Progressive multifocal leukoencephalopathy (PML) is a rare but emerging demyelinating neurologic infection of the CNS caused by reactivation of the John Cunningham (JC) virus.1 Several immunocompromised populations are susceptible for PML, for example, those with hematologic malignancy, HIV infection, transplant recipients, and specific disease-modifying therapies.2 For the total PML population, 1- and 5-year survival rates have been estimated to be 30% and 10%, respectively.2 The most crucial factor in the chances of survival depends on whether immune function can be restored.2 Pembrolizumab is a monoclonal antibody that blocks programmed cell death protein-1 on the surface of the T cell, allowing T cells to be reactivated and to facilitate the clearance of the virus.3 Pembrolizumab treatment of 8 patients with PML led to decreased CSF viral load in all patients and stabilization of clinical deterioration or improvement in 5 patients.4 Subsequently, 2 patients with PML were reported without clinical improvement after pembrolizumab treatment.5,6 In the literature, 11 patients with PML treated with pembrolizumab have been described, of whom 6 had a favorable outcome.4-7
Classification of Evidence
This provides Class IV evidence.
Case 1
A 73-year-old man presented with a subacute progressive language disorder and right-sided hemiparesis. His medical history included ulcerative colitis, for which he was treated with mesalazine. Neurologic examination showed aphasia, a right-sided hemianopsia and a right-sided hemiparesis. MRI findings were consistent with PML (figure), and CSF examination showed a positive PCR for the JC virus (20,000 copies). Additional blood tests showed a lymphocytopenia (0.83 × 109 U/L, ref 1.5–4.0), decreased CD4 (0.19 × 109 U/L, ref 0.3–1.4) and CD8 (0.09 × 109 U/L, ref 0.2–0.9) cell count, and negative HIV test. Subsequently, gene panel testing for detecting immune deficiencies was performed, which turned out to be normal. Based on these findings, the diagnosis of a primary T-cell deficiency was made. The patient was treated with 200 mg of pembrolizumab. After 3 weeks, he clinically deteriorated with mutism and a deterioration of the hemiparesis after which further treatment was discontinued. However, after 3 months, the patient gradually improved. Repeated MRI (figure) showed the stabilization of the left parieto-temporal white matter lesions with reduced edema and residual atrophy. At the 1-year follow-up, patient talked fluently, walked for over an hour, and was able to function independently in his daily living activities. Some cognitive deficiencies persisted.
Figure. Axial MRI FLAIR and Contrast-Enhanced T1 Images (Radiologic Convention, Left = Right) of the 2 Patients at Baseline (T = 0) and after 6 months (T+6 M).
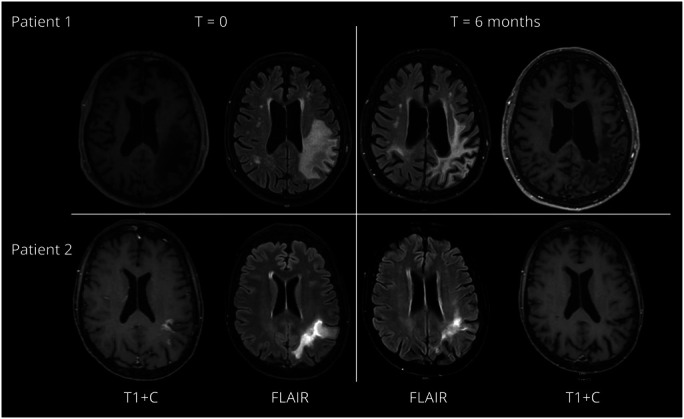
In patient 1 (upper row), at baseline, multiple hyperintense lesions on the fluid-attenuated inverse recovery (FLAIR) sequence were visible. The largest was located in the left parietal cortex. The lesions included the U fibers. After IV gadolinium, no contrast enhancement was visible. At ±6 months, the size of the lesions had decreased and atrophy was visible in the affected areas. In patient 2 (lower row), at baseline, multiple hyperintense lesions on the FLAIR sequence were visible. The largest was located in the left parietal cortex. The lesions included the U fibers. After IV gadolinium, ring enhancement was visible. At ±6 months, the lesions were less outspoken and no contrast enhancement was visible anymore.
Case 2
A 58-year-old woman presented with a progressive speech disorder over a period of 1 month. She had a medical history of polymyositis and systemic sclerosis, for which she was previously treated with rituximab and azathioprine, which were stopped for 1 and 3 years before the onset of symptoms, respectively.
Neurologic examination showed an expressive aphasia with bilateral Babinski reflexes. MRI findings were compatible with PML (figure), and CSF examination showed a positive PCR for the JC virus. Additional blood tests showed a lymphocytopenia (0.55 × 109 U/L, ref 1.5–4.0) and a decreased CD4 (0.17 × 109 U/L, ref 0.3–1.4) and CD8 (0.07 × 109 U/L, ref 0.2–0.9) cell count. The diagnosis of PML was made after which she was treated with pembrolizumab 200 mg. Several weeks later, she noticed a gradual improvement of symptoms. Because of the potential relapse of her polymyositis and systemic sclerosis on additional pembrolizumab treatment, it was decided not to treat the patient with a second dose. Repeated MRI after 6 months showed a subtle improvement of the white matter lesions (figure). One year after the start of her symptoms, her aphasia had markedly improved and Babinski reflexes were no longer present.
Discussion
Treatment with a single dose of pembrolizumab led to substantial clinical improvement in 2 patients with PML and stabilization of their MRI abnormalities at the 1-year follow-up. Our experience indicates, in addition to the existing literature, that a favorable outcome can be achieved in PML associated with rituximab treatment 4 and a primary immune deficiency.4-6 Our patients gradually improved after a single dose of pembrolizumab, whereas the patients described in the literature received up to 12 doses.7 The clinical improvement was observed after 1 year, which is consistent with earlier studies in patients receiving biweekly doses, showing immune reconstitution 4–8 weeks after the first pembrolizumab dose. This is longer than the average median survival (130 days)2 and suggestive that a single dose may be sufficient to result in a sustained suppression of the JC virus. Up to now, no data on the longevity of treatment effect, dosing frequency, and interval are available. In theory, T-cell reactivation can be achieved with a single dose of pembrolizumab.3 Further studies on patient characteristics and biomarkers that predict the success or failure of pembrolizumab treatment, such as the absence of exhausted memory T-cell subsets,6 may provide additional information to guide treatment decisions.
Appendix. Authors

Contributor Information
Fleur Rövekamp, Email: fa.rovekamp@nwz.nl.
Diederik van de Beek, Email: d.vandebeek@amsterdamumc.nl.
Matthijs Brouwer, Email: m.c.brouwer@amsterdamumc.nl.
Study Funding
The authors report no targeted funding.
Disclosure
M. Beudel has no disclosures relevant to this study; F. Rövekamp has no disclosures relevant to this study; D. van de Beek has no disclosures relevant to this study; and M. Brouwer has no disclosures relevant to this study. Go to Neurology.org/NN for full disclosures.
References
- 1.Berger JR, Aksamit AJ, Clifford DB, et al. PML diagnostic criteria: consensus statement from the AAN neuroinfectious disease section. Neurology. 2013;80(15):1430-1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kartau M, Verkkoniemi-Ahola A, Paetau A, et al. The incidence and predisposing factors of John Cunningham virus-induced progressive multifocal leukoencephalopathy in Southern Finland: a population-based Study. Open Forum Infect Dis. 2019;6(2):ofz024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger JR. PD-1 inhibition: a novel approach to the treatment of progressive multifocal leukoencephalopathy. Ann Transl Med. 2019;7(Suppl 8):S281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cortese I, Muranski P, Enose-Akahata Y, et al. Pembrolizumab treatment for progressive multifocal leukoencephalopathy. N Engl J Med. 2019;380(17):1597-1605. [DOI] [PubMed] [Google Scholar]
- 5.Küpper C, Heinrich J, Kamm K, Bücklein V, Rothenfusser S, Straube A. Pembrolizumab for progressive multifocal leukoencephalopathy due to primary immunodeficiency. Neurol Neuroimmunol Neuroinflamm. 2019;6(6):e628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pawlitzki M, Schneider-Hohendorf T, Rolfes L, et al. Ineffective treatment of PML with pembrolizumab: exhausted memory T-cell subsets as a clue? Neurol Neuroimmunol Neuroinflamm. 2019;6(6):e627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rauer S, Marks R, Urbach H, et al. Treatment of progressive multifocal leukoencephalopathy with pembrolizumab. N Engl J Med. 2019;380(17):1676-1677. [DOI] [PubMed] [Google Scholar]


