Abstract
Purpose:
Mandible fractures represent a significant portion of facial fractures in the pediatric population. Pediatric mandibles differ than their adult counterparts due to the presence of mixed dentition. Avoidance of injury to developing tooth follicles is critical. Simple mandible fractures can be treated with intermaxillary fixation (IMF) using either arch bars or bone screws. Here we present an alternative to these methods using silk sutures and an algorithm to assist in treating simple mandible fractures in the pediatric population.
Methods:
A retrospective chart review was performed and the records of one surgeon was examined. Pediatric patients who underwent treatment for a mandible fracture in the operating room between 2011 and 2015 were identified using Common Procedural Terminology (CPT) codes. Data collected included age, sex, type of fracture, type of treatment employed, duration of fixation, and presence of complications.
Results:
Five patients were identified with a mean age of 6.8 years upon presentation. Fracture types were unilateral fractures of the condylar neck (n=3), bilateral fractures of the condylar head (n=1), and a unilateral fracture of the condylar head with an associated parasymphyseal fracture (n=1). IMF was performed in 4 patients using silk sutures, and bone screw fixation was performed in the other patient. No post-treatment complications or malocclusion was reported. Average duration of IMF was 18.5 days.
Conclusions:
An algorithm is presented to assist in the treatment of pediatric mandible fractures. Silk suture fixation is a viable and safe alternative to arch bars or bone screws for routine mandibular fractures.
Introduction:
Facial fractures are less common in the pediatric population for a variety of reasons, including less mineralized and more malleable bone, larger fat pads, and open, compliant sutures [1]. The mandible and maxilla are further stabilized by the presence of unerupted dentition. In addition, there are more safeguards in place such as parental supervision and less risky activity [2]. Pediatric facial fractures account for about 15% of all facial fractures; however, there appears to be an increased incidence in the older pediatric population (12 to 18 years of age) due to interpersonal violence, sports, and recreational vehicle use [1–3].
The incidence of pediatric mandible fractures varies widely in the literature, with published reports between 20–50% of all pediatric facial fractures [1, 4]. Data demonstrates that most mandible fractures occur in patients greater than 6 years of age. One explanation is the higher cranial-to-facial ratios in the younger age group, providing anatomic protection [4, 5]. Management of mandible fractures in pediatric patients with primary or mixed dentition provides a unique challenge. In addition to restoring pre-injury function, care must be taken to choose a treatment technique that minimizes morbidity with future skeletal growth and dental development. Conservative treatment should be chosen whenever possible, and open reduction with internal fixation should be employed only when necessary. Respectable outcomes can be achieved by any technique providing return of pre-injury occlusion and short-term immobilization with intermaxillary fixation (IMF).
Surgeon preference plays the main role in the determination of which method is ultimately used. Guidelines regarding indications for each method of IMF do not exist. An algorithm for the management of mandibular fractures in pediatric patients during primary or mixed dentition is proposed along with a small case series. In addition, a simple, alternative method of IMF using silk suture ligatures is described.
Patients and Methods:
After Institutional Review Board approval, a retrospective chart review was conducted through the records of one l surgeon (KBP) in the Division of Plastic and Reconstructive Surgery at the Washington University in St. Louis School of Medicine. All patients with primary and mixed dentition who underwent treatment for a mandible fracture in the operating room between 2011 and 2015 were identified using Common Procedural Terminology (CPT) codes. Data collected included age, sex, type of fracture, type of treatment employed, time to return to OR for device removal, pre-operative radiography employed, and complications. All follow-up examinations included assessment of occlusion and incisal opening.
IMF Surgical Technique Using Suture or Bone Screws:
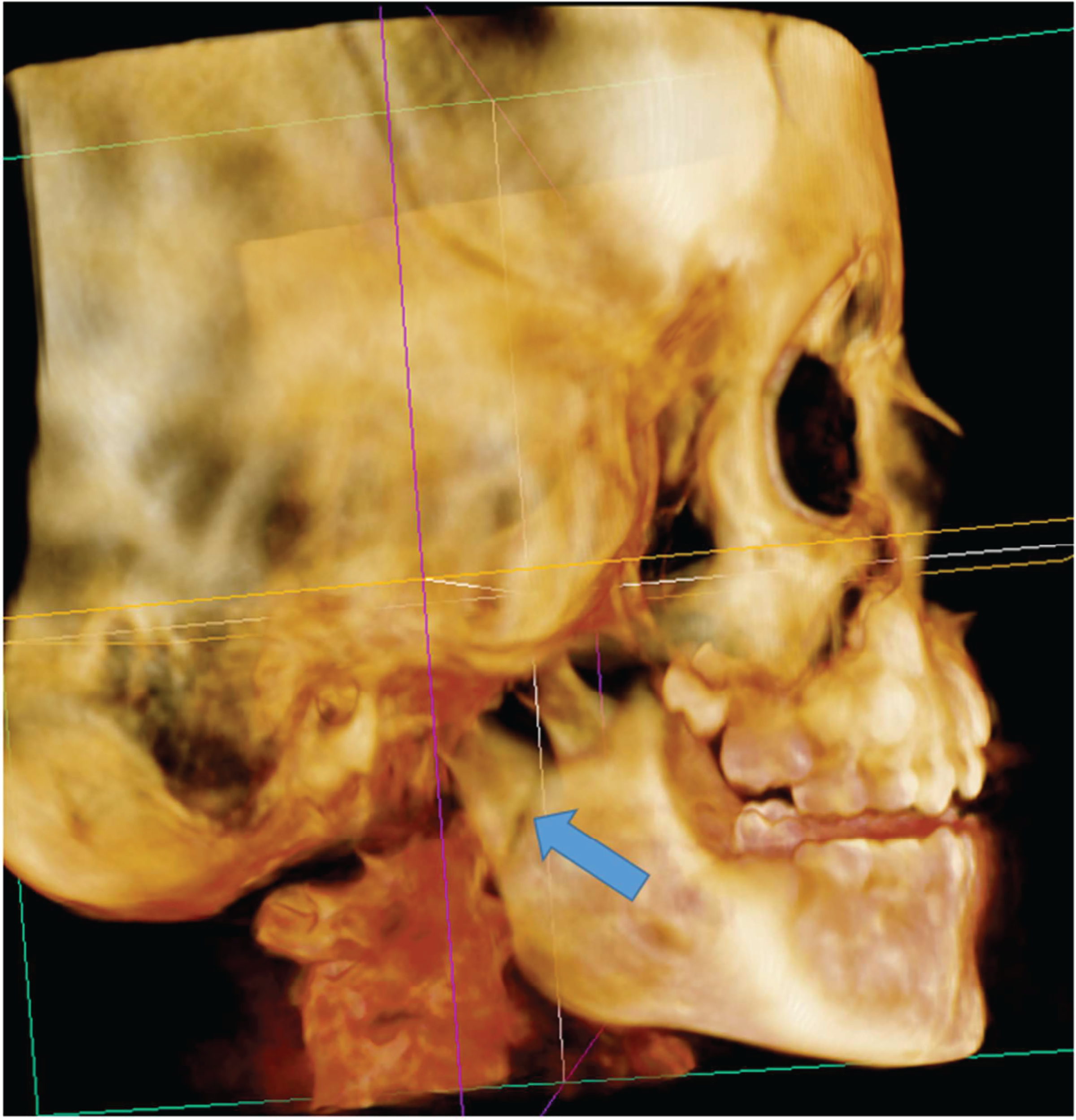
Ability to obtain preinjury occlusion is examined under general anesthesia. If obtained, 0-silk sutures (Ethicon, Inc., Somerville, N.J.), are tied around individual erupted molars and canines in both the mandible and maxilla. Centric occlusion is obtained and the silk sutures are tied tightly to each other (Fig. 1). Suture removal is performed in the operating room after the fracture has healed clinically.
Figure 1.
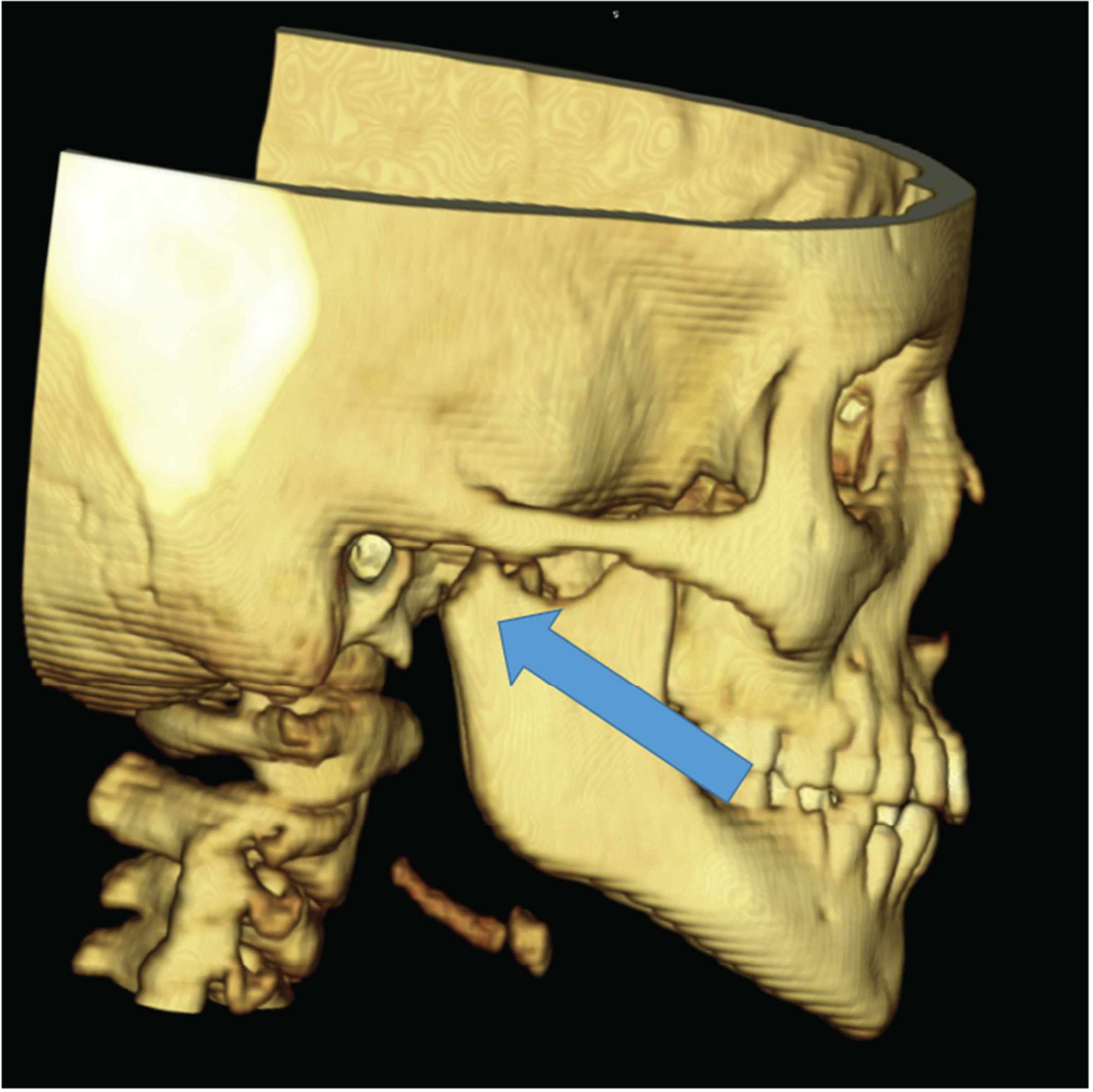

A: Case 1-3D reconstruction demonstrating right mandibular condyle fracture (arrow).
Figure 1B. Intermaxillary fixation with suture ligatures.
For fixation with IMF bone screws, preoperative imaging is used to identify positions of permanent and deciduous dentition; appropriate screw locations are chosen to avoid injury to dental structures. Self-drilling, self-tapping bone screws are placed, two within the mandible and two within the maxilla. Pre-stretched 25-gauge wires are used to fix the patient into centric occlusion.
Results:
We identified five patients with primary or mixed dentition who underwent treatment of an uncomplicated mandible fracture with silk sutures or bone screws. The mean age of these patients was 6.8 years (range 4 to 10 years). Three of the patients were male. Three patients had unilateral fractures of the condylar neck, one patient had bilateral fractures of the condylar head, and one patient had a unilateral fracture of the condylar head with an associated parasymphyseal fracture (Table 1).
Table 1:
Cases of pediatric patients treated using silk sutures and IMF screws.
| Age | Fracture Type | Fixation Method | Period of MMF (days) | Complications |
|---|---|---|---|---|
| 9 | R condylar neck | Silk sutures | 21 | none |
| 5 | L parasymphysis and R condylar head | ORIF + Silk sutures | 17 | none |
| 10 | L condylar neck | IMF screws | 18 | none |
| 4 | BL condylar head | Silk sutures | 18 | none |
| 6 | R subcondylar | Silk sutures | 11 | none |
Intermaxillary fixation was performed using silk sutures (n=4) and bone fixation screws (n=1). One patient required both silk sutures and open reduction and internal fixation (ORIF) using a resorbable plating system (Delta, Stryker Craniomaxillofacial, Kalamazoo, Mich.) due to a displaced parasymphyseal fracture. Total immobilization time with IMF ranged from 11 to 21 days, with a mean of 17 days. There were no postoperative complications reported. Preinjury occlusion was obtained in all patients with eventual return to normal pre-injury incisal opening.
Case Reports:
Case 1
9-year old female with right comminuted mandibular condyle fracture from motor vehicle collision (Figure 1). Patient underwent IMF using 0-silk ties to canines, pre-molars, molars bilaterally on the maxilla and mandible. Centric occlusion was obtained. The silk sutures were removed after 2 weeks and the patient remained on a soft, non-chew diet. At 2 month follow-up, the patient continued to report preinjury occlusion.
Case 2
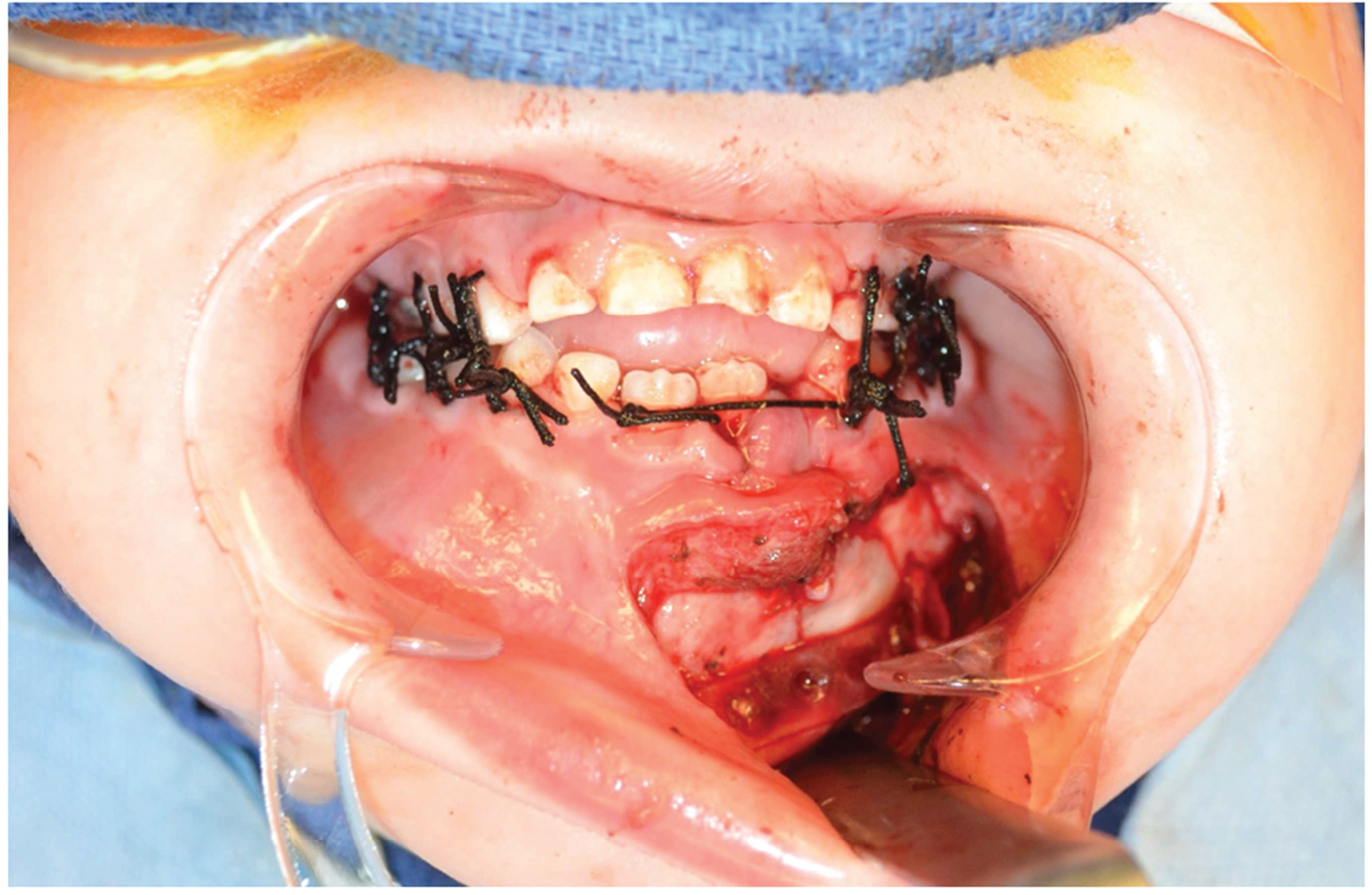
5-year old male sustained a left parasymphyseal fracture and right condylar fracture as an unrestrained back-seat passenger during a motor vehicle collision (Figure 2). The patient was first placed into IMF with 0-silk sutures to the primary dentition prior to open reduction internal fixation. A 0.75 Stryker Delta Absorbable System (Kalamazoo, MI) plate was placed through a left-sided gingivobuccal sulcus incision. A total of four 5-mm screws, two on each side, were placed. Preoperative imaging was reviewed to avoid injury to the tooth buds. The IMF was removed at 2 weeks. At his 3 month follow-up patient was non-tender, maintained good molar occlusion and incisal opening.
Figure 2.
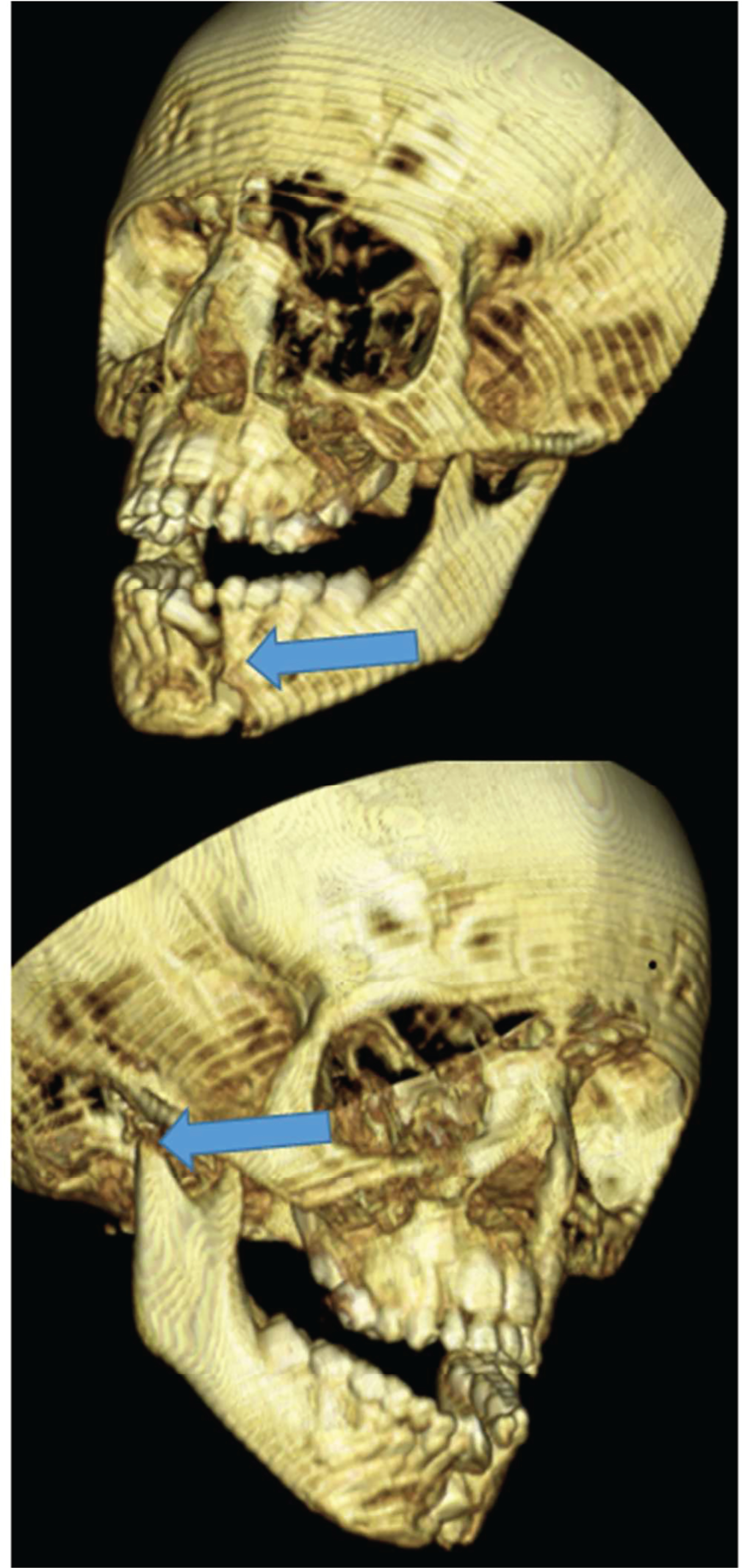
A: Case 2- 3D CT imaging demonstrating the right mandibular condyle and left parasymphyseal fractures (arrows).
Figure 2B. Intra-operative photo demonstrating intermaxillary fixation with suture ligatures and placement of the absorbable plate over the parasymphyseal fracture.
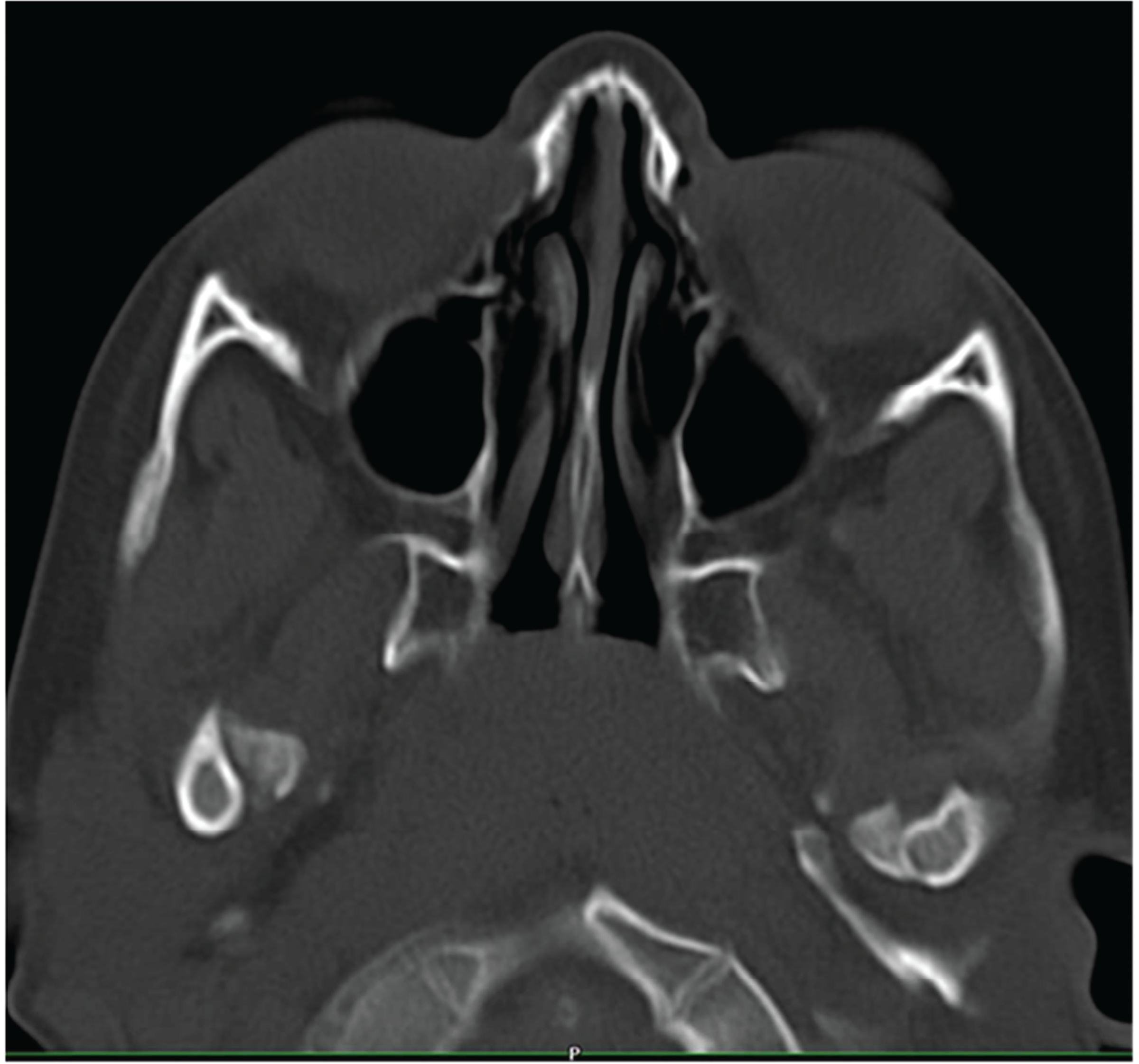
Case 3
10-year old male was involved in an all-terrain vehicle accident. Imaging revealed a left condylar and right body fracture (Figure 3). The patient was placed in centric occlusion with 8mm IMF bone screws (Stryker, Kalamazoo, MI) with two screws in each maxilla and mandible and 25 gauge wires. This decision was based on review of pre-operative imaging, which showed that there was sufficient room for screws. IMF was removed at his 2-week post-op visit and the patient remained in good occlusion at 4 weeks postoperatively.
Figure 3.

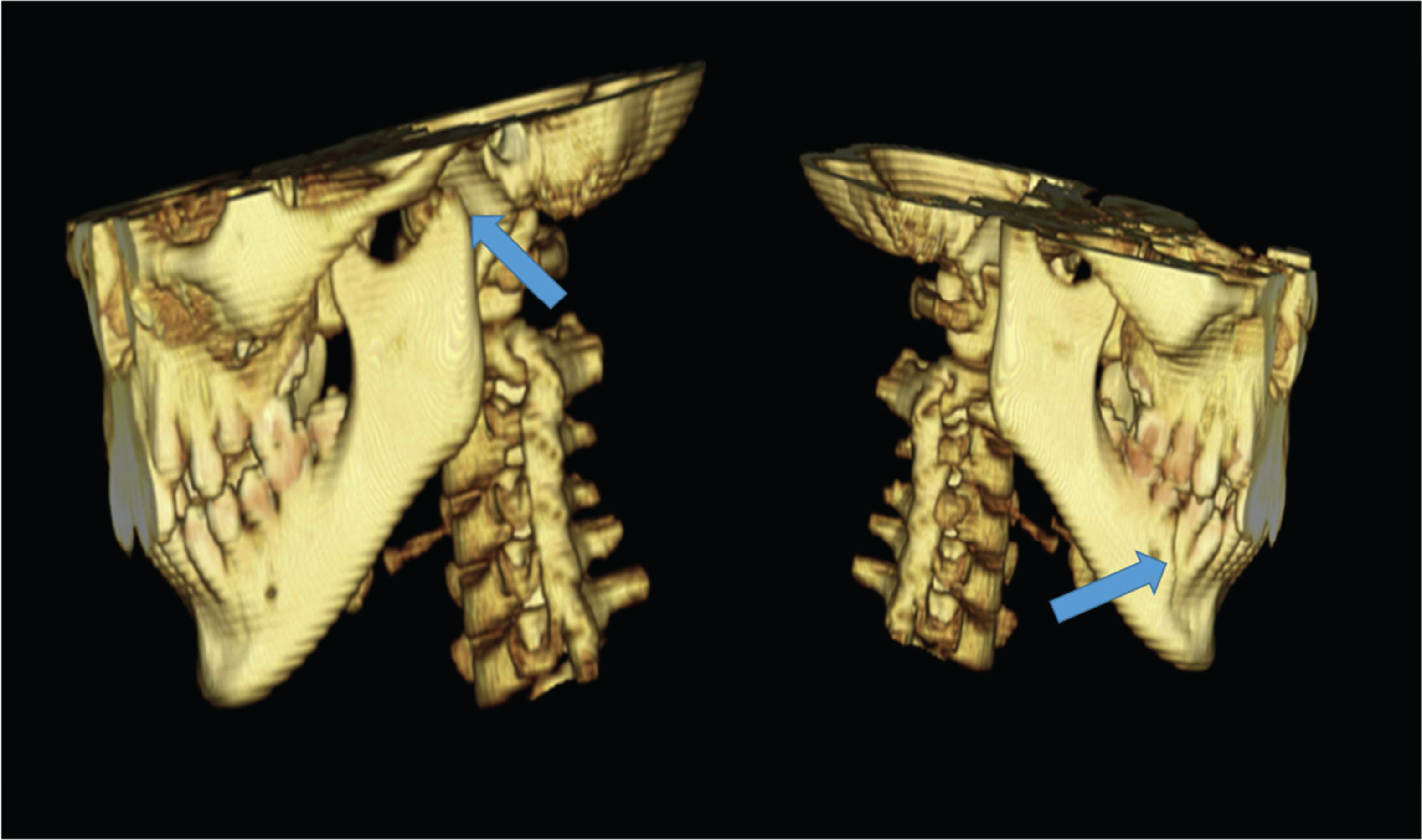
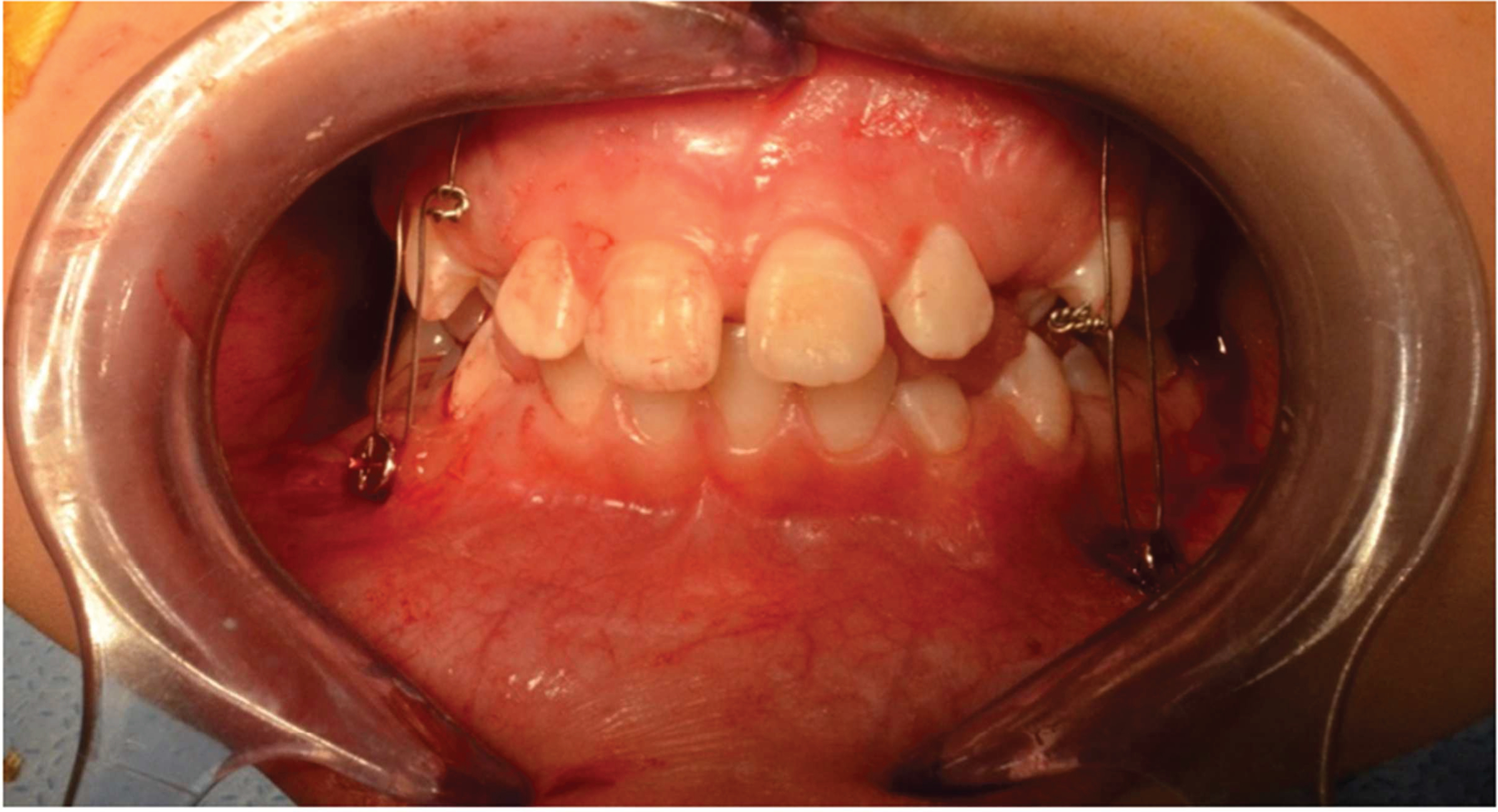
A. Case 3-Preoperative occlusion.
Figure 3B. 3D reconstruction demonstrating left condyle fracture and right body fracture (arrows).
Figure 3C. Demonstration of intermaxillary fixation with IMF screws.
Case 4
4-year old male, fell off his bicycle and sustained bilateral condylar neck fractures (Figure 4). Physical exam showed an anterior open bite. Intraoperatively, the patient was placed into IMF with 0-silk sutures applied to his deciduous molars and canines. The sutures were removed at 2 weeks postoperatively and the patient continued to do well at 8 weeks after the procedure with maintenance of his occlusion.
Figure 4.

A. Case 4-Bilateral condylar fractures demonstrated on preoperative CT scan.
Figure 4B. Postoperative image demonstrating suture IMF.
Case 5
6-year old female fell off of her bicycle and sustained a chin laceration as well as a right subcondylar mandible fracture (Figure 5). After a thorough exam and review of the radiographs, it was determined that the patient needed a closed reduction. Intraoperatively, the patient was placed into IMF with 0-silk sutures applied to her deciduous 1st molars and canines. IMF was removed at 11 days without any complications.
Figure 5.
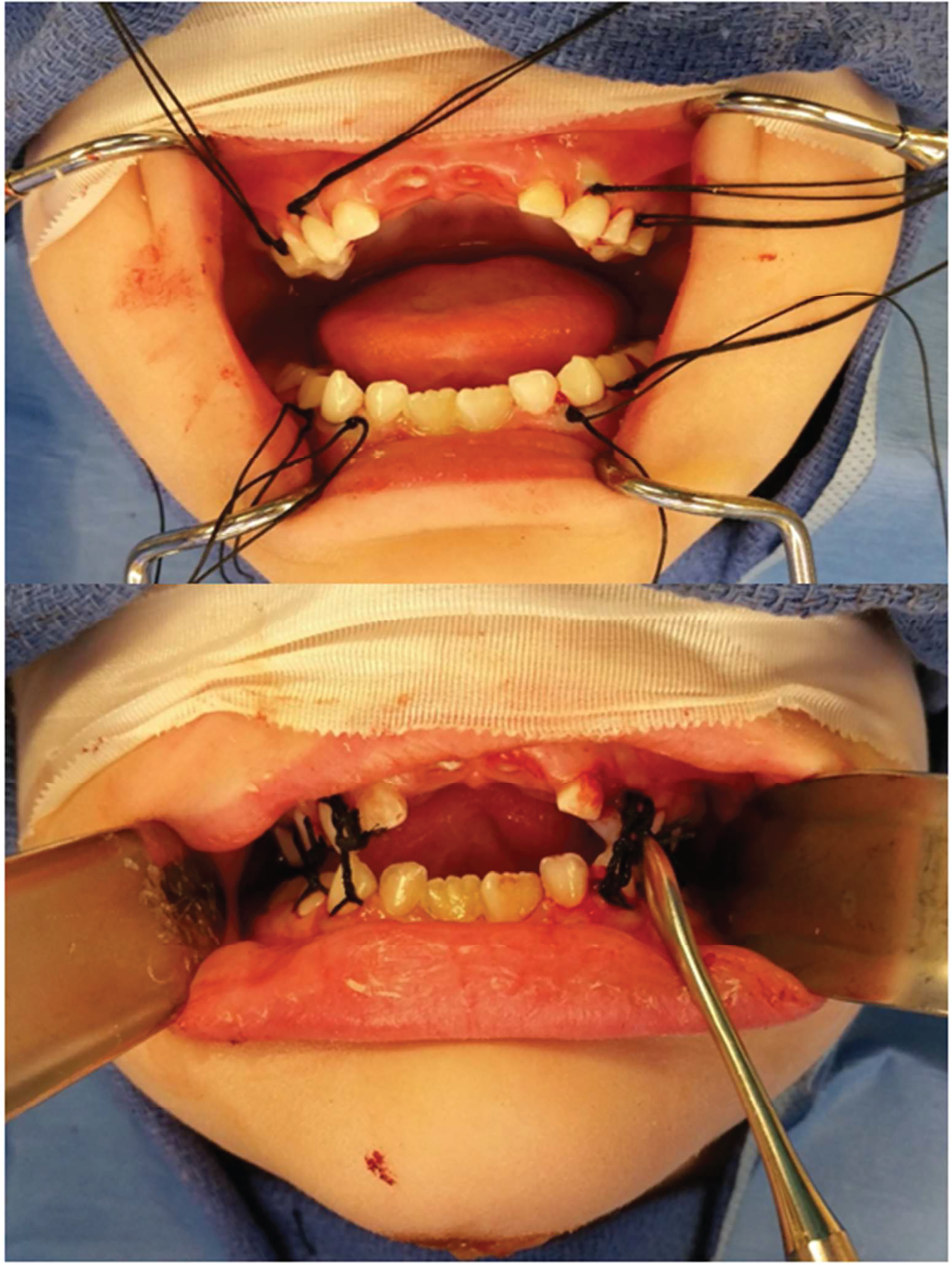
A. Case 5-CT image showing the right subcondylar fracture (arrow).
Figure 5B. Demonstration of suture ligatures around the canine and molars (upper) before being tied to each other to provide IMF (lower).
Discussion:
An algorithm for the management of mandible fractures in the pediatric population may prove beneficial in assisting treatment decisions (Figure 6). Since patients in mixed dentition have tooth follicles within the body of the mandible, care must be taken such that the method of fixation (bone screws) does not impinge upon or injure these tooth follicles. We recommend that all patients potentially requiring fixation with bone screws undergo radiographic imaging with an orthopantogram or computed tomography in order to reveal the number and location of tooth follicles.
Figure 6:
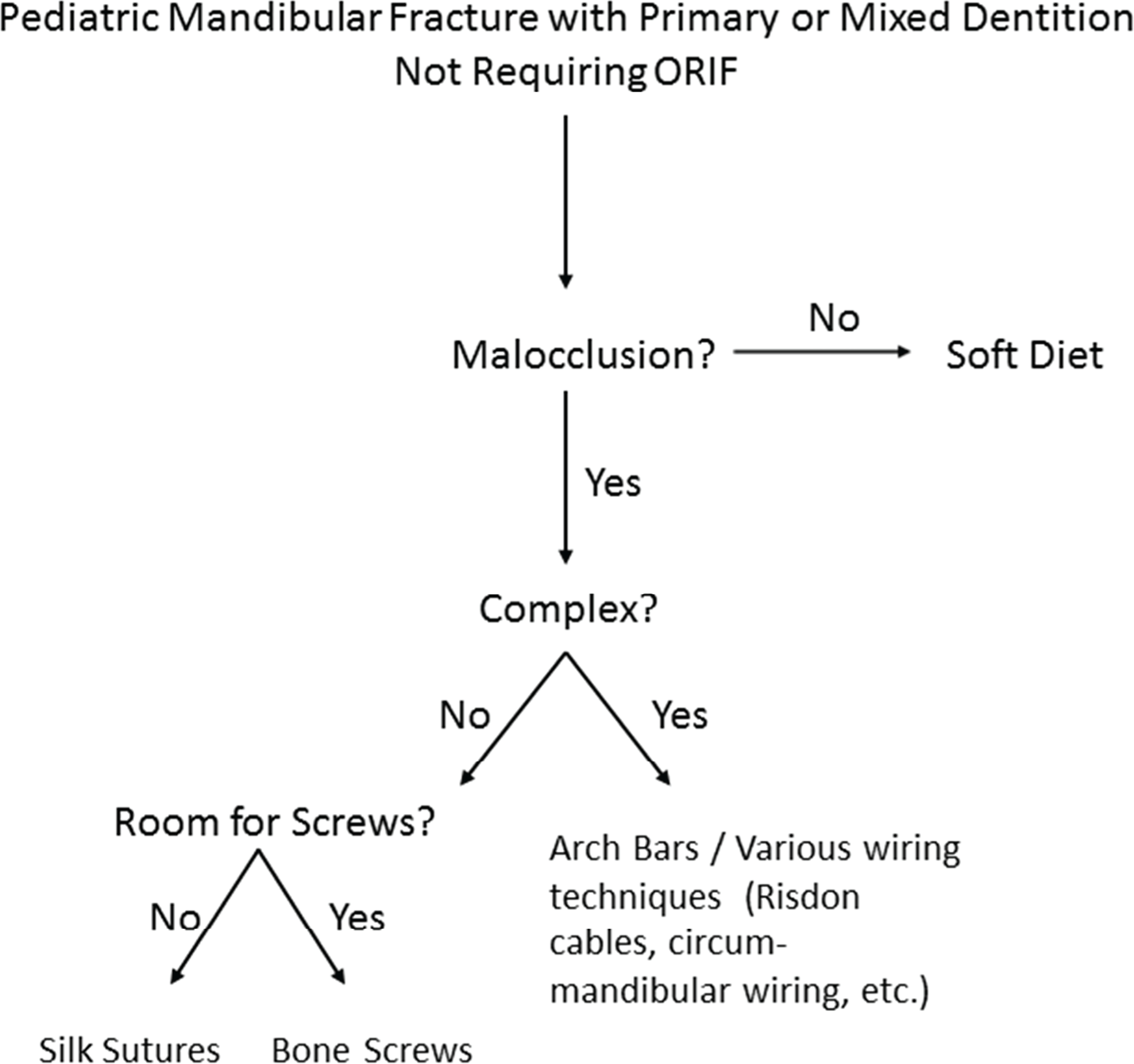
Algorithm for management of simple pediatric mandibular fractures.
Several methods of IMF for pediatric mandible fractures have been described. A fracture resulting in malocclusion must be reduced into pre-injury occlusion and subsequently immobilized. The most traditional method of fixation involves the use of arch bars with or without circummandibular and suspension wiring to the piriform aperture [6, 7]. Circummandibular suspension can be accomplished with either wires or sutures. Alternative methods of IMF include eyelet wires, occlusal splint fixation, bone fixation screws, Risdon cables, orthodontic appliances, and heavy suture ligatures[8–11].
All of the methods of fixation require an operating room and either general anesthesia or sedation for this patient demographic. Most pediatric mandible fractures do not require ORIF, so this modality is excluded from the algorithm. Nevertheless, some patients with severely comminuted fractures may require both IMF and ORIF to achieve adequate stability despite the algorithm, as seen in one of the patients reported in this series.
The first step in patient assessment concerns the presence or absence of malocclusion. When no malocclusion is present, substantial data indicates that conservative treatment of pediatric mandibular fractures by soft diet alone is preferable [4, 6, 9]. These patients have excellent outcomes, with the lowest potential for disruption of future growth or dentition.
When malocclusion is present or a fracture is displaced, it does not meet criteria for conservative management with observation and soft diet. Fixation with Erich arch bars or interdental wiring are the traditional methods of treatment in these fracture types. Disadvantages of arch bar placement include increased patient discomfort and time in the operating room, as well as increased incidence of needlestick-type injury to the operator [12–15]. Arch bars tend to slide down the buccal surface of the primary dentition and may interfere with occlusion. In addition, potential avulsion of deciduous teeth can occur when circumdental wires are tightened. Chronic gingival and mucosal irritation due to relatively oversized arch bars in relation to the size of the primary dentition can also be a nuisance especially considering the pediatric population.
An alternative to immobilization with arch bars is through the use of interdental silk sutures, provided the fracture is not significantly displaced and is stable. Patient perception may be more favorable when discussing that immobility is obtained with “strings” rather than “wires”. Also in case of an emergency, scissors or a sharp cutting tool can release the IMF as opposed to wire cutters, giving the family a peace of mind.
If the patient presents with a complex mandible fracture, IMF alone may not be an adequate treatment. Complex mandible fractures are defined as those that are displaced, comminuted, have an unfavorable fracture line, and may involve the alveolar ridge [16]. These fractures may require fixation with a plating system in addition to IMF (Figure 6).
Although this series was limited to a small cohort of patients, optimal outcomes were obtained, and pre-injury occlusion was achieved without any complications. The alternatives to arch bar fixation described in this series are only appropriate for patients requiring less than 4 weeks of IMF. There is an increased incidence of loss of fixation from screw or suture failure when these methods are used for an extended period of immobilization [13]. When applying this algorithm for patient selection, we have found these approaches to be safe and effective. This provides alternative methods that can applied by surgeons treating pediatric mandible fractures. Furthermore, these alternative methods of immobilization may be better tolerated by patients of the pediatric population.
Acknowledgments
Research reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and Children’s Discovery Institute. The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. We would like to acknowledge Gary Skolnick and Adam Aronson for their contribution to this manuscript.
Footnotes
Financial Disclosure:
Dr. Patel is a consultant for Stryker CMF. The other authors have no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Zimmermann CE, Troulis MJ, Kaban LB: Pediatric facial fractures: recent advances in prevention, diagnosis and management. International Journal of Oral and Maxillofacial Surgery 34:823, 2005 [DOI] [PubMed] [Google Scholar]
- 2.Grunwaldt L, Smith DM, Zuckerbraun NS, Naran S, Rottgers SA, Bykowski M, Kinsella C, Cray J, Vecchione L, Saladino RA, Losee JE: Pediatric facial fractures: demographics, injury patterns, and associated injuries in 772 consecutive patients. Plast Reconstr Surg 128:1263, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Vyas RM, Dickinson BP, Wasson KL, Roostaeian J, Bradley JP: Pediatric facial fractures: current national incidence, distribution, and health care resource use. J Craniofac Surg 19:339, 2008 [DOI] [PubMed] [Google Scholar]
- 4.Smith DM, Bykowski MR, Cray JJ, Naran S, Rottgers SA, Shakir S, Vecchione L, Schuster L, Losee JE: 215 mandible fractures in 120 children: demographics, treatment, outcomes, and early growth data. Plast Reconstr Surg 131:1348, 2013 [DOI] [PubMed] [Google Scholar]
- 5.McGraw BL, Cole RR: Pediatric maxillofacial trauma. Age-related variations in injury. Arch Otolaryngol Head Neck Surg 116:41, 1990 [DOI] [PubMed] [Google Scholar]
- 6.Smartt JM Jr., Low DW, Bartlett SP: The pediatric mandible: II. Management of traumatic injury or fracture. Plast Reconstr Surg 116:28e, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Nishioka GJ, Larrabee WF, Murakami CS, Renner GJ: Suspended circummandibular wire fixation for mixed-dentition pediatric mandible fractures. Arch Otolaryngol Head Neck Surg 123:753, 1997 [DOI] [PubMed] [Google Scholar]
- 8.Ongodia D, Li Z, Xing WZ, Li ZB: Resorbable plates for fixation of complicated mandibular fractures in children. J Maxillofac Oral Surg 13:99, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goth S, Sawatari Y, Peleg M: Management of pediatric mandible fractures. J Craniofac Surg 23:47, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Eppley BL: A resorbable and rapid method for maxillomandibular fixation in pediatric mandible fractures. J Craniofac Surg 11:236, 2000 [DOI] [PubMed] [Google Scholar]
- 11.Madsen M, Tiwana PS, Alpert B: The use of risdon cables in pediatric maxillofacial trauma: a technique revisited. Craniomaxillofac Trauma Reconstr 5:107, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ayoub AF, Rowson J: Comparative assessment of two methods used for interdental immobilization. J Craniomaxillofac Surg 31:159, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Rai A, Datarkar A, Borle RM: Are maxillomandibular fixation screws a better option than Erich arch bars in achieving maxillomandibular fixation? A randomized clinical study. J Oral Maxillofac Surg 69:3015, 2011 [DOI] [PubMed] [Google Scholar]
- 14.Nandini GD, Balakrishna R, Rao J: Self Tapping Screws v/s Erich Arch Bar for Inter Maxillary Fixation: A Comparative Clinical Study in the Treatment of Mandibular Fractures. J Maxillofac Oral Surg 10:127, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rai A: A Simple Method of Preventing Needle Stick Type Injury to the Operator’s Finger While Performing Intermaxillary Fixation. J Maxillofac Oral Surg 13:215, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cornelius CP, Audige L, Kunz C, Rudderman R, Buitrago-Tellez CH, Frodel J, Prein J: The Comprehensive AOCMF Classification System: Mandible Fractures-Level 3 Tutorial. Craniomaxillofac Trauma Reconstr 7:S031, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]


