Abstract
Background:
Musculoskeletal pain (MSP) conditions are common in the educational leaning environment and are often associated with poor ergonomic conditions.
Objective:
This study investigated the prevalence, pattern and possible risk factors of MSP among undergraduate students of occupational therapy and physiotherapy in a South African university.
Methods:
A cross-sectional survey using an internet-based self-designed electronic questionnaire was used to obtain information about participants’ socio-demography, ergonomic hazards, MSP, and relevant personal information. Descriptive statistics, chi-square, and logistic regression were used in analyzing the data.
Results:
There were 145 participants (females 115 (79.3%); physiotherapy (74) 51.03%), making 36.7% of the present undergraduate student population in the two departments. The most prevalent ergonomic work hazards were prolonged sitting (71.7%) and repetitive movements (53.8%). The 12 months prevalence of MSP among the students was 89.7%. The pattern of MSP revealed that pain on the neck region was most prevalent (66.2%) followed by pain in the low back region (64.4%). Duration of daily travels and participation in regular exercise activities were significantly associated with the prevalence of MSP. Logistic model explained 23.6% of the variance in prevalence of MSP and correctly classified 94.1% of cases (, ). The right-handed students were 0.13 times more likely to present with MSP than left-handed students. Also, students who exercised regularly were 9.47 times less likely to present with MSP.
Conclusion:
MSP is highly prevalent among health science undergraduates and is significantly associated with sedentary postures and inadequacy in structured physical activity participation.
Keywords: Musculoskeletal pain, undergraduate student, occupational therapy, physiotherapy
Introduction
Musculoskeletal pain (MSP) is a known consequence of repetitive strain, overuse, and work-related musculoskeletal disorders and these injuries include a variety of disorders that cause pain in bones, joints, muscles, or surrounding structures.1 The pain can be acute or chronic, focal or diffuse. Low back pain is the most common example of MSP.2 Other examples include tendonitis and tendinosis, neuropathies, myalgia, and stress fractures.1 Acute MSP is the pain perceived within a region of the body and believed to arise from the muscles, ligaments, bones, or joints in that region, and these types of pain are named according to the region affected for example back pain, neck pain, shoulder pain, elbow pain, buttock pain, hip pain, knee pain, and ankle pain.3 Excluded from the definition is pain due to severe pathology, such as tumors, fractures, or infections, and systemic and neurological conditions. When MSP lasts longer than three months, generally, it is referred to as chronic pain. Three months is the standard period in which healing takes place. Chronic pain may be considered a disease state and may be associated with a disease or injury.4 Chronic pain may arise from psychological states, serve no biologic purpose, and have no recognizable endpoint.4
MSP conditions are common in the work environment and are often associated with poor ergonomic conditions at work.2 Poor ergonomic conditions exist when the work environment is incompatible with the workers’ bodies and their ability to continue work. Such conditions may cause discomfort, fatigue, pain, and subsequent injuries.5 Factors that occasion the incompatibility of the workplace and the worker are referred to as ergonomic work hazards.5 University students may be prone to acute or chronic MSP conditions because of their exposure to ergonomic hazards like prolonged sitting, prolonged grip, usage of aesthetic but less ergonomic footwear, and the increase in physical demands associated with learning professional skills. These are student-related factors that can be exacerbated by biological factors like the presence of endophenotypes, such as pain amplification and psychological distress.6 The trouble with persistent MSP is significantly crucial in young adults, making their lives more difficult and challenging.7 Studies in Malaysia,8 China,9 Australia,10 Saudi Arabia,11 India,12 Uttar,13 Pakistan,14 UAE,15 Ghana,16 Ethiopia,17 and Brazil18 have documented the pattern of MSP conditions among undergraduate university students.
Some researchers19,20,21 investigated musculoskeletal concerns and associated risk factors among South African students with a specific focus on postural and musculoskeletal concerns associated with laptop usage. Amongst practitioners in South Africa, research on work-related MSP was common from the discipline of dentistry.22,23,24,25,26 It would be essential to know the association amongst risk factors such as ergonomic challenges, family history of MSP, exercise and physical activity on the pattern and prevalence of MSP in a cohort of undergraduate students. Therefore, this study investigated the prevalence, pattern, and possible risk factors of MSP among undergraduate students of Occupational Therapy and Physiotherapy at the University of KwaZulu-Natal, Durban, South Africa.
Methods
This study is reported according to the Survey Reporting Guideline.27 The study was cross sectional, and involved a questionnaire completed by students. We chose to use a survey for this study to allow collection of data at a period when physical distancing was mandated as a public health measure. This study was reviewed and gained ethical approval by the humanities and social sciences research ethics committee of the University of KwaZulu-Natal, South Africa, with protocol reference number HSSREC/00001118/2020.
Questionnaire
An internet-based self-designed electronic questionnaire was used to obtain data on gender, age, marital status, year of study, course of study, duration of daily travel, duration of daily study/usage of laptop, duration of house chores performance, handedness, use of backpacks, participation in exercises/sports, family history of MSP, and smoking habits. The second segment of the questionnaire contained questions on the student’s perspective of their undergraduate course experience with a specific recall of existing ergonomic hazards such as prolonged sitting, lifting of heavy objects (see details in supplementary file). The third segment of the questionnaire included the first part of the standardized Nordic questionnaire.28,29 This was used to measure the presence and absence of MSP in various parts of the body.
Sample selection
The sample included undergraduate students in the discipline of Physiotherapy and Occupational therapy from the University of KwaZulu-Natal, South Africa. These students were selected as their training involved specific knowledge about “musculoskeletal conditions” and by implication these students should have better awareness of body postures and good motor control. The sample size was calculated using the one-sample dichotomous outcome formula.30 The authors used a small effect size of 0.24 based on an anticipated difference in the proportion of students reporting MSP at an alpha of 0.05 and power of 80% in a two-tailed test. It was necessary to involve at least 137 participants in this study. However, all students of physiotherapy and occupational therapy were invited to participate in the survey.
Survey administration
The survey was launched in April 2020 and closed to participants in May 2020. The primary mode of administration was online via SurveyMonkey (www.surveymonkey.com). The online link to the survey was sent via email and WhatsApp messenger to the participants through their departmental online fora. The participants were informed about the intent of the research and made aware of their right to withdraw, and that completion of the questionnaire was taken as consent for the anonymized data provided to be used in the research and dissemination. No financial incentives were provided. It took between 15 and 20 min to complete the survey.
Data analysis
Responses to the online survey became a valid response when a participant completed 70% of the questions in the survey alongside a final submission. The valid responses were transferred to SPSS version 21 for analysis. Frequency distributions and percentages were used in summarizing socio-demographic and individual characteristics of participants. Chi-square and -test were used in making inferences on the association between the 12-month prevalence of MSP and selected demographic/personal variables. Logistic regression analysis was used in determining the factors associated with the 12-month prevalence of MSP in this population.
Results
One hundred and forty-five undergraduate students of Physiotherapy and Occupational therapy participated in this study out of 394 undergraduate students who are currently enrolled in these disciplines resulting in a 36.7% response rate. Of the total participants, 115 (79.3%) were females, while 74 (51.03%) were students of physiotherapy (Table 1). The mean age of the participants was years with a range of 17–26 years. The most prevalent ergonomic work hazards were prolonged sitting (71.7%) and repetitive movements (53.8%) (Fig. 1) and 12-month prevalence of MSP among the students was 89.7% (Fig. 2). Pattern of MSP revealed that pain in the neck region was most prevalent (66.2%) followed by pain in the low back region (64.4%) among the students (Fig. 2). Extended duration of travel and participation in regular exercise activities were significantly associated with greater pain. Students who travelled for a period of more than one hour daily () and those who do not frequently exercise () were significantly more in reporting the presence of pain. None of the ergonomic work hazards evaluated was significantly associated with the presence of MSP (Table 2).
Table 1.
Demographic and personal characteristics of participants ().
| Variable | Characteristics | Frequency () | Percentage (%) |
|---|---|---|---|
| Gender | Male | 30 | 20.7 |
| Female | 115 | 79.3 | |
| Year of study | One | 42 | 28.7 |
| Two | 48 | 32.9 | |
| Three | 36 | 25.2 | |
| Four | 19 | 13.3 | |
| Marital status | Single | 144 | 99.3 |
| Married | 1 | 0.7 | |
| Course of study | Physiotherapy | 74 | 51.0 |
| Occupational therapy | 71 | 49.0 | |
| Handedness | Right | 132 | 91 |
| Left | 13 | 9 | |
| Smoker | Yes | 10 | 6.9 |
| No | 135 | 93.1 | |
| Family History of MSP | Yes | 73 | 50.3 |
| No | 72 | 49.7 | |
| Doing home chores | Yes | 137 | 94.5 |
| No | 8 | 5.5 | |
| Duration of daily personal study | 0–3 h | 78 | 53.8 |
| 4–6 h | 61 | 42.1 | |
| Greater than 7 h | 6 | 4.1 | |
| Duration of daily laptop usage | 0–3 h | 67 | 46.2 |
| 4–6 h | 62 | 42.8 | |
| Greater than 7 h | 16 | 11.0 | |
| Duration of daily travels | Less than 1 h | 95 | 65.5 |
| Greater than 1 h | 50 | 34.5 | |
| Usage of backpack | Yes | 108 | 74.6 |
| No | 37 | 25.4 | |
| Participating in regular exercises | Yes | 87 | 60.0 |
| No | 58 | 40.0 | |
| Participating in sports | Yes | 44 | 30.3 |
| No | 101 | 69.7 |
Fig. 1.
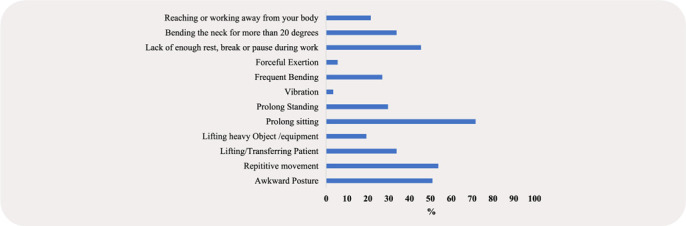
Prevalence of ergonomic hazards as reported by the students.
Fig. 2.
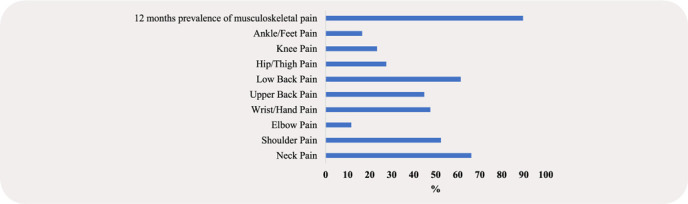
Pattern of MSP in the past 12 months.
Table 2.
Association between perceived ergonomic hazard/demographic/personal variables and the prevalence of MSP.
| Variable | Test statistics | -value |
|---|---|---|
| Awkward posture | 0.04a | 1.00 |
| Repetitive movement | 1.28a | 0.29 |
| Lifting/Transferring patient | 1.42a | 0.39 |
| Lifting heavy object/equipment | 1.72a | 0.30 |
| Prolong sitting | 1.13a | 0.36 |
| Prolong standing | 0.86a | 0.38 |
| Vibration | 0.59a | 1.00 |
| Frequent bending | 0.00a | 1.00 |
| Forceful exertion | 0.04a | 0.59 |
| Lack of enough rest, break, or pause during work | 1.00a | 0.42 |
| Bending the neck by more than 20∘ | 3.13a | 0.09 |
| Reaching or working away from your body | 0.64a | 0.53 |
| Gender | 0.36a | 0.51 |
| Course of study | 0.63a | 0.56 |
| Handedness | 2.49a | 0.14 |
| Year of study | 4.46a | 0.22 |
| Age | 0.19b | 0.84 |
| Usage of cigarette | 1.24a | 0.59 |
| Family history of MSP | 2.94a | 0.09 |
| Doing home chores | 0.04a | 0.59 |
| Duration of daily personal study | 0.87a | 0.65 |
| Duration of daily laptop usage | 0.77a | 0.68 |
| Duration of daily travels | 5.73a | 0.02* |
| Usage of backpack | 0.25a | 0.76 |
| Participating in regular exercises | 4.96a | 0.03* |
| Participating in sports | 2.11a | 0.23 |
Logistic regression was performed using a forward stepwise mode to ascertain the impact of variables (demographic, personal factors, and presence of ergonomic work hazard) on the likelihood that respondents will present with MSP (12-months prevalence of MSP). The model was statistically significant with , . The model explained 23.6% (Nagelkerke of the variance in the prevalence of MSP and correctly classified 94.1% of cases. Right-handed students were 0.13 times more likely to present with MSP than left-handed students. Also, students who exercised regularly were 9.47 times less likely to present with MSP (Table 3).
Table 3.
Factors associated with 12-months prevalence of MSP.
| Variable | Beta | Standard error | Wald | -value | Exp () | Lower CI | Upper CI |
|---|---|---|---|---|---|---|---|
| Constant | 2.11 | 1.15 | 3.39 | 0.066 | 0.12 | ||
| Handedness | 2.07 | 0.89 | 5.48 | 0.019 | 0.13 | 0.02 | 0.71 |
| Participating in regular exercise | 2.25 | 1.12 | 4.02 | 0.045 | 9.47 | 1.05 | 86.39 |
| Bending the neck by more than 20∘ | 1.99 | 1.12 | 3.17 | 0.075 | 0.14 | 0.015 | 1.22 |
Notes: Model Chi-square = 13.73; -value = 0.03; overall percentage predicted = 94.1%; Nagelkerke .
Discussion
Undergraduate rehabilitation students are exposed to several factors in their daily lives that may predispose them to MSP or trigger the occurrence of MSP. In this study, we investigated the presence of MSP in 145 occupational therapy and physiotherapy students at a university in South Africa.
In an academic environment, health science students (including first and second year rehabilitation students) remain seated for prolonged periods often with furniture that is not ergonomically maximized,17 they spend time in health institutions for clinical training, and perform professional activities which may be repetitive.18 With increasing pedagogies that include blended and digital learning, students spend an increased amount of time using their laptops and mobile phones to support their academic activities as well as for their leisure.19,20,21 It was therefore not surprising to note that prolonged sitting and repetitive movements emerged as the most prevalent ergonomic work hazards for students in this study and a high prevalence of MSP in the previous 12 months, especially in the neck region followed by pain in the lower back region. More than 60% of our participants are first and second year rehabilitation students who may have probably not learnt the principles of posture and motor control. This may also explain our observation.
Similar findings have emerged in other studies14,17,18,21,31,32,33 with university health science students. Xie and colleagues showcased the prevalence of musculoskeletal complaints among mobile device users in a systematic review of eight included studies.34 A wide range of prevalence rates of musculoskeletal complaints was reported with the highest prevalence commonly found in neck complaints. Rakhadani et al.21 in a study at the University of Venda, South Africa reported a high prevalence of musculoskeletal concerns among the students, which predominantly included the neck, shoulder, and wrist. This was attributed to prolonged computer use, incorrect sitting posture, and uncomfortable chairs. Long study hours and repetitive use of laptops were noted to increase MSP in the study by Hasan and colleagues.14 Yang et al.31 revealed that severe internet addiction resulted in a higher risk of MSP and Nordin et al.35 concluded that reduced physical fitness and prolonged sitting duration was associated with low back pain amongst health science undergraduates. Internet addiction is associated with adopting static postures for a protracted period usually prolonged sitting and this encourages a sedentary lifestyle resulting in low physical fitness. High prevalence of MSP has been consistently reported to be associated with prolonged static postures and sedentary lifestyle; this fact is corroborated by our present study.
In this study, students who exercised regularly more than nine times are less likely to present with MSP. Generally, engaging in moderate physical activity was associated with reduced risk of neck, shoulder, and low back pain among adolescents.36 Results of a meta-analysis in a systematic review reflected the protective effect of physical activity and reported a modest inverse association between leisure-time physical activity and onset of MSP.37 Since our participants were rehabilitation students knowledgeable about the benefit of physical activity, it is not unlikely that they engaged in safe, structured exercise. Engaging in structured physical exercise training has been shown to reduce or cure MSP.38 Kokic and colleagues’ study amongst physiotherapy and social science students revealed that lower levels of moderate intensity and total physical activity were associated with a higher prevalence of MSP in the previous year.32 However, higher levels of vigorous intensity and total physical activity were also associated with a higher prevalence of MSP, which prevented daily activities. In other studies,39,40 exercise was not associated with MSP. Again, it needs to be emphasized that only structured physical activities may be beneficial towards the reduction in the prevalence of MSP. It is also possible there is a U-shaped relationship between exercise and MSP — both too much and too little may be harmful.
Given that physical fitness and prolonged sitting is a modifiable risk factor, undergraduates should ensure frequent postural adjustments described as micropauses2 to minimize occurrences of MSP. Students should also be encouraged to embrace and sustain structured physical fitness and to integrate physical activity into daily routines whenever possible.
The duration of daily travel was significantly associated with MSP in this study. This is supported by a previous study that included medical students14 in which students who travelled more than one hour had a significant increase in MSP compared with non-medical students. There appears to be limited evidence that supports a causal relationship between the incidence of MSP and travelling. The statistical evidence for the association between prevalence of MSP and duration of daily travel in our study is biologically plausible as vehicular trips subject the body to static posture and prolong sitting which are confirmed ergonomic risk factors for the presence of MSP.2
There was a higher prevalence of MSP in females as compared to males in this study; however, this was not statistically significant. Several other studies reported greater MSP in female health science university students14,18,32 and attributed this finding to the difference in muscle, bone, mass, height, and joint structure of females as compared to males.41 The main factors that determine the presence of MSP in our study population were being right handed and not doing regular exercise. Hence, any student from this study population who is right handed and does no regular exercise has a 23.6% likelihood of presenting with MSP. This reveals that some other factors associated with the presence of MSP may have not been identified in our study.
The data from this study may be subject to recall bias as the respondents were expected to recall a discomfort which may not be present at the time of the survey. More importantly, the study was conducted when “social distancing” was adopted and students were mainly at home doing online classes and no practical sessions on campus. This can lead to systematic under-reporting or over-reporting of MSP. In order to have more accurate information on the incidence of MSP in this study population, a prospective cohort study would suffice. Also, the use of physical examination alongside self-reports will ensure the accuracy of prevalence rates obtained from a cross-sectional study like this. The recall error present in this study is clearly a random recall error as none of the participants has any reason to provide inaccurate information deliberately. A random recall error does not create a vital bias that will affect the reliability of the self-reports on MSP in our study population. Hence, the use of self-reports like this is necessary for the estimation of the burden of MSP among this sub-population when direct examinations are not possible.
Conclusion
The knowledge of MSP amongst rehabilitation students within their academic context, especially in occupational therapy and physiotherapy students, is essential in that the presence of pain may negatively influence their learning experiences and interfere with their ability to effectively execute the physical demands of being a student and student-practitioner. Moreover, given that this is the time in which their professional identities are developing, sensitization on how MSP and musculoskeletal disorders may affect their own lives is imperative. Investigating factors influencing student’s physical health may also assist in advocating health promotion initiatives at an administrative level and include work ergonomic hazards and programs for preventing MSP in students.
Conflict of Interest
The authors declare no competing interests.
Funding/Support
N/A.
Author Contributions
MOO, PG, and OOO designed the study and were the primary investigators. All authors drafted the initial manuscript, critically reviewed the manuscript for intellectual content, and subsequently revised the manuscript for publication. MOO, PG, and OOO read and approved the final version of the manuscript.
Acknowledgment
The authors would like to acknowledge the support given during data collection by the academic leaders of Occupational Therapy and Physiotherapy and their student representatives.
References
- 1. International Association for the Study of Pain. Musculoskeletal pain. 2009. Accessed on June 30, 2020. Available at http://www.aped-dor.org/images/FactSheets/DorMusculoEsqueletica/en/MusculoskeletalPain.pdf.
- 2. Ogunlana MO, Awobayo AO, Oyewole OO, Ayodeji AF. Work and musculoskeletal discomfort of Nigerian health workers: Pattern and predictors. Phys Ther Rev 2019;24(6):389–393, 10.1080/10833196.2019.1662208. [DOI] [Google Scholar]
- 3. International Association for the Study of Pain. Acute musculoskeletal pain. 2009. Accessed on June 30, 2020. Available at https://s3.amazonaws.com/rdcms-iasp/files/production/public/Content/ContentFolders/GlobalYearAgainstPain2/MusculoskeletalPainFactSheets/AcutePain_Final.pdf.
- 4. Grichnik KP, Ferrante FM. The difference between acute and chronic pain. Mt Sinai J Med N Y 1991;58(3):217–220. [PubMed] [Google Scholar]
- 5. Canadian Centre for Occupational Health and Safety. 2015 Catalogue. 2015. Accessed on June 30, 2020. Available at https://www.ccohs.ca/products/ pdf/PSCatalogue.pdf.
- 6. Gottesman II, Gould TD. The endophenotype concept in psychiatry: Etymology and strategic intentions. Am J Psychiatry 2003;160(4):636–645, 10.1176/appi.ajp.160.4.636. [DOI] [PubMed] [Google Scholar]
- 7. Slater H, Jordan JE, Chua J, Schütze R, Wark JD, Briggs AM. Young people’s experiences of persistent musculoskeletal pain, needs, gaps and perceptions about the role of digital technologies to support their co-care: A qualitative study. BMJ Open 2016;6(12):e014007. 10.1136/bmjopen-2016-014007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alshagga MA, Nimer AR, Yan LP, Ibrahim IAA, Al-Ghamdi SS, Radman Al-Dubai SA. Prevalence and factors associated with neck, shoulder and low back pains among medical students in a Malaysian Medical College. BMC Res Notes 2013;6:244. 10.1186/1756-0500-6-244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smith DR, Wei N, Ishitake T, Wang R-S. Musculoskeletal disorders among Chinese medical students. Kurume Med J 2005;52(4):139–146, 10.2739/kurumemedj.52.139. [DOI] [PubMed] [Google Scholar]
- 10. Smith DR, Leggat PA. Prevalence and distribution of musculoskeletal pain among Australian medical students. J Musculoskelet Pain 2007;15(4):39–46, 10.1300/J094v15n04_05. [DOI] [Google Scholar]
- 11. Gharib NM, Hamid NS. Prevalence of mechanical neck pain in Taif University female students: A survey study. J Am Sci 2013;9(6):347–354. [Google Scholar]
- 12. Aggarwal N, Anand T, Kishore J, Ingle GK. Low back pain and associated risk factors among undergraduate students of a medical college in Delhi. Educ Health Abingdon Engl 2013;26(2):103–108, 10.4103/1357-6283.120702. [DOI] [PubMed] [Google Scholar]
- 13. Yunn HT, Nadamurni NU, Wen PS. Prevalence and risk factors of neck pain among medical and health sciences undergraduate students in Universiti Tunku Abdul Rahman (Utar): A cross-sectional study. 2013. Accessed on June 30, 2020. Available at http://eprints.utar.edu.my/1709/1/UTAR_Final_Research_Project.pdf.
- 14. Hasan MM, Yaqoob U, Ali SS, Siddiqui AA. Frequency of musculoskeletal pain and associated factors among undergraduate students. Case Rep Clin Med 2018;7(2):131–145, 10.4236/crcm.2018.72011. [DOI] [Google Scholar]
- 15. Alhariri S, Ahmed A, Kalas A, et al. . Self-reported musculoskeletal disorders and their associated factors among university students in Ajman, UAE. Gulf Med J 2016;5(s2):S61–S70. [Google Scholar]
- 16. Abledu JK, Offei EB. Musculoskeletal disorders among first-year Ghanaian students in a nursing college. Afr Health Sci 2015;15(2):444–449, 10.4314/ahs.v15i2.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wami SD, Mekonnen TH, Yirdaw G, Abere G. Musculoskeletal problems and associated risk factors among health science students in Ethiopia: A cross-sectional study. J Public Health 2020. 10.1007/s10389-020-01201-6 [DOI] [Google Scholar]
- 18. Morais BX, Dalmolin G, de L, Andolhe R, Dullius AIDS, Rocha LP. Musculoskeletal pain in undergraduate health students: Prevalence and associated factors. Rev Esc Enferm U P 2019;53:e03444. 10.1590/S1980-220X2018014403444 [DOI] [PubMed] [Google Scholar]
- 19. Hough R, Nel M. Time and space dimensions of computer laptop use amongst third year students of the University of the Free State. South Afr J Occup Ther 2016;46(1):27–32, 10.17159/2310-3833/2016/v46n1a7. [DOI] [Google Scholar]
- 20. Hough PA, Nel M. Postural risks and musculoskeletal discomfort of three preferred positions during laptop use amongst students. South Afr J Occup Ther 2017;47(1):3–8, 10.17159/2310-3833/2017/v47n1a2. [DOI] [Google Scholar]
- 21. Rakhadani P, Goon D, Mandeya A. Musculoskeletal problems associated with university students computer users: A cross-sectional study. Online J Health Allied Sci 2017;16(2). Accessed on June 30, 2020. Available at https://www.ojhas.org/issue62/2017-2-7.html. [Google Scholar]
- 22. Booyens SJ, van Wyk PJ, Postma TC. Musculoskeletal disorders amongst practising South African oral hygienists. SADJ J South Afr Dent Assoc Tydskr Van Suid-Afr Tandheelkd Ver 2009;64(9):400–403. [PubMed] [Google Scholar]
- 23. Rambabu T, Suneetha K. Prevalence of work related musculoskeletal disorders among physicians, surgeons and dentists: A comparative study. Ann Med Health Sci Res 2014;4(4):578–582, 10.4103/2141-9248.139327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Botha PJ, Chikte U, Barrie R, Esterhuizen TM. Self-reported musculoskeletal pain among dentists in South Africa: A 12-month prevalence study. SADJ J South Afr Dent Assoc Tydskr Van Suid-Afr Tandheelkd Ver 2014;69(5):208, 210–213. [PubMed] [Google Scholar]
- 25. Ellapen TJ, Rugbeer N, Narsigan S, et al. . Incidence of work-related musculoskeletal pain among dentists in Kwa-Zulu Natal: Rehabilitation. Afr J Phys Health Educ Recreat Dance 2010;16(2):231–239. [Google Scholar]
- 26. Moodley R, Naidoo S. The prevalence of musculoskeletal disorders among dentists in KwaZulu-Natal. South Afr Dent J 2015;70(3):98–103. [Google Scholar]
- 27. Grimshaw J. SURGE (The SUrvey Reporting GuidelinE). In: Guidelines for Reporting Health Research: A User’s Manual. John Wiley & Sons, Ltd, 2014:206–213. Accessed on June 30, 2020. Available at https://www.researchgate.net/publication/315708041_SURGE_The_SUrvey_Reporting_ GuidelinE.
- 28. Kuorinka I, Jonsson B, Kilbom A, et al. . Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987;18(3):233–237, 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 29. Crawford JO. The Nordic musculoskeletal questionnaire. Occup Med 2007;57(4):300–301, 10.1093/occmed/kqm036. [DOI] [Google Scholar]
- 30. Sullivan L. Power and sample size determination. In: Essentials of Biostatistics in Public Health. Jones & Bartlett Learning, 2012:169–188. Accessed on June 30, 2020. Available at https://publish.jblearning.com/index.php?mod=jbbrowse&act= book_details&id=1054.
- 31. Yang Y, Yang M, Bai J, et al. . Validation of simplified Chinese version of the pain self-efficacy questionnaire (SC-PSEQ) and SC-PSEQ-2 for patients with nonspecific low back pain in mainland China. Spine 2019;44(20):E1219–E1226, 10.1097/BRS.0000000000003099. [DOI] [PubMed] [Google Scholar]
- 32. Kokic IS, Znika M, Brumnic V. Physical activity, health-related quality of life and musculoskeletal pain among students of physiotherapy and social sciences in Eastern Croatia - Cross-sectional survey. Ann Agric Environ Med AAEM 2019;26(1):182–190, 10.26444/aaem/102723. [DOI] [PubMed] [Google Scholar]
- 33. Reuter PR, Fichthorn KR. Prevalence of generalized joint hypermobility, musculoskeletal injuries, and chronic musculoskeletal pain among American university students. PeerJ 2019;7:e7625. 10.7717/peerj.7625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Xie Y, Szeto G, Dai J. Prevalence and risk factors associated with musculoskeletal complaints among users of mobile handheld devices: A systematic review. Appl Ergon 2017;59(Pt A):132–142, 10.1016/j.apergo.2016.08.020. [DOI] [PubMed] [Google Scholar]
- 35. Nordin NAM, Singh DKA, Kanglun L. Low back pain and associated risk factors among health science undergraduates. Sains Malays 2014;43(3):423–428. [Google Scholar]
- 36. Guddal MH, Stensland SØ, Småstuen MC, Johnsen MB, Zwart J-A, Storheim K. Physical activity level and sport participation in relation to musculoskeletal pain in a population-based study of adolescents. Orthop J Sports Med 2017;5(1). 10.1177/2325967116685543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Shiri R, Falah-Hassani K, Viikari-Juntura E, Coggon D. Leisure-time physical activity and sciatica: A systematic review and meta-analysis. Eur J Pain Lond Engl 2016;20(10):1563–1572, 10.1002/ejp.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Søgaard K, Sjøgaard G. Physical activity as cause and cure of muscular pain: Evidence of underlying mechanisms. Exerc Sport Sci Rev 2017;45(3):136–145, 10.1249/JES.0000000000000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Almhdawi KA, Mathiowetz V, Al-Hourani Z, Khader Y, Kanaan SF, Alhasan M. Musculoskeletal pain symptoms among allied health professions’ students: Prevalence rates and associated factors. J Back Musculoskelet Rehabil 2017;30(6):1291–1301, 10.3233/BMR-169669. [DOI] [PubMed] [Google Scholar]
- 40. Algarni AD, Al-Saran Y, Al-Moawi A, Bin Dous A, Al-Ahaideb A, Kachanathu SJ. The prevalence of and factors associated with neck, shoulder, and low-back pains among medical students at University Hospitals in Central Saudi Arabia. Pain Res Treat 2017;2017:1235706. 10.1155/2017/1235706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. de Sousa Paixão M, Miranda Tassitano R, Rocha de Siqueira G. Prevalência de desconforto osteomuscular e fatores associados em estudantes universitários. Rev Bras Em Promoção Saúde 2013;26(2):242–250, 10.5020/18061230.2013.p242 (in Portuguese). [DOI] [Google Scholar]


