Abstract
Background
Virtual reality (VR) is a technology that produces a virtual manifestation of the real world. In recent years, VR has been increasingly used as a tool in medical education. The use of VR in medical education has large potential, as it allows for distance learning and training which may be challenging to deliver in real life. VR encompasses different tools and applications. There is a need to explore how VR has been employed in medical education to date.
Objective
The objective of this scoping review is to conceptualise the VR tools available and the applications of VR in undergraduate medical education as reported in the literature. This scoping review will identify any gaps in this field and provide suggestions for future research.
Methods and analysis
The relevant studies will be examined using the Joanna Briggs Institute methodological framework for scoping studies. A comprehensive search from a total of six electronic databases and grey literature sources will be performed. The reference list of included studies will be screened for additional studies. The screening and data extraction will be done in parallel and independently by two review authors. Any discrepancies will be resolved through consensus or discussion with a third review author. A data extraction form has been developed using key themes from the research questions. The extracted data will be qualitatively analysed and presented in a diagrammatic or tabular form, alongside a narrative summary, in line with Preferred Reporting Items for Systematic Reviews and Meta-Analysis: extension for Scoping Reviews reporting guidelines.
Ethics and dissemination
All data will be collected from published and grey literature. Ethics approval is therefore not a requirement. We will present our findings at relevant conferences and submit them for publications in peer-reviewed journals.
Keywords: medical education & training, world wide web technology, information technology
Strengths and limitations of this study.
A systematic and comprehensive search of electronic databases and grey literature sources will ensure that all available evidence is identified.
The scoping review will strictly follow the Joanna Briggs Institute methodology for scoping reviews.
A stakeholder consultation will allow us to further validate the findings and address potential gaps in the article.
A formal assessment of the quality of evidence will not be performed and this may lead to some studies of poor quality being included.
Only studies written in English and published after 2010 will be included.
Background
The demand for healthcare and healthcare professionals is rising around the world. By the year 2030, the global economy is projected to create 40 million new healthcare jobs, and yet at present there remains a shortage of 18 million healthcare workers.1 One factor contributing to this shortage has been a lack of effective undergraduate or preregistration medical education, which is defined as any type of initial study that leads to a medical degree that is recognised by relevant governments, and enables entry to the healthcare workforce.2 Medical education today comprises of both classroom theoretical learning as well as hospital-based learning where students are able to gain clinical experience. However, the hospital model has been criticised as being too expensive and impractical.3 To solve this problem, digital education has been seen as a promising way to deliver effective medical education. Digital education (also known as electronic education or e-learning) is defined as the act of teaching and learning via digital technologies.4 It is a broad term that encompasses a large number of methods, from a simple conversion of a book into PDF format to complex modalities such as mobile learning or mobile digital education, virtual patients, virtual reality (VR), serious gaming and gamification, massive open online courses and digital psychomotor skills trainers.5 Although there is a wide array of digital education tools available, in this scoping review we will be focusing on investigating one of the modalities, VR.
VR is defined as an educational tool that uses computer technology to create a three-dimensional (3D) image or environment that can be interacted in a seemingly real or physical way.6 VR is a broad concept that has many different tools and applications. There are three main categories of VR simulators, namely screen-based VR, immersive VR environments and virtual worlds.7 Screen-based VR consist of an interface connected to mechanical devices or haptic units, and can be displayed on any screen but most commonly using a desktop.8 This sort of VR has commonly been used to develop technical psychomotor skills, such as for endoscopic surgery, due to the fact that it can be used repeatedly and require very little time to setup.9 Immersive VR refers to a user in a virtual environment during which time his or her awareness of the real world is disconnected.10 This is most commonly done with the help of VR head-mounted displays (HMDs), such as Oculus Rift or HTC Vive.11 This can be further classified into high-end VR (use of dedicated controllers, eg, Oculus Rift, HTC Vive), mobile VR (use of a magnetic switch, eg, Google cardboard, Samsung Gear) or enhanced VR (a combination of HMDs with data gloves or bodysuits).11 It has been shown that immersive VR is associated with learners being more engaged, and acquired better cognitive, psychomotor and affective skills,12 but immersive VR lacks significant application in medical education to date, possibly due to the high cost of immersive VR that makes it impractical. Virtual worlds are 3D virtual environments based on multiplayer online gaming, freeing users from the constraints of location or time. The use of virtual worlds representing a clinical setting has been used in training emergency personnel on the management of mass-casualty or major incident situations.13–15 Avatars can be generated representing patients, which provides a more realistic simulation for the user.16
The use of VR in medical education can be applied in to two major areas. The first pertains to the use of VR to develop technical competencies, such as procedural skills or those that require extensive 3D visualisation. Examples of its applications has been in areas such as the learning of anatomy, surgical procedures and key skills such as cardiopulmonary resuscitation (CPR).17–20 Tools used in teaching of such skills involves mainly the use of screen-based VR for surgical procedures and 3D visualisation,19 21 and the use of virtual worlds for training of responses to stressful situations, such as CPR or emergency department situations.14 20 A second, less well-researched area, involves using VR to teach ‘soft skills’, such as empathy and communication skills with patients.7 16 22 This commonly involves the use of avatars (virtual patients) that respond in a certain way for users to communicate with.22 Considering the wide diversity of skills that can be practised with VR, coupled with the widespread reach and convenience of digital education, this could be a very powerful educational tool for medical students.
Given the wide array of tools available in the VR toolbox, as well as the diverse areas that VR can be applied to, there is a need to systematically identify the current VR applications available and in use for medical education, as well as identify which aspects of medical education could stand to benefit from VR, as reported in the literature.
Although there are reviews aiming to map different applications of VR is used in nursing and dentistry education, there seem to be none focusing on medical students’ education.23 24 Existing systematic reviews on VR in medical education mainly assess the effectiveness of VR within different surgical disciplines.21 25 This scoping review will instead adopt a much broader focus, by mapping out the extent of VR applications rather than focusing on the effectiveness of VR in a particular discipline.
Objectives
The objective of this scoping review is to identify the different VR tools and applications in undergraduate or preregistration medical education as reported in the literature. This scoping review also aims to identify any gaps in the current literature and provide suggestions for future research on the use of VR in medical education.
Methods
The proposed scoping review will be conducted in accordance with the Joanna Briggs Institute methodology for scoping reviews.26 This comprises of the following six stages: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; (5) collating, summarising and reporting the results and (6) stakeholder consultation. The protocol was registered on the Open Science Framework.27 The study is planned to begin in mid-March 2021 and is planned to end by July 2021.
Stage 1: identifying the research question
The objective of this scoping review is to outline the different VR modes available and the applications of VR in undergraduate or preregistration medical education. In line with the objectives of this scoping review, we have developed the following research questions:
How is VR used in undergraduate or preregistration medical education?
What are the main features of the VR applications in undergraduate or preregistration medical education?
What VR tools are available for undergraduate or preregistration medical education?
Which aspects of undergraduate or preregistration medical education has VR been applied to?
Stage 2: identifying relevant studies
A comprehensive search of the literature will be done using the following electronic databases: MEDLINE (Ovid), EMBASE (Elsevier), Cochrane Central Register of Controlled Trials (CENTRAL; Wiley) and Educational Resource Information Centre (ERIC; Ovid). Grey literature will be searched for through Google Scholar. As a first step, a limited search using keywords is conducted in the databases of MEDLINE. The search strategy will be piloted to check appropriateness of keywords and databases. In all retrieved articles, an analysis of the words contained within the title and abstracts, as well as index terms will be done to develop a full search strategy. Thereafter, a second search using all the identified keywords and index terms will be done across all databases. Finally, the third step will include screening of the reference lists of all studies selected for this scoping review to look for additional sources. A preliminary version of the MEDLINE search can be found in online supplemental appendix 1, which was developed with the help of a medical librarian experienced in the field. The search strategy will include year 2010 to present. We aim to start from 2010 as most literature pertaining to VR for education has been in recent years.28 We will search for literature in the English language only. All references identified will be imported into the reference manager software, EndNote X9. The references from different electronic databases will be combined and any duplicate records will be removed.
bmjopen-2020-046986supp001.pdf (20.6KB, pdf)
Stage 3: study selection
The study selection will follow a two-step screening process, consisting of a title and abstract screening, followed by a full-text review. In both steps, two independent reviews (JH and SV) will screen the articles against the eligibility criteria. Any disagreements will be discussed, and if no consensus can be reached a third reviewer (BMK) will be consulted. We will consider eligible studies based on the criteria in table 1.
Table 1.
Full inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
| Studies on undergraduate or preregistration medical students in any geographical setting. | Studies focusing only on virtual patient simulation, AR, MR, or serious gaming, without any involvement of VR. |
| Studies on VR used in undergraduate or preregistration medical education. | Studies published before 2010. |
| Studies involving the use of VR together with another modality, such as immersive VR, VR-based serious gaming, VR-based virtual patients. | Studies in languages other than English. |
| All primary studies, regardless of study design and relevant systematic reviews. | Opinion pieces, viewpoints and conceptual frameworks, conference abstracts |
AR, augmented reality; MR, mixed reality; VR, virtual reality.
The first step involves the screening of the title and abstract of the references using the reference manager software, EndNote X9. To qualify for the full-text scan, the title and abstract must (1) focus on the use of VR for educational use only and (2) have medical students as a target population. Virtual patients, that is, computer-generated programmes that simulates real-life clinical scenarios, can also be delivered in a VR format. In this scoping review, VR-based virtual patients will be included. We will also include studies on VR-based serious gaming education. Augmented reality (AR: superimposed VR onto the real-world environment)24 and mixed reality (MR: mixing of both virtual and digital elements, allowing one to interact with both simultaneously)29 are distinct entities that make use of VR and are not classified as VR. Studies focussing solely on MR/AR will also be excluded from this review.
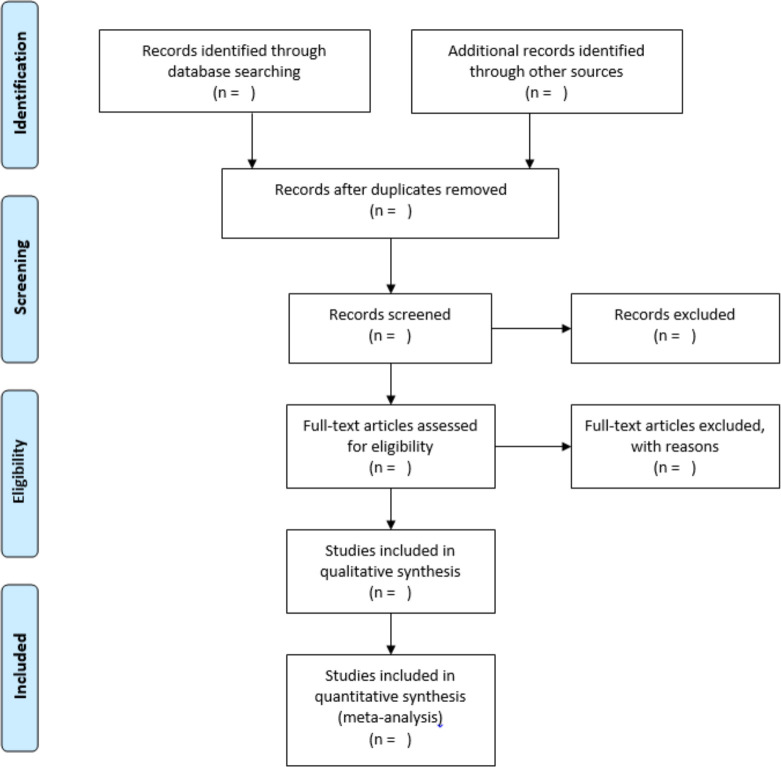
We will consider all primary studies, which includes experimental, observational and qualitative study designs. Systematic reviews will also be considered. The full-texts of the included studies will be retrieved and their citation details imported. Studies excluded at this stage will be described in the ‘Characteristics of excluded studies’ table, where reasons for exclusion will be noted. This process follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines,30 which is depicted in figure 1. Two review authors (JH and SV) will verify the final list of included studies.
Figure 1.
Flow diagram of study selection process, as depicted by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Stage 4: charting the data
Relevant data will be extracted from all included studies in the scoping review by two independent reviewers (JH and SV). A structured data recording form developed by the reviewers will be used and the information recorded on Microsoft Excel. The extracted data include details on the author; year of publication; title; type of study; country of study; WHO income level of country; objective of study; number of participants; year of study; type of VR used; VR mode, equipment used; subject taught; revised subject; duration of use; frequency of use; individual/group delivery; extent of immersion and extent of interactivity. A draft data extraction tool is included in online supplemental appendix 2. The draft data extraction tool will be piloted and revised as necessary during the process of extracting data from each study. Any disagreement that arises between reviewers will be resolved through discussion and a third review author (BMK) will act as an arbiter when disagreements cannot be resolved. We will contact the study authors for any missing or incomplete data.
Stage 5: collating, summarising and reporting the results (results same as data extracted)
To characterise and summarise the results, a map of the data extracted from the included papers will be presented in a diagrammatic or tabular form. In alignment with the objective of this study, we will provide an overview of the target participants, content of VR programmes, types of studies included and the context of each included study. The tabulated and/or charted results will be accompanied by a narrative summary, which will describe how the results meet the objectives and aims of this scoping review. We will report findings in line with the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analysis: extension for Scoping Reviews’ checklist.31 Gap identification will detect areas where there is paucity of data on VR content and its application in undergraduate or preregistration medical education.
Step 6: stakeholder consultation
A stakeholder consultation is planned to validate the findings from the review, add new insights and identify gaps for further research. Stakeholders will include researchers experienced in the field of medical education and digital health professions education. The stakeholder consultation will be done via presenting our study and findings to a group of experts in the field of medical education and collating their feedback. Their feedback will be incorporated into how we present our final article.
Discussion
Our scoping review will aim to provide insight into the existing evidence as well as gaps on the use of VR in medical education and provide recommendations for future research in this area. By exploring the current tools of VR used in medical application, we can identify areas which may have untapped potential. We can also identify aspects of medical education (eg, training of certain skills) which do not have any literature regarding the use of VR, thus representing a potential area of research. We will also show whether different tools of VR have been used in the same aspect of medical education, and if so future research could investigate the efficacy of the difference tools within the same sphere.
Ethics and dissemination
Ethical approval is not required for this study. Future disseminations related to this work will include the publication of the results in a peer-reviewed journal and presentations at conferences.
Supplementary Material
Acknowledgments
The authors thank Rebecca Lavaine David for her help in the development of the search strategy for MEDLINE.
Footnotes
Collaborators: Rebecca Lavaine David.
Contributors: LTC: conceived the idea for the review. JH and SV: wrote the review protocol. LTC and BMK: provided methodological guidance and critically revised the protocol. All authors gave their approval for the final version of the work to be published, and agreed to be accountable for the integrity of the work published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.World Health Organisation . High-Level Commission on health employment and economic growth, 2016. Available: https://www.who.int/hrh/com-heeg/en/
- 2.World Health Organisation . eLearing for undergraduate health professional education: a systematic review informing a radical transformation of health workforce development, 2015. [Google Scholar]
- 3.Van Way CW. Thoughts on medical education. Mo Med 2017;114:417–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Tudor Car L, Soong A, Kyaw BM, et al. Health professions digital education on clinical practice guidelines: a systematic review by digital health education collaboration. BMC Med 2019;17:139. 10.1186/s12916-019-1370-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Car J, Carlstedt-Duke J, Tudor Car L, et al. Digital education in health professions: the need for Overarching evidence synthesis. J Med Internet Res 2019;21:e12913. 10.2196/12913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim JH, Park ST, Lee H, et al. Virtual reality simulations in physics education. 3, 2001. [Google Scholar]
- 7.Bracq M-S, Michinov E, Jannin P. Virtual reality simulation in Nontechnical skills training for healthcare professionals: a systematic review. Simul Healthc 2019;14:188–94. 10.1097/SIH.0000000000000347 [DOI] [PubMed] [Google Scholar]
- 8.Van Herzeele I, Aggarwal R, Neequaye S, et al. Cognitive training improves clinically relevant outcomes during simulated endovascular procedures. J Vasc Surg 2008;48:1223–30. 30.e1. 10.1016/j.jvs.2008.06.034 [DOI] [PubMed] [Google Scholar]
- 9.Blackburn SC, Griffin SJ. Role of simulation in training the next generation of endoscopists. World J Gastrointest Endosc 2014;6:234–9. 10.4253/wjge.v6.i6.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ott M, Freina L, eds. A literature review on immersive virtual reality in education: state of the art and perspectives, 2015. [Google Scholar]
- 11.Radianti J, Majchrzak TA, Fromm J, et al. A systematic review of immersive virtual reality applications for higher education: design elements, lessons learned, and research agenda. Comput Educ 2020;147:103778. 10.1016/j.compedu.2019.103778 [DOI] [Google Scholar]
- 12.Jensen L, Konradsen F. A review of the use of virtual reality head-mounted displays in education and training. Educ Inf Technol 2018;23:1515–29. 10.1007/s10639-017-9676-0 [DOI] [Google Scholar]
- 13.Cohen D, Sevdalis N, Patel V, et al. Tactical and operational response to major incidents: feasibility and reliability of skills assessment using novel virtual environments. Resuscitation 2013;84:992–8. 10.1016/j.resuscitation.2012.12.011 [DOI] [PubMed] [Google Scholar]
- 14.Heinrichs WL, Youngblood P, Harter P, et al. Training healthcare personnel for mass-casualty incidents in a virtual emergency department: VED II. Prehosp Disaster Med 2010;25:424–32. 10.1017/S1049023X00008505 [DOI] [PubMed] [Google Scholar]
- 15.Hudson K, Taylor LA, Kozachik SL, et al. Second life simulation as a strategy to enhance decision-making in diabetes care: a case study. J Clin Nurs 2015;24:797–804. 10.1111/jocn.12709 [DOI] [PubMed] [Google Scholar]
- 16.Quail NPA, Boyle JG. Virtual patients in health professions education. Adv Exp Med Biol 2019;1171:25–35. 10.1007/978-3-030-24281-7_3 [DOI] [PubMed] [Google Scholar]
- 17.Khan R, Plahouras J, Johnston BC, et al. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev 2018;8:Cd008237. 10.1002/14651858.CD008237.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagendran M, Gurusamy KS, Aggarwal R. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2013;2013:CD006575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moro C, Štromberga Z, Raikos A, et al. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ 2017;10:549–59. 10.1002/ase.1696 [DOI] [PubMed] [Google Scholar]
- 20.Wong MAME, Chue S, Jong M, et al. Clinical instructors' perceptions of virtual reality in health professionals' cardiopulmonary resuscitation education. SAGE Open Med 2018;6:205031211879960. 10.1177/2050312118799602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gurusamy KS, Aggarwal R, Palanivelu L, et al. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2009:CD006575. 10.1002/14651858.CD006575.pub2 [DOI] [PubMed] [Google Scholar]
- 22.Dyer E, Swartzlander BJ, Gugliucci MR. Using virtual reality in medical education to teach empathy. J Med Libr Assoc 2018;106:498–500. 10.5195/JMLA.2018.518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fealy S, Jones D, Hutton A, et al. The integration of immersive virtual reality in tertiary nursing and midwifery education: a scoping review. Nurse Educ Today 2019;79:14–19. 10.1016/j.nedt.2019.05.002 [DOI] [PubMed] [Google Scholar]
- 24.Huang T-K, Yang C-H, Hsieh Y-H, et al. Augmented reality (AR) and virtual reality (VR) applied in dentistry. Kaohsiung J Med Sci 2018;34:243–8. 10.1016/j.kjms.2018.01.009 [DOI] [PubMed] [Google Scholar]
- 25.Bernardo A. Virtual reality and simulation in neurosurgical training. World Neurosurg 2017;106:1015–29. 10.1016/j.wneu.2017.06.140 [DOI] [PubMed] [Google Scholar]
- 26.Micah DJ, Peters CG, McInerney P, et al. Chapter 11: Scoping reviews (2020 version) JBI manual for evidence synthesis, 2020. Available: https://synthesismanual.jbi.global/
- 27.Jiang H, Vimalesvaran S, Kyaw BM. Virtual reality in medical students’ education: a scoping review protocol, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kyaw BM, Saxena N, Posadzki P, et al. Virtual reality for health professions education: systematic review and meta-analysis by the digital health education collaboration. J Med Internet Res 2019;21:e12959. 10.2196/12959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tepper OM, Rudy HL, Lefkowitz A, et al. Mixed reality with HoloLens: where virtual reality meets augmented reality in the operating room. Plast Reconstr Surg 2017;140:1066–70. 10.1097/PRS.0000000000003802 [DOI] [PubMed] [Google Scholar]
- 30.Peters MDJ, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141–6. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 31.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-046986supp001.pdf (20.6KB, pdf)