Abstract
Purpose
Conceptual frameworks provide the blueprint for exploratory research and intervention development, design, and testing. This paper discusses the utility of and approaches for developing conceptual frameworks using a mixed-methods case study of barriers and facilitators to colorectal cancer (CRC) screening. We provide the context for developing our initial conceptual framework, describe the methods used to examine the constructs in the framework, and discuss the iterative process leading to a revised framework.
Methods
We used three steps to develop the framework: 1) assemble the “right” research team, 2) develop the framework, and 3) diagram the framework. This framework became our guide for developing the research strategy.
Results
Our iterative process recognized the dynamic interplay between constructs and resulted in a revised conceptual framework which depicted more complicated inter-relationships of the different predisposing, enabling, reinforcing, and system-based factors than we had originally understood. The updated framework led to generate new hypotheses and serves as the basis for designing future intervention studies.
Conclusions
A conceptual framework can support hypothesis building and testing. Researchers can use the framework to systematically guide exploratory research and subsequent intervention development.
Keywords: theory, conceptual framework, formative research, intervention design
INTRODUCTION
Health services and community-based research is increasingly expected to be informed by a conceptual framework (CF) based on exploratory research, existing literature, health behavior theories and experiences of the research team [1,2]. While a variety of terms are used (conceptual model, theoretical model) we choose to use the term conceptual framework for the purpose of this discussion. In 1991, Earp and Ennett lamented the paucity of articles about the process of developing these frameworks to depict the links between theory and practice [3]. More than 20 years later, as investigators increasingly engage in translational research using interdisciplinary teams [4], there remains little guidance for developing these conceptual frameworks.
What is a conceptual framework?
Earp and Ennett advocated for “a diagram of proposed causal linkages among a set of concepts believed to be related to a particular public health problem [3],” providing a visual, graphic representation of how the study constructs are related. By incorporating literature that articulates the existing knowledge and experience, frameworks serve as vehicles to more concisely conceptualize research questions that address the gaps identified in the literature review [5]. In exploratory studies, CFs provide context without hypothesizing about either the directionality or the inter-relationships between the components of the framework. A CF can stimulate thinking about the interplay between different theoretical approaches, including systems, social network, social marketing, and individual behavior change theory. The literature provides numerous examples CFs that have been used to guide the developmental stages for studies of chronic illness [6], prevention efforts [7], and practice improvement [8,9]. They can: 1) organize and synthesize related general or complex behavioral processes into a visual representation, 2) allow the research team to share common language, and 3) guide the investigation with regard to study design, data collection and interpretation, and outcome evaluation.
A good CF guides the research design. Once this architecture is created, researchers can develop, adapt, or utilize existing data collection instruments to address the gaps suggested by the framework. A conceptual framework does not dictate a specific study design or set of measures, i.e., qualitative or quantitative, but suggests the factors for investigation. Typically, the research conducted on the basis of the initial CF leads investigators to identify missing pieces of the architecture, and results in a revision of the original CF. The goal of this iterative approach is to arrive at hypotheses that will be tested in an intervention, and the revised CF will depict the hypothesized relationships between the intervention components and the anticipated outcomes.
Below, we discuss the development and utility of a conceptual framework to study barriers and facilitators to screen for colorectal cancer in Southwestern Hispanics and American Indians. We briefly describe the steps used to develop the CF, and provide the revised CF that resulted from our research, showing a more dynamic relationship between the components of the framework than had been originally conceptualized.
The Example: Colorectal Cancer
Colorectal cancer (CRC) is the fourth most frequently diagnosed cancer in New Mexico and the second leading cause of cancer death [10]. Over the past three decades, incidence and mortality rates have significantly declined nationally and among New Mexican non-Hispanic whites [11,12]. However, incidence rates have remained stable or increased among New Mexican Hispanics and American Indians and mortality rates have not declined among American Indians [12]. Modeling studies suggest that increased uptake of CRC screening largely contributed to declining incidence and mortality rates [11]. While the overall percentage of New Mexicans with up-to-date screening (based on the most recent date of colonoscopy, flexible sigmoidoscopy, and/or fecal blood testing) is comparable to the national average [13], the percentage is significantly higher among non-Hispanic whites (58%) than for Hispanics (46%) or American Indians (33%) [12]. In order to develop an intervention to reduce New Mexican disparities in CRC incidence and mortality, we decided to first investigate the factors influencing CRC screening utilization among these two vulnerable populations.
We conducted an exploratory study in collaboration with Research in Outpatient Settings Network (RIOS Net), a practice-based research network of 250+ primary care providers who serve largely minority underserved populations in New Mexico. RIOS Net providers work mainly in community health centers which are often designated as federally qualified health centers (FQHC), Indian Health Service practices, and University of New Mexico academic practices. The study involved RIOS Net clinics serving Hispanic and American Indian patients from rural and urban settings across the state of New Mexico. The goal of our research was to explore the barriers to CRC seen among patients seen by RIOS Net providers and to identify the screening-related factors that could contribute to the CRC disparity in our state. We anticipated that this research would help us revise or reconstruct the framework, contribute to the CRC screening literature, and guide future intervention studies.
METHODS
Process of Developing the Conceptual Framework
Step 1: Assemble the “Right” Research Team.
Given the diversity of factors that could contribute to CRC screening disparities, we assembled a multidisciplinary team to provide a wide diversity of expertise to the framework development process. Over several months of weekly meetings, the research team together created a “collective wisdom” – developing a common language across medical, epidemiological, anthropological, sociological, psychometric, and public health expertise. Table 1 shows the different domains/disciplines and relevant expertise and methodological contributions of each team member. We each presented literature from our respective specialties that summarized known barriers and facilitators for colonoscopy screening in other populations and discussed their implications for our population. These activities helped shape our study questions, emphasizing the importance of building on, rather than replicating, the work of others.
Table 1:
The Multidisciplinary Team: Disciplines, Expertise, and Methodological Contributions
| Domain/Discipline | Expertise | Methodological Contribution |
|---|---|---|
| Content/Epidemiology (RLR, RMH) | CRC, screening, preventive and evidence based medicine | |
| Clinical Practice (RLR, RMH) | Health systems, Practice Based Research | Instruments reflect real clinical context, research can be conducted on the basis of abstracts of clinical data; research in primary care practice networks |
| Patient-provider communication (RMH) | Dynamics of decision making, patient provider interaction | Familiarity with the literature and articulating areas of investigation within the clinical environment and beyond the patient perspective |
| Medical Anthropology (ALS, CMG) | Cultural and socio-ecological context | Development of qualitative interviewing protocols, instruments and analytical approaches |
| Health Literacy, Behavior Change (DLH) | External/predisposing factors | Identification of pre-existing measures and theoretical constructs |
| Measurement (TLW) | Psychometric analyses | Properties of data collection instruments that increase reliability and validity |
Step 2: Develop the Framework.
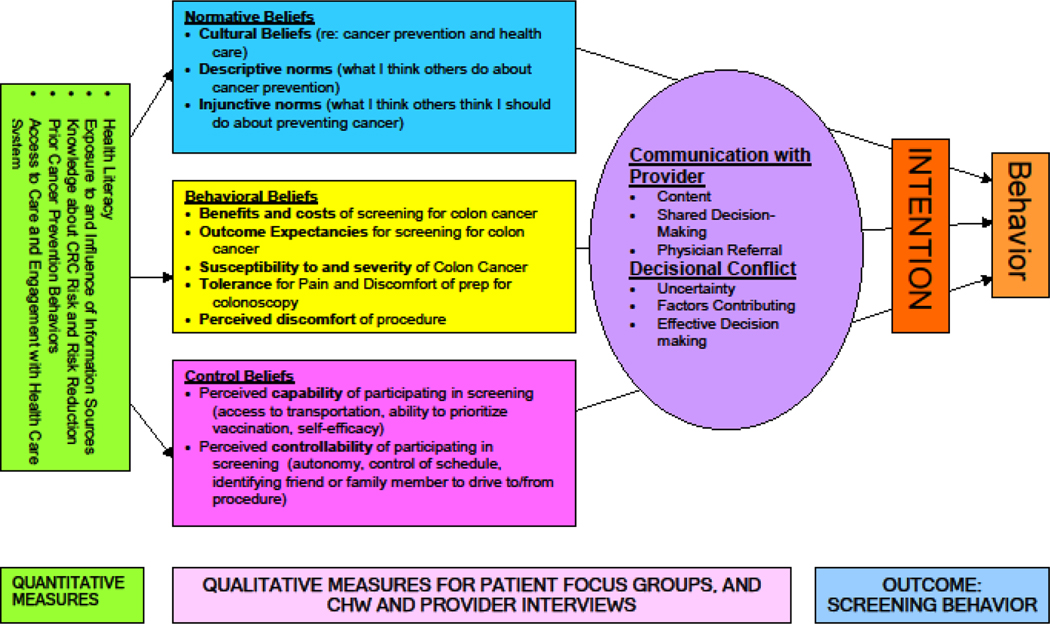
Given our collective experience with research on disparities related to use of preventive strategies for other conditions, we understood that any individual beliefs and behavior would occur in the context of community and cultural norms and practices, systemic factors and health policy influences [14]. Therefore, we constructed the framework to reflect these different “levels” of influence. Team members reviewed the available behavioral and organizational theories that addressed the different components of achieving adequate rates of CRC screening among New Mexican minority populations. Using the PRECEDE-PROCEED framework [15] as a guide, we identified predisposing, enabling and reinforcing factors that might influence CRC screening behaviors. Pre-disposing factors included exposure to knowledge and information about CRC, community and individual experience with cancer, access to screening tests (fecal occult blood test (FOBT), fecal immunochemical test (FIT) and colonoscopy), and other factors known to influence health behavior such as health literacy. Enabling factors included elements from formal behavior change theories. Reinforcing factors included limited elements of the health care system; primarily the influence of patient-provider interaction and decisional conflict, “distress or remorse after a health care decision [16].” Figure 1 depicts the initial CF.
Figure 1:
CRC Initial Conceptual Framework
Step 3: Diagram the Framework.
Our next step was to organize the framework components into a diagram. This process led to a conversation about a rational sequence for integrating the factors from the literature with our own experience with the target populations. However, even though we were working from “known” inter-relationships (e.g., health literacy affects health seeking behavior), we only loosely articulated these relationships given the likely influence of context and culture. In our study, even though CRC screening rates are lower in the Hispanic and American Indian populations, we wanted to avoid assuming that screening barriers would be similar to those observed in other cultural groups. To ensure consensus about the outcome of the above processes, we created a visual blueprint that could be shared by the research team and disseminated for other purposes (e.g., grant applications, recruitment, and presentations). This framework provided a preliminary perspective on the inter-relationships of factors that informed the process of selecting and/or developing measurement tools.
Developing the Research Design and Measures
The CF provided the basis for decisions about the development of a mixed-method research design and data collection measures. For each construct of interest, we determined the most suitable approach to collecting information. We arranged the constructs into two categories, those where validated quantitative measures were available, such as the Health Information National Trends Survey (HINTS) [17] and a health literacy scale [18], and those that were best suited for exploratory/qualitative methods. In our research, we included three different types of participants to explore decision-making processes: patients over the age of 50 eligible for CRC screening (a mixture of those current and not current with screening), RIOS Net primary care providers, and community health workers/nurses. Our patient population was comprised of English speakers and those whose preferred language was not English, so we utilized either bilingual quantitative written instruments (for Spanish) or interview-administered instruments (for American Indian languages), and conducted interviews in the language of choice using interpreters as necessary. Table 2 shows the constructs in the framework and the measures that were used to investigate each identified factor.
Table 2:
Conceptual Framework Constructs
| Construct (PRECEDE- PROCEED) | Construct Components | Measure | Data Collection Strategy |
|---|---|---|---|
| Pre-disposing Factors | Exposure to and influence of information sources, knowledge about cancer risk reduction | Health Information National Trends Survey (HINTS) | Quantitative Survey |
| Prior cancer prevention behaviors | |||
| Access to and engagement with health care and self-efficacy about communication with health care providers | |||
| Health literacy | Validated Health Literacy Scale | ||
| Knowledge of CRC screening tests | Research team | ||
| Enabling Factors | Normative beliefs | Theory of Planned Behavior constructs | Qualitative Interviews |
| Behavioral beliefs | |||
| Control beliefs | |||
| Self-efficacy | |||
| Reinforcing Factors | Communication with provider | Research team | |
| Decisional Conflict | Validated Decisional Conflict Scale |
RESULTS
Revising the Framework
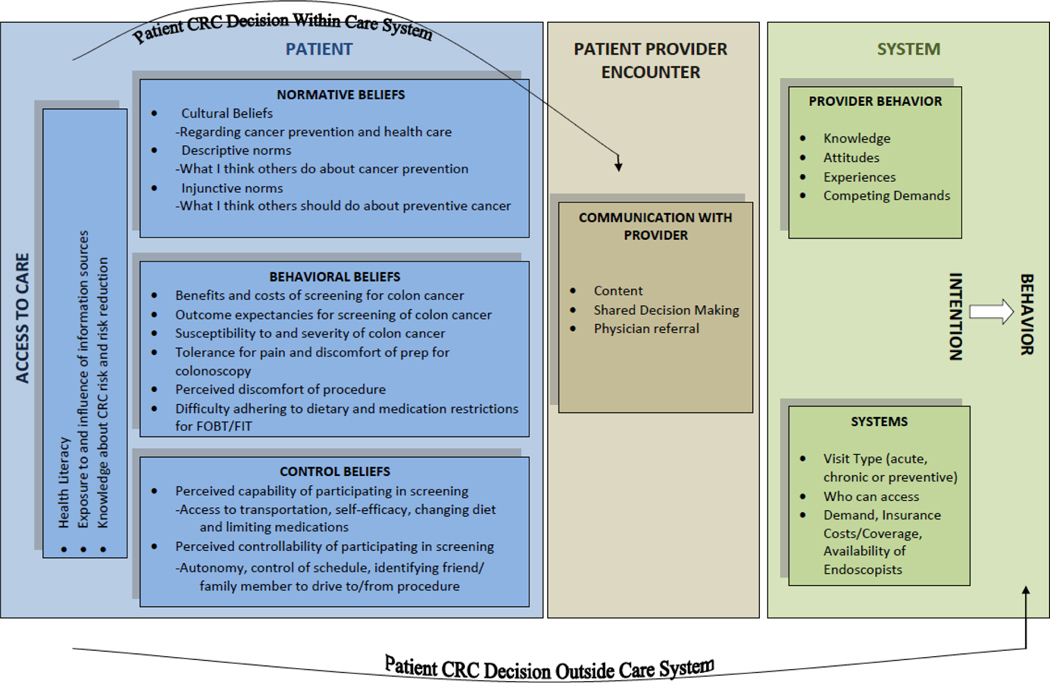
After completing the research, we returned to discussion of the original CF to examine how well it represented, misrepresented or overlooked relationships between the different levels of influence. We discussed how the research results supported, refuted, or identified gaps in our thinking. Here we provide three examples below of how the framework required adjusting: one to remove a factor; the second to add one; and the third to illuminate the role of culture in health seeking behavior. First, we found that the elements of decisional conflict were not mentioned as motivating or inhibiting factors leading to CRC screening behaviors. Therefore, decisional conflict was removed from our framework. Second, we underestimated the influence of the health care system, policies, regulations and resources on provider and patient behavior. Our findings supported recent literature that health systems which do not support adequate opportunities for preventive visits present an important barrier to screening [19, 20]. For study patients, most clinic visits focused on acute or chronic disease management issues. Cancer screening was rarely discussed during these disease management visits, and few patients scheduled preventive visits. Limited resources were also a barrier, particularly the lack of access to health care and dearth of colonoscopy services and trained specialists in rural areas. Therefore, we included the importance of system influences on provider CRC behavior and patient screening decisions in the revised framework. Third, we discovered and incorporated the inhibiting role of machismo (attitudes, behaviors, and qualities associated with masculinity) in CRC screening decisions, especially among recent Mexican male immigrants in the border region of New Mexico [21].
Our iterative process resulted in a revised CF which had a more intricate depiction of the inter-relationships of the different predisposing, enabling, reinforcing and system-based factors (Figure 2). The updated framework has led to the generation of hypotheses for subsequent interventions.
Figure 2:
Revised CRC Framework
DISCUSSION
Our case study demonstrates the inherent benefits to developing a conceptual framework for health behavior/health services/comparative effectiveness research. The following “lessons learned” can guide researchers in developing their own conceptual frameworks. For this theory paper, we use the example of a framework articulating behavioral beliefs and control beliefs related to CRC screening.
The role of team science
The collaborative process involved in developing a conceptual framework serves as a vehicle to facilitate team science, bringing together multidisciplinary expertise to address a specific health problem [22]. The NIH specifically states this as a goal of the Roadmap for future research [23]. Building the framework was essential to developing a common understanding of the CRC screening issues specific to New Mexico and of the current literature on CRC barriers and facilitators, health behavior theory, and contextual factors. Developing a common language among interdisciplinary teams is challenging, but ultimately enriches the research.
Using the literature as a basis for developing the initial model is a way to acknowledge the strengths and limitations of previous research.
The conceptual framework development process required reviewing the relevant literature on screening barriers and facilitators from the team members’ various disciplines. This enabled us to build upon earlier work, identify potential gaps, and question how these findings might differ in our Hispanic and American Indian populations. The team acknowledged that the context of CRC screening in New Mexico (e.g., community and cultural influences among minority populations) was likely to substantially affect the applicability of other findings to our state.
The framework is a dynamic structure.
The framework evolved through an iterative revision process that helped us to identify the range and inter-relationships of relevant factors influencing complex individual and system behaviors. For example, we did not originally anticipate the dynamic between the provider, patient, and system that could facilitate or prevent CRC screening related to colonoscopy. The original framework considered “access to care” as “access to colonoscopy” because we assumed that access to FOBT or FIT would not be constrained by system factors. Throughout the research, we engaged the conceptual framework to test our guiding assumptions and to assess the strength of alternative explanations. Subsequently, some factors were re-conceptualized, allowing us to introduce new constructs or dimensions of influence, or new factors. The new framework is being utilized to articulate hypotheses and design interventions.
The framework is a basis for operationalizing the research.
The framework provides guidance for approaching data collection (e.g., qualitative and/or quantitative). In our study, we adapted previously validated quantitative measures for certain constructs, such as health literacy [17] and prior exposure to cancer prevention information [18]. We also developed unique qualitative measures consisting of patient, community health worker, and provider interview guides to uncover behavioral beliefs and explanatory models not accessible through the quantitative instruments
There are limitations to the framework in identifying and measuring distinct influences on behavior.
During the framework development phase, the investigators are encouraged to refrain from hypothesizing about the factors that affect the health behavior and to articulate “causal” relationships between domains. Sometimes, in fact, creating “naive” hypotheses can lead researchers to divert attention to factors that may not be relevant and away from those more crucial to solving the problem. For example in our research, the first iteration of the framework focused on decisional conflict as a factor in CRC screening uptake and gave insufficient attention to the relationship of the provider and the health system. Based on both the literature and research team experience, we also assumed that one barrier to using a FOBT test would be a “yuck” factor related to stool sampling; however, this did not arise in our findings as an inhibiting factor for CRC screening.
Theoretical constructs and instruments found in the broader literature may not “fit” with the populations and settings of interest.
As researchers review the literature to select theoretical constructs and potentially relevant instruments for data collection, they should consider the context in which the research will be conducted. In some cases, behavioral theories explaining health choices might not be readily transferable across populations. In our case, the literature identified common barriers to CRC screening, but not the specific cultural barriers that we observed in our target populations. For example, we did not anticipate the role of machismo in CRC screening decisions [12]. Before integrating constructs from the literature into the conceptual framework, researchers need to assess whether the explanatory mechanisms are relevant to the current population and/or setting.
A conceptual framework more clearly depicts the relationships between elements.
The framework enables the research team to visualize the potential relationships between factors and realign them as the study progresses [24]. As our revised conceptual framework reveals, we learned that multiple factors at different levels (e.g., the influence of the system on provider availability, visit type, patient-provider communication, and the content of the interaction on CRC screening utilization) influence CRC screening behaviors. Now we are able to hypothesize about the interaction between the domains, providing direction to a subsequent intervention. For example, it might seem self-evident that in order to increase CRC screening, patients must have access to primary care and receive both preventive and chronic care. However, our research showed that the brief primary care visit is often focused on disease management and limits the opportunity to engage in other preventive health topics. The patient may not be cued to CRC screening during chronic or acute care visits, especially when CRC screening is not discussed.
A conceptual framework is useful as a vehicle to engage stakeholders in discussions to guide intervention design and implementation
The framework serves as both a useful vehicle to interpret the research results and as a device to effectively communicate findings and brainstorm solutions/interventions with diverse stakeholder groups [25]. As a result of our exploratory research, we are currently engaging primary care clinicians, community partners, and patients in order to consider how to increase CRC screening without putting stress on the CRC screening delivery system. Preliminary discussions suggest that this can be accomplished by directing patients with a family history to colonoscopy while offering other types of CRC screening to those at lower risk. This iterative process also provided us with an opportunity to return to the literature to determine if there are evidence-based interventions for overcoming screening barriers that can be adapted to our local community contexts.
Conclusion
Our purpose here is to provide an example of how building and utilizing a conceptual framework can establish the architecture for engaging teams of multidisciplinary researchers, designing formative research, revising the CF, discussing interventions, and disseminating results. The development and continued use of a CF serves many important purposes throughout the research continuum. This theoretical approach includes a set of systematic yet flexible steps as a guide for researchers, ideally in the early stages of the research development process.
Acknowledgments:
We would like to acknowledge that financial support for the research presented in this manuscript was provided by the National Cancer Institute (NIH), Grant 5R21CA121066–2.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Jackson C (1997) Behavioral science theory and principles for practice in health education. Health Educ Res 12:143–50. [Google Scholar]
- 2.National Cancer Institute (2005) Theory at a Glance: A Guide for Health Promotion Practice, 2nd edition. Bethesda, MD: National Cancer Institute. [Google Scholar]
- 3.Earp JA, Ennett ST (1991) Conceptual models for health education research and practice. Health Educ Res 6:163–71. [DOI] [PubMed] [Google Scholar]
- 4.Stokols D, Hall KL, Taylor BK, Moser RP (2008) The Science of Team Science: Overview of the Field and Introduction to the Supplement. Am J Prev Med 35: S77–S89. [DOI] [PubMed] [Google Scholar]
- 5.The Encyclopedia of Informal Education. Available at: www.infed.org. Accessed December 13, 2012.
- 6.Weinert CL (2008) Evolution of a conceptual model for adaptation to chronic illness. J Nurs Scholarship.40:364–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickson LM, Dervensky JL, Gupta R (2002) The prevention of gambling problems in youth: A conceptual framework. J Gambl Stud 18:97–159. [DOI] [PubMed] [Google Scholar]
- 8.Solberg LI (2007) Improving medical practice: A conceptual framework. Ann Fam Med 5:251–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anandarajah G (2008) The 3H and BMSEST models for spirituality in multi-cultural whole person medicine. Ann Fam Med 6:448–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62:10–29. [DOI] [PubMed] [Google Scholar]
- 11.Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, et al. (2010) Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 116:544–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffman RM, Stone SN, Viera RL. (2008) Colorectal cancer in New Mexico. A handbook for health care professionals. Albuquerque, NM: New Mexico Department of Health Comprehensive Cancer Program. Available at: http://nmhealth.org/ERD/HealthData/Cancer/FINAL_cpi-04handbook_colorectal.pdf. Accessed February 6, 2012. [Google Scholar]
- 13.U.S. Centers for Disease Control and Prevention (2011) Vital signs: Colorectal cancer screening, incidence, and mortality—United States, 2002–2010. MMWR Morb Mortal Wkly Rep 60:884–89. [PubMed] [Google Scholar]
- 14.McLeroy KR, Bibeau D, Steckler A, Glanz K (1988). An ecological perspective on health promotion programs. Health Educ Quart 15:351–377. [DOI] [PubMed] [Google Scholar]
- 15.Green LW, Kreuter MW, Deeds SG, Partridge KD (1980) Health education planning: A diagnostic approach. Mountain View, CA: Mayfield. [Google Scholar]
- 16.O’Connor AM (1995) Validation of a decisional conflict scale. Med Decis Making 15:25–30. [DOI] [PubMed] [Google Scholar]
- 17.Chew LD, Bradley KA, Boyko EJ (2004) Brief questions to identify patients with inadequate health literacy. Fam Med 36:588–94. [PubMed] [Google Scholar]
- 18.National Cancer Institute. Health information national trends survey. Available at: http://hints.cancer.gov/ Accessed March 7, 2012.
- 19.Guessous I, Dash C, Lapin P, Doroshenk M, Smith RA, Klabunde CN; National Colorectal Cancer Roundtable Screening Among the 65 Plus Task Group. (2010) Colorectal cancer screening barriers and facilitators in older persons. Prev Med 50:3–10. [DOI] [PubMed] [Google Scholar]
- 20.Steinwachs D, Allen JD, Barlow WE, Duncan RP, Egede LE, Friedman LS, Virnig BA (2010) National Institutes of Health State-of-the-Science Conference statement: Enhancing use and quality of colorectal screening. Ann Intern Med 152:663–667. [DOI] [PubMed] [Google Scholar]
- 21.Getrich CM, Sussman AL, Helitzer DL, Hoffman RM, Warner TD, Sánchez V, et al. (2012) Expressions of machismo in colorectal cancer screening among New Mexico Hispanic subpopulations. Qual Health Res 22:546–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hall KL, Feng AX, Moser RP, Stokols D, Taylor BK (2008) Moving the science of team science forward: collaboration and creativity. Am J Prev Med 35:S243–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Institutes of Health. Interdisciplinary Research. nihroadmap.nih.gov/interdisciplinary. Accessed March 7, 2012.
- 24.Cooper LA, Hill MN, Powe NR (2002) Designing and Evaluating Interventions to Eliminate Racial and Ethnic Disparities in Health Care. J Gen Intern Med 17: 477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poland B, Krupa G, McCall D (2009) Settings for health promotion: An analytic framework to guide intervention design and implementation. Health Promot Pract 10:505–16. [DOI] [PubMed] [Google Scholar]