Abstract
Background:
Stretching has been proven to be effective on pain and range of motion (ROM) in patients with plantar fasciitis. Despite recent gain in popularity and the proposed theories of effectiveness of foam roller, there is a lack of literature on the effect of foam rolling on plantar fasciitis.
Objective:
The objective of this study was to compare the effects of foam rolling and stretching on pain and ankle ROM in patients with plantar fasciitis.
Methods:
A total of 50 participants were included and randomly allocated to the stretching and foam roller groups. Visual analog scale (VAS), pressure pain thresholds (PPTs) for gastrocnemius, soleus and plantar fascia and weight-bearing lunge test (WBLT) measurements were recorded at baseline and immediately after treatment.
Results:
Within-group analysis has shown there is a statistically significant difference () in all the outcome measures in both foam roller and self-stretching groups. The between-groups analysis showed no statistical significance difference in VAS, plantar fascia PPT and WBLT parameters (with -values of 0.171, 0.372 and 0.861, respectively); however, significant differences were found in gastrocnemius PPT () and soleus PPT ().
Conclusion:
It was seen that both stretching and foam rolling techniques helped in reducing pain and increasing the ROM. However, the effectiveness of foam roller was superior to stretching in terms of increase in PPTs at gastrocnemius and soleus.
Clinical Trial Registration No:
CTRI/2018/01/011398.
Name of registry:
The Clinical Trials Registry — India (CTRI); https://ctri.nic.in.
Keywords: Ankle, foam rolling, plantar fasciitis, trigger points, stretching
Introduction
Plantar fasciitis has been reported as the most common cause of heel pain, which affects around 10% of the non-athletic and athletic populations.1,2,3 Although plantar fasciitis implies inflammatory condition of plantar fascia, evidences suggest it to be associated with degenerative changes and could be classified as a “fasciosis” or “fasciopathy”.4
The classical signs of plantar fasciitis are severe pain after a period of rest, decrease in pain with activity, restriction in ankle range of motion (ROM) and tenderness over medial aspect of calcaneus.1,2
Gastrocnemius and soleus muscles are connected to the plantar fascia by connective tissues.1 According to Bolívar et al., there is an association between posterior leg muscle tightness and development of plantar fasciitis,5 which explains why pain in plantar fascia could be caused due to reduced extensibility and trigger points present in the posterior leg muscles.6
Physiotherapy management for plantar fasciitis includes electrotherapy,7,8 exercise therapy,9,10 myofascial release,6,11,12 taping,13 night splints,14 orthotic devices,2,15 etc. Stretching of gastrocnemius, soleus and plantar fascia remains an important part of conservative treatment for plantar fasciitis. It helps to increase extensibility of soft tissue thus increasing the flexibility of the muscle.16
Recently, foam rolling has been adopted as a tool for self-myofascial release (SMR) which is presumed to work on the same mechanism of treatment as traditional “myofascial release”. However, it requires application of pressure by the individual using self-body weight.17 The movement between the foam roller and tissue structure causes sweeping pressure as well as direct pressure on the soft tissues. This increases lubricity of the fascial layer18 and causes increase in tissue extensibility by breaking adhesions.19
Despite recent gain in popularity and the proposed theories of effectiveness of foam roller, there is a lack of literature on the effect of foam rolling on plantar fasciitis. Previous studies have proven that foam rolling helps to increase extensibility of tissue structures. Therefore, we hypothesized that it could be effective in relieving pain caused by plantar fasciitis by increasing extensibility of the calf muscles and plantar fascia. Hence, this study was undertaken to assess the effects of foam rolling and self-stretching as well as to explore comparative effects of these treatments on pain and ROM in patients having plantar fasciitis.
Methods
The study was approved by the Institutional Ethics Committee, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education. This study was a randomized parallel-controlled trial conducted in tertiary hospitals from February 2018 to February 2019. Based on a previous study, the sample size was calculated to be 25 in each group using 95% confidence interval and 80% power.6
Patients with heel pain referred by an orthopedic surgeon for physiotherapy were approached and screened for inclusion and exclusion criteria. Inclusion criteria required the patients to be aged between 18 years and 60 years with heel pain having such clinical features as heel pain in the morning with first step, insidious sharp pain under the heel, tenderness on medial calcaneus and symptoms decreasing with slight activity (like walking) and worsening toward the end of the day. Participants were excluded if they were having any other musculoskeletal conditions which would hamper their performance, having a history of inflammatory joint disorder, impaired blood circulation and altered sensation in lower extremity. The purpose of the study was explained, written and informed consent was taken from willing participants. The method of sampling used was stratified random sampling for group allotment using the chit method.
Outcome measures studied were the pain and ROM of ankle joint. Pain was assessed using visual analog scale (VAS) and pain pressure threshold (PPT). VAS was a 10-cm-long horizontal line with no pain and worst possible pain at the extremes of the line. PPT was assessed with a mechanical pressure algometer (force gauge, model M3-50; Mark-10 Corporation, USA). PPT was assessed at three predetermined locations on the affected leg: gastrocnemius (middle point over the muscle belly), soleus (center point of the muscle belly 10 cm above the Achilles tendon) and over the posteromedial aspect of the calcaneus for both the groups. Three trials were performed with 30-s rest in between two successive trials. Mean values of the three trials were taken as pain threshold measurements.6 The reliability of algometer has been reported to be high (; 95% CI: 0.82–0.97).20
ROM assessment for dorsiflexion was done by weight-bearing lunge test (WBLT). It has been shown that this type of test has high inter-rater and intra-rater reliabilities [intra-rater ; inter-rater (angle) and 0.99 (distance)].21 A measurement tape was placed on the floor perpendicular to the wall to measure the linear distance between the big toe and the wall. Participants were made to stand on the tape with their big toe and heel on the tape. The patient was allowed to lean on the wall for better balance. Participants were instructed to lunge their knee toward the wall in order to make contact with it without lifting the heel. The foot was progressively moved away or toward the wall until the maximum ROM of the ankle was attainted without lifting the heel.18 Measurements were taken by another physiotherapist before and immediately after the intervention. Assessor was blinded for group allocation and treatment intervention.
Intervention protocols
Foam roller group
Calf muscles: This involved long sitting, with the affected leg extended on the foam roller and foot relaxed. The non-affected leg was flexed at knee so that the foot was rested on the floor. The participants were instructed to use their arms and non-affected foot to propel their body back and forth from the popliteal fossa to Achilles tendon in continuous motion (Fig. 1(a)).18
Fig. 1.
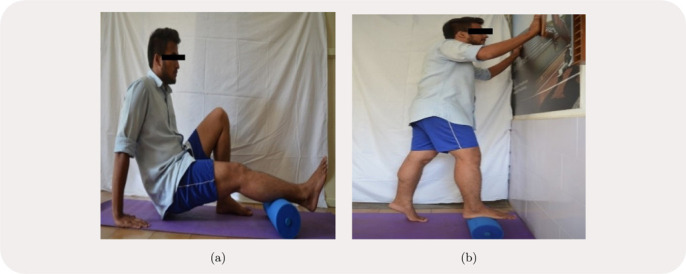
Foam rolling technique for (a) calf muscles and (b) plantar fascia.
Plantar fascia: This involved standing, with the non-affected foot on the floor and affected foot on the foam roller (Fig. 1(b)), the participants were instructed to move their foot back and forth from heel to toes in continuous motion while exerting pressure on the foam roller. They were asked to stop at the point where they felt maximum pain.18 Foam rolling was performed by the participants for 45 s followed by a 15-s rest with five repetitions.
Fig. 2.
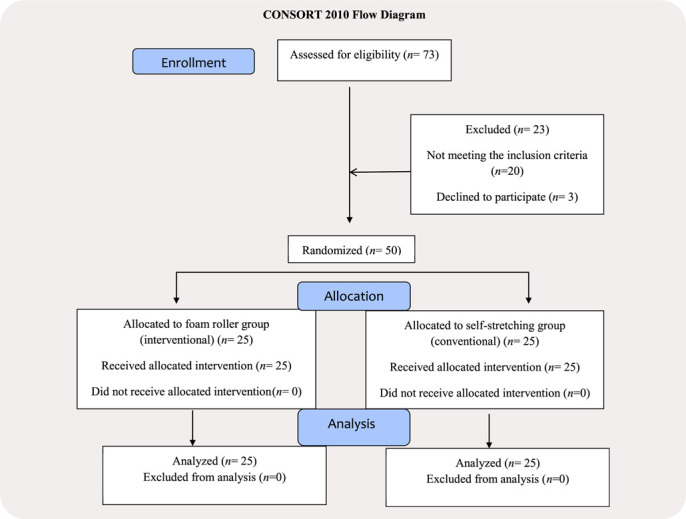
The CONSORT flow diagram.
Self-stretching group
Calf muscles: This involved standing, with the affected foot away from the wall, the participants were asked to lean forward until they felt a stretch in their calf. To focus on the stretching of soleus muscle, the affected knee was bent, whereas to focus on the gastrocnemius muscle, the affected knee was kept in full extension without lifting the heel.6
Plantar fascia: This involved sitting, with the participants crossing the affected foot over the contralateral thigh. They were asked to place fingers of one hand over the base of the toes and those of other hand on the heel and pull the toes back toward the shin, until they felt a stretch at plantar fascia. Participants were instructed to start gently initially and were made to work more aggressively as tolerable later.6 Each stretch was performed for 45 s with five repetitions.16
Statistical Analysis
Data was analyzed using IBM SPSS Statistics version 25.0 for Windows (IBM Corp., Armonk, NY). Level of significance was set at . Test used for the between-groups analysis for age was the Fisher exact test. To analyze gender and affected side, the Chi-square test was used. Independent sample -test was used to evaluate the mean difference between the two groups for all the outcome measures at baseline. For all the outcome measures, the within-group analysis was done using Student’s paired -test and the between-groups analysis by the Mann–Whitney -test.
Results
The CONSORT diagram (Fig. 2) shows the progress of participants at each stage of the study. Gender distributions of both the groups were statistically insignificant (). A total of 18 (72%) male and seven (28%) female participants were allocated in each group. The mean age of participants in the stretching group ( years) and in the foam roller group ( years) was found to be statistically insignificant (). Affected side of the leg in both groups was statistically insignificant (). Participants with right leg affected in the stretching group were 13 (52%) and in the foam roller group were 12 (48%). Participants with left leg affected in the stretching group were 12 (48%) and in the foam roller group were 13 (52%).
Groups were homogenous and not statistically significant in all the parameters except WBLT where the -value for between-groups was statistically significant (Table 1).
Table 1.
Outcome measures at baseline.
| Variable | Stretching () | Foam roller () | -Value |
|---|---|---|---|
| VAS (cm) | 0.754 | ||
| Gastrocnemius PPT (lb) | 0.171 | ||
| Soleus PPT (lb) | 0.521 | ||
| Plantar fasciitis (lb) | 0.307 | ||
| WBLT (cm) | 0.041* |
Notes: *Significant. VAS: visual analog scale and WBLT: weight-bearing lunge test.
After the analysis, it was found that within-group analysis showed a statistically significant difference () in all the outcome measures like VAS, gastrocnemius PPT, soleus PPT, plantar fascia PPT and WBLT in both the foam roller group and self-stretching group (Tables 2 and 3). The -values in these tables were adjusted by multiplying them by two.
Table 2.
Comparison of outcome measures within the stretching group (pre- and post-treatments).
| Stretching () | |||||
|---|---|---|---|---|---|
| Mean and SD | |||||
| Parameter | Pre-treatment | Post-treatment | Mean difference | Change (%) | -Value |
| VAS (cm) | 2.60 | 48.62 | 0* | ||
| Gastrocnemius PPT (lb) | 2.61 | 32.28 | 0* | ||
| Soleus PPT (lb) | 2.32 | 30.45 | 0* | ||
| Plantar fascia PPT (lb) | 3.23 | 42.65 | 0* | ||
| WBLT (cm) | 1.28 | 10.64 | 0* | ||
Notes: VAS: Visual analog scale, PPT: pressure pain threshold and WBLT: weight-bearing lunge test. The -value has been adjusted by multiplying it by 2. *Highly significant at .
Table 3.
Comparison of outcome measures within the foam roller group (pre- and post-treatments).
| Foam roller () | |||||
|---|---|---|---|---|---|
| Mean and SD | |||||
| Parameter | Pre-treatment | Post-treatment | Mean difference | Change (%) | -Value |
| VAS (cm) | 3.01 | 54.65 | 0* | ||
| Gastrocnemius PPT (lb) | 3.18 | 45.46 | 0* | ||
| Soleus PPT (lb) | 3.14 | 44.54 | 0* | ||
| Plantar fascia PPT (lb) | 3.12 | 45.70 | 0* | ||
| WBLT (cm) | 1.20 | 10.64 | 0* | ||
Notes: VAS: visual analog scale, PPT: pressure pain threshold and WBLT: weight-bearing lunge test. The -value has been adjusted by multiplying it by 2. *Highly significant at .
The between-groups analysis showed no statistical significance difference in VAS, plantar fascia PPT and WBLT (with -values of 0.171, 0.372 and 0.861, respectively), however, significant differences were found in gastrocnemius PPT () and soleus PPT () at end of the treatment (Table 4).
Table 4.
Comparison of outcomes between the groups.
| Parameters | Group | Mean difference | SD difference | Change (%) | Median | -Value | |
|---|---|---|---|---|---|---|---|
| VAS (cm) | Stretching | 25 | 2.60 | 1.02 | 48.62 | 2.60 | 0.171 |
| Foam roller | 25 | 3.01 | 1.15 | 54.65 | 2.90 | ||
| Gastrocnemius PPT (lb) | Stretching | 25 | 2.61 | 2.16 | 32.28 | 2.10 | 0.029* |
| Foam roller | 25 | 3.18 | 1.39 | 45.46 | 3.10 | ||
| Soleus PPT (lb) | Stretching | 25 | 2.32 | 1.86 | 30.45 | 1.80 | 0.013* |
| Foam roller | 25 | 3.14 | 1.73 | 44.54 | 3.20 | ||
| Plantar fascia PPT (lb) | Stretching | 25 | 3.23 | 2.21 | 42.65 | 2.20 | 0.372 |
| Foam roller | 25 | 3.18 | 2.75 | 45.70 | 3.60 | ||
| WBLT (cm) | Stretching | 25 | 1.28 | 0.54 | 13.17 | 1 | 0.861 |
| Foam roller | 25 | 1.20 | 0.65 | 10.64 | 1 |
Notes: *Significant.
Discussion
This study compares the immediate effects of foam rolling and stretching on patients with plantar fasciitis. This study showed statistically significant difference in reduction of pain intensity on VAS in the stretching group. Reduction in heel pain may be due to increase in muscle flexibility which causes biomechanical stress on fascia. This leads to increase in Golgi Tendon Organ (GTO) firing resulting in the inhibition of alpha motor neuron activity, thereby relaxing the muscle.22,23,24 At a microstructural level, failure of bonds between collagens reduces stiffness and pain at the musculotendinous unit altering its resting length.16,25,26 These findings are in line with studies which reported decrease in pain after stretching.10,27
In our study, we found significant improvement in PPT in the stretching group. The immediate improvement could be justified by the instantaneous rise in psychosomatic tolerance to discomfort and increase in the viscoelastic properties of the tissue.13 These findings are in line with previous studies which concluded that stretching has shown improvement in PPT scores when performed alone or given with other treatment.6,28
In this study, stretching showed an increase in the post-WBLT score which displayed statistical significance. This may be attributed to the viscoelastic properties of the musculotendinous unit to relax and lengthen. Muscular creep and reduced pain perception may be attributed to increase in tolerance to tissue stretch which contributes to immediate increase in ROM. These findings are in line with a study which reported increased ROM after stretching.28
In our study, foam rolling showed statistically significant difference in pain. These findings may be attributed to biomechanical, physiological and neurological mechanisms. Reduction in pain may be due to increased blood flow which removes waste products and due to activation of cutaneous receptors which blocks the nociceptive stimulus. Decreased cortisol levels and increased dopamine and serotonin levels have been reported to cause pain reduction after the soft tissue release. Foam rolling also causes decrease in tissue adhesion and muscle stiffness thereby causing an increase in soft tissue extensibility and muscle tendon compliance.29,30,31 This is consistent with the findings of previous studies which stated that foam rolling was effective in reducing either chronic pain (muscle tender spots) or latent myofascial trigger points.29,30,32
Foam rolling also showed statistically significant difference in the improvement of PPT. It may be due to activation of descending antinociceptive systems by stimulating the skin and muscle nociceptors.33,34 These findings were similar to previous studies which stated that foam rolling was effective in improving the plantar flexor and iliotibial band PPTs in healthy individuals.33,34
In our study, foam rolling technique has also shown to be effective in improving ROM and hence displaying an increased WBLT score. Possible mechanism for the increase in WBLT score may be change in thixotropic property of the fascia. Friction between foam roller and tissue causes warming effect on fascia, thereby breaking up some fibrous adhesions which results in restoration of soft tissue extensibility and flexibility.17 The normal movements may be interrupted due to the uninterrupted fascia being more viscous and solid in form. Back and forth movement of soft tissue on the foam roller causes overloading of cutaneous receptors by the direct and sweeping pressure. Thus, the friction generated between muscle, fascia and foam roller results in a stretch19,35 which possibly dampens the sensation of stretch end points. These findings were found to be in line with previous studies.17,34,35
Thus, both techniques were effective individually in decreasing pain and increasing the ROM. However, when we compared the effectiveness of both techniques, there was no statistically significant difference in improving any of the outcome measures except the PPTs for gastrocnemius and soleus, which showed statistically significant differences. The statistically significant differences in PPTs of gastrocnemius and soleus may be due to maximum pressure applied by the individuals using their limb weight. On the contrary, no difference in the PPT of plantar fascia may be attributed to inadequate pressure application by the participants and size as well as material of the foam roller.
Stretching and foam rolling have their own advantages and disadvantages. Static stretching does not require availability of specific tool for its application. Though static stretching helps in increasing the range of motion, as a standalone component of warm-up exercises it can be detrimental to strength and performance.36,37 Stretching of muscle before adequate warm-up may predispose muscle to tear and injury. Foam rolling requires availability of instrument and training for its use. Foam roller glides over the tissue and increases its temperature, hence can be used as a part of warm-up before the commencement of traditional rehabilitation. Hence, foam rolling and stretching may be used as an alternative or adjunct to each other in the clinical practice in patients with plantar fasciitis.
The main limitation of this study was the amount of pressure applied during foam rolling. It varied according to the participant’s body weight, ability to take weight on their upper limbs, participant’s tolerance of discomfort and knowledge about the use of foam roller. The second limitation was that the conventional treatments like strengthening or electrotherapy were not included.
Future Implications
Long-term study can be conducted to examine the effects of stretching and foam roller. Combined effect of foam rolling and stretching can be assessed.
Conclusion
We found that both stretching and foam rolling techniques helped in reducing pain and increasing the ROM. However, the effectiveness of foam rolling was superior to stretching in terms of increase in the PPTs at gastrocnemius and soleus.
Conflict of Interest
The authors have no conflict of interest relevant to this paper.
Funding/Support
This research did not receive any specific grant from funding agencies in the public, commercial or non-profit sectors.
Author Contributions
All authors contributed to the study design. Data was collected by Aishwarya R. Ranbhor. Data analysis, interpretation and writing of the manuscript was carried out by Aishwarya R. Ranbhor, Ashish J. Prabhakar and Charu Eapen.
References
- 1. McPoil TG, Martin RL, Cornwall MW, Wukich DK, Irrgang JJ, Godges JJ. Heel pain — Plantar fasciitis clinical practice guidelines linked to the international classification of function, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther 2008;38(4):A1–18. [DOI] [PubMed] [Google Scholar]
- 2. Lareau CR, Sawyer GA, Wang JH, DiGiovanni CW. Plantar and medial heel pain: Diagnosis and management. J Am Acad Orthop Surg 2014;22(6):372–80. [DOI] [PubMed] [Google Scholar]
- 3. Bartold SJ. The plantar fascia as a source of pain — biomechanics, presentation and treatment. J Bodyw Mov Ther 2004;8(3):214–26. [Google Scholar]
- 4. Morral A, Urrútia G, Gich I, Ruiz R, Bonfill X. Radial extracorporeal shock wave device appearance does not influence clinical outcomes: A randomized controlled trial. J Rehabil Med 2019;51(3):201–8. [DOI] [PubMed] [Google Scholar]
- 5. Bolívar YA, Munuera PV, Padillo JP. Relationship between tightness of the posterior muscles of the lower limb and plantar fasciitis. Foot Ankle Int 2013;34(1):42–8. [DOI] [PubMed] [Google Scholar]
- 6. Renan-Ordine R, Alburquerque-Sendín F, de Souza DPR, Cleland JA, Fernández-de-Las-Peñas C. Effectiveness of myofascial trigger point manual therapy combined with a self-stretching protocol for the management of plantar heel pain: A randomized controlled trial. J Orthop Sports Phys Ther 2011;41(2):43–50. [DOI] [PubMed] [Google Scholar]
- 7. D’Andréa Greve JM, Grecco MV, Santos-Silva PR. Comparison of radial shockwaves and conventional physiotherapy for treating plantar fasciitis. Clinics 2009;64(2):97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Osborne HR, Allison GT. Treatment of plantar fasciitis by LowDye taping and iontophoresis: Short term results of a double blinded, randomised, placebo controlled clinical trial of dexamethasone and acetic acid. Br J Sports Med 2006;40(6):545–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Porter D, Barrill E, Oneacre K, May BD. The effects of duration and frequency of Achilles tendon stretching on dorsiflexion and outcome in painful heel syndrome: A randomized, blinded, control study. Foot Ankle Int 2002;23(7):619–24. [DOI] [PubMed] [Google Scholar]
- 10. DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, Baumhauer JF. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain: A prospective, randomized study. J Bone Joint Surg Am 2003;85(7):1270–7. [DOI] [PubMed] [Google Scholar]
- 11. Ajimsha MS, Binsu D, Chithra S. Effectiveness of myofascial release in the management of plantar heel pain: A randomized controlled trial. Foot (Edinb) 2014;24(2):66–71. [DOI] [PubMed] [Google Scholar]
- 12. Yadav AO, Lakshmiprabha R. Comparison of the effects of therapeutic ultrasound v/s myofascial release technique in treatment of plantar fasciitis. Indian J Physiother Occup Ther 2012;6(2):13–6. [Google Scholar]
- 13. Hyland MR, Webber-Gaffney A, Cohen L, Lichtman PTSW. Randomized controlled trial of calcaneal taping, sham taping, and plantar fascia stretching for the short-term management of plantar heel pain. J Orthop Sports Phys Ther 2006;36(6):364–71. [DOI] [PubMed] [Google Scholar]
- 14. Turlik MA, Donatelli TJ, Veremis MG. A comparison of shoe inserts in relieving mechanical heel pain. Foot 1999;9(2):84–7. [Google Scholar]
- 15. Roos E, Engström M, Söderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int 2006;27:606–11. [DOI] [PubMed] [Google Scholar]
- 16. Colby LA, Kisner C, Rose J, Borstad J. The ankle and foot. In: Kisner C, Colby LA, eds. Therapeutic Exercise Foundation and Techniques. 6th ed. New Delhi, India: F. A. Davis Company/Jaypee Brothers Medical Publishers, 2012:868. [Google Scholar]
- 17. Couture G, Karlik D, Glass SC, Hatzel BM. The effect of foam rolling duration on hamstring range of motion. Open Orthop J 2015;9:450–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Škarabot J, Beardsley C, Štirn I. Comparing the effects of self- myofascial release with static stretching on ankle range-of-motion in adolescent. Int J Sports Phys Ther 2015;10:203–12. [PMC free article] [PubMed] [Google Scholar]
- 19. Griefahn A, Oehlmann J, Zalpour C, von Piekartz H. Do exercises with the Foam Roller have a short-term impact on the thoracolumbar fascia?: A randomized controlled trial. J Bodyw Mov Ther 2017;21(1):186–93. [DOI] [PubMed] [Google Scholar]
- 20. Chesterton LS, Sim J, Wright CC, Foster NE. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin J Pain 2007;23:760–6. [DOI] [PubMed] [Google Scholar]
- 21. Bennell K, Talbot R, Wajswelner H, Techovanich W, Kelly D, Hall AJ. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust J Physiother 1998;44(3):175–80. [DOI] [PubMed] [Google Scholar]
- 22. Engkananuwat P, Kanlayanaphotporn R, Purepong N. Effectiveness of the simultaneous stretching of the Achilles tendon and plantar fascia in individuals with plantar fasciitis. Foot Ankle Int 2018;39(1):75–82. [DOI] [PubMed] [Google Scholar]
- 23. Nishikawa Y, Aizawa J, Kanemura N, Takahashi T, Hosomi N, Maruyama H, Kimura H, Matsumoto M, Takayanagi K. Immediate effect of passive and active stretching on hamstrings flexibility: A single-blinded randomized control trial. J Phys Ther Sci 2015;27(10):3167–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sweeting D, Parish B, Hooper L, Chester R. The effectiveness of manual stretching in the treatment of plantar heel pain: A systematic review. J Foot Ankle Res 2011;4(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kay AD, Blazevich AJ. Effect of acute static stretch on maximal muscle performance: A systematic review. Med Sci Sports Exerc 2012;44(1):154–64. [DOI] [PubMed] [Google Scholar]
- 26. Phadke A, Bedekar N, Shyam A, Sancheti P. Effect of muscle energy technique and static stretching on pain and functional disability in patients with mechanical neck pain: A randomized controlled trial. Hong Kong Physiother J 2016;35:5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shivanna, Shankar G. Plantar fasciitis — Pain after stretching: An assessment study. Sch J Appl Med Sci 2014;2(6C):3015–9. [Google Scholar]
- 28. Hanney WJ, Puentedura EJ, Kolber MJ, Liu X, Pabian PS, Cheatham SW. The immediate effects of manual stretching and cervicothoracic junction manipulation on cervical range of motion and upper trapezius pressure pain thresholds. J Back Musculoskelet Rehabil 2017;30(5):1005–13. [DOI] [PubMed] [Google Scholar]
- 29. Cavanaugh MT, Döweling A, Young JD, Quigley PJ, Hodgson DD, Whitten JH, Reid JC, Aboodarda SJ, Behm DG. An acute session of roller massage prolongs voluntary torque development and diminishes evoked pain. Eur J Appl Physiol 2017;117(1):109–17. [DOI] [PubMed] [Google Scholar]
- 30. Wilke J, Vogt L, Banzer W. Immediate effects of self-myofascial release on latent trigger point sensitivity: A randomized, placebo-controlled trial. Biol Sport 2018;35(4):349–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med 2005;35(3):235–56. [DOI] [PubMed] [Google Scholar]
- 32. Rambhia I, Athavale N, Shyam A, Sancheti P. Immediate effect of foam rolling on pain and weight distribution in patients with plantar fasciitis: A pilot study. Int J Physiother Res 2018;6(2):2671–5. [Google Scholar]
- 33. Aboodarda SJ, Spence AJ, Button DC. Pain pressure threshold of a muscle tender spot increases following local and non-local rolling massage. BMC Musculoskelet Disord 2015;16(1):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vaughan B, McLaughlin P. Immediate changes in pressure pain threshold in the iliotibial band using a myofascial (foam) roller. Int J Ther Rehabil 2014;21(12):569–74. [Google Scholar]
- 35. Sullivan KM, Silvey DB, Button DC, Behm DG. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int J Sports Phys Ther 2013;8(3):228–36. [PMC free article] [PubMed] [Google Scholar]
- 36. Page P. Current concepts in muscle stretching for exercise and rehabilitation. Int J Sports Phys Ther 2012;7(1):109–19. [PMC free article] [PubMed] [Google Scholar]
- 37. Behm DG, Chaouachi A. A review of the acute effects of static and dynamic stretching on performance. Eur J Appl Physiol 2011;111(11):2633–51. [DOI] [PubMed] [Google Scholar]


