Abstract
Summary: The endovascular treatment of wide-necked intracranial aneurysms is evolving. We report our initial experience in treating seven wide-neck intracranial aneurysms by using a new self-expanding stent, the Neuroform, in combination with a new generation of coils that incorporate a self-expandable hydrophilic lining, the HydroCoil.
Despite rapid technological advances in endovascular technology, wide-necked intracranial aneurysms remain difficult to treat with associated high recanalization rates. Recently, a stent designed for intracranial use, the Neuroform (Boston Scientific, Natick, MA), has been approved by the U.S. Food and Drug Administration (FDA) on a humanitarian device exemption protocol. Early experience with this stent has been reported in four studies comprising a total of 87 patients in which the stent was successfully and safely deployed as a scaffold for coil deposition in wide-necked aneurysms (1–4).
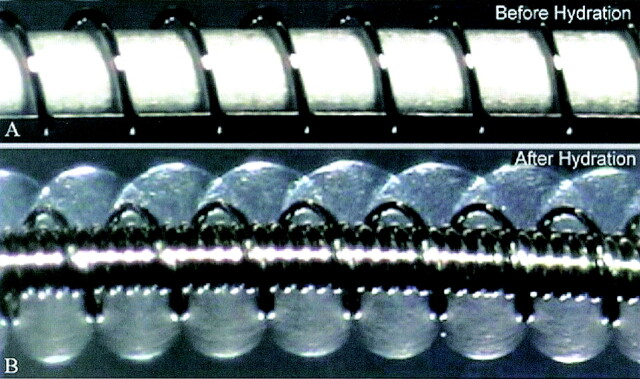
HydroCoil (MicroVention, Aliso Viejo, CA), a new-generation coil, composed of a platinum coil to which a synthetic polymeric hydrogel is attached (5), has been recently approved by the FDA. These coils undergo progressive expansion (hydration) once exposed to the physiologic environment (pH 7.4) of blood (Fig 1; 6,7) and have the theoretical advantage of better space filling between the platinum struts. Preliminary experience using these coils in two series comprising 41 total patients with intracranial aneurysms was recently presented to the Symposium Neuroradiologicum, Paris, France, in 2002 (P. Lylyk, J. Moret, M. Piotin et al, unpublished data) (6). We here report the combined use of these two devices in the treatment of wide-necked aneurysms.
Fig 1.
HydroCoil before (A) and after (B) expansion.
Technique
Patients with unruptured aneurysms were premedicated for 3 days with clopidogrel (75 mg) and aspirin (325 mg). Patients treated acutely after subarachnoid hemorrhage were loaded with clopidogrel (225 mg) and aspirin (325 mg) via nasogastric tube during the coiling procedure once a decision to place the stent was made. All patients were continued on clopidogrel (75 mg) and aspirin (325 mg) postprocedure for a minimum of 3 months. All procedures were performed under general anesthesia with patients heparinized to maintain an activated clotting time (ACT) >300. Follow-up angiography was performed (when possible) at 6 months and at 1 year. Clopidogrel was stopped at 3 months, if there were no untoward clinical events, and the patients were continued on aspirin.
We treated seven intracranial aneurysms (five unruptured) with Neuroform stent-assisted coiling by using HydroCoils. Complete or nearly complete aneurysmal occlusion was achieved in all patients. Clinical information and relevant technical data are recorded in Table 1. There was technical difficulty associated with two stent placements (one maldeployment and one stent migration during coiling) and two minor complications associated with transient ischemic phenomenon. Two patients presented in a delayed fashion with symptomatic hydrocephalus and improved dramatically after ventriculoperitoneal shunt placement.
Neuroform Stent-assisted HydroCoiling
| Case # | Age/Sex | H&H | Fisher | Location | An./Neck Size (mm) | Stent Location | %Hydrocoil Volume | Complications |
|---|---|---|---|---|---|---|---|---|
| 1 | 46M | 0 | 0 | Basilar Apex | 11.4/4.3 | Left P1/Basilar | 67 | Thrombus, Rx. Reopro, No Clinical Change, Hydrocephalus |
| 2 | 41M | 3 | 3 | Basilar Trunk | 8.0/NA | Mid-Basilar | 68 | None |
| 3 | 64M | 0 | 0 | Basilar Trunk | 11.5/6.7 | Mid-Basilar | 72 | Post-op Brain-stem Strokes |
| 4 | 58F | 0 | 0 | Left Ophthalmic | 11.0/4.2 | Left ICA | 63 | None |
| 5 | 40F | 4 | 3 | Left Ophthalmic | 6.0/4.5 | LEFT ICA | 52 | Stent Slippage During Placement |
| 6 | 77M | 0 | 0 | Left Pcomm | 12.0/6.0 | Left ICA | 53 | None |
| 7 | 75F | 0 | 0 | Left Ophthalmic | 15.8/7.5 | Left ICA | 62 | Stent Slippage During Coiling, Hydrocephalus |
Key: H&H: Hunt and Hess; An. = aneurysm, M = male; F = female; ICA = internal carotid artery; Rx. = treatment; NA = not applicable
Illustrative Case
A 58-year-old right-handed woman (case 4) with a history of tobacco smoking and a family member with an intracranial aneurysm was found to have incidental bilateral internal carotid artery (ICA) aneurysms. Eight months after successful coiling of her right ophthalmic aneurysm with pure platinum Guglielmi detachable coils, her left ophthalmic wide-necked aneurysm was treated. Cerebral angiography showed the superiorly directed aneurysm with its origin slightly beyond the left ophthalmic artery. The angiogram showed the aneurysm to measure 11 mm × 7 mm with a 5-mm neck (Fig 2A). Under full heparinization, microcatheterization (Excelsior SL-10, Boston Scientific) beyond the aneurysm was followed by deployment of a Neuroform stent delivery system over an Accelerator 0.014-inch, 300-cm-long exchange microguidewire (Microtherapeutics, Irvine, CA). The stent, measuring 4 mm × 20 mm, was navigated and deployed such that it covered the aneurysm neck and rested from below the anterior choroidal takeoff to the level of the dural ring (Fig 2B). The Excelsior SL-10 microcatheter over a microguidewire was then introduced through the stent into the superior portion of the aneurysmal sac.
Fig 2.
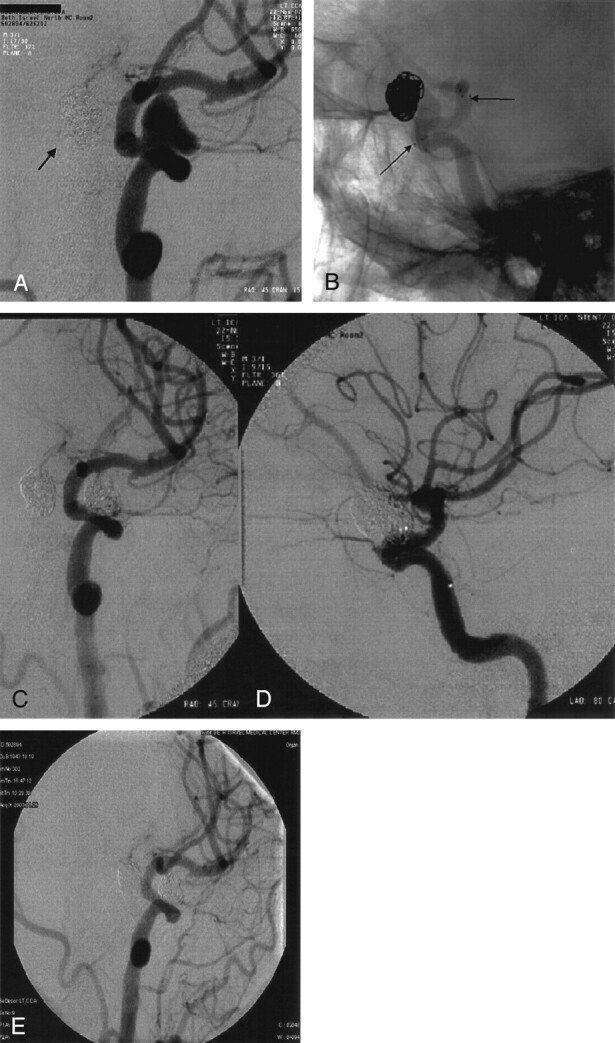
A, Left ICA digital subtraction angiography (oblique view) reveals a paraclinoid aneurysm (arrow points to coil mass of right paraclinoid aneurysm coiled 8 months earlier).
B, Digital nonsubtracted angiogram of the left ICA after stent deployment. The stent proximal and distal markers are visualized (arrows) across the aneurysm neck before deployment.
C and D, After HydroCoil embolization, with an excellent angiographic and clinical result. Coils are again seen in the contralateral previously coiled aneurysm.
E, Follow-up angiography 1 year later shows stable coil occlusion of the left paraclinoid aneurysm with no evidence for in-stent stenosis or aneurysm recanalization.
Successive coil placement leading to near complete obliteration of the aneurysm was accomplished by first placing a microplex 2D coil (MicroVention) measuring 10 mm × 24 cm as a frame, followed by packing with six HydroCoils (Fig 2C, –D). Interim repetitive angiography, performed after each coil placement, documented progressive occlusion of the aneurysm secondary to HydroCoil expansion until there was only minimal residual filling of the anterior aneurysm neck and anterior inferior sac with marked stagnation (Fig 2C, D). Control angiography 3 days later demonstrated preserved internal carotid and ophthalmic artery patency and total obliteration of the aneurysm. One year postprocedure, she remains neurologically well and angiography shows a stable configuration of both her coils and stent without evidence for recanalization or in-stent stenosis (Fig 2E).
Discussion
The Neuroform stent/HydroCoil combination may be an advancement in the treatment of wide-necked intracranial aneurysms. Here we describe the combination of a self-expanding stent designed specifically for intracranial navigation, and used for stent-assisted coil embolization, in conjunction with a new-generation coil designed to expand after deployment to yield markedly increased coil occlusion. Stent-assisted cerebral aneurysm embolization is possibly more effective against future compaction and recanalization than balloon-assisted or unassisted coiling because it permits a denser packing of the aneurysm while preserving parent artery patency and reducing inflow pressures into the aneurysm neck. Four reports on the use of Neuroform-assisted coiling of intracranial aneurysms have been published, but none with the concomitant use of HydroCoils. The largest and most recent series details the use of this stent to assist in the coiling of 42 aneurysms, 15 of which were acutely ruptured (1). More than 90% aneurysmal occlusion was achieved in 39/42 (93%) patients, with an associated procedural complication rate of 10.7%. Angiographic follow-up was obtained in five patients at 6 months and there were no instances of in-stent stenosis or aneurysm recanalization.
HydroCoils are a new hybrid embolic device that is part of the growing line of embolic agents chemically pretreated to enhance their intended function. In this particular instance, carrier platinum coils are coupled to an expandable hydrogel material that results in delayed progressive expansion of the coil once it comes in contact with a water-based substance, such as blood, with a pH of 7.4. The expansion is expected to begin 5 minutes after exposure and completed by 20 minutes. By expanding as much as nine times its prehydrated volume, these coils achieve a more complete volumetric occlusion of aneurysms (8). The ability of this coil to more completely fill the aneurysm contrasts with preexisting platinum coils, where complete angiographic occlusion might represent only 20–30% occlusion of the aneurysmal sac with platinum coils, the rest of the volume occupied by thrombus. An additional apparent advantage of HydroCoils is that they may cause advanced healing and endothelialization at the aneurysm neck (5,8). The first clinical experience demonstrating technical feasibility and increased volumetric aneurysm filling with HydroCoils relative to pure platinum coils in 11 patients was recently published (6).
In addition to the increased volumetric occlusion achieved with HydroCoils alone, the addition of the stent permits tighter packing of the neck with HydroCoils with less risk of protruding coils into the parent vessel. This dual benefit from the stent-HydroCoil combination has particular benefit when treating wide-neck aneurysms and may result in tighter packing of aneurysms and resultant decreased incidence of compaction and recanalization.
Thromboembolic phenomena occurred in 2/7 patients; however, we have no direct evidence that these events were in any way related to the combined use of a stent with HydroCoils. Concerns that expansion of the hydrogel polymer after coil deployment may lead to stent and/or vessel stenosis or that shearing off of the hydrogel polymer during expansion against the stent may lead to thromboembolism are theoretical. We have used HydroCoils as filler coils and finish the coiling procedure with bare platinum. This can avoid placement of exposed hydrogel at the mouth of the aneurysm, in contact with the stent. As we approach the neck of the aneurysm, we pack more slowly, waiting for the HydroCoils to fully expand. Although we do not wait between HydroCoil placements, as we approach occlusion of the aneurysm we wait a full 20 minutes to allow maximal HydroCoil swelling to determine whether additional coils are necessary. We believe that further experience with this technique will resolve these issues. Aggressive perioperative and postoperative anticoagulation is important when using Neuroform stents and HydroCoils. Our anticoagulation regimen has been adopted from those used during coronary stent placement and is in line with the other reports on stent-assisted coiling (2–4,9). Anticoagulation for Neuroform HydroCoiling, is important but the optimal regimen has not yet been defined.
Although we feel that stent-assisted HydroCoil embolization is an improvement in the endovascular treatment of these difficult aneurysms, the results of this report must be interpreted with caution. This study documents the feasibility of using a newly released stent and coil, in combination, in seven human subjects. Despite the use of this technique, 100% aneurysmal occlusion was not achieved; the significance of this for the treatment of acutely ruptured aneurysms or for the long-term efficacy for all aneurysms treated with this technique is not known.
Delayed symptomatic hydrocephalus occurred in two patients in whom we treated unruptured aneurysms with stent-assisted HydroCoiling. We could find no mention of the development of hydrocephalus after coiling of unruptured aneurysms in the literature and have not ourselves experienced this in more than 500 coiled, unruptured intracranial aneurysms. Fortunately, both patients returned to their baseline functioning after shunt placement. The exact role of the HydroCoils in these two cases is under investigation.
Conclusion
The combination of intracranial stents, such as the Neuroform, with self-expandable coils (HydroCoils) designed to increase volumetric filling of the aneurysm may be an improved method of treating certain broad-based aneurysms. We have demonstrated the technical feasibility of using this combination in seven patients with wide-necked aneurysms, at least some of which would be considered surgically difficult lesions in which the risks of open surgery would be high.
Footnotes
A.B. is a stockholder in, scientific advisor to, and receives grant support from the Boston Scientific and MicroVention corporations.
References
- 1.Benitez RP, Silva MT, Klem J, et al. Endovascular occlusion of wide-necked aneurysms with a new intracranial microstent (Neuroform) and detachable coils. Neurosurgery 54:1359–1367 [DOI] [PubMed] [Google Scholar]
- 2.Fiorella D, Albuquerque FC, Han P, McDougall CG. Preliminary experience using the Neuroform stent for the treatment of cerebral aneurysms. Neurosurgery 54:6–16 [DOI] [PubMed] [Google Scholar]
- 3.Henkes H, Bose A, Felber S, et al. Endovascular coil occlusion of intracranial aneurysms assisted by a novel self-expandable nitinol microstent (Neuroform). Intervent Neuroradiol 8:107–119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wanke I, Doerfler A, Schoch B, et al. Treatment of widenecked intracranial aneurysms with a self-expanding stent system: initial clinical experience. AJNR Am J Neuroradiol 24:1192–1199 [PMC free article] [PubMed] [Google Scholar]
- 5.Fujiwara NH, Kallmes DF. Healing response in elastase-induced rabbit aneurysms after embolization with a new platinum coil system. AJNR Am J Neuroradiol 23:1137–1144 [PMC free article] [PubMed] [Google Scholar]
- 6.Cloft HJ, Kallmes DF. Aneurysm packing with HydroCoil embolic system versus platinum coils: initial clinical experience. AJNR Am J Neuroradiol 25:60–62 [PMC free article] [PubMed] [Google Scholar]
- 7.Kallmes DF, Fujiwara NH. New expandable hydrogel-platinum coil hybrid device for aneurysm embolization. AJNR Am J Neuroradiol 23:1580–1588 [PMC free article] [PubMed] [Google Scholar]
- 8.Yoshino Y, Niimi Y, Song JK, et al. Endovascular treatment of intracranial aneurysms: comparative evaluation in a terminal bifurcation canine aneurysm model. J Neurosurg 2004;101:996–1003 [DOI] [PubMed] [Google Scholar]
- 9.Lylyk P, Cohen JE, Ceratto R, Ferrario A, Miranda C. Endovascular reconstruction of intracranial arteries by stent placement and combined techniques. J Neurosurg 2002;97:1306–1313 [DOI] [PubMed] [Google Scholar]