Abstract
Most reports on AKI claim to use KDIGO guidelines but fail to include the urinary output (UO) criterion in their definition of AKI. We postulated that ignoring UO alters the incidence of AKI, may delay diagnosis of AKI, and leads to underestimation of the association between AKI and ICU mortality. Using routinely collected data of adult patients admitted to an intensive care unit (ICU), we retrospectively classified patients according to whether and when they would be diagnosed with KDIGO AKI stage ≥ 2 based on baseline serum creatinine (Screa) and/or urinary output (UO) criterion. As outcomes, we assessed incidence of AKI and association with ICU mortality. In 13,403 ICU admissions (62.2% male, 60.8 ± 16.8 years, SOFA 7.0 ± 4.1), incidence of KDIGO AKI stage ≥ 2 was 13.2% when based only the SCrea criterion, 34.3% when based only the UO criterion, and 38.7% when based on both criteria. By ignoring the UO criterion, 66% of AKI cases were missed and 13% had a delayed diagnosis. The cause-specific hazard ratios of ICU mortality associated with KDIGO AKI stage ≥ 2 diagnosis based on only the SCrea criterion, only the UO criterion and based on both criteria were 2.11 (95% CI 1.85–2.42), 3.21 (2.79–3.69) and 2.85 (95% CI 2.43–3.34), respectively. Ignoring UO in the diagnosis of KDIGO AKI stage ≥ 2 decreases sensitivity, may lead to delayed diagnosis and results in underestimation of KDIGO AKI stage ≥ 2 associated mortality.
Subject terms: Nephrology, Kidney diseases, Acute kidney injury, Risk factors
Introduction
Acute Kidney Injury (AKI) is an important clinical condition with substantial impact on morbidity and mortality. The lack of a common universally accepted definition for AKI has for a long time hampered research and progress1. As a synthesis of different initiatives2–6, the KDIGO criteria became the standard for defining AKI. However, most reports, studies and automated detection and risk prediction tools still use a truncated version of the KDIGO definition based only on a serum creatinine (SCrea) criterion and neglect the urinary output (UO) criterion to define their ground truth definition for AKI7–13. In addition, just as is the case for the selection of a baseline creatinine measure, UO criteria can be implemented in different ways14. As a result, despite the unified definition as proposed by KDIGO, substantial cross-study and cross-model differences remain in what exactly is reported or predicted as AKI7,8,15–18.
So far, the problem of variable meanings of the AKI label was deemed to be only relevant for epidemiology19. It could however also have an important impact for the correct interpretation and transportability of clinical trial results. In addition, with the advent of electronic health records within the last decade, algorithms to automatically diagnose and predict AKI will be implemented in the everyday care of individual patients20,21. Such automated detection algorithms or risk prediction models could be used in early recognition and timely management of AKI22,23 and are considered a highly promising breakthrough for medicine24,25. These algorithms and models, however, are trained on databases which may contain different ‘ground truth’ labels of AKI, all loosely defined within the confines of the KDIGO guidelines, but mostly neglecting the UO criterion. This is problematic for interpretation and external validation because the gold standard against which their performance is assessed may be either different or simply missing in external databases, potentially leading to unsensible or misleading performance assessments.
Within the confines of the KDIGO definition, it can be hypothesized that omitting the UO criterion in the applied definition of AKI substantially downplays the importance of the AKI label if 1/neglecting UO in the ground truth substantially alters the incidence of AKI and leads to missed cases; 2/ neglecting the UO criterion often delays AKI diagnosis; 3/ the UO criterion has an independent association with ICU mortality and may therefore have added prognostic value compared to single use of the SCrea criterion. Several studies have provided evidence that is mostly in line with this hypothesis15,26,27. However, none of these studies has adequately accounted for the time dynamics of AKI diagnosis or documented the number of potentially missed cases or delayed diagnoses induced by ignoring the UO criterion as they evolve over time. Failure to account for the timing of diagnosis may moreover have introduced immortal time bias in assessing the association with adverse outcomes, which may have led to underestimation of these associations28. In this paper, we address these shortcomings with the aim to add to and strengthen the evidence base of the aforementioned hypotheses.
Methods
All 52 beds of the Gent University Hospital (tertiary care) adult intensive care units (ICU) dispose of a commercially available Intensive Care Information System (ICIS) (Centricity Critical Care, GE Healthcare, Germany) to collect granular longitudinal patient data in real time. All data from monitors, ventilators, pumps, radiology results and laboratory results and administered medication are automatically uploaded in the system. In addition, a wide variety of pre-defined items are routinely entered manually by medical staff.
For all patients (aged 16 or older) admitted to our ICU from January 2013 to December 2017, we have included their first ICU episode during this study period for analysis. Raw data relevant for our study were extracted in a pseudonymized way from the ICIS database. Daily serum creatinine (SCrea) and all urinary output (UO) measurements during ICU stay were extracted from the ICIS, along with their corresponding sample times. For SCrea, this information originates from the lab information system directly linked to the ICIS. The study data set was complemented with all available SCrea values available to the lab information system up to 365 days before ICU admission. UO was periodically measured and entered into the ICIS by nursing staff who recorded the reading, mostly from a drainage container of a urinary catheter or from spontaneous urination in a scaled recipient. In addition, for each included patient, time from ICU admission to discharge, vital status at ICU discharge, gender, age, weight, comorbidities and Sequential Organ Failure Assessment (SOFA) score on the day of ICU admission were extracted.
Ethical approval was obtained from the Ethical Committee of Ghent University Hospital (EC nr 201-0705) and informed consent was obtained according to applicable regulations. All methods were performed in accordance with the relevant guidelines and regulations and the declaration of Helsinki.
The KDIGO criteria for AKI stage ≥ 2 diagnosis hinge on two different parameters: 1/ absolute or relative increase in SCrea as compared to a baseline measurement (Screa criterion) and 2/ oliguria during a 12-h period (UO criterion). As primary endpoints we considered (cumulative) incidence of AKI stage ≥ 2 diagnosis during ICU stay as defined by the KDIGO guidelines29, based on either criterion, or both, and the association between diagnosis by each of these criteria and ICU mortality, as a crude reflection of their prognostic value.
We intended to mimic a system in which automated computer code incorporated in an intensive care information system is applied to detect or alert for AKI in real-time. For each patient, we assessed whether and when any Screa measurement was found during their ICU stay that either exceeded 4.0 mg/dl or indicated a > twofold increase relative to one of the following baseline Screa measurements, selected in the order listed below, according to availability:
Screa-1 A baseline Screa measurement as manually entered in the ICIS by the treating physician at ICU admission. Physicians have to enter a (documented) Screa measurement before the current hospitalization and no older than 365 days or, if not available, the lowest measurement of the current hospitalization.
Screa-2 The lowest available pre-ICU measurement up to 365 days before ICU admission as extracted from the lab information system. This could be a value from before or during the index hospitalisation but before admission to ICU.
Screa-3 A back-calculated baseline Screa using the simplified 4-variable Modification of Diet in Renal Disease (MDRD) Study equation assuming an estimated glomerular filtration rate (eGFR) of 75 ml/min/1.73 m2 for every patient30.
In the interest of space, we only provide results for automated AKI diagnosis based on implementation of the Screa criterion relative to a baseline selected by this stepwise approach (henceforth labelled Screa). Readers are referred to the supplemental material for results relative to each of these listed and two additional baseline measurements separately.
To identify patients with AKI stage ≥ 2 based on the UO criterion, UO measurements were first converted to ml/kg/h. Patients’ weight was entered into the ICIS by nursing staff based on recent weight registrations when available in the hospital information system, self-report from the patient, from relatives, or an estimated clinical guess. In line with the KDIGO guidelines, we assessed for each patient whether and when any UO registration was found during their ICU stay at which
UO-1 total UO during the last 12-h period was ≤ 6 ml/kg
UO-2 total UO during each of the last 12 consecutive 1-h periods was ≤ 0.5 ml/kg
UO was calculated in X-hour time windows according to the rules described in Supplementary Material S1 (section “Data preprocessing”).
In addition, to assess the relative impact of ignoring either of these criteria, two composite definitions of AKI stage ≥ 2 were postulated:
Screa-UO-1 which indicates whether a patient is diagnosed based on either the Screa criterion or the UO-1 criterion (as defined above)
Screa-UO-2 which indicates whether a patient is diagnosed based on either the Screa criterion or the UO-2 criterion (as defined above).
Cumulative incidence curves were obtained to assess the dynamics of how the number of incident AKI stage ≥ 2 cases, as diagnosed by each of the aforementioned criteria, accumulates over time. Comparison of these curves enables to retrospectively assess, at each time point, the percentage of cases that were either missed or diagnosed with delay by ignoring either the SCrea criterion or the UO criteria. Additional details on calculation of number of cases missed or diagnosed with delay can be found in Supplementary Material S1 (section “Cumulative incidence curves”).
The associations between diagnosis by each of the aforementioned criteria and ICU mortality, as captured by cause-specific hazard ratios comparing patient time at risk of ICU mortality with versus without diagnosis, were estimated using a series of extended Cox proportional hazards models for time from admission to ICU death. By including AKI stage ≥ 2 diagnosis as a time-varying rather than a time-fixed covariate (coded 1 from the time of AKI diagnosis and 0 otherwise) in the Cox models, the time of diagnosis can be accounted for and immortal time bias can be eliminated31. In these Cox models, ICU discharge was treated as a censoring event, such that the exponentiated coefficient estimates could be interpreted as cause-specific hazard ratios. Unadjusted hazard ratios were estimated using Cox models which included a single time-varying indicator for whether a specific criterion had been reached. In addition, to assess the independent contribution of the SCrea and UO criteria, adjusted Cox models were fitted including separate time-varying indicators for each of these criteria. Finally, to assess the conditional association between diagnosis by each of the criteria and ICU mortality, accounting for other prognostic risk factors, a series of Cox models were fitted adjusted for gender, age and SOFA score on admission. The concordance index was reported for each fitted Cox model to enable a crude comparison in terms of (added) prognostic value of each of the (combined) criteria32. Additional details on statistical methods can be found in Supplementary Material S1. All analyses were conducted in R (version 3.6.0).
Our reporting of this study followed the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) reporting guidelines (supplementary material).
Ethics approval and consent to participate
The Ghent University Hospital Ethics Committee approved the study (EC nr 201-0705) and waived informed consent since all analyses were performed retrospectively on pseudonymized records.
Consent for publication
Not applicable.
Results
We included 13,403 admissions, with demographic and baseline characteristics presented in Table 1. Of note, 84% of the cohort had an indwelling bladder catheter.
Table 1.
Baseline demographic and clinical data.
| Age (mean ± SD) | 60.8 ± 16.8 |
| Gender (% male) | 62.2 |
| Admission SOFA score (mean ± SD) | 7.01 ± 4.1 |
| Weight, kg (mean ± SD) | 76.0 ± 16.7 |
| Median ICU length of stay (hours) (Q1, Q3) | 44 (23, 93) |
| Baseline SCrea (mean ± SD) | 1.28 ± 2.7 |
| Urinary catheter (%) | 84.2 |
| Chronic kidney disease (%) | 16.3 |
| Diabetes (%) | 16.2 |
Depending on the applied criterion (or combination of criteria), incidence of AKI stage ≥ 2 diagnosis varied between 13.2 and 38.7% (Table 2). In Supplementary Table 2, we also list incidences based on the SCrea criterion depending on different choices of baseline SCrea measures, which ranged from 9.5% to 16.5%. Regardless of the applied criterion, patients with AKI vs no AKI were, on average, older, more likely to be male and to have diabetes or chronic kidney disease, and had a higher average SOFA score and weight at admission (Table 2). Of note, patients who were labelled as AKI based on the Screa criterium were more likely to have underlying CKD (40%) vs those labelled as AKI based on UO (20.3–27.0%).
Table 2.
Incidence and demographic data according to different interpretations of the criteria for KDIGO AKI stage ≥ 2.
| Criterion | Incidence of AKI (%) | Age (mean ± SD) | Admission SOFA score (mean ± SD) | Weight, kg (mean ± SD) | Baseline SCrea value, mg/dl (mean ± SD) | Urinary catheter (%) | Gender (% male) | Chronic kidney disease (%) | Diabetes (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AKI | No AKI | AKI | No AKI | AKI | No AKI | AKI | No AKI | AKI | No AKI | AKI | No AKI | AKI | No AKI | AKI | No AKI | ||
| SCrea | 13.2 | 62.3 ± 15.1 | 60.6 ± 17.0 | 9.2 ± 4.5 | 6.7 ± 4.0 | 79.0 ± 17.6 | 75.6 ± 16.5 | 2.73 ± 3.12 | 1.05 ± 2.59 | 66.0 | 61.6 | 43.9 | 12.0 | 22.0 | 15.4 | ||
| UO-1 | 34.3 | 64.1 ± 15.4 | 59.1 ± 17.2 | 8.6 ± 4.3 | 6.2 ± 3.8 | 81.4 ± 17.8 | 73.2 ± 15.3 | 86.2 | 81.4 | 66.6 | 59.9 | 20.3 | 14.1 | 20.1 | 14.2 | ||
| UO-2 | 14.2 | 63.6 ± 15.6 | 60.3 ± 16.9 | 9.0 ± 4.6 | 6.7 ± 4.0 | 82.7 ± 19.3 | 74.9 ± 15.9 | 83.4 | 83.8 | 65.1 | 61.8 | 27.5 | 14.4 | 20.7 | 15.5 | ||
| SCrea-UO-1 | 38.7 | 63.3 ± 15.6 | 59.2 ± 17.3 | 8.4 ± 4.3 | 6.2 ± 3.8 | 80.7 ± 17.7 | 73.1 ± 15.2 | 66.4 | 59.6 | 25.3 | 10.6 | 19.9 | 13.9 | ||||
| SCrea-UO-2 | 20.9 | 62.4 ± 15.7 | 60.4 ± 17.0 | 8.6 ± 4.5 | 6.6 ± 3.9 | 80.7 ± 18.6 | 74.8 ± 15.9 | 65.2 | 61.4 | 35.1 | 11.3 | 20.3 | 15.2 | ||||
SCrea: serum creatinine > 4.0 mg/dl or > 2 × baseline, where baseline = SCrea-1 whenever available, otherwise SCrea-2, or SCrea-3 (when neither SCrea-1 nor SCrea-2 are available) with Screa-1 defined as baseline Screa measurement as manually entered in ICIS by the treating physician at ICU admission; Screa-2 defined as the lowest pre-ICU measurement up to 365 days before ICU admission as extracted from the lab information system; Screa-3 defined as a back-calculated baseline Screa using the simplified 4-variable Modification of Diet in Renal Disease (MDRD) Study equation assuming an estimated glomerular filtration rate (eGFR) of 75 ml/min/1.73 m2 for every patient30; UO-1: total UO during the last 12-h period was ≤ 6 ml/kg; UO-2: total UO during each of the last 12 consecutive 1-h periods was ≤ 0.5 ml/kg; SCrea-UO-1: AKI stage ≥ 2 according to either the SCrea criterion or the UO-1 criterion; SCrea-UO-2: AKI stage ≥ 2 according to either the SCrea criterion or the UO-2 criterion.
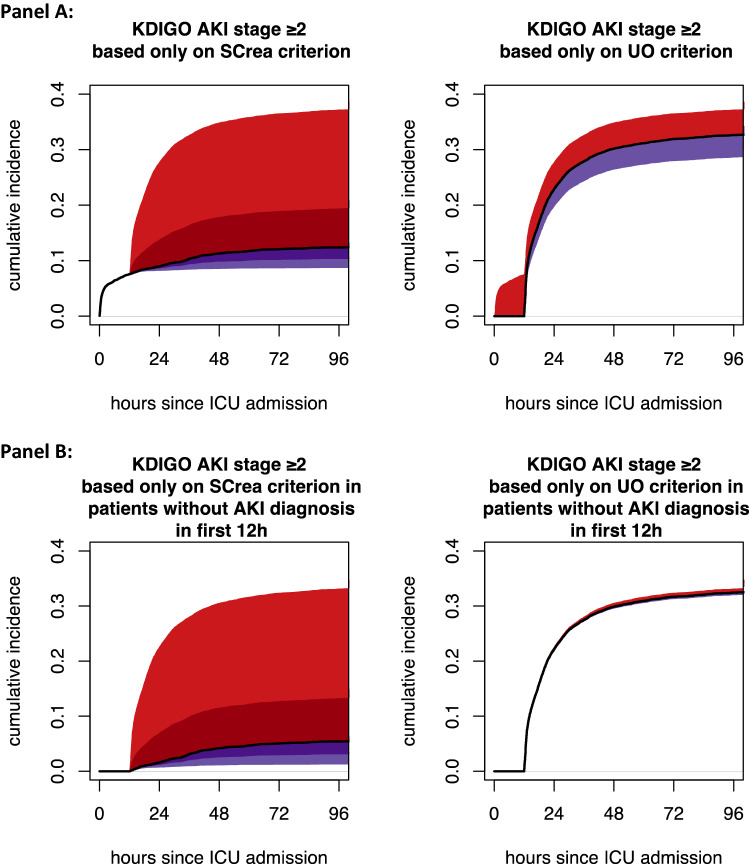
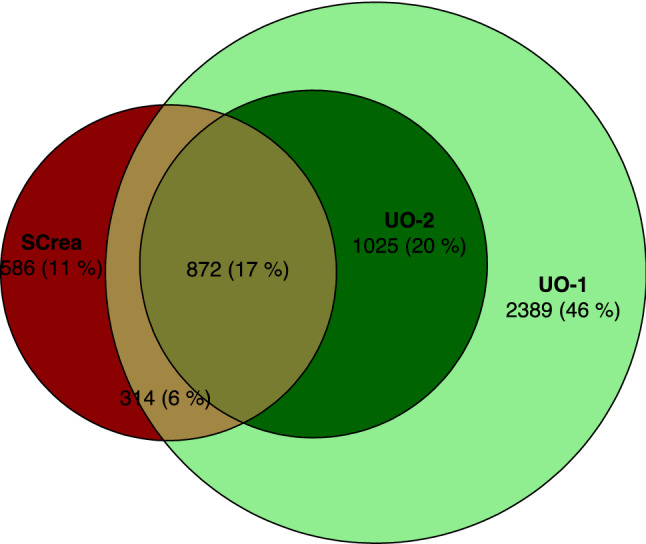
Figure 1 presents the distribution of AKI diagnoses according to the different criteria and their overlap. A minority of diagnoses (11%) is made only based on the SCrea criterion, while the majority of diagnoses (66%) is made only based on the UO criterion. This is also reflected by the red shaded areas in Fig. 2A, which represent the fraction of cases that would be missed over time by ignoring either the UO criterion (left panel) or the SCrea criterion (right panel). The black curves in Fig. 2A depict the cumulative incidence of AKI diagnosis based on the Screa (left panel) and the UO criterion (right panel) as a function of time since ICU admission (hours). As, by definition, patients cannot reach the UO criterion for AKI stage ≥ 2 before 12 h, initially diagnosis of AKI is made only based on the Screa criterion. The purple shaded areas in Fig. 2A represent the fraction of cases over time that are diagnosed with delay by ignoring either the UO criterion (left panel: about 12% of cases) or the SCrea criterion (right panel: about 11% of cases). Figure 2B displays the AKI incidence for patients not diagnosed with AKI within the first 12 h after ICU admission, which illustrates that later diagnosis (after 12 h) is almost exclusively made based on the UO criterion.
Figure 1.
Euler diagram illustrating the distribution and overlap between AKI diagnosis according to different AKI criteria. Numbers indicate the number of patients in that overlap zone, so who would be diagnosed by different criteria. SCrea: serum creatinine > 4.0 mg/dl or > 2 × baseline, where baseline = SCrea-1 whenever available, otherwise SCrea-2, or SCrea-3 (when neither SCrea-1 nor SCrea-2 are available) with Screa-1 defined as baseline Screa measurement as manually entered in ICIS by the treating physician at ICU admission; Screa-2 defined as the lowest pre-ICU measurement up to 365 days before ICU admission as extracted from the lab information system; Screa-3 defined as a back-calculated baseline Screa using the simplified 4-variable Modification of Diet in Renal Disease (MDRD) Study equation assuming an estimated glomerular filtration rate (eGFR) of 75 ml/min/1.73 m2 for every patient30; UO-1: total UO during the last 12-h period was ≤ 6 ml/kg; UO-2: total UO during each of the last 12 consecutive 1-h periods was ≤ 0.5 ml/kg.
Figure 2.
Cumulative incidence of automated AKI diagnosis over time. (A) Cumulative incidence of automated AKI diagnosis since ICU admission, based only on KDIGO Screa criterion (left) or only on KDIGO UO criterion (right) (black curves). Shaded areas represent cases that were, by each time point, either missed (red) or diagnosed with delay (purple) by ignoring the other criterion. (Dark shades in the left panel indicate missed or delayed cases compared to the UO-2 criterion, while the combination of light and dark shades in the left panel indicate missed or delayed cases compared to the UO-1 criterion). (B) Cumulative incidence of automated AKI diagnosis in patients still hospitalized and without AKI diagnosis by the 12th hour since ICU admission, based only on KDIGO Screa criterion (left) or only on KDIGO UO criterion (right) (black curves). Shaded areas represent cases that were, by each time point, either missed (red) or diagnosed with delay (purple) by ignoring the other criterion.
Table 3 displays ICU mortality incidence rates per 1,000 patient days at risk at the ICU with or without AKI diagnosis based on the different criteria (or combinations) and corresponding cause-specific hazard ratios (both unadjusted and adjusted for gender, age, and SOFA score at admission). Considering the UO criterion resulted in relatively higher relative hazards, as well as higher overall discriminative ability (as expressed by the concordance index), as compared to only considering the SCrea criterion. This pattern was found irrespective of whether the UO criterion was (1) strictly interpreted (UO-2) or more broadly (UO-1), (2) considered in combination with SCrea or not, or (3) adjusted for other risk factors or not.
Table 3.
Incidence rates and hazard ratios of ICU mortality for AKI stage ≥ 2 vs no AKI stage ≥ 2 across different criteria.
| KDIGO stage ≥ 2 criterion | Incidence rate of ICU mortality (estimated number of ICU deaths per 1,000 patient days at risk)1 | Unadjusted cause-specific hazard ratio of ICU mortality2 (95% CI) | Concordance index3 | Adjusted cause-specific hazard ratio of ICU mortality4 (95% CI) | Concordance index3 | |
|---|---|---|---|---|---|---|
| Patient days with AKI | Patient days without AKI | |||||
| Cox proportional hazards models including a single criterion as predictor | ||||||
| SCrea | 31.3 | 16.1 | 2.11 (1.85–2.42) | 0.568 | 1.81 (1.56–2.09) | 0.663 |
| UO-1 | 27.2 | 12.6 | 3.00 (2.55–3.54) | 0.593 | 2.59 (2.18–3.09) | 0.680 |
| UO-2 | 36.6 | 14.1 | 3.21 (2.79–3.69) | 0.597 | 2.83 (2.44–3.28) | 0.688 |
| SCrea-UO-1 | 26.5 | 12.1 | 2.85 (2.43–3.34) | 0.604 | 2.54 (2.14–3.02) | 0.683 |
| SCrea-UO-2 | 32.8 | 13.2 | 2.93 (2.57–3.35) | 0.615 | 2.62 (2.27–3.04) | 0.695 |
| Cox proportional hazards model including both SCrea and UO-1 as predictors | ||||||
| SCrea | 1.67 (1.46–1.92) | 0.624 | 1.48 (1.27–1.71) | 0.693 | ||
| UO-1 | 2.63 (2.22–3.11) | 2.35 (1.97–2.82) | ||||
| Cox proportional hazards model including both SCrea and UO-2 as predictors | ||||||
| SCrea | 1.35 (1.16–1.57) | 0.624 | 1.18 (1.01–1.39) | 0.694 | ||
| UO-2 | 2.82 (2.41–3.29) | 2.63 (2.23–3.10) | ||||
1Incidence rate ratios only approximate (cause-specific) hazard ratios when the survival distributions in each group both follow an exponential distribution.
2Estimated by an extended Cox model that treats ICU discharge as a censoring event.
3Concordance indices are displayed for the corresponding Cox model whose exponentiated coefficient estimates are displayed in the column on the left hand side.
4Estimated by an extended Cox model that treats ICU discharge as a censoring event that additionally incorporates gender, age (binned into 4 categories according to quartiles) and SOFA score at ICU admission (binned into 4 categories according to quartiles). As a reference: the concordance index for a Cox model including only gender, age and SOFA score at ICU admission (excl. AKI criteria) equalled 0.640.
SCrea: serum creatinine > 4.0 mg/dl or > 2 × baseline, where baseline = SCrea-1 whenever available, otherwise SCrea-2, or SCrea-3 (when neither SCrea-1 nor SCrea-2 are available) with Screa-1 defined as baseline Screa measurement as manually entered in ICIS by the treating physician at ICU admission; Screa-2 defined as the lowest pre-ICU measurement up to 365 days before ICU admission as extracted from the lab information system; Screa-3 defined as a back-calculated baseline Screa using the simplified 4-variable Modification of Diet in Renal Disease (MDRD) Study equation assuming an estimated glomerular filtration rate (eGFR) of 75 ml/min/1.73 m2 for every patient30; UO-1: total UO during the last 12-h period was ≤ 6 ml/kg; UO-2: total UO during each of the last 12 consecutive 1-h periods was ≤ 0.5 ml/kg; SCrea-UO-1: AKI stage ≥ 2 according to either the SCrea criterion or the UO-1 criterion; SCrea-UO-2: AKI stage ≥ 2 according to either the SCrea criterion or the UO-2 criterion. An extended version of th table is included as Supplementary Table 2.
Discussion
We observed in this study that incidence of AKI stage ≥ 2 diagnosis was higher and the association with ICU mortality stronger when the UO criterion is incorporated in the definition of AKI as compared to when it is not incorporated. We demonstrate the additive and independent predictive value of the UO to the Screa criterion with respect to ICU mortality. Accordingly, neglecting the UO criterion will result in underdiagnosis of AKI, may delay diagnosis of AKI and will underestimate the true relative hazard of ICU mortality associated with the label AKI.
To the best of our knowledge, this study is the first to take into account the time dynamics of AKI diagnosis by either algorithmic application of the SCrea criterion, the UO criterion, or both. Our approach of comparing cumulative incidence curves enabled to shed light on these dynamics and, in particular, to map, at each point in time, the number of potentially missed cases or delayed diagnoses by ignoring either the SCrea or the UO criterion. In particular, due to the time-dependent nature of the UO criterion, AKI presenting before or shortly after ICU admission can only be diagnosed using the SCrea criterion during the first 12 h. After 12 h, we observe a sudden steep increase in number of incident AKI diagnoses based almost exclusively on the UO criterion. Most of these new diagnoses based on the UO criterion would be missed by the SCrea criterion, whereas a small number would still be diagnosed by the SCrea criterion but only later on (Fig. 2B). This emphasizes the importance of the UO criterion for AKI detection after 12 h of admission, and by consequence, for the potential of (early) intervention. In sum, our results demonstrate that ignoring the UO criterion leads to a high number of missed casesand more delayed diagnoses in patients who did not yet have AKI at admission.
Comparisons of estimated associations between diagnosis by each of the criteria (or their combination) and ICU mortality demonstrate that AKI stage ≥ 2 diagnosis based on both the SCrea and UO criteria is more strongly associated with ICU mortality and has higher prognostic discriminative ability than diagnosis based on the SCrea criterion alone. This holds even after adjustment for other prognostic factors such as gender, age, and disease severity at ICU admission. These findings add emphasis on the importance of UO based on earlier reports on the association of UO alone with mortality14,33.
We used two different interpretations of the KDIGO urinary output criterion in our dataset: one more strict (oliguria as determined in each of 12 consecutive 1 h blocks) than the other (oliguria as determined in a moving total 12 h time window). Both options have previously been associated with mortality14. None of the patients who fulfilled the more strict criteria failed the broad criterion.
The different scenarios for baseline SCrea retrieval in our algorithms resulted in wide variation in AKI incidence (see Supplementary Table 1), confirming earlier findings17. Back-calculated values assuming a fixed eGFR, e.g. 75 ml/min/1,73m2, are often used7,34–36, but this approach leads to overestimation of AKI incidence, especially in the elderly and those with pre-existing CKD37–41. As we linked our ICU data system with the lab data system, we were able to retrieve SCrea values before index ICU hospitalization, a more valid baseline, in more than 80% of ICU admissions, which is much higher than reported in most other studies. However, patients suffering from chronic comorbidities and intermittent acute illnesses are more likely to have historical values available than healthy individuals. This is of importance as AKI algorithms will be most useful in cases where AKI is missed because the treating physician did not consider the diagnosis of AKI. A prediction tool that relies on whether a physician ordered Screa, and had thus a suspicion for AKI, will perform poorly for this purpose42. In addition, availability of measures may depend on local standards of care, which may contribute to poor external validity of the AKI algorithm43. The poor external validity of AKI detection algorithms has recently also been demonstrated in other series, where AKI was however only based on Screa change according to a baseline8.
Our findings have important implications for the interpretation of randomized as well as observational clinical studies or automated alert or prediction systems that use a definition of AKI that ignores UO. The use of such a truncated definition stands in sharp contrast with clinical reality, where many clinicians will diagnose AKI based on both Screa and UO. Our findings indicate that these missed cases based on omitting UO are clinically significant, which might be important in randomised controlled trials as opportunities for intervention might be missed. The last decade has witnessed an increased interest in automated alerting and decision support, sparked by the hope that such systems may lead to earlier diagnosis and better tailored management of patients with AKI. Different algorithms for prediction and/or automated alerting for AKI are already being developed44. Given that systematic reviews have highlighted the lack of uniformity and transparency in how AKI is defined within these models7,9,11–13,45,46, most of which ignore UO, it is important for clinicians to be aware of the implications of the use of such a truncated definition of AKI26,27,33,47,48. Current automated decision support systems for AKI may mislead clinicians, as they can no longer be confident on the meaning and implications of the diagnostic label. Our findings indicate that such automated systems should incorporate or be trained on databases that include the UO criterion in their AKI label, and that, accordingly, measurement and registration of UO in electronic health records could be an efficient way to earlier detect patients with or at risk of AKI, and to potentially improve outcomes. Devices that automatically monitor UO might be a worthwhile asset to improve the dismal outcome of AKI in ICU.
Our study is based on highly granular routinely collected data from a large patient cohort, extracted from an operational ICIS database of a large tertiary care ICU. Because this is a single center study however, it is still unclear whether current findings can be extrapolated or generalized to other settings.
From a theoretical perspective, UO could be misleading in patients with either bladder retention or urinary incontinence. However, in our cohort, nearly all patients (84%) had an indwelling bladder catheter, and there was no difference between those with vs without AKI. In anuric patients, a bladderscan is routinely performed to asses eventual retention. Also, it is standard practice in our unit to provide for hygienic reasons to provide an indwelling bladder catheter in patients with urinary incontinence.
A further strength of our analysis is that by accounting for the timing of AKI diagnosis, our analytic approach eliminated immortal time bias. This type of bias may have invalidated the results of other studies that assessed the association between different AKI criteria and adverse outcomes15.
For simplicity and ease of exposition, we have limited the presentation of our results to a single operational definition of the SCrea criterion that uses a specific order of potential choices of serum creatinine baseline based on their availability, as intended by the spirit of KDIGO-AKI definition. In Supplementary Tables 1 and 2 and Supplementary Fig. 1, we present results using a range of different choices of baseline. Many other alternative choices could however potentially have been investigated, such as the median of all pre-ICU creatinine values, or most recent Screa before hospital admission. We can thus not exclude that these other choices would lead to different results, although, given the wide range of considered baselines, this may be considered unlikely.
RRT initiation was not incorporated either in the SCrea criterion, nor included as endpoint because this was considered a rather subjective criterion and its incorporation would, moreover, have conflated the condition with its treatment. Moreover, based on daily practice in our unit, RRT would be started without AKI only in a few exceptional cases, such as lactic acidosis or intoxications irrespective of kidney function.
In conclusion, ignoring UO in the diagnosis of KDIGO AKI stage ≥ 2 decreases sensitivity, may lead to delayed diagnosis and results in underestimation of KDIGO AKI stage ≥ 2 associated mortality.
Supplementary information
Acknowledgements
The authors wish to thank Bram Gadeyne and Veerle Brams for their technical support in the data acquisition phase.
Abbreviations
- AKI
Acute kidney injury
- CKD
Chronic kidney disease
- EHR
Electronic health records
- ICIS
Intensive care information system
- ICU
Intensive care unit
- KDIGO
Kidney disease improving global outcomes
- MDRD
Modification of diet in renal disease
- SCrea
Serum creatinine
- SOFA
Sequential organ failure assessment
- UO
Urinary output
Author contributions
J.V. and W.V.B. conceived the idea of this study. J.V., J.S. and W.V.B. have made substantial contributions to the conception and have drafted the first version of this manuscript. J.S. has contributed to data acquisition and coding. J.S., S.V., and W.V.B. conducted the statistical analysis, and J.S., S.V., P.M. and W.V.B. contributed to interpretation of the data. S.V., P.M., E.H., J.D., and D.B. critically reviewed the manuscript. All authors reviewed the manuscript.
Funding
This study was funded by FWO (Fonds Wetenschappelijk Onderzoek – Flemish Research Council) Grant Project Number 3G068619.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to potential privacy concerns but are available from the corresponding author (in pseudonymized format) on reasonable request.
Competing interests
WVB received travel grants and speaker fees from Fresenius Medical Care, Baxter Healthcare, and Nipro. EH received travel grants and speaker fees from Sopachem and AM Pharma. DB’s institution received grants from Gilead, Astellas, Fisher-Paykel, Baxter, Alexion, and Fresenius Kabi outside the submitted work. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Jill Vanmassenhove and Johan Steen.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-90646-0.
References
- 1.Lameire N, Van Biesen W, Vanholder R. The changing epidemiology of acute renal failure. Nat. Clin. Pract. Nephrol. 2006;2:364–377. doi: 10.1038/ncpneph0218. [DOI] [PubMed] [Google Scholar]
- 2.Hoste EA, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006;10:R73. doi: 10.1186/cc4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Biesen W, Vanholder R, Lameire N. Defining acute renal failure: RIFLE and beyond. Clin. J. Am. Soc. Nephrol. CJASN. 2006;1:1314–1319. doi: 10.2215/CJN.02070606. [DOI] [PubMed] [Google Scholar]
- 4.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure: definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cruz DN, Bagshaw SM, Ronco C, Ricci Z. Acute kidney injury: classification and staging. Contrib. Nephrol. 2010;164:24–32. doi: 10.1159/000313717. [DOI] [PubMed] [Google Scholar]
- 6.Fliser D, et al. A European Renal Best Practice (ERBP) position statement on the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines on acute kidney injury: part 1: definitions, conservative management and contrast-induced nephropathy. Nephrol. Dial. Transpl. Off. Pub. Eur. Dial. Transpl. Assoc. Eur. Renal Assoc. 2012;27:4263–4272. doi: 10.1093/ndt/gfs375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tomašev NGX, Rae JW, Zielinski M, Askham H, Saraiva A, Mottram A, Meyer C, Ravuri S, Protsyuk I, Connell A, Hughes C, Karthikesalingam A, Cornebise J, Montgomery H, Rees G, Laing C, Baker C, Peterson K, Reeves R, Hassabis D, King D, Suleyman M, Back T, Nielson C, Ledsam C, Mohamed S. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature. 2019 doi: 10.1038/s41586-019-1390-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song X, et al. Cross-site transportability of an explainable artificial intelligence model for acute kidney injury prediction. Nat. Commun. 2020;11:5668. doi: 10.1038/s41467-020-19551-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allen DW, et al. Risk prediction models for contrast-induced acute kidney injury accompanying cardiac catheterization: systematic review and meta-analysis. Can. J. Cardiol. 2017;33:724–736. doi: 10.1016/j.cjca.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 10.Caragata R, Wyssusek KH, Kruger P. Acute kidney injury following liver transplantation: a systematic review of published predictive models. Anaesth. Intensive Care. 2016;44:251–261. doi: 10.1177/0310057X1604400212. [DOI] [PubMed] [Google Scholar]
- 11.Hodgson LE, et al. Systematic review of prognostic prediction models for acute kidney injury (AKI) in general hospital populations. BMJ Open. 2017;7:e016591. doi: 10.1136/bmjopen-2017-016591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silver SA, et al. Risk prediction models for contrast induced nephropathy: systematic review. BMJ. 2015;351:h4395. doi: 10.1136/bmj.h4395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson T, et al. Risk prediction models for acute kidney injury following major noncardiac surgery: systematic review. Nephrol. Dial. Transpl. 2016;31:231–240. doi: 10.1093/ndt/gfv415. [DOI] [PubMed] [Google Scholar]
- 14.Macedo E, Malhotra R, Claure-Del GR, Fedullo P, Mehta RL. Defining urine output criterion for acute kidney injury in critically ill patients. Nephrol. Dial. Transpl. 2011;26:509–515. doi: 10.1093/ndt/gfq332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiersema R, et al. Different applications of the KDIGO criteria for AKI lead to different incidences in critically ill patients: a post hoc analysis from the prospective observational SICS-II study. Crit Care. 2020;24:164. doi: 10.1186/s13054-020-02886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siew ED, et al. Commonly used surrogates for baseline renal function affect the classification and prognosis of acute kidney injury. Kidney Int. 2010;77:536–542. doi: 10.1038/ki.2009.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siew ED, et al. Use of multiple imputation method to improve estimation of missing baseline serum creatinine in acute kidney injury research. Clin. J. Am. Soc. Nephrol. CJASN. 2013;8:10–18. doi: 10.2215/CJN.00200112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vanmassenhove J, Lameire N, Dhondt A, Vanholder R, Van Biesen W. Prognostic robustness of serum creatinine based AKI definitions in patients with sepsis: a prospective cohort study. BMC Nephrol. 2015;16:112. doi: 10.1186/s12882-015-0107-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lameire N, Van Biesen W, Vanholder R. The rise of prevalence and the fall of mortality of patients with acute renal failure: what the analysis of two databases does and does not tell us. J. Am. Soc. Nephrol. 2006;17:923–925. doi: 10.1681/ASN.2006020152. [DOI] [PubMed] [Google Scholar]
- 20.Sutherland SM, et al. Utilizing electronic health records to predict acute kidney injury risk and outcomes: workgroup statements from the 15(th) ADQI Consensus Conference. Can. 2016;3:11. doi: 10.1186/s40697-016-0099-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sutherland SM, Goldstein SL, Bagshaw SM. Acute Kidney Injury and Big Data. Contrib. Nephrol. 2018;193:55–67. doi: 10.1159/000484963. [DOI] [PubMed] [Google Scholar]
- 22.Park S, et al. Impact of electronic acute kidney injury (AKI) alerts with automated nephrologist consultation on detection and severity of AKI: a quality improvement study. Am. J. Kidney Dis. 2018;71:9–19. doi: 10.1053/j.ajkd.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 23.Kate RJ, Perez RM, Mazumdar D, Pasupathy KS, Nilakantan V. Prediction and detection models for acute kidney injury in hospitalized older adults. BMC Med. Inf. Decis. Mak. 2016;16:39. doi: 10.1186/s12911-016-0277-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kelly CJ, Karthikesalingam A, Suleyman M, Corrado G, King D. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 2019;17:195. doi: 10.1186/s12916-019-1426-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beam AL, Manrai AK, Ghassemi M. Challenges to the reproducibility of machine learning models in health care. JAMA, J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2019.20866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koeze J, et al. Incidence, timing and outcome of AKI in critically ill patients varies with the definition used and the addition of urine output criteria. BMC Nephrol. 2017;18:70. doi: 10.1186/s12882-017-0487-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allen JC, et al. Definition of hourly urine output influences reported incidence and staging of acute kidney injury. BMC Nephrol. 2020;21:19. doi: 10.1186/s12882-019-1678-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vail, E. A., Gershengorn, H. B., Wunsch, H., Walkey, A. J. Attention to immortal time bias in critical care research. Am. J. Respir. Crit Care Med. (2021). [DOI] [PubMed]
- 29.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl2, 1–138 (2012).
- 30.Levey AS, et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shintani AK, et al. Immortal time bias in critical care research: application of time-varying Cox regression for observational cohort studies. Crit. Care Med. 2009;37:2939–2945. doi: 10.1097/CCM.0b013e3181b7fbbb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat. Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 33.Macedo E, Malhotra R, Bouchard J, Wynn SK, Mehta RL. Oliguria is an early predictor of higher mortality in critically ill patients. Kidney Int. 2011;80:760–767. doi: 10.1038/ki.2011.150. [DOI] [PubMed] [Google Scholar]
- 34.Flechet M, et al. AKIpredictor, an online prognostic calculator for acute kidney injury in adult critically ill patients: development, validation and comparison to serum neutrophil gelatinase-associated lipocalin. Intensive Care Med. 2017;43:764–773. doi: 10.1007/s00134-017-4678-3. [DOI] [PubMed] [Google Scholar]
- 35.Chiofolo C, Chbat N, Ghosh E, Eshelman L, Kashani K. Automated continuous acute kidney injury prediction and surveillance: a random forest model. Mayo Clin. Proc. 2019;94:783–792. doi: 10.1016/j.mayocp.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 36.Mehta RL, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:1–8. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Siew ED, et al. Estimating baseline kidney function in hospitalized patients with impaired kidney function. Clin. J. Am. Soc. Nephrol. CJASN. 2012;7:712–719. doi: 10.2215/CJN.10821011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pickering JW, Endre ZH. Back-calculating baseline creatinine with MDRD misclassifies acute kidney injury in the intensive care unit. Clin. J. Am. Soc. Nephrol. CJASN. 2010;5:1165–1173. doi: 10.2215/CJN.08531109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bagshaw SM, et al. A comparison of observed versus estimated baseline creatinine for determination of RIFLE class in patients with acute kidney injury. Nephrol. Dial. Transpl. 2009;24:2739–2744. doi: 10.1093/ndt/gfp159. [DOI] [PubMed] [Google Scholar]
- 40.Zavada J, et al. A comparison of three methods to estimate baseline creatinine for RIFLE classification. Nephrol. Dial. Transpl. 2010;25:3911–3918. doi: 10.1093/ndt/gfp766. [DOI] [PubMed] [Google Scholar]
- 41.Bernardi MH, et al. Serum creatinine back-estimation in cardiac surgery patients: misclassification of AKI using existing formulae and a data-driven model. Clin. J. Am. Soc. Nephrol. CJASN. 2016;11:395–404. doi: 10.2215/CJN.03560315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Biesen W, Vanmassenhove J, Decruyenaere J. Prediction of acute kidney injury using artificial intelligence: are we there yet? Nephrol. Dial. Transpl. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Renal Assoc. 2020;35:204–205. doi: 10.1093/ndt/gfz226. [DOI] [PubMed] [Google Scholar]
- 43.Agniel D, Kohane IS, Weber GM. Biases in electronic health record data due to processes within the healthcare system: retrospective observational study. BMJ. 2018;361:k1479. doi: 10.1136/bmj.k1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gameiro J, Branco T, Lopes JA. Artificial intelligence in acute kidney injury risk prediction. J. Clin. Med. 2020 doi: 10.3390/jcm9030678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huen SC, Parikh CR. Predicting acute kidney injury after cardiac surgery: a systematic review. Ann. Thorac. Surg. 2012;93:337–347. doi: 10.1016/j.athoracsur.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mohamadlou H, et al. Prediction of acute kidney injury with a machine learning algorithm using electronic health record data. Can. J. Kidney Health Dis. 2018;5:2054358118776326. doi: 10.1177/2054358118776326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kellum JA, et al. Classifying AKI by Urine output versus serum creatinine level. J. Am. Soc. Nephrol. 2015;26:2231–2238. doi: 10.1681/ASN.2014070724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vanmassenhove J, et al. Urinary output and fractional excretion of sodium and urea as indicators of transient versus intrinsic acute kidney injury during early sepsis. Crit Care. 2013;17:R234. doi: 10.1186/cc13057. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to potential privacy concerns but are available from the corresponding author (in pseudonymized format) on reasonable request.