Abstract
BACKGROUND AND PURPOSE: Cervical radiculopathy is a common entity that can become unremitting, seriously disrupting the patient’s work and social activities. The purpose of our study was to evaluate the feasibility, tolerance, and efficacy of transforaminal periganglionic steroid infiltration under CT control.
METHODS: Thirty patients with cervical radiculopathy, despite at least 1 month of appropriate medical treatment, underwent percutaneous periradicular foraminal steroid infiltration under CT control. Sixteen patients had foraminal degenerative stenosis, and 14 patients had disk herniation. The intensity of radicular pain was scored on an analogic visual scale (AVS). Pain relief was classified as excellent when the pain had diminished by 75% or more; good, by 50%–74%; fair by 25%–49%; or poor, by less than 25%. The patients were followed up at 2 weeks and at 6 months.
RESULTS: No local complications occurred after the procedure. The mean AVS pain scores were 6.5 points before the procedure and 3.3 points 2 weeks after, with significant pain relief (P < .001). Pain relief was excellent in 11 patients (37%) and good in seven patients (23%). There was no rebound of pain at the 6-month follow-up. The duration of symptoms before infiltration and the intensity and cause of radiculalgia were not predictive of radicular pain relief.
CONCLUSION: Intraforaminal cervical infiltration produced substantial sustained pain relief, whatever the cause of the radiculalgia. The CT approach ensures the safety of vital structures and allows the precise injection of a steroid specifically targeted to the ganglia.
Cervical radiculopathy is a common entity in clinical practice that is frequently caused by disk herniation or cervical spondylosis (1). Transient cervical radiculopathy reportedly occurs in almost 40% of the population at some time during their lives (2). In most patients, radicular symptoms resolve without any treatment or with simple remedies consisting of rest and use of cervical collars, oral corticosteroid dose-packs, nonsteroidal anti-inflammatory drugs, and nonspecific physical therapy measures. In about 10%–20% of patients (3), however, radiculopathy may continue to develop and become unremitting, seriously disrupting their work, social activities, and recreation. These patients are thus referred to specialists for further evaluation and treatment (4). The optimal care of such patients is then debated on the basis of various parameters. While surgical intervention may be recommended in cases of clear neurologic deficit, associated myelopathic signs, or unbearable pain, epidural steroid injections have been reported to benefit patients with pain who do not improve with medical therapy (3, 5). This procedure involves many nerve roots, with no possible selective nerve block of radicular pain. Furthermore, because of the proximity of the spinal cord, epidural infiltration requires extreme caution, otherwise inaccurate needle placement (intrathecal, subdural, or intravascular positioning) or placement within the fibrous ring of an intervertebral disk is a potential source of complications (6). Compared with lumbar foraminal periradicular infiltration, which has been extensively studied, cervical foraminal periradicular steroid infiltration has been discussed in only a few published reports (7–9).
Morvan et al (10) obtained poor results when using an anterolateral fluoroscopic approach and did not recommend this technique in view of their findings and the relatively invasive nature of the procedure. By contrast, Vallee et al (11) used a fluoroscopically guided, lateral percutaneous approach and obtained substantial sustained relief. As Murtagh (12) noted, CT enables more precise anatomic location of periganglionic nerve roots and easily depicts the position of the needle tip in relationship to the nerve root structure. Therefore, we performed foraminal steroid injection under CT control. The purpose of our study was to evaluate the feasibility, tolerance, and efficacy of cervical transforaminal periganglionic steroid infiltration under CT control in patients with a radiculopathy resistant to conventional medical treatment.
Methods
Study Group
During a 2-year period, 30 patients (14 men and 16 women; age range, 22–77 years; mean age, 49.9 years) underwent percutaneous periradicular foraminal steroid infiltration under CT control for cervical radiculopathy. In our institution, patients are referred for foraminal infiltration on the basis of three clinical criteria and one imaging criterion. The clinical criteria were a diagnosis of cervical radiculopathy established by a referring senior rheumatologist (E.T.); refractory persistent pain despite at least 1 month of appropriate medical treatment including a combination of analgesics, muscle relaxants, and physical therapy techniques; a lack of muscular strength deficit (test score >3), or cervical myelopathy findings. The imaging criterion was the CT detection of an abnormal process involving a nerve root. The radiculopathy level was at C6 in 12 patients, C7 in 14 patients, and C8 in four patients. As determined with CT scanning, 16 patients had foraminal degenerative stenosis due to disk bulging, hypertrophic osteoarthritis of the zygapophyseal joint, or an osteophytic ridge of the posterior vertebral body, and 14 patients had foraminal obstruction due to disk herniation. The mean duration of radiculalgia before infiltration was 2.7 months (1–8 months). During follow-up, patients were evaluated at 2 weeks and at 6 months after the procedure to score the intensity of their radicular pain. According to the policies of our institutional review board, approval was not required for this retrospective analysis.
Procedure
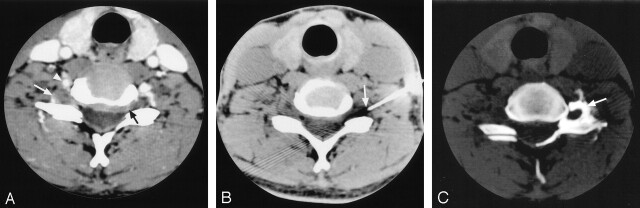
Before therapy, all patients were completely informed about the anticipated benefits and potential risks of the procedure, including the possibility of recurrence of radicular symptoms during injection and/or transient exacerbation after treatment. The patients were placed comfortably in a supine position on the CT table with their arms at their sides. Two-millimeter, axial, contiguous scans were obtained to locate the root ganglion in the intervertebral foramen. A 22-gauge spinal needle was introduced by an anterolateral or lateral approach (with the vertebral artery located to avoid it) and gently pushed to reach the lateral portion of the foramen. Contrast medium (0.3 mL iopanidol) was injected to outline the root ganglion, to verify that the needle tip was not intravascular, and to confirm the correct intraforaminal position of the needle (Fig 1). A corticosteroid (15 mg/3 mL dexamethasone) was then injected slowly. The entire procedure, including patient positioning, lasted about 15 minutes and was performed in an outpatient setting with patients discharged home immediately afterward.
Fig 1.
Images in a patient with a left C6 radicular pain due to posterolateral disk herniation. Pain was completely relieved after infiltration and sustained at clinical follow-up 6 months.
A, Postcontrast CT image at the C5-C6 level shows the vertebral artery (arrowhead) in front of the spinal ganglion (white arrow) and the soft posterolateral disk herniation (black arrow).
B, Needle in contact with the foraminal site of the nerve root (arrow).
C, Control CT scan after foraminal contrast injection shows contrast medium around the spinal ganglion (arrow).
Data Analysis
Patients scored the intensity of radicular pain on an analogic visual scale (AVS) ranging from 0 (no pain) to 10 (maximal intensity). Based on the pain score before the procedure, percentages of pain relief assessed at 2 weeks and at 6 months after infiltration were calculated. These percentages were classified as excellent when the pain was completely resolved or had diminished by 75% or more, good for a diminution of 50%–74%, fair for a diminution of 25%–49%, or poor for a diminution of less than 25% or an increase in pain.
Statistical Analysis
Scores before and after the procedure were compared by using the Wilcoxon signed-rank test for paired values. To identify predictive factors of procedural efficacy, we tested the relationship between radicular pain relief categorized in four classes (excellent, good, fair, or poor) and the following parameters: duration of symptoms before infiltration, intensity of pain according to the AVS score before infiltration by using the nonparametric Kruskal-Wallis test for these quantitative variables, cause of the foraminal disorder (ie, disk herniation or degenerative stenosis), spinal level of radiculopathy. The Fisher exact test was used for these qualitative variables.
Results
The mean AVS scores were 6.5 points before and 3.3 points at 2 weeks after the procedure, with significant pain relief (P < .001). Two weeks after the procedure, pain relief was graded as excellent in 11 patients (37%), nine of whom had no residual pain in nine patients. Pain relief was good in seven patients (23%), fair in two patients (6%) and poor in 10 patients (34%). No local complications occurred after the procedure in this series.
Among the 18 patients for whom pain relief was excellent or good 2 weeks after the procedure, the mean pain score decreased from 6.3 (standard deviation [SD], 1.9) to 1.2 (SD, 1.4), with a mean decrease of 5.1 (SD, 1.6). In these patients, the mean pain score was 0.7 after 6 months of follow-up, and pain relief was classified as still good or excellent for all of these patients. All of these patients discontinued their medical treatment at least 2 weeks after the periradicular injection.
Among the 12 patients for whom pain relief was fair or poor 2 weeks after the procedure, the main pain score decreased from 6.6 (SD, 2.8) to 6.4 (DS, 2.7), with a mean decrease of only 0.2. All of these patients had to resume medical treatment 2 weeks after the procedure. Three had a new infiltration that produced excellent (n = 2) or poor (n=1) pain relief 2 weeks after the second infiltration. In these patients, the mean AVS score at 6 months was 3.9 and decreased to less than to 2 points in four patients who were able to discontinue their medical treatment.
The duration of symptoms and the AVS score before the procedure in the study population and in the four groups classified according to the response to procedure are shown in Table 1. The duration of symptoms before infiltration and the pain intensity graded by using the AVS were not predictive of radicular pain relief. The group of patients with degenerative stenosis had a mean preoperative AVS score of 6.7 and a mean symptom duration of 2.7 months, whereas the group with herniated disks had a mean AVS of 6.2 and a mean symptom duration of 2.6 months. AVS scores and duration of symptoms did not significantly differ between the two groups. The cause of radiculalgia was not correlated with pain-relief outcome (Table 2).
TABLE 1:
Comparison of patients in terms of pain relief
| Measure | Pain Relief |
||||
|---|---|---|---|---|---|
| Total | Excellent | Good | Fair | Poor | |
| No. of patients | 30 | 11 | 7 | 2 | 10 |
| Mean symptom duration, mo | 2.7 | 3.2 | 2.1 | 2.1 | 1.9 |
| Mean AVS score before the procedure | 6.5 | 6 | 7 | 8.5 | 6 |
TABLE 2:
Comparison of symptom duration, AVS score, and pain relief in terms of cause of the radiculalgia
| Measure | All Patients | Patients with Degenerative Stenosis | Patients with a Herniated Disk |
|---|---|---|---|
| No. of patients | 30 | 16 | 14 |
| Mean symptom duration, mo | 2.7 | 2.7 | 2.6 |
| Mean AVS score before the procedure | 6.5 | 6.7 | 6.2 |
| Pain relief, no. of patients (%) | |||
| Excellent | 11 (37) | 5 (31) | 6 (43) |
| Good | 7 (23) | 3 (19) | 4 (29) |
| Fair | 2 (6) | 2 (12) | 0 (0) |
| Poor | 10 (34) | 6 (37) | 4 (29) |
Discussion
Cervical radiculopathy is a pathologic process involving nerve roots that generally arises from cervical disk herniation or spondylosis. Numerous hypotheses have been proposed to explain the mechanisms by which these diseases induce radicular pain, including increased discharge by dorsal root ganglia whose axons have undergone neurotmesis, mechanosensitivity or chemosensitivity of the nerve root itself, and direct pressure on axons or dorsal root ganglia (3, 13). However, it is now well established that dorsal root ganglia play a major role in radiculalgia. Since sensitive afferent C fibers conduct stimuli from the dorsal root ganglion to the spinal cord and since steroids are known to block C-fiber activity (14, 15), corticosteroid injection close to the dorsal root ganglion could explain the efficacy of transforaminal periradicular infiltration. CT scanning facilitates and enhances the efficacy of these procedures by enabling accurate anatomic positioning and precise viewing of the position of the needle tip in relationship to the nerve root structure. This seems particularly important in cervical infiltration because of the small size of the cervical foramina and because of serious potential complications due to inaccurate cervical needle placement. For Murtagh (12), the ease of performance and the decreased X-ray procedural times during spinal intervention afforded by CT (as opposed to conventional fluoroscopy) makes it most desirable to perform this procedure under CT guidance. In comparison, Vallee et al (11) reported that a fluoroscopically guided, lateral percutaneous approach is easy to perform and safe for periradicular corticosteroid injection. These authors highlighted its potential advantages: 1) the procedure can be performed with patients in a sitting position, which may be helpful to gain access to the inferior cervical intervertebral foramen. 2) It avoids intraforaminal contrast injection, which can trigger radicular pain. 3) It is faster and less expensive than other procedures. We decided to perform the procedure under CT guidance because it allows direct identification of nerve root and ganglia in the foramina despite the small size of the nerves and the small amount of surrounding epidural fat at the cervical stage (16), and it enables precise periganglionic positioning of the needle tip. For the procedure we used a contrast-agent injection to document its transforaminal diffusion and avoid subsequent injection of anesthetic and necrolytic agents into undesirable spaces. We agree with Murtagh (12) in that CT images of the exact location of the needle tip and of contrast-agent diffusion must be included in the patient’s record. The procedure was safe, with all injections performed in an outpatient setting and with good tolerance. No technical complications occurred.
We positioned the needle tip within 1–3 mm of the ganglia without attempting to pierce them. As some authors note (12, 17), intraneural needle placemen may induce acute radiculopathy, which constitutes a diagnostic test, but there are no data demonstrating that intraneural injection is therapeutically more effective than closely monitored perineural injection.
Although this study was retrospective, it included a homogeneous group of patients. Patients referred for the procedure had a refractory radiculalgia despite at least 1 month of adequate treatment. Vallee et al (11) included patients with at least 2 months of appropriate medical therapy, whereas Zennaro et al (18) focused on lumbar infiltration and most of the patients had sustained pain for more than 3 months. As noted by Saal et al (19), the decision to proceed with second-intention treatment modalities, including infiltration or surgery, in cases of cervical radiculalgia is made when symptoms persist beyond an arbitrary conservative treatment period of 2–8 weeks. Since pain was judged severe (AVS score ≥6 in 73% of patients) and poorly tolerated in most of our patients, our rheumatologist referred patients after a minimum of 1 month of adequate medical treatment. We evaluated the efficacy of infiltration on radiculalgia and not on neck pain, first because radicular pain is more common and more intense than neck pain in patients with cervical radiculopathy, though both are usually present (3, 20, 21), and secondly because we hypothesized that infiltration in contact with a nerve root would have a direct impact on radicular pain. In a study evaluating the outcome of conservative and surgical treatment of cervical radiculopathy due to disk herniation (contrary to radicular pain), neck pain improved in a minority of patients, irrespective of the treatment used (22). However, Vallee et al (11) reported a good correlation between radicular and neck pain relief after periradicular infiltration and suggested that the nerve root causing radicular pain might also be responsible for neck pain; it would be interesting to confirm these data.
We assessed the efficacy of the treatment on the main outcome parameters, ie, the pain severity graded by means of the AVS and the need for medical treatment. This was done without focusing on other parameters commonly considered in outcome epidemiologic studies (4), such as patient satisfaction or functional status measures, including the ability to perform job-related tasks and participate in social activities. We found that the procedure was sustainably effective, with pain relief classified as good or excellent in 60% of patients. Vallee et al reported similar results, with excellent or good pain relief in 50% of patients at 6 months, whereas Morvan et al (10) noted long-lasting relief in only 14% of treated patients in whom a fluoroscopically anterolateral approach was used. Neither the duration of symptoms before infiltration nor the intensity of pain or cause of the radiculalgia were found to be predictive of radicular pain relief. Some studies have demonstrated that a short duration of pain before treatment was an efficacy factor in the treatment of radicular pain. However, regarding infiltration (11) or surgery (22), other studies (18) did not show any significant difference between chronic and acute pain in terms of treatment success. The fact that the treatment gives the same results whatever the cause of the radiculalgia (spondylosis or hernia) was not expected. Zennaro et al (18) found that lumbar periganglionic, foraminal steroid injection was more successful when pain was due to degenerative disorders than when it was due to nerve involvement resulting from a herniated disk. These authors suggested that this difference in outcome could be attributed to different mechanisms of pain production in disk hernia and in spondylosis. Our data at the cervical stage did not provide any evidence to support this hypothesis.
This study had several limitations, including the fact that it was uncontrolled. Since it is well known that medical treatment may need time to be effective in cervical radiculalgia, it would be important to design randomized controlled trials to compare the efficacy of medical treatment and infiltration. However, prospective studies comparing treatment regimens are bound to fail because a double-blind study design would be hard to apply (22–24). The small patient population did not permit us to evaluate the efficiency of a second infiltration in patients for whom the first procedure did not improve radicular pain. The group undergoing second infiltration consisted of only three patients, an inadequate group size from which to draw any meaningful conclusions. Lastly, our follow-up period was only 6 months, which hindered long-term assessment of periradicular corticosteroid injections in cervical radiculopathy. A recent study on periradicular infiltration for sciatica showed that the effect of infiltration was transitory with a rebound phenomenon at 3 and 6 months (9). This result contrasted with our finding that pain relief was sustained for 6 months.
Conclusion
The results of this study showed that, in 60% of patients who were not responsive to at least 1 month of medical therapy, intraforaminal cervical infiltration produced substantial and sustained pain relief, whatever the cause of the radiculalgia. The CT approach ensures the safety of vital structures and allows the precise injection of a steroid specifically targeted to the ganglia.
References
- 1.Smith MD. Cervical radiculopathy: causes and surgical treatment. Minn Med 1995;78:28–30, 42–45 [PubMed] [Google Scholar]
- 2.Horal J. The clinical appearance of low back disorders in the city of Gothenburg, Sweden: comparisons of incapacitated probands with matched controls. Acta Orthop Scand Suppl 1969;118:1–109 [DOI] [PubMed] [Google Scholar]
- 3.Ellenberg MR, Honet JC, Treanor WJ. Cervical radiculopathy. Arch Phys Med Rehabil 1994;75:342–352 [DOI] [PubMed] [Google Scholar]
- 4.Sampath P, Bendebba M, Davis JD, Ducker T. Outcome in patients with cervical radiculopathy: prospective, multicenter study with independent clinical review. Spine 1999;24:591–597 [DOI] [PubMed] [Google Scholar]
- 5.Stav A, Ovadia L, Sternberg A, Kaadan M, Weksler N. Cervical epidural steroid injection for cervicobrachialgia. Acta Anaesthesiol Scand 1993;37:562–566 [DOI] [PubMed] [Google Scholar]
- 6.Dougherty JH Jr, Fraser RA. Complications following intraspinal injections of steroids: report of two cases. J Neurosurg 1978;48:1023–1025 [DOI] [PubMed] [Google Scholar]
- 7.Gangi A, Dietemann JL. Tomodensitométrie interventionnelle en anesthésie loco-régionale. In: Muller A, ed. Anesthésie Loco-Régionale et Traitement de la Douleur. Paris: Masson,1996. :555–564
- 8.Seibel RM, Grönemeyer DH. Periradicular therapy. In: Seibel RM, ed. Interventional Computer Tomography. Boston: Blackwell,1990. :100–115
- 9.Karppinen J, Ohinmaa A, Malmivaara A, et al. Cost effectiveness of periradicular infiltration for sciatica: subgroup analysis of a randomized controlled trial. Spine 2001;26:2587–2595 [DOI] [PubMed] [Google Scholar]
- 10.Morvan G, Mompoint D, Bard M, Levi-Valensin G. Direct intra-foraminal injection of corticosteroids in the treatment of cervico-brachial pain. In: Bard M, Laredo JD, eds. Interventional Radiology in Bone and Joint. New York: Springer-Verlag,1988. :253–257
- 11.Vallee JN, Feydy A, Carlier RY, Mutschler C, Mompoint D, Vallee CA. Chronic cervical radiculopathy: lateral-approach periradicular corticosteroid injection. Radiology 2001;218:886–892 [DOI] [PubMed] [Google Scholar]
- 12.Murthagh FR. The neuroradiologist as pain therapist. AJNR Am J Neuroradiol 1998;19:353–354 [Google Scholar]
- 13.13 : Rappaport ZH, Devor M. Experimental pathophysiological correlates of clinical symptomatology in peripheral neuropathic pain syndromes. Stereotact Funct Neurosurg 1990;54–55:90–95 [DOI] [PubMed] [Google Scholar]
- 14.Johansson A, Hao J, Sjolund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand 1990;34:335–338 [DOI] [PubMed] [Google Scholar]
- 15.McCormack K. Non-steroidal anti-inflammatory drugs and spinal nociceptive processing. Pain 1994;59:9–43 [DOI] [PubMed] [Google Scholar]
- 16.Pech P, Haughton VM. Lumbar intervertebral disk: correlative MR and anatomic study. Radiology 1985;156:699–701 [DOI] [PubMed] [Google Scholar]
- 17.Quinn SF, Murtagh FR, Chatfield R, Kori SH. CT-guided nerve root block and ablation. AJR Am J Roentgenol 1988;151:1213–1216 [DOI] [PubMed] [Google Scholar]
- 18.Zennaro H, Dousset V, Viaud B, et al. Periganglionic foraminal steroid injections performed under CT control. AJNR Am J Neuroradiol 1998;19:349–352 [PMC free article] [PubMed] [Google Scholar]
- 19.Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine 1996;21:1877–1883 [DOI] [PubMed] [Google Scholar]
- 20.Lunsford LD, Bissonette DJ, Jannetta PJ, Sheptak PE, Zorub DS. Anterior surgery for cervical disc disease, I: treatment of lateral cervical disc herniation in 253 cases. J Neurosurg 1980;53:1–11 [DOI] [PubMed] [Google Scholar]
- 21.Honet JC, Puri K. Cervical radiculitis: treatment and results in 82 patients. Arch Phys Med Rehabil 1976;57:12–16 [PubMed] [Google Scholar]
- 22.Heckmann JG, Lang CJ, Zobelein I, Laumer R, Druschky A, Neundorfer B. Herniated cervical intervertebral discs with radiculopathy: an outcome study of conservatively or surgically treated patients. J Spinal Disord 1999;12:396–401 [PubMed] [Google Scholar]
- 23.van Gijn J, Reiners K, Toyka KV, Braakman R. Management of cervical radiculopathy. Eur Neurol 1995;35:309–320 [DOI] [PubMed] [Google Scholar]
- 24.Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine 2002;27:11–16 [DOI] [PubMed] [Google Scholar]