Abstract
Introduction
Cilostazol may be a novel therapeutic agent for Alzheimer's disease. Its metabolite, OPC‐13015, has a stronger inhibitory effect on type 3 phosphodiesterase than cilostazol.
Methods
We prospectively enrolled patients with mild cognitive impairment to whom cilostazol was newly prescribed. Patients underwent the Montreal Cognitive Assessment (MoCA) twice, at a 6‐month interval. Plasma cilostazol, OPC‐13015, OPC‐13213, and OPC‐13217 concentrations were determined using liquid chromatography‐tandem mass spectrometry.
Results
MoCA score changes from baseline to the 6‐month visit were positively correlated with ratios of OPC‐13015 to cilostazol and total metabolites (n = 19, P = .005). Patients with higher ratios of OPC‐13015 (≥0.18, median value; n = 10) had significantly higher MoCA scores (P = .036) than patients with lower ratios (the ratio <0.18, n = 9). The absolute value of OPC‐13015 concentration in blood was also higher in patients with preserved cognitive function (P = .033).
Discussion
Blood OPC‐13015 levels may be a predictive biomarker of cilostazol treatment for Alzheimer's disease.
Keywords: Alzheimer's disease, cilostazol, drug repositioning, mild cognitive impairment, OPC‐13015, stratified medicine
1. BACKGROUND
Alzheimer's disease (AD) is the most common type of dementia and is characterized by neuropathological changes such as extracellular amyloid beta (Aβ) plaques and intracellular tau tangles. An excess production of Aβ protein, caused by mutations in the amyloid precursor protein (APP) gene, can induce familial cases of AD. In contrast, growing evidence indicates that the removal rate of Aβ is impaired in sporadic AD. Thus a novel therapy that promotes Aβ clearance from the brain is needed. 1 , 2
RESEARCH IN CONTEXT
Systematic review: Soluble amyloid beta (Aβ) drains from the brain along basement membranes in the walls of arteries; such drainage is impaired in Alzheimer's disease (AD). Cilostazol, a selective inhibitor of type 3 phosphodiesterase, can facilitate the clearance of Aβ. OPC‐13015, the active metabolite of cilostazol, has a five times stronger inhibitory effect on type 3 phosphodiesterase than cilostazol.
Interpretation: High blood levels of OPC‐13015, but not the other measured metabolites, were strongly related to a favorable response to cilostazol in patients with mild cognitive impairment (MCI). This suggests that the conversion from cilostazol to OPC‐13015 may promote its disease‐modifying effects for AD.
Future directions: Based on a drug‐repositioning approach, the clinical application of cilostazol for MCI is now aimed at a phase‐II clinical trial. Blood OPC‐13015 levels may be a predictive biomarker of cilostazol treatment, which would facilitate precision/stratified medicine in AD.
HIGHLIGHTS
Cilostazol facilitates brain amyloid beta (Aβ) clearance and ameliorates Alzheimer's disease (AD)
We measured blood levels of OPC‐13015, an active metabolite of cilostazol
High OPC‐13015 levels were related to a favorable response to cilostazol in mild cognitive impairment (MCI)
Blood OPC‐13015 levels may be a predictive biomarker of cilostazol treatment
Our findings may facilitate precision/stratified medicine in AD
Intramural periarterial drainage (IPAD) is one of the major clearance systems of Aβ. 3 Interstitial fluid and solutes in the extracellular matrix, including Aβ, enter IPAD pathways within the basement membranes of capillaries, continue to the basement membranes surrounding smooth muscle cells (SMCs) of intracerebral arteries, and finally lead to the cervical lymph nodes. 3 We previously reported that cilostazol (OPC‐13013) facilitates Aβ clearance via IPAD, resulting in the amelioration of Aβ deposition and cognitive impairments in APP transgenic mice. 4 Cilostazol is a selective inhibitor of type 3 phosphodiesterase (PDE‐3) and is clinically available as an anti‐platelet drug for the prevention of ischemic stroke in East Asia. 5 On the basis of a drug‐repositioning strategy, which is a process aimed at discovering new therapeutic drugs from existing drugs in a clinical setting, 6 a clinical application of cilostazol for AD is expected. 5 Several clinical investigations have reported the beneficial effects of cilostazol on cognitive impairment, 5 , 7 , 8 including a nationwide cohort study. 9 Two clinical trials for patients with mild cognitive impairment (MCI) and small vessel disease are currently being conducted in Japan and the UK. 5 , 10
Cilostazol is metabolized predominantly in the liver. Among its 11 known metabolites, the major metabolites include 3,4‐dehydrocilostazol (OPC‐13015) and 4′‐trans‐hydroxycilostazol (OPC‐13213) (Figure 1). 11 In rats, 4‐cis‐hydroxycilostazol (OPC‐13217) is also detected in the blood, but the levels of OPC‐13217 are relatively low in humans. 11 A specific conversion from cilostazol to OPC‐13015 or OPC‐13213 is associated with polymorphisms of the cytochrome P450 (CYP)2C19 and CYP3A5 genes. 12 OPC‐13015 possesses an inhibitory effect on PDE‐3 that is approximately five times stronger than that of cilostazol, whereas OPC‐13213 has a much weaker effect than cilostazol. 13 , 14
FIGURE 1.
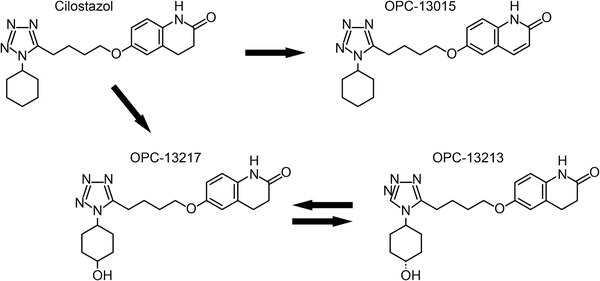
Chemical structural formulae of cilostazol and its metabolites. The major metabolites of cilostazol (OPC‐13013) are 3,4‐dehydrocilostazol (OPC‐13015) and 4′‐trans‐hydroxycilostazol (OPC‐13213). In rats, 4‐cis‐hydroxycilostazol (OPC‐13217) is also detected in the blood, but OPC‐13217 levels are relatively low in humans. Because of the difficulty of measuring the concentrations of OPC‐13213 and OPC‐13217 separately, the total amounts of OPC‐13213 and OPC‐13217 were estimated in this study
On the basis of these previous findings, we hypothesized that the specific conversion from cilostazol to OPC‐13015, rather than OPC‐13213, might be associated with the amelioration of cognitive impairment. Herein, we measured the levels of cilostazol metabolites in patients with MCI. The aim of this study was to reveal whether blood OPC‐13015 levels can be used as a predictive biomarker for cilostazol treatment in AD and MCI.
2. METHODS
2.1. Study design
This prospective study was conducted at the National Cerebral and Cardiovascular Center in Japan. The local ethics committee approved the study protocol (M30‐136). We enrolled consecutive patients who fulfilled the following five criteria: (1) MCI was diagnosed in accordance with the core clinical criteria stated in the National Institute on Aging‐Alzheimer's Association (NIA/AA) classification for MCI 15 ; (2) overall Clinical Dementia Rating (global CDR) score was 0.5; (3) cilostazol was newly prescribed for the purpose of preventing ischemic stroke; (4) written informed consent was provided; and (5) cognitive impairment was not caused solely by cerebrovascular disease (ie, pure vascular MCI was excluded).
2.2. Clinical characteristics and psychological testing
Clinical information was collected from patients’ medical records. Patients’ ages were recorded when blood sampling was performed to measure cilostazol and its metabolites. Low education was defined as a high school diploma or less. Magnetic resonance imaging (MRI) and laboratory findings nearest to the time of blood sampling were described.
The CDR was based on a semi‐structured interview with the patient and a caregiver who could provide an index of global functioning. 16 The rater scored the patients in each of six cognitive domains (memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care). We measured the global CDR score and the CDR Sum of Boxes (CDR‐SB). The global CDR was scored using the rule reported by Morris, 16 and the CDR‐SB was the total of each domain score. 17
The Montreal Cognitive Assessment (MoCA) is a brief cognitive screening tool for patients with MCI. It assesses short‐term memory, visuospatial abilities, executive functions, attention, concentration and working memory, language, and orientation to time and place. 18 In this study, the Japanese version of the MoCA 19 was performed twice for each patient by one trained psychologist (M.Y.) who was blinded to the clinical information. The first MoCA, taken before starting cilostazol treatment, was used for the baseline evaluation; the follow‐up MoCA was examined 6 months later. We defined “cognitive preservation” as no exacerbation from the baseline to the follow‐up MoCA.
2.3. MRI evaluation
Either 1.5 T (Magnetom Sonata; Siemens Medical Solutions, Erlangen, Germany) or 3.0 T (Magnetom Verio or Spectra; Siemens Medical Solutions) scanners were used. Lacunar infarcts and white matter hyperintensities were evaluated using fluid‐attenuated inversion recovery (FLAIR) images. Lacunar infarcts were defined as rounded or ovoid hypointense lesions of 3 to 20 mm in diameter, with a hyperintense rim, and occurred in the basal ganglia, thalamus, internal and external capsule, centrum semiovale, and brainstem. Periventricular hyperintensities (PVHs) and deep white matter hyperintensities (DWMHs) were scored using the Fazekas scale. 20 These changes were analyzed using T1‐ and T2‐weighted images in one patient, because of missing FLAIR data. Cerebral microbleeds were defined as rounded, hypointense foci up to 10 mm in diameter on T2*‐weighted images. 21 The diagnosis of probable or possible cerebral amyloid angiopathy (CAA) were established using the modified Boston criteria. 22
2.4. Measurements of the levels of cilostazol and its metabolites
Within 7 days after blood collection, we measured the plasma concentrations of cilostazol, OPC‐13015, OPC‐13213, and OPC‐13217 using liquid chromatography‐tandem mass spectrometry (LC‐MS/MS), which consisted of a Nexera ultra‐high‐performance liquid chromatograph (Shimadzu Corporation, Kyoto, Japan) and an LCMS‐8040 triple quadrupole mass spectrometer (Shimadzu Corporation). Patients’ plasma was stored at −20°C until the measurement. The metabolite stability was confirmed before this measurement. Cilostazol, cilostazol‐d11, methanol, ultrapure water, and formic acid were purchased from FUJIFILM Wako Pure Chemical Corporation (Osaka, Japan). The OPC‐13015, OPC‐13213, and OPC‐3930 were from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA). The OPC‐13217 was from Toronto Research Chemicals, Inc. (Ontario, Canada).
After adding three times the volume of the internal standard solution (10 ng/mL of cilostazol‐d11 and 10 ng/mL of OPC‐3930 in methanol) into the plasma, the sample was vortexed and centrifuged at 20,000 g for 5 minutes. We then applied 0.5 μL of the supernatant to the LC‐MS/MS system. Chromatographic separation was performed on a Mastro C18 column (100 × 2.1 mm, 3 μm; Shimadzu GLC Ltd., Tokyo, Japan) at a flowrate of 0.3 mL/min at 40°C. The mobile phase consisted of a gradient of (A) water and (B) methanol, both containing 0.1% formic acid, as follows: 0.0 to 0.5 minutes, 30% (B); 0.5 to 2.0 minutes, 30% to 65% (B); 2.0 to 4.0 minutes, 65% (B); 4.0 to 6.5 minutes, 30% (B). Samples were then ionized using the following conditions: nebulizing gas flow, 3 L/minute; drying gas flow, 15 L/minute; desolvation line temperature, 250°C; heat block temperature, 400°C. The mass spectrometer was operated in the positive electrospray ionization mode using multiple reaction monitoring (MRM). The mass transition pairs (m/z) were 370.20 → 288.15 for cilostazol, 368.20 → 125.10 for OPC‐13015, 386.20 → 288.20 for OPC‐13213 and OPC‐13217 (OPC‐13213/13217), 381.20 → 289.20 for cilostazol‐d11, and 354.10 → 111.20 for OPC‐3930. We confirmed that synthetic cilostazol, OPC‐13015, and OPC‐13213/13217 were not detected in the settings for the measurements of the other compounds (Figure 2). The measurement of cilostazol and its metabolites was independently conducted by one researcher (K.S.) who was blinded to the clinical information.
FIGURE 2.
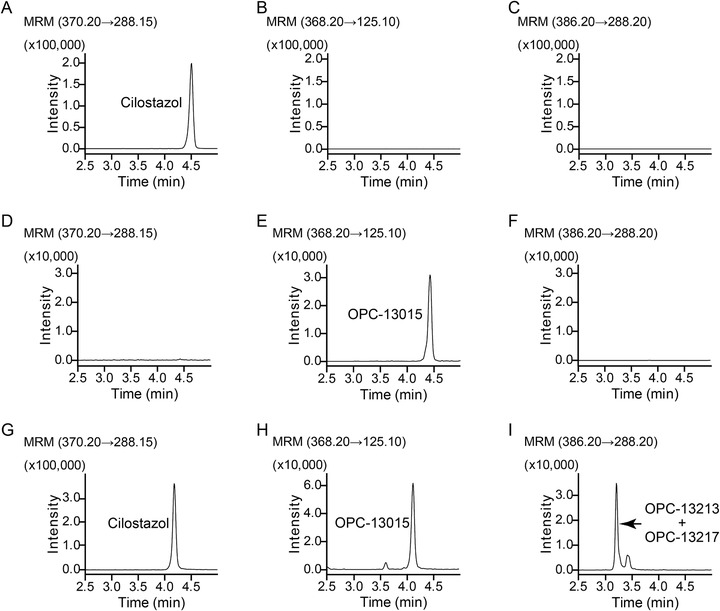
Measurements of the levels of cilostazol and its metabolites. Representative chromatograms of cilostazol, OPC‐13015, and OPC‐13213/13217 in cilostazol standard solution (A‐C), OPC‐13015 standard solution (D‐F), or blood samples from a subject receiving cilostazol (G‐I). The peak for cilostazol was detected in (A), but was not detected using the settings for the measurement of OPC‐13015 (B) or OPC‐13213/13217 (C). The peak for OPC‐13015 was detected in (E), but was not detected using the settings for the measurement of cilostazol (D) or OPC‐13213/13217 (F). Cilostazol (G), OPC‐13015 (H), and OPC‐13213/13217 (I) were detected in blood samples from a subject receiving cilostazol. MRM, multiple reaction monitoring
It was difficult to accurately measure the levels of OPC‐13213 and OPC‐13217 separately. Thus the levels of OPC‐13213 and OPC‐13217 were estimated in this study. We defined the “cilostazol ratio,” “OPC‐13015 ratio,” and “OPC‐13213/13217 ratio” as the proportion of each molecule to the total amount of cilostazol, OPC‐13015, OPC‐13213, and OPC‐13217.
2.5. APOE genotyping
Genotyping of the apolipoprotein E (APOE) gene was performed using a fully automated gene analysis system (GTS‐7000, Shimadzu). This system allows the direct detection of single‐nucleotide polymorphisms (SNPs) from 1 μL of whole blood samples using polymerase chain reaction. 23 We assessed two SNPs, rs429358 and rs7412, which determine the APOE ε allele. The APOE ε2 allele was recognized by rs429358‐T and rs7412‐T, the APOE ε3 by rs429358‐T and rs7412‐C, and the APOE ε4 by rs429358‐C and rs7412‐C. 24 The primer sequences for rs429358 and rs7412 were 5′‐CAAGGAGCTGCAGGCGG‐3′ (forward) and 5′‐CAGCTCCTCGGTGCTCTG‐3′ (reverse) are one pair. 5′‐ CGCAAGCTGCGTAAGCG‐3′ (forward) and 5′‐CGCGGATGGCGCTGAG‐3′ (reverse) are another pair. The probe sets were 5′‐GGACGTGTGCGGCCG‐3′ for rs429358‐T, 5′‐ GGACGTGCGCGGCCG ‐3′ for rs429358‐C, 5′‐CTGCAGAAGCGCCTGGC‐3′ for rs7412‐C, and 5′‐CTGCAGAAGTGCCTGGC‐3′ for rs7412‐T.
2.6. Statistical analyses
Unless otherwise noted, the data are presented as the mean and SD or as the median (interquartile range) for continuous variables, and as numbers and percentages for categorical variables. Continuous variables were compared using the Student t test or Mann‐Whitney U test, as appropriate. Categorical variables were compared using Fisher's exact test. Spearman rank correlation coefficients were calculated to test associations between two variables. Two‐way repeated measures analysis of variance (ANOVA) was used for the comparison of longitudinal data. All analyses were performed using SPSS version 26 (IBM Corp., Armonk, NY, USA). A P‐value < .05 (two‐tailed) was considered statistically significant.
3.
4. RESULTS
Between October 1, 2017 and January 31, 2020, at total of 30 subjects were screened for study entry, and 24 were enrolled after providing informed consent (Figure 3). Of these, two withdrew their consent and one discontinued the cilostazol treatment. Two were further excluded because no cilostazol was detected in the blood. We thus analyzed 19 patients in this study.
FIGURE 3.
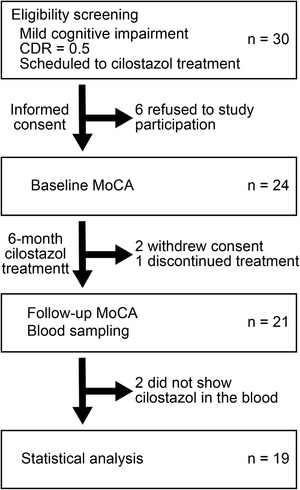
Study design. CDR, Clinical Dementia Rating; MoCA, Montreal Cognitive Assessment
The blood levels of cilostazol and its metabolites varied in each subject and were not correlated with the time from the last dose to blood sampling (Figure 4). Most of the subjects received 100 mg per day of cilostazol for 6 months, although two subjects received 200 mg per day of cilostazol. We therefore estimated the ratio of cilostazol to the total amount of cilostazol and its three metabolites, OPC‐13015, OPC‐13213, and OPC‐13217. In addition to the “cilostazol ratio,” the “OPC‐13015 ratio” and “OPC‐13213/13217 ratio” were also calculated by dividing each level by the total amount of cilostazol and its three metabolites. The dose of cilostazol remained unchanged during the observation period for each patient.
FIGURE 4.
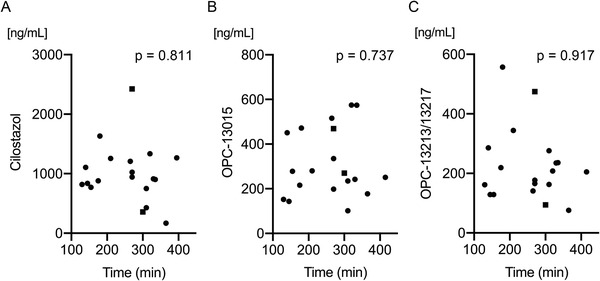
Scatter plots showing the levels of cilostazol and metabolites. Time between the last dose and blood sampling was not associated with the levels of cilostazol (A, Spearman's rho = −0.059), OPC‐13015 (B, Spearman's rho = 0.083), or OPC‐13213 and OPC‐13217 (OPC‐13213/13217) (C, Spearman's rho = −0.026) in patients receiving 100 mg (filled circles) or 200 mg (filled squares) per day of cilostazol. Large individual differences were observed in the concentrations of cilostazol and its metabolites
We divided patients into two groups on the basis of the median of the OPC‐13015 ratio (0.18). The group with higher OPC‐13015 ratios (≥0.18; n = 10) was compared with the group with lower ratios (<0.18; n = 9) for baseline data and the response to cilostazol. Both groups exhibited similar clinical characteristics (Table 1). There was one homozygous ε4/ε4 carrier in each group. In the MRI results, a previous intracerebral hemorrhage in the left parietal lobe was observed in one patient from the lower OPC‐13015 group. No large infarcts were identified. Laboratory tests showed comparable results regarding liver and renal function. The cilostazol ratio was lower in the higher OPC‐13015 group compared with the lower OPC‐13015 group.
TABLE 1.
Clinical characteristics
| OPC‐13015 a | ||||
|---|---|---|---|---|
| Variables | All (n = 19) | ≥0.18 (n = 10) | <0.18 (n = 9) | P‐value |
| Age (years) | 77.8 ± 4.7 | 78.3 ± 4.6 | 77.2 ± 5.0 | .631 |
| Male, n (%) | 13 (68) | 6 (60) | 7 (78) | .628 |
| Low education, n (%) | 10 (53) | 7 (70) | 3 (33) | .179 |
| APOE genotype, n (%) | 1.000 | |||
| E2/E3 | 1 (5) | 1 (10) | 0 (0) | |
| E3/E3 | 9 (47) | 5 (50) | 4 (44) | |
| E3/E4 | 7 (37) | 3 (30) | 4 (44) | |
| E4/E4 | 2 (11) | 1 (10) | 1 (11) | |
| CDR‐Global | 0.5 (0.5‒0.5) | 0.5 (0.5‒0.5) | 0.5 (0.5‒0.5) | 1.000 |
| CDR‐SB | 2.5 (2.0‒3.5) | 2.3 (1.9‒3.1) | 3.5 (2.0‒3.8) | .182 |
| Lacunar infarcts, n (%) | 10 (53) | 6 (60) | 4 (44) | .656 |
| PVH | 1.0 (1.0‒2.0) | 1.0 (1.0‒3.0) | 1.0 (1.0‒2.0) | .661 |
| DWMH | 2.0 (1.0‒3.0) | 1.0 (0.8‒2.3) | 2.0 (1.5‒3.0) | .156 |
| CMB, n (%) | 8 (42) | 4 (40) | 4 (44) | 1.000 |
| CAA, n (%) | .777 | |||
| Probable CAA | 3 (16) | 1 (10) | 2 (22) | |
| Possible CAA | 2 (11) | 1 (10) | 1 (11) | |
| AST | 24.0 (20.0‒28.0) | 26.0 (20.5‒30.0) | 23.0 (19.5‒26.0) | .243 |
| ALT | 16.0 (12.0‒21.0) | 16.5 (11.8‒21.5) | 16.0 (12.5‒21.5) | .905 |
| γ‐GTP | 22.0 (20.0‒31.0) | 22.0 (20.8‒28.8) | 24.0 (17.0‒37.5) | .661 |
| eGFR | 57.9 (50.3‒70.0) | 56.3 (48.3‒62.7) | 70.0 (50.9‒75.8) | .182 |
| Dose of cilostazol, n (%) | 1.000 | |||
| 200 mg/day | 2 (11) | 1 (10) | 1 (11) | |
| 100 mg/day | 17 (90) | 9 (90) | 8 (89) | |
| Cilostazol a | 0.65 (0.60‒0.72) | 0.61 (0.52‒0.65) | 0.72 (0.66‒0.73) | .001 |
| OPC‐13015 a | 0.18 (0.15‒0.27) | 0.26 (0.21‒0.34) | 0.15 (0.14‒0.16) | <.001 |
| OPC‐13213/13217 a | 0.14 (0.12‒0.18) | 0.13 (0.11‒0.19) | 0.14 (0.13‒0.18) | .356 |
Data represent the mean ± standard deviation, median (interquartile range), or number (percentage). Student's t, Mann‐Whitney U, or Fisher's exact tests were used appropriately.
ALT, alanine aminotransaminase; AST, aspartate aminotransaminase; CAA, cerebral amyloid angiopathy; CDR‐SB, Clinical Dementia Rating‐Sum of Boxes; CMB, cerebral microbleeds; DWMH, deep white matter hyperintensity; eGFR, estimated glomerular filtration rate; γ‐GTP, γ‐glutamyl transferase; PVH, periventricular hyperintensity.
The ratio of the molecule to the total amount of cilostazol and its metabolites.
In the higher OPC‐13015 group, the median (interquartile range) score in the MoCA was preserved from 19.5 (16.8‒21.3) points at baseline to 19.5 (17.8‒21.5) at follow‐up. In contrast, these scores deteriorated from 17.0 (15.0‒19.5) to 16.0 (14.5‒17.5) in the lower OPC‐13015 group (Figure 5A); this difference was significant (P = .036). The changes in MoCA scores from baseline to follow‐up in all patients showed a strong positive correlation with the OPC‐13015 ratio (Spearman's rho = 0.617, P = .005, Figure 5B). The cilostazol ratio was slightly lower in patients with cognitive preservation than in those without cognitive preservation (P = .051) (Figure 5C). Furthermore, the OPC‐13015 ratio was significantly higher in patients with cognitive preservation (P = .005), but OPC‐13213/13217 was not significantly different (Figure 5D,E). Notably, the absolute value of the OPC‐13015 concentration in the blood was also significantly higher in patients with cognitive preservation than in those without cognitive preservation (335.0 ng/mL [242.0‒516.0] vs 225.5 ng/mL [145.3‒271.3], P = .033), but the absolute values of cilostazol (1025.0 ng/mL [902.0‒1257.0] vs 828.0 ng/mL [755.5‒1169.8], P = .351) and OPC‐13213/13217 (208.0 ng/mL [141.0‒286.0] vs 184.0 ng/mL [137.3‒261.8], P = .717) were not significantly different between the two groups. No patients had a stroke event or conversion from MCI to dementia during the observation period.
FIGURE 5.
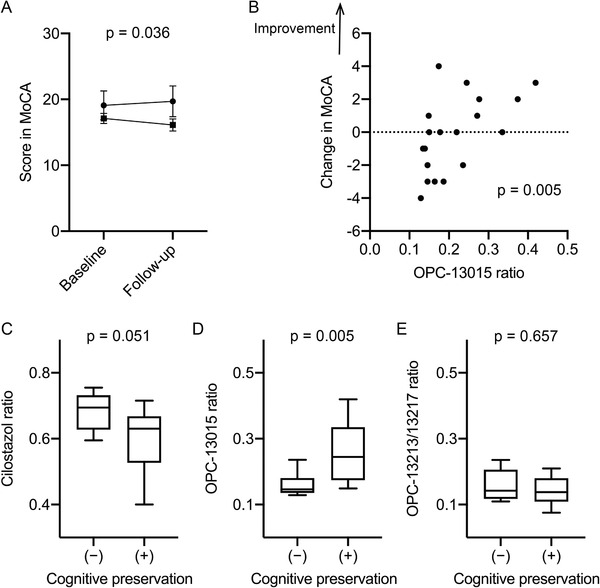
Amelioration of cognitive impairment was related to high OPC‐13015 levels. A, Mean scores in the Montreal Cognitive Assessment (MoCA) were increased in the higher OPC‐13015 group (filled circles, n = 10) compared with the lower group (filled squares, n = 9). Two‐way repeated‐measures analysis of variance; error bars indicate the standard errors. B, The ratio of OPC‐13015 to total analytes was positively correlated with the changes in MoCA from baseline to follow‐up (n = 19, Spearman's rho = 0.617). C‐E, Box‐and‐whisker plots showing the median, quartiles, maximum, and minimum of the ratio of cilostazol and its metabolites. Mann‐Whitney U test. The cilostazol ratio was slightly lower in patients with cognitive preservation (n = 11; change in MoCA from baseline to follow‐up ≥ 0) compared with those without cognitive preservation (n = 8; change in MoCA from baseline to follow‐up < 0) (C). The OPC‐13015 ratio was significantly higher in patients with cognitive preservation (D), whereas the OPC‐13213/13217 ratio was not significantly different between the two groups (E)
5. DISCUSSION
In this prospective study examining cognitive function in MCI patients receiving cilostazol, we revealed that higher scores on the MoCA were associated with a significantly increased ratio of OPC‐13015 to cilostazol and its metabolites in the blood. That is, the OPC‐13015 ratio was higher in patients with cognitive preservation than in those without cognitive preservation. Both the increase in the OPC‐13015 level and the decrease in the cilostazol or OPC‐13213/13217 levels might contribute to the high OPC‐13015 ratio. However, only the absolute value of OPC‐13015 was significantly increased in patients with cognitive preservation, suggesting that an increased level of OPC‐13015 is more strongly associated with cognitive preservation than the levels of the other metabolites. The mean ratio of OPC‐13015 in all participants in the present study was similar to that of previous pharmacokinetic reports in healthy male volunteers. 25 , 26
The brain was not previously believed to contain lymphatic vessels, but two recent investigations have illustrated the presence of lymphatic vessels within the meninges surrounding the cerebrum. 27 , 28 The ablation of meningeal lymphatic vessels aggravates Aβ accumulation, suggesting that promoting intracranial lymphatic systems may be a potential therapeutic approach for AD. 29 IPAD is an alternative mechanism of lymphatic function in the brain parenchyma and plays a pivotal role in the elimination of waste products secreted from neurons and glia. 30 Its importance has been demonstrated in clinical trials of Aβ immunization. In AN‐1792‐vaccinated AD patients, parenchymal Aβ plaques were diminished, whereas cerebrovascular Aβ accumulation was increased. 31 This finding may be partially explained by the excessive antibody‐solubilized senile plaque Aβ that is redeposited in the cerebral vasculature, as well as impaired Aβ clearance through IPAD, 32 demonstrating the necessity of promoting IPAD. 2 Because the driving force of IPAD is the spontaneous contraction and relaxation of cerebrovascular SMCs, 33 , 34 several approaches have been proposed to modulate vasomotion, 3 including the stimulation of α1A adrenergic receptors 35 and the inhibition of PDE‐3. 4 , 36 An amelioration of cerebrovascular Aβ accumulation by cilostazol treatment has been demonstrated in several AD model mouse lines. 4 , 36 Vascular Aβ impairs vasodilation, 37 whereas cilostazol exerts its vasodilatory effects by increasing cAMP levels in vascular SMCs. 38 Cerebrovascular Aβ accumulation in AD patients is positively correlated with PDE‐3 expression in the vessel walls, which may be associated with impaired IPAD. 4 Thus a strong inhibitory effect of OPC‐13015 on PDE‐3 14 may result in the facilitation of IPAD.
Several limitations to the present study should be described. First, we enrolled MCI patients for whom cilostazol was newly prescribed for clinical purposes. Subsequently, all patients had mild cerebrovascular disease, such as lacunar infarcts. It might therefore be difficult to apply the current findings to patients without cerebrovascular disease. However, cerebrovascular disease has been demonstrated previously in the majority of patients with cognitive impairment, especially in older patients. 39 Second, the limited number of cases may have affected the results of this study. In particular, the subgroup analysis should be interpreted with caution, and a large‐scale prospective study is warranted. Third, the drug response was determined by the change in MoCA score over a 6‐month interval, which is a relatively short period. A longer follow‐up should be conducted in future studies.
In conclusion, the conversion from cilostazol to OPC‐13015 was associated significantly with an amelioration of cognitive impairment. The grouping of patients based on the results of biomarkers might facilitate more targeted treatment; this is known as stratified or precision medicine. 40 The OPC‐13015 level is thus expected to be a useful predictive biomarker of cilostazol treatment for dementia.
CONFLICTS OF INTEREST
Mr. Kawakami and Mr. Yamamoto are employees of Shimadzu Corporation, an analytical instrument manufacturer that is not involved in the sale of cilostazol. Dr. Ihara has a patent concerning cilostazol (WO2013187075A1) titled “Prophylactic and/or therapeutic agent for mild cognitive impairment.” Dr. Saito, Mr. Kawakami, Mr. Yamamoto, and Dr. Ihara have applied for a patent concerning the usefulness of evaluating the levels of cilostazol and its metabolites. In addition, Dr. Ihara reports grants from Panasonic, BMS, and Otsuka Pharmaceutical, and personal fees from Daiichi Sankyo Co Ltd, Eisai, and Bayer, which were not involved in the current work. The other authors declare no competing financial interests.
AUTHOR CONTRIBUTIONS
Satoshi Saito designed the study, recruited and followed the participants, analyzed and interpreted the data, and wrote the manuscript; Kaori Shinmyozu, Miho Yamauchi, Shuhei Ikeda, and Yorito Hattori analyzed and interpreted the data and wrote the manuscript; Daisuke Kawakami, Rintaro Yamamoto, and Naoki Hayakawa supervised and made critical revisions of the manuscript for important intellectual content; Masafumi Ihara designed the study, recruited and followed the participants, wrote the manuscript, and supervised all portions of the study. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
The authors wish to thank Prof. Roxana O. Carare at the University of Southampton for her insightful discussion and Ms. Erika Kitajima at the National Cerebral and Cardiovascular Center for her technical assistance. We are also grateful for support from the National Cerebral and Cardiovascular Center Biobank (http://www.ncvc.go.jp/biobank/). We thank Bronwen Gardner, PhD, from Edanz Group (https://en‐author‐services.edanz.com/ac), for editing a draft of this manuscript. This study was funded by a Grant‐in‐Aid from the Japan Society for the Promotion of Science Fellows (19J00106), the Japan Agency for Medical Research and Development (20ek0210120h0002), and the Shimadzu Corporation.
Saito S, Shinmyozu K, Kawakami D, et al. Conversion from cilostazol to OPC‐13015 linked to mitigation of cognitive impairment. Alzheimer's Dement. 2021;7:e12182. 10.1002/trc2.12182
Contributor Information
Satoshi Saito, Email: saitou.satoshi.43m@kyoto-u.jp.
Kaori Shinmyozu, Email: sinmyozu@ncvc.go.jp.
Daisuke Kawakami, Email: daikawa@shimadzu.co.jp.
Miho Yamauchi, Email: yamauchi@ncvc.go.jp.
Shuhei Ikeda, Email: ikeda.shuhei83@ncvc.go.jp.
Yorito Hattori, Email: yoh2019@ncvc.go.jp.
Rintaro Yamamoto, Email: rintaro@shimadzu.co.jp.
Naoki Hayakawa, Email: hayakawa.naoki@ncvc.go.jp.
Masafumi Ihara, Email: ihara@ncvc.go.jp.
3.1. Data availability statement
Raw data were preserved at the National Cerebral and Cardiovascular Center. The derived data supporting the findings of this study are available from the corresponding author on request.
REFERENCES
- 1. Mawuenyega KG, Sigurdson W, Ovod V, et al. Decreased clearance of CNS β‐amyloid in Alzheimer's disease. Science. 2010;330:1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Saito S, Yamamoto Y, Ihara M. Development of a multicomponent intervention to prevent Alzheimer's disease. Front Neurol. 2019;10:490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carare RO, Aldea R, Agarwal N, et al. Clearance of interstitial fluid (ISF) and CSF (CLIC) group—part of Vascular Professional Interest Area (PIA). Alzheimers Dement (Amst). 2020;12:e12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Maki T, Okamoto Y, Carare RO, et al. Phosphodiesterase III inhibitor promotes drainage of cerebrovascular β‐amyloid. Ann Clin Transl Neurol. 2014;1:519‐533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saito S, Kojima S, Oishi N, et al. A multicenter, randomized, placebo‐controlled trial for cilostazol in patients with mild cognitive impairment: the COMCID study protocol. Alzheimers Dement (N Y). 2016;2:250‐257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ihara M, Saito S. Drug repositioning for Alzheimer's disease: finding hidden clues in old drugs. J Alzheimers Dis. 2020;74:1013‐1028. [DOI] [PubMed] [Google Scholar]
- 7. Taguchi A, Takata Y, Ihara M, et al. Cilostazol improves cognitive function in patients with mild cognitive impairment: a retrospective analysis. Psychogeriatrics. 2013;13:164‐169. [DOI] [PubMed] [Google Scholar]
- 8. Ihara M, Nishino M, Taguchi A, et al. Cilostazol add‐on therapy in patients with mild dementia receiving donepezil: a retrospective study. PLoS One. 2014;9:e89516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tai SY, Chien CY, Chang YH, Yang YH. Cilostazol use is associated with reduced risk of dementia: a nationwide cohort study. Neurotherapeutics. 2017;14:784‐791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wardlaw J, Bath PMW, Doubal F, et al. Protocol: the Lacunar Intervention Trial 2 (LACI‐2). A trial of two repurposed licenced drugs to prevent progression of cerebral small vessel disease. Eur Stroke J 2020;5(3):297‐308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Akiyama H, Kudo S, Shimizu T. The metabolism of a new antithrombotic and vasodilating agent, cilostazol, in rat, dog and man. Arzneimittelforschung. 1985;35:1133‐1140. [PubMed] [Google Scholar]
- 12. Lee HI, Byeon JY, Kim YH, et al. Effects of CYP2C19 and CYP3A5 genetic polymorphisms on the pharmacokinetics of cilostazol and its active metabolites. Eur J Clin Pharmacol. 2018;74:1417‐1426. [DOI] [PubMed] [Google Scholar]
- 13. Cui A, Kim YH, Ghim JL, et al. Pharmacokinetic modeling analysis of cilostazol and its active metabolites (OPC‐13015 and OPC‐13213) after multiple oral doses of cilostazol in healthy Korean volunteers. Xenobiotica. 2020;50:288‐296. [DOI] [PubMed] [Google Scholar]
- 14. Liu Y, Shakur Y, Yoshitake M, Kambayashi Ji J. Cilostazol (pletal): a dual inhibitor of cyclic nucleotide phosphodiesterase type 3 and adenosine uptake. Cardiovasc Drug Rev. 2001;19:369‐386. [DOI] [PubMed] [Google Scholar]
- 15. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging‐Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:270‐279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43:2412‐2414. [DOI] [PubMed] [Google Scholar]
- 17. Berg L, Miller JP, Baty J, Rubin EH, Morris JC, Figiel G. Mild senile dementia of the Alzheimer type. 4. Evaluation of intervention. Ann Neurol. 1992;31:242‐249. [DOI] [PubMed] [Google Scholar]
- 18. Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695‐699. [DOI] [PubMed] [Google Scholar]
- 19. Fujiwara Y, Suzuki H, Yasunaga M, et al. Brief screening tool for mild cognitive impairment in older Japanese: validation of the Japanese version of the Montreal Cognitive Assessment. Geriatr Gerontol Int. 2010;10:225‐232. [DOI] [PubMed] [Google Scholar]
- 20. Fazekas F CJ, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer's dementia and normal aging. AJR Am J Roentgenol. 1987;149:351‐356. [DOI] [PubMed] [Google Scholar]
- 21. Cordonnier C, Potter GM, Jackson CA, et al. Improving interrater agreement about brain microbleeds: development of the Brain Observer MicroBleed Scale (BOMBS). Stroke. 2009;40:94‐99. [DOI] [PubMed] [Google Scholar]
- 22. Greenberg SM, Charidimou A. Diagnosis of cerebral amyloid angiopathy: evolution of the Boston criteria. Stroke. 2018;49:491‐497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ohno Y, Kitahara H, Fujii K, et al. High residual platelet reactivity after switching from clopidogrel to low‐dose prasugrel in Japanese patients with end‐stage renal disease on hemodialysis. J Cardiol. 2019;73:51‐57. [DOI] [PubMed] [Google Scholar]
- 24. Wang Z, Dai Z, Shu H, et al. APOE genotype effects on intrinsic brain network connectivity in patients with amnestic mild cognitive impairment. Sci Rep. 2017;7:397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Suri A, Forbes WP, Bramer SL. Effects of CYP3A inhibition on the metabolism of cilostazol. Clin Pharmacokinet. 1999;37(suppl 2):61‐68. [DOI] [PubMed] [Google Scholar]
- 26. Suri A, Bramer SL. Effect of omeprazole on the metabolism of cilostazol. Clin Pharmacokinet. 1999;37(suppl 2):53‐59. [DOI] [PubMed] [Google Scholar]
- 27. Louveau A, Smirnov I, Keyes TJ, et al. Structural and functional features of central nervous system lymphatic vessels. Nature. 2015;523:337‐341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aspelund A, Antila S, Proulx ST, et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J Exp Med. 2015;212:991‐999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Da Mesquita S, Louveau A, Vaccari A, et al. Functional aspects of meningeal lymphatics in ageing and Alzheimer's disease. Nature. 2018;560:185‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tarasoff‐Conway JM, Carare RO, Osorio RS, et al. Clearance systems in the brain‐implications for Alzheimer disease. Nat Rev Neurol. 2015;11:457‐470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nicoll JA, Wilkinson D, Holmes C, Steart P, Markham H, Weller RO. Neuropathology of human Alzheimer disease after immunization with amyloid‐beta peptide: a case report. Nat Med. 2003;9:448‐452. [DOI] [PubMed] [Google Scholar]
- 32. Patton RL, Kalback WM, Esh CL, et al. Amyloid‐beta peptide remnants in AN‐1792‐immunized Alzheimer's disease patients: a biochemical analysis. Am J Pathol. 2006;169:1048‐1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. van Veluw SJ, Hou SS, Calvo‐Rodriguez M, et al. Vasomotion as a driving force for paravascular clearance in the awake mouse brain. Neuron. 2020;105(3):549‐561.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Aldea R, Weller RO, Wilcock DM, Carare RO, Richardson G. Cerebrovascular smooth muscle cells as the drivers of intramural periarterial drainage of the brain. Front Aging Neurosci. 2019;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Frost M, Keable A, Baseley D, et al. Vascular α1A adrenergic receptors as a potential therapeutic target for IPAD in Alzheimer's disease. Pharmaceuticals (Basel). 2020;13:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yakushiji Y, Kawamoto K, Uchihashi K, et al. Low‐dose phosphodiesterase III inhibitor reduces the vascular amyloid burden in amyloid‐β protein precursor transgenic mice. Int J Mol Sci. 2020;21:2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Park L, Koizumi K, El Jamal S, et al. Age‐dependent neurovascular dysfunction and damage in a mouse model of cerebral amyloid angiopathy. Stroke. 2014;45:1815‐1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tanaka T, Ishikawa T, Hagiwara M, Onoda K, Itoh H, Hidaka H. Effects of cilostazol, a selective cAMP phosphodiesterase inhibitor on the contraction of vascular smooth muscle. Pharmacology. 1988;36:313‐320. [DOI] [PubMed] [Google Scholar]
- 39. Toledo JB, Arnold SE, Raible K, et al. Contribution of cerebrovascular disease in autopsy confirmed neurodegenerative disease cases in the National Alzheimer's Coordinating Centre. Brain. 2013;136:2697‐2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Trusheim MR, Burgess B, Hu SX, et al. Quantifying factors for the success of stratified medicine. Nat Rev Drug Discov. 2011;10:817‐833. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Raw data were preserved at the National Cerebral and Cardiovascular Center. The derived data supporting the findings of this study are available from the corresponding author on request.


