Abstract
Summary: Fenestration of the cervical segment of the internal carotid artery (ICA) is considered an extremely rare anatomic variant, with, to the best of our knowledge, only four cases reported in the literature. We report six angiographic observations of apparent fenestration of the cervical ICA, which we believe are secondary to arterial dissection. We discuss the angiographic appearance of these pseudofenestrations and their potential clinical implications.
A sound knowledge of the vascular anatomy of the nervous system is essential for the correct interpretation of cerebrovascular imaging studies. In particular, one must be able to discern actual pathologic conditions from anatomic variants simulating a disease and potentially leading to unwarranted therapeutic measures. It is therefore not surprising that a vast amount of the neuroradiologic literature has classically been devoted to the description of anatomic pitfalls. A reverse situation, in which a pathologic process takes the appearance of an anatomic variant is, on the other hand, rarely encountered or described.
Fenestration, or duplication, of the cervical segment of the internal carotid artery (ICA) is considered an extremely rare anatomic variant (1–6). To the best of our knowledge, only four cases of “true” cervical ICA fenestration, as opposed to ICA duplication, have been reported in the literature (2, 5, 6). We report six angiographic observations of apparent fenestration of the cervical ICA, which we believe are secondary to arterial dissection. We discuss the angiographic appearance of these pseudofenestrations and their potential clinical implications.
Case Reports
Case 1
A 59-year-old woman was admitted for subarachnoid hemorrhage documented by CT. Four-vessel angiography was performed. Smooth tapering of the proximal right ICA was observed, leading to a critical stenosis approximately 2 cm above the bifurcation. Marginal residual flow was detected up to the level of the intracranial ICA, with opacification the ophthalmic artery. The angiographic diagnosis of dissection was made. In addition, a 2.5–3.0-cm-long fenestration was seen in the cervical segment of the left ICA (Fig 1). One of the limbs of the fenestration was slightly irregular. No other cervicocranial anomaly was noted.
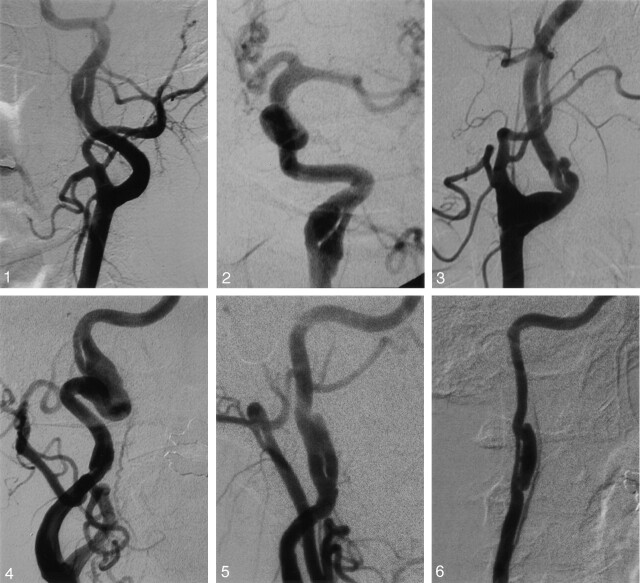
Fig 1.
Case 1, a 59-year-old woman with a left ICA fenestration. DSA, left common carotid injection, oblique view. One limb of the fenestration shows a slight fusiform enlargement.
Fig 2. Case 2, a 52-year-old man with a left ICA fenestration. DSA, left common carotid injection, oblique view. Both limbs of the fenestrated segment show an irregular appearance with fusiform dilatation. Note also the dilatation of the terminal ICA.
Fig 3. Case 3, a 51-year-old woman with a left ICA fenestration. DSA, left common carotid injection, lateral view. Fenestration of the left ICA immediately above the carotid bulb, associated with a proximal kink. Note the irregular appearance of one of the fenestration limbs, with a small distal pseudoaneurysm. The location of the fenestration suggests a possible iatrogenic event during a previous selective ICA angiogram, which remained unconfirmed in view of absent documentation.
Fig 4. Case 4, a 74-year-old man with a right ICA fenestration. DSA, right common carotid injection, oblique view. Fenestration of the distal cervical ICA immediately below the skull base, with a very irregular, enlarged limb that suggested a fusiform ICA aneurysm at MR imaging. Note that the anomaly occurs in a sinuous segment of the ICA (ICA “coiling”).
Fig 5. Case 5, a 41-year-old woman with a right ICA fenestration. DSA, right common carotid injection, oblique view. The two limbs of the fenestration have a slightly irregular contour. One of the limbs shows, after reconnecting to the main lumen, an upward-directed pseudoaneurysmal expansion.
Fig 6. Case 6, a 46-year-old woman with right ICA fenestration. DSA, right common carotid injection, oblique view. Fenestrated segment of the right ICA with marked irregularity of its two limbs. One limb, reduced in caliber, is aligned with the ICA and most likely represents the original ICA lumen. The other limb is excentric and enlarged. It shows, besides the proximal and distal connections to the main lumen, two additional bridges joining the other limb of the fenestration. As an anatomic variant, note the origin of the right ascending pharyngeal artery from the ICA.
Case 2
A 52-year-old man was investigated for a thalamic pain syndrome secondary to a left basal ganglia hemorrhage. MR imaging suggested a left thalamic vascular anomaly, and the patient was referred for angiographic evaluation. Digital subtraction angiography (DSA) showed a developmental venous anomaly (DVA, or venous angioma) in the left basal ganglia region. In addition, anomalies were incidentally noticed in both cervical ICAs. The lesion appeared, on the right side, as a pseudoaneurysm located immediately below the skull base. The left-side anomaly consisted of a fenestration of the distal cervical ICA (Fig 2). One limb of the fenestration was markedly irregular. The diagnosis of bilateral cervical ICA dissection was made.
Case 3
A 51-year-old woman was admitted to another institution for an episode of nausea and vomiting rapidly followed by a right homonymous hemianopsia. MR imaging demonstrated acute infarcts in the left cerebellum and left occipital pole, and DSA revealed a dissection of the left vertebral artery (V4 segment). A left ICA aneurysm (clinoid segment) was incidentally discovered. Although selective catheterization of both ICAs was performed, the carotid bifurcations were not imaged. The patient was later referred to our institution for further evaluation and management of the intracranial aneurysm. A new angiogram obtained 15 months after initial presentation confirmed the left clinoid ICA aneurysm as well as an abnormal left V4 segment compatible with the previous dissection. The left carotid studies revealed a fenestration of the cervical ICA immediately distal to the carotid bifurcation (Fig 3). One limb of the fenestration was associated with a small pseudoaneurysm. Finally, the cervical (V2) segment of the right vertebral artery showed diffuse contour irregularities and a small pseudoaneurysm suggesting an arterial dissection in a context of fibromuscular dysplasia (FMD).
Case 4
A 74-year-old man was evaluated for multiple right hemispheric transient ischemic attacks occurring 10 days after aortic valve replacement. Brain MR imaging showed no evidence of acute ischemic lesion, and the patient was placed on anticoagulation therapy. A fusiform aneurysm of the cervical right ICAwas suspected on the basis of MR angiography findings, prompting the performance of DSA. The right carotid studies revealed a sinuous right cervical ICA (“coiling”) with a fenestration immediately above it (Fig 4). The fenestrated segment was irregular. One of its limbs, being significantly enlarged, was responsible for the fusiform appearance at MR angiography. In addition, contour changes consistent with FMD were seen in the left vertebral artery.
Case 5
A 41-year-old woman with a history of migraine consulted for a newly appearing “whooshing” sound in her left cervical region, accompanied by diaphoresis. Results of her neurologic examination were unremarkable. Brain MR imaging results were normal, but MR angiography revealed bilateral cervical ICA changes consistent with FMD. An ICA fenestration possibly associated with a pseudoaneurysm was visible on the right side. DSA confirmed the diagnosis of right ICA dissection, in which a circulating false lumen was connected to the true lumen before ending blindly in an upward-directed pseudoaneurysm (Fig 5).
Case 6
A 46-year-old woman suffered a right motor strip infarct as a consequence of a severe head trauma during a traffic accident. A follow-up MR study performed 6 months later raised the suspicion of bilateral ICA dissection. DSA confirmed the diagnosis of bilateral ICA dissection with associated pseudoaneurysms. On the right side, the abnormal arterial segment took the appearance of a fenestration with asymmetric arterial limbs, most likely representing a narrowed true lumen and an enlarged, pseudoaneurysmal false lumen (Fig 6).
Discussion
Two types of cervical ICA fenestration are reported in the literature (Table 1). The first type involves the entire cervical segment, from the carotid bifurcation up to the skull base (1, 3, 4). This type, more adequately labeled as cervical ICA duplication, is similar in nature to an aberrant ICA—that is, a variant in which the ascending pharyngeal artery keeps a large connection with the petrous ICA via tympanic anastomoses (4). An aberrant ICA is a rare anatomic variant usually associated with segmental agenesis of the true cervical ICA. In this instance, the aberrant ICA provides collateral flow to the ipsilateral anterior circulation. In exceptional situations, an aberrant ICA occurring with a true cervical ICA results in an apparent ICA duplication (4). This variant, however, has a clear embryologic explanation and bears no relationship to the “true” cervical fenestrations considered in this report.
TABLE 1:
Previously published cases of extracranial internal carotid artery (ICA) fenestration or duplication
| Type | Level | Comment | Reference |
|---|---|---|---|
| 1. Duplication | Complete ICA | Aberrant ICA type | Killien et al., 1980 |
| 2. Fenestration | C2 | Angiographic signs of dissection | Tanaka et al., 1982 |
| 3. Fenestration | C1–C2 | Angiographic signs of dissection | Hasegawa et al., 1985 |
| 4. Fenestration | C1–C2 | Angiographic signs of dissection | Hasegawa et al., 1985 |
| 5. Fenestration | C1–C2 | Angiographic signs of dissection | Nakamura et al., 1993 |
| 6. Duplication | Complete ICA | Aberrant ICA type | Chess et al., 1995 |
| 7. Duplication | Complete ICA | Aberrant ICA type | Koenigsberg et al., 1995 |
The second type of cervical ICA fenestration, or “true” fenestration, is of extremely rare occurrence, with only four cases reported in the literature so far (2, 5, 6). (A second report by Hasegawa et al [7] is not included, because it describes the cases reported in reference 2). This second type of fenestration, which appears as a short arterial segment with two patent lumens, corresponds to the classic definition of a fenestration. The six cases we report herein are of this type, but show as additional common characteristics contour irregularities and size assymetry of the limbs of the fenestration. These vessel wall anomalies ranged from mild ectasia (case 1) to frank pseudoaneurysmal dilatation falsely suggesting a fusiform aneurysm at MR imaging (case 4). These changes, not typically observed in fenestrations of other topographic locations are, on the other hand, commonly associated with arterial dissection. Four of our patients had a clinical history and/or angiographic changes consistent with the diagnosis of arterial dissection in vessels other that the fenestrated ICA (contralateral ICA in cases 1, 2, and 6, vertebral artery in case 4). Three had angiographic signs of fibromuscular dysplasia (cases 3, 4 and 5), a disease with a well-documented association with arterial dissection (8, 9). In four patients, the fenestration was found immediately below the skull base, at the entrance of the carotid canal. This is a typical location for traumatic cervical ICA dissection. The fenestration in one patient was just distal to the carotid bifurcation, a level potentially associated with iatrogenic dissections. This patient underwent previous angiography at another institution with selective ICA catheterization. No images of the carotid bifurcation were provided, however, making it impossible to know whether the fenestrated segment predated the angiogram. An iatrogenic dissection occurring at the time of catheterization can thus not be formally excluded in this case.
Embryologic mechanisms have been proposed for fenestrations involving other cervicocranial vessels. For example, a basilar artery fenestration results from segmental nonfusion of its embryonic precursors (10), a distal vertebral artery fenestration has been linked to passage of the hypoglossal nerve through the fenestrated segment (11), whereas angiographic data suggest that early branching temporopolar arteries may be involved in the formation of MCA fenestrations by interfering with the fusion of embryonic precursors (12). There is, on the other hand, no clear embryologic mechanism that would explain the occurrence of a cervical ICA fenestration.
Careful review of the four cases of cervical ICA fenestration previously reported in the literature revealed interesting findings. In each case, the angiographic documentation shows, at the level of the fenestration, anomalies commonly associated with arterial dissection, such as segmental narrowing or enlargement, the latter taking in one case a pseudoaneurysmal appearance (second case of Hasegawa et al). These changes were mentioned by Hasegawa et al (2), the vessel being described as “markedly elongated and dilated in caliber” (case 1) or “dilated in caliber” (case 2). Of equal interest is the occurrence, in the case reported by Nakamura et al (5), of an acute stroke in the carotid distribution ipsilateral to the fenestration. In this case (as in our case 3), the fenestration was adjacent to a carotid loop (coiling), an anatomic configuration shown to predispose to arterial dissection (13, 14). Nakamura et al concluded that, in their patient, the stroke was secondary to a “thrombus or embolus from the fenestration” (5). In none of these published cases of cervical ICA fenestration was the possibility of a dissection with a double lumen considered.
It is possible to hypothesize that a fenestration of the cervical ICA would itself be an anatomic variant predisposing to arterial dissection. In such a case, however, the constant association observed between the fenestrations and signs of arterial dissection (documented in our six cases and suspected in the four cases reported in the literature, as discussed above) would be difficult to explain, as would be the absence of reported cases of fenestration without these associated abnormalities. We therefore think that our six cases, as well as the four cases previously reported in the literature, consist in the sequellae of a pathologic condition—that is, a segmental arterial dissection with a double lumen sign, rather than a congenital anatomic variant.
Conclusion
A fenestration of the cervical segment of the ICA is a rarely documented anatomic variant. We report six observations of cervical ICA fenestrations appearing as short vascular segments with two parallel arterial lumens. Factors such as the angiographic characteristics of the fenestrated segments, the association with arterial dissections in other craniocervical vessels, and the absence of a clear embryonic mechanism, however, strongly suggest that our findings are in fact arterial dissections with a persistent double lumen rather than congenital anatomic variants. It is suggested that a similar conclusion may be applied to the four cases of cervical ICA fenestration previously reported in the literature.
TABLE 2:
Summary of the reported cases of cervical internal carotid artery (ICA) pseudofenestration and associated findings
| Level | Associated Findings in Fenestrated Artery | Associated Findings in Other Cervicocranial Arteries |
|---|---|---|
| 1. C2 | Slight caliber irregularity | Contralateral ICA dissection |
| 2. C1–C2 | Fusiform dilalation | Contralateral ICA dissection |
| 3. Bifurcation | Pseudoaneurysm | Bilateral vertebral artery dissection, FMD |
| 4. C1–C2 | ICA coiling, fusiform dilatation | FMD |
| 5. C3 | Pseudoaneurysm | FMD |
| 6. C2–C3 | Excentric “false” lumen | Contralateral ICA dissection |
References
- 1.Chess MA, Barsotti JB, Chang JK, et al. Duplication of the extracranial internal carotid artery. AJNR Am J Neuroradiol 1995;16:1545–1547 [PMC free article] [PubMed] [Google Scholar]
- 2.Hasegawa T, Kashihara K, Ito H, Yamamoto S. Fenestration of the internal carotid artery. Surg Neurol 1985;23:391–395 [DOI] [PubMed] [Google Scholar]
- 3.Killien FC, Wyler AR, Cromwell LD. Duplication of the internal carotid artery. Neuroradiology 1980;19:101–102 [DOI] [PubMed] [Google Scholar]
- 4.Koenigsberg RA, Zito JL, Patel M, et al. Fenestration of the internal carotid artery: a rare mass of the hypotympanum associated with persistence of the stapedial artery. AJNR Am J Neuroradiol 1995;16:908–910 [PMC free article] [PubMed] [Google Scholar]
- 5.Nakamura H, Yamada H, Nagao T, et al. Fenestration of the internal carotid artery associated with an ischemic attack–case report. Neurol Med Chir (Tokyo) 1993;33:306–308 [DOI] [PubMed] [Google Scholar]
- 6.Tanaka M, Matsumoto S. Fenestration of the internal carotid artery. Neurol Med Chir (Tokyo) 1982;22:291–294 [DOI] [PubMed] [Google Scholar]
- 7.Hasegawa T, Kashihara K, Kitamura Y, et al. Fenestration of the internal carotid artery in the neck [in Japanese]. No To Shinkei 1985;37:337–342 [PubMed] [Google Scholar]
- 8.Desfontaines P, Despland PA. Dissection of the internal carotid artery: aetiology, symptomatology, clinical and neurosonological follow-up, and treatment in 60 consecutive cases. Acta Neurol Belg 1995;95:226–234 [PubMed] [Google Scholar]
- 9.Mokri B, Sundt TM Jr, Houser OW, Piepgras DG. Spontaneous dissection of the cervical internal carotid artery. Ann Neurol 1986;19:126–138 [DOI] [PubMed] [Google Scholar]
- 10.Padget DH. The development of the cranial arteries in the human embryo. Contr Embryol 1948;212:205–261 [Google Scholar]
- 11.Hassler O. Morphological studies on the large cerebral arteries with reference to the aetiology of subarachnoid haemorrhage. Acta Psychiatr Neurol Scand 1961;36 (Suppl 154):42. [PubMed] [Google Scholar]
- 12.Gailloud P, Albayram S, Fasel JH, et al. Angiographic and embryologic considerations in five cases of middle cerebral artery fenestration. AJNR Am J Neuroradiol 2002;23:585–587 [PMC free article] [PubMed] [Google Scholar]
- 13.Ozdoba C, Sturzenegger M, Schroth G. Internal carotid artery dissection: MR imaging features and clinical-radiologic correlation. Radiology 1996;199:191–198 [DOI] [PubMed] [Google Scholar]
- 14.Petro GR, Witwer GA, Cacayorin ED, et al. Spontaneous dissection of the cervical internal carotid artery: correlation of arteriography, CT, and pathology. AJR Am J Roentgenol 1987;148:393–398 [DOI] [PubMed] [Google Scholar]