INTRODUCTION
Acute Myeloid Leukemia (AML) is a rare childhood cancer that classically presents with fevers, bruising and bleeding, lymphadenopathy, hepatosplenomegaly, and cytopenias.1 Intracranial hypertension has been reported as a sign of central nervous system (CNS) relapse or an adverse effect of treatment in pediatric acute promyelocytic leukemia (AML-M3) patients. AML rarely presents initially with increased intracranial pressure as described in this case review.
We report the case of a 12-year-old male who presented with complaints of gradual vision changes consistent with idiopathic intracranial hypertension (IIH) months prior to a diagnosis of AML. IIH is defined as increased intracranial pressure in the absence of a space-occupying lesion, enlargement of ventricles, or loss of consciousness. It classically presents with headaches, vision changes, cognitive impairment, and papilledema. However, this case suggested a further hematological workup for children with IIH may be necessary.
CASE REPORT
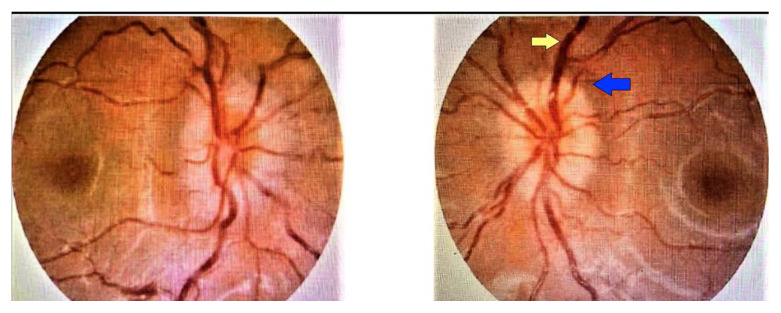
A 12-year-old boy without any significant past medical history was referred to an ophthalmologist for further evaluation of worsening headaches and papilledema. Papilledema was first detected during a vision exam for a new prescription of glasses by an optometrist. The ophthalmologic evaluation revealed diffuse increased nerve fiber layer and scattered defects with enlarged scotoma bilaterally. Fundus photos showed blurred margins bilaterally with vascular tortuosity and venous congestion (Figure 1). These signs of increased intracranial pressure led to a referral for admission to the pediatric hospital medicine service for further workup and management.
Figure 1.
Fundus showed blurred margins bilaterally (blue arrow) with vascular tortuosity (yellow arrow) and venous congestion.
The patient reported no neck stiffness, photophobia, fever, or altered mental state on admission to the pediatric hospital medicine service. His headaches were described as progressive over the six months before admission and episodic without any known aggravating factors. They were mild in intensity (the patient self-scored a three on a numeric pain rating scale of 0–10). He did not require over-the-counter medications for pain relief. His mother reported no family history of any medical conditions.
Medical history revealed an optometrist had suspected papilledema on physical exam as early as nine months before presentation. The patient had severely decreased visual acuity (3/20) in the left eye since birth and normal visual acuity (20/20) in the right eye. General physical examination was unremarkable. He had no weakness, balance, seizure, or hearing problems. The physical exam also did not reveal lymphadenopathy, hepatosplenomegaly, bruising, bleeding, or petechiae. The patient’s mother noted that he had gained 30 pounds since last year. His antenatal and postnatal histories were insignificant.
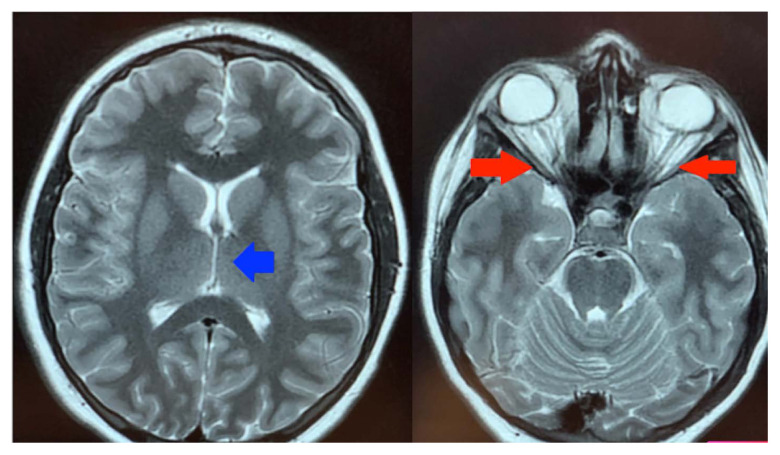
Magnetic resonance imaging (MRI) findings showed distention of optic nerve sheaths with flattening of posterior globes and pituitary gland. The ventricular system appeared slit-like. There were no space-occupying lesions or masses. These findings were highly suggestive of idiopathic intracranial hypertension (Figure 2). Lumbar puncture yielded an opening pressure of 38 cm H2O. Despite the removal of 12 ml cerebrospinal fluid (CSF), the closing pressure remained high (33 cm H2O). The patient was started on acetazolamide 250 mg orally twice daily. Incidentally, admission complete blood count (CBC) showed low hemoglobin of 10.7 gm/dL, mean corpuscular volume was 98 fL, platelet count was 93 x 103/μL, and an elevated white blood cell (WBC) count of 28 x 103/μL. Due to leukocytosis with bicytopenia (anemia and thrombocytopenia), a CBC was repeated and showed increased leukocytosis with a WBC count of 49 x 103/μL with 59% blast cells.
Figure 2.
MRI found distention of optic nerve sheaths (Right figure; red arrow) with flattening of posterior globes and pituitary gland. The blue arrow on the left figure indicates slit like ventricles of IIH.
In contrast, cytology of CSF showed normal lymphocyte count with scattered monocytes, erythrocytes, a few neutrophils, eosinophils, and small numbers of blast cells (< 5%). Peripheral smear showed numerous blasts, and flow cytometry confirmed acute myeloid leukemia (AML). Bone marrow aspirate demonstrated that the patient had acute myeloid leukemia with minimal differentiation (AML-M0). A double-lumen port was placed in the operating room along with bone marrow biopsy and lumbar puncture with concurrent intrathecal cytarabine administration. He was transferred to the pediatric intensive care unit, where chemotherapy was started as per Children’s Oncology Group protocol (AAML0531).
DISCUSSION
Idiopathic intracranial hypertension (IIH) characterizes increased intracranial pressure in the absence of a space-occupying lesion, enlargement of ventricles, or loss of consciousness.2,3 IIH presents with nonspecific symptoms, including headache, visual loss, and papilledema. If not diagnosed and managed timely, it may result in permanent loss of vision, chronic headaches, and other neurological impairment. IIH is a diagnosis of exclusion and follows these Modified Dandy Criteria for IIH (Table 1).4 Criteria include CSF pressure greater than 25 cm H2O, the standard composition of cerebrospinal fluid, and the absence of any structural, anatomic, or vascular lesions that may cause increased intracranial pressure.5
Table 1.
Modified Dandy Criteria for IIH.4
|
The pathophysiology of IIH remains uncertain. Hypotheses suggest etiologies related to CSF’s overproduction, under-absorption of CSF, resistance to the outflow of CSF, or vascular congestion.6–8 Risk factors for IIH include obesity, certain medications, excess vitamin A, severe anemia, coagulopathies, and Addison’s disease.
AML is a malignancy that causes an increase in the number of myeloid cells of the bone marrow, their maturation arrest, and resulting hematopoietic insufficiency (granulocytopenia, thrombocytopenia, or anemia).9 It may be accompanied by leukocytosis. AML often presents with signs of bone marrow abnormalities such as anemia, thrombocytopenia, and low or elevated white blood cells. Common symptoms include fatigue, bruising, bleeding, petechiae, and weight loss. Leukemia also can present initially with ocular manifestation attributed to neoplastic cells directly infiltrating the CNS.
AML presenting with isolated intracranial hypertension is extremely rare. Intracranial hypertension has been reported with CNS relapse of AML and a side effect of treatment of AML variants with all-trans retinoic acid. No case has been reported with AML initially presenting as IIH with papilledema.2,10 Awareness of these ophthalmic manifestations should prompt further laboratory evaluation if no other causes are found and the working diagnosis is IIH.
The exact mechanism behind AML induced IIH has not been well established. To understand the relationship better, it is useful to know the varying mechanisms of IIH. One hypothesis to understand IIH is that increased viscosity resulting from lymphocytosis can lead to reduced CSF absorption.11,12 This could be a likely cause in our patient as he had an elevated systemic WBC count. It also has been speculated that blasts cells can infiltrate the arachnoid granulations directly and alter CSF absorption.13 Still, no such findings were seen on MRI in our case. Overcirculation of blood through the choroid plexus in cases of isolated anemia (due to high cardiac output secondary to anemia) can cause cerebrospinal fluid (CSF) overproduction. Anemia also may cause relative cerebral hypoxia activating autoregulatory mechanisms causing cerebral over circulation that may elevate intracranial pressure. Raised intracranial pressure causes increased optic nerve sheath pressure, leading to elevated ophthalmic venous pressure and reduced central retinal venous outflow and capillary perfusion.14,15
CONCLUSIONS
AML presenting with intracranial hypertension is rare, but this case demonstrated the possibility. This critical case was presented to broaden clinicians’ differential when a child presents with intracranial hypertension and gradual vision changes. Early detection of papilledema/ IIH without a reasonable explanation warrants further workup with a complete blood count with differential, MRI followed by CSF studies including a cell count, pathology review, and flow cytometry to evaluate for leukemic infiltration. Due to the paucity of information regarding pediatric AML and the association of IIH, further investigation is warranted. A retrospective analysis from large clinical trials in the Children’s Oncology Group may be warranted to evaluate the incidence of intracranial hypertension in children that present with newly diagnosed AML. Both scientific and clinical studies are imperative to define the underlying mechanisms and enhance our ability to evaluate and treat similar patients effectively in the future.
REFERENCES
- 1.Gibson BES, Wheatley K, Hann IM, et al. Treatment strategy and long-term results in paediatric patients treated in consecutive UK AML trials. Leukemia. 2005;19(12):2130–2138. doi: 10.1038/sj.leu.2403924. [DOI] [PubMed] [Google Scholar]
- 2.Lipton J, Joffe S, Ullrich NJ. CNS relapse of acute myelogenous leukemia masquerading as pseudotumor cerebri. Pediatr Neurol. 2008;39(5):355–357. doi: 10.1016/j.pediatrneurol.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 3.Mercille G, Ospina LH. Pediatric idiopathic intracranial hypertension: A review. Pediatr Rev. 2007;28(11):77–86. doi: 10.1542/pir.28-11-e77. [DOI] [PubMed] [Google Scholar]
- 4.Smith JL. Whence pseudotumor cerebri? J Clin Neuroophthalmol. 1985;5(1):55–56. [PubMed] [Google Scholar]
- 5.Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59(10):1492–1495. doi: 10.1212/01.wnl.0000029570.69134.1b. [DOI] [PubMed] [Google Scholar]
- 6.Kesler A, Goldhammer Y, Hadayer A, Pianka P. The outcome of pseudotumor cerebri induced by tetracycline therapy. Acta Neurol Scand. 2004;110(6):408–411. doi: 10.1111/j.1600-0404.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 7.Warner JE, Larson AJ, Bhosale P, et al. Retinol-binding protein and retinol analysis in cerebrospinal fluid and serum of patients with and without idiopathic intracranial hypertension. J Neuroophthal. 2007;27(4):258–262. doi: 10.1097/WNO.0b013e31815b9af0. [DOI] [PubMed] [Google Scholar]
- 8.Deonna T, Guignard JP. Acute intracranial hypertension after nalidixic acid administration. Arch Dis Child. 1974;49(9):743. doi: 10.1136/adc.49.9.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Kouchkovsky I, Abdul-Hay M. Acute myeloid leukemia: A comprehensive review and 2016 update. Blood Cancer J. 2016;6(7):e441. doi: 10.1038/bcj.2016.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holmes D, Vishnu P, Dorer RK, Aboulafia DM. All-trans retinoic acid-induced pseudotumor cerebri during induction therapy for acute promyelocytic leukemia: A case report and literature review. Case Rep Oncol Med. 2012;2012:313057. doi: 10.1155/2012/313057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guymer RH, Cairns JD, O’Day J. Benign intracranial hypertension in chronic myeloid leukemia. Aust N Z J Ophthalmol. 1993;21(3):181–185. [PubMed] [Google Scholar]
- 12.Nguyen HS, Haider KM, Ackerman LL. Unusual causes of papilledema: Two illustrative cases. Surg Neurol Int. 2013;4:60. doi: 10.4103/2152-7806.110686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carr F, Tan K, Stevenson W, Ahmad K. A case of acute myeloid leukemia presenting as subacute intracranial hypertension in a young adult. Neuroophthalmology. 2018;43(5):313, 317. doi: 10.1080/01658107.2018.1508303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berk J, Hall D, Stroh I, et al. A child with pancytopenia and optic disc swelling. Pediatrics. 2019;144(5) doi: 10.1542/peds.2018-2887. pii:e20182887. [DOI] [PubMed] [Google Scholar]
- 15.Hayreh SS, Edwards J. Ophthalmic arterial and venous pressures. Effects of acute intracranial hypertension. Br J Ophthalmol. 1971;55(10):649–663. doi: 10.1136/bjo.55.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]