Abstract
Background
The COVID-19 pandemic represents a public health, economic and mental health crisis. We hypothesized that timely government implementation of stringent measures to reduce viral transmission would benefit mental health, as evidenced by reduced rates of depressive symptoms (i.e., Patient Health Questionnaire [PHQ]-9≥10, PHQ-2≥3).
Methods
The systematic review herein (PROSPERO CRD42020200647) evaluated to what extent differences in government-imposed stringency and timeliness of response to COVID-19 moderate the prevalence of depressive symptoms across 33 countries (k=114, N=640,037). We included data from six lower-middle-income countries, nine upper-middle-income countries, and 18 higher-income countries. Government-imposed stringency and timeliness in response were operationalized using the Oxford COVID-19 Government Response (“Stringency”) Index.
Results
The overall proportion of study participants with clinically significant depressive symptoms was 21.39% (95% CI 19.37–23.47). The prevalence of clinically significant depressive symptoms was significantly lower in countries wherein governments implemented stringent policies promptly. The moderating effect of government response remained significant after including the national frequency of COVID cases at the time of study commencement, Healthcare Access and Quality index, and the inclusion of COVID patients in the study.
Limitations
Factors that may have confounded our results include, for example, differences in lockdown duration, lack of study participant and outcome assessor blinding, and retrospective assessment of depressive symptom severity.
Conclusions
Governments that enacted stringent measures to contain the spread of COVID-19 benefited not only the physical, but also the mental health of their population.
Keywords: Depression, Depressive Disorder, Public Health, Pandemic, COVID-19, severe acute respiratory syndrome coronavirus 2
1. Introduction
The current threat of the COVID-19 pandemic to mental health is unprecedented in scale and scope (Xiong et al., 2020). In addition to being a public health crisis, COVID-19 is also a mental health and economic crisis. The prevalence and severity of depression and other mental disorders have increased during the pandemic across geopolitical, cultural, and sociodemographic strata (De Sousa et al., 2020; Moser et al., 2020; Nyashanu et al., 2020; Petterson et al., 2020). Furthermore, government responses to contain infection have significantly reduced economic activities in most world regions, with the externality of significant gross domestic product contraction and increased extreme poverty in low-income countries (Franco et al.et , 2020; Nyashanu et al., 2020; OECD, 2020).
Financial insecurity and unemployment predispose and portend poor mental health outcomes (Ibrahim et al., 2019; Reeves et al., 2014). For example, we recently predicted that suicide mortality will increase by 3-8% in the USA and 5-27% in Canada per year, between 2020 and 2021, as a result of heightened unemployment rates, which are attributable to COVID-19-related lockdown measures (McIntyre and Lee, 2020a, 2020b). School closures, travel restrictions, sudden shifts to working from home, social gathering bans, and other disruptions to social life and day-to-day routines additionally contribute to the mental health burden experienced by individuals under lockdown (Hou et al., 2020a, 2020b; IASC Reference Group on Mental Health and Psychosocial Support in Emergency Settings, 2020; Walker et al., 2020). Individuals working in healthcare settings may be additionally distressed by the risk of being exposed, and/or exposing others, to COVID-19 infection (Chirico et al., 2021; K. Lin et al., 2020).
It can be conjectured that the uncertainty emanating and surrounding events of COVID-19 are independently hazardous to general wellbeing and mental health. In keeping with that view, interventions that reduce uncertainty may protect mental health. For example, results from a recent study indicate that, during the COVID-19 pandemic, widespread face mask usage in the community may mitigate population level rates of psychological distress by providing assurance: by wearing a mask, individuals are protecting their own health and the health of others and, by extension, are being protected by others in the community who are also wearing masks (C. Wang et al., 2020). In addition to the public health, economic and mental health crisis that has played out during COVID-19, malignant uncertainty also exists across many aspects, including but not limited to, accurate information surrounding the risk of COVID-19 to the general population, availability of proven therapeutics, evidence-based vaccines, and return to work (Holmes et al., 2020; World Health Organization, 2020). We hypothesized that the timely implementation of stringent containment measures may mitigate depressive symptom risk by exacting certainty (and reducing helplessness) at the general population level.
We evaluated the impact of the COVID-19 pandemic and government response on measures of depressive symptom presence and severity based on published studies. Our systematic review included studies that evaluated measures of depressive symptom severity in the general population during the COVID-19 pandemic. Studies were pooled across countries to characterize how differences in the stringency and timeliness of government response to COVID-19 moderate the risk for clinically significant depressive symptoms.
2. Methods
We conducted a meta-analytic and systematic review concordant with recommendations from the Cochrane Handbook for Systematic Reviews of Interventions and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, 2019; Moher et al., 2009). Our study protocol, including our Patient, Intervention, Comparison and Outcome (PICO) (strategy, was registered in the International Prospective Register of Systematic Reviews (PROSPERO CRD42020200647) (Lee et al., 2020).
2.1. Inclusion and exclusion criteria
We included studies that evaluated measures of depressive symptom severity in the general population during the COVID-19 pandemic. The COVID-19 pandemic was operationalized as January 1, 2020 to the present time of manuscript writing. We included studies reporting the number or proportion of study participants meeting criteria for clinically significant depressive symptoms. Our preliminary search identified the Patient Health Questionnaire (PHQ) as the most commonly reported standardized depression metric in the extant COVID-19 literature. Moreover, studies using the PHQ consistently used the same cut-off score to detect moderate-to-severe depressive symptoms (i.e., PHQ-9≥10, PHQ-2≥3). To reduce heterogeneity among included studies and minimize the potential confounding effect of differences between depression metrics and scoring methods, we delimited our inclusion criteria to studies reporting categorical depression outcomes using the PHQ.
Studies reporting outcomes for a single country were eligible; those including study participants from more than one country but reporting outcomes separately for each country were also eligible. Studies that explicitly pooled outcomes across multiple countries were ineligible. Study authors, sample sizes, site locations, and enrollment periods were screened to identify duplicate study samples.
2.2. Systematic search strategy and study selection
We searched Ovid MEDLINE/PubMed from inception to September 16, 2020 for relevant publications without language restrictions. The following medical search headings and keywords were used: (Coronavirus Infections/ or Severe Acute Respiratory Syndrome/ or Pandemics/ or "COVID" or "COVID-19" or "coronavirus" or "SARS-CoV-2") and (Mood Disorders/ or depressi* or Depressive Disorder, Major/ or "patient health questionnaire" or "PHQ"). Results were limited to articles published in 2019 or 2020. The complete search strategy and results for the Ovid MEDLINE/PubMed search are listed in Table S1.
The titles and abstracts were reviewed for eligibility (by author YL); full texts of potentially eligible articles were subsequently reviewed in duplicate independently (by authors DC, LMWL, and YL) using Covidence (Veritas Health Innovation, 2021). Any discrepancies in determining eligibility were resolved by consensus (between authors DC, LMWL, and YL).
2.3. Data extraction
The primary outcome measure was the proportion of study participants with clinically significant depressive symptoms. The most commonly used and validated cut-off score of ≥10 on the PHQ-9 (and ≥3 on the PHQ-2) is commensurate with moderate-to-severe severity (Y. Lee et al., 2020a). We assessed the presence of moderate-to-severe symptoms, rather than mild symptoms, as most evidence-based clinical practice guidelines recommend pharmacological interventions and manual-based psychotherapy for patients with moderate-to-severe symptoms. We additionally extracted the following information using a standardized assessment form: full citation, country sampled, sample size, data collection method, recruitment strategy, depression metric and cut-off score(s), proportion of study participants that tested positive for COVID-19, inclusion of inpatients being treated for COVID-19, and study period.
The stringency of government response was operationalized using the Oxford COVID-19 Government Response Index, which ranges from 0 to 100 (least to most stringent government response). At the time of manuscript writing (September 17, 2020), daily index values were available for individual countries from January 1, 2020 to September 16, 2020. Countries were rated on an ordinal scale to capture, 1) whether or not a given policy was enforced and 2) how stringently or comprehensively each policy was implemented. Countries without any publicly available information about a particular policy were assumed to have abstained from its implementation. Eight containment-, two economic support-, and three health-related policies were evaluated. Containment-related policies included school, workplace, and public transportation closures; public event cancellations; public gathering, national travel, international travel restrictions or controls; and stay-at-home requirements. Economic policies included income support and debt relief for households. Health policies included public education campaigns, COVID-19 testing, and contact tracing (Hale et al., 2020).
The timeliness of government intervention was operationalized using the earliest date a country reached a value of 20 or greater on the Oxford COVID-19 Government Response Index, henceforth referred to as the “stringency index.” A cut-off value of 20 was chosen following a preliminary analysis evaluating weekly changes in global mean stringency index. The largest increase in global mean stringency index (i.e., of 20 index points) was observed between the weeks of March 8-14 and March 15-21. The stringency indices have been plotted for each country included in our analysis for reference (Figure S1).
The Healthcare Access and Quality (HAQ) index measured national ratings of personal access to high quality healthcare (GBD 2016 Healthcare Access and Quality Collaborators, 2018). The index ranges from 0-100; a higher score identifies a country with greater access to high quality healthcare. Countries were ranked in descending order by Human Development Index (United Nations Publications, 2020). Countries were categorized using World Bank classifications of income groups (World Bank, 2020).
2.4. Assessment of bias
We adapted the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool and recommended signalling questions to evaluate risk of biases (Sterne et al., 2016) The ROBINS-I tool uses “intervention” to refer to exposure groups in observational studies. In our risk of bias assessments, we considered the intervention to be the COVID-19 pandemic. We rated each study as low, moderate, or serious on each domain of biasbias : 1) confounding, 2) participant selection, 3) intervention classification, 4) missing data, 5) outcome measurement, and 6) reporting. Bias due to deviations from intended interventions was not assessed as all included studies were conducted during the COVID-19 pandemic, implying that there was no deviation from the intervention.
2.5. Statistical analysis
A meta-analysis of proportions was conducted using the meta::metaprop function on R, version 4.0.2 (R Core Team, 2020). We evaluated the moderating effects of the Government Response Index, as well as other covariates, using the meta::metareg function. A restricted maximum likelihood model pooled proportion data and estimated between-study variance (Nyaga et al., 2014). Exact binomial confidence intervals (CI) were calculated for individual studies and 95% CI of pooled estimates were calculated using the Wald method (Molenberghs et al., 2007). Pooled estimates were Freeman-Tukey double arcsine—transformed (Freeman and Tukey, 1950).
Cochrane's Q and I2 tests quantified heterogeneity, between studies and between countries, as being small, moderate, or large (i.e., I2 = 25%, 50%, or 75%, respectively) (Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, 2019). We assessed publication bias using Egger's and Begg's tests using the meta::metabias function (Begg and Mazumdar, 1994; Egger et al., 1997). We used the trim and fill method (metafor::trimfill) to correct for publication bias (Duval and Tweedie, 2000). The metafor::forest and meta::funnel functions created forest and funnel plots (Balduzzi et al., 2019; Viechtbauer, 2010).
3. Results
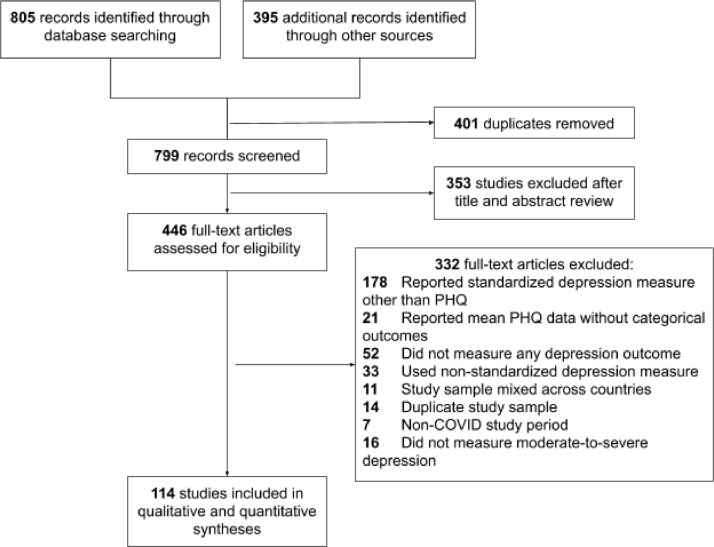
Our database and manual literature searches identified 799 unique records. The full texts of 446 articles were assessed for eligibility. A total of 114 articles reporting categorical depression outcomes using the PHQ were included in the present meta-analysis (Fig. 1 ).
Fig. 1.
Articles identified through database and manual searches were reviewed for eligibility for inclusion in the present meta-analysis. Articles reporting depression outcomes, using the Patient Health Questionnaire, during the COVID-19 pandemic were included. Studies were pooled by country. We evaluated how the stringency of government response to COVID-19 moderated differences across countries in depression outcomes.
We included studies originating in 33 countries, including 18 high-income regions (i.e., Austria, Canada, France, Germany, Greece, Hong Kong Special Administrative Region of the People's Republic of China, Italy, Ireland, Israel, Norway, Poland, Saudi Arabia, South Korea, Spain, Sweden, Switzerland, United Kingdom, USA), nine upper-middle-income countries (i.e., Albania, Bosnia and Herzegovina, Brazil, China, Ecuador, Iran, Jordan, Mexico, Turkey), and six lower-middle-income countries (i.e., Bangladesh, India, Kenya, Nepal, Pakistan, Vietnam). We did not identify any eligible studies from a low-income country. The included studies are summarized in Table S2.
Twenty-six studies used the 2-item PHQ, whereas 88 studies used the 9-item PHQ. Nine studies did not report the cut-off score used to define clinically significant depressive symptoms. All other studies used standard cut-off scores for clinically significant symptom severity (i.e., 10 on PHQ-9, 3 on PHQ-2) (Manea et al., 2012).
3.1. Global prevalence of clinically significant depressive symptoms during COVID-19
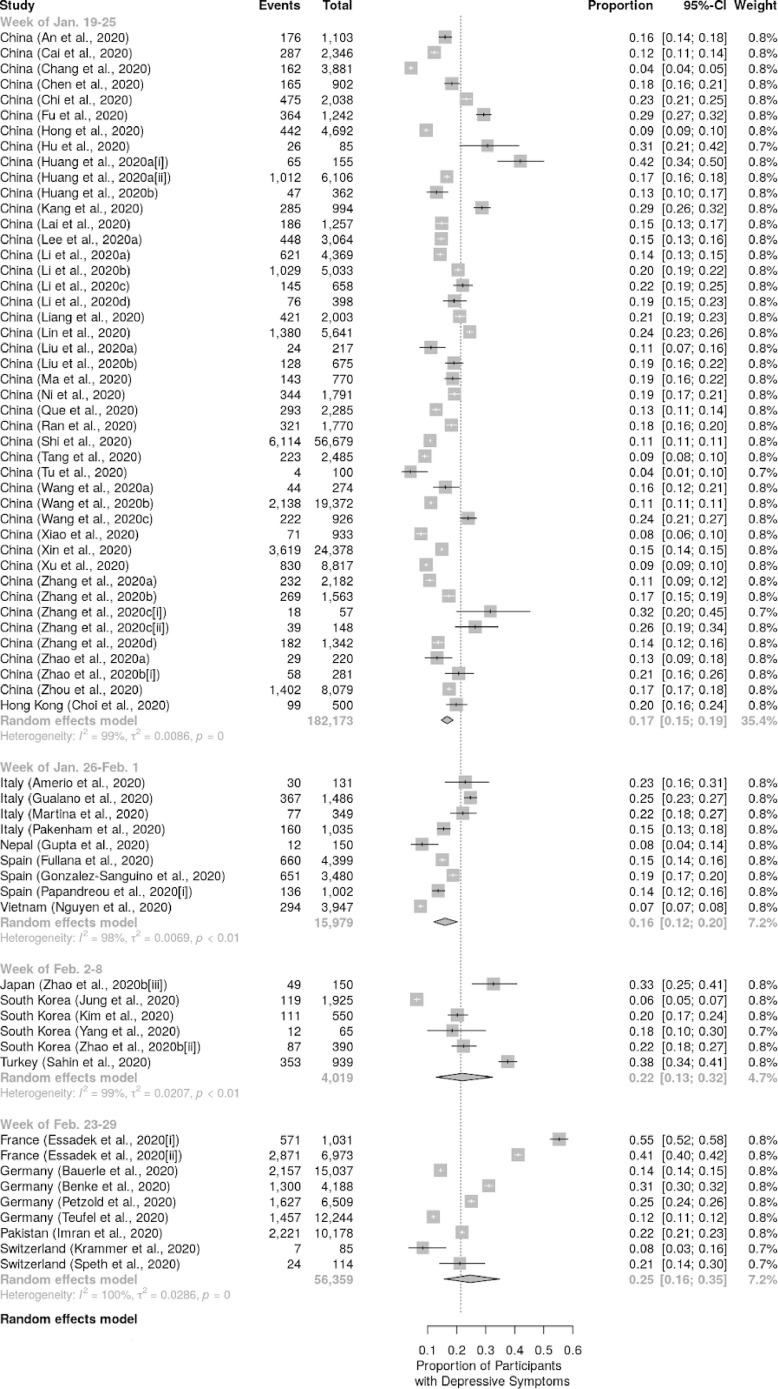
The proportion of study participants meeting criteria for clinically significant depressive symptoms was pooled across 33 countries (k=114, N=640,037). An estimated 21.39% (95% CI 19.37–23.47) of individuals globally had clinically significant depressive symptoms during the COVID-19 pandemic (Fig. 2 ).
Fig. 2.
Forest plot of mean proportion of study participants meeting criteria for clinically significant depressive symptoms using the Patient Health Questionnaire.
We compared the prevalence of clinically significant depressive symptoms across countries using the Human Development Index. The United Nations Development Programme operationalized very high, high, medium, and low Human Development Index values using the thresholds ≥0.892, 0.750, 0.634, 0.507, respectively. Depressive symptom prevalence was higher in countries with a very high Human Development Index (23.52%, 95% CI 20.37–26.82, k=53) and lower in countries with a medium (19.58%, 95% CI 6.67–37.12, k=4) or low Human Development Index (16.69%, 95%CI 1.17–44.44, k=4), relative to countries with a high Human Development Index (20.06%, 95% CI 17.67–22.56, k=64).
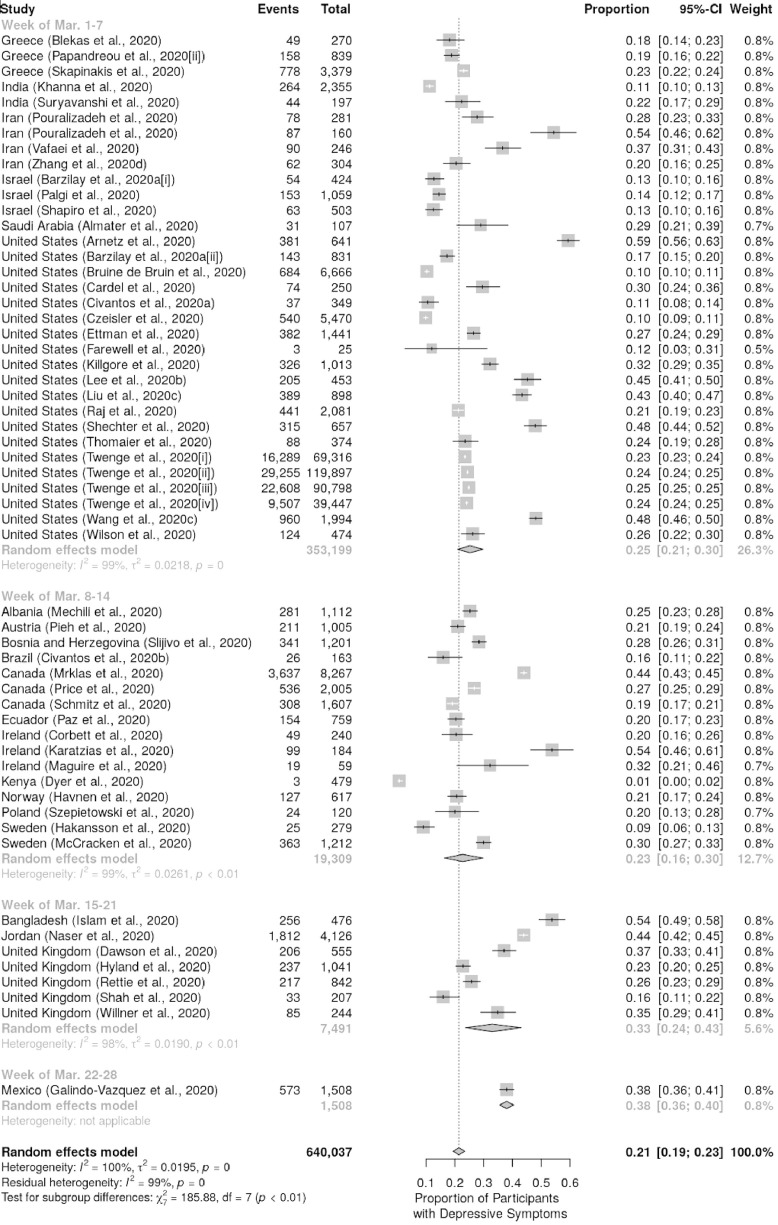
3.2. Government response to COVID-19 moderates depressive symptom prevalence
Studies were pooled by countries and subgrouped by when their governments implemented stringent COVID-19 containment policies (i.e., stringency index of 20 or greater). The prevalence of clinically significant depressive symptoms was significantly lower in countries where governments implemented stringent policies more promptly (Fig. 3 ). The moderating effect of government response was significant after including the national frequency of COVID cases at the time of study commencement, Healthcare Access and Quality index, and the inclusion of COVID patients in the study (Table 1 ). The moderating effect of government response date was significant after removing studies from China in sensitivity analysis (Figure S2).
Fig. 3.
The prevalence of clinically significant depressive symptoms was lower in countries wherein governments implemented stringent lockdown measures at an earlier date. Point size is proportionate to sample size. Abbreviations: CHN, China; HKG, Hong Kong; ITA, Italy; NPL, Nepal; ESP, Spain; VNM, Vietnam; JPN, Japan; KOR, South Korea; TUR, Turkey; FRA, France; DEU, Germany; PAK, Pakistan; CHE, Switzerland; GRC, Greece; IND, India; IRN, Iran; ISR, Israel; SAU, Saudi Arabia; USA, United States; ALB, Albania; AUT, Austria; BIH, Bosnia and Herzegovina; BRA, Brazil; CAN, Canada; ECU, Ecuador; IRL, Ireland; KEN, Kenya; NOR, Norway; POL, Poland; SWE, Sweden; BGD, Bangladesh; JOR, Jordan; GBR, United Kingdom; MEX, Mexico.
Table 1.
Meta-analytic regression results. Studies were pooled by country and subgrouped by date of government response. k=125, QM=66.47, df=7, p<0.001; QE=9485.92, df=117, p<0.001; R2=33.61%.
| Moderator | β | SE | p |
|---|---|---|---|
| Intercept | -57.62 | 13.60 | <0.0001 |
| Government response datea | 0.003 | 0.001 | <0.0001 |
| Study included COVID patientsb | 0.147 | 0.042 | <0.001 |
| National COVID case frequency (ln-transformed)c | 0.020 | 0.005 | <0.0001 |
| Human Development Index rankingd | 0.104 | 0.034 | 0.002 |
| Healthcare Access and Quality index (ln-transformed)e | 0.365 | 0.119 | 0.002 |
| Median stringency indexf | -0.001 | 0.001 | 0.218 |
| Lockdown durationg | 0.0002 | 0.001 | 0.759 |
To compare countries with earlier vs. later lockdown dates, we identified the earliest date in which the country exceeded a stringency index of 20 (denoting a stringent government response to COVID-19).
Studies that included patients who had tested positive for COVID-19 were compared to studies that explicitly excluded patients with COVID-19 or did not report whether study participants had been tested for COVID-19.
For each study, we identified the cumulative count of COVID cases in their country on the first day of the study period; the national case frequency was then ln-transformed.
The United Nations Development Programme ranked countries by Human Development Index in descending order.
The most recent (2016) estimates were extracted for each study and ln-transformed.
The median stringency index was computed for each study for all dates preceding the start date of study.
We estimated the duration of the lockdown in days (up until the study start date) by counting the number of days wherein the stringency index met or exceeded 20.
3.3. Assessment of bias
Study quality was assessed using the revised ROBINS-I tool and the results are summarized in Table 2 . Thirty of 114 studies were assessed as having a moderate overall risk of bias and 84 were rated as having a serious risk of bias. Only eight studies tested study participants for COVID and reported depressive symptom data separately for those with and without COVID; 29 studies asked participants if they had been tested for COVID and reported the percentage of participants who had self-reported a positive COVID test without stratifying depressive symptom data by COVID status. All but three studies assessed at least one confounding variable, such as socio-demographic characteristics (e.g., age, sex, education, income), pre-COVID depression-related data (e.g., mean PHQ score, psychiatric history), and COVID exposure or risk of exposure (e.g., number of cases in participant's municipality or province).
Table 2.
Risk of bias was assessed using the ROBIN-I tool.
| Author | Citation | Confounding | Participant Selection | Intervention Classification | Missing Data | Outcome Measurement | Reporting | Overall Risk-of bias Rating |
|---|---|---|---|---|---|---|---|---|
| Almater | (Almater et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Amerio | (Amerio et al., 2020a) | Low | Moderate | Serious | Low | Moderate | Low | Serious |
| An | (An et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Arnetz | (Arnetz et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Moderate | Serious |
| Barzilay | (Barzilay et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Moderate | Moderate |
| Bauerle | (Bauerle et al., 2020) | Low | Moderate | Serious | Low | Moderate | Low | Serious |
| Benke | (Benke et al., 2020) | Low | Moderate | Serious | Low | Moderate | Serious | Serious |
| Blekas | (Blekas et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Bruine de Bruin | (Bruine de Bruin, 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Cai | (Cai et al., 2020) | Serious | Moderate | Serious | Low | Moderate | Low | Serious |
| Cardel | (Cardel et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Chang | (Chang et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Chen | (Chen et al., 2020) | Low | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Chi | (Chi et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Moderate | Serious |
| Choi | (Choi et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Civantos | (Civantos et al., 2020b) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Civantos | (Civantos et al., 2020a) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Corbett | (Corbett et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Serious | Serious |
| Czeisler | (Czeisler et al., 2020) | Moderate | Low | Serious | Low | Moderate | Low | Serious |
| Dawson | (Dawson and Golijani-Moghaddam, 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Dyer | (Dyer et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Essadek | (Essadek and Rabeyron, 2020) | Low | Moderate | Low | Low | Moderate | Low | Moderate |
| Ettman | (Ettman et al., 2020) | Low | Low | Serious | Low | Moderate | Moderate | Serious |
| Farewell | (Farewell et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Fu | (Fu et al., 2020) | Low | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Fullana | (Fullana et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Moderate | Moderate |
| Galindo-Vazquez | (Galindo-Vázquez et al., 2020) | Low | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Gonzalez-Sanguino | (Gonzalez-Sanguino et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Gualano | (Gualano et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Gupta | (Gupta et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Hakansson | (Håkansson et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Havnen | (Havnen et al., 2020) | Low | Moderate | Serious | Low | Moderate | Low | Serious |
| Hong | (Hong et al., 2020) | Serious | Moderate | Serious | Low | Moderate | Low | Serious |
| Hu | (Hu et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Huang | (J. Huang et al., 2020) | Low | Moderate | Low | Low | Moderate | Low | Moderate |
| Huang | (S. Huang et al., 2020) | Moderate | Serious | Moderate | Low | Moderate | Moderate | Serious |
| Hyland | (Hyland et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Moderate | Serious |
| Imran | ((Imran et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Islam | (Islam et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Jung | (Jung et al., 2020) | Low | Low | Low | Low | Moderate | Low | Moderate |
| Kang | (Kang et al., 2020b) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Karatzias | (Karatzias et al., 2020) | Moderate | Low | Serious | Low | Moderate | Low | Serious |
| Khanna | (Khanna et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Killgore | (Killgore et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Kim | (Kim et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Krammer | (Krammer et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Lai | (Lai et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Lee | (Y. Lee et al., 2020b) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Lee | (S. A. Lee et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Liang | (Liang et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Li | (J. Li et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Li | (G. Li et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Li | (Juanjuan et al., 2020) | Low | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Li | (X. Li et al., 2020) | Low | Moderate | Serious | Low | Moderate | Low | Serious |
| Lin | (L.-Y. Lin et al., 2020) | Moderate | Moderate | Low | Low | Moderate | Low | Serious |
| Liu | (J. Liu et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Liu | (C. H. Liu et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Liu | (D. Liu et al., 2020) | Low | Moderate | Low | Low | Moderate | Moderate | Moderate |
| Ma | (Ma et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Maguire | (Maguire and O'Shea, 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Moderate | Serious |
| Martina | (Martina et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| McCracken | (McCracken et al., 2020) | Low | Moderate | Low | Low | Moderate | Low | Moderate |
| Mechili | (Mechili et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Mrklas | (Mrklas et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Moderate | Serious |
| Naser | (Naser et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Nguyen | (Nguyen et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Ni | (Ni et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Pakenham | (Pakenham et al., 2020) | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Palgi | (Palgi et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Papandreou | (Papandreou et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Serious | Serious |
| Pouralizadeh | (Pouralizadeh et al., 2020) | Low | Moderate | Low | Low | Moderate | Low | Moderate |
| Paz | (Paz et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Petzold | (Petzold et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Pieh | (Pieh et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Price | (Price, 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Que | (Que et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Raj | (Raj et al., 2020) | Low | Moderate | Serious | Low | Moderate | Low | Serious |
| Ran | (Ran et al., 2020) | Moderate | Serious | Serious | Low | Moderate | Low | Serious |
| Rettie | (Rettie and Daniels, 2020) | Low | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Sahin | (Şahin et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Schmitz | (Schmitz et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Shah | (Shah et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Moderate | Serious |
| Shapiro | (Shapiro et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Shechter | (Shechter et al., 2020) | Low | Moderate | Serious | Low | Moderate | Low | Serious |
| Shi | (Shi et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Skapinakis | (Skapinakis et al., 2020) | Low | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Sljivo | (Sljivo, 2020) | Moderate | Serious | Moderate | Low | Moderate | Low | Serious |
| Speth | (Speth et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Suryavanshi | (Suryavanshi et al., 2020) | Low | Moderate | Serious | Low | Moderate | Low | Serious |
| Szepietowski | (Szepietowski et al., 2020) | Low | Moderate | Serious | Moderate | Moderate | Serious | Serious |
| Tang | (Tang et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Teufel | (Teufel et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Thomaier | (Thomaier et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Serious | Serious |
| Tu | (Tu et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Twenge | (Twenge and Joiner, 2020) | Moderate | Low | Serious | Low | Moderate | Low | Serious |
| Vafaei | ( Vafaei et al., 2020) | Moderate | Moderate | Serious | Moderate | Moderate | Low | Serious |
| Wang | (L.-Q. Wang et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Moderate | Serious |
| Wang | (X. Wang et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Wang | (S. Wang et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Wang | (Q. Wang et al., 2020) | Serious | Moderate | Serious | Low | Moderate | Low | Serious |
| Willner | (Willner et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Moderate | Serious |
| Wilson | (Wilson et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Xiao | (Xiao et al., 2020) | Moderate | Moderate | Serious | Low | Moderate | Low | Serious |
| Xin | (Xin et al., 2020) | Moderate | Serious | Moderate | Low | Low | Low | Serious |
| Xu | (Xiaoming et al., 2020) | Low | Moderate | Serious | Low | Moderate | Low | Serious |
| Yang | (Yang et al., 2020) | Moderate | Serious | Moderate | Low | Low | Low | Serious |
| Zhang | (W.-R. Zhang et al., 2020) | Moderate | Serious | Serious | Low | Moderate | Low | Serious |
| Zhang | (Zhang et al., 2021) | Moderate | Serious | Serious | Low | Low | Low | Serious |
| Zhang | (J. Zhang et al., 2020) | Moderate | Low | Low | Low | Low | Low | Moderate |
| Zhang | (S. X. Zhang et al., 2020) | Moderate | Serious | Moderate | Moderate | Moderate | Serious | Serious |
| Zhang | (W. Zhang et al., 2020) | Moderate | Serious | Serious | Low | Moderate | Moderate | Serious |
| Zhao | (R. Zhao et al., 2020) | Moderate | Serious | Serious | Low | Moderate | Low | Serious |
| Zhao | (B. Zhao et al., 2020) | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Zhou | (Zhou et al., 2020) | Moderate | Low | Serious | Low | Low | Low | Serious |
A study that measured and included in its analysis at least one confounding variable was rated as having a low risk of confounding bias; a study that measured but did not include in its analysis at least one confounding variable was rated as having a moderate risk of confounding bias. A study was considered to have moderate risk of selection bias if it excluded individuals with a history of psychiatric diagnoses or was delimited to a particular demographic (e.g., college students, elderly, healthcare workers). A study was assessed as having a low risk of selection bias if it recruited a nationally representative sample. Studies that reported COVID diagnoses (self-reported or as assessed by study personnel) and subgrouped participants by COVID status were rated as having a low risk of bias on the intervention classification domain. Studies that did not report their results separately for participants who had tested positive and participants who had tested negative (or were not tested) received a moderate rating. Studies that did not ask participants about COVID diagnoses were judged as having a serious risk of intervention classification bias.
A study received a low risk of missing data bias unless it failed to report the study start date, study end date or duration, or the cut-off score used to identify cases with clinically significant depressive symptoms (in which case it received a moderate rating). A study received a serious risk of outcome measurement bias if it used different scales or modes of scale administration between study subpopulations or a moderate rating if participants or outcome assessors were unblinded to study outcomes of interest. Non-refereed publications and studies that omitted analyses mentioned in their methods were rated as having moderate risk of reporting bias. Studies that failed to report the analysis sample size were rated as having a serious risk of reporting bias.
Trim and fill did not add any studies (Figure S3). The funnel plot was symmetric and the Egger's and Begg's tests were not significant (Egger's: slope=0.470, p=0.885; Begg's: p=0.105).
4. Discussion
Our systematic review compared the timeliness of government response to COVID-19 across 33 countries and its impact on clinically significant depressive symptoms spanning high-, middle-, and low-income countries. We observed a global depressive symptom prevalence of 21.4% during the COVID-19 pandemic, which is higher than what was observed before the COVID-19 pandemic. For example, a meta-analysis evaluating depression prevalence across 30 countries between 1994 and 2014 reported an aggregate point prevalence of 12.9% (95% CI: 11.1–15.1%, k=90, n=1,112,573) (Lim et al., 2018). Moreover, depressive symptom prevalence was higher in countries with higher Human Development Index values, which contrasts the observation of lower depression prevalence in more developed countries before the COVID-19 pandemic (i.e., 9.8% for very high, 19.2% for high, 29.2% for medium, 11.5% for low Human Development Index) (Lim et al., 2018). Our results replicate accumulating studies reporting increases in depression prevalence during the pandemic.
Moreover, in our meta-analysis, countries that waited to implement stringent lockdown measures evinced a higher prevalence of clinically significant depressive symptoms when compared to countries that implemented stringent lockdown measures sooner. The foregoing moderating effect was significant after adjusting for the total number of COVID-19 cases, access to high-quality healthcare, and the inclusion of COVID-19 patients as study participants. Our findings replicate and extend literature indicating that a rapid public health response is a critical determinant of protecting the mental wellbeing of the general population (Felton, 2002; Kinsman, 2012).
Governments that enacted stringent measures to contain the spread of COVID-19 not only benefited the physical health of their population, but also their mental health, in our meta-analysis. During the 1918 pandemic, swift and timely implementation of social gathering bans and quarantine measures predicted lower mortality rates; American cities that implemented delayed lockdown measures after death rates began to accelerate suffered the highest mortality rates (Bootsma and Ferguson, 2007; Markel et al., 2007). We hypothesized that, in addition to increasing infection-mortality rates, delays in implementing stringent containment measures would result in greater psychiatric morbidity during the present public health crisis.
A swift and stringent government response may reduce mental and emotional distress by augmenting certainty and resilience against uncertainty. Similarly, greater trust in the government and the national public health response has been associated with lower depressive symptom severity (O'Hara et al., 2020; Tee et al., 2020). Uncertainty is malignant: chronic and unpredictable stress provokes psychological distress and begets anxiety and depressive disorders (Bakioglu et al., 2020).
The COVID-19 pandemic can be conceptualized as a pandemic of uncertainty (e.g., infectious disease risk, economic security, and social life). Individuals are additionally struggling to identify trustworthy sources of information (Larson, 2018; Moran, 2020; World Health Organization, 2020). Vulnerable subpopulations (e.g., immigrant or ethnic communities, low literacy or educational attainment) may additionally lack critical health information from government sources (Le et al., 2020). Thus, public health interventions that reduce entropy and exact certitude (i.e., mitigate helplessness) can be hypothesized to reassure citizens and support their mental wellbeing (C. Wang et al., 2020).
However, there exist individuals, within the plurality of the populace, who have not benefited from stringent containment measures (Adam et al., 2021; Amerio et al., 2020b; Mukherjee, 2020; Yi et al., 2020). For example, aggregate community mobility data indicate that high income-earners with greater job security and flexibility were better able to shelter in place than were low income-earners (Bonaccorsi et al., 2020; Srivastava, 2020; Valentino-DeVries et al., 2020). Inadequate workplace support (e.g., lack of personal protective equipment, awareness of mental health needs) may additionally detriment mental wellbeing (Giorgi et al., 2020; Kang et al., 2020a; Pollock et al., 2020; Y.-X. Wang et al., 2020). Moreover, the negative externalities of stringent lockdown policies disproportionately affect vulnerable populations (e.g., health insurance loss due to unemployment, intimate partner violence, low-income households, migrant workers, racialized communities) (Hamadani et al., 2020; Noel et al., 2020; Raj et al., 2020; Simmons-Duffin, 2020).
Similar inequities exist on a global level: a cross-sectional study of 37,696 households in 30 African countries reported that 52% of households in urban areas had access to safe drinking water, sanitation, and electricity, whereas only 12% of households in rural regions had access to the foregoing basic resources (Egger et al., 2020). Only 12% of urban households and 2% of rural households with access to basic resources reported having a stable income source and telephone access (Egger et al., 2020). The United Nations’ Global Report on Food Crises estimates that the economic impact of COVID-19 will push an additional 130 million individuals in low- and middle-income countries into acute food insecurity in 2020 (“United Nations World Food Programme, 2020 - Global Report on Food Crises,” 2020).
4.1. Limitations
We were unable to assess the potential confounding effect of the length of study period as several included studies did not report the study end date or length of the study period. We were also unable to assess differences in duration of lockdown measures across countries and how these differences may moderate depression prevalence. Most of the included studies used convenience or snowball sampling to recruit study participants, rather than a stratified or random sampling method typically used to derive nationally representative study populations, limiting the generalizability of our results. We evaluated the point prevalence of depression, rather than the incidence of new-onset depression, as pre-COVID-19 data were not reported by the vast majority of included studies. Most studies used a well-established cut-off score using a validated and standardized metric of depressive symptom severity with sensitivity and specificity to detect clinical cases of depression; notwithstanding, individuals meeting or exceeding the threshold for moderate-to-severe depressive symptom severity may not meet clinical diagnostic criteria for major depressive disorder. Moreover, our results may be confounded by the lack of study participant and outcome assessor blinding, as well as the retrospective assessment of depressive symptom severity.
5. Conclusions
Taken together, our results underscore the need for governments formulating policy interventions to include the mental health community and representatives of vulnerable populations during the development process. A future study should evaluate how the duration of stringent lockdown measures moderate the incidence of depression due to COVID-19 using nationally representative data.
MeSH keywords: Depression; Depressive Disorder; Public Health; Population Health; Social Medicine; Global Health; Public Policy; Pandemics; Coronavirus Infections; Pandemics / prevention & control*; Humans; Meta-Analysis; Systematic Reviews
Supplementary concepts: COVID-19; severe acute respiratory syndrome coronavirus 2
Summary
The COVID-19 pandemic represents a public health, economic and mental health crisis. We hypothesized that timely government implementation of stringent measures to reduce viral transmission would benefit mental health, as evidenced by reduced rates of depressive symptoms (i.e., Patient Health Questionnaire [PHQ]-9≥10, PHQ-2≥3). The systematic review herein (PROSPERO CRD42020200647) evaluated to what extent differences in the government-imposed stringency and timeliness of response to COVID-19 moderate the prevalence of depressive symptoms across 33 countries (k=114, N=640,037). We included data from six lower-middle-income countries, nine upper-middle-income countries, and 18 higher-income countries.
The overall proportion of study participants with clinically significant depressive symptoms was 21.39% (95% CI 19.37–23.47). The prevalence of clinically significant depressive symptoms was significantly lower in countries wherein governments implemented stringent policies promptly. The moderating effect of government response remained significant after including the national frequency of COVID cases at the time of study commencement, Healthcare Access and Quality index, and the inclusion of COVID patients in the study. Government-imposed stringency and timeliness in response were operationalized using the Oxford COVID-19 Government Response (“Stringency”) Index.
The World Health Organization defines health as physical and mental health, as well as social wellbeing. Governments that enacted stringent measures to contain the spread of COVID-19 benefited, not only the physical health, but also mental health of their population.
Author statement
All authors have approved the final manuscript and note that this is our original work. The article is not under review with any other journal or publication. The authors’ conflicts of interest have been provided.
Author contributions
YL conceptualized the Article. YL, LMWL, DC-L reviewed articles and collected data. YL ran the analysis. YL and LMWL wrote the first draft of the Article and revised it based on feedback from co-authors. All authors reviewed and approved the Article.
Funding
This study received no funding.
Data sharing
Data collected for the meta-analysis, including individual study data and a data dictionary defining each field in the set, will be made available to others upon publication of the meta-analysis herein. The standardized data collection form and individual study data used in the analysis herein will be published online via a public repository (Mendeley DOI). The study protocol is available online (PROSPERO CRD42020200647).
Declaration of Competing Interest
Author YL received salary support from the Global Alliance for Chronic Diseases/Canadian Institutes of Health Research (CIHR)/National Natural Science Foundation of China's Mental Health Team Grant and the CIHR Frederick Banting and Charles Best Canada Graduate Scholarship; personal fees from Braxia Scientific Corp. Author RSM received research grant support from Global Alliance for Chronic Diseases/Canadian Institutes of Health Research (CIHR)/National Natural Science Foundation of China’s Mental Health Team Grant; speaker/consultation fees from Lundbeck, Janssen, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Novo Nordisk, Kris, Sanofi, Eisai ,Intra-Cellular, NewBridge Pharmaceuticals, Abbvie. Author RSM is a CEO of Braxia Scientific Corp. Author EB reports research grant support from Faculty of Health Sciences, Queen's University; Department of Psychiatry, Queen's University, SEAMO, CNPq and FAPESP; reports speaker/consultation fees from Daiichi-Sankyo. Author JDR is the medical director of the Braxia Health (formally known as the Canadian Rapid Treatment Center of Excellence and is a fully owned subsidiary of Braxia Scientific Corp) which provides ketamine and esketamine treatment for depression; he has received research grant support from the American Psychiatric Association, the American Society of Psychopharmacology, the Canadian Cancer Society, the Canadian Psychiatric Association, the Joseph M. West Family Memorial Fund, the Timeposters Fellowship, the University Health Network Centre for Mental Health, and the University of Toronto and speaking, consultation, or research fees from Allergan, COMPASS, Janssen, Lundbeck, and Sunovion. Authors LMWL, DC-L, YL, RBM, RH, NBR, OL, FN, BC, MS, HG, and CL declare no competing interests.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.04.050.
Appendix. Supplementary materials
References
- 2020- Global Report on Food Crises [WWW Document], 2020. URL https://www.wfp.org/publications/2020-global-report-food-crises (accessed 9.29.20).
- Adam C., Henstridge M., Lee S. After the lockdown: macroeconomic adjustment to the COVID-19 pandemic in sub-Saharan Africa. Oxf Rev Econ Policy. 2021 doi: 10.1093/oxrep/graa023. [DOI] [Google Scholar]
- Almater A.I., Tobaigy M.F., Younis A.S., Alaqeel M.K., Abouammoh M.A. Effect of 2019 Coronavirus Pandemic on Ophthalmologists Practicing in Saudi Arabia: A Psychological Health Assessment. Middle East Afr. J. Ophthalmol. 2020;27:79–85. doi: 10.4103/meajo.MEAJO_220_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amerio A., Bianchi D., Santi F., Costantini L., Odone A., Signorelli C., Costanza A., Serafini G., Amore M., Aguglia A. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed. 2020;91:83–88. doi: 10.23750/abm.v91i2.9619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amerio A., Brambilla A., Morganti A., Aguglia A., Bianchi D., Santi F., Costantini L., Odone A., Costanza A., Signorelli C., Serafini G., Amore M., Capolongo S. COVID-19 Lockdown: Housing Built Environment's Effects on Mental Health. Int J Environ Res Public Health. 2020 doi: 10.3390/ijerph17165973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An Y., Yang Y., Wang A., Li Y., Zhang Q., Cheung T., Ungvari G.S., Qin M.-Z., An F.-R., Xiang Y.-T. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J. Affect. Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnetz J.E., Goetz C.M., Sudan S., Arble E., Janisse J., Arnetz B.B. Personal protective equipment and mental health symptoms among nurses during the COVID-19 Pandemic. J. Occup. Environ. Med. 2020 doi: 10.1097/JOM.0000000000001999. [DOI] [PubMed] [Google Scholar]
- Bakioglu F., Korkmaz O., Ercan H. Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int. J. Ment. Health Addict. 2020:1–14. doi: 10.1007/s11469-020-00331-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balduzzi S., Rücker G., Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid. Based. Ment. Health. 2019;22:153–160. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barzilay R., Moore T.M., Greenberg D.M., DiDomenico G.E., Brown L.A., White L.K., Gur R.C., Gur R.E. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl. Psychiatry. 2020;10:291. doi: 10.1038/s41398-020-00982-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauerle A., Teufel M., Musche V., Weismuller B., Kohler H., Hetkamp M., Dorrie N., Schweda A., Skoda E.-M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health. 2020 doi: 10.1093/pubmed/fdaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- Benke C., Autenrieth L.K., Asselmann E., Pané-Farré C.A. Stay-at-home orders due to the COVID-19 pandemic are associated with elevated depression and anxiety in younger, but not older adults: results from a nationwide community sample of adults from Germany. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720003438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blekas A., Voitsidis P., Athanasiadou M., Parlapani E., Chatzigeorgiou A.F., Skoupra M., Syngelakis M., Holeva V., Diakogiannis I. COVID-19: PTSD symptoms in Greek health care professionals. Psychol. Trauma. 2020;12:812–819. doi: 10.1037/tra0000914. [DOI] [PubMed] [Google Scholar]
- Bonaccorsi G., Pierri F., Cinelli M., Flori A., Galeazzi A., Porcelli F., Schmidt A.L., Valensise C.M., Scala A., Quattrociocchi W., Pammolli F. Economic and social consequences of human mobility restrictions under COVID-19. Proc. Natl. Acad. Sci. U. S. A. 2020;117:15530–15535. doi: 10.1073/pnas.2007658117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bootsma M.C.J., Ferguson N.M. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc. Natl. Acad. Sci. U. S. A. 2007;104:7588–7593. doi: 10.1073/pnas.0611071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health:Evidence from a national US survey conducted in March 2020. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020 doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q., Feng H., Huang J., Wang M., Wang Q., Lu X., Xie Y., Wang X., Liu Z., Hou B., Ouyang K., Pan J., Li Q., Fu B., Deng Y., Liu Y. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J. Affect. Disord. 2020;275:210–215. doi: 10.1016/j.jad.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardel M.I., Manasse S., Krukowski R.A., Ross K., Shakour R., Miller D.R., Lemas D.J., Hong Y. COVID-19 impacts mental health outcomes and ability/desire to participate in research among current research participants. Obesity. 2020 doi: 10.1002/oby.23016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J., Yuan Y., Wang D. [Mental health status and its influencing factors among college students during the epidemic of COVID-19] Nan Fang Yi Ke Da Xue Xue Bao. 2020;40:171–176. doi: 10.12122/j.issn.1673-4254.2020.02.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Liu X., Wang D., Jin Y., He M., Ma Y., Zhao X., Song S., Zhang L., Xiang X., Yang L., Song J., Bai T., Hou X. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc. Psychiatry Psychiatr. Epidemiol. 2020 doi: 10.1007/s00127-020-01954-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirico F., Nucera G., Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych Int. 2021;18:1–2. doi: 10.1192/bji.2020.39. [DOI] [Google Scholar]
- Chi X., Becker B., Yu Q., Willeit P., Jiao C., Huang L., Mahhub Hossain M., Grabovac I., Yeung A., Lin J., Veronese N., Wang J., Zhou X., Doig S.R., Liu X., Carvalho A.F., Yang L., Xiao T., Zou L., Fusar-Poli P., Solmi M. Prevalence and psychosocial correlates of mental health outcomes among Chinese College Students During the Coronavirus Disease (COVID-19) pandemic. Frontiers in Psychiatry. 2020 doi: 10.3389/fpsyt.2020.00803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi E.P.H., Hui B.P.H., Wan E.Y.F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civantos A.M., Bertelli A., Gonçalves A., Getzen E., Chang C., Long Q., Rajasekaran K. Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: a national study. Am. J. Otolaryngol. 2020;41 doi: 10.1016/j.amjoto.2020.102694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civantos A.M., Byrnes Y., Chang C., Prasad A., Chorath K., Poonia S.K., Jenks C.M., Bur A.M., Thakkar P., Graboyes E.M., Seth R., Trosman S., Wong A., Laitman B.M., Harris B.N., Shah J., Stubbs V., Choby G., Long Q., Rassekh C.H., Thaler E., Rajasekaran K. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head Neck. 2020;42:1597–1609. doi: 10.1002/hed.26292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett G.A., Milne S.J., Mohan S., Reagu S., Farrell T., Lindow S.W., Hehir M.P., O'Connell M.P. Anxiety and Depression Scores in Maternity Healthcare Workers during the Covid-19 Pandemic. Int. J. Gynaecol. Obstet. 2020 doi: 10.1002/ijgo.13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR. Morb Mort Wkly Rep. 2020 doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D.L., Golijani-Moghaddam N. COVID-19: psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. J Contextual Behav Sci. 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Sousa A., Mohandas E., Javed A. Psychological interventions during COVID-19: challenges for low and middle income countries. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S., Tweedie R. A nonparametric “Trim and Fill” method of accounting for publication bias in meta-analysis. J. Am. Stat. Assoc., doctoral dissertation. 2000;95:89–98. doi: 10.1080/01621459.2000.10473905. [DOI] [Google Scholar]
- Dyer J., Wilson K., Badia J., Agot K., Neary J., Njuguna I., Kibugi J., Healy E., Beima-Sofie K., John-Stewart G., Kohler P. The psychosocial effects of the COVID-19 pandemic on youth living with HIV in Western Kenya. AIDS Behav. 2020 doi: 10.1007/s10461-020-03005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger E.-M., Jones S., Justino P., Manhique I., Santos R. Africa's lockdown dilemma: high poverty and low trust. WIDER Working Paper. UNU-WIDER. 2020 doi: 10.35188/UNU-WIDER/2020/833-7. [DOI] [Google Scholar]
- Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essadek A., Rabeyron T. Mental health of French students during the Covid-19 pandemic. J. Affect. Disord. 2020;277:392–393. doi: 10.1016/j.jad.2020.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19686. e2019686–e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farewell C.V., Jewell J., Walls J., Leiferman J.A. A mixed-methods pilot study of perinatal risk and resilience during COVID-19. J. Prim. Care Community Health. 2020;11 doi: 10.1177/2150132720944074. 2150132720944074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felton C.J. Project Liberty: a public health response to New Yorkers’ mental health needs arising from the World Trade Center terrorist attacks. J. Urban Health. 2002;79:429–433. doi: 10.1093/jurban/79.3.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco E.G., Schwab K, Brende B, Dusek M, Howell L, Kastner A, Kuritzky M, Lukacs R, Shetler-Jones P, Cann O, Elci A, Farnworth E, Islam S.T., Breitinger D, Pickens A, Swanborough J, Albani M, Khatri A, Quinney M, Pope K.N., Bosco F, Jordan A, Krieger Z, Lewis R, Ogee A, Philbeck T, Pipikaite A, Uzunova A. The Global Risks Report. World Economic Forum. 2020 [Google Scholar]
- Freeman M.F., Tukey J.W. Transformations related to the angular and the square root. Ann. Math. Stat. 1950;21:607–611. [Google Scholar]
- Fullana M.A., Hidalgo-Mazzei D., Vieta E., Radua J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020;275:80–81. doi: 10.1016/j.jad.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu W., Wang C., Zou L., Guo Y., Lu Z., Yan S., Mao J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan. China. Transl. Psychiatry. 2020;10:225. doi: 10.1038/s41398-020-00913-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galindo-Vázquez O., Ramírez-Orozco M., Costas-Muñiz R., Mendoza-Contreras L.A., Calderillo-Ruíz G., Meneses-García A. Symptoms of anxiety, depression and self-care behaviors during the COVID-19 pandemic in the general population. Gac. Med. Mex. 2020;156:298–305. doi: 10.24875/GMM.20000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2016 Healthcare Access and Quality Collaborators Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391:2236–2271. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giorgi G., Lecca L.I., Alessio F., Finstad G.L., Bondanini G., Lulli L.G., Arcangeli G., Mucci N. COVID-19-related mental health effects in the workplace: a narrative review. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17217857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Sanguino C., Ausin B., Castellanos M.A., Saiz J., Lopez-Gomez A., Ugidos C., Munoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A.K., Mehra A., Niraula A., Kafle K., Deo S.P., Singh B., Sahoo S., Grover S. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID-19 pandemic. Asian J. Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Håkansson A., Jönsson C., Kenttä G. Psychological Distress and Problem Gambling in Elite Athletes during COVID-19 Restrictions—A Web Survey in Top Leagues of Three Sports during the Pandemic. Int. J. Environ. Res. Public Health. 2020;17:6693. doi: 10.3390/ijerph17186693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale, T., Atav, T., Hallas, L., Kira, B., Phillips, T., Petherick, A., Pott, A., 2020. Coronavirus Government Response Tracker. Variation in US states’ responses to COVID-19.
- Hamadani J.D., Hasan M.I., Baldi A.J., Hossain S.J., Shiraji S., Bhuiyan M.S.A., Mehrin S.F., Fisher J., Tofail F., Tipu S.M.M.U., Grantham-McGregor S., Biggs B.-A., Braat S., Pasricha S.-R. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health. 2020 doi: 10.1016/S2214-109X(20)30366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havnen A., Anyan F., Hjemdal O., Solem S., Gurigard Riksfjord M., Hagen K. Resilience moderates negative outcome from stress during the COVID-19 pandemic: a moderated-mediation approach. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17186461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane; 2019. Cochrane Handbook for Systematic Reviews of Interventions version 6.0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver Cohen, R. Everall, I. Ford, T. John, A. Kabir, T. King, K. Madan, I. Michie, S. Przybylski, A.K. Shafran, R. Sweeney, A. Worthman, C.M. Yardley, L. Cowan, K. Cope, C. Hotopf, M. Bullmore, E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong S., Ai M., Xu X., Wang W., Chen J., Zhang Q., Wang L., Kuang L. Immediate psychological impact on nurses working at 42 government-designated hospitals during COVID-19 outbreak in China: a cross-sectional study. Nurs. Outlook. 2020 doi: 10.1016/j.outlook.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W.K., Lai F.T., Ben-Ezra M., Goodwin R. Regularizing daily routines for mental health during and after the COVID-19 pandemic. J. Glob. Health. 2020;10 doi: 10.7189/jogh.10.020315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W.K., Liu H., Liang L., Ho J., Kim H., Seong E., Bonanno G.A., Hobfoll S.E., Hall B.J. Everyday life experiences and mental health among conflict-affected forced migrants: A meta-analysis. J. Affect. Disord. 2020;264:50–68. doi: 10.1016/j.jad.2019.11.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Liu F., Teng Z., Chen J., Zhao J., Wang X., Wu Y., Xiao J., Wang Y., Wu R. Public Behavior Change, Perceptions, Depression, and Anxiety in Relation to the COVID-19 Outbreak. Open Forum Infect Dis. 2020;7:ofaa273. doi: 10.1093/ofid/ofaa273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, S., Wu, C., Jia, Y., Li, G., Zhu, Z., Lu, K., Yang, Y., Wang, F., Zhu, S., 2020. COVID-19 outbreak: the impact of stress on seizures in patients with epilepsy. Epilepsia n/a. https://doi.org/10.1111/epi.16635. [DOI] [PMC free article] [PubMed]
- Hu Y., Chen Y., Zheng Y., You C., Tan J., Hu L., Zhang Z., Ding L. Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., Martinez A., Vallières F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020 doi: 10.1111/acps.13219. [DOI] [PubMed] [Google Scholar]
- IASC Reference Group on Mental Health and Psychosocial Support in Emergency Settings . Inter-Agency Standing Committee; 2020. Interim Briefing Note Addressing Mental Health and Psychosocial Aspects of COVID-19 Outbreak [WWW Document]https://interagencystandingcommittee.org/system/files/2020-11/IASC%20Interim%20Briefing%20Note%20on%20COVID-19%20Outbreak%20Readiness%20and%20Response%20Operations%20-%20MHPSS_3.pdf URL. accessed 3.4.21. [Google Scholar]
- Ibrahim S., Hunt I.M., Rahman M.S., Shaw J., Appleby L., Kapur N. Recession, recovery and suicide in mental health patients in England: time trend analysis. Br. J. Psychiatry. 2019:1–7. doi: 10.1192/bjp.2019.119. [DOI] [PubMed] [Google Scholar]
- Imran N., Masood H.M.U., Ayub M., Gondal K.M. Psychological impact of COVID-19 pandemic on postgraduate trainees: a cross-sectional survey. Postgrad. Med. J. 2020 doi: 10.1136/postgradmedj-2020-138364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M.A., Barna S.D., Raihan H., Khan M.N.A., Hossain M.T. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juanjuan L., Santa-Maria C.A., Hongfang F., Lingcheng W., Pengcheng Z., Yuanbing X., Yuyan T., Zhongchun L., Bo D., Meng L., Qingfeng Y., Feng Y., Yi T., Shengrong S., Xingrui L., Chuang C. Patient-reported outcomes of patients with breast cancer during the COVID-19 outbreak in the epicenter of China: a cross-sectional survey study. Clin. Breast Cancer. 2020;20:e651–e662. doi: 10.1016/j.clbc.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, S.J., Yang, J.S., Jeon, Y.J., Kim, K., Yoon, J.-H., Lori, C., Koenen, K.C., Kim, H.C., 2020. The Impact of COVID-19 on Psychological Health in Korea: A Mental Health Survey in Community Prospective Cohort Data. https://doi.org/10.2139/ssrn.3618193.
- Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., Wang Y., Hu J., Lai J., Ma X., Chen J., Guan L., Wang G., Ma H., Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., Yao L., Bai H., Cai Z., Xiang Yang B., Hu S., Zhang K., Wang G., Ma C., Liu Z. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav. Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias T., Shevlin M., Murphy J., McBride O., Ben-Ezra M., Bentall R.P., Vallieres F., Hyland P. Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: a population-based study. J. Trauma. Stress. 2020 doi: 10.1002/jts.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna R., Honavar S., Metla A., Bhattacharya A., Maulik P. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian J. Ophthalmol. 2020;68:994. doi: 10.4103/ijo.IJO_1458_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Research. 2020 doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y.-J., Cho J.-H., Kim E.-S. Differences in sense of belonging, pride, and mental health in the Daegu metropolitan region due to COVID-19: comparison between the presence and absence of national disaster relief fund. Int. J. Environ. Res. Public Health. 2020;17:4910. doi: 10.3390/ijerph17134910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsman J. A time of fear”: local, national, and international responses to a large Ebola outbreak in Uganda. Global. Health. 2012;8:15. doi: 10.1186/1744-8603-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krammer S., Augstburger R., Haeck M., Maercker A. [Adjustment Disorder, Depression, Stress Symptoms, Corona Related Anxieties and Coping Strategies during the Corona Pandemic (COVID-19) in Swiss Medical Staff] Psychother. Psychosom. Med. Psychol. 2020;70:272–282. doi: 10.1055/a-1192-6608. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson H.J. The biggest pandemic risk? Viral misinformation. Nature. 2018;562:309. doi: 10.1038/d41586-018-07034-4. [DOI] [PubMed] [Google Scholar]
- Lee S.A., Jobe M.C., Mathis A.A., Gibbons J.A. Incremental validity of coronaphobia: Coronavirus anxiety explains depression, generalized anxiety, and death anxiety. J. Anxiety Disord. 2020;74 doi: 10.1016/j.janxdis.2020.102268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y., Brietzke E., Cao B., Chen Y., Linnaranta O., Mansur R.B., Cortes P., Kösters M., Majeed A., Tamura J.K., Lui L.M.W., Vinberg M., Keinänen J., Kisely S., Naveed S., Barbui C., Parker G., Owolabi M., Nishi D., Lee J., Srisurapanont M., Gill H., Guo L., Balanzá-Martínez V., Partonen T., Nolen W.A., Lee J.-H., Kim J.H., Chavannes N.H., Ewais T., Atienza-Carbonell B., Silven A.V., Yasuma N., Gil A., Novikov A., Lacey C., Versluis A., von Malortie S., Chan L.F., Waqas A., Purgato M., Aardoom J.J., Ly-Uson J.T., Sim K., Tuineag M., van der Kleij R.M.J.J., van Luenen S., Suttajit S., Hajek T., Lee Y.W., Porter R.J., Alsuwaidan M., Rosenblat J.D., Ravindran A.V., Lam R.W., McIntyre R.S. Development and implementation of guidelines for the management of depression: a systematic review. Bull. World Health Organ. 2020;98:683–697H. doi: 10.2471/BLT.20.251405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y., Yang B.X., Liu Q., Luo D., Kang L., Yang F., Ma S., Lu W., Chen-Li D., Rosenblat J.D., Mansur R.B., Nasri F., Subramaniapillai M., Liu Z., McIntyre R.S., Lin K. The synergistic effect of social media use and psychological distress on depression in China during the COVID-19 epidemic. Psychiatry Clin. Neurosci. 2020 doi: 10.1111/pcn.13101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le H.T., Nguyen D.N., Beydoun A.S., Le X.T.T., Nguyen T.T., Pham Q.T., Ta N.T.K., Nguyen Q.T., Nguyen A.N., Hoang M.T., Vu L.G., Tran B.X., Latkin C.A., Ho C.S.H., Ho R.C.M. Demand for Health Information on COVID-19 among Vietnamese. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17124377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Y., Wu K., Zhou Y., Huang X., Zhou Y., Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17186550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., Miao J., Wang H., Xu S., Sun W., Fan Y., Zhang C., Zhu S., Zhu Z., Wang W. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J. Neurol. Neurosurg. Psychiatry. 2020;91:895–897. doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J., Li K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. 2020;19:249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim G.Y., Tam W.W., Lu Y., Ho C.S., Zhang M.W., Ho R.C. Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci. Rep. 2018;8:2861. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin K., Yang B.X., Luo D., Liu Q., Ma S., Huang R., Lu W., Majeed A., Lee Y., Lui L.M.W., Mansur R.B., Nasri F., Subramaniapillai M., Rosenblat J.D., Liu Z., McIntyre R.S. The Mental Health Effects of COVID-19 on Health Care Providers in China. Am. J. Psychiatry. 2020;177:635–636. doi: 10.1176/appi.ajp.2020.20040374. [DOI] [PubMed] [Google Scholar]
- Lin L.-Y., Wang J., Ou-Yang X.-Y., Miao Q., Chen R., Liang F.-X., Zhang Y.-P., Tang Q., Wang T. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Baumeister R.F., Veilleux J.C., Chen C., Liu W., Yue Y., Zhang S. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhu Q., Fan W., Makamure J., Zheng C., Wang J. Online Mental Health Survey in a Medical College in China During the COVID-19 Outbreak. Front. Psychiatry. 2020;11:459. doi: 10.3389/fpsyt.2020.00459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Lu P., Hu L., Huang T., Lu L. Factors Associated with Mental Health Results among Workers with Income Losses Exposed to COVID-19 in China. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17155627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguire S., O'Shea F. Social isolation due to the COVID-19 pandemic has led to worse outcomes in females with inflammatory arthritis. Ir. J. Med. Sci. 2020:1–6. doi: 10.1007/s11845-020-02307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manea L., Gilbody S., McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184:E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markel H., Lipman H.B., Navarro J.A., Sloan A., Michalsen J.R., Stern A.M., Cetron M.S. Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic. JAMA. 2007;298:644–654. doi: 10.1001/jama.298.6.644. [DOI] [PubMed] [Google Scholar]
- Martina S., Amato A., Rongo R., Caggiano M., Amato M. The Perception of COVID-19 among Italian Dentists: An Orthodontic Point of View. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17124384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y.-F., Li W., Deng H.-B., Wang L., Wang Y., Wang P.-H., Bo H.-X., Cao J., Wang Y., Zhu L.-Y., Yang Y., Cheung T., Ng C.H., Wu X., Xiang Y.-T. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020;275:145–148. doi: 10.1016/j.jad.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. Psychological impact of COVID-19 in the Swedish population: Depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur. Psychiatry. 2020;63:e81. doi: 10.1192/j.eurpsy.2020.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre R.S., Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020;19:250–251. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre R.S., Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechili E.A., Saliaj A., Kamberi F., Girvalaki C., Peto E., Patelarou A.E., Bucaj J., Patelarou E. Is the mental health of young students and their family members affected during the quarantine period? Evidence from the COVID-19 pandemic in Albania. J. Psychiatr. Ment. Health Nurs. jpm. 2020;12672 doi: 10.1111/jpm.12672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group PRISMA. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Molenberghs G., Verbeke G., Demétrio C.G.B. An extended random-effects approach to modeling repeated, overdispersed count data. Lifetime Data Anal. 2007;13:513–531. doi: 10.1007/s10985-007-9064-y. [DOI] [PubMed] [Google Scholar]
- Moran P. Social Media: A Pandemic of Misinformation. Am. J. Med. 2020 doi: 10.1016/j.amjmed.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser D.A., Glaus J., Frangou S., Schechter D.S. Years of life lost due to the psychosocial consequences of COVID-19 mitigation strategies based on Swiss data. Eur. Psychiatry. 2020;63:e58. doi: 10.1192/j.eurpsy.2020.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrklas K., Shalaby R., Hrabok M., Gusnowski A., Vuong W., Surood S., Urichuk L., Li D., Li X.-M., Greenshaw A.J. COVID-19 pandemic: prevalence of perceived stress, anxiety, depression, and obsessive-compulsive symptoms vary among healthcare and non-healthcare workers in Alberta. JMIR Mental Health. 2020 doi: 10.2196/22408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee S. Disparities, desperation, and divisiveness: coping with COVID-19 in India. Psychol. Trauma. 2020;12:582–584. doi: 10.1037/tra0000682. [DOI] [PubMed] [Google Scholar]
- Naser A.Y., Dahmash E.Z., Al-Rousan R., Alwafi H., Alrawashdeh H.M., Ghoul I., Abidine A., Bokhary M.A., Al-Hadithi H.T., Ali D., Abuthawabeh R., Abdelwahab G.M., Alhartani Y.J., Al Muhaisen H., Dagash A., Alyami H.S. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. 2020:e01730. doi: 10.1002/brb3.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen H.C., Nguyen M.H., Do B.N., Tran C.Q., Nguyen T.T.P., Pham K.M., Pham L.V., Tran K.V., Duong T.T., Tran T.V., Duong T.H., Nguyen T.T., Nguyen Q.H., Hoang T.M., Nguyen K.T., Pham T.T.M., Yang S.-H., Chao J.C.-J., Van Duong T. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J. Clin. Med. Res. 2020;9 doi: 10.3390/jcm9040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni M.Y., Yang L., Leung C.M.C., Li N., Yao X.I., Wang Y., Leung G.M., Cowling B.J., Liao Q. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Mental Health. 2020;7:e19009. doi: 10.2196/19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noel N., Wright J., Stewart S.I. World Economic Forum; 2020. COVID-19 has hit Black Americans hardest. Healing this divide would lift the nation. [WWW Document]URL https://www.weforum.org/agenda/2020/08/covid19-racial-wealth-gap-black-americans/(accessed 9.11.20) [Google Scholar]
- Nyaga V.N., Arbyn M., Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch. Public Health. 2014;72:39. doi: 10.1186/2049-3258-72-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyashanu M., Simbanegavi P., Gibson L. Exploring the impact of COVID-19 pandemic lockdown on informal settlements in Tshwane Gauteng Province, South Africa. Glob. Public Health. 2020;15:1443–1453. doi: 10.1080/17441692.2020.1805787. [DOI] [PubMed] [Google Scholar]
- OECD, 2020. OECD Economic Outlook, Interim Report March 2020. OECD Publishing. https://doi.org/10.1787/7969896b-en.
- O'Hara L., Abdul Rahim H.F., Shi Z. Gender and trust in government modify the association between mental health and stringency of social distancing related public health measures to reduce COVID-19: a global online survey. Public Global Health. 2020 doi: 10.1101/2020.07.16.20155200. [DOI] [Google Scholar]
- Pakenham K.I., Landi G., Boccolini G., Furlani A., Grandi S., Tossani E. The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. J Contextual Behav Sci. 2020;17:109–118. doi: 10.1016/j.jcbs.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y., Cohen-Fridel S., Keisari S., Hoffman Y. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020;275:109–111. doi: 10.1016/j.jad.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papandreou C., Arija V., Aretouli E., Tsilidis K.K., Bulló M. Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID -19 outbreak: Cross-sectional analysis of two different confinement strategies. Eur Eating Disord Rev. 2020 doi: 10.1002/erv.2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz C., Mascialino G., Adana-Díaz L., Rodríguez-Lorenzana A., Simbaña-Rivera K., Gómez-Barreno L., Troya M., Páez M.I., Cárdenas J., Gerstner R.M., Ortiz-Prado E. Anxiety and depression in patients with confirmed and suspected COVID-19 in Ecuador. Psychiatry Clin. Neurosci. 2020 doi: 10.1111/pcn.13106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petterson S., Westfall J.M., Miller B.F. Projected deaths of despair from COVID-19. Well Being Trust. 2020 [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Maricic Mascarell, L. Betzler, F. Rogoll, J. Große, J. Ströhle, A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020:e01745. doi: 10.1002/brb3.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136 doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock A., Campbell P., Cheyne J., Cowie J., Davis B., McCallum J., McGill K., Elders A., Hagen S., McClurg D., Torrens C., Maxwell M. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst. Rev. 2020;11 doi: 10.1002/14651858.CD013779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouralizadeh M., Bostani Z., Maroufizadeh S., Ghanbari A., Khoshbakht M., Alavi S.A., Ashrafi S. Anxiety and depression and the related factors in nurses of Guilan University of Medical Sciences hospitals during COVID-19: a web-based cross-sectional study. Int J Africa Nurs Sci. 2020 doi: 10.1016/j.ijans.2020.100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price A. Online gambling in the midst of COVID-19: a nexus of mental health concerns, substance use and financial stress. Int. J. Ment. Health Addict. 2020:1–18. doi: 10.1007/s11469-020-00366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Que J., Shi L., Deng J., Liu J., Zhang L., Wu S., Gong Y., Huang W., Yuan K., Yan W., Sun Y., Ran M., Bao Y., Lu L. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj A., Johns N.E., Barker K.M., Silverman J.G. Time from COVID-19 shutdown, gender-based violence exposure, and mental health outcomes among a state representative sample of California residents. EClinMed. 2020;26 doi: 10.1016/j.eclinm.2020.100520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ran L., Wang W., Ai M., Kong Y., Chen J., Kuang L. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: A study of the general population in China at the peak of its epidemic. Soc Sci Med. 2020 doi: 10.1016/j.socscimed.2020.113261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A Language and Environment for Statistical Computing. [Google Scholar]
- Reeves A., McKee M., Stuckler D. Economic suicides in the Great Recession in Europe and North America. Br. J. Psychiatry. 2014;205:246–247. doi: 10.1192/bjp.bp.114.144766. [DOI] [PubMed] [Google Scholar]
- Rettie H., Daniels J. Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID-19 pandemic. Am. Psychol. 2020 doi: 10.1037/amp0000710. [DOI] [PubMed] [Google Scholar]
- Şahin M.K., Aker S., Şahin G., Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 Pandemic in Turkey. J. Community Health. 2020 doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz N., Holley P., Meng X., Fish L., Jedwab J. COVID-19 and depressive symptoms: a community-based study in Quebec. Canada. Can. J. Psychiatry. 2020;706743720943812 doi: 10.1177/0706743720943812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah N., Raheem A., Sideris M., Velauthar L., Saeed F. Mental health amongst obstetrics and gynaecology doctors during the COVID-19 pandemic: results of a UK-wide study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;253:90–94. doi: 10.1016/j.ejogrb.2020.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro E., Levine L., Kay A. Mental health stressors in Israel during the coronavirus pandemic. Psychol. Trauma. 2020;12:499–501. doi: 10.1037/tra0000864. [DOI] [PubMed] [Google Scholar]
- Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., Birk J.L., Brodie D., Cannone D.E., Chang B., Claassen J., Cornelius T., Derby L., Dong M., Givens R.C., Hochman B., Homma S., Kronish I.M., Lee S.A.J., Manzano W., Mayer L.E.S., McMurry C.L., Moitra V., Pham P., Rabbani L., Rivera R.R., Schwartz A., Schwartz J.E., Shapiro P.A., Shaw K., Sullivan A.M., Vose C., Wasson L., Edmondson D., Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L., Lu Z.-A., Que J.-Y., Huang X.-L., Liu L., Ran M.-S., Gong Y.-M., Yuan K., Yan W., Sun Y.-K., Shi J., Bao Y.-P., Lu L. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons-Duffin S. NPR; 2020. Millions Of Americans Have Lost Health Insurance As Unemployment Soars. [Google Scholar]
- Skapinakis P., Bellos S., Oikonomou A., Dimitriadis G., Gkikas P., Perdikari E., Mavreas V. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: a cross-sectional survey of the population. Depress. Res. Treat. 2020:2020. doi: 10.1155/2020/3158954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sljivo A., Medical student, Faculty of Medicine, University of Sarajevo, Sarajevo, Hercegovina, B.A., Kacamakovic, M., Quraishi, I., Kulenovic, A.D., Medical student, Faculty of Medicine, University of Sarajevo, Sarajevo, Hercegovina, B.A., Medical student, Faculty of Medicine, University of Sarajevo, Sarajevo, Hercegovina, B.A., Department of Psychiatry, Clinical Center of University of Sarajevo, University of Sarajevo, Sarajevo, Hercegovina, B.A. Fear and depression among residents of bosnia and herzegovina during Covid-19 outbreak - Internet survey. Psychiatria Danubina. 2020 doi: 10.24869/psyd.2020.266. [DOI] [PubMed] [Google Scholar]
- Speth M.M., Singer-Cornelius T., Oberle M., Gengler I., Brockmeier S.J., Sedaghat A.R. Mood, anxiety and olfactory dysfunction in COVID-19: evidence of central nervous system involvement? Laryngoscope. 2020 doi: 10.1002/lary.28964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava R. Understanding circular migration in India: Its nature and dimensions, the crisis under lockdown and the response of the state. Institute for Human Development. Centre for Employment Studies Working Paper Series-WP. 2020;4:2020. [Google Scholar]
- Sterne J.A., Hernán M.A., Reeves B.C., Savović J., Berkman N.D., Viswanathan M., Henry D., Altman D.G., Ansari M.T., Boutron I., Carpenter J.R., Chan A.-W., Churchill R., Deeks J.J., Hróbjartsson A., Kirkham J., Jüni P., Loke Y.K., Pigott T.D., Ramsay C.R., Regidor D., Rothstein H.R., Sandhu L., Santaguida P.L., Schünemann H.J., Shea B., Shrier I., Tugwell P., Turner L., Valentine J.C., Waddington H., Waters E., Wells G.A., Whiting P.F., Higgins J.P. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suryavanshi N., Kadam A., Dhumal G., Nimkar S., Mave V., Gupta A., Cox S.R., Gupte N. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. 2020;10(11):e01837. doi: 10.1002/brb3.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szepietowski J.C., Krajewski P., Biłynicki-Birula R., Poznański P., Krajewska M., Rymaszewska J., Matusiak Ł. Mental health status of health care workers during the COVID-19 outbreak in Poland: One region, two different settings. Dermatol. Ther. e13855. 2020 doi: 10.1111/dth.13855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tee M.L., Tee C.A., Anlacan J.P., Aligam K.J.G., Reyes P.W.C., Kuruchittham V., Ho R.C. Psychological impact of COVID-19 pandemic in the Philippines. J. Affect. Disord. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teufel M., Schweda A., Dörrie N., Musche V., Hetkamp M., Weismüller B., Lenzen H., Stettner M., Kohler H., Bäuerle A., Skoda E.-M. Not all world leaders use Twitter in response to the COVID-19 pandemic: impact of the way of Angela Merkel on psychological distress, behaviour and risk perception. J. Public Health. 2020 doi: 10.1093/pubmed/fdaa060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomaier L., Teoh D., Jewett P., Beckwith H., Parsons H., Yuan J., Blaes A.H., Lou E., Hui J.Y.C., Vogel R.I. Emotional health concerns of oncology physicians in the United States: fallout during the COVID-19 pandemic. medRxiv: the preprint server for health sciences. 2020 doi: 10.1101/2020.06.11.20128702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu Z.-H., He J.-W., Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: a cross-sectional study. Medicine. 2020;99:e20769. doi: 10.1097/MD.0000000000020769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. U.S. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress. Anxiety. 2020 doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Publications . United Nations Pubn; 2020. Human Development Report 2019: Beyond Income, Beyond Averages, Beyond Today: Inequalities in Human Development in the 21st Century. [Google Scholar]
- Vafaei H., Roozmeh S., Hessami K., Kasraeian M., Asadi N., Faraji A., Bazrafshan K., Saadati N., Aski S.K., Zarean E., Golshahi M., Haghiri M., Abdi N., Tabrizi R., Heshmati B., Arshadi E. Obstetrics healthcare providers’ mental health and quality of life during COVID-19 pandemic: multicenter study from eight cities in Iran. Psychology Research and Behavior Management. 2020 doi: 10.2147/prbm.s256780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentino-DeVries J., Lu D., Dance G.J.X. The New York Times; 2020. Location Data Says It All: Staying at Home During Coronavirus Is a Luxury. [Google Scholar]
- Veritas Health Innovation, 2021 Covidence systematic review software [WWW Document]. URL www.covidence.org (accessed 7.29.19).
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010;36:1–48. [Google Scholar]
- Walker W.H., 2nd, Walton J.C., DeVries A.C., Nelson R.J. Circadian rhythm disruption and mental health. Transl. Psychiatry. 2020;10:28. doi: 10.1038/s41398-020-0694-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Chudzicka-Czupała A., Grabowski D., Pan R., Adamus K., Wan X., Hetnał M., Tan Y., Olszewska-Guizzo A., Xu L., McIntyre R.S., Quek J., Ho R., Ho C. The association between physical and mental health and face mask use during the COVID-19 pandemic: a comparison of two countries with different views and practices. Front. Psychiatry. 2020;11:901. doi: 10.3389/fpsyt.2020.569981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L.-Q., Zhang M., Liu G.-M., Nan S.-Y., Li T., Xu L., Xue Y., Zhang M., Wang L., Qu Y.-D., Liu F. Psychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: a multicenter study. J. Psychiatr. Res. 2020;129:198–205. doi: 10.1016/j.jpsychires.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Luo Y., Lv C., Zheng X., Zhu W., Chen X., Shen M., Kuang Y. Nonadherence to treatment and patient-reported outcomes of psoriasis during the COVID-19 epidemic: a web-based survey. Patient Prefer. Adherence. 2020;14:1403–1409. doi: 10.2147/PPA.S263843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Zhang Y., Ding W., Meng Y., Hu H., Liu Z., Zeng X., Wang M. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. Eur. Psychiatry. 2020;63:e77. doi: 10.1192/j.eurpsy.2020.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Hegde S., Son C., Keller B., Smith A., Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J. Med. Internet Res. 2020;22:e22817. doi: 10.2196/22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y.-X., Guo H.-T., Du X.-W., Song W., Lu C., Hao W.-N. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine. 2020;99:e20965. doi: 10.1097/MD.0000000000020965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willner P., Rose J., Stenfert Kroese B., Murphy G.H., Langdon P.E., Clifford C., Hutchings H., Watkins A., Hiles S., Cooper V. Effect of the COVID-19 pandemic on the mental health of carers of people with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2020 doi: 10.1111/jar.12811. n/a. [DOI] [PubMed] [Google Scholar]
- Wilson J.M., Lee J., Fitzgerald H.N., Oosterhoff B., Sevi B., Shook N.J. Job Insecurity and Financial Concern during the COVID-19 Pandemic are Associated with Worse Mental Health. J. Occup. Environ. Med. 2020 doi: 10.1097/JOM.0000000000001962. [DOI] [PubMed] [Google Scholar]
- World Bank . World Bank Data; 2020. World Bank Country and Lending Groups.https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [WWW Document]URL. accessed 9.16.20. [Google Scholar]
- World Health Organization Immunizing the public against misinformation [WWW Document] 2020 https://www.who.int/news-room/feature-stories/detail/immunizing-the-public-against-misinformation URL. accessed 9.14.20. [Google Scholar]
- Xiao H., Shu W., Li M., Li Z., Tao F., Wu X., Yu Y., Meng H., Vermund S.H., Hu Y. Social Distancing among Medical Students during the 2019 Coronavirus Disease Pandemic in China: Disease Awareness, Anxiety Disorder, Depression, and Behavioral Activities. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17145047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiaoming X., Ming A., Su H., Wo W., Jianmei C., Qi Z., Hua H., Xuemei L., Lixia W., Jun C., Lei S., Zhen L., Lian D., Jing L., Handan Y., Haitang Q., Xiaoting H., Xiaorong C., Ran C., Qinghua L., Xinyu Z., Jian T., Jing T., Guanghua J., Zhiqin H., Nkundimana B., Li K. The psychological status of 8817 hospital workers during COVID-19 Epidemic: A cross-sectional study in Chongqing. J. Affect. Disord. 2020;276:555–561. doi: 10.1016/j.jad.2020.07.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin M., Luo S., She R., Yu Y., Li L., Wang S., Ma L., Tao F., Zhang J., Zhao J., Li L., Hu D., Zhang G., Gu J., Lin D., Wang H., Cai Y., Wang Z., You H., Hu G., Lau J.T.-F. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am. Psychol. 2020;75:607–617. doi: 10.1037/amp0000692. [DOI] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S., Kwak S.G., Ko E.J., Chang M.C. The Mental Health Burden of the COVID-19 Pandemic on Physical Therapists. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17103723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Yena, McIntyre Roger, Lui Leanna, Chen-Li David. PROSPERO International prospective register of systematic reviews; 2020. The mental health impact of COVID-19: disparities in low- and middle-income countries (CRD42020200647) [WWW Document].https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020200647 URL. accessed 8.17.20. [Google Scholar]
- Yi H., Ng S.T., Farwin A., Low P.T.A., Chang C.M., Lim J. Health equity considerations in COVID-19: geospatial network analysis of the COVID-19 outbreak in the migrant population in Singapore. J. Travel Med. 2020 doi: 10.1093/jtm/taaa159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Su M., Zhang J., Liu Z., Zhang B. Survey of Insomnia and Related Social Psychological Factors Among Medical Staffs Involved with the 2019 Novel Coronavirus Disease Outbreak. SSRN Electronic Journal. 2021 doi: 10.2139/ssrn.3542175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T., Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S.X., Liu J., Jahanshahi Afshar, A. Nawaser, K. Yousefi, A. Li, J. Sun, S. S.X., Z. J., L. A., A.J. K., N. A., Y. J., L. At the height of the storm: Healthcare staff's health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W.-R., Wang K., Yin L., Zhao W.-F., Xue Q., Peng M., Min B.-Q., Tian Q., Leng H.-X., Du J.-L., Chang H., Yang Y., Li W., Shangguan F.-F., Yan T.-Y., Dong H.-Q., Han Y., Wang Y.-P., Cosci F., Wang H.-X. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother. Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W., Yang X., Zhao J., Yang F., Jia Y., Cui C., Yang X. Depression and Psychological-Behavioral Responses Among the General Public in China During the Early Stages of the COVID-19 Pandemic: Survey Study. J. Med. Internet Res. 2020;22:e22227. doi: 10.2196/22227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao B., Kong F., Aung M.N., Yuasa M., Nam E.W. Novel Coronavirus (COVID-19) Knowledge, Precaution Practice, and Associated Depression Symptoms among University Students in Korea, China, and Japan. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17186671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao R., Zhou Q., Wang X.-W., Liu C.-H., Wang M., Yang Q., Zhai Y.-H., Zhu D.-Q., Chen J., Fang X.-Y., Tang X.-S., Zhang H., Shen Q., Xu H. COVID-19 Outbreak and Management Approach for Families with Children on Long-Term Kidney Replacement Therapy. Clin. J. Am. Soc. Nephrol. 2020 doi: 10.2215/CJN.03630320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.-J., Zhang L.-G., Wang L.-L., Guo Z.-C., Wang J.-Q., Chen J.-C., Liu M., Chen X., Chen J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020:1–10. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.