Abstract
Background:
Although many studies demonstrated reduced mortality risk with higher greenness, few studies examined the modifying effect of greenness on air pollution–health associations. We evaluated residential greenness as an effect modifier of the association between long-term exposure to fine particles (PM2.5) and mortality.
Methods:
We used data from all Medicare beneficiaries in North Carolina (NC) and Michigan (MI) (2001–2016). We estimated annual PM2.5 averages using ensemble prediction models. We estimated mortality risk per 1 μg/m3 increase using Cox proportional hazards modeling, controlling for demographics, Medicaid eligibility, and area-level covariates. We investigated health disparities by greenness using the Normalized Difference Vegetation Index (NDVI) with measures of urbanicity and socioeconomic status.
Results:
PM2.5 was positively associated with mortality risk. Hazard ratios (HRs) were 1.12 (95% confidence interval (CI) 1.12, 1.13) for NC and 1.01 (95% CI 1.00, 1.01) for MI. HRs were higher for rural than urban areas. Within each category of urbanicity, HRs were generally higher in less green areas. For combined disparities, HRs were higher in low greenness or low SES areas, regardless of the other factor. HRs were lowest in high-greenness and high-SES areas for both states.
Conclusions:
In our study, those in low SES and high greenness areas had lower associations between PM2.5 and mortality than those in low SES and low greenness areas. Multiple aspects of disparity factors and their interactions may affect health disparities from air pollution exposures. Findings should be considered in light of uncertainties, such as our use of modeled PM2.5 data, and warrant further investigation.
Keywords: Air pollution, Health disparities, Mortality, Residential greenness, SES, Urbanicity
Introduction:
Epidemiologic studies have consistently reported associations between long-term exposure to fine particles and mortality.1–5 Previous reviews of studies covering wide geographic areas indicate higher risk of all-cause mortality associated with higher long-term PM2.5 exposure, with substantial heterogeneity across studies.6,7 Differences in several characteristics such as particle composition, populations, and methodologies may explain observed heterogeneity.5,8 However, comparatively fewer studies evaluated which factors modify associations of long-term PM2.5 exposure and mortality. Better understanding of the factors that may contribute to differences in health impacts, and their interactions, would aid decision-makers in establishing more efficient policy to address PM2.5 and vulnerable populations.
A growing body of literature on direct effect of greenness demonstrates associations of higher greenness with reduced risk of mortality.9–11 Green space promotes physical activity, psychological well-being, and general public health.12 Unequal distribution and access to green space is increasingly recognized as an environmental justice issue.13 However, few studies examined residential greenness as an effect modifier of air pollution–health associations.14–16 One study reported decreasing risks of PM2.5-related mortality with increased greenness.17 Another study found that the association between air pollution and cardiovascular mortality was reduced by higher greenness in areas with low socioeconomic status (SES).18 Previous findings on residential greenness as an effect modifier of air pollution’s impact on health are inconsistent, with limited studies showing conflicting results. One study found lower PM10 impacts on non-accidental mortality in less green areas.19 Other work found no evidence of effect modification by neighborhood greenspace on the association between air pollution and stroke.20
Some studies suggested regional differences by urbanicity in PM2.5 health effects.21,22 Most epidemiologic studies investigating air pollution and health were conducted in urban areas as most regulatory ambient monitors are located in populated areas; rural areas are underrepresented. PM2.5 health effects in rural areas may differ from those in urban centers due to different characteristics of exposure and/or population (e.g. PM composition, baseline health status, health care access, health behaviors, and other environmental factors). For example, greenness types and quality may differ by urban and rural features. Research is needed including on nonurban areas and differences between urban and rural areas.
We selected the relatively large and diverse states of North Carolina (NC) and Michigan (MI) with geographies that include extensive agricultural regions and forests, coastal areas, and multiple medium-large urban cities. Both states are heterogeneous in social and environmental characteristics (e.g., poverty patterns, urban–rural population distribution, economic systems).
We evaluated residential greenness as an effect modifier for long-term PM2.5 exposure and mortality for Medicare beneficiaries in NC and MI. We considered differences by urban versus rural areas and investigated combined disparities by greenness and SES.
Methods
Data
We obtained the Medicare beneficiary denominator file from the Centers for Medicare and Medicaid Services (CMS), for Medicare enrollees (≥65 years). We constructed an open cohort of all Medicare beneficiaries residing in NC and MI for 2001–2016, with individual-level data on sex, race, age, residential ZIP code, eligibility for Medicaid, and date of death. This study was approved by the Institutional Review Board of the Harvard T. H. Chan School of Public Health. We estimated ambient PM2.5 levels at 1×1km resolution using previously published ensemble modeling that integrated multiple machine learning algorithms and predictor variables including satellite data, meteorologic variables, land-use variables, elevation, and chemical transport model predictions.23 We generated PM2.5 predictions by an ensemble of three machine learning algorithms including neural network, random forest, and gradient boosting. We used geographically weighted generalized additive modeling to combine PM2.5 predictions from each learner. The model achieved excellent performance, with high agreement between monitored and predicted PM2.5.23
We used annual ZIP-code level averages of maximum daily temperatures and relative humidity based on area-weighted averaging of 4×4km gridded rasters from Gridmet via Google Earth Engine (https://developers.google.com/earth-engine/datasets/catalog/IDAHO_EPSCOR_GRIDMET). For each calendar year (2001–2016), we assigned long-term PM2.5 exposure as annual average concentration. Annual average maximum daily temperature and relative humidity were based on residential ZIP code.
We estimated greenness using Normalized Difference Vegetation Index (NDVI) derived from the Moderate Resolution Imaging Spectroradiometer (MODIS) sensor aboard the Terra satellite image from NASA’s Earth Observing System. We used global MODIS product MOD13Q1 version 5, which has been corrected for atmospheric contamination from water, clouds, and aerosols. This product is a 16-day composite at 250m spatial resolution. NDVI is an indicator of amount of vegetation cover and defined as the ratio of the difference between near-infrared reflectance and red visible reflectance to their sum. NDVI values range from −1 to +1; values close to +1 indicate high density of greenness; −1 represents water features. Areas with no vegetation have NDVI close to zero and very low NDVI (<0.1) represents barren areas of rock, sand, or snow; moderate values (0.2–0.3) represent shrub and grassland, and higher values indicate higher density of vegetation.24 We calculated average NDVI by ZIP code and year. We categorized greenness as tertiles of low, medium, and high.
We used ZIP code level variables from 2010 Census data: percentage Black, percentage Hispanic, median household income, percentage >65 years living below the poverty level, and population density. We used urbanicity classification (i.e., urbanized areas, urban clusters, and rural) based on 2010 Census data. Census categorization includes two types of urban areas: 1) Urbanized Areas (UAs) of ≥50,000 people; and 2) Urban Clusters (UCs) of >2,500 and <50,000 people; rural areas are defined as those not included within an UA or UC.
Statistical analysis
We applied Cox proportional hazard models to estimate hazard ratios (HRs) of mortality relative to long-term PM2.5. Standard Cox proportional hazards models assume HR as independent of time. However, environmental exposures such as air pollution are time-dependent, so we used an extended Cox model with time-dependent variables, which requires no proportional hazards assumptions. Use of time-dependent survival methods allows exposure for survivors at the time of each death and ensures that effects are examined relative to other participants for the same follow-up interval. We calculated person–years from enrollment year to date of death or end of follow-up. Models were controlled for individual-level sex, race/ethnicity (Non-Hispanic White, Non-Hispanic Black, other), age (65–69, 70–74, 75–79, 80–84, 85+ years), Medicaid eligibility as a proxy for individual-level SES, area-level percentage Black, percentage Hispanic, median household income, percentage >65 years living in poverty, and population density, in addition to the regional cluster variable that could relate to compositional differences in PM2.5, and year. We assessed potential effect modification by residential greenness and several factors (e.g., SES, urbanicity).
We evaluated combined disparities of greenness and SES (e.g., low SES neighborhood with low greenness), and greenness and urbanicity (e.g., urban green vs. rural green). SES group was based on lowest and highest quartiles of median household income. Greenness was divided into tertiles (low, medium, high) within each urbanicity group in each state. We performed additional analysis: (1) using the same cutoffs of greenness to categorize greenness across all urbanicity groups in each state; and (2) using the same cutoffs for tertiles of greenness across states. We conducted sensitivity analysis to examine robustness of effect modification of estimates using PM2.5 monitor values rather than prediction modeling estimates. We stratified by state, disparity factor, and combinations of factors. We present results for increments of 1 μg/m3 PM2.5. We used SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Figure 1 shows spatial distributions of PM2.5, NDVI, and urban and rural areas in NC and MI. High urban areas generally had higher PM2.5 and low greenness in both states.
Figure 1.
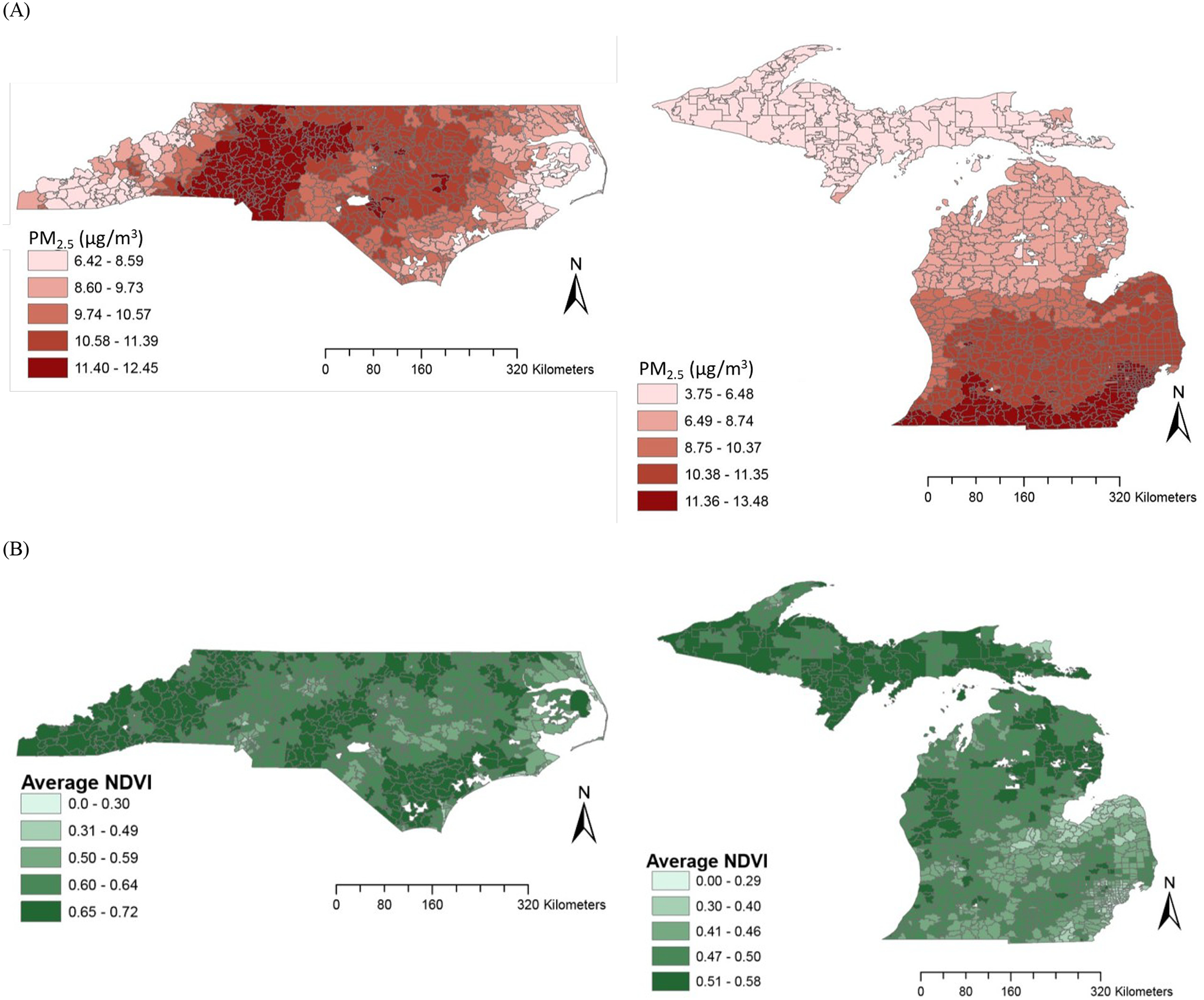
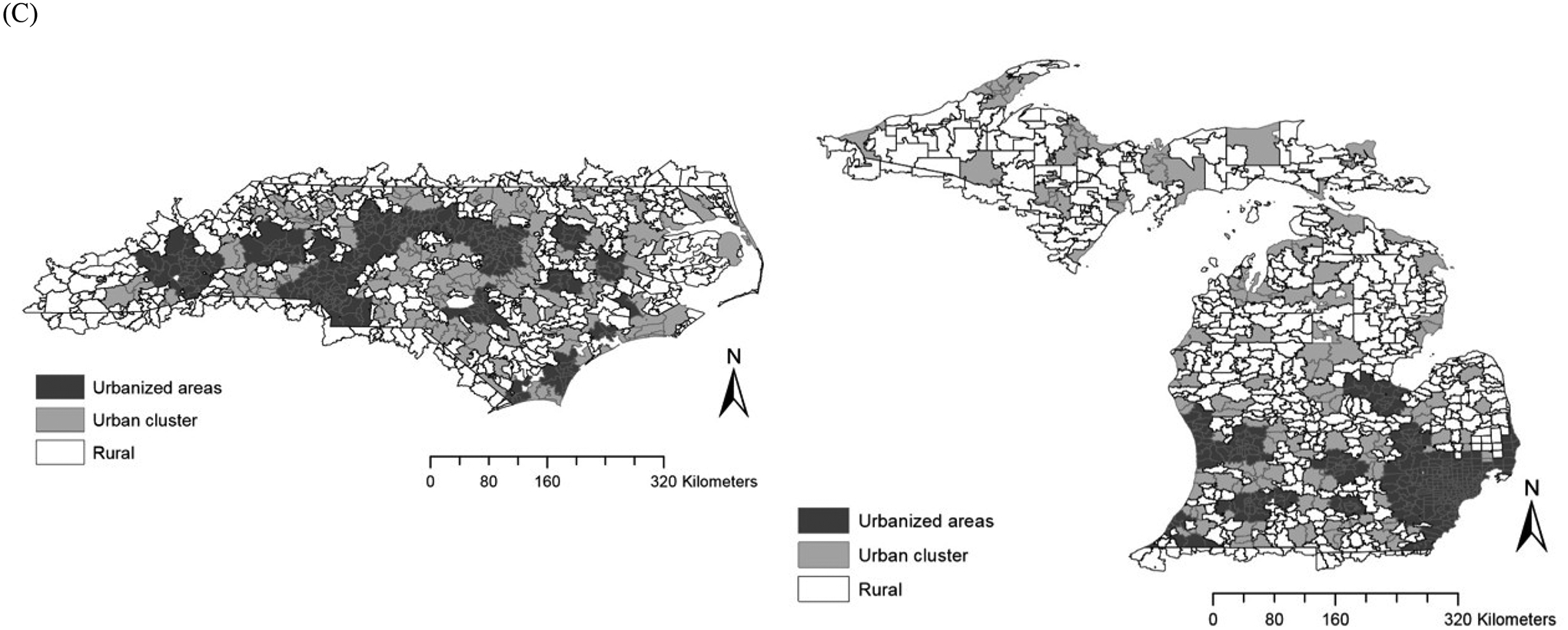
Spatial distribution of (A) annual average PM2.5 (2001–2016), (B) annual average NDVI (2001–2016), and (C) urban and rural areas in North Carolina and Michigan
Our cohort consisted of 1,263,689 participants for NC and 1,318,558 for MI. The total number of deaths was 179,329 (14.2%) for NC and 187,802 (14.2%) for MI. Table 1 provides distributions of greenness and PM2.5 by greenness group by state. Annual average PM2.5 during the study period ranged from 3.61 to 15.73 μg/m3 for NC and 1.80 to 17.33 μg/m3 for MI. PM2.5 concentrations were lower in areas with higher greenness for both states. Annual average PM2.5 concentrations were 8.78 for those living in low-green areas and 7.63 μg/m3 for high green areas in NC and 8.75 in low and 7.55 μg/m3 in high green areas for MI. Average greenness values in total and by greenness group were lower for MI than NC, with similar mean values in the lowest greenness group for NC (0.55) and the highest greenness group in MI (0.52).
Table 1.
Distribution of greenness and PM2.5 concentration by greenness group in North Carolina and Michigan, 2001–2016.
| Mean | SD | Min | 25% | 50% | 75% | Max | IQRw | ||
|---|---|---|---|---|---|---|---|---|---|
| NC | |||||||||
| NDVI | Total | 0.62 | 0.07 | 0.00 | 0.60 | 0.63 | 0.66 | 0.74 | 0.06 |
| Low | 0.55 | 0.08 | 0.00 | 0.54 | 0.58 | 0.60 | 0.61 | 0.05 | |
| Medium | 0.63 | 0.01 | 0.61 | 0.62 | 0.63 | 0.64 | 0.65 | 0.02 | |
| High | 0.67 | 0.02 | 0.65 | 0.66 | 0.67 | 0.69 | 0.74 | 0.03 | |
| PM2.5 | Total | 8.30 | 1.45 | 3.61 | 7.63 | 8.35 | 8.89 | 15.73 | 1.25 |
| Low | 8.78 | 1.37 | 4.16 | 8.00 | 8.54 | 9.09 | 15.73 | 1.09 | |
| Medium | 8.49 | 1.24 | 4.02 | 8.00 | 8.44 | 8.85 | 15.12 | 0.85 | |
| High | 7.63 | 1.47 | 3.61 | 6.64 | 7.76 | 8.55 | 15.10 | 1.91 | |
| MI | |||||||||
| NDVI | Total | 0.46 | 0.06 | 0.00 | 0.42 | 0.48 | 0.50 | 0.62 | 0.08 |
| Low | 0.39 | 0.04 | 0.00 | 0.37 | 0.40 | 0.42 | 0.45 | 0.05 | |
| Medium | 0.47 | 0.01 | 0.45 | 0.46 | 0.48 | 0.49 | 0.49 | 0.03 | |
| High | 0.52 | 0.02 | 0.49 | 0.50 | 0.51 | 0.53 | 0.62 | 0.02 | |
| PM2.5 | Total | 8.23 | 1.57 | 1.80 | 7.53 | 8.05 | 9.01 | 17.33 | 1.47 |
| Low | 8.75 | 1.61 | 1.80 | 7.63 | 8.32 | 9.53 | 17.33 | 1.90 | |
| Medium | 8.39 | 1.31 | 2.98 | 7.69 | 8.11 | 9.15 | 16.15 | 1.45 | |
| High | 7.55 | 1.50 | 2.77 | 6.97 | 7.84 | 8.14 | 15.57 | 1.18 | |
Greenness was divided in groups of low, medium, and high as tertiles; state-specific cutoffs for greenness group: low (<0.61), medium (0.61–0.65), and high (≥0.65) for NC; low (<0.45), medium (0.45–0.49), and high (≥0.49) for MI
SD indicates standard deviation; Min, minimum; Max, maximum; IQRw interquartile range width; NDVI, Normalized Difference Vegetation Index
Table 2 shows characteristics of the study population. Generally, distribution trends of individuals by sex, average age at entry, percentage Hispanic, and percentage Black were similar across greenness group for both states. However, we observed distinct spatial patterns for racial distribution or poverty patterns by greenness group. Distributions by race/ethnicity and eligibility for Medicaid showed similar patterns for both states, with higher percentage of Non-Hispanic Black and Medicaid eligibility in the low greenness group; however, the pattern by greenness group was more substantial in MI than NC. For example, in NC, the percentage of Non-Hispanic Blacks living in areas with low greenness was 44.8%, compared with 74.5% in MI. For median household income and poverty, we found opposite patterns across greenness groups in NC compared with MI. In NC, community-level SES was lower in the highest greenness group. Those living in high greenness areas lived in neighborhoods with lower SES (i.e., median household income was lower and percent of persons living in poverty was higher in high greenness areas), whereas neighborhood-level SES was lower in the lowest greenness group for MI (i.e., median household income was lower and percent of persons living in poverty was higher in low greenness areas).
Table 2.
Characteristics of study population in North Carolina and Michigan
| Characteristics | NC | MI | ||||||
|---|---|---|---|---|---|---|---|---|
| Entire cohort | Greenness | Entire cohort | Greenness | |||||
| Low | Medium | High | Low | Medium | High | |||
| Population | ||||||||
| Persons | 1,263,689 | 418,701 | 423,138 | 421,850 | 1,318,558 | 438,905 | 437,486 | 442,167 |
| Total deaths | 179,329 | 77,262 (43.1) | 61,322 (34.2) | 40,745 (22.7) | 187,802 | 99,369 (52.9) | 55,107 (29.3) | 33,326 (17.8) |
| Sex (n, %) | ||||||||
| Male | 590,491 | 194,456 (32.9) | 196,645 (33.3) | 199,390 (33.8) | 626,913 | 204,119 (32.6) | 207,807 (33.2) | 214,987 (34.3) |
| Female | 673,198 | 224,245 (33.3) | 226,493 (33.6) | 222,460 (33.1) | 691,645 | 234,786 (34.0) | 229,679 (33.2) | 227,180 (32.9) |
| Race/ethnicity (n, %) | ||||||||
| Non-Hispanic White | 1,002,786 | 301,553 (30.1) | 337,288 (33.6) | 363,945 (36.3) | 1,111,015 | 306,751 (27.6) | 390,603 (35.2) | 413,661 (37.2) |
| Non-Hispanic Black | 209,785 | 93,990 (44.8) | 69,808 (33.3) | 45,987 (21.9) | 147,540 | 109,938 (74.5) | 26,195 (17.8) | 11,407 (7.7) |
| Others | 51,118 | 23,158 (45.3) | 16,042 (31.4) | 11,918 (23.3) | 60,003 | 22,216 (37.0) | 20,688 (34.5) | 17,099 (28.5) |
| Age at entry (mean, years) | 65.1 | 65.1 | 65.1 | 65.0 | 65.1 | 65.2 | 65.1 | 65.1 |
| Eligible for Medicaid (n, %) | 164,618 | 60,678 (36.9) | 53,361 (32.4) | 50,579 (30.7) | 123,194 | 62,827 (51.0) | 32,717 (26.6) | 27,650 (22.4) |
| Median household income (1000s of $) | 49.5 | 51.7 | 50.5 | 46.3 | 53.9 | 46.5 | 57.1 | 58.2 |
| Below poverty level (%) | 9.8 | 9.7 | 9.4 | 10.2 | 8.1 | 10.7 | 6.8 | 6.8 |
| Population density (persons/mile2) | 703.6 | 1267.5 | 624.3 | 223.4 | 1603.5 | 3277.9 | 994.8 | 544.4 |
| Population (%) | ||||||||
| Hispanic | 7.8 | 8.8 | 8.5 | 6.0 | 4.0 | 4.8 | 4.2 | 3.0 |
| Black | 19.1 | 25.6 | 19.4 | 12.4 | 12.6 | 26.9 | 7.2 | 3.7 |
| Meteorological variables | ||||||||
| Temperature (°C) | 22.2 (1.5) | 22.6 (1.0) | 22.3 (1.4) | 21.7 (1.9) | 15.4 (1.4) | 15.5 (1.2) | 15.5 (1.4) | 15.1 (1.6) |
| Relative humidity (%) | 88.2 (2.5) | 87.6 (2.9) | 88.1 (2.1) | 89.0 (2.2) | 89.0 (3.1) | 87.2 (2.9) | 89.5 (2.6) | 90.3 (2.9) |
Greenness was divided in groups of low, medium, and high as tertiles; state-specific cutoffs for greenness group: low (<0.61), medium (0.61–0.65), and high (≥0.65) for NC; low (<0.45), medium (0.45–0.49), and high (≥0.49) for MI
eTables 1 and 2 present correlations between study variables by state. NDVI in NC was negatively correlated with population density. Median household income was negatively correlated with poverty and education. Poverty and education were positively correlated. In MI, NDVI was positively correlated with humidity and median household income and negatively correlated with percentage Black, population density, poverty, and low education (less than high school). The link between higher NDVI and lower population density was stronger in MI (r=−0.69) than NC (r=−0.43).
We observed positive associations overall between PM2.5 and mortality in both states (Table 3). HRs between PM2.5 and mortality were 1.12 (95% confidence interval (CI) 1.12, 1.13) for NC and 1.01 (95% CI 1.00, 1.01) for MI. The higher overall risks associated with PM2.5 exposure were more pronounced in NC than in MI. Findings across greenness groups showed that higher greenness was associated with protective (i.e., beneficial) effects of PM2.5 on mortality for both states. Living in high greenness areas was associated with lower PM2.5-associated mortality risk compared to living in areas with low greenness for both states.
Table 3.
Associations between long-term exposure to PM2.5 and total mortality across greenness groups in North Carolina and Michigan
| HR (95% CI) | ||
|---|---|---|
| NC | MI | |
| Total | 1.12 (1.12–1.13) | 1.01 (1.00–1.01) |
| Greenness | ||
| Low | 1.10 (1.09–1.12) | 1.06 (1.05–1.07) |
| Medium | 1.18 (1.17–1.20) | 0.93 (0.92–0.94) |
| High | 0.98 (0.97–0.99) | 0.96 (0.94–0.97) |
HR calculated per 1 μg/m3 for PM2.5; Models were stratified by greenness groups.
Greenness was divided in groups of low, medium, and high as tertiles in each state; state-specific cutoffs for greenness group: low (<0.61), medium (0.61–0.65), and high (≥0.65) for NC; low (<0.45), medium (0.45–0.49), and high (≥0.49) for MI
N for low 418,701 persons, medium 423,138 persons, and high greenness 421,850 persons for NC; low 438,905 persons, medium 437,486 persons, and high greenness 442,167 persons for MI
Adjusted for sex, race, age group, Medicaid eligibility, cluster of PM2.5 composition, year, temperature, relative humidity, percentage Black, percentage Hispanic, median household income, percent below poverty, and population density
Figure 2 and eTables 3–5 show HRs for PM2.5–mortality associations by urbanicity and greenness. Associations were higher in less urbanized areas than urban areas for both states, although effect estimates were slightly higher for urban clusters than rural areas. Within each urbanicity category, HRs were generally higher in less green areas for both states. Additional analysis using the same cutoffs for greenness across all urbanicity groups provided generally similar results (eTable 6).
Figure 2.
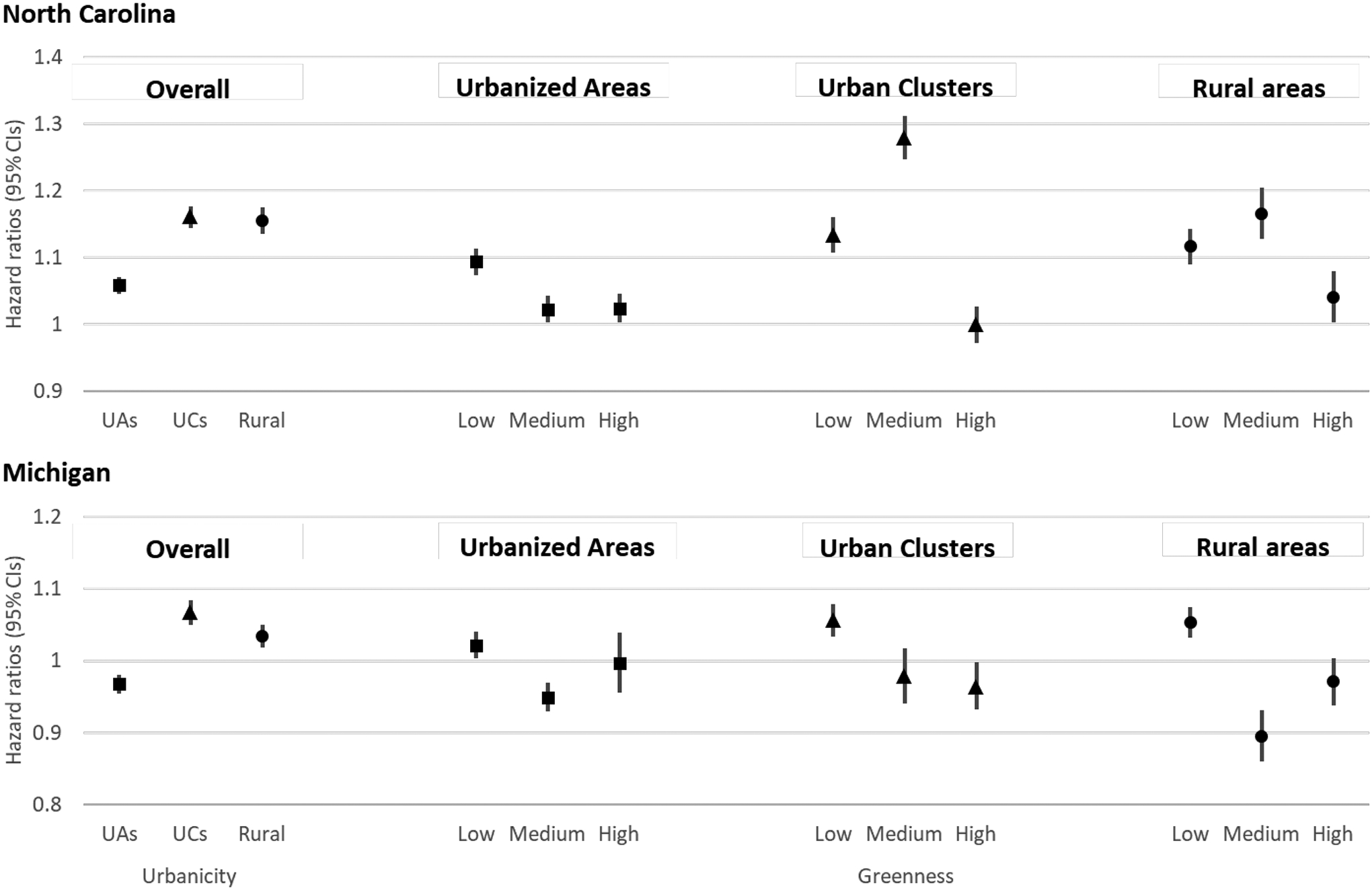
Estimated effects of PM2.5 on mortality by urbanicity (overall, urbanized areas, urban clusters, rural areas) and level of greenness (low, medium, high) in North Carolina and Michigan
Note: Hazard ratio (HR) calculated per 1 μg/m3 for PM2.5. Urbanicity classification (i.e., urbanized areas, urban clusters, and rural) was based on 2010 Census data (Urbanized Areas (UAs) of 50,000 or more people; Urban Clusters (UCs) of at least 2,500 and less than 50,000 people. Rural areas are defined as all population, housing, and territory not included within an urbanized area or urban cluster). Levels of greenness were defined separately by state; greenness was divided in groups of low, medium, and high as tertiles.
In stratified analysis by combinations of greenness and SES (Figure 3, eTable 7), we found that regardless of each factor (i.e., greenness and SES), those in high SES or high greenness areas had lower PM2.5–mortality risks than those in low SES or low greenness areas. People in both high greenness and high SES areas had lower PM2.5–mortality associations for both states. Similarly, those in both low SES and low greenness areas had the highest estimated PM2.5–mortality effects for both states.
Figure 3.
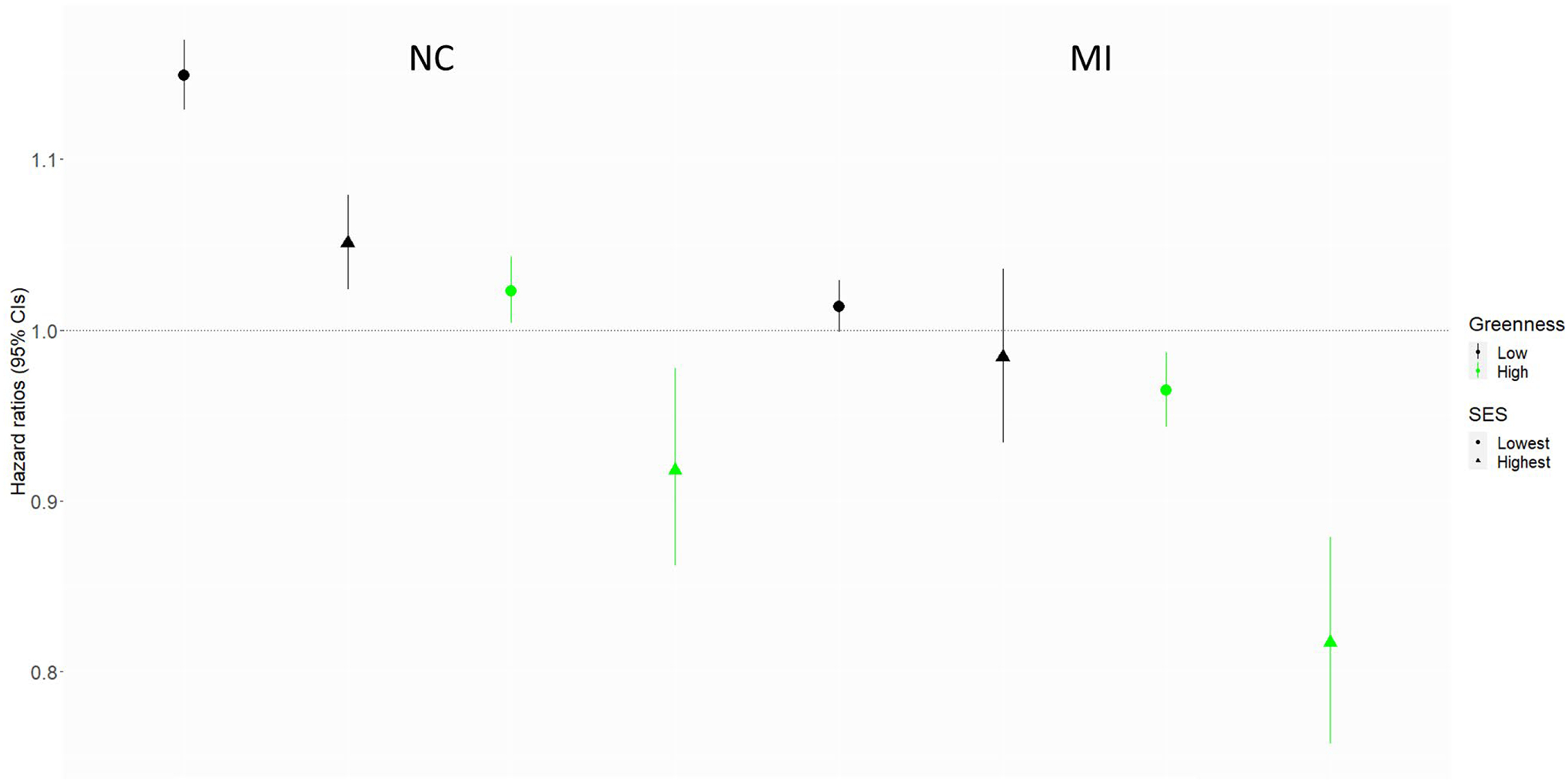
Effects of PM2.5 on mortality by greenness and socioeconomic status (SES) in North Carolina and Michigan.
Note: Hazard ratio (HR) calculated per 1 μg/m3 for PM2.5. SES group was based on the lowest and highest quartiles of median household income. The shape of the central estimate indicates SES (circle for lowest quartile, triangle for highest quartile of median household income); the color of the result indicates level of greenness (black for low, green for high).
As a sensitivity analysis, we compared effect modification by greenness using PM2.5 monitor versus PM2.5 prediction estimates, for the subset of areas with monitors. Distributions of PM2.5 concentration for total and by greenness were substantially similar between predicted and measured values for both states (eTable 8). Effect estimates for total area and by greenness group showed generally similar patterns between PM2.5 prediction estimates and monitor values for both states (eTable 9). Results using the same cutoff for greenness across states showed similar patterns with original findings, which used state-specific cutoffs for most groups; however, we found different findings for the high greenness group in NC due to the relatively low cutoff for high greenness group (eTables 10 and 11). This indicates that the approach using the same cutoffs across states may not reflect relative greenness across areas.
Discussion
We investigated effect modification by residential greenness for long-term PM2.5 exposure and mortality for Medicare beneficiaries in NC and MI. We considered differences by urban versus rural areas and evaluated combined disparities by greenness and SES. We observed positive associations between long-term PM2.5 exposure and mortality in both NC and MI. Our findings show generally protective effects of greenness on PM2.5–mortality associations in both states. When we looked at combined disparities by urbanicity and greenness, HRs were higher for rural than urban areas. Within each category of urbanicity (urbanized areas, urban clusters, rural areas), HRs were generally higher in areas with less greenness. Associations between PM2.5 and mortality were higher in low greenness or low SES areas, regardless of the other factor. In particular, positive associations between PM2.5 and mortality were lower in areas with both high greenness and high SES.
Our results indicating positive associations between long-term PM2.5 exposure and mortality in NC and MI are consistent with previous studies.1,14,25–27 A recent nationwide cohort study of persons ≥65 years in China reported positive associations between long-term PM2.5 exposure and all-cause mortality over a broad range of PM2.5 concentrations.4 Another study examining a large cohort of Medicare beneficiaries (≥65 years) in seven southeastern US states identified positive associations between long-term PM2.5 and mortality.5 Despite differences in study population and methods, previous findings were generally similar to our results.
Our estimates indicate potential beneficial associations of PM2.5 with mortality in high greenness areas for NC and MI, which warrants further study. The distribution of PM2.5 was similar across greenness groups. This indicates that greenness may be an effect modifier rather than confounder in PM2.5–mortality associations. Alternatively, PM2.5’s chemical composition in high greenness areas may differ from that in other areas, even if overall PM2.5 levels are roughly similar. There may exist differences in PM2.5 sources across areas with different greenness levels. Consistent with our findings, previous studies examining greenness as an effect modifier of PM2.5–mortality associations in Canada observed no PM2.5–mortality association in the two greenest quintiles.17
Higher greenness exposure may benefit health through several pathways such as mitigation of air pollution, heat, and noise; increased immune system by psychological restoration for stress and anxiety; and increased physical activity and social cohesion.12, 28 For example, vegetation may reduce air pollution exposure through direct filtering of pollutants such as particles, sulfur dioxide, and carbon monoxide or open spaces may influence indirectly through improving urban air circulation patterns affecting the dispersal of pollutants.11,29 High greenness areas may provide generally less-stressful environments with lower noise and cooler temperature.13 Another possible mechanism is the environmental biodiversity hypothesis suggesting that contact with nature is beneficial for human microbial and immunomodulatory capacity.30
We found generally higher PM2.5–mortality associations in NC than MI. This may result from several factors such as different populations and/or environmental characteristics across regions and their interactions. We found different correlations among variables between the two states, including for correlation between greenness and other covariates. Also, we observed distinct spatial patterns of racial distribution or poverty by greenness group by state. For example, in NC, community-level SES was lower in the highest greenness group, whereas neighborhood-level SES was lower in the lowest greenness group for MI. Another possible reason for different magnitude of effect estimates is within-area variation of exposure and/or within-area distribution of SES across regions. However, although the magnitude of effect estimates differed by state, we observed generally similar patterns of associations by urbanicity, and across greenness groups for both states. Several previous studies found high PM-mortality associations in greener areas.2,14,17 Different patterns of effect estimates by region within a given level of greenness and between areas with high and low greenness may involve several factors such as greenness assessment and differences in health behavior of people living in high vs. low green areas. Greenness measures such as NDVI do not reflect different types of greenness, quality, size, and accessibility, which may differ between the states. Also, potential benefits of greenness could be affected by other factors such as healthy lifestyles, smoking or drinking patterns, and car dependency. Further studies in different locations are needed to evaluate the role of residential greenness in air pollution–health outcomes associations.
Although evidence on the direct effect of greenness and health outcomes is well documented, relatively few studies have been conducted on effect modification by residential greenness in the air pollution–health associations and such findings on effect modification by greenness are inconsistent. We observed that people in low greenness areas had higher risks of death associated with PM2.5 than those in higher greenness areas. Although the distributions of some of demographic characteristics and several indicators of SES across greenness group showed different patterns between NC and MI, we observed generally similar patterns of associations by urbanicity, and across greenness group for both states. Consistent with our findings, a recent study by Sun et al.16 examined the modifying effect of residential greenness on the air pollution–respiratory mortality association. They found that elders living in low greenness areas had higher risk of pneumonia mortality associated with air pollution than those living in higher greenness areas. On the other hand, Kioumourtzoglou et al.25 examined effect modification by greenness on the PM2.5–mortality association in 207 U.S. cities and reported that those living in the highest greenness area had the highest effect estimates, with positive correlations between greenness and some variables such as proportion of black or elderly residents and smoking rates. de Keijzer et al.14 found higher greenness was associated with lower mortality only in areas with lower SES. Another study reported no evidence of effect modification by greenness.20
In this study, we found higher effect of PM2.5 exposure on mortality in less urban areas. The associations were higher in less urbanized areas than those for urbanized areas for both states, although the effect estimates for urban clusters were slightly higher than those for rural areas. Several studies have reported higher health effects of air pollution in rural areas, consistent with our findings. Garcia et al.2 found that estimated impacts of PM2.5 were higher in rural areas for mortality from cardiovascular disease, cardiopulmonary disease, and all causes. Another study investigating long-term exposure to PM2.5 in China reported that the risk of all-cause mortality in people ≥65 years was higher in rural than in urban areas.4 On the other hand, Wang et al.5 found a higher effect of long-term PM2.5 exposure on mortality in urban than in rural areas. The different patterns of effects between urban and rural areas may result from differences in characteristics of the population, health behavior, time spent outdoors, access to health care, PM2.5 composition from different sources and weather patterns, and other environmental factors between urban and rural areas. For example, people living in rural areas may have less access to high quality of health care or larger proportion of PM2.5 in rural areas may derive from biomass fuels. Also, low greenness in rural vs. urban areas may differ. Measure of total greenness by a single indicator does not differentiate between different types of land use between urban and rural areas. For example, large urban areas with high population density tend to lose natural resources and have anthropogenic urban green areas (e.g., urban park vs. natural grassland). Medium cities like urban clusters in our study may be more complex due to several factors such as within area variation of some factors (e.g., SES) than those in large urban areas and some areas may have mixed urban and rural characteristics as our urban and rural classification in this study was based on the population density.
Our findings suggest that regardless of SES, people living in high greenness areas had lower effect of PM2.5 exposure on mortality than those living in less green areas. Also, regardless of greenness level, people living in high SES areas had lower effect of PM2.5 exposure on mortality than those living in low SES areas. Moreover, people living in areas with both high SES and high greenness had substantially lower effects for PM2.5 exposure on mortality for both states. Our findings indicate that people living in low SES areas with high greenness may benefit by having a lower effect of PM2.5 on mortality than those living in low SES with low greenness. Crouse et al. observed similar findings to our study.17 They found that residents in economically deprived neighborhoods with high greenness had lower associations between PM2.5 and mortality than those living in deprived areas with less greenness. Another study also suggested that disadvantaged populations such as those with lower SES may benefit more from greenness than those of higher SES.12 The different findings around health disparities may result from various combinations of several demographic and/or environmental characteristics; factors that often contribute to health disparities are often correlated (e.g., differences in SES between/within greenness group). Thus, further research is needed to consider complex interaction among possible disparity factors on the air pollution–health outcomes association. Our findings of combined disparities contribute to understandings of how multiple disparity factors may affect associations between air pollution and health outcomes (as illustrated in eFigure 1).
Our study has several limitations. We used satellite-derived NDVI data as an indicator of residential greenness. Using a single measure for vegetation does not reflect different kinds of vegetation, accessibility, and quality of greenness, although NDVI is a widely used effective measure of greenness. Moreover, we had no information of actual exposure to green space such as frequency of visiting or using green space. Additional studies considering different types of greenness and detailed data for activity patterns are needed to further evaluate the roles of greenness on the air pollution–health outcomes association. A previous study reported that the use of a predicted exposure can bias the health effect estimate unless all of the confounders included in the health effect regression model are also included in the exposure prediction model.31 In this study, we used predicted PM2.5 estimates from previously published prediction models. Our ensemble model combined three complementary algorithms (neural network, random forest, and gradient boosting) and achieved excellent performance, with better agreement between monitored PM2.5 and predicted PM2.5 (spatial R2=0.89, spatial RMSE=1.26μg/m3, temporal R2=0.85).23 The algorithms used a large number of predictor variables including satellite data, meteorologic variables, land-use variables, and chemical transport model predictions. Our health effect model controlled for several individual- and community-level covariates including regional cluster variable to consider compositional differences in PM2.5, meteorologic variables. The complex prediction model used to estimate PM2.5 concentrations23 used greenness as one of the many input variables. As noted, the model shows very good agreement with monitor values; however, if the prediction model performance differs by greenspace, our results could be affected. However, we confirmed robustness of effect estimates by greenness between PM2.5 prediction estimates and monitor values using the subset of areas with PM2.5 monitors. We adjusted for many individual- and community-level variables in our analysis, but residual confounding may remain, for example because of differences in health behaviors among people living in different greenness groups. Future studies considering more detailed individual-level behavioral data are needed. Strengths of our study include that we could estimate the effect of PM2.5 exposure with large spatiotemporal coverage and high spatiotemporal resolution. Our analysis included a large population of elderly (65 years of age or order) from the Medicare cohort from all areas including rural areas across both states followed for up to 16 years. Future work could investigate whether the association between ambient exposure and personal exposure differs by residential greenness among other relevant factors. Further, we considered multiple dimensions of disparity factors, which can influence the air pollution–mortality association.
Conclusions
We found suggestive evidence that people living in neighborhoods with high greenness have lower mortality risk from long-term exposure to PM2.5 than those living in neighborhoods with low greenness, although there may remain uncertainties due to differences in population characteristics, PM2.5 sources and composition, and other environmental factors across greenness groups. Additionally, in our study, we estimate that people living in low SES areas with high greenness benefited from a lower effect of PM2.5 on mortality than those living in low SES areas with low greenness. The findings from this study contribute to the growing body of literature on greenness as an effect modifier in the air pollution–health outcomes associations. Moreover, our findings regarding combined disparities estimate that multiple aspects of disparity factors and their interactions may contribute to disproportionate mortality burdens from air pollution exposure.
Supplementary Material
Sources of financial support:
This publication was developed under Assistance Agreement No. RD835871 awarded by the U.S. Environmental Protection Agency to Yale University. It has not been formally reviewed by EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the Agency.
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R01MD012769. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of interest: The authors declare no conflict of interest.
Process for obtaining the data and code for replicating the results: The raw data for greenness are publicly available from the NASA’s Earth Observing System. We cannot provide Medicare data due to data use agreement, but the data could be requested from the Centers for Medicare and Medicaid Services. The computing code can be available upon request to the corresponding author.
References
- 1.Di Q, Wang Y, Zanobetti A, Wang Y, Koutrakis P, Choirat C, Dominici F, Schwartz JD. Air pollution and mortality in the Medicare population. N Engl J Med. 2017;376:2513–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia CA, Yap PS, Park HY, Weller BL. Association of long-term PM2.5 exposure with mortality using different air pollution exposure models: impacts in rural and urban California. Int J Environ Health Res. 2016;26(2):145–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hvidtfeldt UA, Sørensen M, Geels C, Ketzel M, Khan J, Tjønneland et al. Long-term residential exposure to PM2.5, PM10, black carbon, NO2, and ozone and mortality in a Danish cohort. Environ Int. 2019;123:265–272. [DOI] [PubMed] [Google Scholar]
- 4.Li T, Zhang Y, Wang J, Xu D, Yin Z, Chen H et al. All-cause mortality risk associated with long-term exposure to ambient PM2.5 in China: a cohort study. Lancet Public Health. 2018;3:e470–477. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Shi L, Lee M, Liu P, Di Q, Zanobetti A, Schwartz J. Long-term exposure to PM2.5 and mortality among older adults in the Southeastern US. Epidemiology. 2017;28(2):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef et al. Long-term air pollution exposure and cardio-respiratory mortality: a review. Environ Health. 2013;12:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pelucchi C, Negri E, Gallus S, Boffetta P, Tramacere I, La Vecchia C. Long-term particulate matter exposure and mortality: a review of European epidemiological studies. BMC Public Health. 2009;9:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kioumourtzoglou MA, Austin E, Koutrakis P, Dominici F, Schwartz J, Zanobetti A. PM2.5 and survival among older adults: effect modification by particulate composition. Epidemiology. 2015;26(3):321–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fong KC, Hart JE, James P. A review of epidemiologic studies on greenness and health: updated literature through 2017. Curr Environ Health Rep. 2018;5:77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gascon M, Triguero-Mas M, Martínez D, Dadvand P, Rojas-Rueda D, Plasencia A, Nieuwenhuijsen MJ. Residential green spaces and mortality: A systematic review. Environ Int. 2016;86:60–67. [DOI] [PubMed] [Google Scholar]
- 11.James P, Hart J, Banay R, Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect. 2016;124:1344–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nieuwenhuijsen MJ, Kruize H, Gidlow C, Andrusaityte S, Antó JM, Basagaña X et al. Positive health effects of the natural outdoor environment in typical populations in different regions in Europe (PHENOTYPE): a study programme protocol. BMJ Open. 2014;4:e004951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jose GVH, Karina P, Patricia H. Urban green spaces as a component of an ecosystem functions, services, users, community involvement, initiatives and actions. Int J Environ Sci Nat Res. 2018;8(1):555730. [Google Scholar]
- 14.de Keijzer C, Agis D, Ambros A, Arevalo G, Baldasano JM, Bande S, et al. The association of air pollution and greenness with mortality and life expectancy in Spain: a small-area study. Environ Int. 2017;99:170–176. [DOI] [PubMed] [Google Scholar]
- 15.Heo S, Bell ML. The influence of green space on the short-term effects of particulate matter on hospitalization in the U.S. for 2000–2013. Environ Res. 2019;174:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun S, Sarkar C, Kumari S, James P, Cao W, Lee RS, Tian L, Webster C. Air pollution associated respiratory mortality risk alleviated by residential greenness in the Chinese Elderly Health Service Cohort. Environ Res. 2020;183:109139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crouse DL, Pinault L, Balram A, Brauer M, Burnett RT, Martin RV et al. Complex relationships between greenness, air pollution, and mortality in a population-based Canadian cohort. Environ Int. 2019;128:292–300. [DOI] [PubMed] [Google Scholar]
- 18.Yitshak-Sade M, James P, Kloog I, Hart JE, Schwartz JD, Laden F, Lane KJ, Fabian MP et al. Neighborhood greenness attenuates the adverse effect of PM2.5 on cardiovascular mortality in neighborhoods of lower socioeconomic status. Int J Environ Res Public Health. 2019;16:814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim S, Kim H, Lee JT. Interactions between ambient air particles and greenness on cause-specific mortality in seven Korean metropolitan cities, 2008–2016. Int J Environ Res Public Health. 2019;16:1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vivanco-Hidalgo RM, Wellenius GA, Basagana X, Cirach M, Gonzalez AG, Ceballos P et al. Short-term exposure to traffic-related air pollution and ischemic stroke onset in Barcelona, Spain. Environ Res. 2018;162:160–165. [DOI] [PubMed] [Google Scholar]
- 21.Bravo MA, Ebisu K, Dominici F, Wang Y, Peng RD, Bell ML. Airborne fine particles and risk of hospital admissions for understudied populations: effects by urbanicity and short-term cumulative exposures in 708 U.S. counties. Environ Health Perspect. 2017;125:594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kloog I, Nordio F, Zanobetti A, Coull BA, Koutrakis P, Schwartz JD. Short term effects of particle exposure on hospital admissions in the Mid-Atlantic states: a population estimate. PLoS One. 2014;9(2):e88578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Q, Amini H, Shi L, Kloog I, Silvern R, Kelly J et al. An ensemble-based model of PM2.5 concentration across the contiguous United States with high spatiotemporal resolution. Environ Int. 2019;130:104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weier J, Herring D. 2000. Measuring vegetation (NDVI&EVI). https://earthobservatory.nasa.gov/features/MeasuringVegetation/ Accessed: 14 August, 2020.
- 25.Kioumourtzoglou MA, Schwartz J, James P, Dominici F, Zanobetti A. PM2.5 and mortality in 207 US cities: Modification by temperature and city characteristics. Epidemiology. 2016;27(2):221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sanyal S, Rochereau T, Maesano CN, Com-Ruelle L, Annesi-Maesano I. Long-term effect of outdoor air pollution and on mortality and morbidity: A 12-year follow-up study for metropolitan France. Int J Environ Res Public Health. 2018;15:2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zeger SL, Dominici F, McDermott A, Samet JM. Mortality in the Medicare population and chronic exposure to fine particulate air pollution in urban centers (2000–2005). Environ Health Perspect. 2008;116:1614–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Markevych I, Schoierer J, Hartig T, Chudnovsky A, Hystad P, Dzhambov AM, de Vries S et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res. 2017;158:301–317. [DOI] [PubMed] [Google Scholar]
- 29.Nowak DJ, Crane DE, Stevens JC. Air pollution removal by urban trees and shrubs in the United States. Urban For Urban Gree. 2006;4:115–123. [Google Scholar]
- 30.Kuo M. How might contact with nature promote human health? Promising mechanisms and a possible central pathway. Front Psychol. 2015;6:1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cefalu M, Dominici F. Does exposure prediction bias health effect estimation? The relationship between confounding adjustment and exposure prediction. Epidemiology. 2014;25(4):583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


