Abstract
We present a patient suffering from a stroke with a free-floating thrombus extending up to the distal internal carotid artery. The thrombus was totally resolved after a 2-week anticoagulation regimen without leaving behind any severe residual stenosis in the carotid bulb. The optimal treatment of this rare condition remains uncertain. We report some important treatment strategies that have been used in the literature, emphasizing the anticoagulation as the mainstay of therapy. Immediate surgical and interventional manipulations carry the risk of thrombus dislodgement and embolization and should be considered if there are recurrent symptoms despite medical management.
Keywords: free floating, thrombus, thrombosis, carotid, anticoagulation, endarterectomy, stroke
Acute internal carotid artery (ICA) thrombosis is a potentially life-threatening clinical condition that can result in brain thromboembolic events and affect the immediate survival. It is a rare condition affecting 0.45 to 1.53% of stroke patients. 1 2 There is a difference between a local thrombus confined to the carotid bulb and a free-floating thrombus (FFT) extending distally up to the siphon. Carotid FFT is an elongated thrombus partially attached to the internal carotid wall, with circumferential blood flow. 3 Detection of a FFT in the distal ICA in patients with acute ischemic stroke, represents a therapeutic dilemma and the optimal treatment in this setting remains uncertain.
We present a case with FFT in the distal ICA causing a stroke, and we analyze the treatment options considering data from the recent literature.
Case Report
A 55-year-old male with a past medical history of smoking, alcoholic cirrhosis, and sleeve gastrectomy for morbid obesity was diagnosed with colon adenocarcinoma. Upon waiting for surgical resection, he suddenly presented with left hemiparesis, walking instability, and confusion. A brain magnetic resonance imaging (MRI) scan revealed brain infracts in parietal, temporal and frontal lobes in the right side. A carotid color duplex showed a <50% stenosis at the level of the carotid bulb and thrombosis of the right ICA. A computed tomography angiography (CTAngio) revealed a FFT beginning from the carotid bifurcation and extending up to the carotid siphon, 7-cm long ( Fig. 1 ). The patient was commenced to enoxaparine 60-mg bid and acetylsalicylic acid of 100 qd. The course after the stroke was uneventful with neurological improvement and a residual paresis of the left arm. After 15 days, a CTAngio showed complete resolution of the thrombus ( Fig. 2 ). The patient continued enoxaparine 60-mg bid and underwent an uneventful subtotal colectomy 2 months after the episode. He was discharged with dual antiplatelet therapy.
Fig. 1.
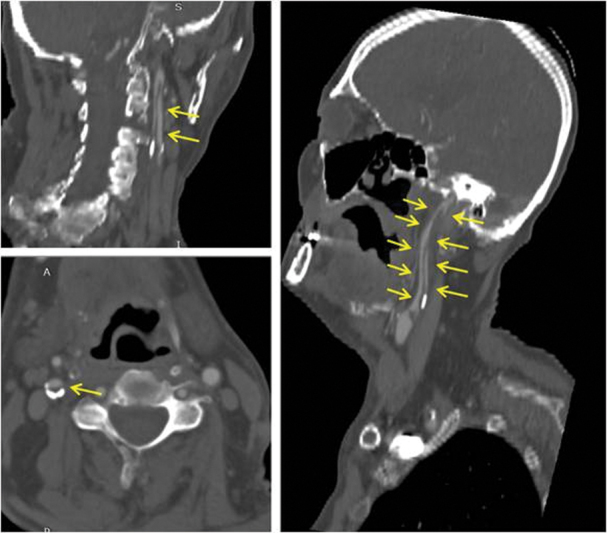
A free floating thrombus (arrows) attached to the carotid bulb is extending distally up to the carotid siphon (arrows).
Fig. 2.
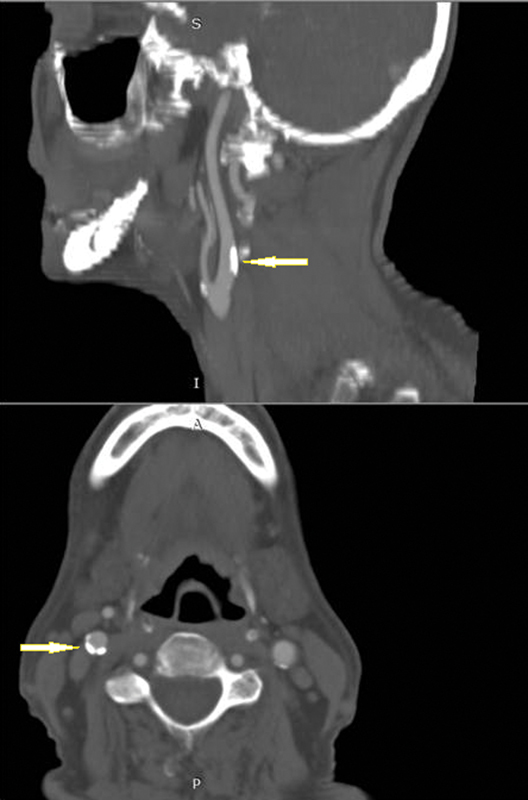
Total lysis of thrombus after treatment uncovers the responsible atheromatic plaque (arrows).
Discussion
FFT in the carotid artery is defined as an extended thrombus stacked to the arterial wall with circumferential blood flow around its most distal part, with cyclic movement relating to the cardiac cycle. 3 The optimal treatment of patients in this setting remains uncertain. There are several case reports in the literature and small observational studies but no data from randomized trials or large clinical studies exist.
A critical analysis of the literature ends up in the following five important points:
Emergency carotid endarterectomy (CEA) and thrombectomy for patients with stroke caused by acute thrombosis of the ICA are associated with a perioperative cerebral event risk of 40%. 4 Emergency open revascularization in case of thrombus extending distally carries the risk of clot dislocation and consequent cerebral embolization during the surgical exposure of the carotid bifurcation, placement of the vascular clamps, and removal of the thrombus by a Fogarty catheter.
Regarding the thrombolysis, there are concerns about the risk of development of recurrent events due to fragmentation and dislodgement of thrombus in patients that receive intravenous tissue plasminogen activator. 2 Similarly, local intra-arterial thrombolysis has the risk of intraluminal manipulation of guides and catheters in association with the lysis effect that can cause the fragmentation of clots and subsequently increase the danger of distal intracerebral embolism.
Direct aspiration of thrombus using distal and proximal balloon protection, and stent-retriever mechanical thrombectomy have been reported with encouraging results. 5 6 These endovascular techniques appear efficient, but their role needs to be validated in larger trials. Regarding carotid artery stenting aiming to trap the thrombus between the stent and the arterial wall, there are concerns about development of new brain infarcts if the thrombus extends distally. 1
Several small observational studies have suggested the safety of short-term intravenous heparin or low molecular weight heparin (LMWH) in this setting. 7 8 Anticoagulation with or without antiplatelet therapy led to complete dissolution of thrombus up to 85% of patients in 12 to 24 weeks in one report. 3 Recent guidelines recommend the safety and usefulness of short-term anticoagulation for nonocclusive, extracranial intraluminal thrombus in the setting of acute ischemic stroke (IIb level of recommendation), and posing, however, the absence of evidence from large trials. 9
Delayed operation: if thrombus is unchanged and the patient remains neurologically stable, a conservative management is continuing with reassessment at a later phase. If thrombus has shrinked in the carotid bulb and the underline causative stenosis or plaque has emerged, a thromboendarterectomy can be performed. It is proposed that surgery should be performed regardless of the degree of carotid stenosis. 10
In our case, the FFT was extending in the ICA lumen, and the operation was considered risky to provoke thrombus dislodgment and distal intracerebral embolism. We decided to start anticoagulation plus antiplatelet treatment to halt the thrombus progression, offering the opportunity for potential fibrinolysis to take place. A repeat CTAngio was performed 15 days later which confirmed the total lysis of thrombus, without any residual atheromatic stenosis. Thus, no indication for delayed intervention was set.
Conclusion
In conclusion, it appears that in patients with FFT distally extended in the ICA, anticoagulation with heparin is initially preferable. Anticoagulation may lead to resolution of thrombus in many cases while interventional or surgical options potentially can cause brain embolization from dislodgement of mobile thrombus and should be considered if there are recurrent symptoms despite medical management.
Footnotes
Conflict of Interest None declared.
References
- 1.Bhogal P, AlMatter M, Aguilar Pérez M, Bäzner H, Henkes H, Hellstern V.Carotid stenting as definitive treatment for free floating thrombus-review of 7 casesClin Neuroradiol2020 [DOI] [PMC free article] [PubMed]
- 2.Fridman S, Lownie S P, Mandzia J. Diagnosis and management of carotid free-floating thrombus: a systematic literature review. Int J Stroke. 2019;14(03):247–256. doi: 10.1177/1747493019828554. [DOI] [PubMed] [Google Scholar]
- 3.Bhatti A F, Leon L R, Jr., Labropoulos N. Free-floating thrombus of the carotid artery: literature review and case reports. J Vasc Surg. 2007;45(01):199–205. doi: 10.1016/j.jvs.2006.09.057. [DOI] [PubMed] [Google Scholar]
- 4.Lee J I, Jander S, Oberhuber A. Stroke in patients with occlusion of the internal carotid artery: options for treatment. Expert Rev Neurother. 2014;14(10):1153–1167. doi: 10.1586/14737175.2014.955477. [DOI] [PubMed] [Google Scholar]
- 5.Yamaoka A, Miyata K, Iihoshi S, Mikuni N. Endovascular treatment of asymptomatic free-floating thrombus in the carotid artery bifurcation: a direct aspiration first-pass technique under double balloon protection. BMJ Case Rep. 2019;12(08):e230295. doi: 10.1136/bcr-2019-230295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fitzpatrick N, Motyer R, Gibney B. Expanding the role of stent-retriever endovascular thrombectomy: a case series of free-floating thrombus. J Neurointerv Surg. 2018;10(12):1164–1167. doi: 10.1136/neurintsurg-2018-013946. [DOI] [PubMed] [Google Scholar]
- 7.Mokin M, Kass-Hout T, Kass-Hout O. Intravenous heparin for the treatment of intraluminal thrombus in patients with acute ischemic stroke: a case series. J Neurointerv Surg. 2013;5(02):144–150. doi: 10.1136/neurintsurg-2011-010134. [DOI] [PubMed] [Google Scholar]
- 8.Vellimana A K, Kadkhodayan Y, Rich K M. Symptomatic patients with intraluminal carotid artery thrombus: outcome with a strategy of initial anticoagulation. J Neurosurg. 2013;118(01):34–41. doi: 10.3171/2012.9.JNS12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powers W J, Rabinstein A A, Ackerson T. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–e418. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 10.Tolaymat B, Irizarry K, Reif M. Considerations beyond stenosis for carotid endarterectomy in treating free-floating thrombus of the carotid artery. Ann Vasc Surg. 2019;60:221–228. doi: 10.1016/j.avsg.2019.02.024. [DOI] [PubMed] [Google Scholar]


