in prosocial values should not occur in the abstract, such as in classrooms or lectures; rather, students should learn from real-world experience [31, 32]. SL incorporates domains of education, such as knowledge, attitudes, skills, intentions, and relationships through a process-oriented participatory approach [33]. SL facilitates the transformation of student knowledge and attitudes in the context of holistic care through work with community organisations [34] to help students become more socially responsible, patient-oriented practitioners [35]. SL is also considered a method for nurturing the service commitments of medical students while promoting interactions with the communities they serve [36, 37]. SL has been argued to transform student perspectives on humanism in medicine, including the perspectives of students who respect and empathise with the struggles and strengths of their patients and peers [38]. For example, the Loyola University Chicago Stritch School of Medicine proposed a 5-year Global Health Fieldwork Fellowship track that was grounded in clinical and service learning, doing so to foster the development of prosocial values, such as professionalism, advocacy, and social justice in their medical students [39]. SL programmes involving work with the homeless have also enhanced the professional and personal education of medical students by improving their understanding of biopsychosocial problems and by developing their empathy, compassion, and social awareness [40, 41].
The effectiveness of SL is often evaluated by assessing students’ qualitative reflections immediately following such programmes. However, in such evaluations, common-method biases may give rise to instructors posing leading questions; thus, instructors may either implicitly or explicitly make assumptions regarding participants’ responses. Few studies have longitudinally explored the effects of SL experience on empathy in medical students. Therefore, we quantitatively and longitudinally examined how preclinical SL experience at medical schools was related to medical students’ empathy in clinical training. Two methods of analysis were employed. First, we longitudinally investigated the change in the level of empathy of medical students during their clinical clerkships. Second, we explored the relationship of medical students’ preclinical SL experience with their empathy during their clerkships.
Methods
This study administered a prospective web-based survey to a cohort of medical students at one medical school in Taiwan.
Study participants
Our study involved a group of fifth-year medical students participating in clinical clerkships as part of a 7-year medical programme at a medical school in Taiwan starting in September 2015. After recruitment at the end of August 2015, 140 of 206 medical students (68%) who agreed to participate in the study returned written informed consent forms.
Measurement
Medical students’ preclinical SL experience
In higher education, SL can be fostered using various formats and is often classified as an academic course, either credited or noncredited. A curriculum-based service team (CBST) refers to a team that participates in community service activities included in credited academic courses, whether a required or elective course [37, 42, 43], with explicit learning objectives [44]. Students in CBSTs perform various activities in small groups in structured learning environments that incorporate preparation, action, reflection, and celebration under the supervision of course instructors [45]. Depending on the instructors’ curriculum design, CBSTs perform several community services that focus on one or several themes during one or more academic semesters. By contrast, extracurricular service teams (ECSTs) are composed of students in voluntary and interdisciplinary societies who perform community services that are outside the curriculum and for which academic credit is not given. ECSTs are typically led by senior students and advised by faculty members; this format is also common in Western medical schools [46, 47]. For medical students, the service themes of CBSTs and ECSTs include caring for older people, people with disabilities, or inpatients; junior student tutoring; health education and promotion; or offering free clinical services in urban, rural, or overseas regions.
In this study, medical students’ preclinical SL experience was measured in terms of their membership of CBSTs and ECSTs and their service intensity in these teams during the preclinical stage of medical school (years 1 to 4 in a 7-year programme). One questionnaire item recorded whether the medical students were members of a CBST or ECST. In terms of service intensity, respondents reported the number of service themes they were engaged in and the average number of hours they spent on planning and preparation, action, reflection, and celebration per service theme for both CBSTs and ECSTs. In another questionnaire item, the students’ reported their perceived SL self-efficacy at the preclinical stage of medical school by using a 5-point scale, with a higher score indicating greater SL efficacy.
Empathy of medical students in clinical clerkships
Several instruments have been developed to measure empathy. The Jefferson Scale of Empathy was applied in this study because it was designed not for the general population but rather for patient care situations [48]. Empathy ratings for medical students were measured using the Jefferson Scale of Physician Empathy-Student version (JSPE-S), which comprises 20 items rated on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree) [3, 48]. The JSPE-S was translated into traditional Chinese and evaluated by English language specialists and Chinese language specialists from Taiwan. An exploratory factor analysis using the principal component method (Kaiser–Meyer–Olkin statistic = 0.919) was performed first because of potential differences in responses due to perceived cultural differences (the questionnaire was originally developed in a Western country). Two items were omitted because their factor loadings were lower than 0.5 after an exploratory factor analysis using varimax rotation with Kaiser normalisation (item 1: physicians’ understanding of their patients’ feelings and the feelings of their patients’ families does not influence medical or surgical treatment; item 18: physicians should not allow themselves to be influenced by strong personal bonds between their patients and their family members). Three common factors were identified, namely perspective taking (nine items), compassionate care (seven items), and standing in patients’ shoes (two items), and their Cronbach’s α values were 0.922, 0.935, and 0.844, respectively. These three factors were adopted from Hojat et al. [3]; perspective taking refers to the students’ perception of patients’ perspectives, compassionate care refers to the students’ understanding of patients’ affective states during inpatient care, and standing in patients’ shoes refers to the students’ ability to understand patients’ experiences. Notably, these items’ locations in the three factors in this study were similar to the item distributions verified in Japanese [49] and Korean [50] studies of medical students and a US study of students of osteopathic medicine [51].
Detailed information is provided in Table 1. For further analysis, three factor scores were calculated for the three factors by using regression methods.
Table 1.
Factor structures for perceived empathy of medical students in clinical clerkships (N = 247)
| Items | Question | Mean | SD | Factor loadings | ||
|---|---|---|---|---|---|---|
| Perspective taking | Compassionate care | Standing in patients’ shoes | ||||
| Item 16 | Physicians’ understanding of the emotional status of their patients, as well as that of their families, is one important component of the physician–patient relationship. | 5.563 | 0.960 | 0.860 | ||
| Item 17 | Physicians should try to think like their patients in order to render better care. | 5.417 | 1.020 | 0.837 | ||
| Item 15 | Empathy is a therapeutic skill without which the physician’s success is limited. | 5.190 | 1.217 | 0.810 | ||
| Item 20 | I believe that empathy is an important therapeutic factor in the medical treatment. | 5.510 | 1.100 | 0.792 | ||
| Item 13 | Physicians should try to understand what is going on in their patients’ minds by paying attention to their nonverbal cues and body language. | 5.405 | 1.103 | 0.754 | ||
| Item 2 | Patients feel better when their physicians understand their feelings. | 5.749 | 0.934 | 0.709 | ||
| Item 10 | Patients value a physician’s understanding of their feelings which is therapeutic in its own right. | 5.130 | 1.243 | 0.699 | ||
| Item 4 | Understanding body language is as important as verbal communication in physician–patient relationships. | 5.729 | 0.977 | 0.672 | ||
| Item 5 | A physician’s sense of humor contributes to a better clinical outcome | 5.389 | 1.014 | 0.671 | ||
| Item 14 | I believe that emotion has no place in the treatment of medical illness. (R) | 5.619 | 1.266 | 0.859 | ||
| Item 8 | Attentiveness to patients’ personal experiences does not influence treatment outcomes. (R) | 5.360 | 1.327 | 0.857 | ||
| Item 12 | Asking patients about what is happening in their personal lives is not helpful in understanding their physical complaints. (R) | 5.514 | 1.331 | 0.852 | ||
| Item 9 | Physicians should not try to stand in their patients’ shoes when providing care to them. (R) | 5.555 | 1.357 | 0.848 | ||
| Item 7 | Attention to patients’ emotions is not important in history taking. (R) | 5.445 | 1.384 | 0.838 | ||
| Item 11 | Patients’ illnesses can be cured only by medical or surgical treatment; therefore, physicians’ emotional ties with their patients do not have a significant influence in medical or surgical treatment. (R) | 5.150 | 1.364 | 0.788 | ||
| Item 19 | I do not enjoy reading nonmedical literature or the arts. (R) | 5.304 | 1.335 | 0.701 | ||
| Item 3 | It is difficult for a physician to view things from patients’ perspectives (R) | 3.879 | 1.260 | 0.901 | ||
| Item 6 | Because people are different, it is difficult to see things from patients’ perspectives. (R) | 3.510 | 1.300 | 0.899 | ||
Note: (1) The item # in Table 1 is marked the same as that in the original version of the Jefferson Scale of Physician Empathy-Student version (JSPE-S) for readability and comparison across studies. (2) Each item was measured on a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). (3) (R) refers to reversed scores for the item (ie, 1 → 7, 2 → 6, 3 → 5, 4 → 4, 5 → 3, 6 → 2, and 7 → 1)
Background information
The medical students’ personal background information, namely sex and age, were recorded.
Data collection
Surveys were conducted at the beginning of the clerkship in September 2015 (T1), followed by three follow-up surveys in December 2015 (T2), April 2016 (T3), and August 2016 (T4). Data on the following were gathered: preclinical SL experience, specifically —membership of and service intensity in both CBST and ECST; demographic characteristics, specifically sex and age; and baseline empathy level (T1). Follow-up surveys were conducted to determine the empathy level of the medical students during their clinical clerkships (T2–T4). The completion of the follow-up surveys was voluntary, and those who completed the baseline (T1) and two or more follow-up surveys (T2–T4) were included in this study. In total, 70 medical students (response rate 34% = 100% × 70/206) with 247 responses were included in our analysis.
Statistical analysis
Descriptive statistics of the medical students’ demographic characteristics, preclinical SL experience, and longitudinal empathy level during their clerkships were analysed. Paired t tests were performed to analyse the dynamics of the medical students in terms of empathy level across the three dimensions of perspective taking, compassionate care, and standing in patients’ shoes; comparisons were performed for T1–T2, T1–T3, T1–T4, T2–T3, T2–T4, and T3–T4.
Generalised estimating equations (GEEs) were used to analyse the repeated measures of empathy in medical students according to selected predictors. Regression of the dependent variable for selected independent variables was conducted using a GEE method for the following reasons [52, 53]. First, a repeated measures analysis was employed for the dependent variable. Second, several missing values were identified for the predictors. Third, robust standard estimates were available for performing consistent and accurate tests of statistical significance. Fourth, the application of the Quasi-likelihood Information Criterion (QIC) reflected the relative efficacy of the proposed model in fitting the data. In this study, three GEEs were used for each dependent variable; a repeated measures analysis was performed on medical students’ empathy factor scores for perspective taking, compassionate care, and standing in patients’ shoes, and the students’ demographic characteristics and preclinical SL experience were applied as predictors. Notably, variables with skewness and kurtosis values greater than 2 and 7 [54], respectively, were transformed (e.g. the students’ age and total hours serving in CBSTs and ECSTs). Statistical analyses were performed using SPSS 25.0 (IBM Corporation, Chicago, IL, USA).
Results
In total, 70 medical students (men: 36, 51%; women: 34, 49%) with response rate 34% were included in our study, with an average age of 23 years. Among them, 54 students (77%) served as CBST members, engaging in an average of six service themes and spending 15 h per theme. In total, 42 students (60%) served as ECST members, engaging in an average of five service themes and spending 31 h per theme. The students reported an average SL self-efficacy score of 3.4 on a 5-point scale. Detailed information is presented in Table 2.
Table 2.
Medical students’ personal backgrounds and preclinical SL experience (N = 70)
| Variables | Scale | Mean (Frequency) | SD (Percentage) |
|---|---|---|---|
| Demographic characteristics | |||
| Sex | Male | (36) | (51) |
| Female | (34) | (49) | |
| Age | 23.486 | 2.005 | |
| Preclinical SL experience | |||
| CBST membership | No | (16) | (23) |
| Yes | (54) | (77) | |
| CBST service intensity: the number of service themes the student engaged in | 6.069 | 6.250 | |
| CBST service intensity: the average time spent per service theme (hrs) | 14.987 | 30.177 | |
| ECST membership | No | (28) | (40) |
| Yes | (42) | (60) | |
| ECST service intensity: the number of service themes the student engaged in | 4.579 | 10.485 | |
| ECST service intensity: the average time spent per service theme (hrs) | 31.029 | 66.420 | |
| Perceived SL self-efficacy (5-point scale) | 3.400 | 0.824 | |
Note: SL: service learning; CBST: curriculum-based service team; ECST: extracurricular service team
Three dimensions of empathy level (perspective taking, compassionate care, and standing in patients’ shoes) were measured over four periods (T1, T2, T3, and T4). The T1, T2, T3, and T4 evaluations were completed by 70, 64, 65, and 48 students, respectively (Table 3). Paired t tests were performed for individual comparisons at two time points; the results revealed that the scores for perspective taking at T2, T3, and T4 were lower than those at T1, and the scores for compassionate care at T2, T3, and T4 were significantly lower than those at T1 (p < 0.05). By contrast, the score for standing in patients’ shoes at T1 was significantly lower than that at T3 (p < 0.05). Detailed information is listed in Table 3.
Table 3.
Medical students’ empathy level across four timelines (N = 247)
Note: *p < 0.05
Table 4 illustrates the GEE results for the effects of predictor variables in repeated measures of medical students’ empathy level in the individual dimensions of perspective taking, compassionate care, and standing in patients’ shoes. The results revealed that (1) the students’ preclinical experience measured by total hours serving in ECSTs was positively related to their empathy in terms of perspective taking (p < 0.05) and (2) that in CBSTs was positively related to students’ empathy in terms of compassionate care (p < 0.05). However, the medical students’ preclinical SL experience in CBSTs and ECSTs was not related to their empathy in terms of standing in patients’ shoes (p > 0.05).
Table 4.
Relationships of medical students’ preclinical SL experience with their empathy level in clinical clerkships: Generalised estimating equation modelling
| Variables | Dimensions of Empathy | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Perspective taking | Compassionate care | Standing in patients’ shoes | |||||||
| Estimates | SE | Sig | Estimates | SE | Sig | Estimates | SE | Sig | |
| Intercept | −1.074 | 1.253 | 0.391 | −1.880 | 1.176 | 0.110 | 1.375 | 1.215 | 0.258 |
| Preclinical SL experience | |||||||||
| CBST membership (default = no) | −0.054 | 0.272 | 0.843 | −0.132 | 0.309 | 0.669 | −0.065 | 0.248 | 0.792 |
| CBST service intensity: total hours serveda | −0.019 | 0.013 | 0.161 | 0.031 | 0.012 | 0.012 | −0.011 | 0.016 | 0.482 |
| ECST membership (default = no) | 0.041 | 0.247 | 0.868 | 0.492 | 0.253 | 0.052 | 0.162 | 0.233 | 0.487 |
| ECST service intensity: total hours servedb | 0.008 | 0.003 | 0.013 | 0.003 | 0.003 | 0.274 | 0.006 | 0.004 | 0.101 |
| Perceived SL self-efficacy | 0.247 | 0.137 | 0.071 | −0.186 | 0.120 | 0.121 | 0.194 | 0.150 | 0.197 |
| Demographic characteristics | |||||||||
| SEX (default = male) | −0.095 | 0.194 | 0.625 | −0.070 | 0.200 | 0.728 | −0.191 | 0.181 | 0.290 |
| AGEc | −0.329 | 1.067 | 0.758 | −1.826 | 1.098 | 0.096 | 1.737 | 1.082 | 0.109 |
| Model fit |
QIC = 1020.826 QICC = 252.786 |
QIC = 846.987 QICC = 246.639 |
QIC = 1123.132 QICC = 245.870 |
||||||
Note:
1. SL: service learning; CBST: curriculum-based service team; ECST: extracurricular service team
2. aCBST service intensity: total hours served was calculated by multiplying the number of service themes a student was engaged in by the average number of hours spent per CBST service theme. The original value of total hours engaged in CBST was transformed using the square root value to meet the assumption of normality
3. bECST service intensity: total hours served was calculated by multiplying the number of service themes a student engaged in by the average number of hours spent per ECST service theme. The original value of total hours engaged in ECST was transformed using square root value to meet the assumption of normality
4. cThe original AGE value was transformed using LN(LN(LG(X))) because of the violation of the normality assumption
Discussion
After longitudinally tracking the empathy levels of 70 medical students during their clerkships for 1 year (i.e. four iterations:T1–T4), our study revealed various changes in empathy level across the dimensions of perspective taking, compassionate care, and standing in patients’ shoes. Specifically, relative to that in T1, the students’ empathy decreased in perspective taking and compassionate care at T2–T4 but increased in standing in patients’ shoes at T3. In addition, our study verified the positive relationship of medical students’ preclinical SL experience in CBSTs and ECSTs on compassionate care and perspective taking, respectively, but not on standing in patients’ shoes in terms of empathy level during their clinical clerkships.
Previous studies have employed a cross-sectional approach and the JSPE-S to determine the empathy level of medical students during medical school, and diverse findings have been reported; for example, in terms of changes in medical student empathy during medical school, several studies have reported decreasing levels [55–60], several have reported increasing levels [49, 50, 61, 62], and others have reported no statistically significant differences [63]. Notably, the cross-sectional designs applied in these studies could not account for the developmental trajectory of medical students or allow for repeated testing. To address these limitations, Costa et al. [64] conducted longitudinal research to collect data on the empathy of preclinical medical students; their results revealed no decline in the medical students’ empathy over time. However, we argue that summed empathy scores might hamper the identification of individual items or distinctive characteristics across the many dimensions of empathy. Therefore, by employing longitudinal tracking of the subconstructs of empathy in medical students, our study discovered that empathy decreased in the dimensions of perspective taking and compassionate care but increased in that of standing in patients’ shoes (Table 3, paired t tests, p < 0.05). A previous study employed the JSPE at the beginning (pretest) and end (posttest) of medical students’ third year of clerkship at a medical school in the United States, noting statistically significant declines in empathy scores for items 2, 10, 11, 12, and 15, which related most closely to the dimensions of perspective taking and compassionate care [65]; these results are consistent with the current findings (Tables 1 and 3). We content that separate investigations into the subconstructs of empathy, such as perspective taking, compassionate care, and standing in patients’ shoes, in medical students enable future investigations of various potential driving factors of or barriers to the development of empathy with respect to these subconstructs.
Most importantly, our study verified the benefits of CBST in cultivating empathy with respect to compassionate care during clinical clerkships (p < .01). The items under compassionate care indicate how much respondents regard health and illness from a holistic perspective; that is, the medical practitioner considers medicine from not only a biomedical perspective (as a science) but also from a psychosocial perspective (as an art) [48]. CBSTs are typically incorporated into various educational domains by instructors to influence students’ planning and preparation, behaviour, reflection and demonstration, and assessment and celebration [32]. By discussing learning objectives with instructors and community partners in academic courses, students can enhance their awareness and gain deeper insights into social problems to identify social needs and acquire strong problem-solving skills [66–68]. Therefore, we argue that the explicit learning objectives of CBSTs are related to cognitive ability, as reflected by academic performance, civic engagement, social skills, and improved attitudes towards the self [69–71]. Therefore, helping medical students regard patient services from a systematic perspective and holistically understand patient concerns may benefit medical students and help them perform compassionate care during their clinical training.
Furthermore, we revealed that engagement in ECSTs helps medical students cultivate empathy with respect to perspective taking during their clinical clerkship (p < .05). The items related to the subconstruct of perspective taking emphasised empathy in interpersonal relationships when determining patients’ cognitive status [48]. ECSTs are typically led by senior students and advised by school faculty [46] and are typically composed of students from many disciplines who collaborate to solve community problems. Such teamwork may provide opportunities for students to build relationships with their partners, faculty, the community, or people they serve to reinforce school and community ties and encourage collaboration [67, 72, 73]. Moreover, an interprofessional service and learning experience was reported to generate the greatest effect on medical students’ perceptions of their competency and training in other disciplines [74]. Moreover, students can apply problem-solving and learning cycles to promote deep learning through service delivery [75]. Therefore, we maintain that ECSTs may provide opportunities to improve medical students’ social awareness and cultural competency in relation to their student peers from other disciplines and their community partners from a diversity of backgrounds [47], thereby increasing their empathy in perspective taking towards patients following their clinical clerkships.
Although our study revealed that medical students’ empathy in terms of standing in patients’ shoes increased in clinical clerkships at T3 (Table 3), we could not verify the potential benefits of SL experience on medical students’ empathy in terms of standing in patients’ shoes (Table 4). Santiago et al. [76] compared medical students’ empathy at two medical schools and argued that student empathy could be increased by implementing earlier and more intensive contact with patients under the supervision of skilled tutors. We contend that clinical training is essential for medical students to learn how to manage real-life situations, and through clinical training, medical students are encouraged to regularly interact with real patients to enhance their practical knowledge [77]. By learning to understand patients’ experiences, medical students gradually develop the ability to provide exceptional medical care during clinical training.
This study has several limitations. First, the service intensity (i.e. the number of service themes engaged in and the average time spent per service theme) of medical students’ SL experience was aggregated across various services themes in CBSTs and ECSTs because of the limited sample size. Thus, we were unable to analyse the effectiveness of individual service themes in SL experience. Second, the SL experience of medical students was analysed only in the context of the preclinical stage of their medical school, and their self-reported information on SL experience may have been affected by recall bias. Third, the successful implementation of CBSTs and ECSTs requires careful planning, the deliberate articulation of rationales and expectations, the strengthening of community relationships, and the conduct of iterated reviews and revisions to the programme [78]. Insufficient time, resources, and effort for effective implementation may burden students and educators with record keeping, transportation, and scheduling [79]. Thus, we could not confirm the quality of the CBST and ECST values reported by the medical students in our study, which may have confounded the effectiveness of SL experience. Fourth, the inclusion of medical students from only one medical school and the small sample size (response rate 34%) with potential respondent bias may hamper the generalizability of the study findings. We got the medical students’ written informed consents around 68% of the cohort of medical students in the study recruitment stage. However, in order to catch the dynamics of the medical students’ empathy levels in their clinical training given the participants’ voluntary survey responses, so as to enhance our study contributions on exploring the SL effects on empathy longitudinally, we might make the trade-off to include the small size (response rate 34%) in our data analysis. Moreover, to assess how medical students’ SL effectiveness is sustained over time, we might call for action to routinely collect or record the medical students’ well-being and soft skills such as empathy into their learning portfolio, especially at their socialization in the clinical training, even after clerkships or postgraduate medical training.
Conclusion
Our study quantitatively and longitudinally explored how medical students’ preclinical SL experience was related to their empathy in clinical clerkships. We found that medical students’ empathy level in their clinical clerkships exhibited different patterns (increasing or decreasing) across the dimensions of perspective taking, compassionate care, and standing in patients’ shoes. Moreover, our study revealed that SL experience in both CBSTs and ECSTs at medical academies may have positive effects on medical students’ empathy in their clinical clerkships and should be promoted at medical schools.
Acknowledgments
The authors thank the Taiwan Ministry of Science and Technology for funding (NSC 102- 2511-S-039-001-MY3, MOST104-2815-C-039-066-U, MOST108-2410-H-182-011-SS3) and supporting the academic and administrative processes in this study. This manuscript was edited by Wallace Academic Editing.
Authors’ contributions
YSY and PCL contributed to the conception and design of the work; the acquisition and interpretation of data; drafting the work. YKL, CDL, and DYC contributed to the acquisition, analysis, and interpretation of data; and revising it critically for important intellectual content. BYJL contributed to the conception and design of the work; the acquisition, analysis, and interpretation of data; drafting the work; and revising it critically for important intellectual content. All the authors made a final approval of the version to be published and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
Taiwan Ministry of Science and Technology provide the funds for this study’s academic and administrative processes and publication (NSC 102–2511-S-039-001-MY3, MOST104–2815-C-039-066-U, MOST108–2410-H-182-011-SS3). The funding body played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The data included in this study, with departmental information and student identities removed, are available for use on reapproval by any eligible research ethics committee.
Declarations
Ethics approval and consent to participate
This work received ethical approval from the Institutional Review Board of China Medical University and Hospital (CMUH105-REC3–001). All participants provided written statements of informed consent. All the study protocol for involving humans was in accordance to guidelines of Declaration of Helsinki in the manuscript.
Consent for publication
Not applicable.
Competing interests
Blossom Yen-Ju Lin, is a member of the editorial board of BMC Medical Education. All authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Stepien KA, Baernstein A. Educating for empathy: a review. J Gen Intern Med. 2006;21(5):524–530. doi: 10.1111/j.1525-1497.2006.00443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hojat M, Erdmann JB, Gonnella JS. Personality assessments and outcomes in medical education and the practice of medicine: AMEE guide no. 79. Med Teach. 2013;35(7):e1267–e1301. doi: 10.3109/0142159X.2013.785654. [DOI] [PubMed] [Google Scholar]
- 3.Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, Callahan CA, Magee M. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36(6):522–527. doi: 10.1046/j.1365-2923.2002.01234.x. [DOI] [PubMed] [Google Scholar]
- 4.Casas RS, Xuan Z, Jackson AH, Stanfield LE, Harvey NC, Chen DC. Associations of medical student empathy with clinical competence. Patient Educ Couns. 2017;100(4):742–747. doi: 10.1016/j.pec.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Thomas MR, Dyrbye LN, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, Shanafelt TD. How do distress and well-being relate to medical student empathy? A multicenter study. J Gen Intern Med. 2007;22(2):177–183. doi: 10.1007/s11606-006-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ. 2014;14(1):219. doi: 10.1186/1472-6920-14-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bertakis KD, Roter D, Putnam SM. The relationship of physician medical interview style to patient satisfaction. J Fam Pract. 1991;32(2):175–181. [PubMed] [Google Scholar]
- 8.Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76–e84. doi: 10.3399/bjgp13X660814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Epstein RM, Hadee T, Carroll J, Meldrum SC, Lardner J, Shields CG. Could this be something serious? Reassurance, uncertainty, and empathy in response to patients’ expressions of worry. J Gen Intern Med. 2007;22(12):1731–1739. doi: 10.1007/s11606-007-0416-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hojat M, Louis DZ, Maxwell K, Markham FW, Wender RC, Gonnella JS. A brief instrument to measure patients’ overall satisfaction with primary care physicians. Fam Med. 2011;43(6):412–417. [PubMed] [Google Scholar]
- 11.Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237–251. doi: 10.1177/0163278704267037. [DOI] [PubMed] [Google Scholar]
- 12.Pollack KI, Alexander SC, Tulsky JA, Lyna P, Coffman CJ, Dolor RJ, Gulbrandsen P, Ostbye T. Physician empathy and listening: associations with patient satisfaction and autonomy. J Am Board Fam Med. 2011;24(6):665–672. doi: 10.3122/jabfm.2011.06.110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zachariae R, Pedersen CG, Jensen AB, Ehrnrooth E, Rossen PB, Von der Maase H. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br J Cancer. 2003;88(5):658–665. doi: 10.1038/sj.bjc.6600798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Attar HS, Chandramani S. Impact of physician empathy on migraine disability and migraineur compliance. Ann Indian Acad Neurol. 2012;15(Suppl 1):S89–S94. doi: 10.4103/0972-2327.100025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Squier RW. A model of empathic understanding and adherence to treatment regimens in practitioner-patient relationships. Soc Sci Med. 1990;30(3):325–339. doi: 10.1016/0277-9536(90)90188-X. [DOI] [PubMed] [Google Scholar]
- 16.Stewart MA. What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med. 1984;19(2):167–175. doi: 10.1016/0277-9536(84)90284-3. [DOI] [PubMed] [Google Scholar]
- 17.Zolnierek KB. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lobchuk MM, Bokhari SA. Linkages among empathic behaviors, physical symptoms, and psychological distress in patients with ovarian cancer: a pilot study. Oncol Nurs Forum. 2008;35(5):808–814. doi: 10.1188/08.ONF.808-814. [DOI] [PubMed] [Google Scholar]
- 19.Rakel D, Barrett B, Zhang Z, Hoeft T, Chewning B, Marchard L, Scheder J. Perceptions of empathy in the therapeutic encounter: effects on the common cold. Patient Educ Couns. 2011;85(3):390–397. doi: 10.1016/j.pec.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rakel DP, Hoeft TJ, Barrett BP, Chewning BA, Craig BM, Niu M. Practitioner empathy and the duration of the common cold. Fam Med. 2009;41(7):494–501. [PMC free article] [PubMed] [Google Scholar]
- 21.Epstein RM, Franks P, Shields CG, Meldrum SC, Miller KN, Campbell TL, Fiscella K. Patient-centered communication and diagnostic testing. Ann Fam Med. 2015;3(5):415–421. doi: 10.1370/afm.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, Shanafelt TD. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 23.Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. 1994;154(12):1365–1370. doi: 10.1001/archinte.1994.00420120093010. [DOI] [PubMed] [Google Scholar]
- 24.Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277(7):553–559. doi: 10.1001/jama.1997.03540310051034. [DOI] [PubMed] [Google Scholar]
- 25.Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med. 2000;173(4):244–250. doi: 10.1136/ewjm.173.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silvester J, Patterson F, Koczwara A, Ferguson E. "Trust me...": psychological and behavioral predictors of perceived physician empathy. J Appl Psychol. 2007;92(2):519–527. doi: 10.1037/0021-9010.92.2.519. [DOI] [PubMed] [Google Scholar]
- 27.Jeffrey D, Downie R. Empathy - can it be taught? J R Coll Physicians Edinb. 2016;46(2):107–112. doi: 10.4997/JRCPE.2016.210. [DOI] [PubMed] [Google Scholar]
- 28.Sng G, Tung J, Ping YS, Lee SS, Win MT, Hooi SC, Samarasekera DD. Complex and novel determinants of empathy change in medical students. Korean J Med Educ. 2016;28(1):67–78. doi: 10.3946/kjme.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kimbler KJ, Ehman AC. Gerontology and youth-focused service learning: the relation between service recipient age and student responses. Gerontol Geriatr Educ. 2015;36(4):384–395. doi: 10.1080/02701960.2014.925890. [DOI] [PubMed] [Google Scholar]
- 30.Buckner AV, Ndjakani YD, Banks B, Blumenthal DS. Using service-learning to teach community health: the Morehouse School of Medicine community health course. Acad Med. 2010;85(10):1645–1651. doi: 10.1097/ACM.0b013e3181f08348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seifer SD. Service-learning: community-campus partnerships for health professions education. Acad Med. 1998;73(3):273–277. doi: 10.1097/00001888-199803000-00015. [DOI] [PubMed] [Google Scholar]
- 32.Stewart T, Wubbena Z. An overview of infusing service-learning in medical education. Int J Med Educ. 2014;5:147–156. doi: 10.5116/ijme.53ae.c907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Du Toit E, Olivera S, Topper K, van de Venter R, Williams M, Ventres W. Toward interprofessional service-learning and social accountability in health: one south African University's process-oriented-participatory journey. J Interprof Care. 2019;33(3):291–294. doi: 10.1080/13561820.2018.1532399. [DOI] [PubMed] [Google Scholar]
- 34.Playford D, Bailey S, Fisher C, Stasinska A, Marshall L, Gawlinski M, Young S. Twelve tips for implementing effective service learning. Med Teach. 2019;41(1):24–27. doi: 10.1080/0142159X.2017.1401217. [DOI] [PubMed] [Google Scholar]
- 35.Olney CA, Livingston JE, Fisch S, Talamantes MA. Becoming better health care providers: outcomes of a primary care service-learning project in medical school. J Prev Interv Commun. 2006;32(1–2):133–147. doi: 10.1300/J005v32n01_09. [DOI] [PubMed] [Google Scholar]
- 36.Belkowitz J, Sanders LM, Zhang C, Agarwal G, Lichtstein D, Mechaber AJ, Chung EK. Teaching health advocacy to medical students: a comparison study. J Public Health Manag Pract. 2014;20(6):E10–E19. doi: 10.1097/PHH.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 37.Elam CL, Sauer MJ, Stratton TD, Skelton J, Crocker D, Musick DW. Service learning in the medical curriculum: developing and evaluating an elective experience. Teach Learn Med. 2013;15(3):194–203. doi: 10.1207/S15328015TLM1503_08. [DOI] [PubMed] [Google Scholar]
- 38.Lee WK, Harris CCD, Mortensen KA, Long LM, Sugimoto-Matsuda J. Enhancing student perspectives of humanism in medicine: reflections from the Kalaupapa service learning project. BMC Med Educ. 2016;16(1):137. doi: 10.1186/s12909-016-0664-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Borah BF. Longitudinal service learning in medical education: an ethical analysis of the five-year alternative curriculum at Stritch School of Medicine. J Med Humanit. 2018;39(4):407–416. doi: 10.1007/s10912-018-9529-x. [DOI] [PubMed] [Google Scholar]
- 40.Chrisman-Khawam L, Abdullah N, Dhoopar A. Teaching health-care trainees empathy and homelessness IQ through service learning, reflective practice, and altruistic attribution. Int J Psychiatry Med. 2017;52(3):245–254. doi: 10.1177/0091217417730288. [DOI] [PubMed] [Google Scholar]
- 41.Clark DL, Melillo A, Wallace D, Pierrel S, Buck DS. A multidisciplinary, learner-centered, student-run clinic for the homeless. Fam Med. 2003;35(6):394–397. [PubMed] [Google Scholar]
- 42.Averill NJ, Sallee JM, Robinson JT, McFarlin JM, Montgomery AA, Burkhardt GA, Schulz-Burton MD, Elam CL. A first-year community-based service learning elective: design, implementation, and reflection. Teach Learn Med. 2007;19(1):47–54. doi: 10.1080/10401330709336623. [DOI] [PubMed] [Google Scholar]
- 43.Borges N, Hartung PJ. Service learning in medical education: project description and evaluation. Int J Teach Learn High Educ. 2007;19:1–7. [Google Scholar]
- 44.Spring K, Grimm R, Dietz N. Community Service and Service Learning in America’s Schools. Washington DC: Corporation for National and Community Service; 2008.
- 45.Hancock CR, Shenk D, George J. Balancing structure and choice in intergenerational service-learning. Gerontol Geriatr Educ. 2013;34(2):115–134. doi: 10.1080/02701960.2012.679371. [DOI] [PubMed] [Google Scholar]
- 46.McWilliams A, Rosemond C, Roberts E, Calleson D, Busby-Whitehead J. An innovative home-based interdisciplinary service-learning experience. Gerontol Geriatr Educ. 2008;28(3):89–104. doi: 10.1300/J021v28n03_07. [DOI] [PubMed] [Google Scholar]
- 47.Sin D, Chew T, Chia TK, Ser JS, Sayampanathan A, Koh G. Evaluation of constructing care collaboration - nurturing empathy and peer-to-peer learning in medical students who participate in voluntary structured service learning programmes for migrant workers. BMC Med Educ. 2019;19(1):304. doi: 10.1186/s12909-019-1740-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, Veloski J, Magee M. The Jefferson scale of physician empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349–365. doi: 10.1177/00131640121971158. [DOI] [Google Scholar]
- 49.Kataoka HU, Koide N, Ochi K, Hojat M, Gonnella JS. Measurement of empathy among Japanese medical students: psychometrics and score differences by gender and level of medical education. Acad Med. 2009;84(9):1192–1197. doi: 10.1097/ACM.0b013e3181b180d4. [DOI] [PubMed] [Google Scholar]
- 50.Roh M, Hahm B, Lee D, Suh D. Evaluation of empathy among Korean medical students: a cross-sectional study using the Korean version of the Jefferson scale of physician empathy. Teach Learn Med. 2010;22(3):167–171. doi: 10.1080/10401334.2010.488191. [DOI] [PubMed] [Google Scholar]
- 51.Hojat M, DeSantis J, Shannon SC, Mortensen LH, Speicher MR, Bragan L, LaNoue M, Calabrese LH. The Jefferson scale of empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ Theory Pract. 2018;23(5):899–920. doi: 10.1007/s10459-018-9839-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organ Res Methods. 2004;7(2):127–150. doi: 10.1177/1094428104263672. [DOI] [Google Scholar]
- 53.Wan TTH, Lin YL, Ortiz J. Contextual, ecological and organizational variations in risk-adjusted COPD and asthma hospitalization rates of rural Medicare beneficiaries. Res Sociol Health Care. 2016;34:135–152. doi: 10.1108/S0275-495920160000034008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kline R. Principles and practice of structural equations modeling. 2. London: Guilford Press; 2005. [Google Scholar]
- 55.Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434–1438. doi: 10.1007/s11606-007-0298-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khademalhosseini M, Khademalhosseini Z, Mahmoodian F. Comparison of empathy score among medical students in both basic and clinical levels. J Adv Med Educ Prof. 2014;2(2):88–91. [PMC free article] [PubMed] [Google Scholar]
- 57.Nunes P, Williams S, Sa B, Stevenson K. A study of empathy decline in students from five health disciplines during their first year of training. Int J Med Educ. 2011;2:12–17. doi: 10.5116/ijme.4d47.ddb0. [DOI] [Google Scholar]
- 58.Shashikumar R, Chaudhary R, Ryali VS, Bhat PS, Srivastava K, Prakash J, Basannar D. Cross sectional assessment of empathy among undergraduates from a medical college. Med J Armed Forces India. 2014;70(2):179–185. doi: 10.1016/j.mjafi.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williams B, Sadasivan S, Kadirvelu A. Malaysian medical students' self-reported empathy: a cross-sectional comparative study. Med J Malaysia. 2015;70(2):76–80. [PubMed] [Google Scholar]
- 60.Youssef FF, Nunes P, Sa B, Williams S. An exploration of changes in cognitive and emotional empathy among medical students in the Caribbean. Int J Med Educ. 2014;5:185–192. doi: 10.5116/ijme.5412.e641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Magalhães E, Salgueira AP, Costa P, Costa MJ. Empathy in senior year and first year medical students: a cross-sectional study. BMC Med Educ. 2011;11(1):52. doi: 10.1186/1472-6920-11-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mostafa A, Hoque R, Mostafa M, Rana MM, Mostafa F. Empathy in undergraduate medical students of Bangladesh: psychometric analysis and differences by gender, academic year, and specialty preferences. ISRN Psychiatry. 2014;2014:375439. 10.1155/2014/375439. [DOI] [PMC free article] [PubMed]
- 63.Rahimi-madiseh M, Tavakol M, Dennick R, Nasiri J. Empathy in Iranian medical students: a preliminary psychometric analysis and differences by gender and year of medical school. Med Teach. 2010;32(11):471–478. doi: 10.3109/0142159X.2010.509419. [DOI] [PubMed] [Google Scholar]
- 64.Costa P, Magalhães E, Costa MJ. A latent growth model suggests that empathy of medical students does not decline over time. Adv Health Sci Educ Theory Pract. 2013;18(3):509–522. doi: 10.1007/s10459-012-9390-z. [DOI] [PubMed] [Google Scholar]
- 65.Hojat M, Mangione S, Nasca TJ, Rattner S, Erdmann JB, Gonnella JS, Magee M. An empirical study of decline in empathy in medical school. Med Educ. 2004;38(9):934–941. doi: 10.1111/j.1365-2929.2004.01911.x. [DOI] [PubMed] [Google Scholar]
- 66.Boss JA. The effect of community service work on the moral development of college ethics students. J Moral Educ. 1994;23(2):183–198. doi: 10.1080/0305724940230206. [DOI] [Google Scholar]
- 67.Eyler J, Giles DE., Jr . Where's the Learning in Service-Learning? Jossey-Bass Higher and Adult Education Series. San Francisco: Jossey-Bass, Inc.; 1999. [Google Scholar]
- 68.Jacoby B. Service-Learning in Higher Education: Concepts and Practices. The Jossey-Bass Higher and Adult Education Series. San Francisco: Jossey-Bass Publishers; 1999. [Google Scholar]
- 69.Celio CI, Durlak J, Dymnicki A. A meta-analysis of the impact of service-learning on students. J Exp Educ. 2011;34(2):164–181. [Google Scholar]
- 70.McLellan JA, Youniss J. Two systems of youth service: determinants of voluntary and required youth community service. J Youth Adolesc. 2003;32(1):47–58. doi: 10.1023/A:1021032407300. [DOI] [Google Scholar]
- 71.Shumer R. Community-based learning: humanizing education. J Adolesc. 1994;17(4):357–367. doi: 10.1006/jado.1994.1032. [DOI] [Google Scholar]
- 72.Asheer S, Zlef S, Neild R. Roadmap for effective school-based practices to support expectant and parenting youth: lessons from the New Heights program in Washington, DC. Matern Child Health J. 2020;24(Suppl 2):125–131. doi: 10.1007/s10995-020-02986-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Eyler J. Reflecting on service: helping nursing students get the most from service-learning. J Nurs Educ. 2002;41(10):453–456. doi: 10.3928/0148-4834-20021001-10. [DOI] [PubMed] [Google Scholar]
- 74.Jones KJ, Vandenberg EV, Bottsford L. Prevalence, formation, maintenance, and evaluation of interdisciplinary student aging interest groups. Gerontol Geriatr Educ. 2011;32(4):321–341. doi: 10.1080/02701960.2011.618958. [DOI] [PubMed] [Google Scholar]
- 75.Anderson ES, Lennox A. The LeiECSTer model of Interprofessional education: developing, delivering and learning from student voices for 10 years. J Interprof Care. 2009;23(6):557–573. doi: 10.3109/13561820903051451. [DOI] [PubMed] [Google Scholar]
- 76.Santiago LM, Rosendo I, Coutinho ML, Maurício KS, Neto I, Simões JA. Comparing empathy in medical students of two Portuguese medicine schools. BMC Med Educ. 2020;20(1):153. doi: 10.1186/s12909-020-02034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wilson BG, Myers KM. Situated cognition in theoretical and practical context. In: Johassen D, Land S, editors. Theoretical foundations of learning environments. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- 78.Raskoff S, Sundeen R. Community service programs in high schools. Law Contemp Probl. 1999;62(4):73–111. doi: 10.2307/1192268. [DOI] [Google Scholar]
- 79.Tsueng G, Kumar A, Nanis SM, Su AI. Aligning needs: integration citizen science efforts into schools through service requirements. Hum Comput (Fairfax) 2019;6(1):56–82. doi: 10.15346/hc.v6i1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data included in this study, with departmental information and student identities removed, are available for use on reapproval by any eligible research ethics committee.