Abstract
Persons suffering with systemic neuromuscular disorders or chronic organ failures, spend less time for daily physical activity, aggravating their mobility impairments. From 2020, patients at risk are also older adults, who, though negative for the SARS-Cov-2 infection, suffer with a fatigue syndrome due to home restriction/quarantine. Besides eventual psycological managements, it could be useful to offer to these patients a rehabilitation workouts easy to learn and to independently repeat at home (Full-Body In-Bed Gym). Inspired by the proven capability to recover skeletal muscle contractility and strength by home-based volitional exercises and functional electrical stimulation (FES), we suggest for this fatigue syndrome a 10–20 min long daily routine of easy and safe physical exercises that may recover from muscle weakness the main 400 skeletal muscles used for every-day activities. Leg muscles could be trained also by an adjunctive neuro-muscular electrical stimulation (NMES) in frail old persons. Many of the exercises could be performed in bed (Full-Body in-Bed Gym), thus hospitalized patients can learn this light training before leaving the hospital. Full-Body in-Bed Gym is, indeed, an extension of well-established cardiovascular-ventilation rehabilitation training performed by patients after heavy surgery. Blood pressure readings, monitored before and after daily routine of Full-Body in-Bed Gym, demonstrate a transient decrease in peripheral resistance due to increased blood flow to major body muscles. Continued regularly, Full-Body in-Bed Gym may help maintaining independence of frail people, including those suffering with the fatigue syndrome related to the restrictions/quarantine imposed to the general population during the COVID-19 pandemic.
Keywords: Skeletal muscle weakness, Home-based Full-Body in-Bed Gym, Borderline mobility impaired persons, Neuro-muscular electrical stimulation, COVID-19 fatigue syndrome
Roughly 400 human skeletal muscles are serious bone-movers, including little muscles of hands, feet, and face. The purpose of this report is to propose a comprehensive gym program to older adults, suffering skeletal muscle fatigue or with the outcomes from prolonged inactivity, to fight muscle atrophy and to maintain the best function and shape of body muscles [1]. Due to their advanced age and associated diseases, geriatric subjects spend little time on physical activity, in particular in the present situation of forced lockdown and quarantine imposed by the COVID-19 pandemic. Indeed, these subjects are, or risk to became, frail and at risk of falling, thus of losing and never recovering their previous physical and functional abilities.
The resulting disuse muscle atrophy further limits their independence, eventually forcing them to bed and hospitalization for long periods [2–4]. In addition to nutritional and pharmacological treatments, physical exercise at home is useful to counteract muscle atrophy in these persons [5–9].
Awaiting development of implantable devices for muscle stimulation, as effective as pacemakers for cardiac arrhythmias [10], implantable stimulators for ventilation supports [11, 12] or cochlear implants for hearing loss [13, 14], education of sedentary patients to perform home physical exercises could be an effective low-cost alternative during and after hospitalization [15–17]. Cardiovascular and ventilation physical rehabilitation protocols of surgical patients are well-established approaches, whose main goal is to reverse muscle weakness [18, 19]. We extended those routines, to a daily short (10–20 min) sequence of easy-to-learn and safe volitional physical exercises to be performed in bed (Full-Body in-Bed Gym) to improve muscles and, hence, mobility of impaired persons [15–17].
The risks are now even worsened by the conditions of lockdown and home restriction/quarantine imposed by the SARSCoV-2 pandemic. A fatigue syndrome related to COVID-19 disease is described in the general population, characterized by both the psychological response to the global problem of COVID-19 pandemic, and by muscle weakness that negatively influence the quality of life of persons for weeks or months after the resolution of an eventual SARS-CoV-2 infection [20–22].
In any case, muscle weakness can affect up to 10% of the population due to changes in people’s ordinary lifestyle due to lockdown measures imposed to control the epidemics [23, 24]. However, the most severe responses are expected later after resolution of an eventual SARS-CoV-2 infection. This post-COVID fatigue syndrome will affect the working capacity when economical recovery will be essential. Besides nutritional, pharmacological and psychotherapy support in the acute phases, it will be mandatory to control the mild cases by general prophylactic measures of healthy lifestyle, i.e., by normalization of sleep–wake schedule and moderate physical activity.
Here, our contribution is to convince practitioners [24–27], and the population at large that Full-Body in-Bed Gym is a valid option despite the minimal effort required [15–17] to counteract the effects of prolonged inactivity and persistent fatigue syndrome.
Workout
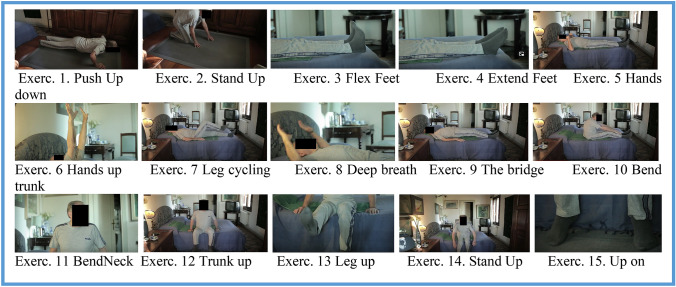
Figure 1 shows the exercises that could be a seasonal warm-up also for active persons, i. e, those able to make at least 20 consecutive push-ups in 3 min. On the other hand, sedentary people should start with five repetitions of each exercise, after advice from their practitioners to avoid exercise pain and eventual joint or muscle lesions. After two weeks, they should add groups of five additional repetitions, up to 20, every additional couples weeks. If compliant, even geriatric patients will progressively increase their muscle strength, when reaching and maintaining 20 daily repetitions. It is advised to start performing the routine at very slow speed, but when the maximum number of each exercise is reached (20 repetitions), improving effects will be obtained by speeding up exercises and thus intensity. A video available at Youtube link: https://www.youtube.com/watch?v=N1RuG3371-Y describes them dynamically [28].
Fig. 1.
The aim of the routine is to stimulate all main skeletal muscles, alternating exercises to mobilize arms and legs, spinal cord and neck, diaphragm and ventilation accessory muscles. The routine (as number of repetitions and speed) is continuously increased in intensity up to fatigue threshold. A video: https://www.youtube.com/watch?v=N1RuG3371-Y describes them dynamically [28]
Theory
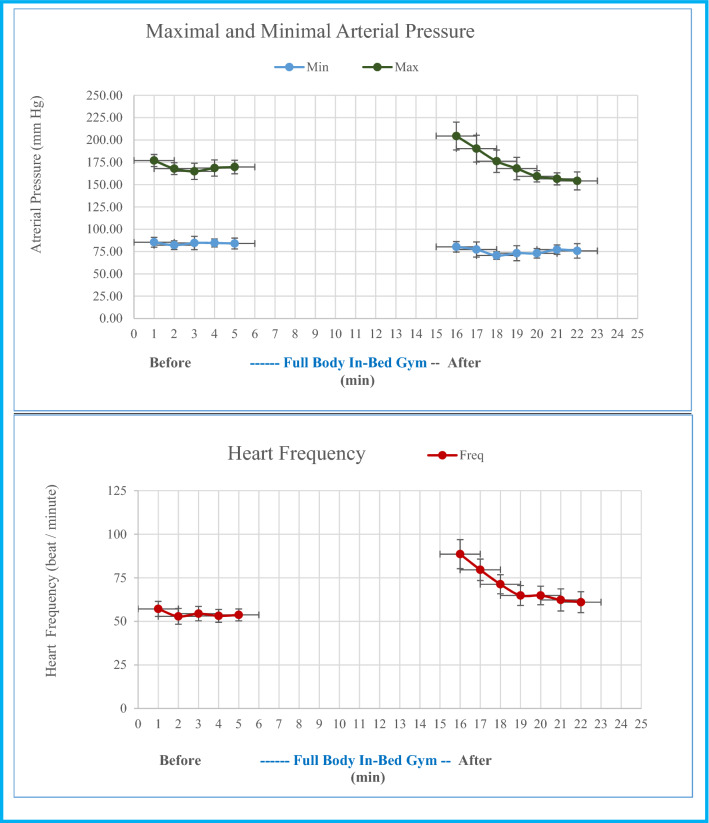
Cautious Full-Body in-Bed Gym helps patients to recover earlier after hospitalization, reducing eventual arterial hypertension [29]. Indeed, after a routine that challenges personal fitness, i.e., induces forehead sweat, increase cardio-pulmonary rates, and maximal, but not minimal blood pressure, in a few minutes, the increased values return to those pre-excersise, together with minimal arterial pressure. Results of a week of trainings are exemplified in Fig. 2. Indeed, peripheral arterial resistance decreasesduring the series of challenging exercises when blood perfusion increases by functional hyperhemia of the main skeletal muscles [17]. Correlations between values of cardiac frequency and maximal arterial pressure are very high (r2 < 0.95) when the results of a week of Full-Body In-bed Gym are analyzed. In addition, within a few days of inpatient care, a Full-body In-Bed Gym program may increase muscle strength, fatigue resistance and independence in daily life activities [16]. Furthermore, Full-Body in-Bed Gym routine mitigates the bad mood that is usually associated to mobility limitations [30]. If Full-Body in-Bed Gym is learned during hospitalisations, monitoring of the response to challenging trainings may include oxygen saturation and many more fitness variables. At home, using wearable devices (e.g. smartwatches, fitbands, smartphones, etc.) would guide during workout, providing heart rate monitoring and oxyhemoglobin saturation, reminder to perform exercises every day, and stopwatch for timing workout [31]. To speed up positive changes, persons are advised to the train twice a day to improve fatigue resistance and cardio-respiratory reserve [32, 33].
Fig. 2.
Arterial pressure and cardiac frequency before and after 10 min of Full-Body In-Bed Gym (25 repetitions of each exercise) during seven consecutive days (November 8 to 16, 2016). Mean ± SD
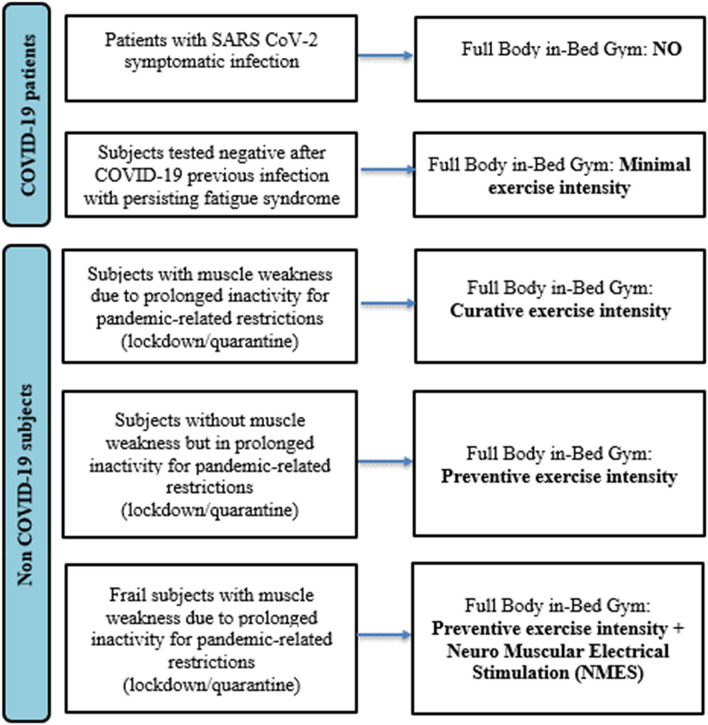
During the initial learning period of Full-Body In-bed Gym, all older adults, if not hospitalized, are advised to be supervised by at least one trainer, if not a health professional to avoid harmful exercises, that are linked to personal fitness and, nothing to say, to comorbidities often present in the elderlies. Although different categories of older subjects with muscle weakness may benefit from a program of Full-Body In-bed Gym, specific pathways are provided for patients recovered from COVID-19 having persistent outcomes and for individuals who have not been infected but have been non-active for a long time (Fig. 3).
Fig. 3.
Flow chart of older adults selection for Full-Body in-Bed Gym program and Neuro Muscular Electrical Stimulation in the COVID-19 scenario
Furthermore, all frail persons may benefit from the Full-Body In-bed Gym program associated with electrical stimulation. If older subjects cannot, or are reluctant to perform volitional physical rehabilitation protocols, functional neuro-muscular electrical stimulation (NMES) may mimic some of those exercises and be almost equally effective. NMES before or during the first weeks of workout is a rational approach for older adults to be submitted to Full-Body In-Bed Gym (Maria Chiara Maccarone, Padova, Italy, personal communication) or early rehabilitation after hip and knee surgical procedures (Helmut Kern, Vienna Austria, personal communication) [34–41].
Altogether, previous results demonstrated that physical exercise, either voluntary or induced by adjunctive NMES, improves functional performance of skeletal muscles, including those essential for ventilation, one of the main issues in post-COVID-19 old adults. Indeed, one of the most successful clinical applications of functional electrical stimulation (FES) is the respiratory support by pacing the diaphragm in quadriplegia and beyond [11, 12, 42–47].
In conclusion, Full-Body in-Bed Gym could help older subjects with muscle weakness due to the pandemic-related inactivity, with the aim to prevent and recover them from skeletal muscle fatigue.
Funding
A&C M-C Foundation for Translational Myology, Padova, Italy sponsored publication of this typescript.
Declartions
Conflict of interest
The authors state that there is no conflict of interest.
Human and animal rights
Our study agreed with the Declaration of Helsinki for the study on human subjects and participants.
Informed consent
Informed consent will be obtained from all individual participants who will be enrolled in future studies. No informed consent is required for this typescript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gava P, Kern H, Carraro U. Age-associated power decline from running, jumping, and throwing male masters world records. Exp Aging Res. 2015;41:115–135. doi: 10.1080/0361073X.2015.1001648. [DOI] [PubMed] [Google Scholar]
- 2.Hopkins RO, Mitchell L, Thomsen GE, et al. Implementing a mobility program to minimize post-intensive care syndrome. AACN Adv Crit Care. 2016;27:187–203. doi: 10.4037/aacnacc2016244. [DOI] [PubMed] [Google Scholar]
- 3.Camillo CA, Osadnik CR, Remoortel H, et al. Effect of “add-on” interventions on exercise training in individuals with COPD: a systematic review. ERJ Open Res. 2016;2:00078–2015. doi: 10.1183/23120541.00078-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czyrny JJ, Kaplan RE, Wilding GE, et al. Electrical foot stimulation: a potential new method of deep venous thrombosis prophylaxis. Vascular. 2010;18:20–27. doi: 10.2310/6670.2010.00001.ErratuminVascular2010Mar-Apr;18(2):121. [DOI] [PubMed] [Google Scholar]
- 5.Oshima K, Asai T, Fukumoto Y, et al. Development and persistence of fear of falling relate to a different mobility functions in community-dwelling older adults: one-year longitudinal predictive validity study. Aging Clin Exp Res. 2021 doi: 10.1007/s40520-020-01756-0. [DOI] [PubMed] [Google Scholar]
- 6.Rossi AP, Urbani S, Gattazzo S, et al. The Mini Sarcopenia Risk Assessment (MSRA) Questionnaire score as a predictor of skeletal muscle mass loss. Aging Clin Exp Res. 2021 doi: 10.1007/s40520-020-01763-1. [DOI] [PubMed] [Google Scholar]
- 7.Sebastião E, Mirda D. Group-based physical activity as a means to reduce social isolation and loneliness among older adults. Aging Clin Exp Res. 2021 doi: 10.1007/s40520-020-01722-w. [DOI] [PubMed] [Google Scholar]
- 8.Eckert T, Wronski P, Bongartz M, et al. Cost-effectiveness and cost-utility of a home-based exercise program in geriatric patients with cognitive impairment. Gerontology. 2021 doi: 10.1159/000512748. [DOI] [PubMed] [Google Scholar]
- 9.Ebner SA, Meikis L, Morat M, et al. Effects of movement-based mind-body interventions on physical fitness in healthy older adults: a meta-analytical review. Gerontology. 2021 doi: 10.1159/000512675. [DOI] [PubMed] [Google Scholar]
- 10.Saleem-Talib S, van Driel VJ, Chaldoupi SM, et al. Leadless pacing: going for the jugular. Pacing Clin Electrophysiol. 2019;42:395–399. doi: 10.1111/pace.13607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glenn WW, Hogan JF, Loke JS, et al. Ventilatory support by pacing of the conditioned diaphragm in quadriplegia. N Engl J Med. 1984;310:1150–1155. doi: 10.1056/NEJM198405033101804. [DOI] [PubMed] [Google Scholar]
- 12.Skalsky AJ, Lesser DJ, McDonald CM. Evaluation of phrenic nerve and diaphragm function with peripheral nerve stimulation and M-mode ultrasonography in potential pediatric phrenic nerve or diaphragm pacing candidates. Phys Med Rehabil Clin N Am. 2015;26:133–143. doi: 10.1016/j.pmr.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 13.Eskridge HR, Park LR, Brown KD. The impact of unilateral, simultaneous, or sequential cochlear implantation on pediatric language outcomes. Cochlear Implants Int. 2021 doi: 10.1080/14670100.2020.1871267. [DOI] [PubMed] [Google Scholar]
- 14.Gallo S, Trevisi P, Rigon C, et al. Auditory outcome after cochlear implantation in children with DFNB7/11 caused by pathogenic variants in TMC1 gene. Audiol Neurootol. 2020 doi: 10.1159/000510156. [DOI] [PubMed] [Google Scholar]
- 15.Carraro U, Karma Gava K, Baba A, et al. Fighting muscle weakness in advanced aging by takehome strategies: Safe anti-aging full-body in-bed gym and functional electrical stimulation (FES) for mobility compromised elderly people. Biol Eng Med. 2016;1:1–4. doi: 10.15761/BEM.1000106. [DOI] [Google Scholar]
- 16.Carraro U, Gava K, Musumeci A et al (2018) Safe antiaging Full-Body In-Bed Gym and FES for lazy persons: home in-bed exercises for fighting muscle weakness in advanced age. In: Masiero S, Carraro U (eds) Rehabilitation medicine for elderly patients, pp 43–52. ISBN 978-3-319-57405-9 ISBN 978-3-319-57406-6. 10.1007/978-3-319-57406-6
- 17.Carraro U, Gava K, Baba A, et al. To contrast and reverse skeletal muscle atrophy by full-body in-bed gym, a mandatory lifestyle for older olds and borderline mobility-impaired persons. Adv Exp Med Biol. 2018;1088:549–560. doi: 10.1007/978-981-13-1435-3_25. [DOI] [PubMed] [Google Scholar]
- 18.Ades PA, Keteyian SJ, Wright JS, et al. Increasing cardiac rehabilitation participation from 20% to 70%: a road map from the million hearts cardiac rehabilitation collaborative. Mayo Clin Proc. 2017;92:234–242. doi: 10.1016/j.mayocp.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vorona S, Sabatini U, Al-Maqbali S, et al. Inspiratory muscle rehabilitation in critically ill adults: a systematic review and meta-analysis. Ann Am Thorac Soc. 2018;15:735–744. doi: 10.1513/AnnalsATS.201712-961OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Soloveva NV, Makarova EV, Kichuk IV. Coronavirus syndrome: COVID-19 psychotrauma. Eur J Transl Myol. 2020;30:9302. doi: 10.4081/ejtm.9302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khosravi M. COVID-19 quarantine: two-way interaction between physical activity and mental health. Eur J Transl Myol. 2020;30:9509. doi: 10.4081/ejtm.2020.9509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Angelini C, Siciliano G. Neuromuscular diseases and Covid-19: advices from scientific societies and early observations in Italy. Eur J Transl Myol. 2020;30:9032. doi: 10.4081/ejtm.2019.9032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moro T, Paoli A. When COVID-19 affects muscle: effects of quarantine in older adults. Eur J Transl Myol. 2020;30:069. doi: 10.4081/ejtm.2019.9069.eCollection2020Jul13.PMID:32782767FreePMCarticle. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Hara J (2020) Rehabilitation after COVID-19. Mayo Clinic News Network. Available at the link: https://newsnetwork.mayoclinic.org/discussion/rehabilitation-after-covid-19/
- 25.Demeco N, Marotta M, Barletta I, et al. Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res. 2020;48:300060520948382. doi: 10.1177/0300060520948382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang TJ, Chau B, Lui M, et al. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil. 2020;99:769–774. doi: 10.1097/PHM.0000000000001505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith JM, Lee AC, Zeleznik H, et al. Home and community-based physical therapist management of adults with post-intensive care syndrome. Phys Ther. 2020;100:1062–1073. doi: 10.1093/ptj/pzaa059.PMID:32280993;PMCID:PMC7188154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Available at Youtube link: https://www.youtube.com/watch?v=N1RuG3371-Y
- 29.Börjesson M, Onerup A, Lundqvist S, et al. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med. 2016;50:356–361. doi: 10.1136/bjsports-2015-095786. [DOI] [PubMed] [Google Scholar]
- 30.Carneiro LS, Fonseca AM, Serrão P, et al. Impact of physical exercise on catechol-O-methyltransferase activity in depressive patients: a preliminary communication. Affect Disord. 2016;193:117–122. doi: 10.1016/j.jad.2015.12.035. [DOI] [PubMed] [Google Scholar]
- 31.Graña Possamai C, Ravaud P, Ghosn L, et al. Use of wearable biometric monitoring devices to measure outcomes in randomized clinical trials: a methodological systematic review. BMC Med. 2020;18:310. doi: 10.1186/s12916-020-01773-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Masiero S, Maccarone MC, Agostini F. Health resort medicine can be a suitable setting to recover disabilities in patients tested negative for COVID-19 discharged from hospital? A challenge for the future. Int J Biometeorol. 2020;64:1807–1809. doi: 10.1007/s00484-020-01947-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Masiero S, Zampieri D, Del Felice A. The place of early rehabilitation in intensive care unit for COVID-19. Am J Phys Med Rehabil. 2020;99:677–678. doi: 10.1097/PHM.0000000000001478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kern H, Carraro U, Adami N, et al. Home-based functional electrical stimulation rescues permanently denervated muscles in paraplegic patients with complete lower motor neuron lesion. Neurorehabil Neural Repair. 2010;24:709–721. doi: 10.1177/1545968310366129. [DOI] [PubMed] [Google Scholar]
- 35.Carraro U, Kern H. Severely atrophic human muscle fibers with nuclear misplacement survive many years of permanent denervation. Eur J Transl Myol. 2016;26:5894. doi: 10.4081/ejtm.2016.5894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carraro U, Kern H, Gava P, et al. Biology of muscle atrophy and of its recovery by FES in aging and mobility impairments: roots and by-products. Eur J Transl Myol. 2015;25:221–230. doi: 10.4081/ejtm.2015.5272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kern H, Barberi L, Löfler S, et al. Electrical stimulation counteracts muscle decline in seniors. Front Aging Neurosci. 2014;24:189. doi: 10.3389/fnagi.2014.00189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carraro U, Kern H, Gava P, et al. Recovery from muscle weakness by exercise and FES: lessons from Masters, active or sedentary seniors and SCI patients. Aging Clin Exp Res. 2017;29:579–590. doi: 10.1007/s40520-016-0619-1. [DOI] [PubMed] [Google Scholar]
- 39.Zampieri S, Mosole S, Löfler S, et al. Physical exercise in aging: nine weeks of leg press or electrical stimulation training in 70 years old sedentary elderly people. Eur J Transl Myol. 2015;25(4):237–242. doi: 10.4081/ejtm.2015.5374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kern H, Carraro U. Home-based functional electrical stimulation of human permanent denervated muscles: a narrative review on diagnostics, managements, results and byproducts revisited 2020. Diagnostics (Basel) 2020;10:529. doi: 10.3390/diagnostics10080529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Recenti M, Ricciardi C, Edmunds K, et al. Machine learning predictive system based upon radiodensitometric distributions from mid-thigh CT images. Eur J Transl Myol. 2020;30(1):8892. doi: 10.4081/ejtm.2019.8892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Albertin G, Ravara B, Kern H, et al. Two-years of home based functional electrical stimulation recovers epidermis from atrophy and flattening after years of complete Conus-Cauda Syndrome. Medicine (Baltimore) 2019;98:e18509. doi: 10.1097/MD.0000000000018509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zampieri S, Pietrangelo L, Loefler S, et al. Lifelong physical exercise delays age-associated skeletal muscle decline. J Gerontol A Biol Sci Med Sci. 2015;70:163–173. doi: 10.1093/gerona/glu006. [DOI] [PubMed] [Google Scholar]
- 44.Glenn WW, Phelps ML. Diaphragm pacing by electrical stimulation of the phrenic nerve. Neurosurgery. 1985;17:974–984. doi: 10.1227/00006123-198512000-00021. [DOI] [PubMed] [Google Scholar]
- 45.Berger D, Bloechlinger S, von Haehling S, et al. Dysfunction of respiratory muscles in critically ill patients on the intensive care unit. J Cachexia Sarcopenia Muscle. 2016;7:403–412. doi: 10.1002/jcsm.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peñuelas O, Keough E, López-Rodríguez L, et al. Ventilator-induced diaphragm dysfunction: translational mechanisms lead to therapeutical alternatives in the critically ill. Intensive Care Med Exp. 2019;7:48. doi: 10.1186/s40635-019-0259-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marrero HDJG, Stålberg EV, Cooray G, et al. Neurogenic vs. myogenic origin of acquired muscle paralysis in intensive care unit (ICU) patients: evaluation of different diagnostic methods. Diagnostics (Basel). 2020;10:966. doi: 10.3390/diagnostics10110966. [DOI] [PMC free article] [PubMed] [Google Scholar]