Abstract
Background
COVID-19 has placed unprecedented demands on infection control professionals (ICPs) and infectious disease (ID) physicians. This study examined their knowledge, preparedness, and experiences managing COVID-19 in the Australian healthcare settings.
Methods
A cross-sectional study of ICPs and ID physician members of the Australasian College for Infection Prevention and Control (ACIPC) and the Australasian Society for Infectious Diseases (ASID) was conducted using an online survey. Descriptive statistics were used to summarise and report data.
Results
A total of 103 survey responses were included in the analysis for ICPs and 45 for ID physicians. A majority of ICPs (78.7%) and ID physicians (77.8%) indicated having ‘very good’ or ‘good’ level of knowledge of COVID-19. Almost all ICPs (94.2%) relied on state or territory's department of health websites to source up-to-date information While most ID physicians (84.4%) used scientific literature and journals. A majority of ICPs (96%) and ID physicians (73.3%) reported feeling ‘moderately prepared’ or ‘extremely prepared’ for managing COVID-19. Most respondents had received specific training about COVID-19 within their workplace (ICPs: 75%; ID physicians: 66.7%), particularly training/certification in PPE use, which made them feel ‘mostly or entirely confident’ in using it. Most ICPs (84.5%) and ID physicians (76.2%) reported having ‘considerably’ or ‘moderately more’ work added to their daily duties. Their biggest concerns included the uncertainties under a rapidly changing landscape, PPE availability, and the community's compliance.
Conclusion
Harmonised information, specific COVID-19 training and education, and adequate support for front-line workers are key to successfully managing COVID-19 and other future outbreaks.
Keywords: COVID-19, Health knowledge, Attitudes, Practice, Infection control, Outbreaks
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic [1] caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is a global health emergency bringing significant and unprecedented challenges to health systems. Governments worldwide have had to implement multimodal containment and mitigation strategies to protect and preserve the community's health and wellbeing and enable health systems to cope with demands for service [[2], [3], [4]]. Australia rapidly developed and implemented the Australian Health Sector Emergency Response Plan for Novel Coronavirus [5] which incorporates four main objectives to contain and prevent the spread of COVID-19 into the community. Objective 3 of the plan focuses on minimising the burden and supporting the Australian healthcare system needs, including key measures to protect healthcare workers (HCWs).
Infection control professionals (ICPs) and infectious diseases (ID) physicians are pivotal in the response to COVID-19 and have been at the frontline of the global response against the pandemic. ICPs manage the implementation and evaluation of infection control programs to prevent and control the spread of healthcare-associated infections and infectious diseases outbreaks [6,7], and ID physicians manage and direct patient care and undertake other public health and antimicrobial stewardship related duties [8,9]. Together, they play a vital role in infection prevention and disease control.
COVID-19 has placed unprecedented professional and personal demands on ICPs and ID physicians to implement effective infection prevention and disease control measures for managing this novel pathogen, including staff education, reinforcement of IPC protocols and adequate use of personal protective equipment (PPE) [[10], [11], [12]]. Previous studies reporting the experiences, knowledge and perception of HCWs dealing with SARS-CoV-1 [13], Ebola [14] and MERS-CoV [15] highlight the impact that outbreaks have had on their daily workload, the relevance of timely and accurate information, and the influence of HCWs attitudes and perception of risk in work-related transmission. While the lessons learned from these previous outbreaks provide valuable insight on how to handle large-scale infectious diseases outbreaks, there is a scarcity of literature focusing on ICPs and ID physicians dealing with these events.
To the best of our knowledge, no research has been conducted on ICPs and ID physicians during COVID-19 in Australia. This study examined ICPs and ID physicians’ knowledge, preparedness, and experiences managing COVID-19 in Australian healthcare settings.
Methods
Study design
A cross-sectional study was conducted in collaboration with the Australasian College for Infection Prevention and Control (ACIPC) and the Australasian Society for Infectious Diseases (ASID).
Setting and population
ICPs and ID physicians with current membership to ACIPC and ASID were invited to participate in this voluntary study. No other inclusion or exclusion criteria were applied. Consent to participate was based on survey submission. Human research ethics approval was sought and granted for this study (University of Sydney HREC 2020/200).
Instrument development
Voluntary and anonymous online surveys were developed using Research Electronic Data Capture (REDcap™) [16] software by a panel of experts in infection prevention and control and infectious diseases. Survey questions were adapted from questionnaires used to study previous outbreaks [13,14,[17], [18], [19], [20]]. The ICP survey comprised of 48 questions and the ID physician survey 55 questions, with 43 common questions between surveys. The survey ‘comprised of’ questions relating to: i) respondents' demographics; ii) respondents' knowledge about SARS-CoV-2 and COVID-19; iii) respondents' preparedness for SARS-CoV-2 and COVID-19; and iv) respondents’ experiences of working in an ongoing outbreak environment. The survey was pilot tested, with modifications to wording and format to improve clarity and readability before distribution.
Data collection and analysis
The surveys were distributed to all college members by their respective secretariats via e-newsletters and emails. At that time, the membership was approximately 1500 for ACIPC and 1000 for ASID. The surveys were active between June and September 2020. Once closed, raw data were downloaded from REDcap™, cleaned in Microsoft Excel, and analysed in IBM SPSS 26®. Individual questions with no response were treated as missing values and excluded from data analysis, with the denominator for those questions adjusted accordingly. Descriptive statistics were used to analyse the data. Open-ended questions were managed in Microsoft Excel, and analysed using conventional content analysis technique [21].
Results
Demographics
There were 115 and 54 survey responses respectively for ICPs and ID physicians. Of these, 12 and nine were respectively excluded due to incompletion beyond the first five demographic questions. Consequently, 103 survey responses were included in the analysis for ICPs (6.9% response rate) and 45 for ID physicians (4.5% response rate).
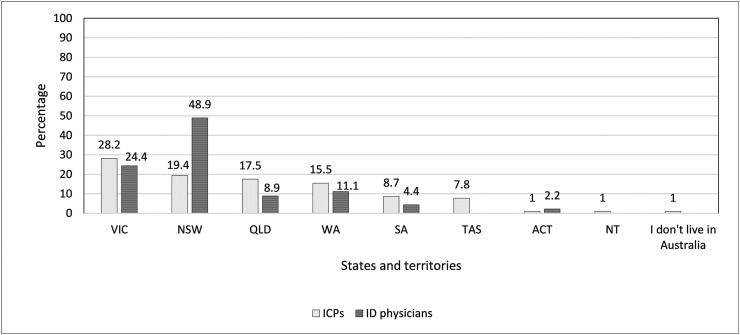
Almost all ICPs (99%, n = 102/103) and all ID physicians reported residing in Australia, with the majority working in New South Wales and Victoria as per Fig. 1 .
Figure 1.
Australian states or territories where respondents currently work.
Of the 45 ID physicians, 42 practiced adult medicine, including 10 dual trained in microbiology and 8 in another medical subspecialty. A further 3 were paediatric ID physicians. Respondents were from departments with an average of seven ID physicians (SD 5.06).
As of 1 January 2020, the average number of years that the respondents had worked in their respective professional field was 17 years for the ICPs (SD 11; minimum <1, maximum 51 years) and 11 years for the ID physicians (SD 10; minimum <1, maximum 46 years).
The majority of ICPs (66%, n = 68) had completed an IPC qualification. Some (19.4%, n = 20) indicated being currently credentialed with ACIPC. Of these, 45% (n = 9) reported holding expert, 15% (n = 3) advanced, and 40% (n = 8) primary infection control credentials.
Knowledge
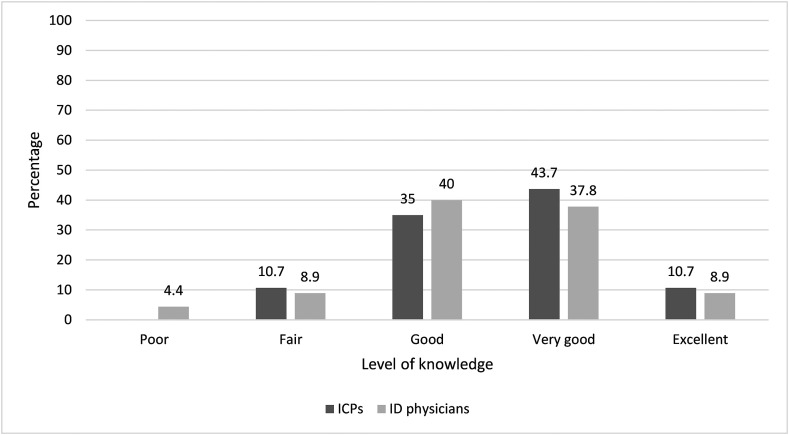
When asked to rate their current knowledge of COVID-19, a majority of ICPs (78.7%, n = 81) selected ‘very good’ or ‘good’. No ICP rated their knowledge as poor. Similarly, a majority of ID physicians (77.8%, n = 35) rated their current COVID-19 knowledge as ‘good’ or ‘very good’, with few (4.4%, n = 2) rating it as poor (Fig. 2 ).
Figure 2.
Respondents' current level of knowledge about COVID-19.
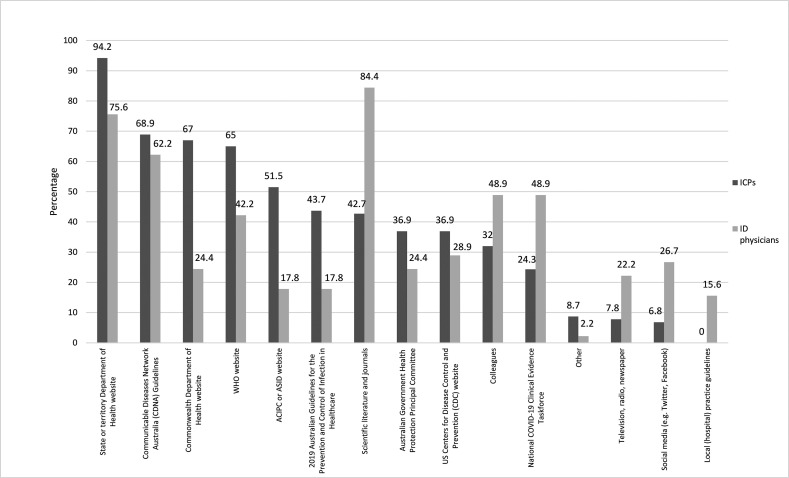
Respondents were provided with a list of 15 sources of COVID-19 information to choose from and asked where they went for up-to-date information (Fig. 3 ). Almost all ICPs (94.2%, n = 97) visited their state or territory department of health websites followed by information provided by the Communicable Diseases Network Australia (CDNA) (68.9%, n = 71). In contrast, most ID physicians (84.4%, n = 38) used scientific literature and journals routinely, followed by information provided by state or territory department of health websites (75.6%, n = 34).
Figure 3.
Sources of up-to-date COVID-19 information used by respondents.
Since the beginning of the pandemic, ACIPC and ASID have provided various links to COVID-19 resources in their respective websites (Table S1). The top three ACIPC resources used by ICPs were the Australian Government Department of Health COVID-19 website link (62.1%, n = 64); Australian states and territories websites links (56.3%, n = 58), and the CDNA National Guidelines for Public Health Units website link (47.6%, n = 49). ID physicians mostly used ASID's Ozbug email discussion forum (84.4%, n = 38); the National COVID-19 Clinical Evidence Taskforce and other evidence-based clinical guidelines (60%, n = 27); and the ASID Interim Guidelines for the Clinical Management of COVID-19 in Adults (40%, n = 18).
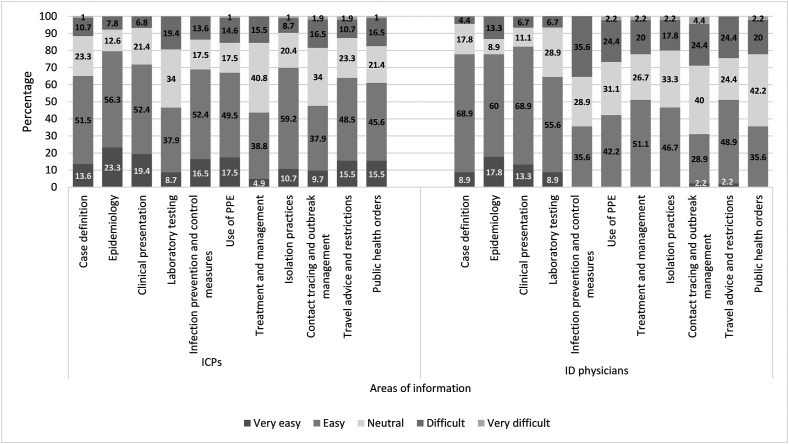
We asked respondents how easy it was to keep up-to-date with 11 areas of COVID-19 information (Fig. 4 ). For ICPs, the top three categories reported as ‘easy’ and ‘very easy’ to follow were: a) epidemiology (79.6%, n = 82); b) clinical presentation (71.8%, n = 70); and c) isolation practices (69.9%, n = 72). For ID physicians, the top three ‘easy’ and ‘very easy’ categories to keep up-to-date with were: a) clinical presentation (82.2%, n = 37); b) case definition and epidemiology (77.8%, n = 35 respectively); and c) laboratory testing (64.5%, n = 29). ‘Contact tracing and outbreak management’; ‘isolation practices’; ‘use of PPE’ and ‘public health orders’ were identified as ‘very difficult’ to keep up-to-date with.
Figure 4.
Keeping up-to-date with COVID-19 information and guidelines across 11 different categories.
Preparedness
On an individual level, a third of ICPs (32/100) and almost half of ID physicians (48.9%, n = 22/45) reported they were ‘not at all prepared’ for COVID-19 on 31 December 2019. However, at the time of survey completion, almost all ICPs (96/100) and the majority of ID physicians (73.3%, n = 33/45) reported feeling ‘moderately prepared’ or ‘extremely prepared’ for managing COVID-19. At a workplace level, most ICPs (80/100) and ID physicians (60%, n = 27/45) reported their workplace was ‘moderately prepared’ or ‘extremely prepared’ to manage COVID-19 into the future. In contrast, a third of ICPs (33/100) and almost half ID physicians (48.9%, n = 22/45) reported that Australia was ‘slightly’ to ‘not at all prepared’ for COVID-19 (Table S2).
In regards to the provision of clear, timely and authoritative information about COVID-19, most respondents (ICPs: 75/100; ID physicians: 68.8%, n = 31/45) agreed information had been accurately provided by their workplace. Likewise, the majority (ICPs: 80/100; ID physicians: 68.9%, n = 31/45) agreed their respective state or territory government health departments had provided clear, timely and authoritative information about COVID-19, as well as the Australian Government Department of Health (ICPs: 86/100; ID physicians: 60%, n = 31/45) (Table S3).
Almost all ICPs (94/100) and most ID physicians (86.7%, n = 39/45) confirmed their workplace had COVID-19 guidelines and an outbreak response plan. Of these, the majority stated they were ‘moderately’ or ‘entirely familiar’ with it (ICPs: 89.4%, n = 84/94; ID physicians 69.2%, n = 27/39), with most ICPs (74.5%, n = 70/94) and ID physicians (66.5%, n = 22/39) feeling it was ‘easy’ or ‘very easy’ to adhere to their workplace guidelines and response plans. Few respondents (ICPs: 4/100; ID physicians: 8.9%, n = 4/45) did not know if their workplace had any.
Most ICPs (75/100) and ID physicians (66.7%, n = 30/45) reported they had received some form of specific education, training, or instruction about COVID-19 within their workplace. As summarised in Table S4, over half of ICPs (59.2%, n = 61/103) identified the instruction received as practical PPE instruction. In contrast, over half of ID physicians (57.8%, n = 26/45) classified the education received as lectures and grand rounds. The majority of ICPs (75.4%, n = 46/61) and ID physicians (76.7%, n = 23/30) rated the provided education, training, or instruction as ‘mostly or entirely adequate’.
A majority of ICPs (72/100) and ID physicians (64.4%, n = 29/45) reported having received specific training or certification in the use of PPE for managing COVID-19, with most respondents rating it to be ‘mostly’ or ‘entirely adequate’ (ICPs: 80.6%, n = 58/72; ID physicians 75.9%, n = 22/29). The vast majority of ICPs (88/100) and ID physicians (75.5%, n = 34/45) reported they were ‘mostly’ or ‘entirely confident’ in using PPE for managing COVID-19 (Table 1 ).
Table 1.
Adequacy of PPE training and respondents’ level of confidence in using PPE for managing COVID-19.
| ICPs |
ID physicians |
|||
|---|---|---|---|---|
| n |
% |
n |
% |
|
| Adequacy of PPE training | ||||
| Not at all adequate | – | – | – | – |
| Slightly adequate | 3 | 4.2 | 1 | 3.4 |
| Somewhat adequate | 11 | 10.3 | 6 | 20.7 |
| Mostly adequate | 29 | 27.1 | 14 | 48.3 |
| Entirely adequate |
29 |
27.1 |
8 |
27.6 |
|
Confidence in using PPE |
||||
| Not at all confident | 1 | 1 | 1 | 2.2 |
| Slightly confident | 2 | 2 | 2 | 4.4 |
| Somewhat confident | 9 | 9 | 8 | 17.8 |
| Mostly confident | 28 | 28 | 19 | 42.2 |
| Entirely confident | 60 | 60 | 15 | 33.3 |
We asked ID physicians if they had been involved in providing/producing information or training for managing COVID-19, with 80% (n = 36/45) confirming participation. Yet, over half of them (57.8%, n = 26/45) did not provide/produce information regarding using PPE for managing COVID-19. Some (37.8%, n = 17/45) reported that their facility had purchased powered air purifying respirators (PAPR) amid COVID-19 but the vast majority (82.4%, n = 14/17) were not involved in their implementation.
Experiences
Most respondents indicated their workplace was involved in assessing and treating suspected and confirmed cases of COVID-19 Whilst few had referred suspected/confirmed COVID-19 cases (Table S5). A majority of ICPs had not cared for confirmed or suspected cases of COVID-19 (79.4%, n = 77/97), while most ID physicians (85.7%, n = 36) had.
The majority of respondents expressed they were ‘slightly’ to ‘somewhat concerned’ about contracting the virus (ICPs: 62.9%, n = 61/97; ID physicians: 66.7%, n = 28/42). While almost a third of ICPs (27.8%, n = 27/97) and few ID physicians (14.3%, n = 6/42) indicated they were ‘not at all concerned’ (Fig. S1). Almost no ID physician had requested to be deployed from their usual work to an area less likely to have direct contact with COVID-19 patients (95.2%, n = 40/42).
Almost no respondent took annual leave (ICPs: 99%, n = 96/97; ID physicians: 97.6%, n = 41/42) or sick leave (ICPs: 97.9%, n = 95/97; ID physicians: 95.2%, n = 40/42). Yet 20% of ID physicians (n = 8/42) had made changes to their living arrangements (e.g., moving out of a shared bedroom). Few ICPs and ID physicians (6.2%, n = 6/97; 21.4%, n = 9/42, respectively) had avoided sharing information about their duties caring for COVID-19 patients at some point, out of fear of a negative reaction. Some reported they had been avoided by their closest circle (12.4%, n = 12/97; 16.7%, n = 7/42, respectively), and had experienced or witnessed some level of discrimination at work (ICPs: 15.5%, n = 15/97; ID physicians: 9.5%, n = 4/42).
The overwhelming majority of ICPs (91.8%, n = 89/97) and ID physicians (95.2%, n = 40/42) reported feeling more stressed at work than usual to some extent due to COVID-19 (Fig. S2). These results were echoed by the majority of ICPs (84.5%, n = 82/97) and ID physicians (76.2%, n = 32/42), who reported their work had ‘considerably’ or ‘moderately’ increased due to the outbreak (Fig. S3).
When asked if their workplace provided staff debriefings and psychological support services, over half of ICPs (54.6%, n = 53/97) and few ID physicians (23.8%, n = 10/42) reported their workplace provided both. The majority of respondents had not used any of these services ICPs: (66%, n = 64/97; ID physicians 83.3%, n = 35/42). Among those ICPs and ID physicians who had attended debriefings, 32% (n = 31/97) and 14.3% (n = 6/42) rated them useful to some extent, respectively. No doctor and almost no ICP used their facility's psychological support services (ICPs: 94.8%, n = 92/97). Those who did rated them ‘useful’ to some extent.
Respondents listed their single biggest issue about COVID-19; these were grouped in themes (Table S6). Among the 67 comments provided by ICPs, the three most common themes were: i) keeping up-to-date with the information (26.9%, n = 18); ii) adequate PPE stock and training availability (22.4%, n = 15); and iii) communication difficulties between executive management and staff (19.4%, n = 13).
ID physicians provided 42 comments, from which the three most common themes were: i) uncertainties surrounding an ongoing pandemic (19%, n = 8); ii) fear and stress management among colleagues and staff due to increased workload, particularly in relation to COVID-19 Victorian second wave (14.3%, n = 6); and iii) keeping track of rapidly changing evidence and information provided by governmental and/or scientific sources (9.5%, n = 4).
Discussion
This study examined ICPs and ID physicians’ knowledge, preparedness, and experiences managing SARS-CoV-2 and COVID-19 in the Australian healthcare settings. The emergence of COVID-19, among various others large-scale outbreaks seen in recent years [19,22,23], is a stark reminder of the threat these outbreaks present to health systems and their performance [24]. As large second and third waves of COVID-19 occur globally, the readiness of HCWs is crucial to an effective response, with ICPs and ID physicians at the forefront of managing suspected or confirmed cases of COVID-19.
Previous experiences with outbreak response has shown that frontline HCWs often face various challenges including, but not limited to, working under an emerging threat environment [15], keeping-up-to-date with growing information [13,20], the availability of training and education [14,17], and the changes in their daily work responsibilities [19]. Our study showed that ICPs and ID physicians working under COVID-19 experienced similar challenges. In terms of knowledge, and as expected, during the pandemic's early stages respondents presented low levels of specific knowledge. Furthermore, they were required to attend to rapidly changing information and take immediate action to minimise the risk of infection and its spread [25]. As the pandemic unfolded and sources of information increased, so did their level of specific knowledge.
Accessing the various official sources of local, national, and international information about COVID-19 facilitated and supported respondents feeling well prepared to manage key areas relating to the pandemic, as it has also been shown in other countries [26,27]. Interestingly, both groups reported different sources for up-to-date information. While most ICPs relied almost exclusively on official state or territory department of health websites, ID physicians used scientific literature and journals. This could be explained by the general nature of their duties, where ICPs predominantly focus on policy development, surveillance coordination, outbreak management and education/training [7], while ID physicians are mostly involved in managing cases and coordinating local responses [28]. Although the vast majority of respondents believed they were provided with clear, timely and authoritative information about COVID-19 by their respective workplace, state or territory health departments, and the federal Department of Health, comments in regards to the overwhelming amounts of information, the challenges to keep-up-to-date with it, and most importantly the presence of discrepancies in the message delivered were echoed across both professional groups. It is crucial to reassure HCWs on where to access official information as well as the provision of non-ambiguous messages to follow, which will ultimately guide and optimise work performance and reduce associated difficulties [29].
Our study also showed that specific education and training programs concerning COVID-19 supported the respondents' general sense of preparedness, with varied types of instruction being reported and highly rated. This is proof of the multimodal strategies implemented in Australia to protect HCWs and to enable the system to cope with the rising demands more broadly. Yet, the fact that a third of ICPs and almost half of ID physicians did not feel prepared for COVID-19 in December 2019 highlights the need for such strategies to be ongoing, as part of HCWs education and training. Due to the pandemic's mode of transmission, it is not surprising that an important proportion of training was focused on the use of PPE, providing attendants with high levels of confidence to perform their daily work in a safe way. Previous studies have reported that with proper use of PPE and good adherence to IPC measures, the risk of SARS-CoV-2 infection for HCWs caring for patients with COVID-19 is considered to be very low [30]. The literature has recognised the lack of awareness and training, as well as the shortage of PPE, as some of the most relevant sources of COVID-19 spread in health settings [31]. Additionally, the majority of respondents were familiar with, and had easily adhered to their workplace COVID-19 guidelines and outbreak response plans, which suggests that the effective level of preparedness displayed by the Australian healthcare system facing the pandemic was strengthened by the early development of such official guidelines [5,32,33]. This was most likely enhanced by the general engagement displayed by these and other HCWs, which is indispensable for combating COVID-19 and other similar potential outbreaks [34].
Despite their direct involvement with COVID-19 related tasks, few respondents expressed moderate or severe levels of concern. As previously discussed, such positive attitude and behaviour is directly related to an adequate level of knowledge. The greater the knowledge, the more confidence and secure HCWs will feel and behave [35]. Since most leave was cancelled for these professionals, no ICP or ID physician reported taking any or having requested to be deployed from their usual work area due to concerns about contracting SARS-CoV-2. Likewise, very few of them requested psychological support. They did however confirm a considerable increase in their workload, which in some instances translated into teams’ exhaustion and anxiety. As reported in previous studies, managing an emerging outbreak represents a great health challenge for HCWs worldwide, with evident changes in their workload, jobs and general life [17,19,36].
This study has some limitations. Due to the voluntary nature of the survey, the groups' workload, and survey-fatigue the study population numbers are low when compared to ACIPC and ASID's respective membership. It is also possible that the respondents had higher than levels of interest and involvement in COVID-19 preparedness and response, hence greater motivation to participate in the study, which may have skewed the final results. Australia has had low levels of infection and deaths associated with COVID-19 compared to other developed countries. This may limit the generalisability of our findings. Furthermore, and as any cross-sectional study, our results have not captured the full experiences of these health professionals across different phases of the pandemic. Nevertheless, our findings provide a broad insight into Australian ICPs and ID physicians' involvement managing COVID-19 which could be useful for future COVID-19 outbreak management needs and other emerging outbreaks.
Although most jurisdictions have not reported circulating virus, elimination of community transmission has not yet been achieved. Healthcare systems must continue with their commitment to staying alert and acting preventively, maintaining a combination of high-quality health care as well as rapid tracing of suspected or confirmed cases. Harmonised information and adequate education and training to these and other front-line HCWs are key to successfully managing COVID-19 and future outbreaks.
Ethics
Human research ethics approval for this study was granted by The University of Sydney Human Research Ethics Committee (Approval 2020/200).
Authorship statement
RZS conceived and designed the study. CS, CL, SN and RZS drafted the study protocol. All authors designed and tested the survey instruments. CS, CL, SN and RZS supervised data collection and curation. All authors analysed and interpreted the data. CS and RZS wrote the first draft of the manuscript, and all authors reviewed and approved the manuscript for submission.
Conflicts of interest
[RZS - Anonymised] [BM – Anonymised] is an [Anonymised] of [Anonymised] but was blinded to this submission in the journal's editorial management system and had no role in the peer review or editorial decision-making whatsoever. There are no other conflicts of interest to declare.
Funding
This study was an investigator-initiated research and did not receive financial support from funding agencies in the public, commercial or not-for-profit sectors.
Provenance and peer review
Not commissioned; externally peer reviewed.
E-mail addresses of the authors
cristina.sotomayor@sydney.edu.au (Cristina Sotomayor-Castillo), shizar.nahidi@sydney.edu.au (Shizar Nahidi), cecilia.z.li@sydney.edu.au (Cecilia Li), debourough.macbeth@health.qld.gov.au (Deborough Macbeth), philip.russo@monash.edu (Philip L Russo), brett.mitchell@newcastle.edu.au (Brett G Mitchell), marilyn.cruickshank@health.nsw.gov.au (Marilyn Cruickshank), tania.sorrell@sydney.edu.au (Tania Sorrell), nicky.gilroy@health.nsw.gov.au (Nicole Gilroy), patricia.ferguson@health.nsw.gov.au (Patricia Ferguson), matthew.watts@health.nsw.gov.au (Matthew Watts), ramon.shaban@sydney.edu.au (Ramon Shaban).
Acknowledgements
The authors would like to thank the Australasian College for Infection Prevention and Control, and the Australasian Society for Infectious Diseases for their support and assistance in distributing the survey to their members.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.idh.2021.05.002.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization Timeline of WHO's response to COVID-19. 2020. https://www.who.int/news-room/detail/29-06-2020-covidtimeline Available from:
- 2.European Centre for Disease Prevention and Control . 2020. Infection prevention and control and preparedness for COVID-19 in healthcare settings. [Google Scholar]
- 3.Communicable Diseases Network Australia . CDNA National Guidelines for Public Health Units; 2020. Coronavirus disease 2019 (COVID-19) [Google Scholar]
- 4.Centers for Disease Control and Prevention . 2020. COVID-19 overview and infection prevention and control priorities in non-US Healthcare settings. [Google Scholar]
- 5.Australian Government Department of Health . 2020. Australian health sector emergency response plan for novel Coronavirus (COVID-19) [Google Scholar]
- 6.Mitchell B., Macbeth D., Halton K., Gardner A., Hall L. Resourcing hospital infection prevention and control units in Australia: a discussion paper. Infect Dis Health. 2017;22:83–88. [Google Scholar]
- 7.Hall L., Halton K., Macbeth D., Gardner A., Mitchell B. Roles, responsibilities and scope of practice: describing the 'state of play' for infection control professionals in Australia and New Zealand. Healthc Infect. 2015;20(1):29–35. [Google Scholar]
- 8.Ostrowsky B., Banerjee R., Bonomo R.A., Cosgrove S.E., Davidson L., Doron S. Infectious diseases physicians: leading the way in antimicrobial stewardship. Clin Infect Dis. 2018;66(7):995–1003. doi: 10.1093/cid/cix1093. [DOI] [PubMed] [Google Scholar]
- 9.Fätkenheuer G., Kern W.V., Salzberger B. An urgent call for infectious diseases specialists. Infection. 2016;44(2):269–270. doi: 10.1007/s15010-016-0886-y. [DOI] [PubMed] [Google Scholar]
- 10.Dancer S.J. Covid-19 exposes the gaps in infection prevention and control. Infect Dis Health. 2020;25(4):223–226. doi: 10.1016/j.idh.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang J., Liu F., Zhou M., Lee Y.F. Will the status of infection prevention and control (IPC) professionals be improved in the context of COVID-19? Am J Infect Contr. 2020;48(6):729–730. doi: 10.1016/j.ajic.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Popescu S. Roadblocks to infection prevention efforts in healthcare SARS-CoV-2/COVID-19 response. Disaster Med Public Health Prep. 2020:1–7. doi: 10.1017/dmp.2020.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deng J.F., Olowokure B., Kaydos-Daniels S.C., Chang H.J., Barwick R.S., Lee M.L. Severe acute respiratory syndrome (SARS): knowledge, attitudes, practices and sources of information among physicians answering a SARS fever hotline service. Publ Health. 2006;120(1):15–19. doi: 10.1016/j.puhe.2005.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piţigoi D., Săndulescu O., Ionescu T., Niţescu B., Niţescu M., Streinu-Cercel A. Assessment of knowledge, attitudes and perceptions regarding Ebola disease in healthcare workers from a tertiary care hospital in Romania. Publ Health. 2018;164:7–15. doi: 10.1016/j.puhe.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan M.U., Shah S., Ahmad A., Fatokun O. Knowledge and attitude of healthcare workers about Middle East Respiratory Syndrome in multispecialty hospitals of Qassim, Saudi Arabia. BMC Publ Health. 2014;14:1281. doi: 10.1186/1471-2458-14-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lam S.K.K., Kwong E.W.Y., Hung M.S.Y., Pang S.M.C., Chiang V.C.L. Nurses' preparedness for infectious disease outbreaks: a literature review and narrative synthesis of qualitative evidence. J Clin Nurs. 2018;27(7–8):e1244–e1255. doi: 10.1111/jocn.14210. [DOI] [PubMed] [Google Scholar]
- 18.Kelly B., Squiers L., Bann C., Stine A., Hansen H., Lynch M. Perceptions and plans for prevention of Ebola: results from a national survey. BMC Publ Health. 2015;15:1136. doi: 10.1186/s12889-015-2441-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alsahafi A.J., Cheng A.C. Knowledge, attitudes and behaviours of healthcare workers in the Kingdom of Saudi Arabia to MERS coronavirus and other emerging infectious diseases. Int J Environ Res Publ Health. 2016;13(12) doi: 10.3390/ijerph13121214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abbag H.F., El-Mekki A.A., Al Bshabshe A.A.A., Mahfouz A.A., Al-Dosry A.A., Mirdad R.T. Knowledge and attitude towards the Middle East respiratory syndrome coronavirus among healthcare personnel in the southern region of Saudi Arabia. J Infect Publ Health. 2018;11(5):720–722. doi: 10.1016/j.jiph.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 22.Ji D., Ji Y.J., Duan X.Z., Li W.G., Sun Z.Q., Song X.A. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014-2015 Ebola outbreak in Sierra Leone: a cross-sectional study. Oncotarget. 2017;8(8):12784–12791. doi: 10.18632/oncotarget.14498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xie M., Chen Q. Insight into 2019 novel coronavirus - an updated interim review and lessons from SARS-CoV and MERS-CoV. Int J Infect Dis. 2020;94:119–124. doi: 10.1016/j.ijid.2020.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morens D.M., Fauci A.S. Emerging pandemic diseases: how we got to COVID-19. Cell. 2020;182(5):1077–1092. doi: 10.1016/j.cell.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolf M.S., Serper M., Opsasnick L., O'Conor R.M., Curtis L., Benavente J.Y. Awareness, attitudes, and actions related to COVID-19 among adults with chronic conditions at the onset of the U.S. Outbreak: a cross-sectional survey. Ann Intern Med. 2020;173(2):100–109. doi: 10.7326/M20-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saqlain M., Munir M.M., Rehman S.U., Gulzar A., Naz S., Ahmed Z. Knowledge, attitude, practice and perceived barriers among healthcare workers regarding COVID-19: a cross-sectional survey from Pakistan. J Hosp Infect. 2020;105(3):419–423. doi: 10.1016/j.jhin.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Foley D.A., Chew R., Raby E., Tong S.Y.C., Davis J.S. COVID-19 in the pre-pandemic period: a survey of the time commitment and perceptions of infectious diseases physicians in Australia and New Zealand. Intern Med J. 2020;50(8):924–930. doi: 10.1111/imj.14941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Foley D.A., Tippett E. COVID-19 response: the perspectives of infectious diseases physicians and clinical microbiologists. Med J Aust. 2020;213(9):431-e1. doi: 10.5694/mja2.50810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prescott K., Baxter E., Lynch C., Jassal S., Bashir A., Gray J. COVID-19: how prepared are front-line healthcare workers in England? J Hosp Infect. 2020;105(2):142–145. doi: 10.1016/j.jhin.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bielicki J.A., Duval X., Gobat N., Goossens H., Koopmans M., Tacconelli E. Monitoring approaches for health-care workers during the COVID-19 pandemic. Lancet Infect Dis. 2020;20(10):e261–e267. doi: 10.1016/S1473-3099(20)30458-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chirico F., Nucera G., Magnavita N. COVID-19: protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. 2020;41(9):1117. doi: 10.1017/ice.2020.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Australian Commission on Safety and Quality in Health Care . 2020. COVID-19 infection prevention and control risk management - guidance. [Google Scholar]
- 33.Australian Government Department of Health . 2020. Coronavirus (COVID-19) guidelines for infection prevention and control in residential care facilities. [Google Scholar]
- 34.Momtazmanesh S., Ochs H.D., Uddin L.Q., Perc M., Routes J.M., Vieira D.N. All together to fight COVID-19. Am J Trop Med Hyg. 2020;102(6):1181–1183. doi: 10.4269/ajtmh.20-0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang M., Zhou M., Tang F., Wang Y., Nie H., Zhang L. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J Hosp Infect. 2020;105(2):183–187. doi: 10.1016/j.jhin.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cotrin P., Moura W., Gambardela-Tkacz C.M., Pelloso F.C., Santos L.D., Carvalho M.D.B. Healthcare workers in Brazil during the COVID-19 pandemic: a cross-sectional online survey. Inquiry. 2020;57 doi: 10.1177/0046958020963711. 46958020963711. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.