Abstract
Background
The use of a mesh in primary ventral or incisional hernia repair lowers the recurrence rate and is the accepted standard of care for larger defects. In laparoscopic primary ventral or incisional hernia repair the insertion of a mesh is indispensable. Different mesh fixation techniques have been used and refined over the years. The type of fixation technique is claimed to have a major impact on recurrence rates, chronic pain, health‐related quality of life (HRQOL) and complication rates.
Objectives
To determine the impact of different mesh fixation techniques for primary and incisional ventral hernia repair on hernia recurrence, chronic pain, HRQOL and complications.
Search methods
On 2 October 2020 we searched CENTRAL, MEDLINE (Ovid MEDLINE(R)) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)), Ovid Embase, and two trials registries. We also performed handsearches, and contacted experts from the European Hernia Society (EHS).
Selection criteria
We included randomised controlled trials (RCTs) including adults with primary ventral or incisional hernia that compared different types of mesh fixation techniques (absorbable/nonabsorbable sutures, absorbable/nonabsorbable tacks, fibrin glue, and combinations of these techniques).
Data collection and analysis
We extracted data in standardised piloted tables, or if necessary, directly into Review Manager 5. We assessed risks of bias with the Cochrane 'Risk of bias' tool. Two review authors independently selected the publications, and extracted data on results. We calculated risk ratios (RRs) for binary outcomes and mean differences (MDs) for continuous outcomes. For pooling we used an inverse‐variance random‐effects meta‐analysis or the Peto method in the case of rare events. We prepared GRADE 'Summary of findings' tables.
For laparoscopic repair we considered absorbable tacks compared to nonabsorbable tacks, and nonabsorbable tacks compared to nonabsorbable sutures as key comparisons.
Main results
We included 10 trials with a total of 787 participants. The number of randomised participants ranged from 40 to 199 per comparison. Eight studies included participants with both primary and incisional ventral hernia. One study included only participants with umbilical hernia, and another only participants with incisional hernia. Hernia size varied between studies.
We judged the risk of bias as moderate to high.
Absorbable tacks compared to nonabsorbable tacks
Recurrence rates in the groups were similar (RR 0.74, 95% confidence interval (CI) 0.17 to 3.22; 2 studies, 101 participants). It is uncertain whether there is a difference between absorbable tacks and nonabsorbable tacks in recurrence because the certainty of evidence was very low. Evidence suggests that the difference between groups in early postoperative, late follow‐up, chronic pain and HRQOL is negligible.
Nonabsorbable tacks compared to nonabsorbablesutures
At six months there was one recurrence in each group (RR 1.00, 95% CI 0.07 to 14.79; 1 study, 36 participants). It is uncertain whether there is a difference between nonabsorbable tacks and nonabsorbable sutures in recurrence because the certainty of evidence was very low. Evidence suggests that the difference between groups in early postoperative, late follow‐up and chronic pain is negligible. We found no study that assessed HRQOL.
Absorbable tacks compared toabsorbable sutures
No recurrence was observed at one year (very low certainty of evidence). Early postoperative pain was higher in the tacks group (VAS 0 ‐ 10: MD −2.70, 95% CI −6.67 to 1.27; 1 study, 48 participants). It is uncertain whether there is a difference between absorbable tacks compared to absorbable sutures in early postoperative pain because the certainty of evidence was very low. The MD for late follow‐up pain was −0.30 (95% CI −0.74 to 0.14; 1 study, 48 participants). We found no study that assessed HRQOL.
Combination of different fixation types (tacks and sutures) or materials (absorbable and nonabsorbable)
There were mostly negligible or only small differences between combinations (e.g. tacks plus sutures) compared to a single technique (e.g. sutures only), as well as combinations compared to other combinations (e.g. absorbable sutures combined with nonabsorbable sutures compared to absorbable tacks combined with nonabsorbable tacks) in all outcomes. It is uncertain whether there is an advantage for combining different fixation types or materials for recurrence, chronic pain, HRQOL and complications, because the evidence certainty was very low or low, or we found no study on important outcomes.
Nonabsorbable tacks compared to fibrin sealant
The two studies showed different directions of effects: one showed higher rates for nonabsorbable tacks, and the other showed higher rates for fibrin sealant. Low‐certainty evidence suggests that the difference between groups in early postoperative, late follow‐up, chronic pain and HRQOL is negligible.
Absorbable tacks compared to fibrin sealant
One recurrence in the tacks group and none in the fibrin sealant group were noted after one year (low certainty of evidence). Early postoperative pain might be slightly lower using tacks (VAS 0 ‐ 100; MD −12.40, 95% CI −27.60 to, 2.80;1 study, 50 participants; low‐certainty evidence). The pattern of pain and HRQOL course over time (up to 1 year) was similar in the groups (low certainty of evidence).
Authors' conclusions
Currently none of the techniques can be considered superior to any other, because the certainty of evidence was low or very low for all outcomes.
Plain language summary
Mesh fixation techniques in ventral hernias
Review question
What are the benefits and harms of different techniques for fixing meshes (patches) in the belly wall in the course of ventral hernia repair.
Background
A hernia is a bulge or weakness, in which tissues or organs from inside the abdomen (the belly) can get trapped, and can cause discomfort and symptoms such as pain. The size of the hernia can be made worse by daily living activities, especially by coughing and straining. Hernias carry a risk of incarceration ( a hernia so occluded that it cannot be returned by manipulation)) and strangulation (when the circulation of blood has been cut off), which is a threat especially in incisional and umbilical hernias (navel area). An incisional hernia is a hernia that occurs through a previously‐made incision in the abdominal wall, i.e. the scar left from a previous surgical operation. The incision could have been made in order to get to an internal organ such as the appendix, or a caesarian section.
Repair of a ventral (abdominal wall) hernia is done by surgery. The choice of the right surgical procedure will depend on different criteria, like size of the hernia, previous surgery, location of the hernia and general health. There are two types of surgery: Open surgery, where the hernia is closed by sewing the layers of the abdominal wall. Often, the surgeon places an additional mesh on a layer of the abdominal wall, which makes a recurrence of the hernia less likely. The other type is called laparoscopic surgery, where the surgeon makes a few small incisions and inserts tiny long instruments and a camera into the abdomen. For the laparoscopic repair of the hernia, a mesh has to be used in every patient.
Different techniques are used to fix the mesh to the abdominal wall in ventral hernia repair. However, the advantages and disadvantages of these techniques are not yet clear. We reviewed the evidence of different fixation techniques for their effect on recurrence, pain, complications and health‐related quality of life in people with a ventral hernia.
Search date
The evidence is current to 2 October 2020.
Study characteristics
We included 10 studies involving 787 persons, with ages ranging from 31 to 62 years. Eight studies included people with primary as well as incisional ventral hernia, one study included people with umbilical (navel area) hernia only, and another study with incisional hernia only. Hernia size varied widely between studies. The number of included participants ranged from 40 to 199. Participant follow‐up was mostly short (less than 12 months).
Key results
The differences between the fixation techniques were small for our analysed outcomes. We could not find any difference between the use of tacks compared to sutures (stitches), the use of absorbable tacks compared to nonabsorbable tacks, the use of absorbable tacks compared to absorbable sutures and the use of fibrin sealant compared to tacks. In addition, the combination of fixation techniques (sutures and tacks) or materials (absorbable and nonabsorbable) showed no advantage for recurrence, pain or other complications.
Certainty of evidence
The certainty of evidence for the main outcomes of recurrence and pain, as well as for complications, was very low or low. The main reason for this was a lack of sufficient data, due to the small number of included participants, and the small number of hernia recurrences. Furthermore, almost all studies were at moderate to high risk of bias, as the healthcare professionals involved were unblinded, i.e. aware of the interventions their patients received.
Summary of findings
Background
Ventral hernia repair is a frequent procedure in abdominal surgery (Dabbas 2011). There are many different surgical options to repair ventral hernias, including mesh or suture repair, different mesh positions, different mesh types, surgical approach (laparoscopic or open repair) and mesh fixation techniques. A systematic review of randomised trials has shown that the high recurrence rate after open suture repair of up to 54% (Paul 1998; Luijendijk 2000) can be significantly lowered by using a mesh (Mathes 2016). In laparoscopic hernia repair the insertion of a mesh is indispensable. There are two types of mesh used in ventral hernia repair: synthetic and biologic (or bioabsorbable) mesh. Using synthetic mesh is the standard of care as recommended by guidelines (Bittner 2019). The use of biologic meshes is mostly restricted to a contaminated/infected field of surgery (Bittner 2019). Different techniques for fixing the mesh in to the abdominal wall may lead to different recurrence rates, pain intensity and complication rates.
Description of the condition
A ventral hernia is the protrusion of organs or tissue in the anterior abdominal wall that occurs spontaneously or at the site of a previous surgical incision.
Ventral hernias are classified according to their location and aetiology (Muysoms 2009). A primary ventral hernia is the protrusion of organs or tissue through a defect or opening in the abdominal wall that has occurred spontaneously without prior surgery (Kingsnorth 2003; Sauerland 2011; Rogmark 2013). As defined by Muysoms 2009, ventral hernias only include hernias of the anterior abdominal wall. Depending on the location, a primary ventral hernia is classified as a (para‐)umbilical (surrounding the navel), epigastric (upper central region of the abdomen) or spigelian hernia (between the muscles of the abdominal wall). Incisional hernias develop at the site of a previous surgical incision of the abdominal wall, and occur in up to 20% of abdominal surgeries (Misra 2006; Abdel‐Baki 2007; Ceccarelli 2008; Hollinsky 2010; Itani 2010; Kaafarani 2010; Venclauskas 2010).
Ventral hernias can cause pain and cosmetic concern. Symptoms such as pain and the size of the protruding bulge can be influenced by activities of daily living, in particular by coughing and straining. Hernias carry a risk of incarceration (e.g. constriction of intestine or omentum) and strangulation (when the circulation of blood has been cut off), which is a threat especially in incisional and umbilical hernias. Surgical repair is therefore recommended for symptomatic ventral hernias.
When hernias are surgically repaired a mesh can be used to support the repair and to reduce tension on the abdominal wall. In open surgical repair of primary or incisional ventral hernias a mesh can be placed using the onlay, sublay or inlay technique. Both the onlay and sublay positioning of the mesh are techniques that reinforce the abdominal wall in addition to the surgical closure of the defect. In the onlay technique, the mesh is positioned between the subcutaneous tissues of the abdominal wall and the anterior rectus sheath. In the sublay technique, the mesh is positioned below the rectus muscle, either between the posterior rectus sheath and the rectus muscle (subfascial) or above the peritoneum between the peritoneum and posterior rectus sheath or muscle (preperitoneal). In the inlay technique the mesh is placed between the edges of the fascia (the layer of abdominal fibrous tissue in which the defect (gap) is located). This technique does not close the defect. Instead, the mesh is sutured to the edges of the defect to bridge the gap. In laparoscopic repair the mesh is inserted intra‐abdominally and fixed to the peritoneum. This is known as intraperitoneal onlay mesh (IPOM) (LeBlanc 1993; Welty 2001; Klinge 2005; LeBlanc 2007; Den Hartog 2008; Sauerland 2011). It is important to use an appropriately‐sized mesh that overlaps the hernia gap by at least four to five centimetres (LeBlanc 2004; Klinge 2005). There are different kinds of mesh material available (DeMaria 2000; Bellows 2013).
Description of the intervention
Many techniques have been developed for fixing the mesh to the abdominal wall. The literature describes the use of tacks (nonabsorbable or absorbable), fibrin glue and sutures (nonabsorbable or absorbable) (Ceccarelli 2008; Bansal 2011).
In the open onlay technique, the mesh overlies the repair and is commonly fixed with sutures. The open sublay repair is typically performed by placing the mesh above the sutured peritoneum or posterior rectus sheath (posterior to the rectus muscle). The mesh is then secured with a few interrupted sutures (absorbable or non‐absorbable) and the anterior rectus sheath is closed above the mesh. The inlay technique is only justified in cases where the defect between the edges of the fascia cannot be closed even after the application of advanced techniques like component separation, and is therefore rarely performed. In this technique the mesh is sutured to the edges of the defect to bridge the gap.
In the laparoscopic (intra‐abdominal) ventral hernia repair the mesh is typically fixed with an outer and inner row of intra‐abdominally placed tacks (absorbable or non‐absorbable). In addition to the tacks and sometimes also instead of tacks, transfacial suture fixation (absorbable or nonabsorbable) can be used to secure the mesh position. There are divergent opinions about whether fascial defects should be closed before placing the mesh in laparoscopically‐performed ventral hernia repair.
How the intervention might work
The different types of mesh fixation techniques, e.g. sutures, tacks or fibrin glue, hold the mesh in place (Eriksen 2007; Ceccarelli 2008; Beldi 2011; Eriksen 2011) and thus contribute to the stability of the mesh. The mesh fixation technique can therefore directly affect the risk of hernia recurrence, as well as patient‐related outcomes (e.g. pain) (Nguyen 2008).
Why it is important to do this review
The different fixation techniques are still debated in the surgical community, and a standard procedure has not yet been established (Wassenaar 2008; Wassenaar 2010). The fixation technique can influence the development of recurrence and chronic pain (Carbonell 2003; Heniford 2003; LeBlanc 2004; Chelala 2007; Wassenaar 2010) and consequently can impair the person's quality of life. There is no up‐to‐date systematic review on fixation methods in primary and incisional ventral hernia repair.
Objectives
To determine the impact of different mesh fixation techniques for primary and incisional ventral hernia repair on hernia recurrence, chronic pain, HRQOL and complications.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) without any language restriction and irrespective of their publication status. We excluded RCTs that only compared a different fixation technique in combination with another mesh type within one treatment arm. We planed to include cluster‐randomised trials.
Types of participants
We included trials in adults (aged 18 years and above) suffering from primary or incisional ventral hernias. We also included people with recurrent hernias. We excluded trials in participants with inguinal hernias.
Types of interventions
We included trials that compared different types of mesh fixation techniques (sutures, tacks or fibrin glue), irrespective of the type of mesh material, positioning of mesh (onlay, sublay, etc.) or surgical access (laparoscopic or open). In cases where more than one fixation method was used in one intervention arm (e.g. sutures and glue), we considered this as a separate technique.
Types of outcome measures
Primary outcomes
Recurrence, diagnosed by a physician or radiologically; we included trials irrespective of the method used for diagnosis or the length of follow‐up.
-
Pain, classified as:
Early postoperative (0 to 14 days postoperatively)
Late follow‐up (15 days to 6 weeks postoperatively)
Chronic (more than 6 to 8 weeks postoperatively) (LeBlanc 2004; Den Hartog 2008).
We accepted pain measures based on a visual analogue scale (VAS) or a numeric rating scale (NRS) measurement, irrespective of the scaling (e.g. zero to 10 or zero to 100) (Breivik 2008). Other types of pain measures were not eligible.
Health‐related quality of life (HRQOL): measured with the Short Form Health Surveys (SF) (SF 2014) or the EuroQol (EQ‐5D) instruments (EQ‐5D 2014) in the early postoperative period (0 to 14 days) or long‐term (at least 6 weeks).
Secondary outcomes
The following secondary outcomes were analysed:
time until return to normal activity (days)
length of hospital stay (total or postoperative) (days)
duration of surgery (minutes)
re‐operation at the same site of hernia repair within three years
local seroma or haematoma (as defined in the primary studies)
local infection (with or without mesh infection)
other early and late intervention‐related complications
Search methods for identification of studies
Electronic searches
We conducted a comprehensive literature search to identify all published and unpublished RCTs with no restrictions by language or by publication status. We searched the following databases to identify eligible studies (last updated 2 October 2020):
Cochrane Colorectal Cancer Group Controlled Trials Register;
the Cochrane Central Register of Controlled Trials (CENTRAL, 2 October 2020) (Appendix 1);
Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to 2 October 2020 (Appendix 2);
Ovid Embase 1974 to 2 October 2020 (Appendix 3).
We also searched the following Internet sources (trial registries) (2 October 2020):
www.who.int/ictrp/en/ (World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP)).
The use of mesh was introduced in the 1990s for ventral hernia repair, but the exact date is unknown. We therefore did not limit the date of publication.
Searching other resources
We handsearched for additional trials by:
cross‐checking the reference lists of all included primary studies;
cross‐checking the reference lists of relevant systematic reviews, which were either known to us (Sauerland 2011; Bellows 2013), or identified during literature search (Mathes 2016; Sajid 2013).
We handsearched available abstracts (from 1996 to 2015) from conference reports of the:
International Congress of the European Hernia Society (EHS);
Congress of the European Association of Endoscopic Surgery (EAES);
Annual meeting of the American Hernia Society (AHS).
We searched the following journals for relevant abstracts until 01 March 2017:
Hernia;
Surgical Endoscopy;
British Journal of Surgery;
Journal of the American College of Surgeons;
World Journal of Surgery.
We contacted experts in the European Hernia society (EHS) to request information about unpublished or ongoing trials.
Data collection and analysis
Selection of studies
Two review authors (MW or BP and TM) independently screened the titles and abstracts of all identified articles. We retrieved the full texts of all possibly relevant articles. We reviewed full‐text articles in detail against the inclusion criteria. In the case of discrepancies we determined eligibility by discussion.
Data extraction and management
We extracted all data using a standardised, previously‐piloted data extraction form, or entered the data directly into Review Manager 5 (RevMan 2020). Participants and study characteristics were extracted by one review author and verified by a second (from MW, BP, TM). The clinical expert (RS) checked all descriptions of the intervention. One review author (TM) performed data extraction of outcomes, and entered the data directly into Revman. Another review author entered the outcome data into a standardised Word table (MW, BP). The data were subsequently compared, with necessary changes performed directly in Revman. We again verified the accuracy of the final entries in Revman against the included publications (MW, BP), discussing discrepancies until we reached consensus. If we had irresolvable differences we consulted a third review author (RS).
We extracted the following data:
study information (first author and date of publication);
study design;
location (country, institution);
dates the study was conducted;
number of participants included in study (n);
inclusion and exclusion criteria;
demographics (age, gender, body mass index, hernia type, co‐morbidity);
details of included hernias (type, size, recurrence);
descriptions of the intervention (e.g. open or laparoscopic, location of the mesh, type of mesh, type of mesh fixation technique);
descriptions of the control intervention;
descriptions of concomitant therapies (e.g. pain medication, drains);
outcomes;
complications;
funding source and conflict of interests.
Assessment of risk of bias in included studies
Two review authors (MW or BP and TM) independently assessed the risks of bias of all included studies, resolving disagreements through discussion. In the case of unresolvable discrepancies we consulted a third review author (RS). We used the Cochrane 'Risk of bias' tool, in Chapter 8.5 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), to evaluate the included studies for risk of bias in the following domains: generation of randomisation sequence, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of outcome data, selective reporting, other potential bias, and a priori definitions of outcome measures. We present the criteria for judging low, high or uncertain risk of bias in Appendix 4. We assessed risk of bias at outcome level, where the assessment might differ (detection bias, attrition bias).
Measures of treatment effect
We calculated risk ratios (RRs) for binary outcomes (incidence of recurrence, re‐operation, seroma/haematoma, infection, complications, incidence of chronic pain) and mean differences (MDs) for continuous outcomes (pain VAS scores, time to normal activity, duration of surgery and hospital stay, quality of life scores). We calculated 95% confidence intervals (CIs) for all effect measures.
Unit of analysis issues
We considered only one treatment per person, even if more than one hernia per person was reported. In practice, individuals with two or more hernias of the abdominal wall are usually treated with one mesh and therefore only one fixation technique. Our analysis was therefore based on the number of individuals, not the number of hernias. We separated multi‐arm studies into different comparisons.
Dealing with missing data
We performed two types of analyses: a completer analyses on all outcomes and, where possible, additional intention‐to‐treat (ITT) sensitivity analyses for hernia recurrence.
Our primary analysis was a completer analysis, i.e. we did not impute any missing outcome data. Where this information (e.g. the number of analysed participants) was not available or only imputed data of an ITT analysis were reported, we contacted the trial authors and requested the necessary data for a completer analysis. If the study authors did not provide the necessary data for a completer analysis, we used the available data (e.g. imputed data for the ITT analysis).
If the number of randomised participants who received the intervention and were lost to follow‐up (or completer) were reported for each study arm, we performed a supplementary ITT sensitivity analysis based on 'best case' and 'worst case' scenarios, to test the robustness of the results. The ‘best case’ scenario assumes that all those lost to follow‐up in the experimental group did not have a recurrence, while all those lost to follow‐up in the control group are assumed to have had a recurrence; the ‘worst case’ scenario is the inverse assumption (Higgins 2011).
Assessment of heterogeneity
Since the surgical procedures might vary from centre to centre and from surgeon to surgeon, we anticipated the presence of some clinical heterogeneity. We therefor used a random‐effects model for statistical pooling of the study outcomes. We calculated the I2 statistic in order to quantify statistical heterogeneity (Higgins 2002; Higgins 2003). Our interpretation of I2 was guided by the Cochrane Handbook for Systematic Reviews of Interventions (10.10.2; Deeks 2021) as follows: 0% to 40% might not be important, 30% to 60% may represent moderate statistical heterogeneity, 50% to 90% may represent substantial statistical heterogeneity, and 75% to 100% represents considerable statistical heterogeneity.
Assessment of reporting biases
We had planned to prepare funnel plots for all comparisons that included at least 10 studies and to analyse the cause for any asymmetries (e.g. publication bias, selective outcome reporting, true heterogeneity). This review only includes 10 trials. Consequently, we did not prepare or present any funnel plots. We searched for the study protocols of each included trial to compare the planned outcomes with those reported.
Data synthesis
We performed meta‐analyses to pool outcome estimates of the included trials. We only pooled data for the same outcome measure and similar durations of follow‐up. For dichotomous outcomes we calculated pooled RRs with 95% CIs using the standard inverse variance random‐effects model (DerSimonian Laird heterogeneity variance estimator based on Mantel‐Haenszel fixed‐effect model). For rare events (fewer than 1%) we used the Peto odds ratio (POR) instead. We pooled mean difference of continuous outcomes also using the standard inverse‐variance random‐effects model specified above.
Subgroup analysis and investigation of heterogeneity
We had planned where possible to analyse subgroup effects by the following predefined variables:
type of hernia: primary or incisional;
positioning of mesh: onlay, sublay, inlay or IPOM;
surgical technique: laparoscopic or open;
size of hernia: small (< 5 cm in diameter) or large (≥ 5 cm in diameter);
type of mesh: synthetic or biological;
different fixation materials (e.g. absorbable compared to non‐absorbable sutures/tacks or different fibrin glues).
We did not perform a subgroup analysis for assessing consistency of intervention effects across studies because we did not identify a sufficient number of trials.
Sensitivity analysis
We had planned to perform a sensitivity analysis to determine the impact of the following variables:
risk of bias: including only studies with low risk of bias (we judged all 'Risk of bias' items to be low risk).
In this review we did not identify and include a sufficient number of trials in our meta‐analyses to perform this sensitivity analysis for assessing the consistency and robustness of results. We will consider this in future updates.
Summary of findings and assessment of the certainty of the evidence
We prepared 'Summary of findings' tables using the GRADE approach and the GRADEpro software to rate the certainty of evidence for recurrence, early postoperative pain, chronic pain, HRQOL (one month or more after surgery) and complications (Guyatt 2011).
Comparator‐group risks were derived from the comparator groups of the included studies. We expressed the comparator‐group risk per 1000, unless there was only one event in the comparator‐group study arm(s). In that case, we used the original number of comparator‐group participants because approximations to 1000 participants would tend to an overestimation of the risk.
One review author performed the GRADE assessment and a second verified the judgements.
Results
Description of studies
Results of the search
The search of electronic databases and the additional sources resulted in 1331 hits, after removing duplicates. After title/abstract screening, we retrieved 22 full‐text articles for detailed evaluation against the inclusion criteria. Ten RCTs (12 publications) satisfied all inclusion criteria and are included in the review (Bansal 2012; Wassenaar 2010; Beldi 2011; Eriksen 2011; Muysoms 2013; Colak 2015; Bansal 2016; Harsløf 2018; Shaukat 2018; Langenbach 2020). As expected, we found no cluster‐RCTs. For two studies there was more than one publication available, but we used only data from one publication for each (Eriksen 2011; Bansal 2012). The process of study selection is illustrated in a PRISMA flow diagram (Figure 1). The search of additional sources revealed no further relevant trials.
1.
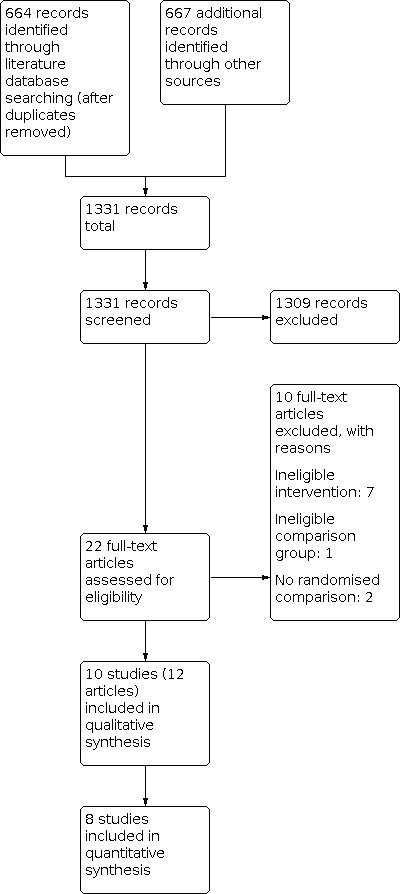
Study flow diagram.
Included studies
Participants
The sample size of all studies was small (range of randomised participants 40 to 199). In all studies the participants were middle‐aged, ranging (median or mean) between 31 and 62 years. The mean body mass index (BMI) was between 25 and 42 kg/m2. Eight studies included participants with primary as well as incisional ventral hernia (Bansal 2012; Wassenaar 2010; Beldi 2011; Muysoms 2013; Bansal 2016; Harsløf 2018; Shaukat 2018; Langenbach 2020). In all but two studies hernias were mostly incisional. One study included only participants with umbilical hernia (Eriksen 2011) and another included only participants with incisional hernia (Colak 2015). Hernia size varied widely between studies; where reported, the mean size ranged from 3 to 190 cm2.
Intervention and comparison
Wassenaar 2010 performed a three‐arm trial, with the following fixation methods: nonabsorbable tacks in combination with nonabsorbable sutures, nonabsorbable tacks in combination with absorbable sutures and nonabsorbable tacks only in double‐crown technique. In Beldi 2011 the participants were randomised to fixation with nonabsorbable tacks or nonabsorbable sutures. In Eriksen 2011, fibrin sealant was compared to nonabsorbable tacks. Bansal 2012 compared non‐absorbable sutures to nonabsorbable sutures in combination with non‐absorbable tacks. Muysoms 2013 investigated the combination of nonabsorbable tacks with nonabsorbable sutures, in comparison to nonabsorbable tacks only. In Colak 2015 absorbable tacks were compared to nonabsorbable tacks. Bansal 2016 compared absorbable tacks combined with absorbable sutures with nonabsorbable tacks combined with nonabsorbable sutures. In Harsløf 2018 three arms were compared; fibrin sealant, nonabsorbable tacks and absorbable tacks. Shaukat 2018 compared nonabsorbable tacks to nonabsorbable sutures. Langenbach 2020 compared absorbable tacks to absorbable sutures.
Mesh repair was done by laparoscopy in eight studies, and in two studies repair was performed openly (Shaukat 2018; Langenbach 2020).
The nonabsorbable tacks used in all the studies were spiral nonabsorbable titanium tacks. The type of mesh varied between studies. In most studies composite meshes (covered meshes to prevent bowel adhesions) were used. In some studies the type of mesh was the same for all participants, whereas in others meshes from different companies were used for different participants according to the surgeons' or institutions' choice. No additional closure of the fascial defect has been reported in eight studies of laparoscopic mesh repair.
Outcomes
All but one study (Shaukat 2018) reported data on hernia recurrence. The follow‐up for recurrence ranged between three months and two years. In one study (Wassenaar 2010) the follow‐up for recurrence was shorter than six months (see Characteristics of included studies tables for the duration of follow‐up for each outcome). Pain (VAS) was reported in all studies. Four studies assessed health‐related quality of life (HRQOL) (Wassenaar 2010; Bansal 2016; Harsløf 2018; Langenbach 2020). Return to normal activity was reported in five studies (Wassenaar 2010; Eriksen 2011; Bansal 2012; Muysoms 2013; Bansal 2016). None of these five trials performed a time‐to‐event analysis and consequently no hazard ratios were reported, but only median time. The re‐operation rate at the same site of hernia was assessed in only one study (Langenbach 2020). Wassenaar 2010 assessed re‐operation rates due to chronic pain (participants with chronic pain) without specifying the pain measure. As we had not defined this as a relevant pain outcome in the protocol, we did not extract the data on this outcome. Three studies did not report on any postoperative complication (Beldi 2011; Harsløf 2018; Shaukat 2018)
Excluded studies
When we screened full texts, we excluded seven studies because of irrelevant comparisons (e.g. no comparison, simultaneous comparison of fixation method and different meshes) (Korenkov 2002; Polat 2005; Navarra 2007; Ammar 2010; Venclauskas 2010; Wéber 2010; Stabilini 2013; Pawlak 2015). Two studies were excluded because the allocation to the groups was not randomised (Afifi 2005; Ambore 2017). A list of all excluded studies with reasons are provided in the section Characteristics of excluded studies.
We identified five ongoing studies (Characteristics of ongoing studies). The conference abstract by Misra 2015 did not contained sufficient information for the assessment of eligibility and data extraction. One published study protocol (Silecchia 2015) was identified by the database search. Three other ongoing studies were identified in trial registries (CTRI/2019/05/019115; NCT01109771; NCT03429374).
Risk of bias in included studies
The 'Risk of bias' graph (Figure 2) and the 'Risk of bias' summary table (Figure 3) provide an overview of the 'Risk of bias' assessment.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Of the 10 included studies, nine were at low risk of bias for randomisation and allocation concealment.
Blinding
It is not possible to blind the surgeon to the intervention group. Only two studies specified that healthcare professionals (other than the surgeon) and the participants were blinded. The risk of performance and detection bias were therefore judged low only for these studies (Eriksen 2011; Harsløf 2018). The risk of detection bias was mostly assessed as unclear because of insufficient reporting. However, recurrence is an objective outcome, and consequently the risk of bias might not be that serious even when the personnel are not blinded. Because pain measures are subjective outcomes, we considered the risk of bias to be higher for this outcome.
Incomplete outcome data
In all but one study there were participants lost to follow‐up. In most studies the number of participants included in the analysis and reasons for dropout were not clear for all outcomes and follow‐up time points. This was particularly true for the pain measures. In the studies that we analysed according to the intention‐to‐treat principle, the method for imputing missing values was mostly not reported. This item was therefore assessed as being at unclear risk of bias, apart from the study that had no dropouts (Langenbach 2020). Information on handling missing data in the studies is given under "support for judgement" in the 'Risk of bias' tables. For all studies we performed a completer analysis, and for six studies (Wassenaar 2010; Beldi 2011; Eriksen 2011; Bansal 2012; Muysoms 2013; Bansal 2016) it was possible to perform a supplemental ITT sensitivity analysis. Information on participant flow (randomised and received treatment, analysed and imputed in the ITT analysis) for each study is presented in the notes in the Characteristics of included studies table.
Selective reporting
We were unable to access study protocols for any of the included studies. We nevertheless assumed that the risk of selective reporting bias was low for nine of the included studies, because all reported results for the outcomes mentioned in the Method section or additional material, and all expected outcomes (recurrence and postoperative complications) were reported (Wassenaar 2010; Beldi 2011; Eriksen 2011; Bansal 2012; Muysoms 2013; Colak 2015; Bansal 2016; Harsløf 2018; Langenbach 2020). Shaukat 2018 did not report on recurrence and we therefore judged this study to be at high risk for selective reporting.
Other potential sources of bias
No other sources of bias were identified.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10
Summary of findings 1. Absorbable tacks compared to nonabsorbable tacks in primary ventral or incisional hernia repair.
| Absorbable tacks compared to nonabsorbable tacks in incisional hernia repair | ||||||
| Patient or population: People needing incisional hernia repair Setting: Hospital Intervention: Absorbable tacks Comparison: Nonabsorbable tacks | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Risk with nonabsorbable tacks | Risk with absorbable tacks | |||||
| Recurrence (1 year to 31 (median) months) | 80 per 1000 | 21 fewer per 1000 (66 fewer to 178 more) |
RR 0.74 (0.17 to 3.22) |
101 (2 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Early postoperative pain (VAS 0 ‐ 10, 1 day) | The mean pain was 3 | MD 0 (0.58 lower to 0.58 higher) | ‐ | 51 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Early postoperative pain (VAS 0 ‐ 100, 2 days) | The mean pain was 55.3 | MD 11.8 lower (27.71 lower to 4.11 higher) |
‐ | 50 (1 RCT) |
⊕⊕⊝⊝b LOW |
‐ |
| Early postoperative pain (VAS 0 ‐ 10, 2 weeks) | The mean pain was 1.1 | MD 0.4 (0.1 |
||||
aRated down by one level for risk of bias (performance bias) and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm). bRated down by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm). cRated down by one level for risk of bias (performance bias) and by one level for imprecision (optimal information size threshold not reached). dRated down by two levels for imprecision (effect estimate is based on very few events).
Summary of findings 2. Nonabsorbable tacks compared to nonabsorbable sutures in primary ventral or incisional hernia repair.
| Nonabsorbable tacks compared to nonabsorbable sutures in primary ventral or incisional hernia repair | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Nonabsorbable tacks Comparison: Nonabsorbable sutures | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with nonabsorbable sutures | Risk with nonabsorbable tacks | |||||
| Recurrence (6 months) | 56 per 1000 | 56 per 1000 (4 to 822) | RR 1.00 (0.07 to 14.79) | 36 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Early postoperative pain (VAS 0 ‐ 10, 1 week) | The mean pain was 0.00 | MD 0.56 lower (1.79 lower to 0.67 higher) |
‐ | 53 (1RCT) |
⊕⊝⊝⊝ VERY LOWb | ‐ |
| Chronic pain (VAS 0 ‐ 10, 6 to 12 months) | Not pooled because of heterogeneity | In both studies pain was higher using tacks Range of MD: 0/3 higher to 1.3 higher |
‐ | 89 (2 RCT) | ⊕⊝⊝⊝ VERY LOWc | ‐ |
| Health‐related quality of life | Not assessed in any study | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; MD; mean difference | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aRated down by one level for risk of bias (performance bias) and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm). bRated down by two levels for risk of bias and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm). cRated down by two levels for risk of bias and by one level for inconsistency.
Summary of findings 3. Absorbable tacks compared to absorbable sutures in primary ventral or incisional hernia repair.
| Absorbable tacks compared to absorbable sutures | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Absorbable tacks Comparison: Absorbable sutures | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with absorbable sutures | Risk with absorbable tacks | |||||
| Recurrence (1 year) | 0 | 0 | not estimable | 48 (1 study) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Early postoperative pain (VAS 0 ‐ 10, sum 0 to 3 days) | ‐ | MD 2.7 lower (6.67 lower to 1.27 higher) | ‐ | 48 (1 study) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Chronic pain (VAS 0 ‐ 10, 6 months) | ‐ | MD 0.1 lower (0.42 lower to 0.22 higher) | ‐ | 48 (1 study) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Health‐related quality of life (6 months) | ‐ | No difference in quality of life (see Table 6) | ‐ | 48 (1 study) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Severe postoperative complications | 150 per 1000 | 215 per 1000 (60 to 756) | RR 1.43 (0.40 to 5.04) | 48 (1 study) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aRated down by one level for risk of bias (performance bias) and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm).
Summary of findings 4. Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures in primary ventral or incisional hernia repair.
| Nonabsorbable tacks plus nonabsorbable suture compared to nonabsorbable suture in primary ventral or incisional hernia repair | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Nonabsorbable tacks plus nonabsorbable sutures Comparison: Nonabsorbable sutures | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with nonabsorbable sutures | Risk with nonabsorbable tacks plus nonabsorbable sutures | |||||
| Recurrence (2 years) | 10 per 1000 | 46 per 1000 (2 to 943) | RR 4.82 (0.24 to 98.03) | 106 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Early postoperative pain (VAS 0 ‐ 10, 1 day) | The mean pain was 3.3 | MD 0.6 higher (0.1 lower to 1.3 higher) | ‐ | 92 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa | ‐ |
| Chronic pain (VAS 0 ‐ 10, 3 months) | The mean pain was 0.2 | MD 0.3 higher (0.07 higher to 0.53 higher) | ‐ | 92 (1 RCT) | ⊕⊕⊝⊝b LOW | ‐ |
| Seroma (7 days) | 173 per 1000 | 111 per 1000 (43 to 291) | RR 0.64 (0.25 to 1.68) | 106 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Mesh infection (postoperative not specified) | 0 per 1000 | 0 per 1000 (0 to 0) | not estimable | 106 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; MD; mean difference | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aRated down by one level for risk of bias (performance bias) and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm). bRated down by one level for risk of bias (performance bias) and by one level for imprecision (optimal information size threshold not reached).
Summary of findings 5. Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures in primary ventral or incisional hernia repair.
| Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures in primary ventral or incisional hernia repair | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Absorbable tacks plus absorbable sutures Comparison: Nonabsorbable tacks plus nonabsorbable sutures | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with nonabsorbable tacks plus nonabsorbable sutures | Risk with absorbable tacks plus absorbable sutures | |||||
| Recurrence (2 years) | 0 | 0 | not estimable | 77 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Early postoperative pain | Not assessed in any study | |||||
| Chronic pain (VAS 0 ‐ 10, 3 months) | The mean pain was 1.0 | MD 0.1 lower (0.39 lower to 0.19 higher) | ‐ | 90 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Chronic pain (VAS 0 ‐ 10, 6 months) | The mean pain was 0.3 | MD 0.2 lower (0.39 lower to 0.01 lower) | ‐ | 90 (1 RCT) | ⊕⊕⊝⊝b LOW | ‐ |
| Health‐related quality of life | Not assessed in any study | |||||
| Seroma (1 week) | 156 per 1000 | 110 per 1000 (37 to 324) | RR 0.71 (0.24 to 2.08) | 90 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; MD; mean difference | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aRated down by one level for risk of bias (performance bias) and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm). 2Rated down by one level for risk of bias (performance bias) and by one level for imprecision (optimal information size threshold not reached).
Summary of findings 6. Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures in primary ventral or incisional hernia repair.
| Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures in primary ventral or incisional hernia repair | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Nonabsorbable tacks Comparison: Nonabsorbable tacks plus nonabsorbable sutures | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with nonabsorbable tacks plus nonabsorbable sutures | Risk with nonabsorbable tacks | |||||
| Recurrence (3 months) | 11 per 1000 | 11 per 1000 (1 to 107) | PO R 1.06 (0.11 to 10.02) |
185 (2 RCTs) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Recurrence (2 years) | Study population | RR 0.33 (0.04 to 2.82) | 63 (1 RCT) | ⊕⊝⊝⊝b VERY LOW | ‐ | |
| 111 per 1000 | 37 per 1000 (4 to 313) | |||||
| Early postoperative pain (VAS 0 ‐ 10, at rest, 4 hours) | The mean pain was 4.4 | MD 1.3 lower (2.34 lower to 0.26 lower) | ‐ | 69 (1 RCT) | ⊕⊕⊝⊝c LOW | ‐ |
| Early postoperative pain (VAS 0 ‐ 10, coughing, 4 hours) | The mean pain was 6.8 | MD 1.6 lower (2.73 lower to 0.47 lower) | ‐ | 69 (1 RCT) | ⊕⊕⊝⊝c LOW | ‐ |
| Chronic pain (VAS 0 ‐ 10, at rest, 3 months) | The mean pain was 0.43 | MD 0.38 lower (0.86 lower to 0.1 higher) | ‐ | 59 (1 RCT) | ⊕⊕⊝⊝c LOW | ‐ |
| Chronic pain (VAS 0 ‐ 10, coughing, 3 months) | The mean pain was 0.78 | MD 0.36 lower (1.11 lower to 0.39 higher) | ‐ | 59 (1 RCT) | ⊕⊕⊝⊝c LOW | ‐ |
| Chronic pain (VAS 0 ‐ 100, 3 month) | The mean pain was 11.2 | MD 5.4 lower (11.79 lower to 0.99 higher) | ‐ | 116 (1 RCT) | ⊕⊕⊝⊝c LOW | ‐ |
| Health‐related quality of life | Not assessed in any study | |||||
| Seroma (3 month) | 11 per 1000 | 2 per 1000 (0 to 99) | P O |
|||
aRated down by one level for risk of bias (performance bias), by one level for imprecision (optimal information size threshold not reached) and by one level for inconsistency (different effect directions between the studies in meta‐analysis). bRated down by one level for risk of bias (performance bias) and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm). cRated down by one level for risk of bias (performance bias) and by one level for imprecision (optimal information size threshold not reached).
Summary of findings 7. Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks only in primary ventral or incisional hernia repair.
| Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks in primary ventral or incisional hernia repair | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Nonabsorbable tacks plus absorbable sutures Comparison: Nonabsorbable tacks | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with nonabsorbable tacks | Risk with nonabsorbable tacks plus absorbable sutures | |||||
| Recurrence (3 month) | 17 per 1000 | 18 per 1000 (1 to 279) | RR 1.07 (0.07 to 16.72) | 116 (1 RCT) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Early postoperative pain | Not assessed in any study | |||||
| Chronic pain (VAS 0 ‐ 100, 3 month) | The mean pain was 4.5 | MD 1.3 lower (5.49 lower to 2.89 higher) | ‐ | 116 (1 study) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Health‐related quality of life | Not assessed in any study | |||||
| Seroma (3 month) | Study population | RR 3.21 (0.13 to 77.22) | 116 (1 study) | ⊕⊝⊝⊝a VERY LOW | ‐ | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Haematoma (3 month) | 50 per 1000 | 54 per 1000 (12 to 255) | RR 1.07 (0.23 to 5.09) | 116 (1 study) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; MD; mean difference | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aRated down by one level for risk of bias (performance bias) and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm).
Summary of findings 8. Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures in primary ventral or incisional hernia repair.
| Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures in primary ventral or incisional hernia repair | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Nonabsorbable tacks plus absorbable sutures Comparison: Nonabsorbable tacks plus nonabsorbable sutures | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with nonabsorbable tacks plus nonabsorbable sutures | Risk with nonabsorbable tacks plus absorbable sutures | |||||
| Recurrence (3 month) | 9 per 1000 | 27 per 1000 (1 to 644) | RR 3.00 (0.12 to 72.10) | 112 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa | ‐ |
| Chronic pain (VAS 0 ‐ 100, 3 month) | The mean pain was 11.2 | MD 6.7 lower (12.9 lower to 0.5 lower) | ‐ | 112 (1 RCT) | ⊕⊕⊝⊝b LOW | ‐ |
| Health‐related quality of life | Not assessed in any study | |||||
| Seroma (3 month) | 0 per 1000 | 0 per 1000 (0 to 0) | RR 3.00 (0.12 to 72.10) | 112 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa | ‐ |
| Haematoma (3 month) | 18 per 1000 | 54 per 1000 (6 to 499) | RR 3.00 (0.32 to 27.97) | 112 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa | ‐ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; MD; mean difference | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aRated down by one level for risk of bias (performance bias) and by two levels for imprecision (effect estimate is based on very few events). bRated down by one level for risk of bias (performance bias) and by one level for imprecision (optimal information size threshold not reached).
Summary of findings 9. Nonabsorbable tacks compared to fibrin sealant in primary ventral or incisional hernia repair.
| Nonabsorbable tacks compared to fibrin sealant in primary umbilical hernia repair | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Nonabsorbable tacks Comparison: Fibrin sealant | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with fibrin sealant | Risk with Nonabsorbable tacks | |||||
| Recurrence (1 year) | Not pooled because of heterogeneity | ‐ | RR ranged from 0.20 to 5.00 | 88 (2 RCTs) | ⊕⊝⊝⊝a VERY LOW | ‐ |
| Early postoperative pain (VAS 0 ‐ 100, 2 days) | The mean pain was 55.9 | MD 0.6 lower (15.92 lower to 14.72 higher) |
‐ | 50 (1 Study) |
⊕⊕⊝⊝b LOW |
‐ |
| Pain (up to 1 year) | No difference in pattern of pain over time | ‐ | 50 (1 RCT) |
⊕⊕⊝⊝b LOW | ‐ | |
| Health‐related quality of life (up to 1 year) | No difference in pattern of quality of life over time | ‐ | 50 (1 RCT) |
⊕⊕⊝⊝b LOW | ‐ | |
| Seroma (30 days) | 386 per 1000 | 359 per 1000 (209 to 622) |
RR 0.93 (0.54 to 1.61) |
88 (2 RCTs) | ⊕⊕⊝⊝b LOW | ‐ |
| Haematoma (30 days) | 211 per 1000 | 158 per 1000 (40 to 613) | RR 0.75 (0.19 to 2.91) | 38 (1 RCT) | ⊕⊕⊝⊝b LOW |
‐ |
| Superficial infection (30 days) | 295 per 1000 | 281 per 1000 (154 to 514) |
RR 0.95 (0.52 to 1.74) |
88 (2 RCTs) | ⊕⊝⊝⊝b VERY LOW | ‐ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; MD; mean difference | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aRated down by one level for inconsistency and by two levels for imprecision (optimal information size threshold not reached and 95% confidence intervals include appreciable benefit and appreciable harm). bRated down by two levels for imprecision (effect estimate is based on only one small study and 95% confidence intervals include appreciable benefit and appreciable harm or P‐values are very large).
Summary of findings 10. Absorbable tacks compared to fibrin sealant in primary ventral or incisional hernia repair.
| Absorbable tacks compared to fibrin sealant in primary ventral or incisional hernia repair | ||||||
| Patient or population: People with primary ventral or incisional hernia repair Setting: Hospital Intervention: Absorbable tacks Comparison: Fibrin sealant | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with fibrin sealant | Risk with absorbable tacks | |||||
| Recurrence (1 year) | 0 | 1 per 25 | RR 3.00 (0.13 to 70.30) | 50 (1 study) | ⊕⊕⊝⊝a LOW |
‐ |
| Early postoperative pain (VAS 0 ‐ 100, 2 days) | The mean pain was 55.9 | MD 12.4 lower (27.6 lower to 2.8 higher) | ‐ | 50 (1 study) | ⊕⊕⊝⊝a LOW |
‐ |
| Pain (up to 1 year) | No difference in pattern of pain over time | ‐ | 50 (1 RCT) |
⊕⊕⊝⊝a LOW |
‐ | |
| Health‐related quality of life (up to 1 year) | No difference in pattern of quality of life over time | ‐ | 50 (1 RCT) |
⊕⊕⊝⊝a LOW |
‐ | |
| Infection (1 month) | 40 per 1000 | 40 per 1000 (3 to 605) | RR 1.00 (0.07 to 15.12) | 50 (1 study) | ⊕⊕⊝⊝a LOW |
‐ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; MD: mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aRated down by two levels for imprecision (effect estimate is based on very few events).
1. Absorbable tacks compared to nonabsorbable tacks (2 studies, 101 participants; Colak 2015; Harsløf 2018; Table 1) ‐ laparoscopic surgery
Primary outcomes
Recurrence rates in the groups were similar (risk ratio (RR) 0.74, 95% confidence interval (CI) 0.17 to 3.22; Figure 4). It is uncertain whether there is a difference between absorbable tacks and nonabsorbable tacks in recurrence because the certainty of evidence was very low. Evidence suggests that the difference between groups in early postoperative, late follow‐up, chronic pain and HRQOL is negligible (Analysis 1.2; Analysis 1.4; Analysis 1.5; Table 11, Table 12).
4.

Forest plot of comparison: 1 Absorbable tacks compared to nonabsorbable tacks, outcome: 1.1 Recurrence (1 year to median 31 months).
1.2. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 2: Pain (VAS 0 ‐ 10, 1 day)
1.4. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 4: Pain (VAS 0 ‐ 10, 2 week)
1.5. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 5: Pain (VAS 0 ‐ 10, 6 months)
1. Pain (VAS 0‐100, day 2 to 1 year) Harslof 2018.
| Change over time | P value |
| Similar pattern | P = 0.418* |
*P value treatment x time interaction for the 3 study groups
2. HRQOL (SF‐36 physical functioning, up to 1 year) Harslof 2018.
| Chane over time | p‐value |
| Similar pattern | P = 0.915* |
*P value treatment x time interaction for the 3 study groups
Secondary outcomes
There were negligible differences between groups in complications (very low‐ or low‐certainty evidence), duration of surgery and length of hospital stay (Analysis 1.6; Analysis 1.9; Analysis 1.10; Table 13).
1.6. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 6: Seroma (3 days)
1.9. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 9: Length of hospital stay (days)
1.10. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 10: Duration of surgery (minutes)
3. Complications Colak 2015.
| Complication | Absorbable tacks | Nonabsorbable |
| Prolonged ileus | 1 | 0 |
| Trocar hernia | 1 | 1 |
| Seroma progressed to cellulitis | 3 | 2 |
| Mesh migration | 0 | 1 |
2. Nonabsorbable tacks compared to nonabsorbablesutures (2 studies, 89 participants; Beldi 2011; Shaukat 2018; Table 2) ‐ laparoscopic and open surgery
Primary outcomes
At six months there was one recurrence in each group (RR 1.00, 95% CI 0.07 to 14.79; Analysis 2.1). It is uncertain whether there is a difference between nonabsorbable tacks and nonabsorbable sutures in recurrence because the certainty of evidence was very low. Evidence suggests that the difference between groups in early postoperative, late follow‐up and chronic pain is negligible (Analysis 2.2; Analysis 2.3; Figure 5 ). It is uncertain whether there is a difference between nonabsorbable tacks and nonabsorbable sutures in chronic pain because the certainty of evidence was very low. We found no study that assessed HRQOL.
2.1. Analysis.

Comparison 2: Nonabsorbable tacks compared to nonabsorbable sutures, Outcome 1: Recurrence (6 months)
2.2. Analysis.

Comparison 2: Nonabsorbable tacks compared to nonabsorbable sutures, Outcome 2: Pain (VAS 0 ‐ 10, 1 week)
2.3. Analysis.

Comparison 2: Nonabsorbable tacks compared to nonabsorbable sutures, Outcome 3: Pain (VAS 0 ‐ 10, 4 to 6 weeks)
5.

Forest plot of comparison: 2 Nonabsorbable tacks compared to nonabsorbable sutures, outcome: 2.4 Pain (VAS 0 ‐ 10, 6 to 12 months).
Secondary outcomes
In Shaukat 2018, more participants in the tacked group had a long hospital stay (defined as 3 to 4 days) (Analysis 2.5). In contrast the median length of hospital stay was six days in both groups in Beldi 2011 (Table 14). The duration of surgery was longer in the suture group in both studies (Analysis 2.6; Table 14). We found no study that assessed complications.
2.5. Analysis.

Comparison 2: Nonabsorbable tacks compared to nonabsorbable sutures, Outcome 5: Length of hospital stay (3 to 4 days)
4. Hospital stay, duration of surgery Beldi 2011.
| Outcome | Tacks (median, range) | Sutures (median, range) | P values |
| Length of hospital stay (days) | 6 (1 – 10) | 6 (3 – 12) | 0.681 |
| Duration of surgery (minutes) | 92 (45 – 310) | 120 (75 – 240) | 0.039 |
2.6. Analysis.

Comparison 2: Nonabsorbable tacks compared to nonabsorbable sutures, Outcome 6: Duration of surgery (minutes)
3. Absorbable tacks comparedto absorbable sutures (1 study, 48 participants; Langenbach 2020; Table 3) ‐ open surgery
Primary outcomes
No recurrence was observed at one year (very low‐certainty evidence). Early postoperative pain was higher in the tacks group (VAS 0 ‐ 10; MD −2.70, 95% CI −6.67 to 1.27; Analysis 3.2). It is uncertain whether there is a difference between absorbable tacks compared to absorbable sutures in early postoperative pain because the certainty of evidence was very low. The MD for late follow‐up pain was −0.30 (95% CI −0.74 to 0.14; Analysis 3.3). HRQOL has not been assessed.
3.2. Analysis.

Comparison 3: Absorbable tacks compared to absorbable sutures, Outcome 2: Pain (VAS 0 ‐ 10, sum 0 to 3 days)
3.3. Analysis.

Comparison 3: Absorbable tacks compared to absorbable sutures, Outcome 3: Pain (VAS 0 ‐ 10, 1 month)
Secondary outcomes
There were more severe complications in the tacks group (RR 3.57, 95% CI0.45 to 28.27; Analysis 3.5). In the tacks group 1 of 28 participants required re‐operation, but none of 20 in the sutures group (Analysis 3.6). Mean length of hospital stay was one day longer in the tacks group (Analysis 3.7).
3.5. Analysis.

Comparison 3: Absorbable tacks compared to absorbable sutures, Outcome 5: Severe postoperative complications
3.6. Analysis.

Comparison 3: Absorbable tacks compared to absorbable sutures, Outcome 6: Reoperation (1 year)
3.7. Analysis.

Comparison 3: Absorbable tacks compared to absorbable sutures, Outcome 7: Length of hospital stay (days)
4. Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures (1 study, 106 participants; Bansal 2012; Table 4) ‐ laparoscopic surgery
Primary outcomes
At two years there were two recurrences in the tacks‐plus‐suture group and zero in the sutures‐only group (RR 4.82, 95% CI 0.24 to 98.03; Analysis 4.1). It is uncertain whether there is a difference between nonabsorbable tacks plus nonabsorbable sutures and nonabsorbable sutures only in recurrence, because the certainty of evidence was very low. Evidence suggests that the difference between groups in early postoperative, late follow‐up and chronic pain is negligible (Analysis 4.2; Analysis 4.3; Analysis 4.4; Analysis 4.5). We found no study that assessed late follow‐up pain or HRQOL.
4.1. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 1: Recurrence (2 years)
4.2. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 2: Pain (VAS 0 ‐ 10, 1 day)
4.3. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 3: Pain (VAS 0 ‐ 10, 1 week)
4.4. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 4: Pain (VAS 0 ‐ 10, 1 months)
4.5. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 5: Pain (VAS 0 ‐ 10, 3 months)
Secondary outcomes
Seroma (RR 0.64, 95% CI 0.25 to 1.68; Analysis 4.6; very low certainty of evidence) and other complications were more frequently observed in the suture group or not identified at all (low certainty of evidence; Table 15). Duration of surgery, length of hospital stay and all other complications showed an effect direction in favour of suture repair only (Analysis 4.2; Analysis 4.3; Analysis 4.4; Analysis 4.7; Analysis 4.9; Analysis 4.10). Return to normal activity was faster in the sutures‐only group (MD 6.60 days, 95% CI 2.89 to 10.31; low certainty of evidence; Analysis 4.8).
4.6. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 6: Seroma (7 days)
5. Complications Bansal 2012.
| Complication | Tacks plus suture | Suture |
| Abandon procedure | ‐ | 2 |
| Divarication of recti | ‐ | 1 |
| Disseminated TB | ‐ | 1 |
| Small bowel injury | ‐ | 1 |
| Bladder injury | ‐ | 1 |
| Suture site sinus | 1 | ‐ |
4.7. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 7: Mesh infection (postoperative not specified)
4.9. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 9: Length of hospital stay (days)
4.10. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 10: Duration of surgery (minutes)
4.8. Analysis.

Comparison 4: Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures, Outcome 8: Time until return to normal activity (days)
5. Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures (1 study, 90 participants; Bansal 2016; Table 5) ‐ laparoscopic surgery
Primary outcomes
No recurrences were observed after two years in either group (Analysis 5.1). It is uncertain whether there is a difference between absorbable tacks plus absorbable sutures and nonabsorbable tacks plus nonabsorbable sutures in recurrence, because the certainty of evidence was very low. Evidence suggests that the difference between groups in chronic pain is negligible (Analysis 5.2; Analysis 5.3). We found no study that assessed early postoperative pain, late follow‐up pain or HRQOL.
5.1. Analysis.

Comparison 5: Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 1: Recurrence (2 years)
5.2. Analysis.

Comparison 5: Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 2: Pain (VAS 0 ‐ 10, 3 months)
5.3. Analysis.

Comparison 5: Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 3: Pain (VAS 0 ‐ 10, 6 months)
Secondary outcomes
There were no differences in complications (very low certainty of evidence), nor in the duration of surgery or length of hospital stay (Analysis 5.4; Analysis 5.5; Analysis 5.6; Analysis 5.7; Analysis 5.8; Table 16; Table 17).
5.4. Analysis.

Comparison 5: Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 4: Seroma (1 week)
5.5. Analysis.

Comparison 5: Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 5: Seroma (1 months)
5.6. Analysis.

Comparison 5: Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 6: Seroma (3 months)
5.7. Analysis.

Comparison 5: Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 7: Length of hospital stay (days)
5.8. Analysis.

Comparison 5: Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 8: Duration of surgery (minutes)
6. Return to normal activity Bansal 2016.
| Absorbable tacks and sutures (mean) | Nonabsorbable tacks and sutures (mean) | P value | |
| Return to normal activity | 7 (estimated from graphs) | 8.5 (estimated from graphs) | 0.36 |
7. Complications Bansal 2016.
| Complication | Absorbable tacks and sutures | Nonabsorbable tacks and sutures |
| Subacute intestinal obstruction | 1 | 1 |
| Small bowel injury | 1 | 0 |
| Pneumonia | 1 | 0 |
| Urinary retention | 1 | 0 |
| Port‐site access | 1 | 0 |
6. Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures (2 studies, 186 participants; Muysoms 2013; Wassenaar 2010; Table 6) ‐ laparoscopic surgery
Primary outcomes Only one recurrence occurred in each group (POR 1.07, 95% CI 0.07 to 17.24; Analysis 6.1; Figure 6) after three months. After two years the incidence of recurrence was higher in the nonabsorbable tacks plus nonabsorbable sutures group (RR 0.33, 95% CI 0.04 to 2.82; Analysis 6.2). It is uncertain whether there is a difference in recurrence between nonabsorbable tacks only and nonabsorbable tacks plus nonabsorbable sutures, because the certainty of evidence was very low. Nonabsorbable tacks plus nonabsorbable sutures may slightly increase early postoperative and chronic pain compared to nonabsorbable tacks alone (Analysis 6.4; Analysis 6.5; Analysis 6.6; Analysis 6.7; Analysis 6.8; Analysis 6.9; Analysis 6.10; Analysis 6.11 Table 18; Table 19; Table 20). Nonabsorbable tacks only and nonabsorbable tacks plus nonabsorbable sutures may make little or no difference to late follow‐up pain. We found no study that assessed HRQOL.
6.1. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 1: Recurrence (3 months)
6.

Forest plot of comparison: 6 Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, outcome: 6.1 Recurrence (3 months).
6.2. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 2: Recurrence (2 years)
6.4. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 4: Pain (VAS 0 ‐ 10, coughing, 4 hours)
6.5. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 5: Pain (VAS 0 ‐ 100, 2 weeks)
6.6. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 6: Pain (VAS 0 ‐ 10, at rest, 4 weeks)
6.7. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 7: Pain (VAS 0 ‐ 10, coughing, 4 weeks)
6.8. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 8: Pain (VAS 0 ‐ 100, 6 weeks)
6.9. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 9: Pain (VAS 0 ‐ 10, at rest, 3 months)
6.10. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 10: Pain (VAS 0 ‐ 10, coughing, 3 months)
6.11. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 11: Pain (VAS 0 ‐ 100, 3 month)
8. HRQOL Wassenaar 2010.
| Outcome | Absorbable sutures plus tacks (mean, 95% CI) | Tacks (mean, 95% CI) | Nonabsorbable sutures plus tacks (mean, 95% CI) |
| General health (SF‐36, 3 months change from baseline) | −15.7 (−23.2 to −8.2) | −13.5 (−18.5 to −8.5) | −13.4 (−18.7 to –−.2) |
9. Complications Wassenaar 2010.
| Complication | Absorbable sutures plus tacks | Tacks | Nonabsorbable sutures plus tacks |
| Urinary retention | 3 | 2 | 1 |
| Prolonged ileus | 1 | ‐ | 1 |
| Bulging | 1 | ‐ | 1 |
| Trocar hernia | 1 | 1 | 1 |
10. Complications Muysoms 2013.
| Complication | Tacks plus suture | Tacks |
| Postoperative ileus | 2 | 1 |
| Urinary tract infection | 2 | 0 |
Secondary outcomes
The differences in the pooled effect estimates for seroma, haematoma, duration of surgery and length of hospital stay were small (very low certainty of evidence; Analysis 6.12; Analysis 6.13; Analysis 6.14; Analysis 6.15).
6.12. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 12: Seroma (3 month)
6.13. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 13: Haematoma (post‐operative)
6.14. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 14: Length of hospital stay (days)
6.15. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 15: Duration of surgery (minutes)
7. Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks alone (1 study, 116 participants; Wassenaar 2010; Table 7) ‐ laparoscopic surgery
Primary outcomes
In the comparison of nonabsorbable tacks plus absorbable sutures versus nonabsorbable tacks alone there was no difference in recurrences at three months (RR 1.07, 95% CI 0.07 to 16.72; Analysis 7.1). It is uncertain whether there is a difference in recurrence between nonabsorbable tacks plus absorbable sutures and nonabsorbable tacks alone because the certainty of evidence was very low or low for these outcomes. Evidence suggests that the difference between groups in early postoperative, late follow‐up and chronic pain is negligible (Analysis 7.2; Analysis 7.3; Analysis 7.4). We found no study that assessed HRQOL.
7.1. Analysis.

Comparison 7: Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks, Outcome 1: Recurrence (3 month)
7.2. Analysis.

Comparison 7: Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks, Outcome 2: Pain (VAS 0 ‐ 100, 2 weeks)
7.3. Analysis.

Comparison 7: Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks, Outcome 3: Pain (VAS 0 ‐ 100, 6 weeks)
7.4. Analysis.

Comparison 7: Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks, Outcome 4: Pain (VAS 0 ‐ 100, 3 month)
Secondary outcomes
Complications (very low certainty of evidence) and the length of hospital stay did not differ between groups (Analysis 7.5 Analysis 7.6; Analysis 7.7). Surgery took longer with tacks plus sutures (MD 13.50 minutes, 95% CI 5.07 to 21.93; Analysis 7.8).
7.5. Analysis.

Comparison 7: Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks, Outcome 5: Seroma (3 month)
7.6. Analysis.

Comparison 7: Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks, Outcome 6: Haematoma (3 month)
7.7. Analysis.

Comparison 7: Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks, Outcome 7: Length of hospital stay (days)
7.8. Analysis.

Comparison 7: Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks, Outcome 8: Duration of surgery (minutes)
8. Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures (1 study, 112 participants; Wassenaar 2010; Table 8) ‐ laparoscopic surgery
Primary outcomes
Only one recurrence was observed in the nonabsorbable tacks with absorbable sutures group (RR 3.00, 95% CI 0.12 to 72.10; Analysis 8.1) at three months. It is uncertain whether there is a difference between nonabsorbable tacks plus absorbable sutures and nonabsorbable tacks plus nonabsorbable sutures in recurrence, because the certainty of evidence was very low. Evidence suggests that the difference between groups in early postoperative, late follow‐up and chronic pain is negligible (Analysis 8.2; Analysis 8.3; Analysis 8.4). It is uncertain whether there is a difference between nonabsorbable tacks plus absorbable sutures and nonabsorbable tacks plus nonabsorbable sutures in chronic pain because the certainty of evidence was very low. We found no study that assessed HRQOL.
8.1. Analysis.

Comparison 8: Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 1: Recurrence (3 month)
8.2. Analysis.

Comparison 8: Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 2: Pain (VAS 0 ‐ 100, 2 weeks)
8.3. Analysis.

Comparison 8: Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 3: Pain (VAS 0 ‐ 100, 6 weeks)
8.4. Analysis.

Comparison 8: Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 4: Pain (VAS 0 ‐ 100, 3 month)
Secondary outcomes
Differences in complication rates (very low certainty of evidence) length of hospital stay and duration of surgery were small ( Analysis 8.5; Analysis 8.6; Analysis 8.7; Analysis 8.8).
8.5. Analysis.

Comparison 8: Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 5: Seroma (3 month)
8.6. Analysis.

Comparison 8: Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 6: Haematoma (3 month)
8.7. Analysis.

Comparison 8: Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 7: Length of hospital stay (days)
8.8. Analysis.

Comparison 8: Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 8: Duration of surgery (minutes)
9. Nonabsorbable tacks compared to fibrin sealant (2 studies, 88 participants; Eriksen 2011; Harsløf 2018; Table 9) ‐ laparoscopic surgery
Primary outcomes
The two studies showed different directions of effect; one showed higher rates for nonabsorbable tacks, the other showed higher rates for fibrin sealant. Data could not be pooled because of heterogeneity; Figure 7). Certainty of evidence was very low. Low‐certainty evidence suggests that the difference between groups in early postoperative, late follow‐up, chronic pain and HRQOL is negligible (Analysis 9.2; Table 11; Table 12; Table 21).
7.

Forest plot of comparison: 9 Nonabsorbable tacks compared to fibrin sealant, outcome: 9.1 Recurrence (1 year).
9.2. Analysis.

Comparison 9: Nonabsorbable tacks compared to fibrin sealant, Outcome 2: Pain (VAS 0 ‐ 100, 2 days)
11. Eriksen 2013 (outcomes for metric scaled variables).
| Outcome | Tacks (median, range) | Sealant (median, range) |
| Pain (VAS 0‐100, during activity, days 0‐10) | 40 (6 – 74) | 21 (2 – 67) |
| Pain (VAS 0‐100, at rest, days 0‐10) | 32 (2 – 73) | 10 (2 – 59) |
| Pain (VAS 0‐100, during activity, 1 year) | 0 (0 – 32) | 0 (0 – 28) |
| Pain (VAS 0‐100, at rest, 1 year) | 0 (0 – 46) | 0 (0 – 24) |
| Time until return to normal activity (days) | 18 (1 – 95) | 7 (1 – 66) |
| Length of hospital stay (days) | 0 (0 – 2) | 0 (0 – 2) |
| Duration of surgery (minutes) | 40 (23 – 130) | 50 (30 – 90) |
Secondary outcomes
No differences in complication rates were observed (low certainty of evidence; Analysis 9.3; Analysis 9.4). The duration of surgery was a little shorter in the nonabsorbable tacks group (Table 21). Participants in the fibrin sealant group returned earlier to daily activities (median 7 versus 18 days).
9.3. Analysis.

Comparison 9: Nonabsorbable tacks compared to fibrin sealant, Outcome 3: Seroma (30 days)
9.4. Analysis.

Comparison 9: Nonabsorbable tacks compared to fibrin sealant, Outcome 4: Haematoma (30 days)
10. Absorbable tacks compared to fibrin sealant (1 study, 50 participants; Harsløf 2018; Table 10) ‐ laparoscopic surgery
Primary outcomes
One recurrence in the absorbable tacks group and none in the fibrin sealant group were reported after one year (low certainty of evidence; Analysis 10.1). Early postoperative pain might be slightly lower using absorbable tacks (VAS 0 ‐ 100; MD −12.40, 95% CI −27.60 to 2.80; Analysis 10.2; low certainty of evidence). The pattern of pain and HRQOL course over time (up to 1 year) was similar in the groups (low certainty of evidence; Table 11; Table 12).
10.1. Analysis.

Comparison 10: Absorbable tacks compared to fibrin sealant, Outcome 1: Recurrence (1 year)
10.2. Analysis.

Comparison 10: Absorbable tacks compared to fibrin sealant, Outcome 2: Pain (VAS 0 ‐ 100, 2 days)
Secondary outcomes
One participant in each group had an infection (low quality of evidence; Analysis 10.3).
10.3. Analysis.

Comparison 10: Absorbable tacks compared to fibrin sealant, Outcome 3: Infection (1 month)
Sensitivity and subgroup analysis
None of our meta‐analyses included more than two studies. It was therefore not possible to perform any subgroup analysis.
Neither could we perform a sensitivity analysis by risk of bias because there were only one or two studies included for each comparison.
We performed a best‐case/worst‐case analysis for the comparison of nonabsorbable tacks compared to nonabsorbable sutures (analysis 2), nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable tacks only (Analysis 6), nonabsorbable sutures plus nonabsorbable tacks compared to nonabsorbable sutures only (Analysis 4), absorbable sutures plus absorbable tacks compared to nonabsorbable sutures plus nonabsorbable tacks (Analysis 5), nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks only (Analysis 7), nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures (Analysis 8), and nonabsorbable tacks compared to fibrin sealant (Analysis 9) (Bansal 2012; Wassenaar 2010; Beldi 2011; Eriksen 2011; Muysoms 2013; Bansal 2016). None of the sensitivity analyses changed the results significantly compared to the completer analysis (data not shown). We did not conduct best‐case and worst‐case analyses for the other comparisons due to missing information (number of included participants or lost to follow‐up by group).
Publication bias
We could not assess the risk of publication bias because there were only one or two studies included in each meta‐analysis.
Discussion
Summary of main results
We included 10 studies reporting data and 10 different comparisons in this review. The certainty of evidence was low or very low for almost all comparisons and outcomes. In addition to the low certainty of evidence, the follow‐up period of most studies was too short (range: three months to two years) for a conclusive assessment of recurrence and chronic pain. Given these limitations, the results of this review should be interpreted with caution. Overall, the differences between the fixation techniques were small for the primary outcomes (recurrence, pain, health‐related quality of life (HRQOL)). In addition, postoperative complications such as haematoma and seroma differed only slightly or negligibly between the groups.
Overall completeness and applicability of evidence
Most studies assessed our primary outcomes (recurrence, pain and complications). However, there is a lack of studies that address health‐related quality of life (HRQOL).
Another important deficit is that follow‐up duration was mostly too short for a conclusive comparison of recurrences. In only four studies was the follow‐up longer than one year (Bansal 2012; Muysoms 2013; Colak 2015; Bansal 2016). The relevance of the incompleteness of evidence becomes apparent in the comparison of nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable tacks in Muysoms 2013 (Analysis 6.1; Analysis 6.2). After three months, there was one recurrence in the nonabsorbable tacks plus nonabsorbable suture group and none in the nonabsorbable tacks group. However, after a follow‐up period of two years, there was one hernia in the nonabsorbable tacks group and four in the nonabsorbable tacks plus nonabsorbable suture group (RR 0.33, 95% CI 0.04 to 2.82). Furthermore, other studies have shown that fewer than half of the recurrences occur within the first six month after surgery (Ballem 2008). Thus, an "accurate" and significant difference would only be recognised after a sufficient length of follow‐up (probably at least two years).
Most studies considered primary and incisional ventral hernias, but In one study comparing fibrin sealant with nonabsorbable tacks and in another study comparing absorbable tacks with nonabsorbable tacks, only umbilical hernias or incisional hernias were included, respectively (Colak 2015; Eriksen 2011). This might limit the applicability of results to other hernia types because the surgical results may differ between hernia types (Köckerling 2015). Noticeably, in the meta‐analysis of fibrin sealant compared to nonabsorbable tacks, the effect direction of the two included studies for different hernia types conflicted for recurrence. Apart from the two studies mentioned above, no other study applied many or strict inclusion criteria for hernia type and for participant characteristics such as co‐morbidity or weight. This increases the external validity of the included studies. In addition to the type of hernia (primary, incisional, and recurrent), the hernia size (width) is an important variable to stage and compare the complexity of the hernia and its repair. Most studies excluded large defects, but no uniform classification (e.g. the European Hernia Society classification (Muysoms 2009)) has been applied to characterise the size (and localisation) of the hernia. Moreover, all but two of the included studies compared mesh fixation techniques in laparoscopic hernia repair with intraperitoneal onlay mesh. In clinical practice, laparoscopic repair is widely applied for primary ventral hernia and incisional hernias with limited size. However, patients with recurrent hernias or incisional hernias with large defects will still undergo open surgery in most hospitals. In contrast to the laparoscopic approach, in open ventral hernia repair the use of sutures is not challenged. But, as already discussed for inguinal hernia repair the use of self‐gripping meshes will be further investigated and might preclude any mesh fixation in open ventral hernia repair (Zhang 2014).
We must assume that patient populations vary between the hospitals that performed the included studies (which are involved in research activities, e.g. university hospitals) and the many 'other' hospitals that perform hernia repair in usual care. This reduces the applicability of our results to other hospitals and settings (e.g. ambulatory care). Moreover, the skills of the surgeon and the hospital volume are important determinants of the results of the surgical procedure (Archampong 2012; Pieper 2013). They may vary in other hospitals, especially if we assume that the studies were predominantly performed by specialist surgeons and higher‐volume hospitals. In addition, it should be considered that the fixation techniques were applied as part of a trial. Most studies did not report experience level with a certain technique. We can therefore assume that in the intervention group, surgeons were at the beginning of their learning curve. Applicability to other settings is also limited because in clinical practice there are many different mesh types and subtypes of the fixation methods (number of tacks, different producers, products, etc.). Furthermore, the healthcare delivery (surgery, nursing care, etc.) can vary between different settings (e.g. staffing).
Quality of the evidence
We rated the certainty of evidence as very low or low for almost all comparisons and outcomes. One main reason for this was a high degree of imprecision because of small sample sizes from one study and low event rates. Thus, an existing effect might not have been detected because the trials were underpowered. Imprecision had a particular influence on the certainty of evidence for the outcomes of recurrence and complications, because of their low (short‐term) incidence. Even pooled results of recurrences showed very wide confidence intervals. Often only one or two recurrences were observed and consequently the different event distribution between groups might well have been coincidental.
A second reason for the low certainty of evidence was the risk of bias of included studies. They all suffered from known bias or were at risk of unknown bias because of the lack of reporting of methods applied. The surgeon cannot be blinded. Although it could have been implemented, in only two of the studies was an attempt to blind the participants reported (Eriksen 2011; Harsløf 2018). Only two studies reported that they mitigated detection bias by stating that outcome assessment was performed blindly (Eriksen 2011, Harsløf 2018). The risk of detection bias was unclear for all other trials. Moreover, some trials were not analysed according to an intention‐to‐treat (ITT) principle, which is a particular problem because the necessary information on the number of dropouts to perform an intention‐to‐treat sensitivity analysis was often not reported. Where ITT data were reported, the data imputation methods were not specified.
Potential biases in the review process
We did not conduct a search of the grey literature databases for additional unpublished material.
Agreements and disagreements with other studies or reviews
A systematic review with meta‐analysis of controlled studies on mesh fixation techniques could not find an obvious superiority of any fixation method for recurrence or pain (Reynvoet 2014), which is in agreement with our findings. The overall incidence of recurrences was low, with slightly more recurrences occurring if nonabsorbable sutures and nonabsorbable tacks were combined, compared to nonabsorbable tacks only. In contrast to this and to our findings, a systematic review with network meta‐analysis that included cohort studies came to the conclusion that sutures are superior compared to tacks for recurrence (Baker 2018). This difference in strength of conclusion probably arises because of differences in the judgement of the certainty of evidence. We argue that this finding from non‐randomised evidence might be spurious because the surgeon considers prognostic factors in the choice of the fixation technique, consequently giving rise to a high risk of confounding bias (Sterne 2016).
Another systematic review by Sajid 2013 that included RCTs and non‐RCTs on nonabsorbable tacks (with and without sutures) compared to sutures alone (absorbable and nonabsorbable) for incisional hernias is also in accord with our findings. Participants reported slightly lower pain scores when nonabsorbable tacks were used (with and without sutures) compared to sutures alone, and there were no clinically or statistically significant differences in other outcomes (Sajid 2013). In addition, a prospective cohort study with 50 participants could not find a difference in pain measures when nonabsorbable tacks were compared to nonabsorbable sutures (Nguyen 2008).
We can assume that the effect of tack fixation on recurrence and pain strongly depends on the number of tacks used for fixation. However, a study with 80 participants on the prognostic value of the number of tacks for chronic pain did not find a clinically relevant effect (Schoenmaeckers 2012). In Beldi 2011, on nonabsorbable tacks compared to nonabsorbable sutures included in this review, the difference in long‐term pain was very small. The detection of marginal differences between the fixation techniques is also supported by a systematic review on mesh fixation which shows that relative effects did not vary widely between the surgical procedures that were being used (fixation, intra‐abdominal mesh position, mesh type) (Mathes 2016). We could not find a difference between absorbable and nonabsorbable tacks. A cohort study including 816 participants suggested that absorbable tacks are associated with a higher rate of recurrences (Christoffersen 2015). In this cohort study, the median follow‐up was 40 months and the difference only became apparent after 12 months. In the included studies the maximum follow‐up was 12 and 24 months (Colak 2015; Bansal 2016), suggesting that the follow‐up of the included trials in our review was too short to fully assess this outcome.
Authors' conclusions
Implications for practice.
Currently none of the techniques can be considered superior to any other because the certainty of evidence was low or very low for all outcomes.
The studies were underpowered, and most of them only had a short follow‐up period. It is therefore unclear whether there is any clinically relevant difference between the fixation techniques, or whether a difference simply did not become apparent.
Implications for research.
RCTs that compare nonabsorbable tacks with absorbable tacks as well as tacks with sutures in a clearly‐defined group (hernia classification according to the EHS) are needed. The RCTs should overcome the serious limitations of the current evidence. These includes a sufficient sample size, blinded outcome assessment, appropriate methods for handling missing data (e.g. multiple imputation) and a sufficient length of follow‐up (at least two years).
History
Protocol first published: Issue 3, 2015
Acknowledgements
We thank the Cochrane Colorectal Cancer Group, and the Abdomen and Endocrine Network for their assistance. We thank Michaela Eikermann for her contribution to the protocol.
Appendices
Appendix 1. The Cochrane Library search strategy
CENTRAL, The Cochrane Library issue 2 2017 #1 MeSH descriptor: [Hernia, Ventral] explode all trees #2 (incision* or ventral or ventralis or abdomen or abdominal or umbilical or paraumbilical or epigastric* or spigel* or spiegel*) near/3 (herni* or herniorrhaph* or hernioplast*):ti,ab,kw #3 (#1 or #2) #4 MeSH descriptor: [Surgical Mesh] explode all trees #5 mesh:ti,ab,kw #6 (#4 or #5) #7 (#3 and #6)
Appendix 2. MEDLINE search strategy
Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present, 1 March 2017 1. exp Hernia, Ventral/ 2. ((incision* or ventral or ventralis or abdomen or abdominal or umbilical or paraumbilical or epigastric* or spigel* or spiegel*) adj3 (herni* or herniorrhaph* or hernioplast*)).mp. 3. 1 or 2 4. exp Surgical Mesh/ 5. mesh.mp. 6. 4 or 5 7. 3 and 6 8. randomized controlled trial.pt. 9. controlled clinical trial.pt. 10. randomized.ab. 11. placebo.ab. 12. clinical trials as topic.sh. 13. randomly.ab. 14. trial.ti. 15. 8 or 9 or 10 or 11 or 12 or 13 or 14 16. Exp animals/ not humans.sh. 17. 15 not 16 18. 7 and 17
Appendix 3. Embase search strategy
Ovid Embase 1974 to 2017 Week 09 1. *abdominal wall hernia/ 2. ((incision* or ventral or ventralis or abdomen or abdominal or umbilical or paraumbilical or epigastric* or spigel* or spiegel*) and (herni* or herniorrhaph* or hernioplast*)).m_titl. 3. 1 or 2 4. exp surgical mesh/ 5. mesh.mp. 6. 4 or 5 7. 3 and 6 8. CROSSOVER PROCEDURE.sh. 9. DOUBLE‐BLIND PROCEDURE.sh. 10. SINGLE‐BLIND PROCEDURE.sh. 11. (crossover* or cross over*).ti,ab. 12. placebo*.ti,ab. 13. (doubl* adj blind*).ti,ab. 14. allocat*.ti,ab. 15. trial.ti. 16. RANDOMIZED CONTROLLED TRIAL.sh. 17. random*.ti,ab. 18. 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 19. (exp animal/ or exp invertebrate/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans or man or men or wom?n).ti.) 20. 18 not 19 21. 7 and 20
Appendix 4. Criteria for judging risk of bias in the ‘Risk of bias’ assessment tool
|
RANDOM SEQUENCE GENERATION Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence. | |
| Criteria for a judgement of ‘Low risk’ of bias. | The investigators describe a random component in the sequence generation process such as:
*Minimization may be implemented without a random element, and this is considered to be equivalent to being random. |
| Criteria for the judgement of ‘High risk’ of bias. | The investigators describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, for example:
Other non‐random approaches happen much less frequently than the systematic approaches mentioned above and tend to be obvious. They usually involve judgement or some method of non‐random categorization of participants, for example:
|
| Criteria for the judgement of ‘Unclear risk’ of bias. | Insufficient information about the sequence generation process to permit judgement of ‘Low risk’ or ‘High risk’. |
|
ALLOCATION CONCEALMENT Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment. | |
| Criteria for a judgement of ‘Low risk’ of bias. | Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation:
|
| Criteria for the judgement of ‘High risk’ of bias. | Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on:
|
| Criteria for the judgement of ‘Unclear risk’ of bias. | Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement – for example if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed. |
|
BLINDING OF PARTICIPANTS AND PERSONNEL Performance bias due to knowledge of the allocated interventions by participants and personnel during the study. | |
| Criteria for a judgement of ‘Low risk’ of bias. | Any one of the following:
|
| Criteria for the judgement of ‘High risk’ of bias. | Any one of the following:
|
| Criteria for the judgement of ‘Unclear risk’ of bias. | Any one of the following:
|
|
BLINDING OF OUTCOME ASSESSMENT Detection bias due to knowledge of the allocated interventions by outcome assessors. | |
| Criteria for a judgement of ‘Low risk’ of bias. | Any one of the following:
|
| Criteria for the judgement of ‘High risk’ of bias. | Any one of the following:
|
| Criteria for the judgement of ‘Unclear risk’ of bias. | Any one of the following:
|
|
INCOMPLETE OUTCOME DATA Attrition bias due to amount, nature or handling of incomplete outcome data. | |
| Criteria for a judgement of ‘Low risk’ of bias. | Any one of the following:
|
| Criteria for the judgement of ‘High risk’ of bias. | Any one of the following:
|
| Criteria for the judgement of ‘Unclear risk’ of bias. | Any one of the following:
|
|
SELECTIVE REPORTING Reporting bias due to selective outcome reporting. | |
| Criteria for a judgement of ‘Low risk’ of bias. | Any of the following:
|
| Criteria for the judgement of ‘High risk’ of bias. | Any one of the following:
|
| Criteria for the judgement of ‘Unclear risk’ of bias. | Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’. It is likely that the majority of studies will fall into this category. |
|
OTHER BIAS Bias due to problems not covered elsewhere in the table. | |
| Criteria for a judgement of ‘Low risk’ of bias. | The study appears to be free of other sources of bias. |
| Criteria for the judgement of ‘High risk’ of bias. | There is at least one important risk of bias. For example, the study:
|
| Criteria for the judgement of ‘Unclear risk’ of bias. | There may be a risk of bias, but there is either:
|
Data and analyses
Comparison 1. Absorbable tacks compared to nonabsorbable tacks.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Recurrence (1 year to median 31 months) | 2 | 101 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.17, 3.22] |
| 1.2 Pain (VAS 0 ‐ 10, 1 day) | 1 | 51 | Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.58, 0.58] |
| 1.3 Pain (VAS 0 ‐ 100, 2 days) | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐11.80 [‐27.71, 4.11] |
| 1.4 Pain (VAS 0 ‐ 10, 2 week) | 1 | 51 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.01, 0.81] |
| 1.5 Pain (VAS 0 ‐ 10, 6 months) | 1 | 51 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐0.08, 1.08] |
| 1.6 Seroma (3 days) | 1 | 51 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.23, 2.54] |
| 1.7 Seroma (1 month) | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.62, 2.42] |
| 1.8 Infection (1 month) | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.03, 1.59] |
| 1.9 Length of hospital stay (days) | 1 | 51 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.19, 0.39] |
| 1.10 Duration of surgery (minutes) | 1 | 51 | Mean Difference (IV, Random, 95% CI) | 2.00 [‐27.68, 31.68] |
1.1. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 1: Recurrence (1 year to median 31 months)
1.3. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 3: Pain (VAS 0 ‐ 100, 2 days)
1.7. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 7: Seroma (1 month)
1.8. Analysis.

Comparison 1: Absorbable tacks compared to nonabsorbable tacks, Outcome 8: Infection (1 month)
Comparison 2. Nonabsorbable tacks compared to nonabsorbable sutures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Recurrence (6 months) | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.07, 14.79] |
| 2.2 Pain (VAS 0 ‐ 10, 1 week) | 1 | 53 | Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐1.79, 0.67] |
| 2.3 Pain (VAS 0 ‐ 10, 4 to 6 weeks) | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.4 Pain (VAS 0 ‐ 10, 6 to 12 months) | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.5 Length of hospital stay (3 to 4 days) | 1 | 53 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.25, 1.23] |
| 2.6 Duration of surgery (minutes) | 1 | 53 | Mean Difference (IV, Random, 95% CI) | ‐13.77 [‐16.04, ‐11.50] |
2.4. Analysis.

Comparison 2: Nonabsorbable tacks compared to nonabsorbable sutures, Outcome 4: Pain (VAS 0 ‐ 10, 6 to 12 months)
Comparison 3. Absorbable tacks compared to absorbable sutures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Recurrence (1 year) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 3.2 Pain (VAS 0 ‐ 10, sum 0 to 3 days) | 1 | 48 | Mean Difference (IV, Random, 95% CI) | ‐2.70 [‐6.67, 1.27] |
| 3.3 Pain (VAS 0 ‐ 10, 1 month) | 1 | 48 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.74, 0.14] |
| 3.4 Pain (VAS 0 ‐ 10, 6 months) | 1 | 48 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.42, 0.22] |
| 3.5 Severe postoperative complications | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 3.57 [0.45, 28.27] |
| 3.6 Reoperation (1 year) | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.17 [0.09, 50.74] |
| 3.7 Length of hospital stay (days) | 1 | 48 | Mean Difference (IV, Random, 95% CI) | 1.00 [‐0.88, 2.88] |
| 3.8 Seroma | 1 | 48 | Odds Ratio (M‐H, Random, 95% CI) | 0.33 [0.03, 3.95] |
3.1. Analysis.

Comparison 3: Absorbable tacks compared to absorbable sutures, Outcome 1: Recurrence (1 year)
3.4. Analysis.

Comparison 3: Absorbable tacks compared to absorbable sutures, Outcome 4: Pain (VAS 0 ‐ 10, 6 months)
3.8. Analysis.

Comparison 3: Absorbable tacks compared to absorbable sutures, Outcome 8: Seroma
Comparison 4. Nonabsorbable tacks plus nonabsorbable sutures compared to nonabsorbable sutures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Recurrence (2 years) | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 4.82 [0.24, 98.03] |
| 4.2 Pain (VAS 0 ‐ 10, 1 day) | 1 | 92 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.10, 1.30] |
| 4.3 Pain (VAS 0 ‐ 10, 1 week) | 1 | 92 | Mean Difference (IV, Random, 95% CI) | 0.60 [0.17, 1.03] |
| 4.4 Pain (VAS 0 ‐ 10, 1 months) | 1 | 92 | Mean Difference (IV, Random, 95% CI) | 0.80 [0.43, 1.17] |
| 4.5 Pain (VAS 0 ‐ 10, 3 months) | 1 | 92 | Mean Difference (IV, Random, 95% CI) | 0.30 [0.07, 0.53] |
| 4.6 Seroma (7 days) | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.25, 1.68] |
| 4.7 Mesh infection (postoperative not specified) | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 4.8 Time until return to normal activity (days) | 1 | 100 | Mean Difference (IV, Random, 95% CI) | 6.60 [2.89, 10.31] |
| 4.9 Length of hospital stay (days) | 1 | 110 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.20, 0.14] |
| 4.10 Duration of surgery (minutes) | 1 | 110 | Mean Difference (IV, Random, 95% CI) | ‐22.70 [‐29.14, ‐16.26] |
Comparison 5. Absorbable tacks plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Recurrence (2 years) | 1 | 77 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 5.2 Pain (VAS 0 ‐ 10, 3 months) | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.39, 0.19] |
| 5.3 Pain (VAS 0 ‐ 10, 6 months) | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.39, ‐0.01] |
| 5.4 Seroma (1 week) | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.24, 2.08] |
| 5.5 Seroma (1 months) | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.12, 3.80] |
| 5.6 Seroma (3 months) | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 5.7 Length of hospital stay (days) | 1 | 90 | Mean Difference (IV, Random, 95% CI) | 0.75 [‐0.32, 1.82] |
| 5.8 Duration of surgery (minutes) | 1 | 89 | Mean Difference (IV, Random, 95% CI) | 9.30 [‐0.68, 19.28] |
Comparison 6. Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Recurrence (3 months) | 2 | 185 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.07 [0.07, 17.24] |
| 6.2 Recurrence (2 years) | 1 | 63 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 2.82] |
| 6.3 Pain (VAS 0 ‐ 10, at rest, 4 hours) | 1 | 69 | Mean Difference (IV, Random, 95% CI) | ‐1.30 [‐2.34, ‐0.26] |
| 6.4 Pain (VAS 0 ‐ 10, coughing, 4 hours) | 1 | 69 | Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐2.73, ‐0.47] |
| 6.5 Pain (VAS 0 ‐ 100, 2 weeks) | 1 | 116 | Mean Difference (IV, Random, 95% CI) | ‐4.40 [‐12.17, 3.37] |
| 6.6 Pain (VAS 0 ‐ 10, at rest, 4 weeks) | 1 | 69 | Mean Difference (IV, Random, 95% CI) | 0.18 [0.13, 0.23] |
| 6.7 Pain (VAS 0 ‐ 10, coughing, 4 weeks) | 1 | 69 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.91, 0.87] |
| 6.8 Pain (VAS 0 ‐ 100, 6 weeks) | 1 | 116 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐6.76, 6.36] |
| 6.9 Pain (VAS 0 ‐ 10, at rest, 3 months) | 1 | 59 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.86, 0.10] |
| 6.10 Pain (VAS 0 ‐ 10, coughing, 3 months) | 1 | 59 | Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐1.11, 0.39] |
| 6.11 Pain (VAS 0 ‐ 100, 3 month) | 1 | 116 | Mean Difference (IV, Random, 95% CI) | ‐5.40 [‐11.79, 0.99] |
| 6.12 Seroma (3 month) | 2 | 186 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.16 [0.00, 8.10] |
| 6.13 Haematoma (post‐operative) | 2 | 186 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.09, 11.04] |
| 6.14 Length of hospital stay (days) | 2 | 186 | Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.63, 0.25] |
| 6.15 Duration of surgery (minutes) | 2 | 186 | Mean Difference (IV, Random, 95% CI) | ‐12.52 [‐27.20, 2.16] |
6.3. Analysis.

Comparison 6: Nonabsorbable tacks compared to nonabsorbable tacks plus nonabsorbable sutures, Outcome 3: Pain (VAS 0 ‐ 10, at rest, 4 hours)
Comparison 7. Nonabsorbable tacks plus absorbable sutures compared to nonabsorbable tacks.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Recurrence (3 month) | 1 | 116 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.07, 16.72] |
| 7.2 Pain (VAS 0 ‐ 100, 2 weeks) | 1 | 116 | Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐7.16, 6.16] |
| 7.3 Pain (VAS 0 ‐ 100, 6 weeks) | 1 | 116 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐8.03, 3.23] |
| 7.4 Pain (VAS 0 ‐ 100, 3 month) | 1 | 116 | Mean Difference (IV, Random, 95% CI) | ‐1.30 [‐5.49, 2.89] |
| 7.5 Seroma (3 month) | 1 | 116 | Risk Ratio (M‐H, Random, 95% CI) | 3.21 [0.13, 77.22] |
| 7.6 Haematoma (3 month) | 1 | 116 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.23, 5.09] |
| 7.7 Length of hospital stay (days) | 1 | 116 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.26, 1.06] |
| 7.8 Duration of surgery (minutes) | 1 | 116 | Mean Difference (IV, Random, 95% CI) | 13.50 [5.07, 21.93] |
Comparison 8. Nonabsorbable tack plus absorbable sutures compared to nonabsorbable tacks plus nonabsorbable sutures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Recurrence (3 month) | 1 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.12, 72.10] |
| 8.2 Pain (VAS 0 ‐ 100, 2 weeks) | 1 | 112 | Mean Difference (IV, Random, 95% CI) | ‐4.90 [‐11.92, 2.12] |
| 8.3 Pain (VAS 0 ‐ 100, 6 weeks) | 1 | 112 | Mean Difference (IV, Random, 95% CI) | ‐2.60 [‐7.66, 2.46] |
| 8.4 Pain (VAS 0 ‐ 100, 3 month) | 1 | 112 | Mean Difference (IV, Random, 95% CI) | ‐6.70 [‐12.90, ‐0.50] |
| 8.5 Seroma (3 month) | 1 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.12, 72.10] |
| 8.6 Haematoma (3 month) | 1 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.32, 27.97] |
| 8.7 Length of hospital stay (days) | 1 | 112 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.47, 0.87] |
| 8.8 Duration of surgery (minutes) | 1 | 112 | Mean Difference (IV, Random, 95% CI) | 6.90 [‐0.98, 14.78] |
Comparison 9. Nonabsorbable tacks compared to fibrin sealant.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Recurrence (1 year) | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.2 Pain (VAS 0 ‐ 100, 2 days) | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐15.92, 14.72] |
| 9.3 Seroma (30 days) | 2 | 88 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.54, 1.61] |
| 9.4 Haematoma (30 days) | 1 | 38 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.19, 2.91] |
| 9.5 Superficial infection (30 days) | 2 | 88 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.52, 1.74] |
9.1. Analysis.

Comparison 9: Nonabsorbable tacks compared to fibrin sealant, Outcome 1: Recurrence (1 year)
9.5. Analysis.

Comparison 9: Nonabsorbable tacks compared to fibrin sealant, Outcome 5: Superficial infection (30 days)
Comparison 10. Absorbable tacks compared to fibrin sealant.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 Recurrence (1 year) | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 70.30] |
| 10.2 Pain (VAS 0 ‐ 100, 2 days) | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐12.40 [‐27.60, 2.80] |
| 10.3 Infection (1 month) | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.07, 15.12] |
| 10.4 Seroma (1 months) | 1 | 50 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.33, 3.06] |
10.4. Analysis.

Comparison 10: Absorbable tacks compared to fibrin sealant, Outcome 4: Seroma (1 months)
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bansal 2012.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India Study dates Between May 2007 and December 2011 |
|
| Participants |
Inclusion criteria Non‐recurrent primary or incisional ventral hernia (defect size of 2 ‐ 5 cm) without significant comorbidity Patient characteristics (nonabsorbable tacks with nonabsorbable sutures (55) / nonabsorbable sutures only (55)) Age (mean, SD): 45.9 (10.6) / 44.6 (13.6) Gender (male, %): 21.8 / 40.0 BMI (kg/m2, mean, SD): 29.3 (5.0) / 28.2 (5.3) Hernia type (incisional, %): 61.8 / 58.2 Hernia size (mean, SD, cm2): 189.7 (71.5) / 178.5 (70.8) Comorbidity: NR |
|
| Interventions | Intervention/control: suture (transfascial) fixation with nonabsorbable tacks (double crown, 1 – 2 cm distance) versus suture fixation (polypropylene) Mesh: heavyweight polypropylene mesh Intra‐abdominal mesh position: NR Surgical approach: laparoscopic |
|
| Outcomes | Recurrence (follow‐up 2 years), pain, return to activity, local infection, seroma, haematoma, length of hospital stay, duration of surgery | |
| Notes |
Funding source(as originally reported) Not reported Declarations of interest for the primary investigators (as originally reported) Virinder Kumar Bansal and Vimi Rewari have no conflict of interest or financial ties to report Data for sensitivity analyses Randomised: 55/55 Analysed: 54/52 Imputed in ITT sensitivity analysis: 1/3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done by using computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon not blinded. Other caregivers and participants unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Tendentially recurrence "lower risk" (objective outcome), pain "higher risk" (subjective outcome) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on missing data and reasons for dropout |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it seems that the published reports include all expected outcomes, including those that were prespecified |
| Other bias | Low risk | None detected |
Bansal 2016.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Department of Surgical Disciplines, All India Institute of Medical Sciences, New Delhi, India Study dates Between May, 2012 to April, 2014 |
|
| Participants |
Inclusion criteria Non‐recurrent primary or incisional ventral hernia (≤ 15 cm) without significant comorbidity Patient characteristics (absorbable tacks and absorbable sutures (45) / nonabsorbable tacks and nonabsorbable sutures (45)) Age (mean, SD): 47.2 (11.4) / 45.9 (12.5) Gender (male, %): 20.0 / 31.1 BMI (kg/m2, mean, SD): 25.2 (3.8) / 26.2 (5.2) Hernia type (incisional, %): 75.6 / 75.6 Hernia size (mean, SD, cm2): 33.6 (45.4) / 42.6 (59.1) Comorbidity: No significant comorbidity |
|
| Interventions | Intervention/control: absorbable tacks (double crown, 1.5 – 2 cm distance) and absorbable sutures compared to nonabsorbable tacks (double crown, 1.5 – 2 cm distance) and nonabsorbable sutures Mesh: Polypropylene‐polyglecaprone composite flexible mesh Intra‐abdominal mesh position: NR Surgical approach: laparoscopic |
|
| Outcomes | Recurrence (follow‐up 2 years), pain, return to activity, local infection, seroma, length of hospital stay, duration of surgery, quality of life | |
| Notes |
Funding source(as originally reported) Not reported. Declarations of interest for the primary investigators (as originally reported) The authors declare no conflicts of interest Data for sensitivity analyses Randomised: 45/45 Analysed: 39/38 Imputed in ITT sensitivity analysis: 6/7 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done by using computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon not blinded. Other caregivers and participants unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Observer blinded at follow‐up visits so recurrence etc "low risk" (objective outcome), pain "higher risk" (subjective outcome) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reasons for dropout not reported |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it seems that the published reports include all expected outcomes, including those that were prespecified |
| Other bias | Low risk | None detected |
Beldi 2011.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Department of Visceral Surgery and Medicine, Bern University Hospital, University of Bern, Switzerland Study dates Between April 2005 and January 2008 |
|
| Participants |
Inclusion criteria Primary or incisional ventral hernia (≤ 8 cm diameter) Patient characteristics (nonabsorbable tacks (18) / nonabsorbable suture (18)) Age (median, range): 55 (34 – 75) / 60 (40 – 79) Gender (male, %): 62.5 / 83.3 BMI (kg/m2, mean, range): 28.7 (24.2 – 35.4) / 28.4 (23.6 – 35.9) Hernia type (incisional, %): 61 / 56 Hernia size (mean, cm2): 12.6 / 12.6 Comorbidity: NR |
|
| Interventions | Intervention/control: nonabsorbable tacks (every 5 cm) versus nonabsorbable sutures Mesh: composite mesh Intra‐abdominal mesh position: NR Surgical approach: laparoscopic |
|
| Outcomes | Recurrence (6 months), pain, length of hospital stay, duration of surgery | |
| Notes |
Funding source(as originally reported) The study was funded by Sofradim/Covidien. We thank Brigitte Wanner for meticulous data collection, control of data, and analysis of radiographs Declarations of interest for the primary investigators (as originally reported) Guido Beldi and Daniel Candinas have no conflicts of interest or financial ties to disclose Data for sensitivity analyses Randomised: 20/20 Analysed: 18/18 Imputed in ITT sensitivity analysis: 2/2 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permutated blocks of 20 |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon not blinded. Other caregivers and participants unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Tendentially recurrence "lower risk" (objective outcome), pain "higher risk" (subjective outcome) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Intention‐to‐treat according authors but not all randomised participants were analysed, imputation method unclear and no reasons for dropout reported |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it seems that the published reports include all expected outcomes, including those that were prespecified |
| Other bias | Low risk | None detected |
Colak 2015.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Department of General Surgery, Samsun Training and Research Hospital, Turkey Study dates Between December 2010 and June 2014 |
|
| Participants |
Inclusion criteria Midline incisional ventral hernia (laparoscopic), no conversion to open surgery, no urgent surgery Patient characteristics (absorbable tacks (26) / nonabsorbable tacks (25)) Age (mean, SD): 50.7 (9.9) / 56.1 (11.8) Gender (male, %): 34.6 / 40.0 BMI (kg/m2, mean, SD): 32.9 (4.6) / 35.4 (5.1) Hernia type (incisional, %): 100 / 100 Hernia size (mean, cm2): 67.0 (23.1) / 62.9 (22.4) Comorbidity (n): Diabetes: 7 / 6 Hypertension: 6 / 3 Asthma: 6 / 4 Coronary artery disease: 1 / 2 |
|
| Interventions | Intervention/control: absorbable tacks (helical, 1.5 – 2 cm distance) versus nonabsorbable tacks (helical, 1.5 – 2 cm distance) Mesh: composite mesh Intra‐abdominal mesh position: NR Surgical approach: laparoscopic |
|
| Outcomes | Recurrence (follow‐up 1 year), pain (primary outcome), seroma, haematoma, length of hospital stay, duration of surgery | |
| Notes |
Funding source(as originally reported) Not reported. Declarations of interest for the primary investigators (as originally reported) None Data for sensitivity analyses Randomised: 25/26 Analysed: 25/26 No ITT sensitivity analysis performed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated by a computer |
| Allocation concealment (selection bias) | Low risk | Allocation according to numbers given to the surgeon just before operation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon not blinded. Other caregivers and participants unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Tendentially recurrence "lower risk" (objective outcome), pain "higher risk" (subjective outcome) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of allocated participants equal to number of analysed participants. But no information on missing data |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it seems that the published reports include all expected outcomes, including those that were prespecified |
| Other bias | Low risk | None detected |
Eriksen 2011.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Three centres, Denmark Study dates Between August 2009 and March 2010 |
|
| Participants |
Inclusion criteria Primary or recurrent umbilical hernia (1.5 to 5 cm) and anaesthesiologists grade I – III Patient characteristics (nonabsorbable tacks (19) / fibrin sealant (19)) Age (median, range): 45 (31 – 67) / 59 (34 – 69) Gender (male, %): 68.4 / 73.7 BMI (kg/m2, mean, range): 31.1 (24.8 – 38.8) / 31.2 (19.0 – 38.3) Hernia type (recurrent): 5 / 2 Hernia size: NR Comorbidity: NR |
|
| Interventions | Intervention/control: nonabsorbable tacks (double crown, 1 – 2 cm distance) versus fibrin sealant Mesh: composite mesh Intra‐abdominal mesh position: NR Surgical approach: laparoscopic |
|
| Outcomes | Recurrence (follow‐up 1 year), pain (primary outcome), return to activity, local infection, seroma, haematoma, length of hospital stay, duration of surgery | |
| Notes |
Funding source(as originally reported) The study was supported by a grant from Baxter Healthcare Corporation, Bioscience Division. Declarations of interest for the primary investigators (as originally reported) The authors declare no conflict of interest Data for sensitivity analyses Randomised: 20/20 Analysed: 19/19 Imputed in ITT sensitivity analysis: 1/1 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation was performed. The randomisation sequence was generated by a computer |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Surgeon not blinded. All other caregivers and participants blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Those assessing the outcome parameters were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reported ITT analysis but not all randomised participants analysed. It is reported that there are no people lost to follow‐up. Which participants are included in the analysis/not included in the analysis is unclear (e.g. received treatment, complete baseline assessment). No information on imputation method |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it seems that the published reports include all expected outcomes, including those that were prespecified |
| Other bias | Low risk | None detected |
Harsløf 2018.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Three surgical hospital departments (Horsens, Randers, Aarhus), Denmark Study dates Between March 2013 to March 2016 |
|
| Participants |
Inclusion criteria
Exclusion criteria
Patient characteristics (nonabsorbable tacks (25) / absorbable tacks (25) / fibrin sealant (25)) Age (mean, SD): 58.1 (11.2) / 60.2 (10.8) / 56.7 (9.8) Gender (male, %): 18 (72.0%) / 15 (60.0%) / 21 (84.0%) BMI (kg/m2, mean, range): 29.9 (3.8) / 28.8 (4.0) / 29.2 (3.8) Hernia type (incisional, %): 4 (16.0%) / 6 (24.0%) / 9 (36.0%) Hernia size (mean, SD, cm2): 3.0 (1.0) / 3.3 (1.3) / 3.0 (1.0) Comorbidity: NR |
|
| Interventions | Intervention/control: nonabsorbable tacks compared to absorbable tacks compared to fibrin sealant (25) Mesh: composite, lightweight, large‐pore, polypropylene mesh Intra‐abdominal mesh position: NR Surgical approach: laparoscopic |
|
| Outcomes | Recurrence, pain (primary outcome), HRQOL, postoperative complications | |
| Notes |
Funding source(as originally reported) Not reported. Declarations of interest for the primary investigators (as originally reported) The authors declare that they have no conflict of interest. Data for sensitivity analyses Randomised: 25/25/25 Analysed: 23/20/21 Imputed in ITT sensitivity analysis: 2/5/4 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was generated by a computer |
| Allocation concealment (selection bias) | Low risk | Randomisation was generated by a computer |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Nurses and participants are blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, nurses, and persons assessing the outcome parameters were blinded to the group assignment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Intention‐to‐treat according to authors, but use of Last‐Observation‐Carried forward. Reasons for dropout not reported for each group |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the study registry entry are reported |
| Other bias | Low risk | None detected |
Langenbach 2020.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Department of Surgery, Helios St. Elisabeth Klinik Oberhausen, Germany Study dates Between January 2016 until January 2018 |
|
| Participants |
Inclusion criteria Abdominal wall hernia needing open surgery, written informed consent, no co‐existing chronic diseases with permanent use of analgesics, no neuro‐muscular diseases with chronic pain sensation, no emergency operations or other simultaneous interventions, no pregnancy or patients with previous IPOM procedure Patient characteristics (absorbable tacks (28) / absorbable sutures (20)) Age (mean, SD): 62.2 (15.3), 61.4 (12.8) Gender (male, %): 11 (39%) / 8 (40%) BMI (kg/m2, mean, range): 34.0 (6.6) / 31.2 (6.3) Hernia type (incisional, %): 20 (71%) / 17 (85%) Hernia size (median, range): 33 (4 – 204) / 46 (4 – 616) Comorbidity:
|
|
| Interventions | Intervention/control: absorbable tacks (2 cm distance) compared to absorbable sutures (2 cm distance) Mesh: composite mesh Intra‐abdominal mesh position: IPOM Surgical approach: open |
|
| Outcomes | Recurrence (1 year), pain (primary outcome), HRQOL, return to activity, postoperative complications, duration of surgery | |
| Notes |
Funding source(as originally reported) Not reported. Declarations of interest for the primary investigators (as originally reported) There is no conflict of interests Data for sensitivity analyses Randomised: 28/20 Analysed: not reported Imputed in ITT sensitivity analysis: not applicable |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random list |
| Allocation concealment (selection bias) | Low risk | Group allocations were stored in sequentially‐numbered opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon not blinded. Other caregivers and participants unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Tendentially recurrence "lower risk" (objective outcome), pain "higher risk" (subjective outcome) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it seems that the published reports include all expected outcomes, including those that were prespecified |
| Other bias | Low risk | None detected |
Muysoms 2013.
| Study characteristics | ||
| Methods | Randomised controlled trial Location International multicenter, Spain and Belgium Study dates Between December 2004 and July 2008 |
|
| Participants |
Inclusion/exclusion criteria Primary and incisional ventral hernias. Parastomal hernias and all hernias close to bony structures, like suprapubic, subxiphoidal, subcostal hernias, and lumbar hernias were excluded Patient characteristics (nonabsorbable tacks with nonabsorbable sutures (43) / nonabsorbable tacks only (33)) Age (mean, SD): 56.7 (16.2) / 59.8 (9.4) Gender (male, %): 52 / 59 BMI (kg/m2, mean, range): 29.6 (6.5) / 29.3 (4.7) Hernia type (incisional, %): 72 / 78 Hernia size (mean, SD, cm2): 45.6 (50.6) / 46.5 (55.4) Comorbidity: NR |
|
| Interventions | Intervention/control: nonabsorbable tacks (1 – 2 cm distance) with nonabsorbable sutures compared to nonabsorbable tacks (double crown, 1 – 2 cm distance) Mesh: different meshes in the centres Intra‐abdominal mesh position: intra‐peritoneal Surgical approach: laparoscopic |
|
| Outcomes | Recurrence (follow‐up 2 years), pain (primary outcome), return to activity, local infection, seroma, haematoma, length of hospital stay, duration of surgery | |
| Notes |
Funding source(as originally reported) This study was performed with a research grant from WL Gore & Ass, Flagstaff, USA Declarations of interest for the primary investigators (as originally reported) The co‐authors declare no conflict of interest. Data for sensitivity analyses Randomised: 43/33 Analysed: 36/27 Imputed in ITT sensitivity analysis: 7/6 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | MS Excel random function |
| Allocation concealment (selection bias) | Low risk | Allocation of a specific participant was sent to the surgeon after receiving the informed consent |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon not blinded. Other caregivers and participants unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported. Tendentially recurrence "lower risk" (objective outcome), pain "higher risk" (subjective outcome) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not all randomised participants analysed. No information on reasons for dropout |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it seems that the published reports include all expected outcomes, including those that were prespecified |
| Other bias | Low risk | None detected |
Shaukat 2018.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Surgery Department of Dow University Hospital, Dow University of Health Sciences, Karachi, Sindh, Pakistan Study dates Between January 2015 to December 2016 |
|
| Participants |
Inclusion/exclusion criteria Ventral hernias (non‐ obstructed or strangulated) Patient characteristics (nonabsorbable sutures (30) / nonabsorbable tacks (23)) Age (mean, SD): 46.47 (8.17) / 31.32 (4.49) Gender (male, %): 8 (26.7%) / 0 BMI (kg/m2, mean, SD): 42.04 (9.0) / 28.37 (5.35) Hernia type (incisional, %): 12 (40.0%) / 9 (39.1%) Hernia size (≥ 4 cm cm2): 26 (86.7%) / 13 (56.5%) Comorbidity: NR |
|
| Interventions | Intervention/control: nonabsorbable tacks versus nonabsorbable sutures Mesh: NR Intra‐abdominal mesh position: onlay Surgical approach: Open |
|
| Outcomes | Pain, length of hospital stay, duration of surgery | |
| Notes |
Funding source(as originally reported) Not reported Declarations of interest for the primary investigators (as originally reported) Not reported Data for sensitivity analyses Randomised: 30/23 Analysed: not reported. Imputed in ITT sensitivity analysis: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported, imbalance in participant characteristics suggests problem with randomisation |
| Allocation concealment (selection bias) | Unclear risk | No information reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon not blinded. Other caregivers and participants unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on amount of dropouts reported |
| Selective reporting (reporting bias) | High risk | Outcomes that are expected to be reported, like recurrence or postoperative complications are not stated in the publication |
| Other bias | Low risk | None detected |
Wassenaar 2010.
| Study characteristics | ||
| Methods | Randomised controlled trial Location Not reported Study dates Between August 2005 and July 2008 |
|
| Participants |
Inclusion criteria Primary and incisional ventral hernia Patient characteristics (nonabsorbable tacks with absorbable sutures (56) / nonabsorbabletacks only (60) / nonabsorbable tacks with nonabsorbable sutures (56)) Age (mean, SD): 54.7 (12.9) / 51.6 (13.8) / 52.4 (12.7) Gender (male, %): 69.6 / 55.0 / 64.3 BMI (kg/m2, mean, range): 29.1 (4.9) / 28.7 (5.4) / 29.9 (5.7) Hernia type (incisional, %): 35.7 / 35.0 / 30.4 Hernia size (mean, SD, cm2): 23.4 (61.5) / 22.5 (56.1) / 11.3 (29.6) Comorbidity: NR |
|
| Interventions | Intervention/control: nonabsorbable tacks (1 – 2 cm distance) plus absorbable sutures compared to nonabsorbable tacks (double crown, 1 – 1.5 cm distance) compared to nonabsorbable tacks (1 – 2 cm distance) plus nonabsorbable sutures Mesh: polytetrafluoroethylene mesh Intraabdominal mesh position: NR Surgical approach: laparoscopic |
|
| Outcomes | Recurrence (3 months), pain (primary outcome), HRQOL, return to activity, local infection, seroma, haematoma, length of hospital stay, duration of surgery | |
| Notes |
Funding source(as originally reported) WL Gore & Associates, Flagstaff, AZ, provided financial support for preparation of the manuscript. Declarations of interest for the primary investigators (as originally reported) Eelco Wassenaar and Srdjan Rakic have no conflicts of interest or financial ties to disclose Data for sensitivity analyses Randomised: 66/68/65 (received intervention: 57/63/57) Analysed: 56/60/56 Imputed in ITT sensitivity analysis: 1/3/1 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised random generation |
| Allocation concealment (selection bias) | Low risk | Generation of a number just before the operation. The number was given to the surgeon, who then used the mesh‐fixation technique previously assigned to that number |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon not blinded. Other caregivers unclear, participants blinded until they requested allocation information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported.Tendentially recurrence "lower risk" (objective outcome), pain "higher risk" (subjective outcome) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not all randomised participants analysed. Reaons for dropout/discontinuation not reported for all participants |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it seems that the published reports include all expected outcomes, including those that were prespecified |
| Other bias | Low risk | None detected |
ASA: American Society of Anesthesiologists; BMI: body mass index; HRQOL: health‐related quality of life; SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Afifi 2005 | Non‐randomised study |
| Ambore 2017 | Non‐randomised study: Study participants are selected randomly, but not randomly allocated |
| Ammar 2010 | Intervention/control: mesh repair compared to suture repair. No comparisons of different mesh fixation methods |
| Korenkov 2002 | Intervention: use of different fixation is linked to use of different implants |
| Navarra 2007 | Intervention/control: laparoscopic versus open repair |
| Pawlak 2015 | Comparison: use of different mesh materials and fixation methods at the same time |
| Polat 2005 | Intervention/control: comparison of different intra‐abdominal mesh positions |
| Stabilini 2013 | Intervention/control: laparoscopic bridging (mesh repair) compared to open anatomical reconstruction (no mesh) |
| Venclauskas 2010 | Intervention/control: comparison of different intra‐abdominal mesh positions |
| Wéber 2010 | Intervention/control: comparison of different intra‐abdominal mesh positions and mesh compared to suture (2 factorial design) |
Characteristics of studies awaiting classification [ordered by study ID]
Misra 2015.
| Methods | RCT |
| Participants | ventral and incisional hernias |
| Interventions | absorbable tacks compared to nonabsorbable tacks |
| Outcomes | ‐ |
| Notes | ‐ |
Characteristics of ongoing studies [ordered by study ID]
CTRI/2019/05/019115.
| Study name | ‐ |
| Methods | RCT |
| Participants | Ventral hernia repair |
| Interventions | absorbable tacks compared to nonabsorbable tacks |
| Outcomes | ‐ |
| Starting date | ‐ |
| Contact information | ‐ |
| Notes | ‐ |
NCT01109771.
| Study name | ‐ |
| Methods | RCT |
| Participants | Primary, incisional or recurrent midline ventral hernia requiring elective laparoscopic repair |
| Interventions | Permanent mesh fixation compared to absorbable mesh fixation |
| Outcomes | Pain, recurrence |
| Starting date | December 2014 |
| Contact information | ‐ |
| Notes | ‐ |
NCT03429374.
| Study name | ‐ |
| Methods | RCT |
| Participants | Patient with midline ventral hernia (primary or incisional) with a defect size between 2 and 5 cm and eligible for laparoscopic repair |
| Interventions | Mesh fixation with tacks compared to mesh fixation with glue |
| Outcomes | Pain, recurrence |
| Starting date | 12 February 2018 |
| Contact information | ‐ |
| Notes | ‐ |
Silecchia 2015.
| Study name | ‐ |
| Methods | RCT |
| Participants | Ventral and incisional hernias |
| Interventions | Absorbable tacks compared to nonabsorbable tacks |
| Outcomes | Pain, recurrence |
| Starting date | June 2014 |
| Contact information | ‐ |
| Notes | ‐ |
Differences between protocol and review
We did not apply the double data entry method for all data. Data of participant, intervention and study characteristics were only extracted by one review author and verified by a second review author. Data extraction of outcomes was done by one review author (TM) directly into Revman, and another review author entered data into a Word‐sheet (MW, BP). We subsequently aligned the results.
We searched Embase and MEDLINE via Ovid, instead of Embase and Pubmed, respectively.
Where there were very few studies available for the meta‐analysis (four or fewer) we pooled the outcomes, even if the I2 statistic was above our prespecified threshold, because heterogeneity estimates are not reliable in this situation.
Contributions of authors
Tim Mathes: idea for the review, data extraction, risk of bias assessment, GRADE assessment, analyses and interpretation of data, preparation of the manuscript.
Barbara Prediger: data extraction, risk of bias assessment, GRADE assessment, revision of the manuscript.
Maren Walgenbach: idea for the review, data extraction, risk of bias assessment, revision of the manuscript.
Robert Siegel: clinical advice, interpretation of data, preparation and revision of the manuscript.
Sources of support
Internal sources
-
None, Germany
Not applicable
External sources
-
None, Other
Not applicable
Declarations of interest
Tim Mathes: no conflict of interest.
Maren Walgenbach: no conflict of interest.
Barbara Prediger: no conflict of interest.
Robert Siegel: no conflict of interest.
New
References
References to studies included in this review
Bansal 2012 {published data only}
- Bansal VK, Misra MC, Babu D, Singhal P, Rao K, Sagar R, et al. Comparison of long-term outcome and quality of life after laparoscopic repair of incisional and ventral hernias with suture fixation with and without tacks: a prospective, randomized, controlled study. Surgical Endoscopy 2012;26(12):3476-85. [DOI: 10.1007/s00464-012-2390-5] [DOI] [PubMed] [Google Scholar]
- Bansal VK, Misra MC, Kumar S, Rao YK, Singhal P, Goswami A, et al. A prospective randomized study comparing suture mesh fixation versus tacker mesh fixation for laparoscopic repair of incisional and ventral hernias. Surgical Endoscopy 2011;25(5):1431-8. [DOI: 10.1007/s00464-010-1410-6] [DOI] [PubMed] [Google Scholar]
Bansal 2016 {published data only}
- Bansal VK, Asuri K, Panaiyadiyan S, Kumar S, Subramaniam R, Ramachandran R, et al. Comparison of absorbable versus nonabsorbable tackers in terms of long-term outcomes, chronic pain, and quality of life after laparoscopic incisional hernia repair: a randomized study. Surgical Laparoscopy Endoscopy and Percutaneous Techniques 2016;26(6):476-83. [DOI] [PubMed] [Google Scholar]
Beldi 2011 {published data only}
- Beldi G, Wagner M, Bruegger LE, Kurmann A, Candinas D. Mesh shrinkage and pain in laparoscopic ventral hernia repair: a randomized clinical trial comparing suture versus tack mesh fixation. Surgical Endoscopy 2011;25(3):749-55. [DOI: 10.1007/s00464-010-1246-0] [DOI] [PubMed] [Google Scholar]
Colak 2015 {published data only}
- Colak E, Ozlem N, Kucuk G, Aktimur R, Kesmer S, Yildirim K. Prospective randomized trial of mesh fixation with absorbable versus nonabsorbable tacker in laparoscopic ventral incisional hernia repair. International Journal of Clinical Experimental Medicine 2015;8(11):21611-6. [PMC free article] [PubMed] [Google Scholar]
Eriksen 2011 {published data only}
- Eriksen JR, Bisgaard T, Assaadzadeh S, Jorgensen LN, Rosenberg J. Fibrin sealant for mesh fixation in laparoscopic umbilical hernia repair: 1-year results of a randomized controlled double-blinded study. Hernia 2013;17(4):511-4. [10.1007/s10029-013-1101-z] [DOI] [PubMed] [Google Scholar]
- Eriksen JR, Bisgaard T, Assaadzadeh S, Jorgensen LN, Rosenberg J. Randomized clinical trial of fibrin sealant versus titanium tacks for mesh fixation in laparoscopic umbilical hernia repair. British Journal of Surgery 2011;98(11):1537-45. [DOI: 10.1002/bjs.7646] [DOI] [PubMed] [Google Scholar]
Harsløf 2018 {published data only}
- Harsløf S, Krum‐Moller P, Sommer T, Zinther N, Wara P, Friis‐Andersen H. Effect of fixation devices on postoperative pain after laparoscopic ventral hernia repair: a randomized clinical trial of permanent tacks, absorbable tacks, and synthetic glue. Langenbeck's Archives of Surgery 2018;403(4):529-37. [DOI: 10.1007/s00423-018-1676-z] [DOI] [PubMed] [Google Scholar]
Langenbach 2020 {published data only}
- Langenbach MR, Enz D. Mesh fixation in open IPOM procedure with tackers or sutures? a randomized clinical trial with preliminary results. Hernia 2020;24(1):79-84. [DOI: 10.1007/s10029-019-01991-z] [DOI] [PubMed] [Google Scholar]
Muysoms 2013 {published data only}
- Muysoms F, Vander Mijnsbrugge G, Pletinckx P, Boldo E, Jacobs I, Michiels M, et al. Randomized clinical trial of mesh fixation with "double crown" versus "sutures and tackers" in laparoscopic ventral hernia repair. Hernia 2013;17(5):603-12. [DOI: 10.1007/s10029] [DOI] [PubMed] [Google Scholar]
Shaukat 2018 {published data only}
- Shaukat N, Jaleel F, Jawaid M, Zulfiqar I. Is there difference in chronic pain after suture and stapler fixation method of mesh in ventral hernia? Is stapler fixation method quicker? a randomized controlled trial. Pakistan Journal of Medical Sciences 2018;34(1):175-18. [DOI: 10.12669/pjms.341.13904] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wassenaar 2010 {published data only}
- Wassenaar E, Schoenmaeckers E, Raymakers J, Van der Palen J, Rakic S. Mesh-fixation method and pain and quality of life after laparoscopic ventral or incisional hernia repair: a randomized trial of three fixation techniques. Surgical Endoscopy 2010;24(6):1296-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Afifi 2005 {published data only}
- Afifi RY. A prospective study between two different techniques for the repair of a large recurrent ventral hernia: a double mesh intraperitoneal repair versus onlay mesh repair. Hernia 2005;9(4):310-5. [DOI] [PubMed] [Google Scholar]
Ambore 2017 {published data only}
- Ambore VK, More JP, Bhandarwar AH, Gandhi SS, Patel CB, Taori R. Comparative study of tacker vs glue fixation of mesh in laparoscopic intraperitoneal onlay mesh repair of ventral hernias. World Journal of Laparoscopic Surgery 2017;10(3):87-90. [DOI: 10.5005/jp-journals-10033-1312] [DOI] [Google Scholar]
Ammar 2010 {published data only}
- Ammar SA. Management of complicated umbilical hernias in cirrhotic patients using permanent mesh: randomized clinical trial. Hernia. Hernia 2010;14(1):35-8. [DOI: 10.1007/s10029-009-0556-4] [DOI] [PubMed] [Google Scholar]
Korenkov 2002 {published data only}
- Korenkov M, Sauerland S, Arndt M, Bograd L, Neugebauer EA, Troidl H. Randomized clinical trial of suture repair, polypropylene mesh or autodermal hernioplasty for incisional hernia. British Journal of Surgery 2002;89(1):50-6. [DOI] [PubMed] [Google Scholar]
Navarra 2007 {published data only}
- Navarra G, Musolino C, De Marco ML, Bartolotta M, Barbera A, Centorrino T. Retromuscular sutured incisional hernia repair: a randomized controlled trial to compare open and laparoscopic approach. Surgical Laparoscopy Endoscopy & Percutaneous Techniques 2007;17(2):86-90. [DOI] [PubMed] [Google Scholar]
Pawlak 2015 {published data only}
- Pawlak M, Hilgers R-D, Bury K, Lehmann A, Owczuk R, Śmietański M. Comparison of two different concepts of mesh and fixation technique in laparoscopic ventral hernia repair: a randomized controlled trial. Surgical Endoscopy 2015;30(3):1188–97. [DOI] [PubMed] [Google Scholar]
Polat 2005 {published data only}
- Polat C, Dervisoglu A, Senyurek G, Bilgin M, Erzurumlu K, Ozkan K. Umbilical hernia repair with the prolene hernia system. American Journal of Surgery 2005;190(1):61-4. [DOI] [PubMed] [Google Scholar]
Stabilini 2013 {published data only}
- Stabilini C, Bracale U, Pignata G, Frascio M, Casaccia M, Pelosi P, et at. Laparoscopic bridging vs. anatomic open reconstruction for midline abdominal hernia mesh repair [LABOR]: single-blinded, multicenter, randomized, controlled trial on long-term functional results. Trials 2013;14(357):n.a.. [DOI: 10.1186/1745-6215-14-357] [DOI] [PMC free article] [PubMed] [Google Scholar]
Venclauskas 2010 {published data only}
- Venclauskas L, Maleckas A, Kiudelis M. One-year follow-up after incisional hernia treatment: results of a prospective randomized study. Hernia 2010;14(6):575-82. [DOI: 10.1007/s10029-010-0686-8] [DOI] [PubMed] [Google Scholar]
Wéber 2010 {published data only}
- Wéber G, Baracs J, Horváth OP. "Onlay" mesh provides significantly better results than "sublay" reconstruction. Prospective randomized multicenter study of abdominal wall reconstruction with sutures only, or with surgical mesh--results of a five-years follow-up [Kedvezőbb műtéti eredmények „onlay” hálóval,mint „sublay” helyzetben beültetettelVarrattal, illetve hálóbeültetéssel történő hasfal-rekonstrukció prospektív,randomizált, multicentrikus vizsgálata – ötéves utánkövetés eredményei]. Magyar Sebeszet 2010;65(5):302-11. [DOI: 10.1556/MaSeb.63.2010.5.3] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Misra 2015 {unpublished data only}
- Misra MC et al. PROSPECTIVE RANDOMIZED CONTROLLED. In: Congress of EHS and AHS 2015. Vol. CO13:12. 2015.
References to ongoing studies
CTRI/2019/05/019115 {published data only}
- CTRI/2019/05/019115. Assessment of patient outcomes and surgeons difficulty in two techniques of endoscopic hernia managament.
NCT01109771 {published data only}
- NCT01109771. Absorbable versus permanent mesh fixation trial in laparoscopic midline ventral hernia repair (SORBET). clinicaltrials.gov/ct2/show/NCT01109771 (first received 23 April 2010).
NCT03429374 {published data only}
- NCT03429374. Tacks versus glue for mesh fixation in laparoscopic ventral hernia repair treating defects between 2 and 5 cm width. clinicaltrials.gov/ct2/show/NCT03429374.
Silecchia 2015 {published data only}
- Silecchia G, Cavallaro G, Raparelli L, Olmi S, Baldazzi G, Campanile F. Titanium versus absorbable tacks comparative study (TACS): a multicenter, non-inferiority prospective evaluation during laparoscopic repair of ventral and incisional hernia: study protocol for randomized controlled trial. Trials 2015;16(1):249. [NCT02076984] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abdel‐Baki 2007
- Abdel-Baki NA, Bessa SS, Abdel-Razek AH. Comparison of prosthetic mesh repair and tissue repair in the emergency management of incarcerated para-umbilical hernia: a prospective randomized study. Hernia 2007;11(2):163-7. [DOI] [PubMed] [Google Scholar]
Archampong 2012
- Archampong D, Borowski D, Wille-Jørgensen P, Iversen LH. Workload and surgeon´s specialty for outcome after colorectal cancer surgery. Cochrane Database of Systematic Reviews 2012, Issue 3. Art. No: CD005391. [DOI: 10.1002/14651858.CD005391] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 2018
- Baker JJ, Oberg S, Andresen K, Klausen TW, Rosenberg J. Systematic review and network meta-analysis of methods of mesh fixation during laparoscopic ventral hernia repair. British Journal of Surgery 2018;105(1):37-47. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ballem 2008
- Ballem N, Parikh R, Berber E, Siperstein A. Laparoscopic versus open ventral hernia repairs: 5 year recurrence rates. Surgical Endoscopy 2008;22(9):1935-40. [DOI: 10.1007/s00464-008-9981-1] [DOI] [PubMed] [Google Scholar]
Bansal 2011
- Bansal VK, Misra MC, Kumar S, Rao YK, Singhal P, Goswami A, et al. A prospective randomized study comparing suture mesh fixation versus tacker mesh fixation for laparoscopic repair of incisional and ventral hernias. Surgical Endoscopy 2011;25(5):1431-8. [DOI: 10.1007/s00464-010-1410-6] [DOI] [PubMed] [Google Scholar]
Bellows 2013
- Bellows CF, Smith A, Malsbury J, Helton WS. Repair of incisional hernias with biological prosthesis: a systematic review of current evidence. American Journal of Surgery 2013;205(1):85-101. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bittner 2019
- Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D, et al. Update of guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-Part A. Surgical Endoscopy 2019;33(10):3069-139. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Breivik 2008
- Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. British Journal of Anaesthesia 2008;101(1):17-24. [PMID: ] [DOI] [PubMed] [Google Scholar]
Carbonell 2003
- Carbonell AM, Matthews BD, Kercher KW, Heniford BT. Technique for introducing large composite mesh while performing laparoscopic incisional hernioplasty. Surgical Endoscopy 2003;17(9):1506. [DOI: 10.1007/s00464-002-8777-y] [DOI] [PubMed] [Google Scholar]
Ceccarelli 2008
- Ceccarelli G, Casciola L. Comparing fibrin sealant with staples for mesh fixation in laparoscopic transabdominal hernia repair: a case control-study. Surgical Endoscopy 2008;22(3):668-73. [DOI] [PubMed] [Google Scholar]
Chelala 2007
- Chelala E, Thoma M, Tatete B, Lemye AC, Dessily M, Alle JL. The suturing concept for laparoscopic mesh fixation in ventral and incisional hernia repair: mid-term analysis of 400 cases. Surgical Endoscopy 2007;21(3):391–5. [DOI: 10.1007/s00464-006-9014-x] [DOI] [PubMed] [Google Scholar]
Christoffersen 2015
- Christoffersen MW, Brandt E, Helgstrand F, Westen M, Rosenberg J, Kehlet H, et al. Recurrence rate after absorbable tack fixation of mesh in laparoscopic incisional hernia repair. British Journal of Surgery 2015;102(2):541-7. [DOI: 10.1002/bjs.9750] [DOI] [PubMed] [Google Scholar]
Dabbas 2011
- Dabbas N, Adams K, Pearson K, Royle G. Frequency of abdominal wall hernias: is classical teaching out of date? Journal of the Royal Society of Medicine Short Reports 2011;2(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2021
- Deeks JJ, Higgins JP, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). The Cochrane Collaboration, 2021. Available from www.training.cochrane.org/handbook.
DeMaria 2000
- DeMaria EJ, Moss JM, Sugerman HJ. Laparoscopic intraperitoneal polytetrafluoroethylene (PTFE) prosthetic patch repair of ventral hernia. Prospective comparison to open prefascial polypropylene mesh repair. Surgical Endoscopy 2000;14(4):326-9. [DOI] [PubMed] [Google Scholar]
Den Hartog 2008
- Den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW. Open surgical procedures for incisional hernias. Cochrane Database of Systematic Reviews 2008, Issue 3. Art. No: CD006438. [CENTRAL: CD006438] [DOI: 10.1002/14651858.CD006438] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
EQ‐5D 2014
- EuroQol Group. EQ-5D Products. Available from: https://euroqol.org/ (accessed 27 August 2014).
Eriksen 2007
- Eriksen JR, Gögenur I, Rosenberg J. Choice of mesh for laparoscopic ventral hernia repair. Hernia 2007;11(6):481-92. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al, GRADE Working Group. GRADE guidelines: 7. Rating the quality of evidence - inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294-302. [DOI: 10.1016/j.jclinepi.2011.03.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Heniford 2003
- Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Annals of Surgery 2003;238(3):391-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine 2002;21(11):1539-58. [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;3627(7414):557-60. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/. [www.cochrane-handbook.org]
Hollinsky 2010
- Hollinsky C, Kolbe T. Tensile strength and adhesion formation of mesh fixation systems used in laparoscopic incisional hernia repair. Surgical Endoscopy 2010;24(6):1318-24. [DOI] [PubMed] [Google Scholar]
Itani 2010
- Itani KM, Hur K, Kim LT, Anthony T, Berger DH, Reda D, et al. Veterans Affairs Ventral Incisional Hernia I: comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: a randomized trial. Archives of Surgery 2010;145(4):322-8. [DOI] [PubMed] [Google Scholar]
Kaafarani 2010
- Kaafarani HM, Kaufman D, Reda D, Itani KM. Predictors of surgical site infection in laparoscopic and open ventral incisional herniorrhaphy. Journal of Surgical Research 2010;163(2):229-34. [DOI: 10.1016/j.jss.2010.03.019] [DOI] [PubMed] [Google Scholar]
Kingsnorth 2003
- Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet 2003;362(9395):1561-71. [PMID: ] [DOI] [PubMed] [Google Scholar]
Klinge 2005
- Klinge U, Conze J, Krones CJ, Schumpelick V. Incisional hernia: open techniques. World Journal of Surgery 2005;29(8):1066-72. [PMID: ] [DOI] [PubMed] [Google Scholar]
Köckerling 2015
- Köckerling F, Schug-Pass C, Adolf D, Reinpold W, Stechemesser B. Is pooled data analysis of ventral and incisional hernia repair acceptable? Frontiers in Surgery 2015;2(15):fsurg.2015.00015. eCollection 2015. [DOI: 10.3389/fsurg.2015.00015] [DOI] [PMC free article] [PubMed] [Google Scholar]
LeBlanc 1993
- LeBlanc KA, Booth WV. Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surgical Laparoscopy and Endoscopy 1993;3(1):39-41. [PMID: ] [PubMed] [Google Scholar]
LeBlanc 2004
- LeBlanc KA. Laparoscopic incisional and ventral hernia repair: complications - how to avoid and handle. Hernia 2004;8:323–31. [DOI: 10.1007/s10029-004-0250-5] [DOI] [PubMed] [Google Scholar]
LeBlanc 2007
- LeBlanc KA, Elieson MJ, Corder JM 3rd. Enterotomy and mortality rates of laparoscopic incisional and ventral hernia repair: a review of the literature. Journal of the Society of Laparoendoscopic Surgeons 2007;11(4):408-14. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Luijendijk 2000
- Luijendijk RW, Hopp WC, Van den Tol MP, De Lange DC, Braaksama MM, IJzermans JN, et al. A comparison of suture repair with mesh repair for incisional hernia. New England Journal of Medicine 2000;343(6):392-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mathes 2016
- Mathes T, Walgenbach M, Siegel R. Suture versus mesh repair in primary and incisional ventral hernias: a systematic review and meta-analysis. World Journal of Surgery 2016;40(4):826-35. [PMID: ] [DOI] [PubMed] [Google Scholar]
Misra 2006
- Misra MC, Bansal VK, Kulkarni MP, Pawar DK. Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. Surgical Endoscopy 2006;20(12):1839-45. [DOI] [PubMed] [Google Scholar]
Muysoms 2009
- Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, et al. Classification of primary and incisional abdominal wall hernias. Hernia 2009;13:407-14. [10.1007/s10029-009-0518-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nguyen 2008
- Nguyen SQ, Divino C, Buch M, Schnur KE, Weber J, Katz KJ, et al. Postoperative pain after laparoscopic ventral hernia repair: a prospective comparison of sutures versus tacks. Journal of the Society of Laparoendoscopic Surgeons 2008;12(2):113-6. [PMC free article] [PubMed] [Google Scholar]
Paul 1998
- Paul A, Korenkov M, Peters S, Köhler L, Fischer S, Troidl H. Unacceptable results of the Mayo procedure for repair of abdominal incisional hernias. European Journal of Surgery 1998;164(5):361-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pieper 2013
- Pieper D, Mathes T, Neugebauer E, Eikermann M. State of evidence on the relationship between high-volume hospitals and outcomes in surgery: a systematic review of systematic reviews. Journal of the American College of Surgeons 2013;216(5):1015-25. [DOI: 10.1016/j.jamcollsurg.2012.12.049] [DOI] [PubMed] [Google Scholar]
RevMan 2020 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version 5.4. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2020.
Reynvoet 2014
- Reynvoet E, Deschepper E, Rogiers X, Troisi R, Berrevoet F. Laparoscopic ventral hernia repair: is there an optimal mesh fixation technique? a systematic review. Langenbeck's Archives of Surgery 2014;399(1):55-63. [DOI] [PubMed] [Google Scholar]
Rogmark 2013
- Rogmark P, Petersson U, Bringman S, Eklund A, Ezra E, Sevonius D, et al. Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Annals of Surgery 2013;258(1):37-45. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sajid 2013
- Sajid MS, Parampalli U, McFall MR. A meta-analysis comparing tacker mesh fixation with suture mesh fixation in laparoscopic incisional and ventral hernia repair. Hernia 2013;17(02):159-66. [DOI: 10.1007/s10029-012-1017-z] [DOI] [PubMed] [Google Scholar]
Sauerland 2011
- Sauerland S, Walgenbach M, Habermalz B, Seiler C, Miserez M. Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database of Systematic Reviews 2011, Issue 3. Art. No: CD007781. [DOI: 10.1002/14651858.CD007781.pub2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schoenmaeckers 2012
- Schoenmaeckers EJ, De Haas RJ, Stirler V, Raymakers JT, Rakic S. Impact of the number of tacks on postoperative pain in laparoscopic repair of ventral hernias: do more tacks cause more pain? Surgical Endoscopy 2012;26(2):357-60. [DOI: 10.1007/s00464-011-1876-x] [DOI] [PubMed] [Google Scholar]
SF 2014
- SF Community. SF Materials Available. Available from: https://www.rand.org/health-care/surveys_tools/mos.html (accessed 27 August 2014).
Sterne 2016
- Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Clinical research ed.) 2016;355:i4919. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Venclauskas 2010
- Venclauskas L, Maleckas A, Kiudelis M. One-year follow-up after incisional hernia treatment: results of a prospective randomized study. Hernia 2010;14(6):575-82. [DOI: 10.1007/s10029-010-0686-8] [DOI] [PubMed] [Google Scholar]
Wassenaar 2008
- Wassenaar EB, Raymakers JT, Rakic S. Impact of the mesh fixation technique on operation time in laparoscopic repair of ventral hernias. Hernia 2008;12(1):23-25. [PMID: 17668146] [DOI] [PMC free article] [PubMed] [Google Scholar]
Welty 2001
- Welty G, Klinge U, Klosterhalfen B, Kasperk R, Schumpelik V. Functional impairment and complaints following incisional hernia repair with different polypropalene meshes. Hernia 2001;5(3):142-7. [DOI: 10.1007/s100290100017] [DOI] [PubMed] [Google Scholar]
Zhang 2014
- Zhang C, Li F, Zhang H, Zhong W, Shi D, Zhao Y. Self-gripping versus sutured mesh for inguinal hernia repair: a systematic review and meta-analysis of current literature. Journal of Surgical Research 2014;185(2):653-60. [DOI: 10.1016/j.jss.2013.07.035] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Protocol
- Walgenbach M, Mathes T, Siegel R, Eikermann M. Mesh fixation techniques in primary ventral or incisional hernia repair. Cochrane Database of Systematic Reviews 03 March 2015, Issue 3. Art. No: CD011563. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]


