Abstract
The novel coronavirus (COVID-19) has become a pandemic and the risk perception plays an important role in self-protection and spread prevention. This study attempts to explore the intrinsic characteristic of risk perception and the spatial distribution of it, which have not been involved in previous studies. To attach this purpose, data from questionnaire conducted in China and Korea (samples of 897 respondents in China and 340 respondents in South Korea) are used to produce risk perception of COVID- 19. Results reveal four principal findings: (1) risk perception of COVID-19 can be categorized into perceived social risk and perceived risk of being infected; (2) the internal differences are most pronounced in perceived risk of being infected about oneself in China, and in perceived social risk disorder about local community in South Korea; (3) the spatial distribution of risk perception is not consistent with that of epidemic severity, for high-risk perception spread out beyond the epicenter with different performance in the two categories; and (4) among the influence factors, trust in information, familiarity with epidemic situation, and interpersonal distance from suffers in the epicenter are found to have a significant influence on different aspects of risk perception. The theoretical and practical implications of this study enrich the understanding of risk perception of epidemic, and provide specific suggestions for preventing this ongoing epidemic spread across the population.
Keywords: Risk perception, COVID-19, Influence factors, International comparison
1. Introduction
The outbreak of the new coronavirus (COVID-19), which has now escalated to a pandemic, was first confirmed in Wuhan city, China. New cases and deaths continued to rise worldwide since December 2019, reaching approximately 100 million confirmed cases and 2.4 million deaths a year later, in December 2020 [1], while cases and deaths continue to rise, despite the massive effort undertaken by WHO and countries. The consensus on prevention is that wearing a mask, physical distancing, and avoiding crowds are crucial to protect people from COVID-19, because public agency and engagement with self-protection from the virus play an important role in deterring the spread of the disease across the population [2,3]. Researches in different countries and cases provide evidences that behavioral patterns can change so that individuals can avoid infection from emerging diseases (N. M. [[4], [5], [6], [7]], and that those behavioral responses to the risk of infection are related to the individuals’ risk perception [[8], [9], [10]]. A recent survey indicates that unreasonable fear may occur if risk perception is unrealistically high, thus leading to social unrest and pressure on healthcare [11]. However, individuals tend not to adopt protective measures if their risk perception is low [12], which is not conductive to avoid cross-infection, especially when real risks are underestimated. Therefore, an analysis of risk perception can provide insight into perspectives of psychological and social science for policymakers, which is conducive to risk management of the ongoing pandemic in terms of mental and physical health.
To date, research on risk perceptions of the pandemic include the Severe Acute Respiratory Syndrome [13,14] and the Middle East Respiratory Syndrome [15], which belong to the same kind of coronavirus. However, as COVID-19 is a new disease, there is no similar experience that can be used as a reference. In addition to infection and death, the pandemic poses severe challenges to the economy, daily life, and social order, with highly contagious and fatal consequences. Whereas research on risk perception focuses on perceived death and infection risks, very few researchers have examined the perception of socio-economic risks [16]. Relevant theoretical and empirical studies on COVID-19 suggest that risk perception has a significant impact on individual preventive behaviors [17,18], adherence to precautionary guidelines [19], mental and emotional health [20], and the effectiveness of preventive measures, such as lockdowns and quarantine [21]. It is essential to understand the public risk perception of COVID-19, its manifold dimensions and contributing factors. By targeting recommendations and management only to those with unreasonable risk perception, pandemic can be contained more effectively without unnecessary misallocation of resources. In this paper we identify the characteristics and contributing factors of risk perception of COVID-19 by means of a comparative analysis between China and South Korea, to determine similarities and differences in specific aspects of risk perception. Furthermore, we investigate factors that affect individuals’ risk perception of COVID-19.
The main contributions of our work are summarized as follows. First, the results of our research shed light on the formation of risk perception of this ongoing pandemic and the ensuing crisis, thus contributing to the discussion over effective prevention of the disease's spread. Second, contrary to previous research, we investigate the spatial distribution characteristics of risk perception and our work can serve as a guideline for psychotherapists and policymakers to identify susceptible and vulnerable areas. Finally, this is an international comparison of risk perceptions of COVID-19. Concerns over COVID-19 affect individuals globally in numerous ways and extents. Comparison between countries is essential to provide insight into pandemic prevention and control around the world, so that policymakers both in the United Nations and individual countries can better understand mass psychology when deciding to implement measures, such as quarantine.
The paper is structured as follows. Section 2 contains a literature review on risk perception and its contributing factors. Section 3 presents our methodology, including questionnaire design, entropy weight, and data collection. Section 4 describes the results of our analysis, the characteristics of the spatial distribution of risk perception in China and South Korea, the specific representations of risk perception in different contents, and the contributing factors to risk perception. Finally, Section 5 discusses the results and their implications.
2. Literature review
2.1. Risk perception
Risk perception refers to an individual's subjective identification of risk that one may face [22], determined by uncertainty and fear [23]. Risk perceptions of the pandemic differ significantly due to a wide range of perceptions of life, death, severity and uncertainty [24]. A nation-wide survey in the U.S.A. reveals that differences in perceived risk of infection are more significant than considerations of perceived fatality at the initial stage of the COVID-19 pandemic [25]. Regarding uncertainty, healthcare professionals are deemed more familiarized with COVID-19 both in terms of experience and knowledge, and their perception of risk infection is higher than that of the general population [11]. The situation is different than in the case of Ebola, for which healthcare professionals express lower levels of risk perception [26]. A survey among COVID-19 patients in Wuhan, China, during the early stage of the outbreak finds that individuals aged 20 to 44 and older age groups show significantly different risks. Compared with the older respondents, perceived risk of infection among younger patients is lower, but the perceived risk of death is higher [27]. Moreover, political views affect risk perceptions of the pandemic, as some groups show more confidence in leaders' ability to handle COVID-19 [28].
2.2. Factors that affect risk perception
Identifying the factors that influence risk perception is essential to our understanding of risk structure and formation [29]. Risk perception of the pandemic depends on several factors, such as the level of trust in authorities [15,28,30], sources of information, professional knowledge [27], and sociodemographic characteristics [31,32]. Governments and WHO dominate the prevention against COVID-19 at a global scale and high levels of popular satisfaction with governments can relieve individuals' risk perception [33]. Government guidelines are the most important factor in shaping individuals’ intention to indulge to preventive measures, especially when people regard such guidelines as positive and motivational [12]. The formation of risk perception of uncertain risk is related to information [34], because people tend to search for information when they face an unknown and uncertain calamity [32] and the public can only rely on mass media, their own knowledge and experience. Public trust in the accuracy of pandemic-related information can influence risk perception [35]. Trust in local governments has a greater influence on risk perception than that of the central government, because people believe that the former can be more receptive towards local communities, their perceptions and sensitivities [36].
As for sociodemographic characteristics, it has been convincingly argued that differences in professional knowledge, gender, age, education, and income related to different risk perceptions. Professional knowledge influences the way people assess risk. The general public largely depends on personal experience to evaluate risk, while experts tend to rely on professional traits and evaluate the situation by employing analytical skills [37]. Empirical studies show that risk assessment models can shape individuals' risk perception, and that perceived health risks differ between experts and the general populace [38]. Risk perception over health risks hazard in females is higher than that of males [39,40], partly because of different social roles [41] and exposure to environmental disruption [42]. Elderly people are more likely to have high levels of risk perception, especially for health risks [43] and death [44]. Research on environmental risk has long found that education is positively related to perceptions of environmental risk [45], but no direct relationship between education and risk perception of the pandemic has been detected. Finally, research shows that income is a significant factor in individuals’ risk perception of COVID-19, and that it is associated with the availability of healthcare resource.
Besides, the psychological typhoon eye effect reveals the relationship between risk perception and distance, including geographical distance from the epicenter, interpersonal relationship distance from the sufferer [46,47], and the involvement in threat of danger [48]. This effect is different from the ripple effect. Moreover, a survey about risk perception of COVID-19 indicates that both the psychological typhoon eye effect and ripple effect are at play, which dominated in different distance from Wuhan, China [49]. Accordingly, this paper explores the relationship between risk perception of COVID-19 and geographical distance, including the distance from residence to the epicenter and the interpersonal relationship distance from the sufferer in the epicenter.
3. Methodology
3.1. Questionnaire design
This paper investigates the contributing factors and the characteristics of individuals' risk perception of COVID-19. Preliminary dimensions and factors of risk perception are obtained by previous research on COVID-19 and other epidemics. And then, we conducted a questionnaire survey. The survey consists of three sections. The first captures demographic information of participants. The second comprises seven questions regarding risk perception, which is classified into social risk perception and infection risk perception. A five-point Likert scale is applied to measure the perceived extent of each question, from ‘extremely high’ (5) to ‘extremely low’ (1). Finally, the third section investigates the factors that affect risk perception. Drawing on previous literature, we propose the following categorization of contributing factors: trust in information, familiarity with COVID-19, level of satisfaction with governments, sociodemographic characteristics of respondents, and distance (Table 1 ). The epicenter of COVID-19 in China is Wuhan and the epicenter in South Korea is Seoul, as indicated by the confirmed cases. Also, we investigate risk perception in areas around the epicenters in particular to detect the presence of the ripple effect and/or the psychological typhoon eye effect.
Table 1.
Influence factors of risk perception.
| Category | Details | Symbol | Mean |
|
|---|---|---|---|---|
| China | South Korea | |||
| Information | Trust in TV news | T1 | 4.147 | 3.781 |
| Trust in government website | T2 | 4.285 | 3.872 | |
| Trust in social software | T3 | 4.058 | 3.081 | |
| Familiarity | Familiarity with COVID-19 | F1 | 3.934 | 3.687 |
| Familiarity with situation in epicenter | F2 | 3.619 | 3.981 | |
| Familiarity with situation in local community | F3 | 3.896 | – | |
| Satisfaction with governments | Satisfaction with the government in epicenter | S1 | 2.324 | 3.028 |
| Satisfaction with the local government | S2 | 3.562 | 3.171 | |
| Satisfaction with the central government | S3 | 3.765 | 3.412 | |
| Sociodemographic characteristics | Live in rural or urban area | Residence | – | – |
| Education level | Education | – | – | |
| career | Career | – | – | |
| Distance | Geographical distance from residence to epicenter | D1 | 4.491 | 4.507 |
| Interpersonal relationship distance from the sufferer in epicenter | D2 | 1.952 | 1.962 | |
3.2. Data collection
The survey was conducted online during February 2020 in China and October 2020 in South Korea. Both countries enacted cost-effective measures quicker than other countries, especially in Europe, and were more severely affected than most other countries during the period of our survey. Therefore, it is representative for crisis management and pandemic control. We chose February to circulate the questionnaire in China, one month after the COVID-19 outbreak in Wuhan, precisely because at that time the disease was at its peak and risk perception was representative of the real situation. In South Korea the disease rebounded in October significantly and we chose this month because of the severity of the situation and individuals’ risk perception is noteworthy. A total of 897 valid questionnaires have been received from China and 340 from South Korea; Table 2 illustrates demographic information of respondents.
Table 2.
Demographic information about respondents.
| Characteristic | Type | Percentage (%) |
|
|---|---|---|---|
| China | South Korea | ||
| Gender | Male | 54.80 | 50.70 |
| Female | 45.20 | 49.30 | |
| Age | 16–18 | 1.80 | 24.60 |
| 18–36 | 50.50 | 25.60 | |
| 37–55 | 39.00 | 25.60 | |
| 55+ | 8.70 | 24.20 | |
| Education | With or below junior high school | 2.90 | 14.70 |
| Senior high school and college | 14.50 | 13.30 | |
| Undergraduate | 45.00 | 60.20 | |
| Post-graduate | 37.60 | 11.80 | |
| Residence | Urban | 58.70 | 52.10 |
| Rural | 14.30 | 47.90 | |
| Career | Medical worker | 6.24 | 2.41 |
| Civil server | 24.53 | 3.59 | |
| Researcher | 17.73 | 0.51 | |
| Self-employed | 5.57 | 10.09 | |
| Others | 45.93 | 83.40 | |
3.3. Data analysis
3.3.1. Principal component analysis
Principal component analysis represents a transfer and projection of original data, which is conducted by SPSS version 25 in this paper to complete dimension reduction of risk perception. In the process of its transformation, every original data contributes different to principal components, and objects that have the largest variance can be maintained. Steps in this process are summarized as follows:
Consider there are n samples and every sample has m variables. The assessment matrix is established in Eq. (1). In this paper, samples are respondents and variables are questions about risk perception in questionnaire, which are measured by five-point Likert scale.
| (1) |
The correlation matrix R = can be obtained by calculating the mean and standard deviation of factor j in matrix X:
| (2) |
| (3) |
The eigenvalue and eigenvector of matrix R can be determined by Eq. (4):
| (4) |
where λi (i = 1, 2, …, m) and (i = 1, 2, …, m) are the eigenvalues and eigenvectors of matrix R, respectively, corresponds to the principal components, and λi corresponds to the variance obtained from each principal component. The effect of each eigenvalue is given by the contribution rate. A larger contribution rate indicates a larger eigenvalue. The largest eigenvalues represent the principal components regarding most of the variability in the observed data. The cumulative contribution rate α for a specific eigenvalue λk (i = 1, 2, …, m) can be obtained by Eq. (5):
| (5) |
If the value of α is equal to or more than 90%, k principal components are considered to contain sufficient information to represent the complex original data array. The matrix , composed of k principal components, can be expressed by Eq. (6):
| (6) |
In this matrix, the largest contribution rate is given by the first principal component, followed by the other components, which have gradually decreasing contribution rates.
3.3.2. Entropy weight
Entropy weight is applied to analyze the internal variation in risk perception, which is a measure of system disorderliness that originates from thermodynamics. The smaller the entropy weight is, the larger the internal variance will be [50]. In this paper, we applied this method to see the variance of different aspects of risk perception.
For is the value of the jth aspect of risk perception of the ith respondent, and the score matrix of risk perception can be expressed as follows.
| (7) |
The eigenvalue and entropy weight are calculated using Eq. (8), (9), is the eigenvalue andis the entropy weight.
| (8) |
| (9) |
3.3.3. ANOVA
Analysis of Variance (ANOVA) is conducted with SPSS to identify the critical factors that affect risk perception, which has been wildly applied in the field of research on risk perception [21,51]. The 5% and 1% level of significance are used for our test. Factors with the significance value (p-Value) of 5% are considered to have a significant impact, and factors with the value of 1% are considered to have an extremely significant impact.
4. Results
4.1. Preliminary analysis
The internal consistency of the questionnaire measured by Cronbach's alpha is 0.704 in the Chinese sample and 0.681 in the South Korean sample, thus indicating acceptable consistency that supports further analysis. Besides, dimension reduction analysis divides the seven questions on risk perception into two categories: perceived infection and perceived social risk (as shown in Table 3 ).
Table 3.
The rotated component matrix of risk perception.
| Category | Details | Symbol | Component 1 | Component 2 | |
|---|---|---|---|---|---|
| China | Perceived social risk | Anxiety about the epidemic situation | RP1 | 0.562 | |
| Perceived risk of day-to-day life about Wuhan | RP2 | 0.744 | |||
| Perceived risk of day-to-day life about local community | RP3 | 0.802 | |||
| Perceived social disorder about local community | RP4 | 0.810 | |||
| Perceived social disorder about Wuhan | RP5 | 0.792 | |||
| Perceived risk of infection | Perceived infection about oneself | RP6 | 0.947 | ||
| Perceived infection about families | RP7 | 0.948 | |||
| South Korea | Perceived social risk | Anxiety about the epidemic situation | RP1 | 0.538 | |
| Perceived risk of day-to-day life about Seoul | RP2 | 0.802 | |||
| Perceived risk of day-to-day life about local community | RP3 | 0.782 | |||
| Perceived social disorder about local community | RP4 | 0.771 | |||
| Perceived social disorder about Seoul | RP5 | 0.781 | |||
| Perceived risk of infection | Perceived infection about oneself | RP6 | 0.886 | ||
| Perceived infection about families | RP7 | 0.854 |
4.2. Characteristics of risk perception in China and South Korea
4.2.1. The internal variance of risk perception
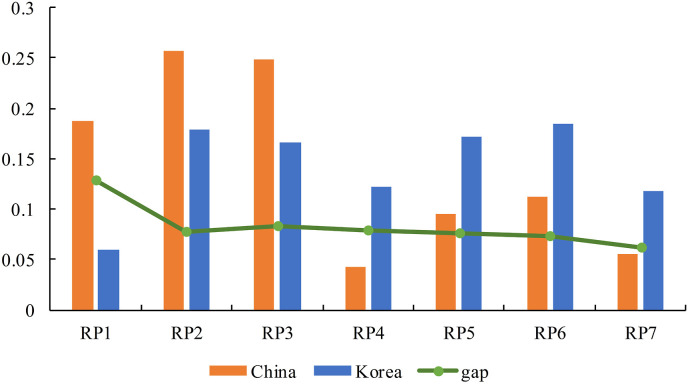
The internal variance of risk perception measured by entropy weight is shown in Table 4 and the comparison of China and South Korea is presented in Fig. 1 . The more the internal variance weight, the more significant impact it has on risk perception of COVID-19. Among Chinese respondents, the perceived infection risk about oneself (RP6) accounts for the largest number of internal variance (0.257), followed by the perceived infection of family members (RP7) (0.2491), indicating that perceived risk of infection is a significant aspect in general risk perception of COVID-19. The lowest variance of risk perception relates to the perceived risk of daily life (RP2) and of social disorder in Wuhan (RP5), which indicates that individuals shared similar perceptions of social risk in the epicenter during the period of the investigation.
Table 4.
The internal variance of risk perception.
| Risk perception | Internal variance |
The gap | ||
|---|---|---|---|---|
| China | South Korea | |||
| Perceived social risk | RP1 | 0.1878 | 0.0596 | 0.13 |
| RP2 | 0.0433 | 0.1221 | 0.08 | |
| RP3 | 0.0954 | 0.1717 | 0.08 | |
| RP4 | 0.1118 | 0.1842 | 0.07 | |
| RP5 | 0.0557 | 0.1178 | 0.06 | |
| Perceived risk of being infected | RP6 | 0.2570 | 0.1791 | 0.08 |
| RP7 | 0.2491 | 0.1656 | 0.08 | |
Fig. 1.
The comparative internal variance of risk perception in China and South Korea.
Among South Korean respondents, the perceived risk of social disorder in the local community (RP4), of disruption in daily life in the local community (RP3), and of infection of oneself (RP6) are the three risk perceptions with the most significant impact on general risk perception (their respective internal variance weights are 0.1842, 0.1717, and 0.1791). Anxiety over the pandemic returned the lowest internal variance.
The internal difference in the perception of social risk in China is bigger than in South Korea, while one in risk perception of infection in South Korea is bigger than that in China. The gap of internal variance is miniscule except for the one in anxiety, and the variance of anxiety in China is much higher than in South Korea. The minimum gap exists in the perceived social disorder about epicenter, with the variance in South Korea being higher than in China. Besides, the internal variance relating to anxiety and perceived risk of infection in China are higher than in South Korea, indicating that differences in severity and risk perception of infection are more pronounced in China. The gap indicates that risk perception in China and South Korea differ in specific aspects, even though both countries fight against the same pandemic.
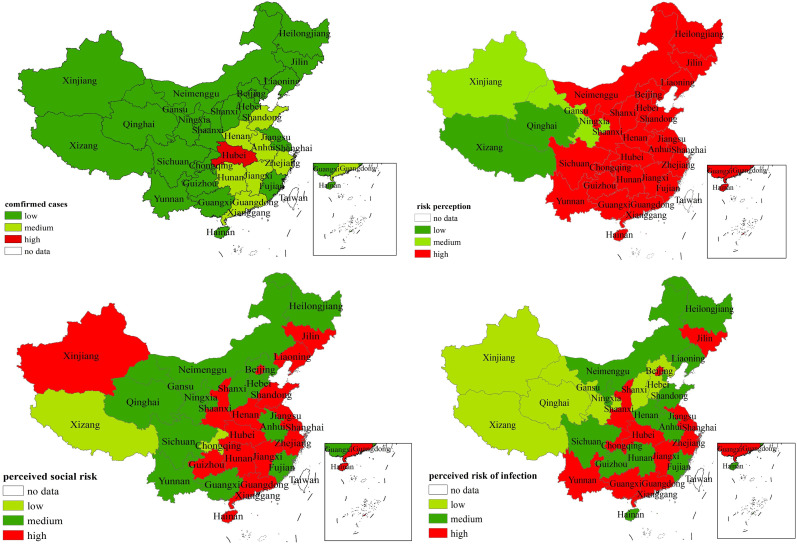
4.2.2. Spatial distribution of risk perception
We measure risk perception of COVID-19 by the weighted average of seven questions presented in the preliminary analysis, and use entropy weight to calculate the weight for every question. In China, the spatial distribution of risk perception is inconsistent with that of confirmed cases, and the distributions of perceived social risk and infection risk in specific provinces also differ (as shown in Fig. 2 ). During the time of our investigation the epicenter of COVID-19 was located in Hubei, which does not coincide with the epicenter of risk perception, as the general risk perception in the southern and eastern regions is higher than that in the northwest region. Regarding the two aspects of risk perception, both perceived social risk and infection risk are high in Jilin, Jiangsu, Shanghai, Zhejiang, Guangdong, Jiangxi, Shaanxi, Beijing, and Hubei; all these areas could benefit from more concentrated efforts to meet individual psychological requirements. Perceived social risk in Liaoning, Henan, Hunan, and Guizhou is higher than the perceived risk of being infected, thus indicating preventive measures should be focused more on mitigating social risk and management, such as working to maintain social stability.
Fig. 2.
Characteristics of risk perception and its spatial distribution in China.
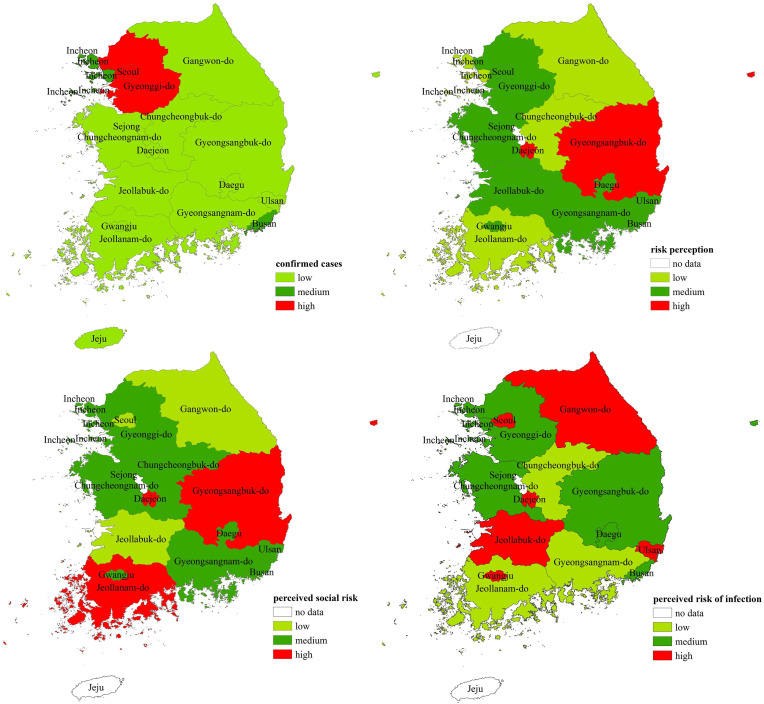
In South Korea two epicenters for the severity and risk perception of COVID-19 clearly emerge (Fig. 3 ). The most confirmed cases were reported from Seoul and Gyeonggi-do, but risk perception peaked in Gyeongsangbuk-do and Daejeon. A number of precautionary measures to control the spread of the pandemic and mitigate anxiety can be implemented in accordance to the specific characteristics to tackle high levels of risk perception. In Daejeon, the focus should be on mitigating unreasonable fear and anxiety, because the perceived social risk and risk of infection are high. As for Gyeongsangbuk-do, precautionary measures should focus on improving perceptions of risks on daily life and social order risks, because the perceived social risk is higher than the perceived risk of infection. Additionally, Gangwon-do should be monitored closely, because it reports the lowest numbers of confirmed cases, together with the lowest levels of general risk perception and perceived social risk, but high levels of perceived risk of infection.
Fig. 3.
Characteristics of risk perception and its spatial distribution in South Korea.
4.3. Contributing factors in risk perception
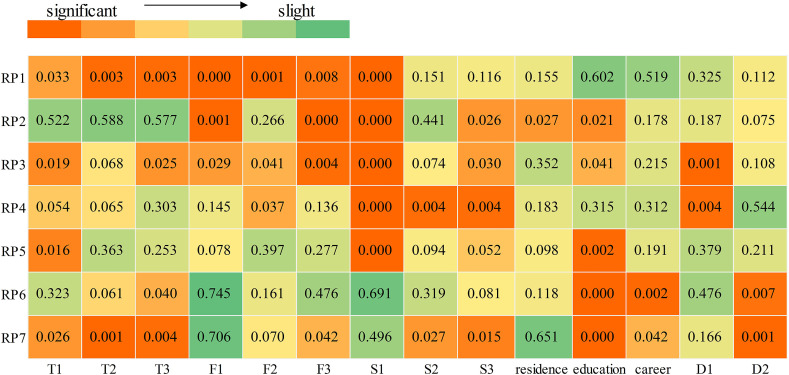
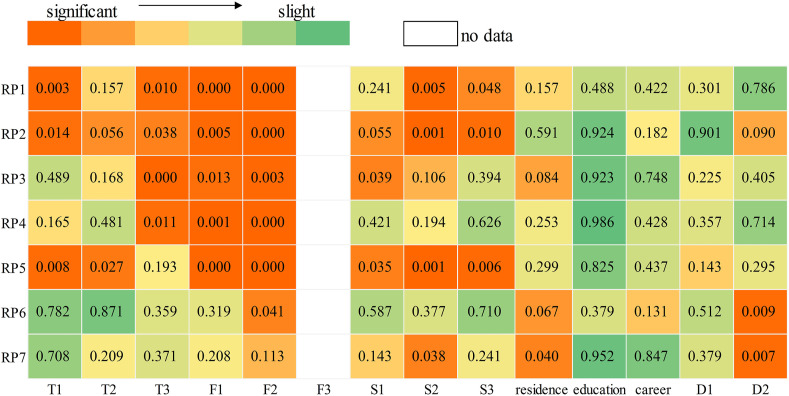
4.3.1. China
Fig. 4 illustrates ANOVA results for risk perception, which indicate the contributing factors to risk perception in China. Level of satisfaction with local governments at the epicenter (S1) and with the central government (S3), trust in government websites (T2), and education level strongly correlate with the vast majority of risk perception of COVID-19. Regarding sociodemographic characteristics, place of residence has little impact on risk perception, whereas career can significantly influence the perception of risk of infection, either for oneself or their family. In terms of distance, geographical distance (D1) significantly affects perceived social risk in local communities, whereas interpersonal relationship distance (D2) is important for the perceived risk of being infected. Contributing factors affect different aspects of risk perception, thus indicating that the risk perception management should tailor measures onto the factors that are significantly associated with those specific risks.
Fig. 4.
ANOVA results for risk perception in China.
Furthermore, we identify the prevalent concerns of risk perception. Anxiety over the situation (RP1), perceived risk of disruption of the daily life of the local community (RP3), and perceived risk of infection of family members (RP7) are the main concerns of risk perception. Anxiety is a typical reaction on the face of stress, as the severity and spread of a pandemic that has disrupted people's lives dramatically, especially of those who lived in quarantine for long periods of time, aggravate stress across the population. As for the risk perception of infection, people seem to care more about the safety of their families.
4.3.2. South Korea
In South Korea, familiarity with the situation in the local community (F2), familiarity with COVID-19 (F1), and levels of satisfaction with the local government (S2) strongly correlate with the vast majority of risk perception Fig. 5 . Sociodemographic characteristics have little impact on risk perception, except for the place of residence. Interpersonal relationship distance (D2) is an important factor contributing to perceived risk of infection about oneself and their family. Geographical distance (D1) has little effect on risk perceptions, which indicates that both psychological typhoon eye effect and ripple effect do not appear/are of lesser importance in South Korea.
Fig. 5.
ANOVA results for risk perception in South Korea.
The prevalent concerns of risk perception in South Korea are the perceived risk of disruption to daily life in the epicenter (RP2), anxiety over the situation (RP1), and the risk of comprising social order in the epicenter (RP5). Therefore, people appeared more concerned over social risk during this pandemic, especially in Daegu, at the time of our investigation. Therefore, anxiety over the pandemic is a common major concern in China and South Korea and both central governments should focus their efforts in avoiding the spread of unreasonable fear.
5. Discussion and conclusion
The two categories of risk perception of COVID-19, over social risk and infection, show different internal variance. Risk perceptions with high internal variance suggest significant differences, and the specific aspects require more attention. Therefore, authorities in China should focus their efforts and resources more on targeting risk perception of infection, whereas in South Korea the focus should revolve around the perceived social risk close to epicenters of the pandemic.
As for spatial distribution, the characteristics of risk perception are not the same as the severity of epidemic. In China, areas where risk perception is highly correlated with population distribution, as southern and eastern provinces are densely populated. In South Korea, the spatial distribution of population coincides with that of confirmed cases, but differs from the distribution of high-risk perceptions. Seoul and Gyeonggi-do are the most densely populated areas and reported the most confirmed cases during our investigation, but show medium levels of risk perception. High-risk perception areas are Gyeongsangbuk-do and Daejeon, yet they both reported relatively low numbers of confirmed cases. The distribution of high-level risk perceptions is more extensive than that of confirmed cases both in China and South Korea, and the representation of it performs differently in perceived social risk and infection. Measures tackling issues with risk perception cannot be limited exclusively in the epicenters, but combined efforts to improve physical and psychological healthcare are required to prevent further spread of the virus across the population.
Trust in TV news and information communicated by government websites and mass media are closely related to risk perception both in China and South Korea. This indicates that appropriate efforts to uphold public trust in communication of information can affect risk perception significantly. Governments play a leading role in the fight against the pandemic and people are more likely to abide by guidelines when their confidence in the government is high. In addition, the public lacks access to full evidence and knowledge of ongoing conditions, hence they rely on institutions they trust to obtain knowledge and evaluate risk [52], which can lead to changes in perceptions and behavior (especially the way and extend to which people employ protective measures). Therefore, improving public opinion of the government is conducive to prevent the spread of the virus across the population and enhance the confidence to combat COVID-19. Intensive efforts must be put into circulating reliable and timely information on the development of pandemic, the economic situation and the condition of the healthcare system, to help the public understand reality.
Familiarity with the current condition of the pandemic has a significant influence on the perceived social risk, including anxiety and perceived risk over daily life, partly because of the numerous uncertainties regarding this new virus, effective treatment, and its negative impact on social economy. Many studies have detected a correlation between knowledge and risk perception of COVID-19, thus indicating that people with limited knowledge tend to be more pessimistic [21,53,54]. Expert knowledge of the pandemic has been linked convincingly to higher willingness of individuals to comply with preventive measures [12,55]. Therefore, the popularization of science regarding COVID-19 and the implementation of reliable and acceptable preventive guidance can help individuals make more objective risk assessment.
Our results also reveal that interpersonal relationship distance from carriers and patients in the epicenter can significantly affect the perceived risk of infection. The distance is classified into the following categories. The local people in the epicenter Wuhan or Seoul and live there during this epidemic. The local people in the epicenter but not live there during this epidemic. Not the local people but have families and friends there. Not the local people but have been there during this epidemic. And not the local people and have no interpersonal relationship with there. Local residents whose families live in the epicenter are more concerned over the risk of infection, because high numbers of confirmed cases increase the probability of infection and cause additional psychological pressure. Moreover, interpersonal relationship distance also makes influences the uncertainty of being the one who has close contact with COVID-19 patients. Intensive efforts should be targeted towards mental healthcare according to these kinds of relationship distance, to deter outbursts of public panic that would only be harmful to the prevention of the pandemic.
This paper expands the scope of previous research and investigates intrinsic characteristics of risk perception and its spatial distribution. ANOVA analysis reveals significant contributing factors and the major perceived risks, which can function as reference for governments in their attempt to deter outbursts of unreasonable public fear and panic over social risk and infection. To the best of our knowledge, this is the first study to analyze the risk perception of COVID-19 from both a comparative and a spatial perspective. We explore the internal mechanisms of the significant contributing factors, yet there remains ample room for further research. We show the impact of distance on risk perception, but future research can explore potential correlation to the ensuing psychological effects, such as the ripple or the psychological typhoon eye effect.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This paper is supported by the Institutes of Science and Development of the Chinese Academy of Sciences (Y9X3541H) of the People's Republic of China, and the National Office for Philosophy and Social Sciences (19AZD019).
References
- 1.WHO, 2020a. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 .
- 2.Epstein, Joshua M. Modelling to contain pandemics. Nature. 2009;460(7256):687. doi: 10.1038/460687a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferguson, Neil Capturing human behaviour. Nature. 2007;446(7137):733. doi: 10.1038/446733a. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson N.M., Cummings D.A., Fraser C., Cajka J.C., Cooley P.C., Burke D.S. Strategies for mitigating an influenza pandemic. Nature. 2006;442(7101):448–452. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lau J.T.F., Tsui H., Lau M., Yang X. SARS transmission, risk factors, and prevention in Hong Kong. Emerg. Infect. Dis. 2004;10(4):587–592. doi: 10.3201/eid1004.030628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadique M.Z., Edmunds W.J., Smith R.D., Meerding W.J., Beutels P. Precautionary behavior in response to perceived threat of pandemic influenza. Emerg. Infect. Dis. 2007;13(9):1307–1313. doi: 10.3201/eid1309.070372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steelfisher G.K., Blendon R.J., Bekheit M.M., Lubell K. The public's response to the 2009 H1N1 influenza pandemic. N. Engl. J. Med. 2010;362(22):e65. doi: 10.1056/NEJMp1005102. [DOI] [PubMed] [Google Scholar]
- 8.Funk S., Gilad E., Watkins C., Jansen V.A.A. The spread of awareness and its impact on epidemic outbreaks. Proceedings of the National Academy of ences. 2009;106(16):6872–6877. doi: 10.1073/pnas.0810762106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poletti P., Ajelli M., Merler S. Risk perception and effectiveness of uncoordinated behavioral responses in an emerging epidemic. Math. Biosci. 2012;238(2):80–89. doi: 10.1016/j.mbs.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Seeman N., Ing A., Rizo C. 2008. Healthcare Quarterly. [DOI] [PubMed] [Google Scholar]
- 11.Peres D., Monteiro J., Almeida M., Ladeira R. Risk perception of COVID-19 among the Portuguese healthcare professionals and general population. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmad M., Iram K., Jabeen G. Perception-based influence factors of intention to adopt COVID-19 epidemic prevention in China. Environ. Res. 2020;190:109995. doi: 10.1016/j.envres.2020.109995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith R.D. Responding to global infectious disease outbreaks: lessons from SARS on the role of risk perception, communication and management. Soc. Sci. Med. 2006;63(12):3113–3123. doi: 10.1016/j.socscimed.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tracy C.S., Rea E., Upshur R.E. Public perceptions of quarantine: community-based telephone survey following an infectious disease outbreak. BMC Publ. Health. 2009;9 doi: 10.1186/1471-2458-9-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sunhee K., Seoyong K. Exploring the determinants of perceived risk of Middle East respiratory Syndrome (MERS) in South Korea. Int. J. Environ. Res. Publ. Health. 2018;15(6):1168. doi: 10.3390/ijerph15061168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gruchoła M., Sławek-Czochra M. “The culture of fear” of inhabitants of EU countries in their reaction to the COVID-19 pandemic – a study based on the reports of the Eurobarometer. Saf. Sci. 2021;135 doi: 10.1016/j.ssci.2020.105140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jose R., Narendran M., Bindu A., Beevi N., L M., Benny P.V. Public perception and preparedness for the pandemic COVID 19: a Health Belief Model approach. Clinical Epidemiology and Global Health. 2021;9:41–46. doi: 10.1016/j.cegh.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee S.Y., Yang H.J., Kim G., Cheong H.K., Choi B.Y. Preventive behaviors by the level of perceived infection sensitivity during the South Korea outbreak of Middle East Respiratory Syndrome in 2015. Epidemiology & Health. 2016;38 doi: 10.4178/epih.e2016051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen L., Liu Y., Chang Y., Wang X., Luo X. Public opinion analysis of novel coronavirus from online data. Journal of Safety Science and Resilience. 2020;1(2):120–127. doi: 10.1016/j.jnlssr.2020.08.002. [DOI] [Google Scholar]
- 21.Iqbal M.A., Younas M.Z. Public knowledge, attitudes, and practices towards COVID-19 in Pakistan: a cross-sectional study. Child. Youth Serv. Rev. 2021;120:105784. doi: 10.1016/j.childyouth.2020.105784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bauer R.A. 1960. Consumer Behavior as Risk Taking; pp. 384–398. Chicago, IL. [Google Scholar]
- 23.Slovic P. The Perception of risk. Risk Society & Policy. 2000;69(3) 112-112. [Google Scholar]
- 24.Shen Z., Zhong Z., Xie J., Ding S., Li S., Li C. Development and psychometric assessment of the public health emergency risk perception scale: under the outbreak of COVID-19. Int. J. Nurs. Sci. 2020 doi: 10.1016/j.ijnss.2020.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bruine de Bruin W., Bennett D. Relationships between initial COVID-19 risk perceptions and protective health behaviors: a national survey. Am. J. Prev. Med. 2020;59(2):157–167. doi: 10.1016/j.amepre.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sridhar S., Brouqui P., Fontaine J., Perivier I., Ruscassier P., Gautret P., Regner I. Risk perceptions of MSF healthcare workers on the recent Ebola epidemic in West Africa. New Microbes New Infect. 2016;12:61–68. doi: 10.1016/j.nmni.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhong Y., Liu W., Lee T.Y., Zhao H., Ji J. Risk perception, knowledge, information sources and emotional states among COVID-19 patients in Wuhan, China. Nurs. Outlook. 2020 doi: 10.1016/j.outlook.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shao W., Hao F. Confidence in political leaders can slant risk perceptions of COVID-19 in a highly polarized environment. Soc. Sci. Med. 2020;261:113235. doi: 10.1016/j.socscimed.2020.113235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang J. The influence of culture on South Koreans' risk perception. J. Risk Res. 2015;18(1–2):69–92. [Google Scholar]
- 30.Ye M., Lyu Z. Trust, risk perception, and COVID-19 infections: evidence from multilevel analyses of combined original dataset in China. Soc. Sci. Med. 2020;113517 doi: 10.1016/j.socscimed.2020.113517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guillon M., Kergall P. Attitudes and opinions on quarantine and support for a contact-tracing application in France during the COVID-19 outbreak. Publ. Health. 2020;188:21–31. doi: 10.1016/j.puhe.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Narayana G., Pradeepkumar B., Ramaiah J.D., Jayasree T., Yadav D.L., Kumar B.K. Knowledge, perception, and practices towards COVID-19 pandemic among general public of India: a cross-sectional online survey. Curr Med Res Pract. 2020;10(4):153–159. doi: 10.1016/j.cmrp.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Siegrist M., Gutscher H., Earle T. Perception of risk: the influence of general trust, and general confidence. J. Risk Res. 2005;8(2):145–156. [Google Scholar]
- 34.Zaller J.R. The nature and origins of mass opinion. Soc. Forces. 1992;73(1) [Google Scholar]
- 35.WHO Rolling updates on coronavirus disease (COVID-19) 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
- 36.Liang M., Tom C. Government trust, social trust, and citizens' risk concerns: evidence from crisis management in China. Publ. Perform. Manag. Rev. 2018:1–22. [Google Scholar]
- 37.Slovic P., Finucane M.L., Peters E., Macgregor D.G. Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Social Science Electronic Publishing. 2004;24(2):311–322. doi: 10.1111/j.0272-4332.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- 38.Hussey L.K., Arku G. Conceptualizations of climate-related health risks among health experts and the public in Ghana. Soc. Sci. Med. 2019 doi: 10.1016/j.socscimed.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 39.Finucane M.L., Slovic P., Mertz C.K., Flynn J., Satterfield T.A. Gender, race, and perceived risk: the 'white male' effect. Health Risk Soc. 2000;2(2):159–172. [Google Scholar]
- 40.Mccright A.M., Dunlap R.E. Cool dudes: the denial of climate change among conservative white males in the United States. Global Environ. Change. 2011;21(4):1163–1172. [Google Scholar]
- 41.Davidson D.J., Freudenburg W.R. Gender and environmental risk concerns: a review and analysis of available research. Environ. Behav. 1996;28(3):302–339. [Google Scholar]
- 42.Paul M., Bunyan B. Is there a "race" effect on concern for environmental quality? Publ. Opin. Q. 1998;(4):4. [Google Scholar]
- 43.Kim Y.H., Park I.K., Kang S.J. Age and gender differences in health risk perception. Cent. Eur. J. Publ. Health. 2018;26(1):54–59. doi: 10.21101/cejph.a4920. [DOI] [PubMed] [Google Scholar]
- 44.Zhou F., Yu T., Du R., Fan G., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229) doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liere K.D.V., Dunlap R.E. The social bases of environmental concern: a review of hypotheses, explanations and empirical evidence. Publ. Opin. Q. 1980;44(2):181–197. [Google Scholar]
- 46.Shu, Li Progression of the "psychological typhoon eye" and variations since the wenchuan earthquake. PloS One. 2010 doi: 10.1371/journal.pone.0009727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shu Li, Li-Lin Rao, Xiao-Peng Ren, Zheng Psychological typhoon eye in the 2008 wenchuan earthquake. PloS One. 2009;4(3) doi: 10.1371/journal.pone.0004964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng R., Rao L.L., Zheng X.L., Cai C., Wei Z.H., Xuan Y.H., Li S. The more involved in lead-zinc mining risk the less frightened: a psychological typhoon eye perspective. J. Environ. Psychol. 2015;44:126–134. doi: 10.1016/j.jenvp.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang S.X., Huang H., Wei F. Geographical distance to the epicenter of Covid-19 predicts the burnout of the working population: ripple effect or typhoon eye effect? Psychiatr. Res. 2020;288:112998. doi: 10.1016/j.psychres.2020.112998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shannon C.E. A mathematical theory of communication. Bell System Technical Journal. 1949;27(4):379–423. [Google Scholar]
- 51.Peng Y., Zhu X., Zhang F., Huang L., Xue J., Xu Y. Farmers' risk perception of concentrated rural settlement development after the 5.12 Sichuan Earthquake. Habitat Int. 2018;71:169–176. doi: 10.1016/j.habitatint.2017.11.008. [DOI] [Google Scholar]
- 52.Cvetkovich T.C.E.G.T. Praeger; 1995. Social Trust: toward a Cosmopolitan Society. [Google Scholar]
- 53.Azlan A.A., Hamzah M.R., Sern T.J., Ayub S.H., Mohamad E. Public knowledge, attitudes and practices towards COVID-19: a cross-sectional study in Malaysia. PloS One. 2020;15(5) doi: 10.1371/journal.pone.0233668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhong B.L., Luo W., Li H.M., Zhang Q.Q., Li Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int. J. Biol. Sci. 2020;16(10):1745–1752. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Delpont M., Racicot M., Durivage A., Fornili L., Guerin J.u., Vaillancourt J.i., Paul M.C. Transboundary and Emerging Diseases; 2020. Determinants of Biosecurity Practices in French Duck Farms after a H5N8 Highly Pathogenic Avian Influenza Epidemic: the Effect of Farmer Knowledge, Attitudes and Personality Traits. [DOI] [PubMed] [Google Scholar]