Abstract
Using data from the fourth wave of the National Study of Adolescent Health, this paper offers a preliminary investigation of factors implicated in the physical and mental health of bisexual individuals. The roles of sleep, socioeconomic status, feelings of disrespect, and reported lack of health insurance are considered. Further, this study examines depression as a psychological stress response and systemic inflammation as a physiological stress response. Systemic inflammation in this population was estimated using the biomarker C-reactive protein (CRP). Reported acute illness in the past month and blood pressure serve as measures of physical health outcomes. Analyses revealed a pattern of elevated CRP (>3mg/L) among participants who reported no health insurance coverage. For participants who reported no health insurance coverage and identified as mostly homosexual, bisexual, or mostly heterosexual, feelings of disrespect were associated both with their sleep outcomes as well as their total household income. Moreover, linear regression showed that CRP significantly predicted blood pressure values. These analyses serve to bring health disparities and specific considerations for individuals attracted to more than one gender further into scientific conversation. Suggestions for further study of bisexual minority stress and bisexual health are offered.
Keywords: bisexuality, minority stress, socioeconomic status, c-reactive protein, sleep, health insurance
Introduction
As shown in Kaestle & Ivory’s 2012 content analysis of bisexuality in medical literature, currently accepted medical knowledge may not be entirely accurate or, at least, current treatment options may be less effective because of specific considerations that must take place for bisexual individuals that are often overlooked in the medical atmosphere. In part, this is due to the history of evaluations occurring primarily in heterosexual individuals or of analyses observing sexual minorities as a group, rather than looking at bisexual individuals separately. One of the issues brought to light by Kaestle & Ivory (2012) is the often-adopted view of bisexuality as a path by which infections spread, particularly in epidemiological research, which leads to research problematizing bisexuality rather than research focused on protective effects for bisexual individuals and specialized interventions and treatments (Kaestle & Ivory, 2012).
Jones (2010) describes the experience of bisexual individuals as an “invisible minority” within the LGBTQ+ community. This notion arises because bisexual individuals are often viewed as “straight” in queer spaces or media, often when bisexual individuals are in relationships with partners of another gender, while carrying the burden of sexual minority stress, a specific kind of chronic stress specific to members of the queer community. Jones (2010) describes the term “biphobia”, a succinct descriptor for the exclusion of bisexual individuals from peer social support under the premise of these individuals being perceived as not “queer enough.” This, unfortunately, ignores the real discrimination these individuals experience as a part of the queer community while destroying the social support group this community is supposed to offer.
Feinstein & Dyar (2017) address some poignant health disparities for bisexual individuals: mental health, substance use, and sexual health. They propose a mechanism by which these health disparities occur: bisexual minority stress. Bisexual minority stress is described as “increased risk for negative health outcomes … due to chronic stress related to bisexual stigma and discrimination.” (Feinstein & Dyar, 2017, p. 44–45).
Altered patterns of sleep have been proposed as mechanism for the health outcomes associated with discrimination. Bakour et al. (2017) explores the connection between sleep duration trajectories and systemic inflammation. Buckhalt et al. (2007) describes the ways sleep affects cognitive function and further examines these effects as moderated by socioeconomic status (SES), and a more recent paper (Philbrook et al., 2017) examines the moderating effects of sex and ethnicity.
Of further concern is the effect of socioeconomic status (SES) on health (Lynch, Kaplan, & Salonen, 1997; Lynch, Kaplan, & Schema, 1997; Lynch & Kaplan, 2000). Generally, there is a positive relationship between income and health outcomes, which is to say that health improves as income increases. In the United States, especially for minority populations, this is likely related to better access to quality health insurance and health care, and subsequently better health outcomes (Sudano & Baker, 2006; Monheit & Vistnes, 2000). Baker et al. (2001) report that participants that are either continuously or intermittently uninsured show worsened health outcomes, including lower ratings of self-reported health and greater chance of mobility issues with age.
Another measure that may be associated with these social factors is inflammation. There is substantial literature tying psychosocial stress to cardiovascular pathology (Williams & Littman, 1996; Lynch et al., 1998; Rozanski et al., 1999). Both Black & Garbutt (2002) and Lick et al. (2013) propose connections between inflammatory response and social pressure. In Black and Garbutt’s 2002 review they offer a model and many potential pathways by which psychosocial stress may affect one’s inflammation and individual pathogenesis of cardiovascular disease. Further, Lick et al. (2013) cite immune dysregulation, a broad term including inflammation, as one of many proposed pathways linking minority stress to negative health outcomes for sexual minorities.
It is clear that inflammation is a key factor underlying health outcomes associated with social pressures. One potential marker for altered inflammatory response is the high sensitivity C-reactive protein (CRP) (Genest, 2010; Arima et al., 2008; Schmidt et al., 2003). CRP has been implicated in depressive symptoms (Krogh et al., 2012), a domain of health that is of particular concern for bisexual individuals (Barker, 2015). Kohler-Forsberg et al. (2017) shows a linear regression between CRP values and scores on the Montgomery-Asberg Depression Rating Scale, even when controlling for age gender, anti-inflammatory and psychotropic drug treatment, BMI, smoking, and inflammatory diseases. White et al. (2017) fleshes out the connection between CRP and depression in older populations and suggests that the association between CRP and depression can be modified by antidepressant treatment, potentially suggesting a physiological connection between depression and CRP.
Drawing on the model presented in Lick et al. (2013), the present study sets out to test a proposed model by which the effect of sociocultural stressors on health status for plurisexual individuals is mediated by psychological and physiological stress responses and health behaviors. While Lick et al. (2013) also suggest a mediational role of appraisal and cognitive style, that part of the model is not tested in the current study due to the available variables. The hypothesized model is shown in figure one. Total household income and feelings of disrespect are conceptualized as sociocultural stressors. Reported diagnoses of depression are conceptualized as a psychological stress response, and CRP values are conceptualized as a physiological stress response. Trouble falling and staying asleep are labeled as health behaviors, and health status is measured by reported acute illness and participant blood pressure values.
Figure 1.
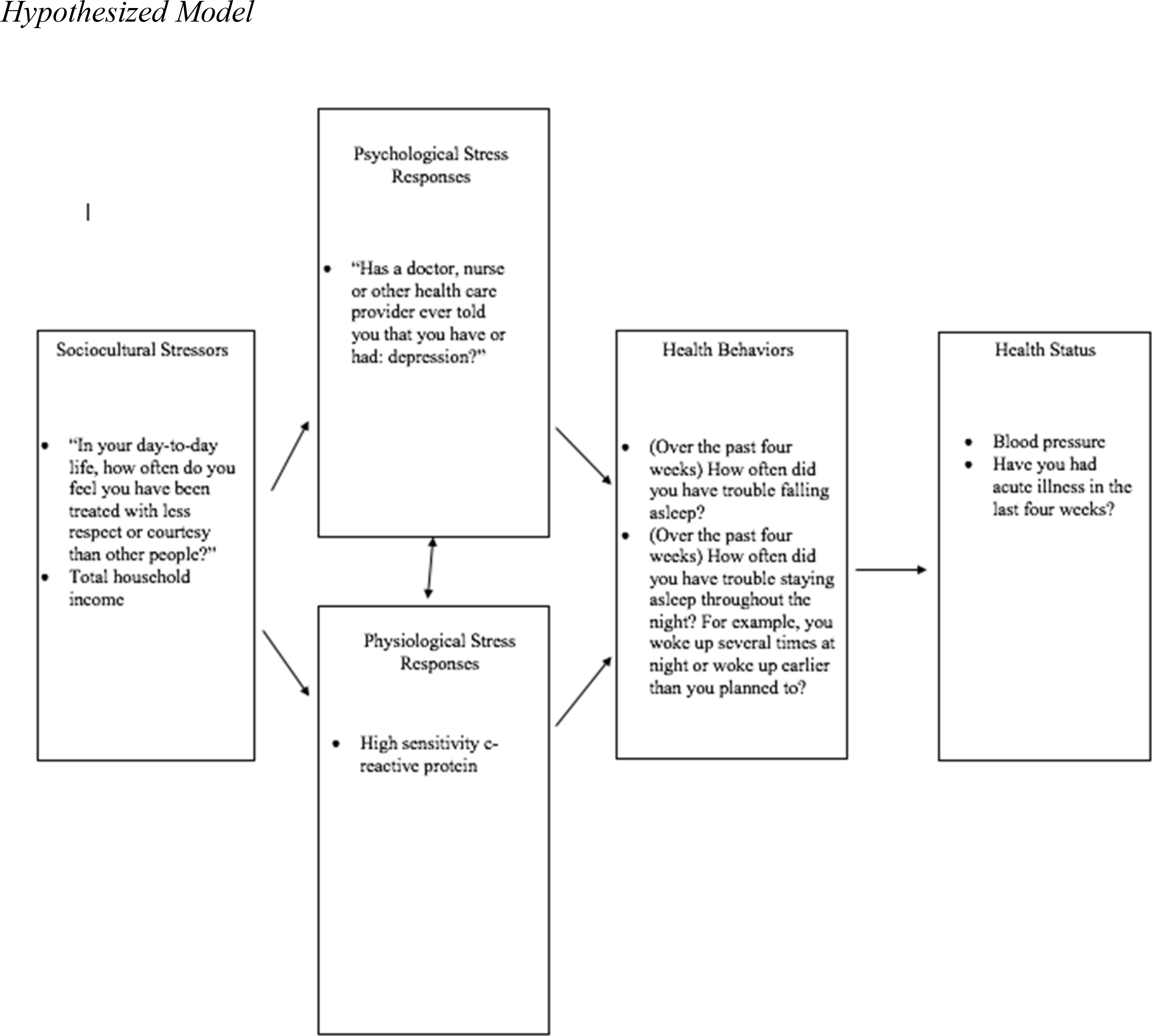
Hypothesized Model
While there are many other variables that may fit within the umbrellas of our mediators (psychological and psychological stress responses and health behaviors), the roles of sleep, depression, and CRP are critical pieces of understanding health outcomes for bisexual or plurisexual individuals. Clinical interventions may benefit from a deeper understanding of the external factors contributing to depression, sleep disturbances, inflammation, hypertension, or acute illness especially in a group vulnerable to sociocultural stressors. On a legislative level, understanding these factors may serve as evidence for universal health care as a human right, as it is presently shown that physiological stress responses vary given access to health care (although it should be noted that some of this sample may still receive health care despite reporting no health insurance in 2008).
It is presently hypothesized that the effect of the exposures (total household income and feelings of being treated with less respect than others) on measured health outcomes (blood pressure and acute illness) are mediated by diagnoses of depression, CRP values, and trouble falling/staying asleep.
Materials and Methods
Data were obtained from Add Health, The National Longitudinal Study of Adolescent to Adult Health. Data for the current study was selected from wave IV of the Add Health study, which was collected in 2008 when participants were age 24–34. Responses to a multitude of survey questions were recorded in in-home interviews conducted with each participant. Dried blood spot (DBS) analysis was also conducted in-home in order to determine CRP values for each participant. Blood pressure was collected using an arm cuff. Systolic and diastolic blood pressure values were combined in the variable “blood pressure classification,” with categories for normal blood pressure, prehypertension, and two degrees of hypertension. These values were extracted for present analyses. Participants with missing data were excluded from analyses.
Among many others, participants were asked to answer each of the following questions. The first item was “In your day-to-day life, how often do you feel you have been treated with less respect or courtesy than other people?” The second item was “(Over the past four weeks) How often did you have trouble falling asleep?” The third item was“(Over the past four weeks) How often did you have trouble staying asleep throughout the night? For example, you woke up several times at night or woke up earlier than you planned to?” The fourth item was “Thinking about your income and the income of everyone who lives in your household and contributes to the household budget, what was the total household income before taxes and deductions in {2006/2007/2008}? Include all sources of income, including non-legal sources.” The fifth item was “Which of the following best describes your current health insurance situation?” The sixth item was “Has a doctor, nurse or other health care provider ever told you that you have or had depression?” The seventh item was “Have you had acute illness in the last four weeks?” The eighth item was “Please choose the description that best fits how you think about yourself.” (100% heterosexual/straight, mostly heterosexual/straight but somewhat attracted to people of your own sex, bisexual/attracted to men and women equally, mostly homosexual/gay but somewhat attracted to people of the opposite sex, 100% homosexual/gay, or not sexually attracted to either males or females).
In other words, these are single questions being conceptualized as variables rather than using measures with multiple questions analyzed as a single variable. The present variables can be more easily described as feelings of disrespect, trouble falling asleep, trouble staying asleep, total household income, diagnoses of depression, and acute illness. Lastly, a modified version of the Kinsey scale was included that allowed participants to choose the response label that best fits them rather than asking participants to respond to a series of questions to determine their score on the continuum.
Analytic Strategy
First, an exploratory analysis was run by comparing the mean CRP values for participants without health insurance (n = 950). Participants were only included in the analysis of CRP means if they reported no health insurance above and responded to the modified Kinsey scale. Elevated CRP was operationalized in Shanahan et al. (2014) as greater than 3mg/L.
Further analyses included responses only from participants who reported they had no health insurance and who reported a 2, 3, or 4 on the modified Kinsey scale. Analysis was conducted using SPSS to run Pearson’s correlations between responses to questions listed above as well as participants’ CRP and blood pressure values, excluding cases of missing data list-wise (n = 114). A p-value of less than 0.05 was designated to be a significant association. These correlations were run as a potential indicator that our present variables met the qualifications for mediation, which they did not. While mediation could not be established, linear regression was still run using the values mentioned above (n = 114).
Demographic analyses were run on participants who reported “you have no health insurance” and responded to the modified Kinsey scale. The original sample size is 950, but 122 participants refused a survey question inquiring about total household income, so the sample size is 828 for that demographic analysis. In the demographic analyses of participants who reported no health insurance and identified as mostly heterosexual, bisexual, or mostly homosexual, there were missing cases of total household income, so the sample size is 117, while the other demographic variables had 133 cases.
Results
Results of demographic analyses are included in table 1. This first analysis includes all participants who reported no health insurance coverage. While unable to disaggregate participants who were cisgender or transgender, this analysis does break down the sample demographically by assigned sex and race of respondent as reported by the interviewer. As for SES, the sample demographics for total household income and highest education level achieved to date are given. Household income may be the better estimate of participant SES, as education level might be skewed due to the younger age of participants (24 to 34 years old). These same analyses were run for plurisexual participants, or those who identified as mostly homosexual, bisexual, and mostly heterosexual. Results are shown in table 2.
Table 1.
Demographics of Participants Without Health Insurance
| Race of Respondent as Reported by Interviewer | Number | Percentage |
|---|---|---|
| White | 680 | 71.6 |
| Black or African American | 248 | 26.1 |
| American Indian/Alaskan Native | 5 | 0.5 |
| Asian or Pacific Islander | 17 | 1.8 |
| Assigned Sex | Number | Percentage |
| Male | 518 | 54.5 |
| Female | 432 | 45.5 |
| Total Household Income | Number | Percentage |
| Less than 5,000 | 36 | 4.3 |
| 5,000 to 9,999 | 42 | 5.1 |
| 10,000 to 14,999 | 66 | 8.0 |
| 15,000 to 19,999 | 66 | 8.0 |
| 20,000 to 24,999 | 75 | 9.1 |
| 25,000 to 29,999 | 82 | 9.9 |
| 30,000 to 39,999 | 106 | 12.8 |
| 40,000 to 49,999 | 111 | 13.4 |
| 50,000 to 74,999 | 132 | 15.9 |
| 75,000 to 99,999 | 61 | 7.4 |
| 100,000 to 149,999 | 29 | 3.5 |
| 150,000 or more | 22 | 2.7 |
| Highest Education Level Achieved to Date | Number | Percentage |
| 8th grade or less | 9 | 0.9 |
| Some high school | 146 | 15.4 |
| High school graduate | 238 | 25.1 |
| Some vocational/technical training after high school | 48 | 5.1 |
| Completed vocational/technical training after high school | 64 | 6.7 |
| Some college | 328 | 34.5 |
| Completed college (bachelor’s degree) | 79 | 8.3 |
| Some graduate school | 16 | 1.7 |
| Completed a master’s degree | 9 | 0.9 |
| Highest Education Level | Number | Percentage |
| Some graduate training beyond a master’s degree | 5 | 0.5 |
| Some post baccalaureate professional education | 4 | 0.4 |
| Completed post baccalaureate professional education | 4 | 0.4 |
Table 2.
Demographics of Plurisexual Participants Without Health Insurance
| Race of respondent as reported by interviewer | Number | Percentage |
|---|---|---|
| White | 104 | 78.2 |
| Black or African American | 26 | 19.4 |
| American Indian/Alaskan Native | 1 | 0.8 |
| Asian or Pacific Islander | 2 | 1.5 |
| Assigned Sex | Number | Percentage |
| Male | 24 | 18.0 |
| Female | 109 | 82.0 |
| Total Household Income | Number | Percentage |
| Less than 5,000 | 3 | 2.3 |
| 5,000 to 9,999 | 6 | 4.5 |
| 10,000 to 14,999 | 10 | 7.5 |
| 15,000 to 19,999 | 11 | 8.3 |
| 20,000 to 24,999 | 9 | 6.8 |
| 25,000 to 29,999 | 10 | 7.5 |
| 30,000 to 39,999 | 20 | 15.0 |
| 40,000 to 49,999 | 12 | 9.0 |
| 50,000 to 74,999 | 16 | 12.0 |
| 75,000 to 99,999 | 11 | 8.3 |
| 100,000 to 149,999 | 4 | 3.0 |
| 150,000 or more | 5 | 3.8 |
| Highest Education Level Achieved to Date | Number | Percentage |
| 8th grade or less | 1 | 0.8 |
| Some high school | 18 | 13.5 |
| High school graduate | 15 | 11.3 |
| Some vocational/technical training after high school | 9 | 6.8 |
| Completed vocational/technical training after high school | 8 | 6.0 |
| Some college | 58 | 43.6 |
| Completed college (bachelor’s degree) | 17 | 12.8 |
| Some graduate school | 2 | 1.5 |
| Highest Education Level | Number | Percentage |
| Completed a master’s degree | 2 | 1.5 |
| Some graduate training beyond a master’s degree | 3 | 1.5 |
The mean CRP values for participants without health insurance were all greater than 3mg/L, except for participants who reported that they are mostly homosexual, but somewhat attracted to the opposite sex. These values are shown in table 3. Mean CRP for participants who reported attraction to multiple genders (or responded with a 2,3, or 4 to question 6) is 4.51mg/L, with a standard deviation of 6.71.
Table 3.
Mean hsCRP Values of Participants Without Health Insurance
| Sexual Self Definition | Mean (hsCRP) (mg/L) | N | Standard Deviation |
|---|---|---|---|
| (1) 100% heterosexual (straight) | 4.963 | 799 | 8.770 |
| (2) Mostly heterosexual, but somewhat attracted to same sex | 5.046 | 98 | 7.936 |
| (3) Bisexual, that is, attracted to men and women equally | 4.743 | 28 | 5.510 |
| (4) Mostly homosexual, but somewhat attracted to opposite sex | 1.517 | 7 | 0.715 |
| (5) 100% homosexual (gay) | 3.849 | 14 | 6.855 |
| (6) Not sexually attracted to either males or females | 8.936 | 4 | 9.228 |
| Total | 4.940 | 950 | 8.548 |
Feelings of disrespect were significantly associated with trouble falling asleep (r = 0.194, p < 0.05) and trouble staying asleep (r = 0.220, p < 0.01). Feelings of disrespect were also significantly associated with total household income (r = −0.227, p < 0.01) with participants reporting reduced household income also tending to report feelings of disrespect. Interestingly, participants’ reported total household income was not associated with their sleep quality. Diagnoses of depression were significantly associated with feelings of disrespect (r = .198, p < 0.05), trouble falling asleep (r = .344, p < 0.01), and trouble staying asleep (r = .277, p < 0.01). Blood CRP level was measured as a marker for inflammation in these participants. CRP was not significantly associated with any of the measures observed except for blood pressure values (r = .247, p < 0.01).
While none of the hypothesized exposures predicted the measured outcomes, feelings of disrespect were a significant predictor of trouble falling asleep (B = .194, p < 0.05) and trouble staying asleep (B = .220, p < 0.05). None of the hypothesized mediators predicted any measured outcomes except for CRP values, which predicted blood pressure values (B = .247, p < 0.01).
Discussion
The connection between participants feeling as if they are treated with less respect and having trouble falling and/or staying asleep is not an entirely novel discovery but is worth examining because of the population reporting these issues (bisexual individuals without health insurance, or rather, participants who responded with a Kinsey 2, 3, or 4 and who reported no health insurance). This connection further corroborates the proposed mechanism of sleep as a pathway between minority stress and negative health outcomes.
The negative relationship between total household income and feelings of disrespect is unsurprising, as lower SES is often linked to discrimination (Fuller-Rowell et al., 2012; Caputo, 2003; Kessler et al., 1999). What this does tell us is that there may be a protective role of income in the connection between minority stress and health outcomes, and even more so if being of lower SES is conceptualized as lack of health care. This is not to say that wellness should be stratified by status, but instead that there are even more reasons why greater social mobility, economic equality, and access to health care as a human right are needed in the United States specifically.
Notably, only blood pressure values showed a statistically significant relationship with CRP values. This is likely due to the lack of demographic controls in the analyses, which is to say that commonly used controls like gender and race/ethnicity were ignored. This decision was made because of the small number of participants (of all genders and ethnicities) who reported no health insurance and identified as bisexual or plurisexual.
Further, there was not a statistically significant connection between total household income and trouble falling or staying asleep. This puzzling finding may be due to lack of demographic controls as well as sample size and is contradictory to a large body of literature on sleep and SES (El-Sheikh et al., 2010; Marco et al., 2011; Buckhalt, 2011).
The connections shown presently between sleep and depression are critical for the understanding of bisexual or plurisexual needs in health care from the perspective of a provider or a legislator. Individuals who do not identify with monosexuality are seemingly vulnerable to sociocultural stressors in unique ways, and any health care system should reflect the needs of those that it serves. These present analyses show how sleep and access to treatment could potentially make a lasting positive difference in the lives of nonmonosexual individuals.
Limitations and Future Directions
The scale used in the study to measure sexuality or sexual identity was a modified version of the Kinsey Scale (Kinsey, 1998) which offers multiple categories of sexuality; however, these categories might not align with one’s definition of bisexuality. Some bisexual individuals may feel more attracted to one gender than the other, and therefore the wording of this scale, that they would be “mostly homosexual” or “mostly heterosexual”, might throw off responses in unexpected ways. Additionally, the label of Kinsey 6 is described in the add health study as “not sexually attracted to either males or females.” While this could be operationalized as asexuality, there may be participants who feel sexual attraction, but their feelings do not ascribe to the label of male or female, which could lead them to choose the Kinsey 6 label, further complicating results. Some participants may identify as pansexual or queer, while feeling equal attraction to feminine and masculine presenting partners, but be deterred from choosing the Kinsey 3 label, as it uses the term bisexual, implicitly excluding pansexuality and queer identities from this category.
The problem here is not with the respondents, but with the measure being used. While the Add Health study does word their prompt for this question, “please choose the description that best fits how you think about yourself,” appropriately leaving the question up to some interpretation by the participant, this can complicate any conclusions drawn from the data. Notably, there are other measures of sexual behavior in the Add Health data, for example, the number of male or female sexual partners reported by the participant. These measures are complicated by the existence of non-binary and genderqueer gender identities, as is the Kinsey scale. Further, as elucidated in Fricke & Sironi (2017), there can be different health implications when the measure of sexuality as a broad term is changed; it would seem that sexual minority behavior is implicated differently in the health of sexual minorities than sexual minority identity.
For these reasons, it is prudent to include multiple measures of identity in future research examining bisexual identity or sexual minority identities as a whole. The Storms Sexuality Axis could be a potentially more accurate measure, because it allows one to place themselves on a continuum, as identity is almost always more continuous than categorical. The Klein Sexual Orientation Grid (KSOG) could also be of use when examining sexual minority identity over time and dives deeper into different fixtures of sexuality beyond current behavior or current identity. Both of these measures are described in greater detail in Gibson et al. (2014).
Galupo et al. (2014) focuses on a thematic analysis of sexual minority individuals’ reactions to the conceptualization and measurement of sexual orientation through the use of the Kinsey Scale and the KSOG. While the Kinsey scale was the first attempt to measure the fluidity and diversity of human sexual behavior, it still has its shortcomings, like obscuring within-group differences among bisexual or plurisexual individuals with varied attraction to different genders. Research employing the KSOG has still tended to view nonmonosexual individuals as a monolith rather than a group made up of individual, subjective experiences.
Also highlighted in Galupo et al. (2014) are the experiences of transgender and gender nonconforming individuals, whose gender identity or expression may not fit into traditional gender categories, which complicates results drawn from research employing the Kinsey scale or the KSOG. Also mentioned is the distinction that even though research often uses measures to capture sexual orientation, these measures may not always line up with the survey responses the participants would choose themselves. For example, someone may experience attraction to multiple genders but still identify with the label “lesbian” or “gay”. These scales often do not account for the complexity and fluidity of sexual orientation and gender identity and sometimes research can conflate all of the above. The reality of an individual’s identity and behavior defies simplicity and reduction, as is to be expected in any measurement of human experience. The current study attempts to approximate one conceptualization of the nonmonosexual experience and naturally falls short of the reality of any one individual.
As mentioned in White et al. (2017), there may be effects of antidepressant medications on CRP. While the present sample reported no health insurance coverage, it is still possible that some of this group regularly takes antidepressant medications. Future research with this sample might benefit from a sensitivity analysis based on reported medication use. Another prudent limitation relates to the self-report measures used. It is unclear whether the validity of the questions asked is changed when reduced to individual items. Moreover, it seems that not all of these measures have been validated for use with bisexual or plurisexual individuals.
While this paper did not parse out results demographically, that does not mean that intersectionality should be ignored; quite the opposite. Notably, there were no variables in the dataset that would allow us to disaggregate participants identifying cisgender or transgender. It is the responsibility of future science to determine the nuances of the relationships described presently by race/ethnicity, gender identity, SES, ability, or any other marker of disadvantage.
Table 4.
Pearson’s Correlations for Plurisexual Participants Without Health Insurance
| Blood Pressure | Have you had acute illness in the last four weeks? | High sensitivity c-reactive protein (hsCRP) | Has a doctor, nurse, or other health care provider ever told you that you have or had depression? | Total household income | In your day-to-day life, how often do you feel you have been treated with less respect or courtesy than other people? | Over the past four weeks, how often did you have trouble falling asleep? | Over the past four weeks, how often did you have trouble staying asleep throughout the night? | |
|---|---|---|---|---|---|---|---|---|
| Have you had acute illness in the last four weeks? | r = −.001 p = .495 |
r = 1 | r = .013 p = .447 |
r = .080 p = .199 |
r = −.017 p = .430 |
r = .017 p = .430 |
r = .108 p = .127 |
r = −.013 p = .444 |
| High sensitivity c-reactive protein (hsCRP) | r = .247** p = .004 |
r = .013 p = .447 |
r = 1 | r = −.138 p = .071 |
r = −.068 p = .236 |
r = .123 p = .097 |
r = .019 p = .419 |
r = .012 p = .449 |
| Has a doctor, nurse, or other health care provider ever told you that you have or had depression? | r = −.086 p = .182 |
r = .080 p = .199 |
r = −.138 p = .071 |
r = 1 | r = −.109 p = .124 |
r = .198** p = .017 |
r = .344** p = .000 |
r = .277** p = .001 |
| Total house hold income | r = −.017 p = .429 |
r = −0.17 p = .430 |
r = −.068 p = .236 |
r = −.109 p =.124 |
r =1 | r = −.227** p = .008 |
r = −.044 p = .322 |
r = −.001 p = .496 |
| In your day to day-to-day life, how often do you feel you have been treated with less respect or courtesy than other people? | r = −.001 p = .495 |
r = .017 p = .430 |
r = .123 p = .097 |
r = .198* p = .017 |
r = −.227** p = .008 |
r = 1 | r = .194* p = .019 |
r = .220** p = .009 |
| Over the past four weeks, how often did you have trouble falling asleep? | r = .139 p = .070 |
r = .108 p = .127 |
r = .019 p = .419 |
r = .344** p =.000 |
r = −.044 p = .322 |
r = .194* p = .019 |
r = 1 | r = .565** p = .000 |
| Over the past four weeks, how often did you have trouble staying asleep throughout the night? | r = .155 p = .050 |
r = −.013 p = .444 |
r = .012 p = .449 |
r = .277** p = .001 |
r = −.001 p = .496 |
r = .220** p = .009 |
r = .565** p = .000 |
r = 1 |
Correlation is significant at the 0.01 level.
Correlation is significant at the 0.05 level.
Acknowledgments
This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining Data Files from Add Health should contact Add Health, The University of North Carolina at Chapel Hill, Carolina Population Center, Carolina Square, Suite 210, 123 W. Franklin Street, Chapel Hill, NC 27516 (addhealth_contracts@unc.edu). No direct support was received from grant P01-HD31921 for this analysis.
The author would like to thank Mx. Regan Collins, Dr. Richard Chapman, Ms. Leslie Chapman, Mr. Elliot Glover, Mr. Greg Parsons, and Dr. Wendy Reed for their oversight and encouragement.
References
- Arima H, Kubo M, Yonemoto K, Doi Y, Ninomiya T, Tanizaki Y, Hata J, Matsumura K, Iida M, & Kiyohara Y (2008). High-sensitivity C-reactive protein and coronary heart disease in a general population of Japanese: the Hisayama study. Arteriosclerosis, thrombosis, and vascular biology, 28(7), 1385–1391. [DOI] [PubMed] [Google Scholar]
- Baker DW, Sudano JJ, Albert JM, Borawski EA, & Dor A (2001). Lack of health insurance and decline in overall health in late middle age. The New England Journal of Medicine, 345, 1106–1112. [DOI] [PubMed] [Google Scholar]
- Bakour C, Schwartz S, O’Rourke K, Wang W, Sappenfield W, Couluris M, & Chen H (2017). Sleep Duration Trajectories and Systemic Inflammation in Young Adults: Results From the National Longitudinal Study of Adolescent to Adult Health (Add Health). Sleep, 40(11), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker MJ (2015) Depression and/or Oppression? Bisexuality and Mental Health, Journal of Bisexuality, 15:3, 369–384. [Google Scholar]
- Black PH, & Garbutt LD (2002). Stress, inflammation and cardiovascular disease. Journal of Psychosomatic Research, 52(1), 1–23. [DOI] [PubMed] [Google Scholar]
- Buckhalt JA (2011). Insufficient Sleep and the Socioeconomic Status Achievement Gap. Child Development Perspectives, 5(1), 59–65. [Google Scholar]
- Buckhalt JA, El‐Sheikh M and Keller P (2007), Children’s Sleep and Cognitive Functioning: Race and Socioeconomic Status as Moderators of Effects. Child Development, 78: 213–231. [DOI] [PubMed] [Google Scholar]
- Caputo RK (2003). The Effects of Socioeconomic Status, Perceived Discrimination and Mastery on Health Status in a Youth Cohort. Social Work in Health Care, 37(2), 17–42. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Kelly RJ, Buckhalt JA, & Hinnant JB (2010). Children’s sleep and adjustment over time: the role of socioeconomic context. Child development, 81(3), 870–883. [DOI] [PubMed] [Google Scholar]
- Feinstein BA, & Dyar C (2017). Bisexuality, Minority Stress, and Health. Current Sexual Health Reports, 9(1), 42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fricke J, & Sironi M (2017). Dimensions of sexual orientation and sleep disturbance among young adults. Preventive Medicine Reports, 8 (February), 18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Rowell TE, Evans GW, & Ong AD (2012). Poverty and Health: The Mediating Role of Perceived Discrimination. Psychological Science, 23(7), 734–739. [DOI] [PubMed] [Google Scholar]
- Galupo MP, Mitchell RC, Grynkiewicz AL, & Davis KS (2014). Sexual Minority Reflections on the Kinsey Scale and the Klein Sexual Orientation Grid: Conceptualization and Measurement. Journal of Bisexuality, 14(3–4), 404–432. [Google Scholar]
- Genest J (2010). C-reactive protein: Risk factor, biomarker and/or therapeutic target? Canadian Journal of Cardiology, 26, 41A–44A. [DOI] [PubMed] [Google Scholar]
- Gibson MA, Alexander J, & Meem DT (2014). Finding Out: An Introduction to LGBT Studies. SAGE. [Google Scholar]
- Harris KM, & Udry RJ (n.d.). National Longitudinal Study of Adolescent to Adult Health (Add Health) Wave IV, 2008 (N. L. S. of A. to A. H. A.-E. K. S. N. I. of C. H. and H. Development (ed.); V3 ed.). UNC Dataverse. [Google Scholar]
- Jones RL (2010). Troubles with bisexuality in health and social care. In: Jones, Rebecca L and Ward Richard eds. LGBT Issues: Looking beyond Categories. Policy and Practice in Health and Social Care (10). Edinburgh: Dunedin Academic Press, pp. 42–55. [Google Scholar]
- Kaestle CE, & Ivory AH (2012). A Forgotten Sexuality: Content Analysis of Bisexuality in the Medical Literature over Two Decades. Journal of Bisexuality, 12(1), 35–48. [Google Scholar]
- Kessler RC, Mickelson KD, & Williams DR (1999). The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of health and social behavior, 40(3), 208–230. [PubMed] [Google Scholar]
- Kinsey AC (1998). Sexual Behavior in the Human Male. Bloomington: Indiana University Press. muse.jhu.edu/book/42035. [Google Scholar]
- Kinsey AC (1998). Sexual Behavior in the Human Female. Bloomington: Indiana University Press. muse.jhu.edu/book/42036. [Google Scholar]
- Köhler-Forsberg O, Buttenschøn HN, Tansey KE, Maier W, Hauser J, Dernovsek MZ, Henigsberg N, Souery D, Farmer A, Rietschel M, McGuffin P, Aitchison KJ, Uher R, & Mors O (2017). Association between C-reactive protein (CRP) with depression symptom severity and specific depressive symptoms in major depression. Brain, Behavior, and Immunity, 62, 344–350. 10.1016/j.bbi.2017.02.020 [DOI] [PubMed] [Google Scholar]
- Krogh J, Benros ME, & Nordentoft M (2012). hsCRP in depressed outpatients. Any association to depressive symptoms? Neurology, Psychiatry and Brain Research, 18(2), 64–65. [Google Scholar]
- Lick DJ, Durso LE, & Johnson KL (2013). Minority Stress and Physical Health Among Sexual Minorities. Perspectives on Psychological Science, 8(5), 521–548. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Everson SA, Kaplan GA, Salonen R, & Salonen JT (1998). Does low socioeconomic status potentiate the effects of heightened cardiovascular responses to stress on the progression of carotid atherosclerosis?. American journal of public health, 88(3), 389–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch JW, & Kaplan GA (2000). Socioeconomic position. In Berkman LF, & Kawachi I (Eds.), Social epidemiology (pp. 13–35). New York: Oxford University Press, Inc. [Google Scholar]
- Lynch JW, Kaplan GA, & Salonen JT (1997). Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Social Science & Medicine, 44, 809–819. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA, & Shema SJ (1997). Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. The New England Journal of Medicine, 337, 1889–1895. [DOI] [PubMed] [Google Scholar]
- Marco CA, Wolfson AR, Sparling M, & Azuaje A (2011). Family Socioeconomic Status and Sleep Patterns of Young Adolescents. Behavioral Sleep Medicine, 10(1), 70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monheit AC, & Vistnes JP (2000). Race/ethnicity and health insurance status: 1987 and 1996. Medical Care Research & Review, 57(Suppl. 1), 11–35. [DOI] [PubMed] [Google Scholar]
- Philbrook LE, Hinnant JB, Elmore-Staton L, Buckhalt JA, & El-Sheikh M (2017). Sleep and cognitive functioning in childhood: Ethnicity, socioeconomic status, and sex as moderators. Developmental Psychology, 53, 1276–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter S, Gupta SC, Chaturvedi MM, & Aggarwal BB (2010). Oxidative stress, inflammation, and cancer: How are they linked? Free Radical Biology and Medicine, 49(11), 1603–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozanski A, Blumenthal JA, & Kaplan J (1999). Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation, 99(16), 2192–2217. [DOI] [PubMed] [Google Scholar]
- Shanahan L, Bauldry S, Freeman J, & Bondy CL (2014). Self-rated health and C-reactive protein in young adults. Brain, Behavior, and Immunity, 36, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A, Solimano A, and Tim W (2003). C-reactive protein and Other Circulating Markers of Inflammation in the Prediction of Coronary Heart Disease. The New England Journal of Medicine, 1695–1702. [DOI] [PubMed] [Google Scholar]
- Sudano JJ, & Baker DW (2006). Explaining US racial/ethnic disparities in health declines and mortality in late middle age: The roles of socioeconomic status, health behaviors, and health insurance. Social Science and Medicine, 62(4), 909–922. [DOI] [PubMed] [Google Scholar]
- White J, Kivimäki M, Jokela M, & Batty GD (2017). Association of inflammation with specific symptoms of depression in a general population of older people: The English Longitudinal Study of Ageing. Brain, Behavior, and Immunity, 61, 27–30. 10.1016/j.bbi.2016.08.01 [DOI] [PubMed] [Google Scholar]
- Williams RB, & Littman AB (1996). Psychosocial factors: role in cardiac risk and treatment strategies. Cardiology clinics, 14(1), 97–104. [DOI] [PubMed] [Google Scholar]


