Abstract
In this article, we report a case of a 61-year-old male who was diagnosed with SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), presenting with acute respiratory distress syndrome requiring intubation and hemodynamic support, marked D-Dimer and troponin I elevation, worsening ST-elevation myocardial infarction on repeat electrocardiograms, and a negative coronary angiogram ruling out a coronary artery thrombosis or occlusion. With worsening diffuse ST-segment elevation on electrocardiograms and reduced ejection fraction on echocardiography in the setting of systemic inflammation, fulminant myocarditis was highly suspected. Despite optimal medical treatment, the patient’s condition deteriorated and was complicated by cardiac arrest that failed resuscitation. Although myocarditis was initially suspected, the autopsy revealed no evidence of myocarditis or pericarditis but did demonstrate multiple microscopic sites of myocardial ischemia together with thrombi in the left atrium and pulmonary vasculature. Additionally, scattered microscopic cardiomyocyte necrosis with pathological diagnosis of small vessel micro-thrombotic occlusions. These findings are potentially exacerbated by inflammation-induced coagulopathy, hypoxia, hypotension, and stress, that is, a multifactorial etiology. Further research and an improved understanding are needed to define the precise pathophysiology of the coagulopathic state causing widespread micro-thrombosis with subsequent myocardial and pulmonary injury.
Keywords: myocardial injury, STEMI, myocarditis, COVID-19, SARS-CoV-2 infection, coagulopathy, micro-thrombotic emboli
Case Presentation
The patient is a 61-year-old male, with a past medical history significant for hypertension, obesity (body mass index: 33 kg/m2), and hyperlipidemia, presenting to the emergency department during the onset of the coronavirus disease 2019 (COVID-19) pandemic. The patient presented with a 2-week history of progressive shortness of breath, cough, generalized fatigue, and muscle aches. He denied any chest, arm, or jaw pain or pressure. His past medical history was negative for diabetes mellitus, cardiovascular disease, or chronic lung, liver, or kidney disease. The patient denied current or previous tobacco use.
On arrival, the patient was visibly distressed, tachypneic with a respiratory rate above 50 breaths per minute, and hypoxic with a blood oxygen saturation of 85% on 15 L of oxygen via a simple mask. He was hypotensive with a blood pressure of 68/42 mm-Hg and tachycardic with a heart rate above 140 beats per minute. On physical examination, he was alert but diaphoretic with significant respiratory distress, weak peripheral pulses, and cool extremities. Based on his recent history and present condition, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was suspected, and he was immediately moved to a negative pressure isolation room where the decision was made for early sedation, intubation, and circulatory support with norepinephrine, vasopressin, and dobutamine, with a workup for sepsis and septic shock. Laboratory results were remarkable for positive SARS-CoV-2 and negative for other viral and bacterial respiratory pathogens. D-dimer level was significantly elevated (32 563 ng/mL; normal <230 ng/mL) as well as cardiac troponin I level (7.457 ng/mL; normal <0.034 ng/mL). Other laboratory results are shown in Table 1.
Table 1.
Biochemical Results on Admission and Trend During Hospitalization.
| Value | Reference range | |||
|---|---|---|---|---|
| WBC | 15.7 | 3.4-11 (×103/µL) | ||
| Platelet | 151 | 147-395 (×103/µL) | ||
| Hemoglobin | 13.6 | 11.3-16.8 g/dL | ||
| Creatinine | 1.16 | 0.66-1.25 mg/dL | ||
| INR | 1.5 | 0.9-1.1 | ||
| CRP | 306.8 | ≤5 mg/L | ||
| LDH | 707 | 120-246 U/L | ||
| IL-6 | 23 | <5 pg/mL | ||
| D-dimer | 32 563 | <230 ng/mL | ||
| Ferritin | 2831.22 | 21.81-274.66 ng/mL | ||
| CK | 86 | 55-170 U/L | ||
| Day 4 | Day 3 | Day 2 | Day 1 | |
| D-Dimer | 32 563 | 2816 | — | 1603 |
| Troponin | 7457 | 5852 | 2214 | 0.768 |
| Platelets | 151 | 242 | 294 | 385 |
| INR | 1.5 | 1.2 | 1.2 | 1.3 |
Abbreviations: CK, creatine kinase; CRP, C-reactive protein; IL-6, interleukin-6; INR, international normalized ratio; LDH, lactate dehydrogenase; WBC, white blood cell.
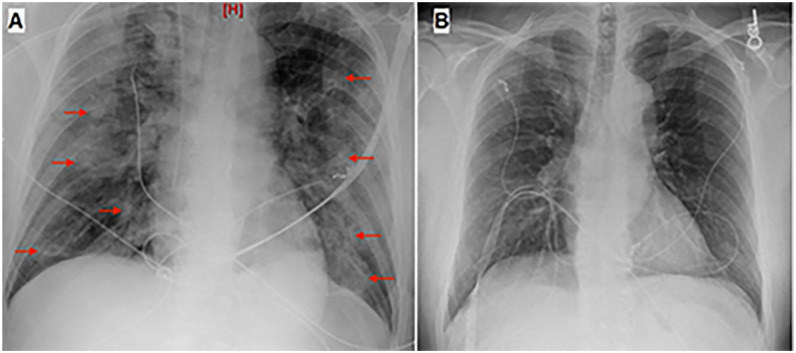
New diffuse bilateral airspace opacities indicating pulmonary infection were detected on chest X-ray in comparison to a one performed 2 weeks prior, when he presented to the emergency department with a mild cough and myalgia (Figure 1). Pulmonary embolism (PE) was suspected, and the patient was started on immediate anticoagulation with heparin infusion. A bedside transthoracic echocardiography was performed rather than computed tomography pulmonary angiography given the hemodynamic instability of the patient and the risk for patient deterioration during transportation and disease transmission to other patients and health care workers. The echocardiography revealed normal right ventricle size and systolic pressure, mildly elevated pulmonary arterial pressure of 31 mm Hg, and moderate global hypokinesis of the left ventricle (LV) with reduced overall systolic function; ejection fraction (EF) 30% to 35%. These findings were remarkably different from his echocardiography performed 4 months prior, at which time the LV systolic function was normal with an EF of 62%.
Figure 1.
Chest X-ray anteroposterior view demonstrating new diffuse bilateral airspace opacities (red arrows) (A) with comparison to chest X-ray performed 2 weeks prior (B).
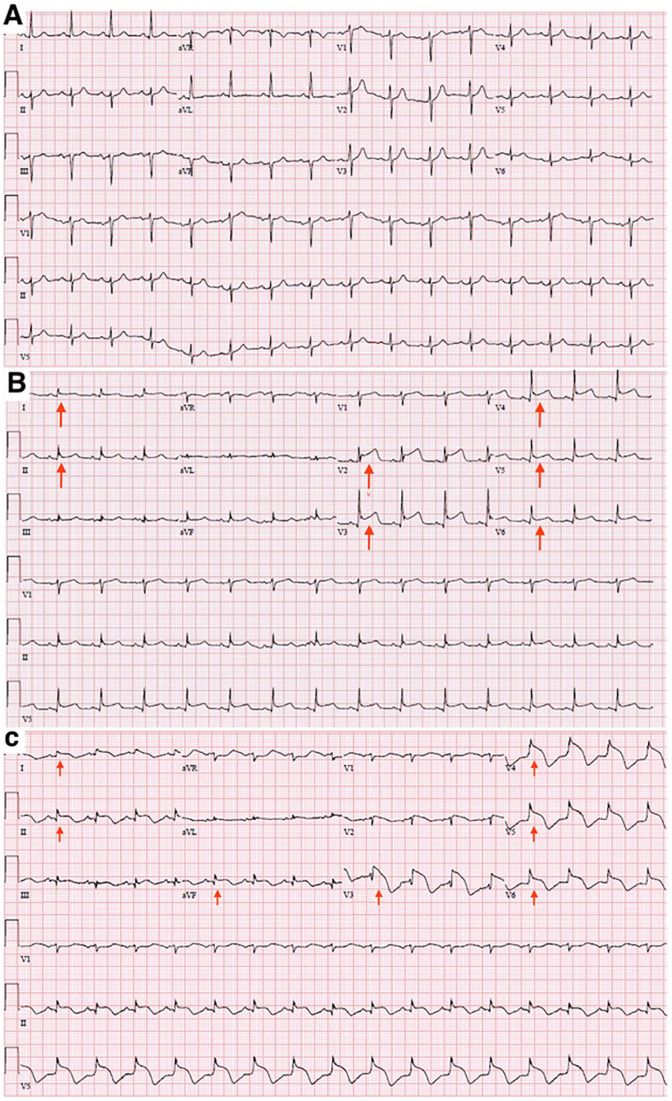
Electrocardiogram (ECG) demonstrated diffuse, mainly anterolateral, ST elevation (leads I, II, and V2-V6), markedly abnormal with new ischemic changes when compared with an ECG recorded 2 weeks prior (Figure 2A and B). The ECG findings along with the significantly elevated cardiac troponin-I levels were consistent with ST-elevation myocardial infarction (STEMI), raising the suspicion of acute coronary syndrome secondary to acute coronary occlusion, acute myocarditis, or extensive coronary microvascular thrombosis in the settings of COVID-19. Therefore, the patient was immediately started on acute coronary syndrome treatment protocol with dual antiplatelet therapy (aspirin and ticagrelor) along with the ongoing heparin infusion and inotropic support with norepinephrine, vasopressin, and dobutamine.
Figure 2.
Electrocardiogram (ECG) demonstrating sinus rhythm and new ST elevation in the anterior and lateral leads (I, II, V2, V3, V4, V5, and V6) (red arrows) (B) compared with normal ECG from 2 weeks earlier (A). Subsequent ECG shows new ST elevation in lead aVF and worsening ST elevation in lead II (inferior leads) as well as worsening ST elevation in anterolateral leads (I, V3-V6), demonstrating diffuse ST elevation that is not confined to a single coronary territory (red arrows) (C).
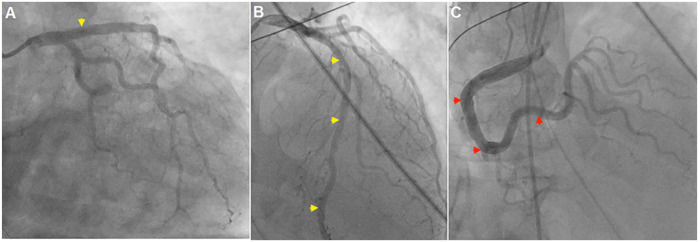
After discussion with the interventional cardiology team, coronary angiography with left heart catheterization (LHC) was initially deferred given the suspicion for myocarditis in the settings of the severe inflammatory state and septic shock, as well as the risk of infection transmission to health care workers. Thrombolytics were not advised due to the potential risk for pulmonary hemorrhage in severe SARS-CoV-2 infection. Despite optimal medical treatment, the patient’s ECG revealed new ST elevation in lead aVF and worsening ST elevation in lead II (inferior leads) as well as worsening ST elevation in anterolateral leads (I, V3-V6), demonstrating diffuse ST elevation that is not confined to a single coronary territory (Figure 2C). In addition, multiple episodes of ventricular tachycardia were observed on telemetry. The decision was then made to proceed to emergent LHC, and coronary angiography was performed, which unexpectedly revealed widely patent normal left and right coronary arteries, with no epicardial stenosis or thrombosis and no evidence for delayed coronary filling (Figure 3).
Figure 3.
Coronary angiography demonstrating widely patent left (yellow arrowheads) (A, B) and right (red arrowheads) (C) coronary arteries, with no evidence for significant epicardial stenosis, thrombosis, or delayed emptying.
Left ventriculography was negative for Takotsubo cardiomyopathy, showing diffuse hypokinesis (EF reported as 40% to 45%) and left ventricular end-diastolic pressure of 22 mm Hg. Epicardial coronary thrombosis, STEMI, and Takotsubo cardiomyopathy were excluded. SARS-CoV-2-induced fulminant myocarditis became the primary working diagnosis. However, prior thrombosis with distal showering of emboli and or COVID-related micro-thrombotic occlusions could not be ruled out. Steroid therapy was started, but unfortunately a few hours later, the patient suffered a cardiac arrest that failed cardiopulmonary resuscitation and subsequently expired.
Autopsy revealed patent coronaries without significant atherosclerotic changes or evidence of acute myocardial infarct. Scattered focal ischemic changes were identified on histopathological examination of the ventricular myocardium throughout the heart, characterized by hyper-eosinophilic myocytes with signs of nuclear degeneration. No inflammatory neutrophil infiltrates adjacent to these ischemic fibers were seen, nor was there evidence for myocarditis or pericarditis. Interstitial edema and an increased number of macrophages (as identified by CD68 staining) were observed. Autopsy also revealed an adherent organizing left atrial thrombus (1.5 cm) and marked thromboembolism of the left pulmonary artery as suspected on initial admission with diffuse pulmonary vascular microthrombi, pulmonary consolidation, and some associated hemorrhage with early hyaline membrane formation.
Discussion
Myocardial injury is a common sequela among patients hospitalized with SARS-CoV-2 infection, more frequently reported in intensive care unit patients,1 and it correlates with worse prognosis and higher mortality.2,3 The pathophysiology of myocardial injury in patients with SARS-CoV-2 infection is not yet precisely defined but is believed to be multifactorial. Possible underlying mechanisms include ischemia due to macro- or micro-thrombotic arterial occlusions, non-ischemic myocarditis, local, and/or systemic inflammation with coagulopathy as well as hypoperfusion secondary to hypotension, hypoxia, and shock.4 Recent reports suggest that SARS-CoV-2 recognizes human ACE2 more efficiently than SARS-CoV (the first identified SARS-CoV epidemic virus that appeared in 2002), facilitating viral entry into cardiac myocytes and causing direct cardiotoxicity.5 Localization of SARS-CoV-2 viral particles in the myocardium strongly endorses the potential for direct virus-mediated cardiotoxicity.6
Coronary macro-thrombosis can be predisposed by stress-induced activation of the autonomic nervous system causing coronary vasoconstriction along with endothelial and smooth muscle cell dysfunction, macrophage, and platelet activation that eventually precipitate atheromatous plaque instability and rupture.7 Hypoxemia secondary to severe lung injury in SARS-CoV-2 infection is also believed to contribute to cardiotoxicity. Hypoxemia causes reduction of energy supply to cardiomyocytes, enhancing intracellular acidosis and calcium influx, and facilitating myocytes apoptosis.4
Coagulopathy with arterial and pulmonary microthrombi has also been reported in severe SARS-CoV-2 infection.8 A meta-analysis including 8271 CVOID-19 patients reported incidence of venous thromboembolism, deep vein thrombosis, and PE in 21%, 20%, and 13%, respectively.9 Elevated D-dimer on admission can predict thrombotic and bleeding complications, as well as mortality.10 The excessive immune and inflammatory responses with high cytokine levels (eg, IL-6 and IL-8), referred to as cytokine storm, in severe SARS-CoV-2 infection contribute to coagulopathy activation and directly correlates with higher mortality.11,12 High levels of IL-6, as in our patient, stimulate hemopoiesis by enhancing the expression of factor VIII, fibrinogen, and von-Willebrand factor, activation of endothelial cells and platelet production, and reduce the levels of protein S and antithrombin.13 This can also accelerate the formation of less stable arteriolar thrombi as evidenced in WT mice experiments.14 Moreover, severe inflammation can cause alteration of circulating soluble uPA receptor (suPAR) and serine proteases that are essential in the thrombotic and thrombolytic cascades. Outside of activation of coagulation pathways, these toxic inflammatory responses lead to accumulation of reactive oxygen species and damaging inflammatory cells in the myocardium causing cellular apoptosis and myocardial injury.
In our case, the presence of ischemic myocardium, PE, diffuse lung small vessel and left atrium thrombosis on autopsy, along with elevated D-dimer and international normalized ratio (INR) levels on presentation is highly suggestive of an ongoing coagulopathic state. Similarly, as reported in the literature, our patient’s D-dimer levels were elevated far out of proportion to abnormalities in the prothrombin time/INR, activated partial thromboplastin time, or platelet count which does not fit the classic criteria of disseminated intravascular coagulopathy but might represent a pathophysiological distinct viral coagulopathy.15
In an autopsy case series of 32 patients who died of COVID-19, 28 patients (88%) revealed widespread micro-thrombosis and/or macro-thrombosis. These thrombi were seen most frequently in the respiratory and cardiovascular systems.8 In another autopsy case series of 10 patients who died of acute respiratory distress syndrome secondary to COVID-19, coronary arteries had no acute thrombus or significant stenosis. Microscopic examination in these patients revealed individual myocyte necrosis, and rarely, adjacent lymphocytes, which did not support a diagnosis of myocarditis.16 The autopsy in our case demonstrated scattered focal ischemic changes throughout the ventricular myocardium in addition to diffuse pulmonary emboli. On pathologic microscopic examination, myocardial necrosis was characterized by hypereosinophilic myocytes with signs of nuclear degeneration but no evidence of myocarditis or pericarditis. We believe these autopsy findings of scattered microscopic cardiomyocyte necrosis likely represented small vessel micro-thrombotic occlusions potentially exacerbated by coagulopathy, hypoxia, hypotension, systemic inflammation, and stress, thus exemplifying a multifactorial etiology. Another less likely etiology is emboli showering from the left atrial thrombus, as reported in cases with embolic myocardial infarction and atrial fibrillation. Autopsy in these cases usually reveals red thrombo-emboli of distal epicardial arteries.17
A baseline ECG is recommended for all hospitalized COVID-19 patients with ST-segment elevation and cTnI being reliable indicators of myocardial infarction.18,19 Our patient’s ECG exhibited ST-segment elevation in the anterolateral leads (I, II, V2, V3, V4, V5, and V6) and elevated cTnI levels (7.457 ng/mL), raising suspicion for STEMI, but compounded by the presence of hypotension, pulmonary consolidation, hypoxia, and respiratory distress requiring intubation. Although early invasive strategy is recommended in high-risk patients with STEMI with mortality benefits, the American College of Cardiology and Society for Cardiovascular Angiography and Interventions recommended pursuing optimal medical treatment in COVID-19 patients and considering the risk of viral transmission to health care workers and other patients before proceeding with percutaneous coronary intervention.20 Conservative medical management was implemented first in our patient with no improvement, and a subsequent LHC demonstrated normal coronaries with no thrombosis or occlusion. These findings question the necessity of LHC in our patient in the first place.
Takotsubo cardiomyopathy can result from the physical and emotional stress associated with COVID-19.21 It is characterized by transient regional wall-motion abnormalities involving the left ventricular apex and mid-ventricle. Typically, echocardiography and ventriculography show akinesis or hypokinesis of the mid and apical segments of the LV with sparing of the basal systolic function, described as apical ballooning. Patients commonly present with ST-segment elevation in the precordial leads with relatively minimal or modest elevation of cardiac enzyme and biomarker levels.22,23 In our case, echocardiography and ventriculography showed diffuse LV hypokinesis without apical ballooning or mid-ventricle wall motion abnormalities. Also, our patient’s cardiac enzymes and biomarkers were significantly elevated making the diagnosis of Takotsubo cardiomyopathy unlikely.
A definitive diagnosis of PE was not made due to pulmonary and hemodynamic instability and the high risk of rapid acute respiratory distress syndrome related decompensation as has been reported in COVID-19. However, the patient was treated with heparin infusion beginning early on admission. A potentially more advantageous treatment pathway could include emergent plasmapheresis to treat the underlying cytokine storm in the earlier stages of the infection at presentation with potentially later intra-arterial thrombolysis with tissue-type plasminogen activator (tPA) or thrombectomy to debulk the PE. Plasmapheresis has been reported to have positive outcomes in COVID-19 patients.24,25 The obvious drawback to this would be the lack of resources to undergo plasmapheresis for every hemodynamically unstable COVID-19 patient with signs of coagulopathy.
Conclusion
Myocardial injury is a potentially fatal complication of SARS-CoV-2 infection with a yet unclear pathophysiology that requires better definition. Given the emergence of the new SARS-CoV-2 mutation with the risk of accelerated transmission and rapid spread, further extensive research with an improved understanding of SARS-CoV-2-induced coagulopathy and widespread vascular thrombosis (micro-thrombotic arterial occlusions and pulmonary emboli) is greatly needed to improve current therapeutic approaches and survival.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Anup Solsi  https://orcid.org/0000-0002-9985-0907
https://orcid.org/0000-0002-9985-0907
References
- 1. Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huang Z, Huang P, Du B, et al. Prevalence and clinical outcomes of cardiac injury in patients with COVID-19: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. 2021;31:2-13. doi: 10.1016/j.numecd.2020.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Babapoor-Farrokhran S, Gill D, Walker J, Rasekhi RT, Bozorgnia B, Amanullah A. Myocardial injury and COVID-19: possible mechanisms. Life Sci. 2020;253:117723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94:e00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tavazzi G, Pellegrini C, Maurelli M, et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911-915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Libby P, Simon DI. Inflammation and thrombosis: the clot thickens. Circulation. 2001;103:1718-1720. [DOI] [PubMed] [Google Scholar]
- 8. Elsoukkary SS, Mostyka M, Dillard A, et al. Autopsy findings in 32 patients with COVID-19: a single-institution experience. Pathobiology. 2021;88:56-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Malas MB, Naazie IN, Elsayed N, et al. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and meta-analysis. EClinicalMedicine. 2020;29:100639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pedersen SF, Ho YC. SARS-CoV-2: a storm is raging. J Clin Invest. 2020;130:2202-2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kaplan B, Sulentic C, Holsapple M, et al. Toxic responses of the immune system. In: Toxicology. McGraw Hill Education. [Google Scholar]
- 13. Kerr R, Stirling D, Ludlam CA. Interleukin 6 and haemostasis. Br J Haematol. 2001;115:3-12. [DOI] [PubMed] [Google Scholar]
- 14. Senchenkova EY, Komoto S, Russell J, et al. Interleukin-6 mediates the platelet abnormalities and thrombogenesis associated with experimental colitis. Am J Pathol. 2013;183:173-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Al-Samkari H, Karp Leaf RS, Dzik WH, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020;136:489-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fox SE, Akmatbekov A, Harbert JL, et al. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8:681-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shibata T, Kawakami S, Noguchi T, et al. Prevalence, clinical features, and prognosis of acute myocardial infarction attributable to coronary artery embolism. Circulation. 2015;132:241-250. [DOI] [PubMed] [Google Scholar]
- 18. Bangalore S, Sharma A, Slotwiner A, et al. ST-segment elevation in patients with Covid-19—a case series. N Engl J Med. 2020;382:2478-2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sandoval Y, Januzzi JL, Jr, Jaffe AS. Cardiac troponin for assessment of myocardial injury in COVID-19: JACC review topic of the week. J Am Coll Cardiol. 2020;76:1244-1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Welt FGP, Shah PB, Aronow HD, et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from the ACC’s Interventional Council and SCAI. J Am Coll Cardiol. 2020;75:2372-2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Singh S, Desai R, Gandhi Z, et al. Takotsubo syndrome in patients with COVID-19: a systematic review of published cases. SN Compr Clin Med. Published online October 6, 2020. doi: 10.1007/s42399-020-00557-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bybee KA, Kara T, Prasad A, et al. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med. 2004;141:858-865. [DOI] [PubMed] [Google Scholar]
- 23. Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408-417. [DOI] [PubMed] [Google Scholar]
- 24. Balagholi S, Dabbaghi R, Eshghi P, et al. Potential of therapeutic plasmapheresis in treatment of COVID-19 patients: immunopathogenesis and coagulopathy. Transfus Apher Sci. 2020;59:102993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Khamis F, Al-Zakwani I, Al Hashmi S, et al. Therapeutic plasma exchange in adults with severe COVID-19 infection. Int J Infect Dis. 2020;99:214-218. [DOI] [PMC free article] [PubMed] [Google Scholar]