Abstract
Background
Headache after cervical or lumbar puncture has long been attributed to early mobilization; however, there is little evidence for this. We performed a systematic literature review and meta-analysis of randomized controlled trials to assess whether longer bed rest is better than immediate mobilization or short bed rest in preventing headache.
Methods
We searched EMBASE (1988 to March 2001), MEDLINE (1966 to May 2001), Pascal Biomed (1996 to February 2001), Current Contents (1997 to September 1999), PsycINFO (1966 to May 2001), the Cochrane Controlled Trial Register (last search May 15, 2001), textbooks and references of the papers selected. Studies were eligible if patients underwent cervical or lumbar puncture for any reason and were randomly assigned to either a long or a short period of bed rest. Data were abstracted independently by 2 investigators to a predefined form.
Results
We found 16 randomized controlled trials involving 1083 patients assigned to immediate mobilization or a short period of bed rest (up to 8 hours) and 1128 patients assigned to a longer period of bed rest (0.5 to 24 hours). Puncture was performed for anesthesia (5 trials), myelography (6 trials) and diagnostic reasons (5 trials). None of the trials showed that longer bed rest was superior to immediate mobilization or short bed rest for preventing headache after puncture. When pooling the results of the trials in the myelography group and the diagnostic group, the relative risks of headache after puncture were 0.93 (95% confidence interval [CI] 0.81–1.08) and 0.97 (95% CI 0.79–1.19) respectively. We did not pool the results from the trials in the anesthesia group because of clinical heterogeneity, but shorter bed rest appeared to be superior.
Interpretation
There was no evidence that longer bed rest after cervical or lumbar puncture was better than immediate mobilization or short bed rest in reducing the incidence of headache.
Headache is a frequent problem following cervical or lumbar puncture. Several textbooks recommend bed rest to prevent headache.1,2,3,4,5,6,7,8,9 Bed rest, ranging from a few hours up to 24 hours, is frequently used in several countries. A relatively recent survey of neurology and neurosurgery departments in the United Kingdom showed that bed rest between 6 and 24 hours is practised in 10% of the centres and bed rest between 1 and 6 hours in 70%.10 In a survey conducted in France, bed rest to prevent headache after epidural anesthesia was reported in 76% of obstetric units surveyed, lasting up to 24 hours in 46% of the institutions.11 In an Austrian survey, 24 hours of bed rest after lumbar puncture was practised in 48% of the country's neurological departments.12 In Sweden, the average duration of bed rest was reported to be less than 3 hours.13
We performed a systematic literature review and meta-analysis of randomized controlled trials to assess whether longer bed rest is better than immediate mobilization or short bed rest in preventing headache after cervical or lumbar puncture.
Methods
We searched EMBASE (1988 to March 2001), MEDLINE (1966 to May 2001), Pascal Biomed (1996 to February 2001), Current Contents (1997 to September 1999), PsycINFO (1966 to May 2001) and the Cochrane Controlled Trial Register (last search May 15, 2001) for relevant articles. The search strategy was as follows: (“headache,” “cephalea” or “cephalalgia”) and (“bed rest,” “bedrest,” “bed-rest,” “posture,” “recumbency” or “recumb*”) and (“lumbar,” “postlumbar,” “spinal,” “dural,” “puncture,” “punct*” or “postpunct*”) and (“randomised,” “randomized” or “randomi*”). We also searched textbooks (Appendix 1) and references of papers retrieved in the electronic search for relevant references. We did not attempt to find unpublished studies. There were no language restrictions.
Studies were eligible if patients underwent lumbar or cervical puncture for any reason and were randomly assigned to either a long or a short period of bed rest. We made no restrictions in terms of absolute duration of bed rest. Furthermore, we required that the occurrence of headache (our end point) was recorded in absolute numbers.
Two of us (J.T. and H.H.) abstracted data independently to a predefined form. In addition to data on intervention and outcome, we recorded study characteristics such as reason for the lumbar or cervical puncture, age, sex, needle size and how the puncture was performed. We also recorded whether the authors specified that the outcome was postpuncture headache (generally defined as pain increase in the upright position and decrease in the recumbent position). If postpuncture headache was specified, we used the definition given by the authors; otherwise we used the incidence of any headache.
We recorded whether the trial was reported according to the CONSORT criteria,14 the most important being the blinding of the assessor of the end point to the intervention and inention-to-treat analysis of the data. Because of the nature of the intervention, the patients always knew their treatment assignment, which may have unblinded the assessor.
We intended to combine data quantitatively if clinical heterogeneity was assumed to be negligible or irrelevant and if there was no evidence of statistical heterogeneity. Clinical heterogeneity may be caused by differences in study populations, interventions or definitions of the end point.15 In cases of severe heterogeneity we did not pool the data, because the trials may have measured a different effect altogether. We assessed statistical heterogeneity using the χ2 test, with a p value of less than 0.05 indicating significance. We used a fixed-effects model for quantitative data synthesis.
We drew a funnel plot to assess whether there was evidence of publication bias. The standard normal deviate of the relative risk (natural logarithm of the relative risk divided by its standard error) was plotted against the estimate's precision (inverse of the standard error). We then used linear regression analysis to regress the standard normal deviate against precision. Significant publication bias or heterogeneity was likely if the constant of the regression equation did not equal zero, indicated by a p value of less than 0.1.16 We used the trim-and-fill method to assess the impact of potential publication bias and the robustness of the estimate.17,188 This is a simple method by which “asymmetric” trials are identified — visually in our study — in the funnel plot and excluded (“trimmed”). Thereafter, the true centre of the funnel is estimated, and the trimmed trials are reinserted and mirrored to the opposite direction using the new centre of the funnel plot as the axis (“filled”). An adjusted pooled estimate was then calculated. We assessed robustness of the model by comparing the new estimate with the unadjusted estimate as a kind of sensitivity analysis.
Results
Trial characteristics
Fig. 1 shows how the trials were identified. A total of 16 randomized controlled trials were included in the final analysis,13,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33 involving 1083 patients assigned to immediate mobilization or a short period of bed rest and 1128 patients assigned to a longer period of bed rest (Fig. 2).

Fig. 1: Selection process of randomized controlled trials for meta-analysis.
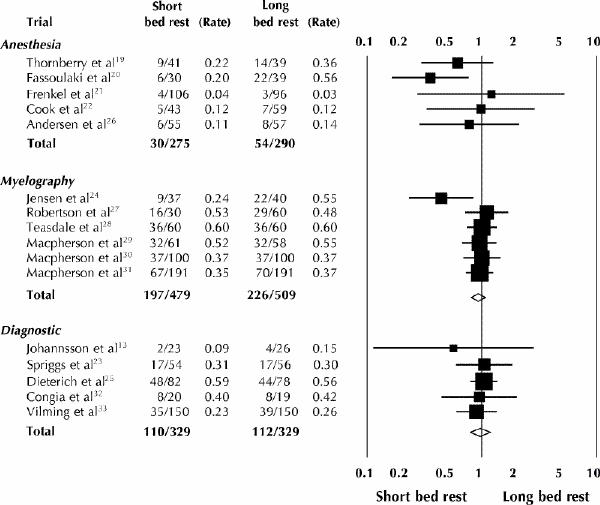
Fig. 2: Absolute and relative effect size for short bed rest versus long bed rest to prevent headache after lumbar or cervical puncture. (An expanded version of the figure, with relative risks and 95% confidence intervals, is available online at www.cma.ca/cmaj/vol-165/issue-10/pdf/thofig2.pdf).
Cervical or lumbar puncture was used to administer anesthesia (in 5 trials), to perform myelography (in 6 trials) and for diagnostic reasons (in 5 trials). Eleven studies compared immediate mobilization with bed rest (from 30 minutes to 24 hours); the remaining 5 studies compared a short period of bed rest (from 30 minutes to 8 hours) with a longer period (from 4 to 24 hours).
Overall, there was clinical heterogeneity not only in terms of the reason for the puncture and the duration of bed rest but also in general patient characteristics (Table 1, available online at www.cma.ca/cmaj/vol-165/issue-10/pdf/thotable1s.pdf): 1 study included only young women in labour,19 1 study enrolled only elderly men20 and another study included only young men.21
Several of the studies provided insufficient clinical details (e.g., age, sex and needle size) to allow adequate assessment of clinical heterogeneity (Table 2, available online at www.cma.ca/cmaj/vol-165/issue-10/pdf/thotable2s.pdf). In 2 studies the results were not analyzed according to the intention-to-treat principle;22,23 in the remaining studies, most likely no patients were excluded, but this detail was not explicitly mentioned. The investigator assessing the outcome was most likely not blinded to the intervention in 8 studies.
In general the quality of reporting was not satisfactory (Table 3, available online at www.cma.ca/cmaj/vol-165/issue-10/pdf/thotable3s.pdf).
There was no evidence of statistical heterogeneity with use of the χ2 test (χ2 = 14.5, 14 degrees of freedom [df], p = 0.42), which does not rule out heterogeneity because of low sensitivity. Visual inspection of the funnel plot (Fig. 3) showed that 3 studies were outliers; 2 were published in the English language,19,20 the third in Danish.24 The constant of the regression model for the funnel plot was –1.02 (95% confidence interval [CI] –2.1 to 0.04), a p value of 0.06 indicating possible bias or heterogeneity.
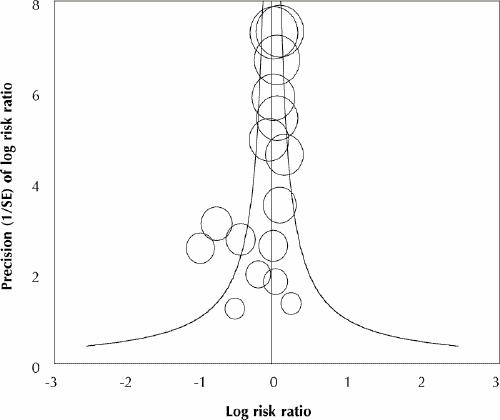
Fig. 3: Funnel plot, to assess whether there is evidence of publication bias. The standard normal deviate of the relative risk (natural logarithm of the relative risk divided by its standard error [SE]) is plotted against the estimate's precision (inverse of the SE).
Effect of bed rest on postpuncture headache
We did not combine the results over all the trials because we believe that the 3 reasons for puncture represented relevant clinical heterogeneity. Therefore, we stratified the trials according to the 3 reasons for puncture.
Anesthesia
The long period of bed rest was 24 hours in all 5 trials. The short period of bed rest ranged from immediate mobilization to 8 hours (Table 1 [available online]). This group of trials had a high degree of clinical heterogeneity: 1 trial included only elderly men who underwent spinal anesthesia for transurethral resection of the prostate,20 1 trial included only women who received spinal anesthesia for cesarean section,19 and 1 trial included only young men.21 One trial20 had an extreme effect size in favour of short bed rest (Fig. 2). Even though there was no statistical heterogeneity (χ2 = 3.7, 4 df, p = 0.45), we did not attempt overall quantitative data synthesis because of clinical heterogeneity. None of the studies, however, showed that long bed rest was superior to immediate mobilization or short bed rest in preventing postpuncture headache in any of the clinical situations described (Fig. 2).
Myelography
Most of the 6 studies in this group did not give sufficient information on patient characteristics (e.g., age and sex). All compared immediate mobilization with bed rest of 12 hours (1 trial) or 24 hours (5 trials). One trial24 had an extreme effect size in favour of immediate mobilization (Fig. 2). There was no statistical heterogeneity (χ2 = 6.3, 5 df, p = 0.45). If we assume sufficient clinical homogeneity (which is certainly unproven), the pooled effect size indicated no benefit of bed rest over immediate mobilization (relative risk 0.93, 95% CI 0.81 to 1.08).
Diagnosis
The participants in the 5 trials in which lumbar puncture was performed for diagnostic reasons were comparable in terms of age and sex. Patients in the short bed rest group were mobilized immediately in 4 trials and after 30 minutes in 1 trial. Those in the long bed rest group were mobilized after 30 minutes in 1 trial and after 4 to 24 hours in the remaining trials. There was no statistical heterogeneity (χ2 = 0.9, 4 df, p = 0.93). None of the trials showed a significant effect in favour of long bed rest over short bed rest. When combining the trials quantitatively, we found no effect in favour of long bed rest (relative risk 0.97, 95% CI 0.79 to 1.19).
Sensitivity analysis
When we excluded the 2 outright outliers (Fig. 2),20,24 the regression analysis for the funnel plot showed no evidence of bias or heterogeneity (constant 0.4, 95% CI 1.0 to 1.7, p = 0.15).
If publication bias were present, we would want to estimate its impact on the effect size. We visually identified 3 outlying trials (Fig. 3): 2 in the anesthesia group19,20 and 1 in the myelography group.24 If we ignore clinical heterogeneity and combine the anesthesia trials, the pooled relative risk of long bed rest compared with short bed rest is 0.62 (95% CI 0.41 to 0.93). When we used the trim-and-fill method, the adjusted effect size was greatly reduced toward unity (relative risk 0.96, 95% CI 0.69 to 1.32), which indicates that the findings would be sensitive to publication bias, if present.
When we applied the trim-and-fill method to the myelography group, which also had an outlying trial,24 the pooled effect size was only slightly reduced (relative risk 0.99, 95% CI 0.86 to 1.14). This indicates that, if publication bias were present, it most likely would not influence the findings.
We did not apply the trim-and-fill method to the diagnostic group of trials because there were no outliers and publication bias seemed not to be a problem here. Exclusion of the trial in which immediate mobilization was compared with mobilization after 30 minutes25 influenced the pooled effect size only marginally (relative risk 0.93, 95% CI 0.69 to 1.24).
Interpretation
We found no evidence that longer bed rest after cervical or lumbar puncture was better than immediate mobilization or short bed rest in reducing the incidence of headache after diagnostic puncture, myelography or spinal anesthesia. At worst, bed rest may even cause headache in particular patient groups: in a trial involving patients who received spinal anesthesia20 and in another involving patients who underwent puncture for myelography,24 headache occurred more frequently in those with long bed rest than in those with short or no bed rest. The quality of most trials was, however, only moderate.
We tried to address any kind of known bias; in particular we addressed publication bias by including papers published in any language. Indeed, we found 5 papers not published in English, 1 of which had a surprisingly large effect size.24 We did not attempt to identify unpublished papers. Even though we cannot be sure, it seems unlikely that studies with a relevant, or statistically significant, effect size remain unpublished, and according to the funnel plot, it seems that the asymmetry is not caused by a lack of small studies with negative results but rather by 2 small trials with an extreme effect size.20,24 For the anesthesia group of trials, publication bias seems possible, and if present it may overestimate the effect. Publication bias is apparently not a problem for the trials investigating bed rest after puncture for diagnostic reasons or myelography.
Our exclusion of grey literature (unpublished studies, with limited distribution) may lead to exaggerated estimates of intervention effectiveness.34 The pooled effect size in our meta-analysis of the long bed rest compared with immediate mobilization or short bed rest is already very close to 1 (no effect), with a sufficiently narrow 95% CI furthermore, so a further reduction would not influence our conclusion. The pooled effect size in the myelography group of trials was also not sensitive to the trim-and-fill method.
When clinical heterogeneity is present, quantitative synthesis of outcome data is inappropriate, because the groups are simply not comparable. Statistical heterogeneity is either the result of undetected clinical heterogeneity or a true effect. In the first case, data should not be pooled, and in the second case, there are methods to deal with it.35
The quality of reporting was in general not satisfactory, especially when rigorous standards were applied.14 When examining the articles, none of us had the impression that any of the studies was obviously invalid. However, it is hard to say how much the quality of reporting was associated with the internal validity of these studies, even though there is good evidence that low-quality trials increase the effect size.36,37 As mentioned earlier, there was evidence of no effect, or a clinically irrelevant effect, in most of the trials.
Two systematic reviews have addressed this topic: a review of bed rest as a poorly evaluated but frequently prescribed therapy for a wide range of diseases,38 and a report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology.39 In the first review the authors searched only MEDLINE and the Cochrane Controlled Trial Register, and in the second review the authors searched only MEDLINE.
In addition to the 10 randomized controlled trials identified by these 2 reviews, we could identify another 6 randomized controlled trials, 4 of which were published in languages other than English, and all but 1 showed no difference in outcome between long bed rest and short bed rest. Thus, our review provides currently the most comprehensive information necessary for evidence-based health care.
In conclusion, we found no evidence that longer bed rest after cervical or lumbar puncture is better than immediate mobilization or short bed rest in reducing the occurrence of headache.
Acknowledgments
We thank Alfons Lüftenegger, who helped with the translation of the Scandinavian articles.
Appendix 1.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. Marcus Müllner, University Klinik für Notfallmedizin, Allgemeines Krankenhaus Wien, Währinger Gürtel 18-20 / 6D, A-1090, Vienna, Austria; fax +431 40400 1965; marcus.muellner@univie.ac.at
References
- 1.Northfield DWC. Headache associated with intracranial hypertension and hypotension. In: Vinken PJ, Bruyn GW, editors. Handbook of clinical neurology. Vol 5. Amsterdam: North Holland Publishing Company; 1968. p. 56-74.
- 2.Dalmer J. Lumbal- und subokzipitalpunktion. In: Quandt J, Sommer H, editors. Neurologie, Grundlagen und Klinik. 2nd ed. Stuttgart: Gustav Fischer Verlag; 1982. p. 123-39.
- 3.Gunderson CH. Essentials of clinical neurology. New York: Raven Press; 1990.
- 4.Suchenwirth R, Kendel K. Klinische Neurologie. 4th ed. Stuttgart: Gustav Fischer Verlag; 1990.
- 5.Hahn JM. Checkliste Innere Medizin. Stuttgart: Georg Thieme Verlag; 1997.
- 6.Klingelhöfer J, Spranger M. Klinikleitfaden Neurologie, Psychiatrie. Stuttgart: Gustav Fischer Verlag; 1997.
- 7.Mumenthaler M, Mattle H. Neurologie. 10th ed. Stuttgart, New York: Georg Thieme Verlag; 1997.
- 8.Gleixner C, Müller M, Wirth S. Neurologie und Psychiatrie. Breisach: Medizinische Verlags und Informationsdienste; 1998.
- 9.Poeck K, Hacke W. Neurologie. 10th ed. Berlin, Heidelberg, New York: Springer-Verlag; 1998.
- 10.Serpell MG, Haldane GJ, Jamieson DRS, Carson D. Prevention of headache after lumbar puncture: questionnaire survey of neurologists and neurosurgeons in United Kingdom. BMJ 1998;316:1709-10. [DOI] [PMC free article] [PubMed]
- 11.Souron V, Simon L, Hamza J. Dural taps in peridural analgesia for labor: management by French anethesiologists in 1997. Ann Fr Anesth Reanim 1999;18:941-8. [DOI] [PubMed]
- 12.Thoennissen J, Lang W, Laggner AN, Müllner M. Bettruhe nach lumbalpunktion: eine österreichweite umfrage. Wien Klin Wochenschr 2000;112:1040-3. [PubMed]
- 13.Johannsson G, Bertholds E, Hakansson S. Planläge efter lumbalpunktion onödigt och tidskrävande. Lakartidningen 1992;98:4030-1. [PubMed]
- 14.Altman DG. Better reporting of randomised controlled trials: the CONSORT statement. BMJ 1996;313:570-1. [DOI] [PMC free article] [PubMed]
- 15.Thompson SG. Why sources of heterogeneity in meta-analysis should be investigated. In: Chalmers I, Altman DG, editors. Systematic reviews. London (UK): BMJ Publishing Group; 1995. p. 48-63.
- 16.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [DOI] [PMC free article] [PubMed]
- 17.Sutton AJ, Duval SJ, Tweedie, RL, Abrams KR, Jones DR. Empirical assessment of effect of publication bias on meta-analyses. BMJ 2000;320:1574-7. [DOI] [PMC free article] [PubMed]
- 18.Gilbody SM, Song F, Eastwood AJ, Sutton A. The causes, consequences and detection of publication bias in psychiatry. Acta Psychiatr Scand 2000;102:241. [DOI] [PubMed]
- 19.Thornberry EA, Thomas TA. Posture and post-spinal headache. Br J Anaesth 1988;60:195-7. [DOI] [PubMed]
- 20.Fassoulaki A, Sarantopoulos C, Andreopoulou K. Is early mobilisation associated with lower incidence of postspinal headache? A controlled trial in 69 urologic patients. Anaesthesiol Reanim 1991;16:375-8. [PubMed]
- 21.Frenkel C, Altscher T, Groben V, Hörnchen U. Inzidenz von postspinalem Kopfschmerz in einem jungen Patientenkollektiv. Anaesthesist 1992;41:142-5. [PubMed]
- 22.Cook PT, Davies MJ, Beavis RE. Bed rest and postlumbar puncture headache: the effectiveness of 24 hours' recumbency in reducing the incidence of postlumbar puncture haedache. Anaesthesia 1989;44:389-91. [DOI] [PubMed]
- 23.Spriggs DA, Burn DJ, French J, Cartlidge NEF, Bates D. Is bed rest useful after diagnostic lumbar puncture? Postgrad Med J 1992;68:581-3. [DOI] [PMC free article] [PubMed]
- 24.Jensen TT, Eggert W, Hansen KF, Fink M. Bivirkninger efter lumbal metrizamid-myelografi hos oppengaende og sengeliggende patienter. Ugeskr Laeger 1987;147:2016-7. [PubMed]
- 25.Dieterich M, Brandt TH. Is obligatory bed rest after lumbar puncture obsolete? Eur Arch Psychiatr Neurol Sci 1985;235:71-5. [DOI] [PubMed]
- 26.Andersen APD, Wanscher MCJ, Hüttel MS. Postspinaler Kopfschmerz. Ist die 24stündige Bettruhe eine Prophylaxe? Reg Anaesth 1986;9:15-7. [PubMed]
- 27.Robertson WD, Lapointe JS, Nugent RA, Robinson RG, Daly LF. Positioning of patients after metrizamide lumbar myelography. AJR Am J Roentgenol 1980;134:947-8. [DOI] [PubMed]
- 28.Teasdale E, Macpherson P. Incidence of side effects following direct puncture cervical myelography, bed rest versus normal morbility. Neuroradiology 1983;25:85-7. [DOI] [PubMed]
- 29.Macpherson P, Teasdale E, Macpherson PY. Radiculographie: Is routine bed rest really necessary? Clin Radiol 1983;34:325-6. [DOI] [PubMed]
- 30.Macpherson P, Teasdale E. Radiculography with non-ionic contrast medium: routine bed rest is unnecessary. Clin Radiol 1984;35:287-8. [DOI] [PubMed]
- 31.Macpherson P, Teasdale E. Routine bed rest is unnecessary after cervical myelography. Neuroradiology 1985;27:214-6. [DOI] [PubMed]
- 32.Congia S, Tronci S, Ledda M. Lumbar puncture headache and posture: electroencephalographic correlations. Boll Lega It Epil 1985;5:237-8.
- 33.Vilming ST, Schrader H, Monstad I. Post-lumbar-puncture headache: the significance of body posture. Cephalalgia 1988;8:75-8. [DOI] [PubMed]
- 34.McAuley L, Pham B, Tugwell P, Moher D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses. Lancet 2000;356:1228-31. [DOI] [PubMed]
- 35.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [DOI] [PubMed]
- 36.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408-12. [DOI] [PubMed]
- 37.Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609-13. [DOI] [PubMed]
- 38.Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet 1999;354:1229-33. [DOI] [PubMed]
- 39.Evans RW, Armon C, Frohman EM, Goodin DS. Assessment: prevention of post-lumbar puncture headaches. Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2000;55:909-14. [DOI] [PubMed]


