Abstract
Exposure to acute versus chronic stressors and threats activates the immune system in adaptive and maladaptive manners, respectively. While acute activation of the immune system in response to threat is homeostatically regulated by glucocorticoid negative feedback, chronic activation of the immune system arising from persistent stress exposure can contribute to an allostatic load with an inflammatory diathesis that has been implicated in stress-related psychopathology, including of depression and anxiety. Increased inflammation in the periphery and in the brain arising from chronic stress exposure can alter neurotransmitter metabolism and impact activation of brain regions to increase adverse behavioral health symptoms (e.g. anhedonia, anxiety, fatigue) and emotion dysregulation. While interventions targeting the immune system and its downstream effects on the brain for the treatment of depression and other psychiatric disorders has been of great interest as they have shown some efficacy in treating stress-related behavioral health disorders, future studies are necessary to better characterize the contexts under which anti-inflammatory agents should be used to treat stress-related psychopathology.
Introduction.
Exposure to a vast array of stressors is pervasive throughout our modern-day society, and contributes significantly to the risk for adverse behavioral outcomes, including depression and anxiety (1). One critical player in the response to stress and its impact on health is the immune system, which includes both innate and adaptive immune responses. Of special relevance is that the context (e.g. acute versus chronic) of stress exposure can significantly influence how the organism and the immune system responds to threat. While acute activation of the immune system in response to threat is homeostatically regulated by neuroendocrine mechanisms, chronic activation of the immune system arising from persistent stress exposure can contribute to an allostatic load with an inflammatory diathesis that has been implicated in the pathophysiology of mood and anxiety disorders (1). Herein we will review the immunology of acute and chronic stress exposure, integrate this discussion with the emerging literature linking heightened immune activation and inflammation to mood and anxiety disorders, and consider the translational implications of the immune system’s role in these psychiatric conditions.
Homeostatic regulation of immune activation in response to acute stress exposure.
In the context of acute stressor exposure, rapid engagement of the sympathetic nervous system (SNS) results in the activation of cells mediating the innate and adaptive immune response via efferent projections from the SNS to the bone marrow and lymphoid tissues to prepare the body for injury and wound repair that may result from a threat (2). The innate immune response functions quickly (within minutes to hours) to provide organismal defense against pathogens and/or tissue damage or destruction from wounding. This natural immunity is mediated by an array of leukocytes, including granulocytes (neutrophils, eosinophils, basophils, and mast cells), monocytes/macrophages, and natural killer (NK) cells, which produce inflammation (e.g. cytokines and reactive oxygen species) and engage in phagocytosis to destroy and dispose of the pathogens, respectively and initiate the wound healing process. While innate immunity is fast-acting upon threat exposure, acquired immunity requires days to generate response to specific pathogens. Cells mediating acquired immunity include different classes of lymphocytes that express antigen-specific receptor sites on their surfaces. The release of adrenaline and noradrenaline from the sympathetic-adrenal-medullary axis upon threat exposure activates monocytes/macrophages and lymphocytes via beta-adrenergic receptors to induce the innate and specific immune responses (3), respectively.
Upon exposure to an acute stressor, SNS signaling via adrenaline and noradrenaline induces rapid alterations in the absolute numbers and the proportion of leukocytes in circulation that function to traffic immune cells to sites of wounds across vertebrate species, including humans (4). This occurs in tandem with a redistribution of leukocytes within compartments critical for immune system function, as there is an initial increase in lymphocytes and monocytes in the blood that is subsequently followed by a decrease as these cells enter organ compartments, such as the skin, lungs and lymph nodes, that may be a site of wounding and/or infiltration by pathogens (2). For instance, acute stress exposure (e.g. physical restraint) in mice results in a more robust increase in the infiltration of leukocytes, including neutrophils, macrophages, and NK and T cells, at the site of surgery or wounding (5). A concomitant upregulation in gene expression of pro-inflammatory gene expression, including tumor necrosis factor (TNF), interferon gamma (IFNg), and interleukins 1beta (IL-1b) and 6 (IL-6), occurs upon at the site of this acute-stress induced redistribution of immune cells (6).
The ability of acute stress exposure to induce changes in gene expression is mediated by the activity of nuclear factor-κB (NF-κB), a redox-sensitive transcription factor whose activity increases pro-inflammatory cytokine secretion from mononuclear cells. More specifically, translational studies show that increases in noradrenaline following acute psychosocial stress (e.g. Trier Social Stress Test; TSST) and immobilization (e.g. restraint) stress exposure, in humans and mice respectively activates NF-κB to induce IL-6 release (7). In vitro and in vivo studies also show that pharmacological blockade of adrenergic signaling via a1-adrenergic antagonists blocks this stress-induced NF-κB activity (7). It is important to note however that the ability for adrenaline to induce pro- or anti-inflammatory cascades within the innate immune system is dependent upon cell-specific expression of different beta-adrenergic receptors subtypes (3).
Adrenaline and noradrenaline release upon threat-induced activation of the sympathetic-adrenomedullary axis occurs in tandem with aldosterone release that acts via mineralocorticoid receptors to decrease neutrophils, helper T cells and NK (8). Parallel threat-induced activation of the hypothalamic-pituitary-adrenal (HPA) axis results in de novo cortisol synthesis and release from the adrenal cortex that acts via glucocorticoid receptors to impact immune cell distribution and activity (8). Low concentrations of corticosterone in rodents have been shown to enhance acute stress-induces redistribution of T cells and delayed-type hypersensitivity (DTH) of the skin, while also leading to trafficking of immune cells to the brain (meninges) in association with decreased anxiety-like behavior (9). In contrast, high doses and chronic doses of corticosterone or the synthetic glucocorticoid dexamethasone suppress DHT (10) and increase anxiety- and depressive-like behaviors in laboratory animals. This bimodal, or biphasic, response of the immune system to acute stress-induced release of glucocorticoids is dependent upon negative feedback mechanisms at the level of glucocorticoid receptor to inhibit NF-κB and the downstream release of pro-inflammatory cytokines, and act to restore homeostasis (11). Taken together, existing data indicate that acute stress exposure enhances innate and acquired immunity to increase the chances of organismal survival in the face of potential wounding and pathogen entry, while chronic exposure to stress may have more detrimental effects.
Chronic stress-induced allostasis facilitates increased systemic inflammation.
Under conditions wherein organisms are exposed to chronic (e.g. unrelenting, constant) stressors, glucocorticoid negative feedback inhibition of immune activation is impaired in a manner that drives allostasis (e.g. maintenance of organismal stability by altering physiological properties to counteract threats) (11) and facilitates increased levels of systemic inflammation. Chronic stress exposure results in diminished glucocorticoid negative feedback of the HPA axis arising from glucocorticoid resistance (12). Glucocorticoid resistance is believed to be due in part to inhibitory effects of cytokines on glucocorticoid receptor (GR) function, as well as stress-induced epigenetic modifications of molecules that regulate the GR, including FKBP5 (13). Consequences of this glucocorticoid resistance includes hypercortisolemia and increased activation of the immune system that can result in heightened pro-inflammatory cytokine and increased risk for individuals to become sick upon pathogen exposure (12).
Translational work in female rhesus macaques where the chronic psychosocial stress exposure associated with social subordination (e.g. constant harassment from higher-ranking animals) can be manipulated via social rank rearrangements shows that low social status causally alters immune gene expression profiles of NK, helper T cells, B cells and cytotoxic T cells towards expression profiles that denoted increased lymphocyte proliferation, heightened innate immune responses, and augmented cytokine responses (14). These social stress effects on proinflammatory gene expression at rest (e.g. in the absence of pathogen exposure) are most potently seen in NK and helper T cells, and are exacerbated upon in vitro stimulation with lipopolysaccharide (LPS) (14), a component of gram-negative bacteria that is used commonly to invoke a strong inflammatory response by binding toll like receptor 4 (TLR4) on monocytes. More specifically, LPS stimulation in subordinate, chronically stressed monkeys, results in the enrichment of genes associated with response to bacterial infection, including the inflammatory response and cytokine production (14), and lower expression of genes involved in the antiviral response and type I interferon signaling (15). Of note, this stress-related increase in expression of inflammatory genes and decreased antiviral genes (labeled the Conserved Transcriptional Response to Adversity) is believed to be related to chronic sympathetic nervous system activation and has been found in the context of a variety of chronic stressors in humans, including low socioeconomic status (16).
Genes upregulated by LPS and more highly expressed in subordinate female macaques include members of the NF-κB transcription factor complex, including NFKBID, NFKNIZ, and NFKB1, as well as the STAT3 and STAT5A transcription factors that are involved in proinflammatory cytokine response (14). This LPS-induced increase in NF-κB activity in chronically stressed monkeys is due to the polarization of the TLR4 signaling cascade towards the inflammatory MyD88-dependent pathway and away from the antiviral TRIF-dependent pathway that is favored in more dominant monkeys (14, 15). Interestingly, social subordination also drives an exaggerated expression of NF-κB and interferon-associated genes upon challenge with a viral mimic that can also be proinflammatory in nature (15). Critically, the increase in proinflammatory response upon LPS-stimulation is mediated by diminished glucocorticoid sensitivity in low-ranking animals (14).
The alterations in immune cell gene expression described above due to chronic psychosocial stress exposure in female rhesus macaques are associated with changes in chromatin structure, and thus, DNA accessibility to glucocorticoids (14). More specifically, low-ranking females present chromatin landscapes that are more accessible for NF-κB transcription factor binding sites, whereas high-ranking females show more accessible binding sites for AP-1, the glucocorticoid receptor cofactor that is involved in anti-inflammatory responses and inhibition of NF-κB (17). Importantly, in vitro dexamethasone administration also results in the enrichment of transcription factor binding sites for AP-1, suggesting that glucocorticoid resistance resulting from chronic subordination stress alters the dynamics of glucocorticoid-mediated gene expression in immune cells and chromatic accessibility to drive systemic inflammation (17). Taken together, these data underscore the mechanisms by which maladaptive allostatic consequences of chronic stress exposure can drive a pro-inflammatory state that increases risk for adverse health outcomes, including stress-related psychopathology (1).
Increased inflammation in individuals with stress-related psychopathology.
Systemic inflammation is associated with stress-related psychopathology (1). Systematic reviews and meta-analyses of available data on the relationship between inflammation and depression and fear and anxiety disorders support the notion that these stress-related conditions are associated with increased systemic inflammation as assessed by circulating concentrations of C-reactive protein (CRP) and cytokines (Table 1). Meta-analytic results indicate that glucocorticoid resistance is an important component of this increased inflammation in patients with depression (18).
Table 1.
Summary of systematic reviews and meta-analyses a on the relationship between inflammation and stress-related psychopathology.
| Disorder/Condition | Reference (Year) | # of Studies/Cases | CRP | TNF | IL-1b | IL-6 | IFNg | Others |
|---|---|---|---|---|---|---|---|---|
| Depression | Osimo et. al. 2020 | 107/5166 | ↑ | ↑ | - | ↑ | - | ↑ IL-3, IL-18, sIL-2R |
| Bipolar Disorder | Dargel et. al. 2015 | 11 | ↑ | NA | NA | NA | NA | NA |
| Modabbernia et. al. 2013 | 30/1351 | NA | ↑ | - | ↑ | - | ↑ sIL-2R, sIL-6R, IL-4, IL-10, sTNFR1 | |
| Anxiety, Traumatic Stress | Renna et al. 2018 | 41/1077 | - | ↑ | ↑ | ↑ | - | NA |
| PTSD | Yang et. al. 2020 | 42/1887 | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ IL-2; ↑ leukocytes |
| Generalized Anxiety Disorder | Costello et al. 2019 | 14/1188 | ↑ | NA | NA | NA | NA | NA |
| Panic Disorder | Quagliato et. al. 2018 | 11/887 | NA | - | ↑ | ↑ | - | ↑ IL-5 |
| Obsessive Compulsive Disorder | Cosco et al. 2019 | 16/538 | NA | - | - | - | - | NA |
NA - Not assessed; - denotes null finding; ↑ denotes significantly higher in cases compared to healthy controls
It is important to note that while most work to date focuses on peripheral blood concentrations of inflammatory biomarkers in stress-related psychiatric conditions (Table 1) (19–26), heightened inflammation is also seen in the brain. More specifically, a systemic review and meta-analysis shows that cerebral spinal fluid (CSF) concentrations of IL-6 and TNF are increased in individuals with depression (27). Increased microglia activation, the central mediators of the immune system, as assessed by PET neuroimaging, and greater expression of TNF and TLR4 in post-mortem brain tissue have also been described in individuals with depression (27). While these existing large-scale and reproducible data highlight the association between inflammation and stress-related psychiatric disorders, the cross-sectional nature of the majority of the studies limits our ability to determine the cause and effect relationship between stress-induced inflammation and behavior. Nevertheless, translational studies in human and pre-clinical models clearly show that peripheral and central inflammation can directly impact brain function to drive psychiatric symptoms and blocking inflammation can reduce symptoms of depression and anxiety in patients with increased inflammation.
Mechanisms by which inflammation contributes to stress-related symptoms.
The notion that stress-induced inflammation can induce affective symptomology was first highlighted by the finding that administration of the inflammatory cytokine, interferon-alpha, for the treatment of infectious diseases and cancer induced depressive symptoms (28). Since then, a significant body of literature has emerged that describes the causal effects of acute and chronic inflammatory stimuli on the emergence of affective symptoms. For example, administration of typhoid vaccination induces depressed mood, anhedonia, and fatigue (29). Neuroimaging studies have further shown that these inflammatory stimuli as well as endogenous inflammation in patients with depression can alter the functional connectivity and activation of brain regions implicated in the pathophysiology of stress-related psychopathology, including the prefrontal cortex (PFC), striatum, dorsal anterior cingulate cortex (dACC) and amygdala (29). These studies indicate that inflammation decreases functional connectivity between the PFC and striatum in a manner that predicts reward deficits, anhedonia and psychomotor slowing.
Cytokines released in the periphery in response to stress exposure can impact the brain by passing through leaky regions of the BBB, being actively transported across the BBB, activating endothelial and perivascular macrophages lining the brain to release their own cytokines into the brain parenchyma, and activating cytokine receptors on the vagus nerve and other peripheral afferent nerves to signal the brain (30). Peripheral cytokines released in response to stress exposure can also recruit activated monocytes and macrophages from the blood into the brain, wherein they produce their own cytokines and activate microglia which themselves can release cytokines locally in the brain (31). Finally, recent data indicate that stress-induced activation of NF-kB and TNF signaling pathways in endothelial cells in the nucleus accumbens can lead to a local reduction in the integrity of the blood brain barrier (32), allowing direct access of inflammatory cytokines to this brain region and ultimately depressive-like behavior.
Once in the brain, cytokines can influence behavior via their ability to alter the metabolism of neurotransmitters, including monoamines and glutamate. These effects of central cytokines on neurotransmitters are mediated through effects on neurotransmitter synthesis, release and reuptake, leading to decreased monoamine availability and increased extrasynaptic glutamate, which can be excitotoxic (30). In addition, increased activation of indoleamine 2,3 dioxygenase (IDO), the enzyme that acts to convert tryptophan into kynurenine, leads to greater levels of kynurenine. This increased kynurenine is then broken down into quinolinic acid, a N-methyl-D-aspartate (NMDA) receptor agonist, which can further contribute to glutamate excitotoxicity and oxidative stress (30). Cytokine-induced alterations in the IDO/kynurenine can decrease serotonin and dopamine levels, as well as increase glutamate levels (30), which have been linked to increased stress-related symptoms, including depressed mood, anhedonia, and psychomotor slowing (30).
Clinical considerations and implications regarding the immunology of stress.
Under conditions of chronic stressor exposure, the emergence of a proinflammatory allostatic state can contribute to psychiatric symptoms across depression and anxiety disorders via site-specific cytokine actions on neurotransmitter systems in brain regions underlying emotion regulation and affect (Figure 1). Accordingly, interventions targeting the immune system and its downstream effects on the brain for the treatment of depression and other psychiatric disorders has been of great interest. A number of strategies have been employed including blocking inflammation itself through pharmacologic or behavioral means or attempting to reverse the downstream effects of inflammation on neurotransmitter systems.
Figure 1.
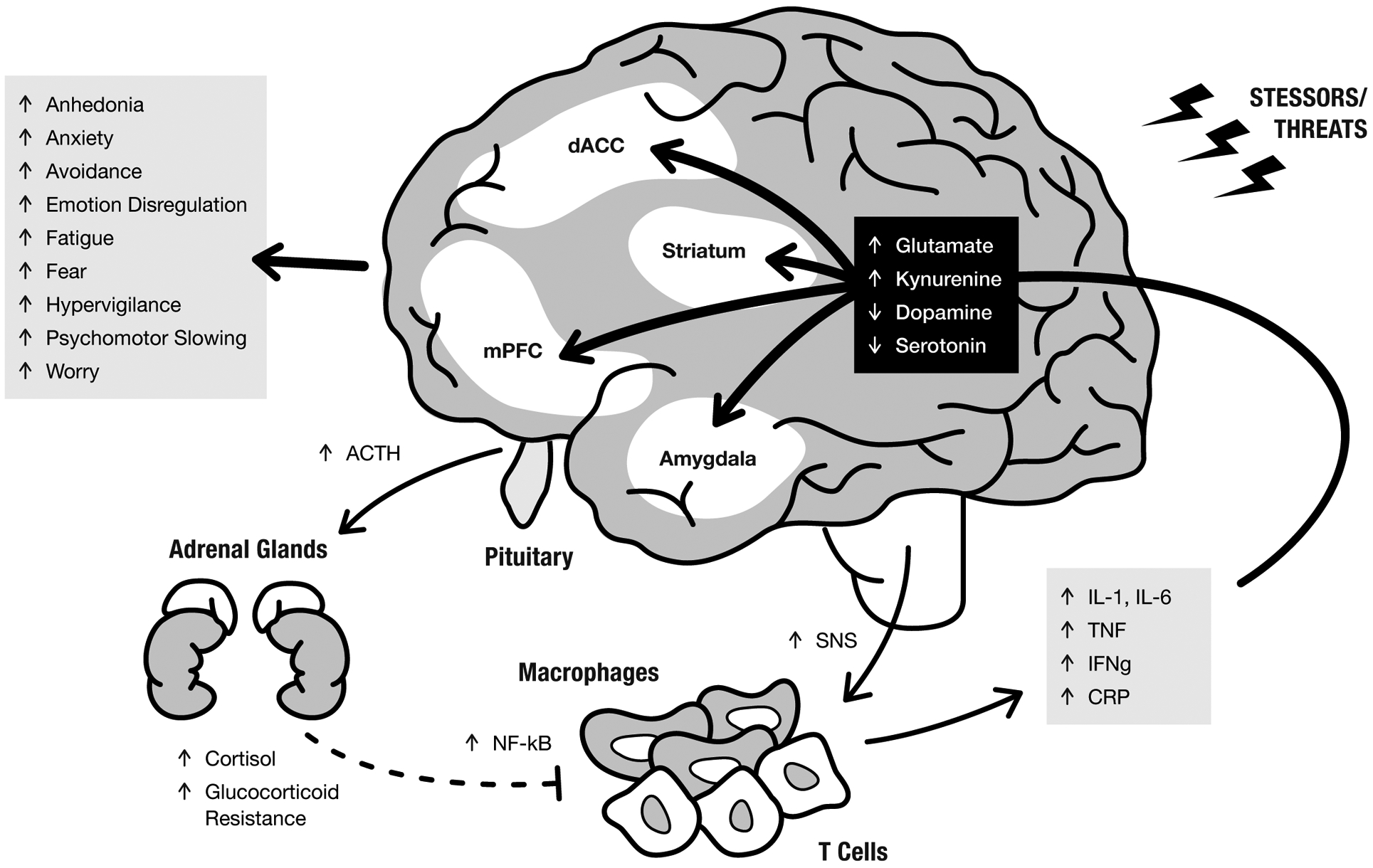
Exposure to chronic stressors and threats drives adrenocorticotropic hormone (ACTH) and cortisol release, as well as increased activity of the sympathetic nervous system (SNS). SNS activation of Nf-kB activity in immune cells increases expression of proinflammatory cytokines (e.g. IL-1,IL-6, TNF, IFNg) and CRP. Glucocorticoid resistance develops wherein cortisol does not as effectivity inhibit Nf-kB activity, thus creating a proinflammatory allostatic state that can contribute to psychiatric symptoms via cytokine actions on glutamate, kynurenine, dopamine, and serotonin systems in brain regions underlying emotion regulation and affect, including the striatum, dorsal anterior cingulate (dACC), medial prefrontal cortex (mPFC), and amygdala.
Probably the most convincing data that blocking inflammation can reduce depressive symptoms comes from studies using cytokine antagonists in patients with autoimmune and inflammatory disorders, albeit the impact of these drugs on the underlying disease complicate interpretation of these findings. Meta-analyses of other medications that putatively target the impact of inflammation on the brain including COX-2 inhibitors, aspirin, and minocycline (a tetracycline antibiotic that decreases microglial activation) have revealed some evidence of effectiveness in otherwise healthy depressed individuals, however the off-target effects of these medications and the fact that increased inflammation occurs in only about 1/3 of depressed patients leaves some level of doubt regarding the specificity of findings relative to inflammation (33, 34). Only a handful of studies have used anti-cytokine therapies in depression, and the results suggest that baseline inflammation (as reflected by CRP) is an important predictor of response, and symptoms that seem most responsive relate to anhedonia, psychomotor retardation and anxiety (34). The notion that baseline levels of inflammation may be an important consideration for pharmacological treatment extends past the use of anti-inflammatory agents, as translational studies have shown that greater inflammation in depression is also associated with resistance to conventional antidepressant treatments (35). The variability in the inflammatory profiles of individuals diagnosed with major depression is highlighted by a recent systematic review and meta-analysis reports that approximately one quarter of individuals with MDD show low-grade inflammations (CRP of >3 mg/L) and approximately half show mildly elevated CRP levels (CRP of >1 mg/L) (33).
Other pharmacological and behavioral interventions shown to be efficacious for the treatment of stress-related psychopathology may be immunomodulatory in nature, and thus could provide benefits through their abilities to attenuate systemic inflammation (36). Therapy with serotonin reuptake inhibitors (SSRIs), such as fluoxetine, paroxetine, sertraline, citalopram, escitalopram and fluvoxamine, decreases peripheral concentrations of IL-6, IL-1b, and TNF (37), although these effects appear to be largely related to treatment response and likely the associated reduction in stress. Mindfulness-based interventions have been shown in meta-analyses to decrease biomarkers of inflammation, including IL-6 and TNF across depression and anxiety disorders (38), and cognitive behavioral therapy for the treatment of depression normalizes cytokine levels (39). Finally, drugs such as ketamine (a NMDA antagonist) and levodopa (LDOPA; precursor of dopamine) that are efficacious for treating depression (40) may be acting by blocking or circumventing the downstream effects of stress-induced cytokines on glutamate or dopamine, respectively.
Although existing data suggest targeting the immunology of chronic stress may be a valid intervention for stress-related psychopathology, the majority of research to date has taken place in the context of depression. Future translational and clinical research is necessary to better determine the mechanism by which the immune system and inflammation contributes to anxiety disorders, and whether interventions targeting the immune system, or it effects on the brain are efficacious in these conditions. Other factors that contribute significantly to individual variability in the immunology of stress exposure and may be important for treatment considerations in stress-related psychopathology include genetics and epigenetics, biological sex, and the presence of other sources of inflammation that may interact with stress, such as smoking, diet, and comorbid medical conditions including obesity, metabolic syndrome, diabetes, cardiovascular disease or cancer. It is also important that more long-term studies leveraging these approaches are undertaken to assess whether the efficacy of the treatments are long-lasting, even in conditions where individuals continue to be exposed to chronic stressors. Finally, it is important to understand the maladaptive mental health consequences of the immunology of stress across the lifespan, starting in childhood.
Learning Objectives
After reading this article, you should be able to:
Discuss the immunology of acute and chronic stress exposure.
Describe the impacts of inflammation on the brain and behavior in the context of stress-related psychopathology.
Consider the clinical implications of the stress of immunology.
Multiple Choice Questions - Please select the best answer.
- Based on the current research, what proportion of individuals with major depression are thought to have significantly elevated peripheral concentrations of CRP (>3 mg/L)?
- 33%
- 25%
- 50%
- 80%
- 66%
- Which does not occur under homeostatic regulation of the immune system upon acute stress/threat exposure?
- SNS activation of macrophages and T Cells
- Glucocorticoid resistance
- Glucocorticoid negative feedback inhibition of NF-kB activation
- Increases innate and acquired immunity to facilitate the chances of organismal survival in the face of potential wounding and pathogen
- Acute redistribution of immune cells
- Decreased sensitivity of glucocorticoid receptors that occurs with chronic stress/threat exposure does not results in:
- Upregulation of pro-inflammatory gene expression
- Increased activation of microglia in the brain
- Increased ability for glucocorticoids to shut down stress-induced activation of the immune system
- Dysregulation of central neurotransmitter metabolism and function
- Increase symptoms of anhedonia, anxiety, and fatigue
- Based on current research, the activity of which brain region are impacted by inflammatory insults?
- Prefrontal cortex
- Amygdala
- Anterior cingulate cortex
- Striatum
- All of the above
- Based on the most recent meta-analysis, which marker(s) of inflammation are not consistently elevated in depression?
- C-reactive protein
- IL-6
- TNF
- IFNg
- TNF and IL-6
Funding
This review was supported in part by the National Institute of Health: AG057235 (VM), MH115174 (VM) and AG062334 (VM).
Author Biography
Meghna Ravi, BSA is a fourth-year graduate student in the Emory University Graduate Program in Neuroscience. Dr. Andrew H. Miller, MD is the Vice Chair of Research and the William P. Timmie Professor of Psychiatry and Behavioral Sciences at Emory University. His clinical and translational research focuses the impact of inflammatory cytokines on dopamine and the reward circuitry in the brain. Dr. Vasiliki Michopoulos is an Assistant Professor of Psychiatry and Behavioral Sciences at Emory University, and a core scientist at the Yerkes National Primate Research Center. Her research focuses on how psychosocial stress exposure (including trauma) across the lifespan adversely affects behavior and physiology using a translational neuroscience approach across non-human primates and humans.
Footnotes
Declaration of Interest
The authors declare no conflict of interest.
References
- 1.McEwen BS. Central effects of stress hormones in health and disease: Understanding the protective and damaging effects of stress and stress mediators. European journal of pharmacology. 2008; 583(2–3): 174–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhabhar FS, Malarkey WB, Neri E, McEwen BS. Stress-induced redistribution of immune cells--from barracks to boulevards to battlefields: a tale of three hormones--Curt Richter Award winner. Psychoneuroendocrinology. 2012; 37(9): 1345–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kenney MJ, Ganta CK. Autonomic nervous system and immune system interactions. Compr Physiol. 2014; 4(3): 1177–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herbert TB, Cohen S. Stress and immunity in humans: a meta-analytic review. Psychosom Med. 1993; 55(4): 364–79. [DOI] [PubMed] [Google Scholar]
- 5.Viswanathan K, Dhabhar FS. Stress-induced enhancement of leukocyte trafficking into sites of surgery or immune activation. Proceedings of the National Academy of Sciences of the United States of America. 2005; 102(16): 5808–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viswanathan K, Daugherty C, Dhabhar FS. Stress as an endogenous adjuvant: augmentation of the immunization phase of cell-mediated immunity. Int Immunol. 2005; 17(8): 1059–69. [DOI] [PubMed] [Google Scholar]
- 7.Bierhaus A, Wolf J, Andrassy M, Rohleder N, Humpert PM, Petrov D, et al. A mechanism converting psychosocial stress into mononuclear cell activation. Proceedings of the National Academy of Sciences of the United States of America. 2003; 100(4): 1920–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller AH, Spencer RL, hassett J, Kim C, Rhee R, Ciurea D, et al. Effects of selective type I and II adrenal steroid agonists on immune cell distribution. Endocrinology. 1994; 135(5): 1934–44. [DOI] [PubMed] [Google Scholar]
- 9.Lewitus GM, Cohen H, Schwartz M. Reducing post-traumatic anxiety by immunization. Brain Behav Immun. 2008; 22(7): 1108–14. [DOI] [PubMed] [Google Scholar]
- 10.Dhabhar FS, McEwen BS. Enhancing versus suppressive effects of stress hormones on skin immune function. Proceedings of the National Academy of Sciences of the United States of America. 1999; 96(3): 1059–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McEwen BS, Wingfield JC. What is in a name? Integrating homeostasis, allostasis and stress. Hormones and behavior. 2010; 57(2): 105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences of the United States of America. 2012; 109(16): 5995–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zannas AS, Jia M, Hafner K, Baumert J, Wiechmann T, Pape JC, et al. Epigenetic upregulation of FKBP5 by aging and stress contributes to NF-kappaB-driven inflammation and cardiovascular risk. Proceedings of the National Academy of Sciences of the United States of America. 2019; 116(23): 11370–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Snyder-Mackler N, Sanz J, Kohn JN, Brinkworth JF, Morrow S, Shaver AO, et al. Social status alters immune regulation and response to infection in macaques. Science (New York, NY. 2016; 354(6315): 1041–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanz J, Maurizio PL, Snyder-Mackler N, Simons ND, Voyles T, Kohn J, et al. Social history and exposure to pathogen signals modulate social status effects on gene regulation in rhesus macaques. Proceedings of the National Academy of Sciences of the United States of America. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knight JM, Rizzo JD, Logan BR, Wang T, Arevalo JM, Ma J, et al. Low Socioeconomic Status, Adverse Gene Expression Profiles, and Clinical Outcomes in Hematopoietic Stem Cell Transplant Recipients. Clin Cancer Res. 2016; 22(1): 69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Snyder-Mackler N, Sanz J, Kohn JN, Voyles T, Pique-Regi R, Wilson ME, et al. Social status alters chromatin accessibility and the gene regulatory response to glucocorticoid stimulation in rhesus macaques. Proceedings of the National Academy of Sciences of the United States of America. 2019; 116(4): 1219–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perrin AJ, Horowitz MA, Roelofs J, Zunszain PA, Pariante CM. Glucocorticoid Resistance: Is It a Requisite for Increased Cytokine Production in Depression? A Systematic Review and Meta-Analysis. Front Psychiatry. 2019; 10: 423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osimo EF, Pillinger T, Rodriguez IM, Khandaker GM, Pariante CM, Howes OD. Inflammatory markers in depression: A meta-analysis of mean differences and variability in 5,166 patients and 5,083 controls. Brain Behav Immun. 2020; 87: 901–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dargel AA, Godin O, Kapczinski F, Kupfer DJ, Leboyer M. C-reactive protein alterations in bipolar disorder: a meta-analysis. The Journal of clinical psychiatry. 2015; 76(2): 142–50. [DOI] [PubMed] [Google Scholar]
- 21.Modabbernia A, Taslimi S, Brietzke E, Ashrafi M. Cytokine alterations in bipolar disorder: a meta-analysis of 30 studies. Biological psychiatry. 2013; 74(1): 15–25. [DOI] [PubMed] [Google Scholar]
- 22.Renna ME, O’Toole MS, Spaeth PE, Lekander M, Mennin DS. The association between anxiety, traumatic stress, and obsessive-compulsive disorders and chronic inflammation: A systematic review and meta-analysis. Depress Anxiety. 2018; 35(11): 1081–94. [DOI] [PubMed] [Google Scholar]
- 23.Yang JJ, Jiang W. Immune biomarkers alterations in post-traumatic stress disorder: A systematic review and meta-analysis. Journal of affective disorders. 2020; 268: 39–46. [DOI] [PubMed] [Google Scholar]
- 24.Costello H, Gould RL, Abrol E, Howard R. Systematic review and meta-analysis of the association between peripheral inflammatory cytokines and generalised anxiety disorder. BMJ Open. 2019; 9(7): e027925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quagliato LA, Nardi AE. Cytokine alterations in panic disorder: A systematic review. Journal of affective disorders. 2018; 228: 91–6. [DOI] [PubMed] [Google Scholar]
- 26.Cosco TD, Pillinger T, Emam H, Solmi M, Budhdeo S, Matthew Prina A, et al. Immune Aberrations in Obsessive-Compulsive Disorder: a Systematic Review and Meta-analysis. Molecular neurobiology. 2019; 56(7): 4751–9. [DOI] [PubMed] [Google Scholar]
- 27.Enache D, Pariante CM, Mondelli V. Markers of central inflammation in major depressive disorder: A systematic review and meta-analysis of studies examining cerebrospinal fluid, positron emission tomography and post-mortem brain tissue. Brain Behav Immun. 2019; 81: 24–40. [DOI] [PubMed] [Google Scholar]
- 28.Raison CL, Demetrashvili M, Capuron L, Miller AH. Neuropsychiatric adverse effects of interferon-alpha: recognition and management. CNS drugs. 2005; 19(2): 105–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harrison NA, Brydon L, Walker C, Gray MA, Steptoe A, Critchley HD. Inflammation causes mood changes through alterations in subgenual cingulate activity and mesolimbic connectivity. Biological psychiatry. 2009; 66(5): 407–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haroon E, Raison CL, Miller AH. Psychoneuroimmunology meets neuropsychopharmacology: translational implications of the impact of inflammation on behavior. Neuropsychopharmacology. 2012; 37(1): 137–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D’Mello C, Le T, Swain MG. Cerebral microglia recruit monocytes into the brain in response to tumor necrosis factoralpha signaling during peripheral organ inflammation. J Neurosci. 2009; 29(7): 2089–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Menard C, Pfau ML, Hodes GE, Kana V, Wang VX, Bouchard S, et al. Social stress induces neurovascular pathology promoting depression. Nature neuroscience. 2017; 20(12): 1752–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Osimo EF, Baxter LJ, Lewis G, Jones PB, Khandaker GM. Prevalence of low-grade inflammation in depression: a systematic review and meta-analysis of CRP levels. Psychol Med. 2019; 49(12): 1958–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bavaresco DV, Uggioni MLR, Ferraz SD, Marques RMM, Simon CS, Dagostin VS, et al. Efficacy of infliximab in treatment-resistant depression: A systematic review and meta-analysis. Pharmacology, biochemistry, and behavior. 2020; 188: 172838. [DOI] [PubMed] [Google Scholar]
- 35.Chamberlain SR, Cavanagh J, de Boer P, Mondelli V, Jones DNC, Drevets WC, et al. Treatment-resistant depression and peripheral C-reactive protein. Br J Psychiatry. 2019; 214(1): 11–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu JJ, Wei YB, Strawbridge R, Bao Y, Chang S, Shi L, et al. Peripheral cytokine levels and response to antidepressant treatment in depression: a systematic review and meta-analysis. Molecular psychiatry. 2020; 25(2): 339–50. [DOI] [PubMed] [Google Scholar]
- 37.Wang L, Wang R, Liu L, Qiao D, Baldwin DS, Hou R. Effects of SSRIs on peripheral inflammatory markers in patients with major depressive disorder: A systematic review and meta-analysis. Brain Behav Immun. 2019; 79: 24–38. [DOI] [PubMed] [Google Scholar]
- 38.Sanada K, Montero-Marin J, Barcelo-Soler A, Ikuse D, Ota M, Hirata A, et al. Effects of Mindfulness-Based Interventions on Biomarkers and Low-Grade Inflammation in Patients with Psychiatric Disorders: A Meta-Analytic Review. Int J Mol Sci. 2020; 21(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dahl J, Ormstad H, Aass HC, Sandvik L, Malt UF, Andreassen OA. Recovery from major depressive disorder episode after non-pharmacological treatment is associated with normalized cytokine levels. Acta Psychiatr Scand. 2016; 134(1): 40–7. [DOI] [PubMed] [Google Scholar]
- 40.Park LT, Falodun TB, Zarate CA Jr. Ketamine for Treatment-Resistant Mood Disorders. Focus (Am Psychiatr Publ). 2019; 17(1): 8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]


