ABSTRACT
Kaposi sarcoma (KS) is an angioproliferative neoplasm associated with human herpesvirus-8. Gastrointestinal KS has been well documented in immunosuppressed solid organ transplant patients, with only 26 iatrogenic cases published in patients with inflammatory bowel disease. We report a 24-year-old patient with ulcerative colitis, maintained on cyclosporine for 2 years, who presented with watery, nonbloody diarrhea and weight loss. Colonoscopy revealed human herpesvirus-8-positive hemorrhagic nodules throughout the colon and terminal ileum, with diffuse lymphadenopathy on computed tomography consistent with KS. As gastrointestinal KS may present with symptoms that mimic inflammatory bowel disease, it is critical to maintain suspicion in patients on prolonged immunosuppression to reduce complications.
INTRODUCTION
Kaposi sarcoma (KS) is an angioproliferative neoplasm that may present as 1 of 4 subtypes: classic, endemic, human immunodeficiency virus (HIV)-associated, and iatrogenic.1–6 Human herpesvirus-8 (HHV8) is the causative agent of each of these clinical subtypes, which may present with benign violaceous macules and subcutaneous nodules or involve the lymph nodes and viscera.2,3,5,6 Iatrogenic KS typically presents similarly to classic KS, with mucosal and cutaneous lesions, and has been associated with the use of cyclosporine, azathioprine, infliximab, methotrexate, and corticosteroids.1–5,7 Although iatrogenic KS more often develops in patients undergoing solid organ transplants, there have been rare reports of iatrogenic KS in patients with inflammatory bowel disease (IBD) on immunosuppressants.1–6,8–13 Gastrointestinal involvement is most often asymptomatic, although it may present with abdominal pain, diarrhea, and rectal bleeding, resembling an IBD flare.4,6 Screening endoscopy is not performed in patients without risk factors such as low CD4 <100 cells/μL, men who have intercourse with men, and presence of cutaneous KS lesions.6 The current treatment for KS is doxorubicin, with paclitaxel as a second-line therapy.14 However, to our knowledge, chemotherapeutic agents have only been reported in 1 case of KS in a patient with IBD.15
Since the first case reported in 1966, there have been 26 published cases of iatrogenic KS in patients with IBD —20 with ulcerative colitis (UC) and 6 with Crohn's disease.15,16 These patients were on prolonged immunosuppressants because of severe refractory disease.5,16 We present the 21st case of an HIV-negative patient with UC who was diagnosed with disseminated iatrogenic KS and the second case in a patient with IBD that responded to pegylated liposomal doxorubicin.
CASE REPORT
A 24-year-old HIV-negative man with a history of UC and psoriasis presented with 12 episodes of watery, nonbloody diarrhea per day and a 20-pound weight loss over 1 month. The onset of diarrhea coincided with the start of amoxicillin, which he was taking for a periodontal abscess. The patient reported that his UC had been well-controlled on a stable dose of cyclosporine 125 mg twice daily for 2 years before the time his care was assumed, with eventual plans to switch to a biologic agent. Thus, he attributed the diarrhea and weight loss to antibiotic use. He was initially diagnosed with UC at age 15 and had previously trialed mesalamine and intermittent prednisone without optimal response.
Because of profound diarrhea, he was evaluated in the emergency department, with laboratory results notable for pancytopenia (Hgb 7 g/dL, white blood cell 3,100 cells/μL, and Plt 125,000 cells/μL), severe hypokalemia to 1.8 mmol/L, and CD4 267 cells/μL. Stool analysis was positive for enteropathic Escherichia coli and norovirus which were believed to be the cause of diarrhea. He was admitted to the intensive care unit for potassium repletion and completed a 7-day course of ciprofloxacin. Because of concern for cytomegalovirus infection as an etiology of his diarrhea, he was evaluated with colonoscopy and was found to have multiple hemorrhagic and ulcerated nodules in the terminal ileum and entire colon (Figure 1). Biopsy revealed vasoformative spindle cell lesions compatible with KS that were HHV-8-positive, CD34-positive, and CD31-positive, and cytomegalovirus-negative (Figure 2). In addition, the biopsy showed active enteritis and cryptitis in the small intestine and colon, respectively.
Figure 1.
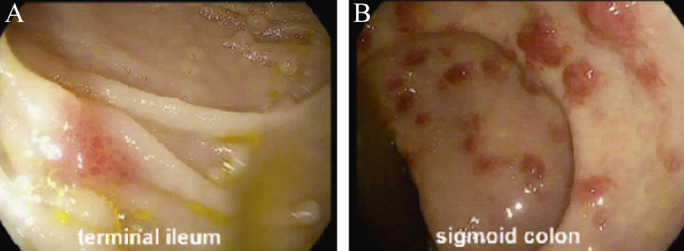
Colonoscopy images displaying hemorrhagic and ulcerated nodules in the (A) terminal ileum and (B) sigmoid colon.
Figure 2.
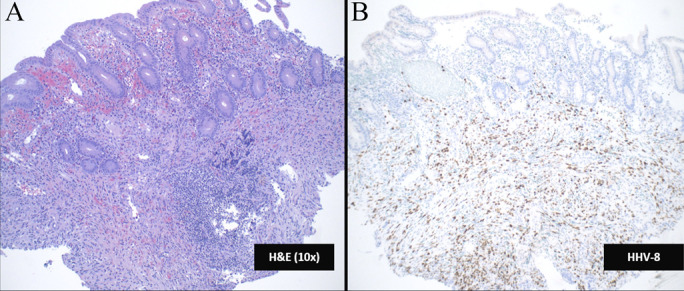
(A and B) Hematoxylin and eosin stain that stained tissue sections of the colon biopsies demonstrates a vasoformative lesion composed of spindle cells with many small, poorly formed, slit-like vascular spaces involving the lamina propria and submucosa. Immunohistochemical stains demonstrate that this lesion is positive for endothelial markers CD31 and CD34 and for human herpesvirus-8.
Thoracic, abdominal, and pelvic computed tomography demonstrated diffuse lymphadenopathy, and peritonsillar and lung masses. An axillary lymph node biopsy was performed, and histologic examination demonstrated replacement of the lymph node by vasoformative spindle cells similar to those seen in the colon biopsy. Residual lymph node follicles and architecture were seen at the periphery of the specimen, confirming that a lymph node was sampled. Immunohistochemical stains (CD34) confirmed the vascular nature of the spindle cells, and an HHV-8 immunostain was positive (Figure 2). The patient was started on rituximab and pegylated liposomal doxorubicin 20 mg/m2. Cyclosporine, emtricitabine, and tenofovir were discontinued, with a plan to evaluate for optimal maintenance therapy after completion of KS treatment. After initiation of these therapies, he reported a reduction in stool frequency to 3 stools per day, and the tonsillar masses regressed.
DISCUSSION
This report discusses a case of iatrogenic KS in a patient with UC maintained on cyclosporine for 2 years. Previous reports of KS in patients with IBD described the characteristic cutaneous lesions after prolonged immunosuppressive therapy.17,18 Intestinal KS is exceedingly rare in HIV-negative individuals, with 5 reported cases of combined cutaneous and gastrointestinal involvement and 18 reported cases with gastrointestinal manifestations alone.15 Several therapies have been implicated in iatrogenic KS; however, few cases reported patients with IBD on long-term cyclosporine as in our patient.1,16 In the absence of skin lesions, KS may be difficult to identify in patients with IBD because its nonspecific symptomatology can be confounded by those of IBD itself.
Based on current literature, there is no association between the development of iatrogenic KS and the duration of IBD activity.4 Gastrointestinal involvement is usually asymptomatic and can occur in the absence of cutaneous lesions as demonstrated in our patient, which may obscure the diagnosis. Because KS most often affects the submucosa, superficial bowel biopsies rarely detect it and require submucosal biopsies with histologic evaluation.3 Previous cases of KS in patients with IBD suggest cessation of the immunosuppressive agent may be sufficient for disease resolution in the absence of systemic HHV-8 infection.5 Given the difficulty with preventing acute IBD flares on discontinuing these agents, patients in several cases needed partial or total colectomy for resolution of symptoms without recurrence.1,2,17,18
Because of evidence of disseminated KS in our patient, rituximab and pegylated liposomal doxorubicin were initiated. Pegylated liposomal doxorubicin has been shown in several studies to be the preferred treatment of HIV-associated KS with gastrointestinal involvement, with similar efficacy in classic KS.6,19,20 However, there are limited cases that report the use of chemotherapeutic agents in patients with iatrogenic KS. We report the first known case of disseminated iatrogenic KS secondary to cyclosporine in a patient with IBD that has responded to treatment with pegylated liposomal doxorubicin with rituximab and did not require surgical intervention.
DISCLOSURES
Author contributions: All authors contributed equally to this article. ML Borum is the article guarantor.
Previous presentation: This case was presented at the Crohn's & Colitis Congress; February 7-9, 2019; Las Vegas, Nevada.
Financial disclosure: None to report.
Informed consent could not be obtained for this case report. All identifying information has been removed.
Contributor Information
Karan Chawla, Email: karan078@email.gwu.edu.
Nadeem Tabbara, Email: tabbara.nadeem@gmail.com.
Daniel Szvarca, Email: danielszvarca@gmail.com.
Anna Stachura, Email: annastachura93@gmail.com.
Brian Theisen, Email: btheisen@mfa.gwu.edu.
Matthew Chandler, Email: mchandler@mfa.gwu.edu.
Marie L. Borum, Email: mborum@mfa.gwu.edu.
REFERENCES
- 1.Girelli CM, Serio G, Rocca E, Rocca F. Refractory ulcerative colitis and iatrogenic colorectal Kaposi's sarcoma. Dig Liver Dis. 2009;41(2):170–4. [DOI] [PubMed] [Google Scholar]
- 2.Hamzaoui L, Kilani H, Bouassida M, et al. Iatrogenic colorectal Kaposi sarcoma complicating a refractory ulcerative colitis in a human immunodeficiency negative-virus patient. Pan Afr Med J. 2013;15(1):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Svrcek M, Tiret E, Bennis M, Guyot P, Fléjou JF. KSHV/HHV8-associated intestinal Kaposi's sarcoma in patient with ulcerative colitis receiving immunosuppressive drugs: Report of a case. Dis Colon Rectum. 2009;52(1):154–8. [DOI] [PubMed] [Google Scholar]
- 4.Duh E, Fine S. Human herpesvirus-8 positive iatrogenic Kaposi's sarcoma in the setting of refractory ulcerative colitis. World J Clin Cases. 2017;5(12):423–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Windon AL, Shroff SG. Iatrogenic Kaposi's sarcoma in an HIV-negative young male with Crohn's disease and IgA nephropathy: A case report and brief review of the literature. Int J Surg Pathol. 2018;26(3):276–82. [DOI] [PubMed] [Google Scholar]
- 6.Lee AJ, Brenner L, Mourad B, Monteiro C, Vega KJ, Munoz JC. Gastrointestinal Kaposi's sarcoma: Case report and review of the literature. World J Gastrointest Pharmacol Ther. 2015;6(3):89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moosa MR. Kaposi's sarcoma in kidney transplant recipients: A 23-year experience. QJM. 2005;98(3):205–14. [DOI] [PubMed] [Google Scholar]
- 8.Kumar V, Soni P, Garg M, et al. Kaposi sarcoma mimicking acute flare of ulcerative colitis. J Investig Med High Impact Case Rep. 2017;5(2):2324709617713510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pédulla F, Sisteron O, Chevallier P, Piche T, Saint-Paul MC, Bruneton JN. Kaposi's sarcoma confined to the colorectum: A case report. Clin Imaging. 2004;28(1):33–5. [DOI] [PubMed] [Google Scholar]
- 10.Kang MJ, Namgung KY, Kim MS, et al. A case of Kaposi's sarcoma associated with ulcerative colitis. Korean J Gastroenterol. 2004;43(5):316–9. [PubMed] [Google Scholar]
- 11.Cohen RL, Tepper RE, Urmacher C, Katz S. Kaposi's sarcoma and cytomegaloviral ileocolitis complicating long-standing Crohn's disease in an HIV-negative patient. Am J Gastroenterol. 2001;96(10):3028–31. [DOI] [PubMed] [Google Scholar]
- 12.Koop HO, Holodniy M, List AF. Fulminant Kaposi's sarcoma complicating long-term corticosteroid therapy. Am J Med. 1987;83(4):787–9. [DOI] [PubMed] [Google Scholar]
- 13.Puy-Montbrun T, Pigot F, Vuong PN, et al. Kaposi's sarcoma of the colon in a young HIV-negative woman with Crohn's disease. Dig Dis Sci. 1991;36(4):528–31. [DOI] [PubMed] [Google Scholar]
- 14.Schneider JW, Dittmer DP. Diagnosis and treatment of Kaposi sarcoma. Am J Clin Dermatol. 2017;18(4):529–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li J, Niu Z, Xue Y, et al. Kaposi sarcoma combined with severe ulcerative colitis: A case report and literature review. Beijing Da Xue Xue Bao Yi Xue Ban. 2020;52(2):373–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pioche M, Boschetti G, Cotte E, et al. Human herpesvirus 8-associated colorectal Kaposi's sarcoma occurring in a drug-induced immunocompromised patient with refractory ulcerative colitis: Report of a new case and review of the literature. Inflamm Bowel Dis. 2013;19(2):E12–5. [DOI] [PubMed] [Google Scholar]
- 17.Bursics A, Morvay K, Abrahám K, et al. HHV-8 positive, HIV negative disseminated Kaposi's sarcoma complicating steroid dependent ulcerative colitis: A successfully treated case. Gut. 2005;54(7):1049–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rodriguez-Pelaez M, Fernandez-Garcia MS, Gutierrez-Corral N, et al. Kaposi's sarcoma: An opportunistic infection by human herpesvirus-8 in ulcerative colitis. J Crohns Colitis. 2010;4(5):586–90. [DOI] [PubMed] [Google Scholar]
- 19.Cooley T, Henry D, Tonda M, Sun S, O'Connell M, Rackoff W. A randomized, double-blind study of pegylated liposomal doxorubicin for the treatment of AIDS-related Kaposi's sarcoma. Oncologist. 2007;12(1):114–23. [DOI] [PubMed] [Google Scholar]
- 20.Di Lorenzo G, Kreuter A, Di Trolio R, et al. Activity and safety of pegylated liposomal doxorubicin as first-line therapy in the treatment of non-visceral classic Kaposi's sarcoma: A multicenter study. J Invest Dermatol. 2008;128(6):1578. [DOI] [PubMed] [Google Scholar]


