Abstract
While social inequality is widely recognised as being a risk factor for COVID-19 infection or serious forms of the disease, many questions still remain concerning the perception of hazard and protective measures by the most vulnerable populations.
This mixed-methods study aimed (1) to describe the self-perceived health and protective measures linked to COVID-19 of homeless people in one of the largest and poorest cities in France, and (2) to assess which skills and resources they used to address the COVID-19 pandemic. The quantitative survey addressed these questions among a sample of 995 homeless people living either on the streets, in homeless shelters or in squats/slums, whereas the qualitative survey was constructed from 14 homeless interviewees. Both data collections were carried out between June and July 2020.
Results showed that COVID-19 infection was clearly perceived by homeless people as a risk, but the experience of being homeless placed this risk among several others. Different practices of protection were observed according to the type of living place. Lockdown of the general population severely impacted the survival systems of the populations furthest from housing, with alarming rates of people without access to water or food. 77% of homeless participants reported that they encountered significant financial difficulties. All interviewees were particularly attentive to their health, with awareness and even a familiarity with the risks of infectious diseases long before the pandemic.
Using a capability framework, our study showed a predominant lack of external health-related resources for homeless people, while internal health-related resources were more developed than expected. None of the places and lifestyles studied was favourable to health: collective shelters due to a greater restriction of people's choices, slums and street life due to a greater lack of basic resources.
Keywords: Homelessness, COVID-19, Lockdown, Perceptions, Practices, Health inequalities
Highlights
-
•
Stay-at-Home Orders were announced to protect population, but could not be observed by people without home.
-
•
Homeless people living rough or in slums have been even more under-resourced during the crises despite public mobilization.
-
•
Emergency shelters were perceived as a high-risk place of contamination, despite a scrupulous respect of protective measures.
-
•
Homeless people are more familiar with infectious diseases and associated protective measures, which translate into good skills and practices in dealing with COVID-19.
-
•
For interviewees, COVID-19 was one more risk, among many others.
1. Introduction
Evidence of socio-economical inequalities in relation to COVID-19 is already emerging (Bello-Chavolla et al., 2020; Holmes et al., 2020), and suggests that the current outbreak is a ‘syndemic pandemic’, which interacts with and exacerbates existing social inequalities in chronic disease and the social determinants of health (Bambra, Riordan, Ford, & Matthews, 2020). Homelessness, which represents an extreme form of health inequality, is growing steadily in most countries where it is measured. As shown by the number of press publications on the subject, public opinion has been moved by the plight of the homeless during the COVID-19 crisis, and most authorities have mentioned these populations as targets for specific policies, e.g in Europe (Rahman, 2020). Indeed, homeless people appear to be particularly vulnerable to the COVID-19 infection (Holmes et al., 2020; Kirby, 2020; Maxmen, 2020), with specific living conditions as overcrowded accommodations or frequent contacts with people through community services (food distributions or day-care facilities). Research that has focused on the issue of homelessness and COVID-19 considered measures to control the spread of the virus in shelters, the prevalence of positive cases, or factors associated with transmission in shelters (Vandentorren, 2021). Despite this research, little has been published to our knowledge on homeless people's living experience and their perception of COVID-19 and the COVID-19-related crisis. Yet, homeless people's experience of the COVID-19 outbreak and of lockdown appears to unique, since staying at home is, by definition, impossible for the homeless. Potential consequences of lockdown for the homeless population may affect their resources, with panhandling or illegal work activities (Poremski et al., 2015) having been shut down. In addition, being moved for sheltering may have potentially destabilized the aid and assistance network.
In France before the COVID-19 crisis, 3.5 million people are considered precariously housed and 141,500 homeless, a number which has increased by 44% over the past decade (Mordier, 2016). Specialized associations estimate that this figure could have doubled during the crisis (; ). Marseille is the second most-populated city in France (863,310 inhabitants), and one of its poorest, with almost one third of its population living under the threshold of poverty (INSEE, 2020). The first French lockdown was ordered on March 17, 2020, and it mobilised emergency social action to ensure that a maximum of homeless people were given shelter: hotels and holiday resorts were used in addition to existing shelters that were already full. The ‘winter eviction ban’,1 mandated each year by French government, was extended by decree. Accommodation conditions and lengths of stay were suspended for the duration of lockdown. At the same time, the majority of organisations providing welfare benefits were forced to close and work from home. Outreach teams, however, had to continue their support missions, while reorganising their activities to ensure the health safety of their staff and of the people receiving.
These early issues brought up many questions concerning the perception of hazard and protective measures by the most vulnerable populations: How did lockdown temporarily modify the daily practices of homeless people? How did homeless people mobilise their resources? First, these questions led to a survey on three types of extremely vulnerable populations with regards to housing: people living rough, people living in homeless shelters and people living in slums. Second, we investigated the role of the types of homeless accommodations as structural factors that could contribute to addressing differences in qualitative findings and adapted solutions. More precisely, we suggest that examination of the relationship between homeless living settings and resources may help us understand and address disparities in an epidemic context for homeless people.
The objectives of this study were to describe the self-perceived health and protective measures linked to COVID-19 of homeless people in a large city in France, and assess which kinds of resources they used to address the COVID-19 pandemic.
2. Methods
2.1. Study design
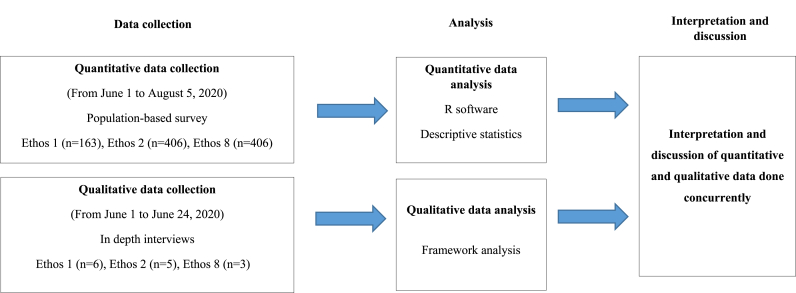
This analysis was built using a mixed-methods approach, which was the most appropriate to develop a more complete understanding of the question, with the experience of homeless people in various settings retrieved as narratives on one hand, and the relationship between resources and type of accommodation measured among all participants on the other hand. Multiplying observation methods would reduce the multiple blind spots of this pandemic for complex questions such as hazard perception and protective measures.
To address the research questions, the study applied a concurrent triangulation mixed methods design using qualitative and quantitative approaches (Fig. 1). A population-based cohort study was carried out among homeless people living in Marseille, with a recruitment from 18 outreach teams in more than 50 different locations including streets, slums, squats, emergency or transitional shelters and drop-in centres, and qualitative data were obtained from 14 in-depth interviews offered systematically to the first participants enrolled. We privileged qualitative and quantitative interviews in the participant's native language. Participants had the choice between a physical translator from the research team, or a telephone translator thanks to ‘ISM translation’, a company that provides professional telephone translation in 75 languages. Physical translation in 8 languages was available since the research team recruited people from the territory's main communities as mediators and translators in Albanian, Arabic, Georgian, Romanian, and Serbian. In addition, four interviewers spoke native Arabic, English, German and Spanish.
Fig. 1.
A concurrent triangulation mixed methods design.
The data originates from the ongoing COVIDHomeless study (NCT04408131).
2.2. Quantitative survey
2.2.1. Sample
The quantitative study design and sample size has been described elsewhere (Loubière et al., 2021). In brief, participants were enrolled between June 1 and August 5, 2020. Participants signed a consent form to participate after having received information on the study's purposes, intended data use, and being ensured anonymity. Recruitment was based on typology from work by the FEANTSA (European Federation of National Organisations Working with the Homeless) that provides a descriptive framework of living conditions for people with poor housing conditions. This graded typology, called ETHOS (European Typology of Homelessness and housing exclusion), defines thirteen categories (Amore et al., 2011).
In order to focus on the homeless people the furthest from housing, we decided to select the ETHOS categories characterized by the greatest residential instability. As a result, eligible individuals were aged over 18 and were classified in the following ETHOS typology: 1) living rough (ETHOS1), 2) living in emergency accommodations (emergency shelters and hotels) (ETHOS2); and 3) living in insecure accommodations (i.e., illegal occupation of land, squat or slum) (ETHOS8).
Stabilization shelters (ETHOS 3) were not included at the beginning of the study since lengths of stay were suspended for the duration of the lockdown (and therefore ETHOS 3 no longer really corresponded to its definition: ‘homeless shelter where the period of stay is intended to be short term’). We decided to include this living condition in the study when they started receiving people from the street again. Nevertheless, the population from ETHOS 3 was not included in the current analysis because their recruitment began after the qualitative collection was completed. ETHOS categories 4 to 7 were not included as they refer to more stable accommodations: (women's shelters (ETHOS 4), accommodation for immigrants (ETHOS 5), people living in institution (healthcare or penal) (ETHOS 6)).
A choice among the categories of homeless people was necessary since we could not do random sampling in the absence of reliable census data on the population living rough (ETHOS 1) and in squats or slums (ETHOS 8) in Marseille. We decided to be as exhaustive as possible on one point in time. We chose therefore to work with all outreach teams from public health and social services and community partners to identify people living on the streets or in slums. We set a 2-month inclusion period (June to August 2020): during this period, no less than 18 outreach teams accompanied by members of the research team went to all of the known places where people from ETHOS 1 or 8 were present at that time. The research project was proposed to all the people present in these places, with successive meetings with the targeted population during the 2 months of inclusion in order not to miss anyone.
It was much easier to be exhaustive for ETHOS 2 and 3, as these facilities are well known in Marseille. In a similar way to the process developed for ETHOS 1 and 8, several meetings were organized in each facility during the 2 months of inclusion in order to present the project to all the people sheltered in the facility.
Follow-up visits were planned with the participants and their support team at 3 and 6 months from inclusion. These visits consisted of face-to-face meeting to answer a questionnaire and perform a rapid COVID-19 serological test. If participants had COVID-19 symptoms between scheduled visits, they or their usual support team could alert the research team, which was able to test them quickly for SARS-CoV-2 and provide guidance to the most appropriate solutions.
2.2.2. Data collection
A face-to-face survey was implemented using ‘Redcap’ e-CRF software (www.project-redcap.org) to investigate medical, public health and socio-economic issues. The questionnaire included demographic characteristics, ETHOS typology of homelessness before national first lockdown, history of accommodations since the COVID-19 outbreak, and medical data such as comorbidities (i.e., significant chronic or acute illness), and any medical events linked to COVID-19 infection (i.e., symptoms, hospitalizations, isolation measures, etc.).
In addition, we addressed several questions about 1) self-reported compliance with preventive measures (i.e. wearing masks, hand washing, physical distancing), 2) self-perceived health, 3) unmet needs related to health (i.e., somatic or psychiatric illnesses or addiction disorders), and 4) financial resources and difficulties related to access to primary/essential resources (i.e. food, water, hygiene and cleaning products).
2.3. Qualitative survey
This qualitative survey is a “rapid qualitative research study” (Johnson & Vindrola-Padros, 2017) aiming to collect a set of qualitative data at a period close to the critical point of the episode in order to rapidly report on health and social issues with the aim to guide field work.
2.3.1. Sample
The qualitative collection was carried out between June 1 and June 24, 2020. A sociologist familiar with this kind of terrain met the first participants enrolled in the study in order to collect data as close as possible of their experience, and systematically offered them an interview. Interviews were carried out in each of the 3 ETHOS categories (1, 2 and 8) and until data saturation. Eligible participants were recruited alongside the first phase of the COVIDHomeless cohort recruitment process. There were no refusals among homeless people invited to participate in the qualitative survey. In order to ensure a high participation rate and representativeness, people who were uncomfortable with the French language received information and a consent form to sign in their native language, and interviews were carried out with the presence of an interpreter to facilitate the communication flows when needed. The sample was considered adequate after 14 interviews because it was both appropriate in its composition and of sufficient size since no new themes emerged from the last narratives of the interviewees. A total of Among the 14 individuals were who were interviewed: 6 people belonged to the ‘ETHOS 1’ category (i.e., living rough); 5 people belonged to the ‘ETHOS 2’ category (i.e., living in emergency shelters); and 3 people belonged to the ‘ETHOS 8’ category (i.e., living in slums).
2.3.2. Data collection
Face-to-face semi-standardised interviews were carried out, recorded and transcribed verbatim. Each of the people was interviewed at their living or begging place. All the participants were informed of the study objectives. At the end of the interview, they were given a 10-euro voucher to repay them for time spent with the researcher. In addition, observations were noted daily in a field book and transcribed.
2.4. Data analyses
2.4.1. Quantitative analysis
Descriptive analyses were presented as frequencies and percentages for categorical variables, and as means and standard deviations for continuous variables. Fisher's exact test and Wilcoxon rank-sum test were used to compare the characteristics between types of accommodation before the French national lockdown (i.e., ETHOS categories of homeless typology). Regression analyses were performed to test the significance of the differences between participants according to their type of accommodation on sociodemographic and medical characteristics, resource issues, compliance of preventive measures or any complaints related to uncovered health care or social needs during the COVID-19 outbreak. Adjusted odds ratios were reported (i.e. adjustments on age, country of birth, education level, and length of homelessness), with a 95% confidence interval. Post hoc multiple comparisons using the Tukey test were performed to address pairwise comparisons between accommodation categories. Statistical analysis was performed using R version 3.6.0 (RStudio, Inc., Massachusetts, USA).
2.4.2. Comparison between ETHOS categories
Defining and understanding homelessness at a global level led to develop valid measurement of homeless populations like ETHOS typology, based on operational categories related to the place and conditions of living (Busch-Geertsema, 2016). These living places correspond to very different living conditions, ranging for totally institutional (shelters) to totally non-institutional (streets or slums). ETHOS categories were chosen and compared to better examine structural factors constituted by living places, since structures differ between themselves according to a set of parameters that are as much related to the resources made available (in publicly funded establishments), as to the concentration of people in the same place (heterogeneous according to the type of accommodation but relatively homogeneous within the same type of accommodation). This comparison between policy-relevant subgroups was also chosen to enlighten decision-makers on the disparities in living conditions and the level of exposure to risk in the homeless population.
2.5. Qualitative analysis
The interview grid was designed to ask the homeless people: 1) how they perceived the COVID-19 pandemic (i.e. the types of sources of information they had access to, and their understood of the COVID-19 infection and the lockdown); 2) what their living conditions were during the COVID-19 lockdown (especially the places where they had or had not stayed); and 3) what had been the impact of lockdown on their financial situation, their access to food, their acceptability of control measures (i.e., lockdown, preventive measures, testing and screening strategies), and their level of perception of the health hazard. In vivo manual coding was used. Analytical categories were extracted from the data. Social regularities resulting from this categorisation became the subjects for analysis shown here. Five analytical categories with sub-dimensions were finally extracted from the data collected (Table 1).
Table 1.
Qualitative survey framework: analytical categories and sub-categories.
| Analytical categories | Analytical sub-categories |
|---|---|
| Causes/Consequences of lockdown |
|
| |
| Perceived health and coronavirus |
|
| |
| Type of housing and acceptability of housing |
|
| |
| |
| Being locked down outside |
|
| |
| |
| |
| Acceptability of control measures |
|
| |
| |
|
2.6. Mixed-methods analysis
After carrying out separate quantitative and qualitative analyses, results were then crossed. The results of the qualitative research were balanced with the quantitative findings to identify potential explanations for the observed relationships between accommodation types, resource availability, attitudes towards preventive measures, and homeless people's perceptions of risk for COVID-19.
2.7. Ethical considerations
The COVIDHomeless study was designed and carried out in compliance with the Declaration of Helsinki and with legal and regulatory provisions. It was approved by the ethics committee on May 28, 2020 (CPP IDF VI - number 44–20; ID: 2020-AO1398-31). All of the people included in this study provided written informed consent.
3. Results
3.1. Quantitative results
Between June 1 and August 5, 2020, we enrolled 1274 individuals. 995 of whom lived, at the time of lockdown, in streets (n = 163, 16.4%), emergency shelters (n = 406; 40.8%) or slums/squats (n = 426; 42.8%) and were included in our analysis (Table 2). The mean age was 39.2 (standard deviation: 14.2) years. The majority of respondents were men (71.7%), and had a lower secondary level of education or had obtained no school qualifications (80.1%). A large majority of responders were foreign (84.8%) and were born abroad, mostly from African countries (42.3%) or Europe (37.1%). About one third of our sample (34.8%) reported long-term homelessness (>5 years).
Table 2.
Sociodemographic characteristics of the quantitative study population (n = 995).
| Sociodemographic characteristics | Total N = 995 |
ETHOS 1 Living rough N = 163 |
ETHOS 2 Emergency shelters N = 406 |
ETHOS 8 Squats N = 426 |
|---|---|---|---|---|
| n (%) or mean (SD) | n (%) or mean (SD) | n (%) or mean (SD) | n (%) or mean (SD) | |
| Women | 286 (28.74%) | 35 (21.47%) | 57 (14.04%) | 194 (45.54%) |
| Age, year | 39.2 (14.2) | 40.4 (13.4) | 41.3 (15.4) | 36.9 (12.8) |
| Age, median (IQR), year | 37.0 (21.0) | 39 (20.5) | 38.5 (22.7) | 35.0 (20.0) |
| French nationality | 148 (14.98%) | 55 (33.95%) | 63 (15.59%) | 30 (7.11%) |
| Do not speaking French | 435 (44.57%) | 44 (27.16%) | 116 (28.86%) | 275 (66.75%) |
| Country of Birtha,b | ||||
| France | 159 (16.03%) | 68 (41.98%) | 60 (14.81%) | 31 (7.29%) |
| European union | 179 (18.04%) | 19 (11.73%) | 20 (4.94%) | 140 (32.94%) |
| Outside European union | 189 (19.05%) | 19 (11.73%) | 30 (7.41%) | 140 (32.94%) |
| Africa | 420 (42.34%) | 44 (27.16%) | 274 (67.65%) | 102 (24%) |
| Other | 45 (4.54%) | 12 (7.41%) | 21 (5.19%) | 12 (2.82%) |
| Education attainment | ||||
| No diploma | 473 (51.3%) | 70 (46.98%) | 158 (41.25%) | 245 (62.82%) |
| Lower secondary | 357 (38.72%) | 62 (41.61%) | 178 (46.48%) | 117 (30%) |
| Upper secondary or vocational | 92 (9.98%) | 17 (11.41%) | 47 (12.27%) | 28 (7.18%) |
| Don't know or missing | ||||
| Health insurance c,a | 648 (67.08%) | 98 (64.05%) | 302 (76.65%) | 248 (59.19%) |
| Length of homelessness, | ||||
| <3 months | 78 (8.12%) | 7 (4.43%) | 22 (5.45%) | 49 (12.28%) |
| 3–12 months | 193 (20.08%) | 33 (20.89%) | 111 (27.48%) | 49 (12.28%) |
| 1–5 years | 356 (37.04%) | 62 (39.24%) | 163 (40.35%) | 131 (32.83%) |
| >5 years | 334 (34.76%) | 56 (35.44%) | 108 (26.73%) | 170 (42.61%) |
| Having change of accommodation during COVID-19 crisis, Yes | 414 (41.6%) | 99 (66.00%) | 160 (41.13%) | 155 (37.80%) |
| Having financial resources | 577 (60.23%) | 104 (68.42%) | 227 (57.61%) | 246 (59.71%) |
| Having a working situation | 788 (82.25%) | 133 (87.5%) | 343 (87.06%) | 312 (75.73%) |
| Tobacco consumption, Yes | 514 (56.42%) | 116 (76.82%) | 194 (51.05%) | 204 (53.68%) |
| Alcohol (at least 3 glasses), Yes | 245 (24.62%) | 78 (51.66%) | 86 (22.93%) | 47 (12.81%) |
| Having at least one comorbidity d | 476 (47.84%) | 93 (57.06%) | 208 (51.23%) | 175 (41.08%) |
| Psychiatric or addiction comorbidities | 227 (22.81%) | 77 (47.24%) | 85 (20.94%) | 65 (15.26%) |
| Having ever been infected with the COVID-19 virus, yes | 21 (2.8%) | 0 (0%) | 24 (5.9%) | 3 (0.7%) |
SD: standard deviation.
∗ETHOS: the European typology for homelessness and housing exclusion.
Missing data were less than 3% and were not reported.
“European Union” countries: Belgium, Bulgaria, Germany, Hungary, Italy, Poland, Portugal, Romania, Czech Republic, Slovakia, and Spain. “Outside European Union” countries: Albania, Armenia, Bosnia, Croatia, Moldavia, Montenegro, Serbia, Russia including Chechenia, and Ukraine.
3.1.1. Self-reported compliance with protective measures
At least three-quarters reported good compliance with the preventive measures against COVID-19 and obviously, understanding of what lockdown meant in the context of COVID-19 was high (92.8%). Table 3 shows the results of regression models. Participants living in emergency shelters exhibited higher self-reported compliance rates compared to their counterparts in streets or slums concerning all preventive measures (P < 0.0001), with odds ratios ranging between 2.9 and 4.2. Reported overall compliance with preventive measures was higher in emergency shelters vs. streets (OR 5.9 [3.7–9.6]), but also in slums compared to streets (OR 2.9 [1.8–4.6]).
Table 3.
Unmet healthcare needs, self-reported compliance with preventive measures, difficulties in access to resources (N = 995).
| Total N = 995 | ETHOS 1 Living rough N = 163 | ETHOS 2 Emergency shelters N = 406 | ETHOS 8 Squats N = 426 | P-value In Univariate analysis | Adjusted OR (95%CI) | |||
|---|---|---|---|---|---|---|---|---|
| Compliance with preventive measures | ||||||||
| Wearing mask | 684 (71.92%) | 89 (58.94%) | 338 (86.45%) | 257 (62.84%) | <0.0001 | ETHOS2 vs.1 | 4.10 | (2.60–6.45) |
| ETHOS2 vs. 8 | 2.94 | (1.81–4.76) | ||||||
| ETHOS8 vs.1 | 1.40 | (0.91–2.13) | ||||||
| Hand washing | 710 (74.74%) | 96 (63.16%) | 346 (88.72%) | 268 (65.69%) | <0.0001 | ETHOS2 vs.1 | 4.03 | (2.49–6.51) |
| ETHOS2 vs. 8 | 3.12 | (1.88–5.26) | ||||||
| ETHOS8 vs.1 | 1.29 | (0.83–1.99) | ||||||
| Physical distancing | 710 (74.89%) | 94 (62.25%) | 347 (88.75%) | 269 (66.26%) | <0.0001 | ETHOS2 vs.1 | 4.21 | (2.61–6.80) |
| ETHOS2 vs. 8 | 2.94 | (1.78–4.76) | ||||||
| ETHOS8 vs.1 | 1.43 | (0.94–2.22) | ||||||
| Overall compliance | 749 (79.51%) | 88 (58.28%) | 349 (89.72%) | 312 (77.61%) | <0.0001 | ETHOS2 vs.1 | 5.93 | (3.66–9.59) |
| ETHOS2 vs. 8 | 2.04 | (1.19–3.57) | ||||||
| ETHOS8 vs.1 | 2.90 | (1.84–4.57) | ||||||
| Access to financial resources | ||||||||
| Reporting financial | 744 (76.62%) | 131 (82.39%) | 263 (66.41%) | 350 (84.13%) | 0.0002 | ETHOS1 vs.2 | 2.08 | (1.29–3.33) |
| difficulties since | ETHOS1 vs.8 | 0.85 | (0.51–1.43) | |||||
| SARS-CoV-2 crisis | ETHOS8 vs.2 | 2.43 | (1.53–3.86) | |||||
| Reporting difficulties in getting access to primary resources | ||||||||
| Water | 277 (28.59%) | 60 (38.96%) | 19 (4.79%) | 198 (47.37%) | <0.0001 | ETHOS1 vs.2 | 14.31 | (7.12–20.0) |
| ETHOS8 vs. 2 | 17.43 | (8.91–34.09) | ||||||
| ETHOS8 vs.1 | 1.31 | (0.86–1.99) | ||||||
| Food | 465 (47.79%) | 93 (60.0%) | 96 (24.06%) | 276 (65.87%) | <0.0001 | ETHOS1 vs.2 | 4.34 | (2.86–6.67) |
| ETHOS8 vs. 2 | 4.71 | (3.11–7.12) | ||||||
| ETHOS8 vs.1 | 1.08 | (0.71–1.64) | ||||||
| Hygiene products | 330 (34.92%) | 74 (49.01%) | 31 (7.93%) | 225 (55.83%) | <0.0001 | ETHOS1 vs. 2 | 11.11 | (6.67–20.0) |
| ETHOS8 vs. 2 | 11.87 | (6.08–20.73) | ||||||
| ETHOS8 vs.1 | 1.04 | (0.68–1.58) | ||||||
| Cleaning products | 286 (30.95%) | 52 (36.11%) | 20 (5.22%) | 214 (53.9%) | <0.0001 | ETHOS1 vs.2 | 10.00 | (5.56–20.0) |
| ETHOS8 vs 2 | 17.51 | (9.10–33.69) | ||||||
| ETHOS8 vs.1 | 1.74 | (1.13–2.70) | ||||||
| Unmet healthcare needs | ||||||||
| About physical health | 160 (16.67%) | 27 (17.65%) | 84 (21.27%) | 49 (11.89%) | NS | ETHOS1 vs. 2 | 0.82 | (0.47–1.34) |
| ETHOS 8 vs.1 | 0.61 | (0.35–1.06) | ||||||
| ETHOS8 vs. 2 | 0.50 | (0.29–0.86) | ||||||
| About mental health | 228 (23.77%) | 50 (32.89%) | 109 (27.59%) | 69 (16.75%) | <0.0001 | ETHOS2 vs.1 | 0.70 | (0.46–1.08) |
| ETHOS2 vs.8 | 1.96 | (1.20–3.17) | ||||||
| ETHOS1 vs. 8 | 2.78 | (1.58–4.88) | ||||||
3.1.2. Self-perceived health
One half (47.8%) reported having at least one comorbidity and 22.8% reported having psychiatric or addiction comorbidities. The main comorbidities reported by the study participants were as follows: cardiovascular pathology (11.9%), diabetes (7.4%), obesity or chronic respiratory pathology (7.1%), chronic renal failure (1.8%) and cancer (1.2%). Overall, 15.2% reported having psychiatric or addiction comorbidities and estimates were different between ETHOS categories: 31.3% in ETHOS 2, 15.3% in ETHOS 8 and ETHOS 1.
Only 2.8% reported known prior Covid-19 infection. The proportion of people experiencing prior COVID-19 infection was much higher in participants living in ETHOS2 (5.9%) than in their counterparts from ETHOS 1 (0%) or ETHOS 8 (0.7%).
3.1.3. Unmet needs related to health
One quarter of our participants reported having unmet healthcare needs during lockdown (Table 3); and among those who reported psychiatric comorbidities, one half had unmet psychiatric care needs. We found no statistically significant differences between street and emergency shelter categories for unmet healthcare needs, although participants from slums reported lower rates of unmet healthcare needs compared to emergency shelter participants (OR 0.50 [0.29–0.86]).
3.1.4. Difficulties related to access to primary resources
Overall, 77% of our participants reported having encountered financial issues during the COVID-19 outbreak (Table 3). 42% had changed accommodation at least once since the onset of the COVID-19 crisis: 66% of people living rough (ETHOS 1), 41% of people living in emergency shelters (ETHOS 2), 38% of people living in slums (ETHOS 8). Estimates of difficulties in access to essential resources were significantly different between ETHOS1 (rough sleeping) and ETHOS2 (emergency shelters) categories: 38.9% vs. 4.8% for water (OR 14.3 [95%CI: 7.1–25]; P < 0.0001); 60.0% vs. 24.1% for food (OR: 4.3 [95%CI: 2.8–6.7]; P < 0.0001); 49.0% vs 7.9% for hygiene products (OR: 11.1 [6.7–20]; P < 0.0001) and 36.1% vs. 5.2% for cleaning products (OR: 10.0 [5.6–20]; P < 0.0001). Similarly, homeless participants living rough reported higher rates of financial difficulties since the COVID-19 crisis (OR: 2.1 [1.3–3.3], P = 0.002).
3.2. Qualitative results
Characteristics of the 14 interviewees are shown in Table 4. These include ETHOS category, the time spent without housing, whether they had been infected or not by COVID-19 prior to the interview, the potential presence of comorbidities and where the interview took place. Participants were aged between 19 and 63 years old at the time of the interview. The majority of respondents were men (11/14).
Table 4.
Characteristics of the qualitative study participants (n = 14).
| Living conditions according to ETHOS typology | Interview's number | Time spent without housing | Prior COVID-19 Infection | Comorbidity | Gender |
|---|---|---|---|---|---|
| ETHOS 1 Sleeping on the street | Ali | 3 months | NO | Medical history of hepatitis | Male |
| Ahmad | 18 months | NO | Severe psychiatric disorders | Male | |
| Saïd | 2 months | NO | Asthma | Male | |
| Paul | 192 months (16 years) | YES | Alcoholic; Smoker; Wound | Male | |
| Florence | 48 months | NO | Asthma | Female | |
| Romain | 180 months (15 years) | NO | Heart disease | Male | |
| ETHOS 2 Sleeping in homeless shelter | Jo | 72 months | NO | None | Male |
| Razzak | 6 months | YES | None | Male | |
| Aziz | 3 months | YES | None | Male | |
| Hassan | 18 months | NO | Dialysis kidney disease | Male | |
| Adrien | 4 months | NO | Asthma | Male | |
| ETHOS 8 Sleeping in slums | Douchka | 120 months (10 years) | NO | Multiple comorbidities | Female |
| Aldo | 24 months | NO | None | Male | |
| Mariska | 24 month | NO | None | Female |
ETHOS: the European typology for homelessness and housing exclusion.
3.2.1. Self-reported compliance with protective measures
3.2.1.1. Structural difficulties in homeless shelters preventing the effective application of protective measures
In shelters, protection resources were made available to the people they accommodated. In addition, the teams of social workers did their best to reorganize shelters, with fewer people than usual, and rearrangement of the time and type of collective activities. The sheltered people were sometimes able to choose to remain isolated in their room or to stay only with the people they were used to seeing.
“Did you manage to get out during lockdown during the day for a bit?
No no all day I stayed in the room.
As a precaution?
To go where ? When we say to stay at home, it is not normal to go out. If you catch him outside and bring him here, it's not good. You have to protect yourself and protect others.
So you really followed all the instructions to the letter?
Yes.” (Hassan, emergency shelters).
Although protective resources were made available, control measures were more difficult to apply, mainly because of the asylum-like architecture of the centres and the concentration of people (almost 300 people living in the emergency accommodation centre where we interviewed participants).
“I caught COVID-19 here. I don't know. I'm very careful. Really careful. I don't share. I do my best. And I got it (…) There are lots of people. I stayed here for a month and then I got it. There are several of us here. We eat in just one room (…) There is no lockdown.
What do you mean?
There are 300 of us here. It's better outside than in.
It's safer outside?
That's right (…)
So here with 300 people, do you think you are protected?
I think that there can't be lockdown with 300 people (…)
Is it possible to stay at a distance here from other people?
That depends on who.
And there are also lots of door handles here.
Yes we see people working, cleaning, but you clean and 5 min later it needs doing again.” (Aziz, emergency shelters).
“How do you think you caught it?
I don't know how I caught it, but one thing's for certain, I caught it here. There are lots of people here and you don't know who's ill, who isn't ill (…) You know being shut in with 300 people!
How did you find being in lockdown with 300 people?
It was OK, I'm not someone who confronts other people. I don't stay with just anybody. I stay with 2, 3 or 4 people. But some people, they know everyone and blah, blah, blah. It's not easy. But 300 people isn't easy. For example, I think that the first time they found 6 people who were positive for Corona. I think they spread the virus to each other. We were all shut in together here! I thought that we would catch it here. That's normal. I took 2 tests that were negative and the last one was positive.” (Razzak, emergency shelters).
The people living in these centres regularly expressed the fact that the close proximity induced by a high concentration of people living together made it more than difficult to apply control measures, especially social distancing.
3.2.1.2. A routine practice on the streets (ETHOS 1) and in slums (ETHOS 8)
Observations differ for people living in streets or in slums. For all of the people from streets and slums met during this study, access to water and hygiene products was a daily struggle. However, relationships with one another, conviviality and proximity were an everyday issue. The following observations were made in this context.
Protective health measures were already in routine practice among the homeless people we met, especially concerning the optimal organisation of everyday health safety (remaining far enough away from others, not getting too close, not drinking from the same bottle, etc.). Some people were used to living with health problems that can quickly deteriorate on the streets (such as wounds), but also with other people who may suffer from infectious diseases (hepatitis, HIV, etc.). Not drinking from the same bottle, not exchanging any everyday items that come into bodily contact (touching the mouth, eyes, potentially infected with blood from small wounds) are common practices.
“Us, on the streets, we're used to staying at a distance. I'm never chummy with other people. I always stay a good metre away from them. He shows me an arm's length. That really avoids violence and the rest. There you go, that's social distancing for me.” (Laurent, sleeping rough).
“Look, our friend has HIV, we know very well that if he cuts himself, or is injured or anything, he doesn't let us touch him, that's good. He keeps us safe anyway (…) [One day, after he got an injured lip] I said to him, listen, look, take a tissue, a wipe, disinfect yourself, don't drink after us or don't drink before us, don't eat using our things and keep on doing that until you get care. And he automatically knows that he's not allowed to touch us or anything else, and we don't touch him. We are safe, because we protect ourselves.
It's true that he stays further apart than you, is that how you organise yourselves?
Yes (…) we don't know if he's got hepatitis or something, he's very ill, that's for sure. But as long as we don't know if he's got hepatitis, we don't drink after him or eat after him. It's not being nasty to him, since we also need to stay safe. Yes OK, there are microbes and everything, but on top of that, if he's ill, we're careful.” (Florence, sleeping rough).
Data collected in the slums revealed particular attention being paid to everyday hygiene conditions (maintenance of living quarters, of common areas, cleaning items that were brought in from outside).
“Is there any water here?
Yes there's water. There are toilets. There's a bit of everything. Everyone washes the floors every day. Three people clean the pavement even outside. Someone else washes the outside dustbins.
Do you do that all the time?
Yes every day, every day. Every day the same things.
I mean did you do that even when there wasn't coronavirus?
It's three people today, three others tomorrow, each bedroom takes turns. It's the same thing for the toilets. One girl cleans in the morning, another at lunchtime and another in the evening. We do that all the time.
How long has this cleaning been going on?
For a very long time. It's been like this for over six months.” (Mariska, slums).
3.2.2. Self-perceived health
3/14 qualitative participants reported prior COVID-19 infection and two thirds (9/14) reported having at least one comorbidity.
Health: a constant concern for the homeless.
On the whole, we observed that the interviewees who were living rough paid particular attention to their health. They were all, as much as possible, very attentive to their health, to their personal hygiene and to the hygiene of the place where they used to live.
“When you see me like this, I'm in the street. I've got a tooth brush, I've got shaving-cream. I've left my suitcases somewhere. I only need a change of clothes. I've got another pair of trousers and a shirt.
You always look immaculate.
Yes. And when I could afford it, I had the same things.” (Ahmad, living rough).
“We always leave the place very clean, we use bin bags and everything, it's spotless, and we've also got a toilet just next door, a private toilet. I can go and have a wash, get changed and everything, but we still keep the surroundings clean (…) Because they said to us, yes you're living without masks anyway, you don't get healthcare here, I said, yes we do, every day there are organisations that come, they take our temperature each time.” (Florence, living rough).
Maintaining or improving existing state of health is primordial, for themselves and even for their animals, if they have any:
“And your animals?
My babies, those are my babies. The Alsatian dog (…), I've got his whole vaccination book and that, see here, at the beginning of the year, he had his last shot, and now we're going to get the little one sterilised and get the other one chipped. That way, we're able to manage all three (…) We make them safe. We just want to protect them like us. (…) We protect them and them, they protect us at night. That way we can sleep just a tiny bit even if we don't sleep for long.” (Florence, sleeping rough).
The vast majority of the interviews revealed that particular attention was paid to the health of others. In other words, they did not focus solely on their own health but also cared for others living in the same place. This observation raises the question of the meaning of collective in this population, and the taking into consideration of the network's solidarity in times of COVID-19 pandemic.
3.2.3. Unmet needs related to health
Concerning the perception of the health hazard due to COVID-19, data showed that homeless people had much more important problems in their lives than the outbreak of this virus. COVID-19 was effectively perceived as being an additional danger but it was directly put into perspective by a regular experience of risk. Maintaining a living place, access to stable and adequate accommodation, access to healthcare, and access to food are subjects often considered to be key priorities for self-preservation, and these health factors were clearly identified by the people concerned. The people we interviewed had regular experience of extremely violent trauma. They brought this trauma up with us to put the risk of COVID-19 into perspective.
“Are you scared of coronavirus?
Oh no, no, me I'm not scared. We drank water in Chad. We took off our helmet took a piece of string and put the helmet into the well to get some water. There was very little water. We put purification tablets in it. We drank the water. It was black, green, blue, any colour. Afterwards we found corpses in it. We found bones, skulls and everything. The companies before us had thrown their dead bodies there. It was Libyans back then.
So you're not afraid of coronavirus!
Oh no, not scared. I picked up heads, feet. God only knows what I've seen. If I told you everything, you wouldn't sleep tonight. I prefer to leave you be, it's better.” (Ahmad, sleeping rough).
Having said that, while the virus is not a major concern, it remains a risk factor for people with comorbidities, especially asthma, morbid obesity, diabetes and high blood pressure.
“So finally are you scared of coronavirus or not?
It's normal to be, it affects your morale. As well as not knowing where I'm going to live and so on, there is Corona. It's two-in-one: coronavirus plus, when I get out of here, where will I go? (…) That's where we are, tomorrow they say “you're leaving” well, you leave. But where to? Outside and lockdown. Two-in-one.
That's what worries you the most?
I'm asthmatic, I'm in danger. And if I get Corona I'll die straight away. Do you understand?” (Saïd, sleeping rough).
For the people who were locked down in emergency shelters, the main concern was finding long-term accommodation. Homeless people can be divided into those who want to live in accommodation, of any type (“Now my priority is to find a room, and get back to work. That's all …“Ali) and those who have lost all hope of finding accommodation fitting their demands, especially with regards to entry criteria for the shelters (i.e., presence of animals, use of psychoactive substances, irregular immigrants, lack of income), the period of allotment which takes too long, or even conditions of hygiene and dignity in certain centres.
“Do you know M. [One of the emergency centres4 in Marseille]?
Yes, I stayed there for two days, I left, it was Baghdad in there (…) They should be ashamed, that shouldn't exist (…) I slept there for one day, I said this isn't possible, there were 5, 6 of us with mattresses everywhere, it's not surprising people are ill. Me, I caught a fungal infection, I caught body lice, fleas, products cost a lot, I hadn't got the money, I had to steal them (…) me I slept with my dog, it was cleaner in the kennels.” (Romain, sleeping rough).
One of the major concerns for people living in slums is preserving their living quarters, being worried about any information concerning a potential eviction in which they would lose their essential goods and resources, demanding considerable effort to replace them.
Today I'm accompanying the teams from the organisations (Médecins du Monde and AMPIL – Humanitarian and social associations in Marseille) on their rounds. The first conversations begin between the interpretors and the inhabitants. Their main concern is a potential eviction from the slums. Field book 24th June 2020.
To note, not all slums and squats in Marseille have the same conditions of installation and organization. In one of the largest squats in the city, two fires broke out within a few weeks apart.
3.2.3.1. Difficulties related to access to primary resources
The severe impact of COVID-19 lockdown on living conditions of the most vulnerable populations.
3.2.3.1.1. Loss of income
For the majority of people interviewed in this study, lockdown was directly associated with loss of employment and therefore loss of a major part of their income.
“I did odd cooking jobs before lockdown. Seeing as everything is shut, we're all out of a job now. Since these jobs were undeclared, well now we're all left with nothing.
Was it lockdown that caused you to stop working?
It stopped dead my job. I was working evenings in a snack bar (…) It shut for lockdown. Now we're out of lockdown, but it's still shut. (…) I went back there yesterday, it's opening again just doing take-away. But he's not employing anyone else because he can manage on his own.” (Ali, sleeping rough).
For others, whose daily income was from begging, lockdown also coincided with a loss of income:
“How was begging during lockdown? Did you get as much?
No, it's got better now in the past week, fortnight, but at the beginning it was really hard.” (Florence, sleeping rough).
For some, lockdown coincided directly with being thrown out on the streets and the start of being homeless.
“You tried to stay with some friends but the friends didn't answer?
They weren't my friends, some people in Algeria told me to go to see these people for help. I went there for 15 days then I had an asthma attack and they were afraid it was coronavirus.
When did they throw you out?
At the beginning of lockdown. Three weeks into lockdown. I spent three days outside then I went to see Médecins Du Monde {Doctor of the World NGO}.” (Saïd, sleeping rough).
This latter interviewee described how lockdown created or worsened insecure living conditions. In addition, lockdown brought to light populations who are invisible in ordinary contexts. Outreach teams discovered new categories of people who, in ordinary times, are not accompanied by social workers. These new homeless service users had different stories to tell according to their living place. For instance, some people living temporarily with family/friends (i.e., living in conventional housing but not the usual or place of residence due to lack of housing, ETHOS 8.1 category) had to leave their insecure accommodation and to daily alternate between public places and emergency shelters. Other people had to leave institutions even during lockdown. Notably, the French Ministry of Justice chose to release people at the end of their prison sentence, i.e. around 13,500 throughout France. Finally, people who managed to stay in housing thanks to undeclared income-generating activities found themselves without any resources and were among the newcomers in the public space (i.e. sleeping rough or needing community aid services).
2.4.2. Difficulties in access to essential resources
Access to food and hygiene products was a major challenge for the most vulnerable people during lockdown. During this period, homeless people received less support from citizens (individuals staying at home, closed stores or restaurants), and the organisation of local social actions was restructured for several weeks. As a consequence, access to everyday consumer products (particularly food assistance and hygiene products) was reduced for the most vulnerable people. However, the situation was not the same for all of the people interviewed. The main differences were due to the solidity of solidarity networks and people's knowledge of food aid distribution networks. For the people who had long abandoned the idea of finding adequate housing and who had therefore settled into a life of homelessness, solidarity networks are solidly established throughout the year, summer and winter alike. Some people who are anchored to being homeless have even set up networks of redistribution of food according to what they can pick up and the people they meet during the day.
“For food, there are the mobile social rounds, sometimes I'll get four bags of food. I redistribute them, every time I see the mobile teams I tell them I'm your redistribution assistant (…) As soon as I see a bloke, who hasn't got much, I say, here, take this, there's some cheese, some other things, some pepper.” (Paul, rough sleeping)
“We also need to eat a bit, people give us things, it's true that there are things we can't eat. But we make other people happy, because we collect it, if there's someone who hasn't got anything, we give it to them, we make them happy and they accept, it suits everyone instead of filling the bins with stuff, we give it to people. There we can pick up brioches, we'll meet a friend or a woman, we'll give it to them, with a child, we'll give it to them. But no, it's OK, we get by.” (Florence, rough sleeping)
It seems as though this population living rough suffered less from lockdown with regards to food compared to their counterparts in slums, even more for allophone populations who have little understanding of the organisation of support services. As for people who had recently become homeless, they had more difficulty getting access to food, as was reported several times during lockdown by the organisations providing support for the most vulnerable.
For certain families living in slums, social and medico-social organisations distributed food vouchers, which enabled them to get essential goods (food, baby hygiene products or female hygiene products, cleaning products in the health context of COVID-19).
“He was able to buy food and nappies for his baby using vouchers. He doesn't get any welfare benefit. It was very difficult for him to find food because of the travel restrictions, the lack of money.” (Aldo, slums), via an interpreter.
To note, and contrary to participants living rough or in slums, people living in homeless shelters had regular access to food and hygiene products in the shelters that remained open.
4. Discussion
This mixed-methods approach study of homeless people living in Marseille, a high-density urban area, set out to analyse describe the self-perceived health and protective measures linked to COVID-19 in this extremely vulnerable population, and to assess which kinds of resources they brought into practice to address the COVID-19 pandemic. The study identified intersections between the quantitative results and the qualitative findings, which both enlighten daily experiences of the COVID-19 outbreak in the context of homelessness.
We found apparently divergent findings in the quantitative and qualitative results regarding the implementation of protective measures against the COVID-19 infection. In the quantitative survey, 88% of people sheltered in collective accommodations reported good compliance in maintaining physical distancing. At the same time, all of the interviewees living in the same collective accommodation highlighted the difficulties to protect themselves from COVID-19 in view of the high density in these accommodations and their asylum organisations: groups forming at different times in the building (coffee, line-ups for the canteen, etc.), physical items in the building being touched permanently (door handles, furniture, common TV rooms). Effectively, we observed statistically higher rates of infection in emergency shelters in our seroprevalence study (Loubière et al., 2021), consistent with other studies in emergency shelters (Dubost et al., 2020; Kirby, 2020). In spite of a good application of barrier measures in emergency shelters, the density and organization of such places do not permit the protection of the people accommodated from COVID-19, as was correctly perceived by interviewees.
In other forms of housing organization, whether makeshift arrangements in public space or squats and slums, the study showed that while people were much more free to choose their contacts (in terms of frequency and levels of proximity, in particular), access to health protection resources was quite insufficient (in particular water and hygiene products). Just as access to water and hygiene products are major elements of public health, an inventory of existing infrastructures must be placed at the centre of attention of public policies in terms of access to healthcare.
Interestingly, our quantitative data extended our qualitative findings by pointing to health as a constant concern for homeless people living rough that may explain the differences regarding compliance with protective measures among participants from different ETHOS categories. In France, a study among 3741 homeless adults living in cities of 20,000 or more inhabitants and attending emergency shelters or food distribution services, reported an estimate of 85% of them having consulted in general practitioner’ offices within the previous 12 months (Moisy, 2015). Over the same period of time, 94% of the general population consulted a doctor during the year (Statista, 2013). To note, these studies did not distinguish between homeless people attending shelters and those living rough. Markedly, self-perceived health (physical and mental) was a determinant associated with healthcare service utilisation, as in other studies (Loubière et al., 2020). As alluded to by Gardella et al. health appears to be an asset to be preserved in order to carry on with projects of integration, or as a level to be reached, the first stepping-stone to “pull through”, i.e. to find a job and accommodation (Gardella et al., 2008, p. 39). And our qualitative findings suggest that the repeated experience of major traumas (such as the biographical factors which led to their lack of individual accommodation or the daily struggle to keep their make-shift housing) contributes to nourishing a survival process, as described by Pichon (Pichon, 1996).
Our qualitative study shows that homeless people maintained maximum self-care practices in unsanitary spaces, and this was particularly true for the interviewees from streets and slums, corroborating previous studies on this subject. Indeed, Leibler and colleagues showed that “hygiene behaviors among people experiencing homelessness likely reflect the availability of sanitation facilities, perception as to the safety or usability of these facilities, as well as personal practices” (Leibler et al., 2017, p. 7). Stolte and Hodgetts described this preserved personal practices, referring to a system of integrated tactics that is enriched daily and that allows homeless people to alter or retexture particular places to better meet their health needs (Stolte & Hodgetts, 2015). Recently, Corburn and colleagues provided an overview of what have been learned from earlier pandemics such as HIV and Ebola outbreaks in slums (Corburn et al., 2020). They reported already observed skills by slum residents in developing innovative ideas about how to improve hygiene and well being following Ebola epidemics. In the current COVID-19 crisis, and despite deterioration in living conditions during lockdown, homeless people have organized their health risk reduction practices as much as possible. The salient points of this study, once this first level of knowledge has been acquired, therefore remains both the provision of protection resources and, at the same time, access to protection resources.
Our study confirms the severe impact of the crisis on financial incomes in this population, whereas prior research indicates that maintaining the little financial income that homeless people possess is a determinant factor in restoring their skills (Toro et al., 1995). The loss of income issue was analysed in the general French population from the first days of lockdown to its end (mid-May 2020) (INSERM, 2020), and results showed that the proportion of people in financial difficulty rose from 11.7% to 14.8% due to lockdown, or even 24.6% if one includes those with a declared bank overdraft. However, after three weeks of lockdown, 34.3% of people in financial difficulty due to lockdown suffered from anxiety-depressive disorders, versus 20% of those who did not have such difficulties. Our quantitative results showed that 77% of the homeless participants reported that they encountered significant financial difficulties during lockdown, with people living rough, in squats or slums being twice more at risk of facing financial difficulties since the COVID-19 outbreak. Our interviewees also acknowledged the impact of lockdown on their financial resources. For example, the collection and sale of iron was one of the most common sources of income in the slums, a non-declared activity that suddenly stopped with lockdown. Distributions of service vouchers were often the only source of income for accessing food and hygiene products for people living rough or in slums/squats. The lockdown of the general population severely impacted the survival systems of the populations furthest from housing, with alarming rates of people without access to water or food.
If the COVID-19 pandemic exacerbated the economic vulnerability of the most insecure populations, we show that there were marked differences between accomodations categories in the levels of difficulty in accessing essential resources. In our quantitative data, participants who had recently become homeless (i.e. < 3 months), and those who had spent more than 5 years homeless, reported more difficulty getting access to food (53% and 56% respectively, compared to 37% and 44% for those with 3–12 months or 1–5 years of being homeless; p < 0.001). This latter proportion increased to 75% of recently homeless participants among the subgroup of people living rough or in slums (ETHOS1 and ETHOS8, respectively). This observation was reported many times during lockdown by the humanitarian organisations providing support for the most vulnerable (Mesa Vieira et al., 2020). One can hypothesize that the issue of understanding the French language would be a determining factor in getting help to find food assistance (Algert et al., 2006; Martin-Fernandez et al., 2018). Among the COVIDHomeless cohort, one half of the people who became homeless recently or people with long periods of homelessness were allophone. Especially for homeless newcomers who faced language barriers, whether or not this was associated with a different culture, solidarity networks were practically non-existent or limited (Bingham et al., 2019).
The small number of interviewees is the main limitation of this study. Saturation for the research question was reached after 14 interviews, and was confirmed by an important observation time and other informal non-transcribed conversations. Participants' experiences of risk and protective measures were more similar in slums due to the importance of the community, than in streets where more interviews were necessary to account for the heterogeneity of the experiences of people living there. Moreover, pathways in housing are much more complex than ETHOS categories, which reflect a situation at a given time, whereas homeless people often move from category to another over time. The ‘permeability’ between homeless types of accommodation, or ETHOS categories is attested by the paths of the interviewees since all of whom had already experienced each of the 3 living conditions (street, emergency shelter, and squat/slum). These periods of homelessness even alternate with times when people are hosted by someone, travel or go to institutions like hospital or jail. Interpretation via ETHOS categories therefore has its limits, even if the study period was peculiar, with less mobility due to the government measures mentioned in the introduction.
The mixed-method approach provides a richer view of our research question and is the main strength of this study. Semi-structured interviews explored in-depth the means of the verbatim to reveal the participant's own voice; while interviewer-administered questionnaires are not able to correctly capture the part of the answer which reflects the participant's own individual practice or self-perception of good practice in such situations (DeJonckheere & Vaughn, 2019). Quantitative analysis of a large number of questionnaires improves the quality of the conclusions, as well as the qualitative researcher's former knowledge of this particular fieldwork.
The capability model seems interesting to use to report our results. According to this framework, capabilities, i.e. the effective freedom to be and to do, correspond to the intersection between the person's internal resources, those that allow him/her to make choices, and the external resources provided by society (Sen, 2010). In our study, everyone's internal health-related resources appeared to be well developed, with an interest, skills and know-how to stay as healthy as possible. However, we found lots of obstacles facing the capabilities of homeless people, depending on their living locations. 1) For people living in slums or on the streets, internal resources found greater latitude to express themselves, and a number of choices remained possible to protect oneself, such as the frequency and level of proximity of contacts, in particular, or making their own makeshift arrangements. On the other hand, at the level of external resources, there was a serious lack of basic goods such as water or food, aggravated by the lockdown and social crisis. 2) For people in emergency shelters, external resources of basic essentials were more often available, but people's choices were more often limited by the organization of the accommodation. We have shown that people in emergency shelters were much more at risk of infection than in the street or slums (Loubière et al., 2020, Loubière et al., 2021), despite sustained attention to compliance with barrier measures. Briefly, none of the places and lifestyles studied were favourable to health. Collective shelters because they restricted people's choices, slums and street life because basic resources were not available.
Other studies have used the capacity framework to address homelessness (e.g. Batterham, 2019; Nicholls, 2010; O’Shaughnessy et al., 2020). All of them described the impact of no longer having a home on many of the 10 central functions described by Nussbaum (Nussbaum, 2012, pp. 55-57). McNaughton Nicholls and O'Shaughnessy even assumed that housing is more than a material resource, and rather a key enabling or constraining force for all the functions required for a “well lived” life (Nicholls, 2010; O’Shaughnessy et al., 2020). By making people stay at home for lockdown, some governments themselves revealed the fact that access to housing is a major social determinant of health.
Far from being reduced to the sole absence of housing (Jouve & Pichon, 2015), homelessness, taken in its complexity, requires very great attention from the public authorities. This study shows that a health risk such as the COVID-19 epidemic can be contextualized, or even relativized, among the risks of homeless life, starting with the lack of real opportunity to access a space, an adapted and secure life. The uncertainty relating to the length of stay in accommodation, the uncertainty relating to the possible eviction from a slum, the uncertainty relating to the possibilities of social support to obtain administrative rights is maintained by the emergency logics with which the public authorities manage the field of social action (Cefaï & Gardella, 2011; Damon, 2002; Jouve & Pichon, 2015).
5. Conclusion
This study contributes to a better understanding of the issues at stake and the experience of the homeless in COVID-19 context. It shows the issues faced by the homeless that were exacerbated by the political health crisis, namely the lack of housing, but also the amount of experience and the capacity of homeless people to adapt to a new health issue. People without housing mobilise, as much as possible, daily practices to stay in decent conditions, but the available resources are not yet sufficient. The current episode shows how the fundamental needs have been previously misjudged, or even disregarded. A better understanding of the most precarious people's needs in a society is one of the constitutive elements of democratic governance. This study raises the question of a sustainable and holistic approach towards the needs of homeless people in a particular health context.
Authorship statement
Category 1:
Conception and design of study: Aurelie Tinland, Sandrine Loubiere, Camille Allaria, Emilie Mosnier.
Acquisition of data: Elisa Monfardini, Camille Allaria.
Analysis and/or interpretation of data: Aurelie Tinland, Sandrine Loubiere, Camille Allaria, Emilie Mosnier.
Category 2:
Drafting the manuscript: Camille Allaria, Aurelie Tinland, Sandrine Loubiere, Emilie Mosnier.
Revising the manuscript critically for important intellectual content: Elisa Monfardini.
Category 3:
Approval of the version of the manuscript to be published: Camille Allaria, Sandrine Loubière, Emilie Mosnier, Elisa Monfardini, Pascal Auquier, Aurelie Tinland.
Funding
This work was supported by the DGOS (PHRC-COVID-19: 20–0047). The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The authors alone are responsible for the findings.
Conflict of interest statement
All authors have nothing to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the ethics committee on May 28, 2020 (number 44–20, ID 2020-AO1398-31). The database was anonymized and declared to the French regulatory commission (Commission Nationale Informatique et Libertés, CNIL, n 2018172 v 0).
Consent to participate
Informed written consent was obtained from all individual participants included in the study.
Consent for publication
Not required.
Data availability
The datasets generated and analysed during the current study are not publicly available due to special authorizations for the transfer of databases given by the CNIL. Upon prior authorization by the CNIL, the dataset would be available from the corresponding author upon reasonable request.
Authors’ contribution
AT, EmiM, PA and SL obtained funding and were involved in initial design of the research. CA, AT, EmiM and EliM contributed to data acquisition. SL did the statistical analysis. CA, AT and SL wrote the first draft of the manuscript. EmiM, EliM and PA contributed to the critically revision steps. All authors approved the final manuscript for publication.
Acknowledgements
Our first acknowledgements go to the study participants, who agreed to join the research.
We would like to express a huge thank you to our coordinator Marine Mosnier, and our interviewers and peer-workers who contributed so energetically to the quantitative data collection: Grace Inegbeze, Huette Snjezana, Nathalie Vuagniaux, Ilyes Hamouda, Carole Reynes, Mathieu Ledu, Lisa Haase, Alejandro Vernet, Matthieu Deschamps, Annie Nguyen, Lina Ndjock, Ahmed Chaïma, Samar Soltani, Razafindramamba Ando, Myriam Soltani.
We would like to thank our partners for their involvement with homeless people:
ASSAb network: Cyril Farnarier
Homeless outreach teams: ADDAP13, AMPIL, ASUD, Bus 31/32, Equipe Mobile d’Aide (EMA) Saralogisol, Equipe Mobile santé ADJ Marceau, Equipe Mobile Gare et Connexion ADJ Marceau, MARSS-APHM, Nouvelle Aube, Mission Bidonville Médecins du monde, PASS adulte APHM, Réseau Santé Marseille Sud (RSMS).
Emergency shelters: UHU La Madrague-ville, St Louis, Sleep'in (groupe SOS Solidarité), Forbin (Fondation St Jean de Dieu), Marius Macias (AAJT).
We also thank Justine Buand who did the hard work of translating this paper into English.
We are very grateful to our funders the French Directorate of Health care facilities (DGOS) – research grant PHRC COVID-19 (COVID-homeless-0047) for their trust and confidence.
Finally, nothing would have been possible without our sponsors: APHM Marseille Public Hospital (Emilie Garrido, Jean Dhorne), and Médecins Du Monde - Doctors of the World (Thomas Bosetti, Guillaume Debrie, Cristina Thevenot, Juan-Diego Poveda), and we thank them warmly for their support.
Footnotes
Winter eviction ban’ is a period of year during which evictions are suspended by French law. This period usually runs from November to March.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100829.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Algert S.J., Reibel M., Renvall M.J. Barriers to participation in the food stamp program among food pantry clients in Los Angeles. American Journal of Public Health. 2006;96:807–809. doi: 10.2105/AJPH.2005.066977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amore K., Baker M., Howden-Chapman P. The ETHOS definition and classification of homelessness: An analysis. European Journal of Homelessness. 2011;5 [Google Scholar]
- Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health jech. 2020;74(11):964–968. doi: 10.1136/jech-2020-214401. 2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham D. Homelessness as capability deprivation: A conceptual model. Housing, Theory and Society. 2019;36:274–297. doi: 10.1080/14036096.2018.1481142. [DOI] [Google Scholar]
- Bello-Chavolla O.Y., González-Díaz A., Antonio-Villa N.E., Fermín-Martínez C.A., Márquez-Salinas A., Vargas-Vázquez A.…Gutiérrez-Robledo L.M. Unequal impact of structural health determinants and comorbidity on COVID-19 severity and lethality in older Mexican adults: Considerations beyond chronological aging. J Gerontol A Biol Sci Med Sci. 2020;76(3):e52–e59. doi: 10.1093/gerona/glaa163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham B., Moniruzzaman A., Patterson M., Distasio J., Sareen J., O'Neil J., Somers J.M. Indigenous and non-indigenous people experiencing homelessness and mental illness in two Canadian cities: A retrospective analysis and implications for culturally informed action. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-024748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cefaï D., Gardella E. La Découverte; Paris: 2011. L’urgence sociale en action: Ethnographie du Samusocial de Paris, bibliothèque du MAUSS. [Google Scholar]
- Corburn J., Vlahov D., Mberu B., Riley L., Caiaffa W.T., Rashid S.F., Ko A., Patel S., Jukur S., Martínez-Herrera E., Jayasinghe S., Agarwal S., Nguendo-Yongsi B., Weru J., Ouma S., Edmundo K., Oni T., Ayad H. Slum health: Arresting COVID-19 and improving well-being in urban informal settlements. Journal of Urban Health. 2020;97:348–357. doi: 10.1007/s11524-020-00438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damon J. Presses universitaires de France; Paris, France: 2002. La question SDF. Critique d’une action publique. Le lien social. [Google Scholar]
- DeJonckheere M., Vaughn L.M. Semistructured interviewing in primary care research: A balance of relationship and rigour. Fam Med Com Health. 2019;7 doi: 10.1136/fmch-2018-000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubost C.-L., Pollak C., Rey S. Les dossiers de la DREES; 2020. Les inégalités sociales face à l’épidémie de Covid-19. [Google Scholar]
- Gardella E., Laporte A., Le Méner E. Entre signification et injonction. Pour un travail sur le sens du recours aux soins des sans-abri. Sciences Sociales et Santé. 2008;26:35–46. doi: 10.3406/sosan.2008.1895. [DOI] [Google Scholar]
- Holmes L., Enwere M., Williams J., Ogundele B., Chavan P., Piccoli T., Chinaka C., Comeaux C., Pelaez L., Okundaye O., Stalnaker L., Kalle F., Deepika K., Philipcien G., Poleon M., Ogungbade G., Elmi H., John V., Dabney K.W. Black–white risk differentials in COVID-19 (SARS-COV2) transmission, mortality and case fatality in the United States: Translational epidemiologic perspective and challenges. International Journal of Environmental Research and Public Health. 2020;17 doi: 10.3390/ijerph17124322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- INSEE . 2020. Dossier complet commune de Marseille (13055.https://www.insee.fr/fr/statistiques/2011101?geo=COM-13055 [WWW Document]. URL. [Google Scholar]
- INSERM . 2020. Chômage et difficultés financières ont fragilisé la santé mentale durant le confinement.https://www.inserm.fr/actualites-et-evenements/actualites/chomage-et-difficultes-financieres-ont-fragilise-sante-mentale-durant-confinement [WWW Document]. www.inserm.fr. URL. [Google Scholar]
- Johnson G.A., Vindrola-Padros C. Rapid qualitative research methods during complex health emergencies: A systematic review of the literature. Social Science & Medicine. 2017;189:63–75. doi: 10.1016/j.socscimed.2017.07.029. [DOI] [PubMed] [Google Scholar]
- Jouve É., Pichon P. Le chez-soi, le soi, le soin. L’expérience limite des personnes sans domicile fixe comme modèle de compréhension de la vulnérabilité sanitaire. Les Annales de la Recherche Urbaine. 2015;110:46–55. doi: 10.3406/aru.2015.3166. [DOI] [Google Scholar]
- Kirby T. 2020. Efforts escalate to protect homeless people from COVID-19 in UK. The Lancet Respiratory Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibler J.H., Nguyen D.D., León C., Gaeta J.M., Perez D. Personal hygiene practices among urban homeless persons in boston, MA. International Journal of Environmental Research and Public Health. 2017;14 doi: 10.3390/ijerph14080928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loubière S., Monfardini E., Allaria C., Mosnier M., Allibert A., Ninove L.…Tinland A. Seroprevalence of SARS-CoV-2 Antibodies Among Homeless People Living Rough, in Shelters and Squats: A Large Population-Based Study in France. Preprints. 2021:2021050766. doi: 10.20944/preprints202105.0766.v1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loubière S., Taylor O., Tinland A., Vargas-Moniz M., O’Shaughnessy B., Bokszczanin A.…Auquier P. Europeans’ willingness to pay for ending homelessness: A contingent valuation study. Social Science & Medicine. 2020;112802 doi: 10.1016/j.socscimed.2020.112802. [DOI] [PubMed] [Google Scholar]
- Martin-Fernandez J., Lioret S., Vuillermoz C., Chauvin P., Vandentorren S. Food insecurity in homeless families in the paris region (France): Results from the ENFAMS survey. International Journal of Environmental Research and Public Health. 2018;15 doi: 10.3390/ijerph15030420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxmen A. Coronavirus is spreading under the radar in US homeless shelters. Nature. 2020;581:129–130. doi: 10.1038/d41586-020-01389-3. [DOI] [PubMed] [Google Scholar]
- Mesa Vieira C., Franco O.H., Gómez Restrepo C., Abel T. COVID-19: The forgotten priorities of the pandemic. Maturitas. 2020;136:38–41. doi: 10.1016/j.maturitas.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moisy M. La santé et le recours aux soins des personnes sans domicile en France en 2012. BEH. Bulletin Epidemiologique Hebdomadaire. 2015:662–670. [Google Scholar]
- Nicholls C.M. Housing, homelessness and capabilities. Housing, Theory and Society. 2010;27:23–41. doi: 10.1080/14036090902764588. [DOI] [Google Scholar]
- Nussbaum M. 2012. Capabilités : Comment créer les conditions d’un monde plus juste ? Flammarion. [Google Scholar]
- O’ Shaughnessy B.R., Manning R.M., Greenwood R.M., Vargas-Moniz M.J., Loubière S., Spinnewijn F., Gaboardi M., Wolf J.R., Bokszczanin A., Bernad R., Blid M., Ornelas J., The HOME-EU consortium study group home as a base for a well-lived life: Comparing the capabilities of homeless service users in housing first and the staircase of transition in Europe. Housing, Theory and Society. 2020;1–22 doi: 10.1080/14036096.2020.1762725. [DOI] [Google Scholar]
- Pichon P. Survivre la nuit et le jour. La préservation de soi face au circuit d’assistance. Polix. 1996;9:164–179. doi: 10.3406/polix.1996.1037. [DOI] [Google Scholar]
- Poremski D., Distasio J., Hwang S.W., Latimer E. Employment and income of people who experience mental illness and homelessness in a large Canadian sample. Canadian Journal of Psychiatry. 2015;60:379–385. doi: 10.1177/070674371506000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen A. Flammarion; Paris: 2010. L’idée de justice. [Google Scholar]
- Statista . 2013. Visites chez le généraliste par an France.https://fr.statista.com/statistiques/535570/frequence-anuelle-de-consultation-medecin-generaliste-france/ [WWW Document], URL. [Google Scholar]
- Stolte O., Hodgetts D. Being healthy in unhealthy places: Health tactics in a homeless lifeworld. Journal of Health Psychology. 2015;20:144–153. doi: 10.1177/1359105313500246. [DOI] [PubMed] [Google Scholar]
- Toro P.A., Bellavia C.W., Daeschler C.V., Owens B.J., Wall D.D., Passero J.M., Thomas D.M. Distinguishing homelessness from poverty: A comparative study. Journal of Consulting and Clinical Psychology. 1995;63:280–289. doi: 10.1037/0022-006X.63.2.280. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analysed during the current study are not publicly available due to special authorizations for the transfer of databases given by the CNIL. Upon prior authorization by the CNIL, the dataset would be available from the corresponding author upon reasonable request.