Supplemental Digital Content is available in the text.
Keywords: coronavirus disease 2019, education, global pandemic, pediatric, preparation, simulation, training
OBJECTIVES:
Early preparation for the training and education of healthcare providers, as well as the continuation or modification of routine medical education programs, is of great importance in times of the coronavirus disease 2019 pandemic or other public health emergencies. The goal of this study was to characterize these self-reported efforts by the pediatric simulation community.
DESIGN:
This was a global, multicenter survey developed via a Delphi process.
SETTING:
International survey study.
SUBJECTS:
The survey was sent to 555 individual members of the three largest international pediatric simulation societies (The International Pediatric Simulation Society, International Network for Simulation-based Pediatric Innovation, Research & Education, and Netzwerk Kindersimulation e.V.) between April 27, 2020, and May 18, 2020.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
Description of coronavirus disease 2019 pandemic simulation-based preparation activities of pediatric acute and critical care healthcare providers. The Delphi process included 20 content experts and required three rounds to reach consensus. The survey was completed by 234 participants (42.2%) from 19 countries. Preparation differed significantly between the geographic regions, with 79.3% of Anglo-American/Anglo-Saxon, 82.6% of Indian, and 47.1% of European participants initiating specifically coronavirus disease 2019-related simulation activities. Frequent modifications to existing simulation programs included the use of telesimulation and virtual reality training. Forty-nine percent of institutions discontinued noncoronavirus disease 2019-related simulation training.
CONCLUSIONS:
The swift incorporation of disease-specific sessions and the transition of standard education to virtual or hybrid simulation training modes occurred frequently. The approach used, however, depended heavily on local requirements, limitations, and circumstances. In particular, the use of telesimulation allowed education to continue while maintaining social distancing requirements.
Since December 2019, the world has experienced the pandemic spread of severe acute respiratory syndrome coronavirus 2 disease (1). Preparedness as well as efforts and innovations by healthcare institutions to manage this pandemic are of utmost importance (2). It is critical to learn from others’ simulation-based education efforts and to find ways to continue teaching during times of social distancing as we prepare for future pandemics or disasters (3). To address this, we conducted a survey, developed via a Delphi process, to improve our understanding of the simulation-based response to coronavirus disease 2019 (COVID-19) within the global pediatric simulation community of the three largest pediatric simulation organizations representing 10% of worldwide countries. The specific aims of this study were: 1) to survey pediatric healthcare providers (HCPs) on their preparation for simulation-based medical education of COVID-19 cases and 2) to characterize pediatric simulation-based practices and innovations for non-COVID-19 related contents during the pandemic.
MATERIAL AND METHODS
Study Design
A two-phase study was conducted by three international pediatric simulation societies (The International Pediatric Simulation Society [IPSS], International Network for Simulation-based Pediatric Innovation, Research & Education [INSPIRE], and Netzwerk Kindersimulation e.V. [NKS]) (Fig. 1). This study received exempt status by the Medical University of Vienna’s Institutional Review Board.
Figure 1.
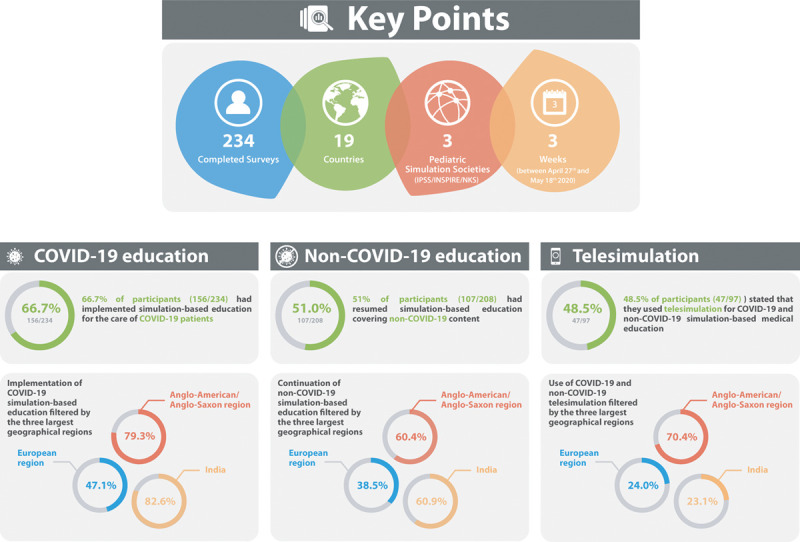
Key points and overview of most important results. COVID-19 = coronavirus disease 2019.
Phase-1: Delphi Process
A three-round Delphi study was conducted, using SurveyMonkey (www.surveymonkey.com). To establish a representative pool of international content experts, 20 members of these three societies (10 members of IPSS/INSPIRE and 10 members of NKS) were asked to participate. In the first round, an initial draft of the survey was distributed among the experts, who were asked to rate the importance of each question and to give suggestions for improvement (4–6). In the second and third rounds, an individual survey was emailed to each expert. Each individual survey contained updated questions, the overall mean ratings from the previous rounds, and their own prior ratings. Delphi participants were again asked to rate each question and (if a question was rated poorly) to suggest amendments. Only questions with ratings exceeding an a priori defined cutoff of 60% of the overall mean value (mean value > 3) were included in the final survey (7).
Phase-2: Online Survey
The final survey was sent to all members of these three societies (NKS: 162 members in five European countries; IPSSW: 307 members in 28 countries; and INSPIRE: 137 members in 20 countries) via SurveyMonkey followed by two reminders, each 4 days apart. Participants were instructed to answer each question according to current local practice. The survey was conducted in English only; therefore, comprehension was evaluated at the end (with ratings on a scale from 1 to 5).
Data Analysis
Categorical data were summarized with absolute and relative frequencies, continuous data using mean and sd, or median and interquartile range, as appropriate. Differences between the countries were analyzed using the chi-square test or Fisher exact test, as appropriate. The corrected p value after Bonferroni correction was set to 0.006. Statistical analysis was performed using IBM SPSS V.26 (SPSS, Chicago, IL).
RESULTS
Participants
A total of 555 different HCPs (excluding duplicate mailings to members of two or all three societies) received the survey, and 234 (42.2%) respondents completed it. Respondents were situated in 19 countries: Argentina, Austria, Australia, Brazil, Canada, Germany, India, Italy, Latvia, Malaysia, New Zealand, Qatar, Saudi Arabia, Sri Lanka, Sweden, Switzerland, United Arab Emirates, United Kingdom, and United States. Key results are summarized in Table 1 and Figure 1. More results available in supplemental material (http://links.lww.com/PCC/B642).
TABLE 1.
Responses for the Three Major Topics: Coronavirus Disease 2019 Simulation, Noncoronavirus Disease 2019 Simulation, and Telesimulation As Well As to Coronavirus Disease 2019 Simulation Topics
| Questions and Answers (Responses, n) | n (%) |
|---|---|
| Specific simulation-based trainings for COVID-19 (n = 234) | 156 (66.7) |
| Real medical equipment for training (n = 130) | Yes |
| Yes, new material in every training | 10 (7.7) |
| Yes, (re)usage of parts of actual PPE | 72 (55.4) |
| Yes, only expired material | 20 (15.4) |
| Other nonessential material/equipment | 57 (43.8) |
| No special trainings for this | 5 (3.8) |
| Other | 16 (12.3) |
| Training frequency (n = 130) | Yes |
| Once | 8 (6.2) |
| Once a month | 6 (4.6) |
| Once a week | 34 (26.2) |
| 2–3 times a week | 57 (43.8) |
| Every day | 21 (16.2) |
| Other | 10 (7.7) |
| Continuation of non-COVID-19 simulation activities (n = 208) | 107 (51.4) |
| Modifications due to COVID-19 (n = 97) | Yes |
| None | 10 (10.3) |
| Smaller numbers of participants | 63 (64.9) |
| Change of training site | 29 (29.9) |
| Change of training mode | 40 (41.2) |
| Other | 48 (49.5) |
| Barriers for continuation (n = 97) | Yes |
| Staffing issues/lack of personal resources | 48 (49.5) |
| Financial issues | 15 (15.5) |
| Logistical issues (i.e., room for training or simulation mannequin) | 32 (33) |
| Time-related issues | 30 (30.9) |
| Infection concerns | 62 (63.9) |
| Hospital regulations | 40 (41.2) |
| Social distancing requirements | 81 (83.5) |
| Lack of other options (i.e., telesimulation) | 12 (12.4) |
| Training with real equipment would be unethical due to acute shortages of PPE for clinical work | 40 (41.2) |
| Other | 8 (8.2) |
| Usage of telesimulation (COVID-19 or non-COVID-19) (n = 97) | 47 (48.5) |
| Location of learners (n = 47) | Yes |
| In situ with the simulation mannequin in their working environment | 8 (17) |
| In our simulation center with the simulation mannequin | 12 (25.5) |
| At home at their screen while confederates are with the simulation mannequin | 32 (68.1) |
| Other | 10 (21.3) |
| Software (n = 47) | Yes |
| Local simulation software’s telesimulation function | 11 (23.4) |
| Zoom | 29 (61.7) |
| Google Hang-outs | 2 (4.3) |
| Skype | 7 (14.9) |
| Microsoft Teams | 14 (29.8) |
| Other | 20 (42.6) |
COVID-19 = coronavirus disease 2019, PPE = personal protective equipment.
COVID-19 Specific Trainings
In total, 66.7% of participants (156/234) implemented COVID-19 specific simulation training. We filtered the responses for the three largest geographical areas (European [excluding United Kingdom] vs Anglo-American/Anglo-Saxon [United Kingdom, United States, Canada, Australia, and New Zealand] countries vs India). Although United Kingdom geographically belongs to Europe, the healthcare system is different from most other European countries and more similar to the system in other English-speaking countries. Analyzed by geographical area: 47.1% in the European Region (41/87), 79.3% in the Anglo-American/Anglo-Saxon region (88/111), and 82.6% in India (19/23) conducted COVID-19 specific simulation trainings. Differences between the Europe and Anglo-American/Anglo-Saxon regions, and Europe and India were statistically significant (p < 0.001, p = 0.002).
Modalities for COVID-19 Simulation-Based Education
Personal protective equipment (PPE) training was most commonly conducted using videos (78.5% [102/130]) and in situ training (76.2% [99/130]). Airway management training and training of cardiopulmonary resuscitation of (suspected) COVID-19 patients were most often delivered in situ (78.5% and 63.1%, respectively).
Non-COVID-19 Simulation-Based Education
Fifty-one percent (107/208) of respondents continued non-COVID-19-related simulation. Analyzed by geographical area, 38.5% in the European Region (30/78), 60.4% in the Anglo-American/Anglo-Saxon region (58/96), and 60.9% in India (14/23) continued non-COVID-19-related simulations. There was a statistically significant difference between Europe and the Anglo-American/Anglo-Saxon area (p < 0.004). Ten percent of respondents (10/97) had not implemented any training modifications. The most common modifications and barriers are shown in Table 1.
Use of Telesimulation
Altogether 48.5% (47/97) initiated telesimulation activities both for COVID-19 and non-COVID-19 educations. Telesimulation was a novel technology for 80.9% (38/47) and was replacing a live-simulation curriculum in 68.1% (32/47).
DISCUSSION
The COVID-19 pandemic has significantly influenced medical education and simulation training worldwide. We uncovered significant differences between the intercontinental geographic regions in terms of COVID-19 preparatory simulations and continuation of non-COVID-19-related simulations. Although most participants in the Anglo-American/Anglo-Saxon region (79.3%) and in India (82.6%) initiated educational activities for the care of COVID-19 patients, this was only true for 47.1% of European respondents. This could reflect heterogeneity in HCP willingness to adopt and promote such training modalities and/or a potential lack of support from institutions or superiors across these regions (8–10). In situ simulation was the most prevalent training mode for COVID-19 simulations. It allows for immediate practice and testing of new processes and procedures, such as handling PPE (11–13). Airway management and cardiopulmonary resuscitation were the most prevalent topics of COVID-19-related simulations, an unsurprising finding given the high infection risk these procedures pose (14).
Interestingly, non-COVID-19 simulations were also continued during the lockdown phase in some areas, although this varied significantly by region. The differences in use of telesimulation were most striking, as many resource-rich regions did not adopt their approach as frequently as expected. Stricter data safety regulations in Europe may also have influenced this (15). Adoption of telesimulation could have helped simulation programs continue prior activities early in the pandemic decreasing infection concerns (16, 17). Further exploration of these observations further characterizing and understanding different telesimulation or virtual reality interventions may be valuable and could yield important insights regarding regional preparedness.
Although IPSS and INSPIRE have an Anglo-American/Anglo-Saxon dominance, NKS is mostly present in German-speaking countries in Europe, which might have neglected responses from other countries in Europe that reported more severe pandemic progression, for example, France and Spain. In addition, despite the attempt to obtain an international sample, only about 10% of global countries were represented with a notable absence of countries with large population: for example, China. Furthermore, response bias is also possible, as more active members of each organization were more likely to answer this survey. More than one member from each institution might have represented their simulation practice, since this survey was conducted in a deidentified manner. This might have resulted as the overrepresentation of larger healthcare systems. To evaluate the practice differences across different areas of the world, we used a chi-square test (Fisher exact test). However, the comparison was made for Europe versus Anglo-America/Anglo-Saxony versus India, not on a country level, as this was not appropriate due to small sample sizes. Furthermore, the results are limited to a demographic description of impact or outcome variables. Finally, the described geographical differences could in part be explained by different outbreak onsets and varying legal restrictions.
CONCLUSIONS
Three leading international pediatric simulation societies (NKS, IPSS, and INSPIRE) collaborated to conduct a global survey of simulation training during COVID-19. Early preparation to continue medical education programs in times of a pandemic or other public health emergencies is very important and depends heavily on local requirements, limitations, and circumstances. In the future, new technology such as telesimulation or virtual reality might offer a method to continue education and simulation training while maintaining social distance.
ACKNOWLEDGMENTS
We thank for the contributions of members of the International Network for Simulation-based Pediatric Innovation, Research and Education, the International Pediatric Simulation Society, and Netzwerk Kindersimulation e.V., facilitating the distribution of and the response to our survey. We also thank Jonathan Duff, Ashley Keilman, Travis Whitfill, Brittany Dahlen, Cara Doughty, Leah Mallory, Mark Adler, Mark Cicero, Nancy Tofil, Reinis Balmaks, Alex Staffler, Anja Grosse Lordemann, Annika Paulun, Ellen Heimberg, Katharina Bibl, Nicole Mueller, Roland Berger, Thomas Hoppe, Thomas Werner, and Timm Freudenberg for serving as content expert reviewers during the Delphi process.
Supplementary Material
Footnotes
*See also p. 590.
Drs. Wagner and Gross conceptualized and designed the study, drafted the initial article, and reviewed and revised the article. Dr. Jaki, Dr. Löllgen, Dr. Mileder, Dr. Eibensteiner, Mr. Ritschl, Dr. Steinbauer, Mr. Gottstein, Dr. Abulebda, and Dr. Calhoun designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the article. All authors approved the final article as submitted and agree to be accountable for all aspects of the work.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/pccmjournal).
Dr. Calhoun’s institution received funding from Sanofi Pasteur and he received funding from the Society for Simulation in Healthcare. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Zhu N, Zhang D, Wang W, et al. : A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382:727–733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chou R, Dana T, Buckley DI, et al. : Epidemiology of and risk factors for coronavirus infection in health care workers: A living rapid review. Ann Intern Med 2020; 173:120–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aron DC, Headrick LA: Educating physicians prepared to improve care and safety is no accident: It requires a systematic approach. Qual Saf Health Care 2002; 11:168–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iglesias CP, Thompson A, Rogowski WH, et al. : Reporting guidelines for the use of expert judgement in model-based economic evaluations. Pharmacoeconomics 2016; 34:1161–1172 [DOI] [PubMed] [Google Scholar]
- 5.Hsu CC, Sandford BA: The Delphi technique: Making sense of consensus. Pract Assess Res Evaluation 2007; 12:1–8 [Google Scholar]
- 6.Eibensteiner F, Ritschl V, Ariceta G, et al. : Rapid response in the COVID-19 pandemic: A Delphi study from the European Pediatric Dialysis Working Group. Pediatr Nephrol 2020; 35:1669–1678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hasson F, Keeney S, McKenna H: Research guidelines for the Delphi survey technique. J Adv Nurs 2000; 32:1008–1015 [PubMed] [Google Scholar]
- 8.Wagner M, Heimberg E, Mileder LP, et al. : Status quo in pediatric and neonatal simulation in four central European regions: The DACHS survey. Simul Healthc 2018; 13:247–252 [DOI] [PubMed] [Google Scholar]
- 9.Fandler M, Habersack M, Dimai HP: Have “new” methods in medical education reached German-speaking Central Europe: A survey. BMC Med Educ 2014; 14:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stocker M, Laine K, Ulmer F: Use of simulation-based medical training in Swiss pediatric hospitals: A national survey. BMC Med Educ 2017; 17:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ellison AM, Kotelchuck M, Bauchner H: Standard precautions in the pediatric emergency department: Knowledge, attitudes, and behaviors of pediatric and emergency medicine residents. Pediatr Emerg Care 2007; 23:877–880 [DOI] [PubMed] [Google Scholar]
- 12.Visentin LM, Bondy SJ, Schwartz B, et al. : Use of personal protective equipment during infectious disease outbreak and nonoutbreak conditions: A survey of emergency medical technicians. CJEM 2009; 11:44–56 [DOI] [PubMed] [Google Scholar]
- 13.Seale H, Corbett S, Dwyer DE, et al. : Feasibility exercise to evaluate the use of particulate respirators by emergency department staff during the 2007 influenza season. Infect Control Hosp Epidemiol 2009; 30:710–712 [DOI] [PubMed] [Google Scholar]
- 14.European Resuscitation Council European Resuscitation Council COVID-19 Guidelines. 2020. Available at: https://erc.edu/sites/5714e77d5e615861f00f7d18/content_entry5ea884fa4c84867335e4d1ff/5ea885f34c84867335e4d20e/files/ERC_covid19_pages.pdf?1588257310. Accessed December 7, 2020 [DOI] [PMC free article] [PubMed]
- 15.Frielitz FS, Storm N, Hiort O, et al. : [The creation of a data protection policy: A guide to telemedicine healthcare projects]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2019; 62:479–485 [DOI] [PubMed] [Google Scholar]
- 16.McCoy CE, Sayegh J, Alrabah R, et al. : Telesimulation: An innovative tool for health professions education. AEM Educ Train 2017; 1:132–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gross IT, Whitfill T, Auzina L, et al. : Telementoring for remote simulation instructor training and faculty development using telesimulation. BMJ Simulation and Technology Enhanced Learning 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


