Abstract
Objective
The Korean Society of Lipid and Atherosclerosis (KSoLA) has published the Dyslipidemia Fact Sheets in Korea 2020 to provide an overview of magnitude and management status of dyslipidemia and their recent trends therein.
Methods
The Fact Sheets were based on the analyses of Korean adults aged 20 years or older of the 2007–2018 Korea National Health and Nutrition Examination Survey (KNHANES) and the 2002–2018 National Health Insurance Big Data (NHI-BD).
Results
Between 2007 and 2018, the crude prevalence of hypercholesterolemia increased from 9.0% to 20.7%. During the same period, its management rate also improved yet remained unsatisfactory. In 2018, the prevalence of dyslipidemia was 45.6% in men and 31.3% in women, which increased with older age and presence of metabolic abnormalities. Indeed, the number of people diagnosed with dyslipidemia has increased nearly 8-fold from 1.5 million in 2002 to 11.6 million in 2018; alongside, the number of people receiving pharmacological treatment for dyslipidemia has also risen. Of the 7.7 million people treated for dyslipidemia in 2018, statin accounted for the majority (91.8%) of lipid-lowering drug prescriptions, followed by ezetimibe (14.6%), fibrate (8.5%), and omega-3 acid (5.9%). The most frequently used combination therapy was statin plus ezetimibe, accounting for 72% of dual therapy prescriptions.
Conclusion
Dyslipidemia continues to impose a substantial disease burden in Korea. Both healthcare practitioners and patients need to actively adopt guideline-recommended lifestyle modification and pharmacological treatment for comprehensive, timely, and sustained management.
Keywords: Dyslipidemias, Hypercholesterolemia, Lipids, Korea
INTRODUCTION
Despite substantial improvements in cardiovascular disease (CVD) management and outcomes in recent decades, CVD remains the leading cause of mortality globally1 and in Korea.2 With rapid population aging, CVD accounts for substantial per-patient healthcare costs and a considerable macroeconomic burden.3 Moreover, the healthy life-year and quality-adjusted life-year losses attributable to CVD are projected to exponentially rise by 2025.4 Nonetheless, a considerable proportion of this burden can be reduced through interventions targeting major CVD precursors, including hypertension, diabetes mellitus, and dyslipidemia.5
To promote the comprehensive prevention and treatment of dyslipidemia, the Korean Society of Lipid and Atherosclerosis (KSoLA) has recently published the Dyslipidemia Fact Sheets in Korea 2020, which present up-to-date information on the epidemiology and management status of dyslipidemia based on nationally representative datasets. In this edition, we extended the analyses to adults aged 20 years or above to underscore the importance of primordial prevention.6 We firmly believe that these fact sheets can increase the public awareness of dyslipidemia and foster active collaboration among patients and healthcare professionals.
MATERIALS AND METHODS
1. Data source
The Dyslipidemia Fact Sheets in Korea 2020 analyzed 2 nationally representative datasets: the Korea National Health and Nutrition Examination Survey (KNHANES) and the National Health Insurance Big Data (NHI-BD). The KNHANES is an ongoing, nationwide surveillance system administered by the Korea Centers for Disease Control and Prevention that assesses health status and the distribution of chronic disease risk factors. It collects detailed information on demographics, disease status, lifestyle, anthropometric characteristics, and biochemical measurements from on-site health examinations.7 We analyzed adults aged 20 years or older with lipid measurements and information on physician diagnosis and treatment for dyslipidemia between 2007 and 2018. The National Health Insurance Service (NHIS) is the single provider of universal healthcare coverage in Korea. The NHI-BD contains sociodemographic information and health insurance claims data of the entire Korean population.8 We analyzed adults aged 20 years or older with insurance claims for dyslipidemia between 2002 and 2018. The study protocol was approved by the Institutional Review Board of Yonsei University Health System, Seoul, Korea (approval 4-2020-0207). The requirement for informed consent was waived, because this was a retrospective study of de-identified, routinely collected data.
2. Definitions of hypercholesterolemia and dyslipidemia: based on the KNHANES
Hypercholesterolemia was defined as a total cholesterol level ≥240 mg/dL or taking a lipid-lowering drug.9 Both crude and age-standardized prevalence were reported. Direct standardization was performed based on the 2005 Korean population structure provided by the Population and Housing Census, Statistics Korea. The awareness rate was defined as the proportion of people who self-reported a physician diagnosis of hypercholesterolemia among all people with hypercholesterolemia. The treatment rate was defined as the proportion of people taking lipid-lowering drugs ≥20 days per month among all people with hypercholesterolemia. Separate control rates were calculated for having total cholesterol <200 mg/dL among (1) all people with hypercholesterolemia and (2) people pharmacologically treated for hypercholesterolemia.
Hyper-low-density lipoprotein (LDL)-cholesterolemia was defined as a serum LDL-cholesterol level ≥160 mg/dL or taking a lipid-lowering drug. Hypo-high-density lipoprotein (HDL)-cholesterolemia was defined as a serum HDL-cholesterol level <40 mg/dL. Hypertriglyceridemia was defined as a serum triglyceride level ≥200 mg/dL. Dyslipidemia was then defined as satisfying one of the definitions stated above.9
3. Healthcare utilization for dyslipidemia: based on the NHI-BD
The diagnosis of dyslipidemia was defined as ≥1 health insurance claim with the International Classification of Diseases, 10th revision code E78 each year. Treatment was defined as ≥1 health insurance claim for a dyslipidemia diagnosis and a lipid-lowering drug prescription each year. Adherence to treatment was defined as being prescribed lipid-lowering drugs ≥290 days (80%) each year. Lipid-lowering drugs were classified as (1) statins, (2) ezetimibe, (3) fibrate, (4) omega-3 acid, or (5) others, including niacin or cholestyramine. If the regimen of lipid-lowering drugs had been switched, the one with the longest duration in the given year was selected as the representative regimen.
RESULTS
1. Prevalence and management of hypercholesterolemia
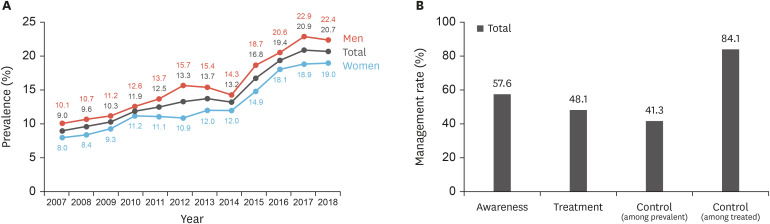
In 2018, the mean serum total cholesterol levels in adults aged 20 years or older were 192 mg/dL in men and 194 mg/dL in women (Supplementary Data 1, page 13). Between 2007 and 2018, the crude prevalence of hypercholesterolemia increased from 9.0% to 20.7% (Fig. 1A). The increase was particularly pronounced in the most recent 5 years, as the prevalence increased from 14.3% to 22.4% in men and from 12.0% to 19.0% in women. This increasing trend persisted after age-standardization (Supplementary Data 1, page 5). The rising prevalence was accompanied by an improvement in management status (Supplementary Data 1, pages 8-11). However, even in 2016–2018, only 57.6% of adults with hyperlipidemia were aware of their disease status and fewer than half (48.1%) received pharmacological treatment (Fig. 1B). Consequently, only 41.3% of all adults with hypercholesterolemia achieved a total cholesterol level <200 mg/dL (i.e., controlled). However, among adults undergoing treatment, 84.1% had controlled total cholesterol levels. Despite higher awareness and treatment rates in women, the control rate among those who were treated was higher in men.
Fig. 1. Prevalence and management of hypercholesterolemia in Korean adults.
(A) Crude prevalence of hypercholesterolemia in Korean adults, 2007–2018. (B) Management status of hypercholesterolemia in Korean adults, 2016–2018.
2. Prevalence of dyslipidemia
Overall, the prevalence of dyslipidemia was 45.6% in men and 31.3% in women (Supplementary Data 1, page 14), and increased with age (Fig. 2A). The prevalence was higher in men before the age of 60 years, whereafter the sex trend reversed (Fig. 2B). The prevalence of dyslipidemia was also higher among people with metabolic abnormalities; nearly 70% of people with diabetes and 60% of people with hypertension also had dyslipidemia (Supplementary Data 1, pages 22-24).
Fig. 2. Prevalence of dyslipidemia in Korean adults.
(A) Prevalence of dyslipidemia in Korean adults by age, 2016–2018 (p for trend: <0.0001). (B) Prevalence of dyslipidemia in Korean adults by sex and age, 2016–2018 (p for trend in men: <0.0001 and p for trend in women: <0.0001, respectively).
Based on the analyses of each lipid component, 19.2% of Korean adults had hyper-LDL-cholesterolemia, 16.1% had hypertriglyceridemia, and 17.7% had hypo-HDL-cholesterolemia (Supplementary Data 1, pages 16-21). Notably, 25.7% of men and 43.7% of women aged 60 years or older had hyper-LDL-cholesterolemia. A large sex difference in hypertriglyceridemia was observed among adults 40–49 years, in whom the prevalence was nearly 4 times higher in men (32.0%) than in women (7.9%).
3. Treatment for dyslipidemia
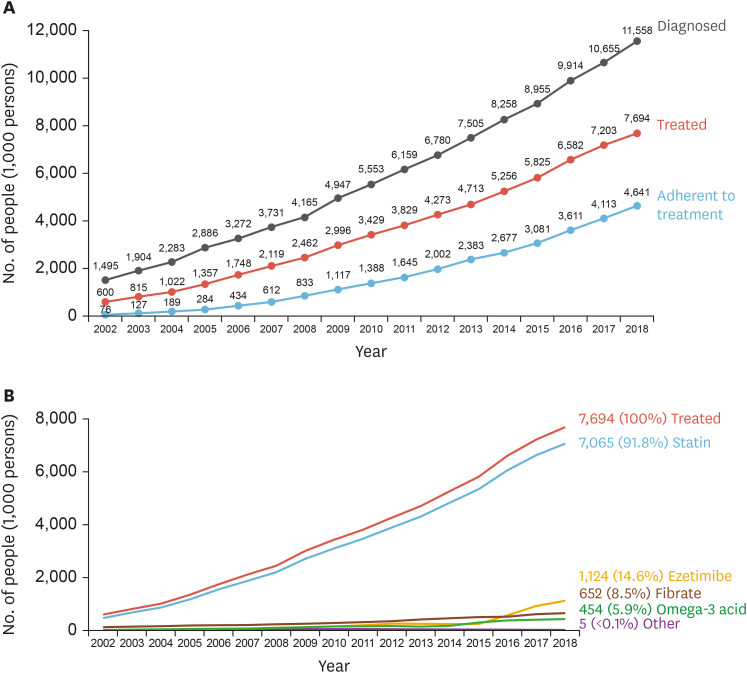
The number of people diagnosed with dyslipidemia increased nearly 8-fold from 1.5 million in 2002 to 11.6 million in 2018 (Fig. 3A). Naturally, the number of people receiving pharmacological treatment for dyslipidemia also rose to 7.7 million in 2018. Nearly 75% were simultaneously treated for hypertension, diabetes, or both (Supplementary Data 1, pages 28-29). However, only 4.6 million people were adherent to treatment, comprising approximately 40% of all patients with dyslipidemia.
Fig. 3. Diagnosis and treatment of dyslipidemia in Korean adults.
(A) Changes in the estimated number of Korean adults diagnosed, treated, and adherent to treatment for dyslipidemia, 2002–2018. (B) Changes in the estimated number of Korean adults with dyslipidemia by lipid-lowering drugs, 2002–2018.
Of the 7.7 million people treated for dyslipidemia in 2018, statins accounted for the majority of lipid-lowering drug prescriptions (Fig. 3B). In fact, 7.1 million people received statins, which accounted for 91.8% of total lipid-lowering prescriptions, followed by ezetimibe (14.6%), fibrate (8.5%), and omega-3 acid (5.9%). The use of dual therapy for dyslipidemia steadily increased to 18.6% in 2018 (Supplementary Data 1, pages 32-33). The most frequently used combination therapy was a statin plus ezetimibe, which accounting for 72% of dual therapy prescriptions (Supplementary Data 1, pages 36-37).
DISCUSSION
The Dyslipidemia Fact Sheets in Korea 2020 deliver an overview of the magnitude and management status of dyslipidemia in Korean adults aged 20 years or older. Overall, we observed a steady increase in dyslipidemia prevalence and dyslipidemia-related healthcare use. Simultaneously, the management status has also improved, but there remains room for improvement.
As suggested by clinical guidelines,9 it is critical for both patients and healthcare providers to initiate early and sustained management of suboptimal atherosclerotic CVD risk factors. As shown, the prevalence of hypercholesterolemia increased at an alarming rate in the last 5 years. By 2018, the prevalence of dyslipidemia reached 38.4%, which is comparable to the prevalence in other high-income (e.g., U.S., Japan) and neighboring (e.g., China) countries.10,11,12 This is unsurprising, as relevant lifestyle factors, such as physical activity and diet, have been worsening.13 In addition, the prevalence of dyslipidemia increased with age. This is of particular concern, as old age14 and longer exposure to elevated cholesterol levels15 are independently associated with CVD progression and treatment complications. Furthermore, the presence of dyslipidemia was common among people with diabetes or hypertension. The concurrent exposure to multiple metabolic abnormalities highlights the urgency for comprehensive cardiovascular health maintenance to prevent target organ damage.16
Despite the high prevalence, fewer than 60% of adults with hypercholesterolemia were aware of their condition. This requires immediate attention. A modest treatment rate relative to the awareness rate and a high control rate (approximately 85%) among treated individuals suggest that promoting awareness may effectively improve the population-level control of hypercholesterolemia. Indeed, a significant proportion of atherosclerotic CVD events are avoidable through primordial prevention, including smoking cessation,17 regular engagement in physical activity,18 and adherence to a healthy diet.19 Therefore, nationwide public health programs should consider early diagnosis and management across the entire age spectrum given their acceptable cost-effectiveness and minimal moral hazard. In healthcare settings, practitioners should actively work with patients to evaluate their circumstances for lifestyle modifications, to identify potential barriers (e.g., environmental factors), to implement measurable goals, and to monitor progress.5
The proportion of people on dual therapy among those treated for dyslipidemia has steadily increased since 2015, predominantly driven by an increase of statin plus ezetimibe combination therapy. This coincides with findings from the IMProved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT), in which the combination of a statin with ezetimibe improved cardiovascular outcomes compared with statin monotherapy after acute coronary syndrome.20 In addition, the increment in overall prescriptions of ezetimibe was almost entirely in the form of combination therapy, whereas ezetimibe monotherapy accounted for a negligible proportion. These findings are in alignment with the recent increase in combination therapy and expansion of reimbursement coverage for ezetimibe.
A substantial proportion (74%) of people treated for dyslipidemia received concurrent treatment for hypertension and/or diabetes. This proportion is expected to further increase with rapid population aging in Korea. Consequently, increasing healthcare expenditures will be inevitable. Moreover, patients will be burdened with multiple drug use, the risk of adverse drug reactions, or unexpected drug-drug interactions. A multidisciplinary approach may improve health outcomes with fewer complications among these high-risk populations.21
In conclusion, despite the established causal role of cholesterol levels in CVD progression, dyslipidemia continues to impose a considerable burden in Korea. In order to curb the rising dyslipidemia prevalence and to improve its management, monitoring trends in individual risk factors may provide evidence for tailored public health programs. In clinical settings, active communication and shared decision-making between healthcare practitioners and patients are essential for fulfilling the guideline recommendations. This mutual participation may be fostered by personalized interventions that account for individuals' health and socioenvironmental background.
Footnotes
Funding: This study was supported by the Korean Society of Lipid and Atherosclerosis.
Conflict of Interest: The authors have no conflict of interest to declare.
- Conceptualization: Cho SMJ, Lee H, Lee HH, Joo HJ, Hong SJ, Kim HC.
- Data curation: Cho SMJ, Lee H, Lee HH, Kim HC.
- Formal analysis: Cho SMJ, Lee H, Lee HH, Baek J, Heo JE.
- Funding acquisition: Joo HJ, Hong SJ, Kim HC.
- Investigation: Cho SMJ, Lee H, Lee HH, Baek J, Heo JE, Joo HJ, Hong SJ, Kim HC.
- Methodology: Cho SMJ, Lee H, Lee HH, Baek J, Heo JE, Hong SJ, Kim HC.
- Project administration: Lee H, Joo HJ, Hong SJ, Kim HC.
- Resources: Kim HC.
- Supervision: Lee H, Hong SJ, Kim HC.
- Validation: Cho SMJ, Lee H, Lee HH, Kim HC.
- Visualization: Cho SMJ, Lee H.
- Writing - original draft: Cho SMJ, Lee H, Lee HH.
- Writing - review & editing: Cho SMJ, Lee H, Lee HH, Baek J, Heo JE, Joo HJ, Hong SJ, Kim HC.
SUPPLEMENTARY MATERIAL
Dyslipidemia fact sheets in Korea, 2020
References
- 1.GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee SW, Kim HC, Lee HS, Suh I. Thirty-year trends in mortality from cardiovascular diseases in Korea. Korean Circ J. 2015;45:202–209. doi: 10.4070/kcj.2015.45.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee YR, Cho B, Jo MW, Ock M, Lee D, Lee D, et al. Measuring the economic burden of disease and injury in Korea, 2015. J Korean Med Sci. 2019;34:e80. doi: 10.3346/jkms.2019.34.e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roth GA, Nguyen G, Forouzanfar MH, Mokdad AH, Naghavi M, Murray CJ. Estimates of global and regional premature cardiovascular mortality in 2025. Circulation. 2015;132:1270–1282. doi: 10.1161/CIRCULATIONAHA.115.016021. [DOI] [PubMed] [Google Scholar]
- 5.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e563–e595. doi: 10.1161/CIR.0000000000000677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gooding HC, Gidding SS, Moran AE, Redmond N, Allen NB, Bacha F, et al. Challenges and opportunities for the prevention and treatment of cardiovascular disease among young adults: report from a National Heart, Lung, and Blood Institute Working Group. J Am Heart Assoc. 2020;9:e016115. doi: 10.1161/JAHA.120.016115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017;46:799–800. doi: 10.1093/ije/dyw253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhee EJ, Kim HC, Kim JH, Lee EY, Kim BJ, Kim EM, et al. 2018 Guidelines for the management of dyslipidemia. Korean J Intern Med. 2019;34:723–771. doi: 10.3904/kjim.2019.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics. National Health and Nutrition Examination Survey (NHANES) public use data files. Centers for Disease Control and Prevention website [Internet] Hyattsville (MD): National Center for Health Statistics; c2021. [accessed on 15 February 2021]. Available from: https://www.cdc.gov/nchs/nhanes/ [Google Scholar]
- 11.Ministry of Health, Labour, and Welfare. National Health and Nutrition Survey in Japan [Internet] Tokyo: Ministry of Health, Labour, and Welfare; 2015. [accessed on 15 February 2021]. Available from: http://www.mhlw.go.jp/toukei/itiran/gaiyo/k-eisei.html. [Google Scholar]
- 12.Huang Y, Gao L, Xie X, Tan SC. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Popul Health Metr. 2014;12:28. doi: 10.1186/s12963-014-0028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee HJ, Suh B, Yoo TG, Lee H, Shin DW. Trends in cardiovascular health metrics among Korean adults. Korean J Fam Med. 2013;34:403–412. doi: 10.4082/kjfm.2013.34.6.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ho CK, Walker SW. Statins and their interactions with other lipid-modifying medications: safety issues in the elderly. Ther Adv Drug Saf. 2012;3:35–46. doi: 10.1177/2042098611428486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shapiro MD, Bhatt DL. “Cholesterol-Years” for ASCVD risk prediction and treatment. J Am Coll Cardiol. 2020;76:1517–1520. doi: 10.1016/j.jacc.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1046–e1081. doi: 10.1161/CIR.0000000000000624. [DOI] [PubMed] [Google Scholar]
- 17.Verbiest M, Brakema E, van der Kleij R, Sheals K, Allistone G, Williams S, et al. National guidelines for smoking cessation in primary care: a literature review and evidence analysis. NPJ Prim Care Respir Med. 2017;27:2. doi: 10.1038/s41533-016-0004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orrow G, Kinmonth AL, Sanderson S, Sutton S. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012;344:e1389. doi: 10.1136/bmj.e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 20.Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387–2397. doi: 10.1056/NEJMoa1410489. [DOI] [PubMed] [Google Scholar]
- 21.Lalonde L, Goudreau J, Hudon É, Lussier MT, Bareil C, Duhamel F, et al. Development of an interprofessional program for cardiovascular prevention in primary care: a participatory research approach. SAGE Open Med. 2014;2:2050312114522788. doi: 10.1177/2050312114522788. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Dyslipidemia fact sheets in Korea, 2020