Abstract
Reproductive coercion (RC) describes a range of behaviors that restrict reproductive autonomy including pregnancy coercion, birth control sabotage, and controlling the outcome of a pregnancy. RC is associated with pregnancies that are mistimed and unwanted (i.e. unintended). Past research demonstrates that Latina women have higher risk for RC and for unintended pregnancy. This cross-sectional descriptive study with Latina women (n=482) examined prevalence and risk factors for RC, evaluated the association of RC and unintended pregnancy among women with a past-year pregnancy, and explored use of safety and harm reduction strategies. A tablet survey was administered to women attending a community health center, between the ages of 15 and 45, who self-identified as Latina and who had a dating or sexual partner in the past year. Approximately 1 in 6 (16.8%) experienced past-year RC and risk factors included younger age (AOR 0.95, 95% CI 0.91–1.00, p=0.038) and concurrent intimate partner violence (IPV; AOR 4.47, 95% CI 2.06–9.70, p<0.001). IPV questions were specific to the partner involved with RC behaviors. For the 185 participants who reported a past-year pregnancy, RC was associated with lower pregnancy planning scores (β −0.27, 95% CI −0.41 −0.13, p<0.001). The combination of experiencing RC and IPV appeared particularly potent in lowering pregnancy planning scores (β −0.15, 95% CI −0.29 – 0.00, p=0.052). Approximately 10.6% of participants engaged in harm reduction strategies, most commonly ending an unhealthy or abusive relationship (6.1%) and using less detectable methods of contraception so that partners would not find out (3.4%). The study articulates the risk of RC and its intersection with IPV and unintended pregnancy for Latina women. Providers working with racially and ethnically marginalized women have an important role in promoting safety and harm reduction strategies that include offering less detectable methods of contraception and support in leaving unhealthy and abusive relationships.
Keywords: Coercion, Marginalized Populations, Hispanic Americans, Intimate Partner Violence, Unplanned Pregnancy, Quantitative Research, Reproductive Health, Health Inequities
Introduction
Reproductive coercion (RC) describes a range of behaviors that restrict reproductive autonomy including coercion to get pregnant, sabotaging contraception, and controlling the outcome of a pregnancy. It is a critical area of research in women’s health because of its association with intimate partner violence (IPV; Clark et al., 2014) and with health outcomes such as unintended pregnancy (Decker et al., 2017; Holliday et al., 2017; McCauley et al., 2017; E. Miller et al., 2014; Paterno et al., 2018). IPV and unintended pregnancy have associated negative health outcomes (Campbell, 2002; Campbell et al., 2018; Hall et al., 2017; Kost & Lindberg, 2015; Massetti et al., 2018) and unintended pregnancy is an area of health inequities for marginalized populations such as Latina and African American women (Finer & Zolna, 2011; Kim et al., 2016).
Women who resist RC and preserve their autonomous reproductive decision-making use a variety of safety and harm reduction strategies (Allsworth et al., 2013; McCauley et al., 2018; Paterno et al., 2017). Guidelines for providers who encounter women experiencing RC include recommending less detectable methods of contraception and abortion and social services referral (American College of Obstetricians & Gynecologists, 2013; Chamberlain & Levenson, 2012).
Demographic risk factors for RC have been identified in some studies, including younger age (Center for Impact Research, 2000; Rosenfeld et al., 2017), less education (E. Miller et al., 2014; E. Miller, Decker, et al., 2010; Upadhyay et al., 2014), higher religious activity (Wright et al., 2018), non-Hispanic Black, multiracial or Latina, or women born in the United States when compared to those born elsewhere (Clark et al., 2014; Hess & Del Rosario, 2018; Holliday et al., 2017; E. Miller, Decker, et al., 2010; E. Miller et al., 2014; Rosenfeld et al., 2017; Sutherland et al., 2015; Upadhyay et al., 2014). Relationship factors have also been examined, revealing greater age discrepancy with partner (Center for Impact Research, 2000; Rosenbaum et al., 2016), not being married (Clark et al., 2014; E. Miller et al., 2014; Rosenfeld et al., 2017), and multiple sex/dating partners (Fasula et al., 2018; Katz et al., 2017; Paterno et al., 2018) to be significant risk factors. RC is also strongly associated with IPV (Hill et al., 2019; Holliday et al., 2017; Willie et al., 2019) but questions remain about the nature of this association and whether RC is a type of IPV or a distinct phenomenon.
RC behaviors are associated with numerous health outcomes (in addition to unintended pregnancy) including PTSD and depression (Alexander et al., 2016; Anderson et al., 2017; Fasula et al., 2018; McCauley, Falb, et al., 2014), abortion (Cha et al., 2016), sexually transmitted infection (Fasula et al., 2018; Jones et al., 2016; Northridge et al., 2017), preterm birth (Liu et al., 2016), and decreased breastfeeding (Wallenborn et al., 2018).
RC has been studied in diverse populations of women, but not in Latina women specifically, despite evidence that Latina women have higher risk for RC (Clark et al., 2014; E. Miller et al., 2014; Sutherland et al., 2015) as well as for unintended pregnancy (Finer & Zolna, 2016; Kim et al., 2016). Prevalence of RC in community samples of Latina women ranges from 14 (Clark et al., 2014) to 17 percent (E. Miller, Decker, et al., 2010; Sutherland et al., 2015). Latina women are noted in some studies to be less likely to seek help or report IPV to police due to concerns about their own or other family members’ legal immigration status (Pitts, 2014; Reina et al., 2014), and it may be that help-seeking for RC is similarly limited.
The purpose of this study was to explore demographic and partner-related risk factors for RC, association of RC with unintended pregnancy and IPV, and the use of RC safety and harm reduction strategies among Latina women attending an urban health center.
Methods
Design & Sample
We conducted a cross-sectional survey with Latina women presenting for care at three locations of a Federally Qualified Health Center (FQHC) serving low-income, primarily immigrant residents of a mid-Atlantic metropolitan area, between January and August 2018. The development of the survey was informed by qualitative research (Grace et al., 2020). The study survey was field-tested with 11 Latina women, including cognitive interviewing to identify unexpected issues with wording and interpretation. Eligible women were between the ages of 15 and 45, self-identified as Latina, Hispanic or Spanish, and had a dating or sexual partner in the past year. Research assistants who were fluent in Spanish and English distributed flyers in clinic waiting rooms and interested women were screened for eligibility and completed the survey in Spanish or English on a tablet computer with audio-assistance capability. The survey was also available to complete from home using a web link (6 women (1.2%) chose this option). Eligibility screening was completed 771 times, 123 women were ineligible (16.0%; no dating/sexual partner in past year, under 15 or over 45 years of age, did not identify as Latina/Hispanic/Spanish). A total of 648 eligible women provided consent and began the survey; of them, 148 women (22.8%) did not complete it either due to inadequate time or loss of interest, and 18 women (2.8%) did not have complete data for the key variables of RC and/or IPV, generating a final sample of 482 women. We analyzed differences between those who did and did not complete the survey, among the 648 women who began the survey. Non-completers were significantly more likely to have never had an abortion (98.6% vs. 92.4%, p=0.007), to be not married (58.8% vs. 32.1%, p<0.001), to have more than one past year sexual partner (21.6% vs. 11.2%, p= 0.005) to have a partner who used drugs (16.7% vs 5.4%, p=0.013) and to not be currently pregnant (82.4% vs. 72.8%, p=0.018). Power analysis indicated a sample size of 500 was sufficient to detect statistically significant differences in key outcomes.
Measures
Potential correlates were suggested by existing literature, and included demographics, such as age, education, race, nativity, employment, parity, relationship status, years in the United States and partner demographics and characteristics, such as age, length of relationship, and substance use. The measures were translated, back-translated and field-tested. The primary outcome of interest was RC; RC was also examined as a predictor for the other outcome of interest, unintended pregnancy.
Reproductive coercion.
Past-year RC was measured with 13 yes/no questions derived from adaptations of existing RC measures which have been tested in observational and intervention RC research, including substantial numbers of Latina participants (Clark et al., 2014; Dick et al., 2014; Kazmerski et al., 2015; McCauley, Dick, et al., 2014; E. Miller et al., 2011, 2014; E. Miller, Decker, et al., 2010). Additional questions on abortion coercion were added, and questions were adapted to isolate pregnancy-promoting intent from coercive behaviors, based on recent literature (Katz et al., 2017; Katz & Sutherland, 2017). Five questions assessed pregnancy coercion, four questions assessed birth control sabotage, and four questions assessed controlling the outcome of a pregnancy. RC was defined as a positive response to any item.
Unintended pregnancy.
The 6-item London Measure of Unplanned Pregnancy (LMUP; Barrett et al., 2004) was used with slight adaptations based on interview data from the earlier phase of the study. The LMUP assesses planning, wantedness and timing of pregnancy. Participants were asked about any pregnancy that occurred in the past year. Responses were scored from zero to two, resulting in a pregnancy planning score of zero to twelve, with a higher score indicating greater planning, and interpretation categories of “planned” (10–12), “ambivalent” (4–9), and “unplanned” (0–3) (Cronbach alpha .70 in this sample).
Partner substance abuse.
The Alcohol Use Disorder Identification Test (AUDIT) and Drug Abuse Screening Tool (DAST-10) were re-worded to assess partner substance use. Alcohol use was measured with five questions on frequency of alcohol use behaviors (Cronbach alpha .70). Binge drinking, considered 5 or more drinks in 2 hours (Centers for Disease Control & Prevention (CDC), 2018), was scored as a response of anything greater than “3 or 4” in response to the question “How many drinks containing alcohol does your partner have on a typical day when they are drinking?”, or a response of anything greater than “Never” in response to the question “How often does your partner have six or more drinks on one occasion?”. Drug use was measured with six yes/no questions from the DAST-10 Scale (Yudko et al., 2007; Cronbach alpha .70). A “yes” response to any question was scored as “partner drug use”. These items referred specifically to the partner who was asked about in RC questions.
IPV.
The 4-item HARK scale (Sohal et al., 2007) assesses physical violence, sexual violence and controlling behaviors and was used to measure past-year IPV. We used a cutoff score of ≥ 1 which has 81% sensitivity and 95% specificity when compared to the 30 items of the Composite Abuse Scale (CAS; Sohal et al., 2007). These items referred specifically to the partner who was asked about in RC questions.
Acculturation.
The 4-item Brief Acculturation Scale for Hispanics (BASH) assessed what language the participant uses to read, speak and think (Cronbach alpha .88). Responses ranging from 1 for “Spanish only” to 5 for “English only” were summed and divided by the number of completed items. A score of 3 or less was considered “low” acculturation and greater than 3 was considered “high” acculturation.
Safety and Harm Reduction Strategies
Actions taken by women to stay safe in coercive relationships or to maintain their autonomous reproductive decision-making when faced with coercive behaviors were assessed with 6 investigator-developed yes/no questions based on qualitative data from the study (Grace et al., 2020) and questions from current IPV (Glass et al., 2015) and RC studies (Tancredi et al., 2015). Examples of questions included “Did you change your method of birth control so your partner could not tamper with (mess with) it?” and “In the past year, have you hidden a method of birth control from your partner?”
Data Analysis
Descriptive statistics (means, standard deviations, and frequencies) were used to describe the sample, the prevalence of types of RC behaviors and the prevalence of safety and harm reduction strategies used. Chi square and t-tests were used to examine differences between those who had and had not experienced RC on risk factors and covariates. To account for possible multicollinearity, variables that were significantly related (p<0.05) to RC in the bivariate analyses (with the exception of one variable, current pregnancy, which was believed to have a spurious association) were entered into an adjusted logistic regression model with RC as the outcome, to determine the independent effects of the predictor variables with RC. For participants who reported a past-year pregnancy (n=185), unintended pregnancy score was handled continuously for analysis, following a categorization for illustrative purposes. T-tests and ANOVA were used to examine differences in mean unintended pregnancy scores by covariates. Multiple linear regression was used to examine the relationship between RC and unintended pregnancy score for these participants. In adjusted models, variables that were significantly related to unintended pregnancy in the bivariate analysis were entered into a linear regression with unintended pregnancy score as the outcome. The first adjusted model predicting unintended pregnancy focused on RC as a primary exposure. In the second model IPV, which is known to co-occur with RC, was added. The third model explored combinations of RC and IPV through a categorical variable (RC only, IPV only, both IPV and RC, and none) to clarify these distinct experiences in isolation and in combination. Mean imputation was conducted for individual missing items in the unintended pregnancy score (n=5 participants, 1.0% of full sample). Thereafter, the sample size floated to accommodate small amounts of missing data in other variables. The direction and significance of results using the floating sample size approach was confirmed by sensitivity analyses using mean imputation and missing indicator method; all results presented use the floating sample method for precision. Analyses were conducted in SPSS Statistics 25.0 (IBM Corp., 2017).
Ethics/IRB
The study was approved by the Johns Hopkins Medicine Institutional Review Board (IRB00129418). Research Assistants received standardized human subjects research ethics training as well as IPV advocacy training including safety assessment, technology safety, IPV resource referrals, and suicidality protocols. Participants reviewed tablet-based survey/questionnaire informed consent covering the nature of the questions, information about confidentiality, and the voluntary nature of the study including that they can refuse to answer any question. To thank them for their time, participants had the opportunity to enter a raffle for one of twenty $50 retail gift cards.
Results
The mean age of the study sample was 30.48 (SD 6.86; Table 1). Most participants were from the Central American countries of El Salvador (49.8%), Guatemala (12.4%) and Honduras (11.2%); just over 9 percent of the sample was born in the United States (US). The majority of participants who were not born in the US had lived there for more than 5 years (71.0%), but the majority of participants had low levels of acculturation (96.0%, not presented in table). Twenty-one percent of the full sample were missing at least one item of data. The majority of key variables were missing data from fewer than 5 percent of the sample, with the exception of length of time lived in the US (5.0%) in which most missing data (4.6%) was due to participants indicating “don’t know” or “refuse to answer” as a response, ever had an abortion (missing 7.7%) and partner age (missing 6.0%).
Table 1.
Characteristics of the Study Population and Distribution of Reproductive Coercion (N=482)
| Characteristic | Prevalence %1 (N) | Experienced RC N=812 %1 (n) | Did not experience RC N=4012 %1 (n) | p-value3 | Adjusted Multiple Regression N=4312 ß (95% CI) p-value4 |
|---|---|---|---|---|---|
| Coercive/violent behaviors | |||||
| Experienced RC in past year | -- | -- | -- | ||
| Yes | 16.8 (81) | ||||
| No | 83.2 (401) | ||||
| Experienced IPV in past year | <0.001 | 4.47 (2.06, 9.70) p<0.001 | |||
| Yes | 10.2 (49) | 32.1 (26) | 5.7 (23) | ||
| No | 89.8 (433) | 67.9 (55) | 94.3 (378) | ||
| Combinations of past year IPV/RC | -- | -- | -- | ||
| Neither | 78.4 (378) | ||||
| RC and IPV | 5.4 (26) | ||||
| RC only | 11.4 (55) | ||||
| IPV only | 4.8 (23) | ||||
| Demographics | |||||
| Age (mean, SD) | 30.48, 6.86 | 27.60, 7.08 | 31.06, 6.68 | <0.001 | 0.95 (0.91, 1.00) p=0.038 |
| Born in the US | 0.001 | 1.14 (0.49, 2.64) p=0.769 | |||
| Yes | 9.1 (43) | 18.8 (15) | 7.1 (28) | ||
| No | 90.9 (432) | 81.3 (65) | 92.9 (367) | ||
| Country of Birth | N/A | ||||
| United States | 9.1 (43) | ||||
| El Salvador | 49.8 (236) | ||||
| Guatemala | 12.4 (59) | ||||
| Honduras | 11.2 (53) | ||||
| Mexico | 9.7 (46) | ||||
| Other Caribbean or Central | |||||
| American country | 3.8 (18) | ||||
| South America | 1.9 (9) | ||||
| Other | 2.1 (10) | ||||
| Currently employed | 0.711 | ||||
| Yes | 43.1 (204) | 45.0 (36) | 42.7 (168) | ||
| No | 56.9 (269) | 55.0 (44) | 57.3 (225) | ||
| Education | 0.932 | ||||
| Less than high school diploma or GED | 40.1 (192) | 38.3 (31) | 40.5 (161) | ||
| High school diploma, GED or some college | 43.4 (208) | 44.4 (36) | 43.2 (172) | ||
| Associates degree or higher | 16.5 (79) | 17.3 (14) | 16.3 (63) | ||
| Importance of religion in daily life | 0.122 | ||||
| Very important | 71.3 (340) | 64.2 (52) | 72.7 (288) | ||
| Somewhat or not important | 28.7 (137) | 35.8 (29) | 27.3 (108) | ||
| Years living in the US | 0.516 | ||||
| 5 years or less | 29.0 (133) | 26.0 (20) | 29.7 (113) | ||
| More than 5 years | 71.0 (325) | 74.0 (57) | 70.3 (268) | ||
| Sexual, reproductive and relationship history | |||||
| Currently pregnant | 0.028 | ||||
| Yes | 27.2 (131) | 17.3 (14) | 29.2 (117) | ||
| No | 72.8 (351) | 82.7 (67) | 70.8 (284) | ||
| Ever had a miscarriage | 0.922 | ||||
| Yes | 23.9 (112) | 23.5 (19) | 24.0 (93) | ||
| No | 76.1 (357) | 76.5 (62) | 76.0 (295) | ||
| Ever had an abortion | 0.001 | 2.25 (0.93, 5.47) p=0.073 | |||
| Yes | 7.6 (34) | 16.7 (13) | 5.7 (21) | ||
| No | 92.4 (411) | 83.3 (65) | 94.3 (346) | ||
| Currently married to partner (includes common-law marriage) | <0.001 | 0.73 (0.40, 1.33) p=0.305 | |||
| Yes | 67.9 (326) | 48.1 (39) | 71.9 (287) | ||
| No | 32.1 (154) | 51.9 (42) | 28.1 (112) | ||
| Number of sexual partners in past year | <0.001 | 1.905 (0.92, 3.97) p=0.085 | |||
| 1 | 88.8 (428) | 76.5 (62) | 91.3 (366) | ||
| More than 1 | 11.2 (54) | 23.5 (19) | 8.7 (35) | ||
| Partner factors | |||||
| Age discrepancy with partner (mean, SD) | 2.50, 5.75 (n=453) | 3.13, 6.00 | 2.38, 5.69 | 0.299 | |
| Partner binge drinking | <0.001 | 1.71 (0.95, 3.07) p=0.075 | |||
| Yes | 28.7 (136) | 48.8 (39) | 24.6 (97) | ||
| No | 71.3 (338) | 51.2 (41) | 75.4 (297) | ||
| Partner drug use | <0.001 | 1.61 (0.58, 4.48) p=0.361 | |||
| Yes | 5.4 (26) | 17.5 (14) | 3.0 (12) | ||
| No | 94.6 (453) | 82.5 (66) | 97.0 (387) | ||
Column percents.
Sample size floats to accommodate small amounts of missing data
Based on t-test or chi-square.
Based on logistic regression.
Reproductive coercion
Approximately 1 in 6 (16.8%; n=81) women in the sample experienced one or more forms of RC in the past year, and 10.2% (n=49) experienced IPV in the past year (Table 1). Of those who experienced RC, 67.9% (n=55/81) did not also experience IPV (Figure 1). Just over 5 percent of the sample experienced both RC and IPV (5.4%), roughly the same proportion that experienced IPV without RC (4.8%), and about half as many as experienced RC without IPV (11.4%). Types of RC behaviors experienced were grouped into three main categories according to RC literature: pregnancy coercion, birth control sabotage, and controlling the outcome of a pregnancy (Table 2). The most commonly experienced RC behavior was telling a woman not to use birth control (43.2% of those who experienced RC), followed by taking off the condom while having sex (38.2% of those who experienced RC). Other more commonly reported RC behaviors were making a woman have sex without a condom (21.0% of those who experienced RC) and forcing or pressuring a woman to become pregnant (19.8% of those who experienced RC).
Figure 1.
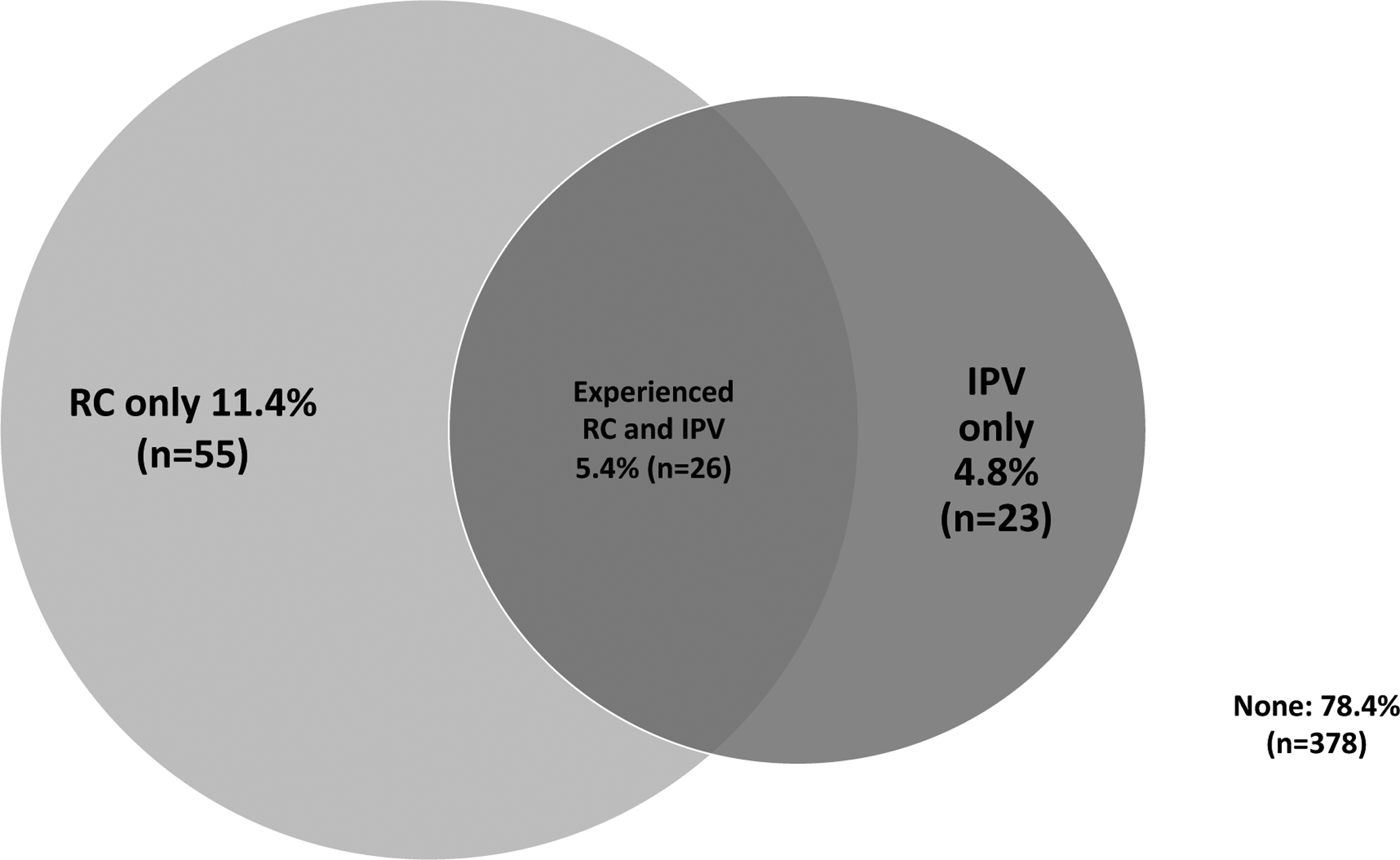
Experiences of past-year reproductive coercion and intimate partner violence among sample (N=482)
Note: Circles represent mutually exclusive categories.
Table 2.
Types of RC Experienced1 in the Past Year
| Behavior | N | Sample prevalence (n=482) % | Prevalence in Women who Experienced RC (n=81) % |
|---|---|---|---|
| Pregnancy Coercion | |||
| Told you not to use any birth control | 35 | 7.4 | 43.2 |
| Tried to force or pressure you to become pregnant | 16 | 3.3 | 19.8 |
| Said they would leave you if you did not get pregnant | 7 | 1.5 | 8.6 |
| Told you they would have a baby with someone else if you did not get pregnant | 7 | 1.5 | 8.6 |
| Hurt you physically because you did not agree to get pregnant | 3 | 0.6 | 3.7 |
| Birth Control Sabotage | |||
| Taken off the condom while having sex | 31 | 6.5 | 38.2 |
| Made you have sex without a condom | 17 | 3.6 | 21.0 |
| Taken your birth control away or kept you from going to clinic to get birth control | 5 | 1.0 | 6.2 |
| Put holes in condom or broken condom on purpose while having sex | 1 | 0.2 | 1.2 |
| Controlling the Outcome of Pregnancy | |||
| Tried to MAKE you get an abortion | 7 | 1.5 | 8.6 |
| Tried to STOP you from getting an abortion | 5 | 1.1 | 6.2 |
| Violence or threats to try to MAKE you get an abortion | 4 | 0.8 | 4.9 |
| Violence or threats of violence to try to STOP you from getting an abortion | 0 | 0.0 | 0.0 |
Not mutually exclusive, i.e., women can experience more than one type of RC
Risk factors for RC
Participants who experienced RC were younger than those who did not experience RC (27.60 vs. 31.06, p<0.001; Table 1) and more likely to be born in the United States (18.8% vs. 7.1%, p=0.001) and also to experience IPV (32.1% vs. 5.7%, p<0.001). RC was also significantly associated with not currently being pregnant at the time of the survey (82.7% vs. 70.8% p=0.028), and with having had one or more abortions (16.7% vs. 5.7%, p=0.001). Relationship status was associated with RC; participants who experienced RC were significantly less likely to be married (legally or common-law; 48.1% vs. 71.9%, p<0.001) than those who did not experience RC, and more likely to have had more than one past-year partner (23.5% vs. 8.7%, p<0.001). RC was significantly associated with having a partner who binge drinks (48.8% vs. 24.6%, p <0.001) and who uses drugs (17.5% vs. 3.0%, p<0.001). In an adjusted model, RC was significantly associated with IPV (AOR 4.47, 95% CI 2.06–9.70, p<0.001) and younger age (AOR 0.95, 95% CI 0.91–1.00, p=0.038).
RC, IPV, and unintended pregnancy
One hundred eighty-five women (38.4% of the full sample) reported a pregnancy in the past year (Table 3). The average unintended pregnancy score was 8.29; when unintended pregnancy score was categorized, 48.1% (n=89) of pregnancies were planned, 40.5% (n=75) were ambivalent, and 11.4% (n=21) were unplanned (data not shown). When unintended pregnancy was handled categorically, those who experienced past-year RC were more likely to have an unplanned pregnancy than those who did not experience RC (34.3% vs. 6.0%, p<0.001; data not shown).
Table 3:
Associations of Unintended Pregnancy with RC, IPV, and Covariates, Among Participants with a Past-Year Pregnancy (N=185)
| Characteristic | n | UIP Score (SD) | Standardized Regression Coefficient ß (95% CI) p-value | Adjusted Multiple Regression (n=177) ß (95% CI) p-value | ||
|---|---|---|---|---|---|---|
| Model 1 (RC and covariates) | Model 2 (RC, IPV and covariates) | Model 3 (RC/IPV categories and covariates) | ||||
| Coercive/violent behaviors | ||||||
| Experienced RC in past year | −0.27 (−0.41, −0.12) p<0.001 | −0.15 (−0.30, −0.00) p=0.038 | −0.12 (9–0.27, 0.03) p=0.116 | -- | ||
| Yes | 35 | 6.46 (4.05) | ||||
| No | 150 | 8.72 (2.96) | ||||
| Experienced IPV in past year | −0.25 (−0.40, −0.11) p=0.001 | -- | −0.1 (−0.25, 0.05) p=0.204 | -- | ||
| Yes | 19 | 5.84 (3.17) | ||||
| No | 166 | 8.57 (3.21) | ||||
| Combinations of past year IPV/RC | 0.26 (0.12, 0.41) p<0.001 | |||||
| Neither | 143 | 8.82 (2.94) | ref | |||
| RC and IPV | 12 | 5.42 (3.42) | −0.15 (−0.29, 0.00) p=0.052 | |||
| RC only | 23 | 7.00 (4.31) | −0.12 (−0.26, 0.03) p=0.113 | |||
| IPV only | 7 | 6.57 (2.76) | −0.08 (−0.23, 0.06) p=0.239 | |||
| Demographics | ||||||
| Age (mean, SD) | 185 | -- | 0.27 (0.12, 0.41) p<0.001 | 0.20 (0.05, 0.34) p=0.008 | 0.20 (0.05, 0.35) p=0.007 | 0.20 (0.05, 0.35) p=0.007 |
| Born in the US | −0.20 (−0.35, −0.06) p=0.006 | −0.07 (−0.21, 0.08) p=0.378 | −0.06 (−0.20, 0.09) p=0.465 | −0.06 (−0.21, 0.09) p=0.443 | ||
| Yes | 17 | 6.18 (3.49) | ||||
| No | 164 | 8.50 (3.22) | ||||
| Currently employed | −0.08 (−0.22, 0.07) p=0.307 | -- | -- | -- | ||
| Yes | 53 | 7.91 (2.95) | ||||
| No | 129 | 8.45 (3.39) | ||||
| Education | 0.05 (−0.09, 0.20) p=0.478 | -- | -- | -- | ||
| Less than high school diploma or GED | 65 | 8.26 (3.07) | ||||
| High school diploma, GED or some college | 84 | 8.01 (3.51) | ||||
| Associates degree or higher | 35 | 8.91 (3.21) | ||||
| Importance of religion in daily life | −0.15 (−0.29, 0.00) p=0.049 | −0.04 (−0.19, 0.11) p=0.597 | −0.04 (−0.19, 0.11) p=0.593 | −0.04 (−0.18, 0.11) p=0.608 | ||
| Very important | 133 | 8.60 (3.13) | ||||
| Somewhat or not important | 49 | 7.51 (3.67) | ||||
| Length of time lived in the US | 0.13 (−0.01, 0.28) p=0.076 | -- | -- | -- | ||
| 5 years or less | 63 | 7.68 (3.44) | ||||
| More than 5 years | 112 | 8.61 (3.24) | ||||
| Sexual, reproductive and relationship history | ||||||
| Currently pregnant | 0.03 (−0.11, 0.18) p=0.657 | -- | -- | -- | ||
| Yes | 104 | 8.39 (3.08) | ||||
| No | 81 | 8.17 (3.59) | ||||
| Ever had an miscarriage | 0.13 (−0.02, 0.27) p=0.088 | -- | -- | -- | ||
| Yes | 50 | 8.98 (3.15) | ||||
| No | 134 | 8.05 (3.34) | ||||
| Ever had an abortion | −0.13 (−0.28, 0.02) p=0.090 | -- | -- | -- | ||
| Yes | 12 | 6.67 (4.25) | ||||
| No | 161 | 8.37 (3.27) | ||||
| Currently married to partner (includes common-law marriage) | 0.29 (0.14, 0.43) p<0.001 | 0.13 (−0.02, 0.28) p=0.101 | 0.12 (−0.02, 0.27) p=0.112 | 0.12 (−0.03, 0.27) p=0.121 | ||
| Yes | 142 | 8.81 (3.02) | ||||
| No | 43 | 6.57 (3.63) | ||||
| Number of sexual partners in past year | −0.01 (−0.16, 0.13) p=0.852 | -- | -- | -- | ||
| 1 | 175 | 8.30 (3.31) | ||||
| More than 1 | 10 | 8.10 (3.38) | ||||
| Partner Factors | ||||||
| Age discrepancy with partner (mean, SD) | 171 | -- | −0.14 (−0.29, 0.01) p=0.073 | -- | -- | -- |
| Partner binge drinking | −0.11 (−0.25, 0.04) p=0.158 | |||||
| Yes | 46 | 7.72 (3.40) | ||||
| No | 136 | 8.52 (3.27) | ||||
| Partner drug use | −0.27 (−0.41, −0.13) p<0.001 | −0.15 (−0.30, −0.01) p=0.040 | −0.13 (−0.27, 0.02) p=0.101 | −0.13 (−0.27, 0.02) p=0.102 | ||
| Yes | 11 | 4.82 (2.93) | ||||
| No | 173 | 8.54 (3.19) | ||||
Based on t-test or ANOVA.
Based on linear regression.
The mean pregnancy planning score was lower for women who experienced RC (6.46 vs. 8.72, p<0.001), indicating less planning. In bivariate analysis, additional factors significantly associated with lower pregnancy planning scores were experiencing past-year IPV, younger age, being born in the US, lower importance of religion, not being currently married to partner, and partner drug use. In adjusted models, RC remained significantly associated with lower pregnancy planning scores (β −0.154, 95% CI −0.301, −0.007, p=0.038), as did age (β 0.197, 95% CI 0.050, 0.344, p=0.008) and partner drug use (β −0.153, 95% CI −0.300, −0.006, p=0.040). In the second model which examined both RC and IPV in the presence of covariates, RC attenuated to non-significance (β −0.122, 95% CI −0.269, 0.025, p=0.116) as did IPV (β −0.101, 95% CI −0.248, 0.046, p=0.204). When RC and IPV experiences were explored as mutually exclusive categories, the combination of past-year IPV and RC was associated with unintended pregnancy with borderline statistical significance (β −0.147, p=0.052). RC in isolation demonstrated a nonsignificant trend (β −0.115, p=0.113).
Safety and harm reduction strategies for RC
The most common safety strategy used by the full sample of women in the study was ending a relationship because it felt unhealthy, unsafe or abusive (6.1% of all women; 27.9% of women who had experienced IPV and/or RC; out of all those who ended relationships in the past year, this was the reason given by 42.6%). This was followed by use of a less detectable method of contraception so that a partner would not find out (3.4% of women, 10.1% of women who used specified methods did so for this reason; Table 4). Other safety or harm reduction strategies that were used are presented in Table 4. In total, 10.6% (n=49) of participants used a safety or harm reduction strategy to prevent an RC behavior or minimize the risk of pregnancy from RC in the previous year. Two-thirds (66.7%, n=54) of those who experienced RC used one of these strategies regardless of whether it was specifically used to prevent RC (for example, reported they used an IUD in the past year), and nearly one-quarter (24.7%, n=20) used one of these strategies specifically to prevent RC (for example, reported they used an IUD in the past year so that a partner would not find out they were using contraception).
Table 4.
Use of Safety/Harm Reduction Strategies in the Sample and Within Subgroups, by Domain
| Full sample % (n/n) | % (n/n) within relevant subgroup | |
|---|---|---|
| Safety in Contraception | ||
| Used less detectable method of contraception in past year (IUD, implant, injectable) so partner would not find out about use | 3.4% (16/471) | 10.1% (16/158) of participants who used less detectable methods |
| Changed method of contraception in past year so that partner would not tamper with it | 0.6% (3/478) | 5.1% (3/59) of those who changed method at all |
| Hidden a method of contraception from partner in past year due to fear partner would be upset with you for using it | 0.4% (2/480) | 50% (2/4) of those who hid a method at all |
| Abortion-related safety | ||
| Had an abortion in past year in order to keep partner from controlling you | 0.2% (1/480) | 8.3% (1/12) of participants who had abortions |
| Did not tell partner about abortion you had in the past year due to fear of partner or thinking partner would be upset/angry | 0.4% (2/480) | 16.7% (2/12) of people who had abortions |
| Relationship Change | ||
| Ended a relationship in the past year because it felt unhealthy, unsafe or abusive | 6.1% (29/473) | 42.6% (29/68) of those who ended relationships27.9% (29/104) of those who experienced RC and/or IPV |
| Any Safety Strategy | ||
| Used any safety strategy in past year | 10.6% (49/463) | |
| Experienced RC and used any safety strategy | 4.1% (20/482) |
Discussion and Implications
In this sample of Latina women seeking services at a community health center, prevalence of RC was 16.8%, and significant risk factors in adjusted models included IPV and younger age. Supporting the notion of the healthy immigrant effect (the idea that residents of a country who are foreign-born have improved health outcomes over their native-born counterparts; L. S. Miller et al., 2016; Urquia et al., 2012), this study found that participants who immigrated to the United States had significantly lower rates of RC than those who were born in the US, however, time lived in the US was not associated with RC. The most common types of RC experienced, telling a woman not to use birth control and removing a condom while having sex, highlight the importance of less detectable methods of contraception for women who wish to control their fertility while negotiating or escaping these coercive aspects of their relationships.
Findings on prevalence and correlates of RC among this sample of Latina women were aligned with existing literature in many areas. However, unlike other studies which found age discrepancy with partner to be a significant risk factor for RC (Center for Impact Research, 2000; Rosenbaum et al., 2016), age discrepancy was not a significant risk factor in our sample of Latina women. Using violence or threats of violence to prevent a woman from having an abortion was not experienced by any women in this study, in contrast with qualitative research reports on behaviors to sabotage abortion including violence (Hathaway et al., 2005; Moore et al., 2010; Nikolajski et al., 2015; Thiel de Bocanegra et al., 2010; Tsui et al., 2011). Evidence linking abortion history with RC in this sample is consistent with other studies (Sutherland et al., 2015) and may be explained by the strong association between RC and unintended pregnancy (p<0.001).
Evidence linking partner substance use with RC is consistent with research demonstrating the connection between sexual assault and binge drinking (Abbey et al., 2014), as well as research with Latina women showing IPV to be associated with partner substance abuse (Hazen & Soriano, 2007), and also may reflect the strong association between IPV and RC (p<0.001). Overall, rates of alcohol use and abuse in Latino populations are noted to be lower than in non-Hispanic White populations (Chartier & Caetano, 2010; Lipsky & Caetano, 2009). Women who reported more than one sexual or romantic partner in the past year were also more likely to experience RC. This is consistent with other RC studies (Fasula et al., 2018; Katz & Sutherland, 2017), and additionally, multiple sexual partners may reflect relationship instability, which has been found to increase risk for RC (Paterno et al., 2018). While past qualitative evidence shows some perpetrators of RC using violence to control the outcome of a pregnancy by causing a miscarriage (Coggins & Bullock, 2003; Grace et al., 2020; Moore et al., 2010), this study did not find any significant association between RC and miscarriage, likely because a large number of pregnancies end in miscarriage irrespective of violence or coercion (American College of Obstetricians & Gynecologists (ACOG), 2018). More research may be needed to understand the relationship between pregnancy and not experiencing RC; the relationship may reflect the complexity of feelings about the pregnancy by the woman, leading to altered perceptions of pregnancy intention or circumstances under which it occurred (Rocca et al., 2019), or it may be that an existing pregnancy eliminates the necessity for RC by the abusive partner.
The association between RC and unintended pregnancy was supported in our sample of Latina women. The first regression model which examines only the effect of RC on unintended pregnancy (without controlling for IPV), shows RC having a significant effect on pregnancy planning score similar to the strength of partner substance abuse. When adding IPV to the model, the effect of RC on unintended pregnancy attenuated to non-significance. When examined as mutually exclusive exposure combinations, only the combination of RC and IPV had a borderline effect on pregnancy intention, while each of IPV and RC in isolation were not significantly associated. Previous research has wrestled with the question of whether it is RC, IPV or the combination that impacts unintended pregnancy (Hill et al., 2019; E. Miller et al., 2012, 2014; E. Miller & Silverman, 2010). Pregnancy intention is affected by a complex array of motivations in all relationships, including those that are non-violent (Ajzen & Klobas, 2013; Alexander et al., 2019; Carter et al., 2013; Rocca et al., 2010). In this study, RC and IPV had a synergistic effect on unintended pregnancy, which may reflect the combined impact of an abuser’s desire for power and control with the focus on pregnancy-related outcomes. It may be that women who experience RC behaviors without accompanying violence or abuse are better able to resist attempts to control their fertility, and that the impact of IPV on unintended pregnancy is due primarily to overlap with RC behaviors.
RC was strongly associated with IPV in this study, and findings are strengthened by the measuring of past year experiences of RC and IPV with the same partner. This advances prior research that asks about past year RC and IPV, which may have been experienced from different partners. Despite this strong association, the majority of those who experienced RC did not also experience any other form of IPV, lending support to the proposition that RC and IPV are distinct but related phenomena in this sample of primarily Central American women, as suggested by other researchers (Fay & Yee, 2018; E. Miller, Jordan, et al., 2010). The categorical exploratory analysis of the influence of RC and IPV experiences (as mutually exclusive or combined experiences) was underpowered but suggests that RC has a unique role in unintended pregnancy either with or without IPV, and a synergistic effect when both are present. This points to the critical importance of assessing for RC whenever IPV is reported and offering less detectable methods of contraception to anyone who reports RC. It also illuminates the need to further address these relationships in future research.
Some women did use the recommended less-detectable methods of contraception in order to maintain reproductive autonomy, but more women separated from their partners due to the relationship being unhealthy, unsafe or abusive. Qualitative research findings offer caution that even less-detectable methods of birth control may be detected by a coercive partner (Dasari et al., 2015; Grace et al., 2020), which may account for the low utilization of these methods among women experiencing RC. Providers should fully inform women of the limits of non-detectability of these methods, when following guidelines to offer them to women experiencing RC. Women with low levels of acculturation, like the majority of women in this study, are found to less frequently use these less detectable methods in at least one other study (Roncancio et al., 2012). This highlights the salience of this study’s focus on Latina women and the critical need for continued work to identify and support recommendations for women seeking to protect themselves from RC. Overall, the small number of participants using safety and harm reduction strategies points to the need for information, resources, and a healthcare and policy response to this challenge to women’s health.
Limitations and Strengths
Findings should be considered in light of several limitations. Survey noncompletion was more common among women who also had risk factors for RC; it is possible that data were biased in favor of those with lower risk, and therefore RC may be underreported. Two key variables had more than 5 percent missing data: history of abortion, which women in this sample may have been reluctant to report, and partner age, which women in this sample may not have known. These are significant factors in other RC literature, and this data absence may have biased the results, but sensitivity analysis confirmed the direction and significance of findings. Cross-sectional design precludes conclusions about temporality of RC relative to unintended pregnancy. Results are most relevant to the low-income Latina women receiving or accompanying someone receiving health services in this urban area, the majority of whom were from four Central American countries. Findings may not be generalizable to women from other countries or living in rural areas or from higher income groups. Retrospective data may have recall or social desirability bias. Despite the large sample size of 482, analyses exploring the relationship between RC and unintended pregnancy were restricted to a smaller subset of women who had a past-year pregnancy and were not sufficiently powered to detect more modest effect estimates. Study strengths include use of a continuous measure of unintended pregnancy, cognitive interviewing to field-test the survey prior to data collection, and availability of survey audio-assistance for participants with limited or reduced literacy.
Conclusion
This study adds to the growing body of literature on RC by identifying risk factors and outcomes of RC specific to a population of Latina women. Findings support the risk factors identified in other studies as also being relevant in this population and highlight areas for providers to have heightened suspicion for RC, such as when working with women experiencing unintended pregnancy, seeking abortion, or who are suspected or confirmed to be experiencing IPV. This study points to the importance of addressing RC in unintended pregnancy interventions for Latina women. Providers may also have increased vigilance for RC among Latina women who are younger, were born in the United States, who are single, who report partners who binge drink or use drugs, or who report more than one sexual partner in the prior year. In any woman who reports RC, especially those with other risk factors for unintended pregnancy such as younger age and being single, the use of existing provider guidelines for RC is supported in Latina women, with perhaps the greatest benefit to be gained from offering support services to plan for safety and harm reduction when making decisions about leaving unhealthy and unsafe relationships.
Acknowledgements:
This study would not have been possible without the contributions of all of the women who generously shared their stories, and without the Mary’s Center staff, providers and management who supported this study and helped recruit participants.
Grant numbers and funding information:
Funding support for E. Miller: NICHD K24HD075862
Funding support for K. Grace:
American College of Nurse Midwives Fellowship for Graduate Education, American Nurses Foundation (Anne Zimmerman, RN, FAAN Nursing Research Grant and Dorothy A. Cornelius Nursing Research Grant), the Melissa Institute for Violence Prevention and Treatment (Belfer-Aptman Scholars Award), the National League for Nursing (NLN Foundation Scholarship Award), and the Council for the Advancement of Nursing Science/Southern Nursing Research Society Nursing Science Advancement (NSA) Dissertation Grant Award
Funding support for K. Alexander:
NIH/NICHD/OWH K12HD085845
Author Biographies:
Karen Trister Grace, PhD, MSN, CNM, FACNM, is a Postdoctoral Fellow in Population Family and Reproductive Health at the Johns Hopkins Bloomberg School of Public Health in Baltimore, MD., an Adjunct Instructor at Georgetown University School of Nursing & Health Studies in Washington, DC, and in clinical practice at Mary’s Center for Maternal Child Health in the Washington, DC metro area.
Michele R. Decker, ScD, MPH, is an Associate Professor of Population Family and Reproductive Health at the Johns Hopkins Bloomberg School of Public Health in Baltimore, MD. She leads the Women’s Health and Rights program of the Center for Public Health and Human Rights.
Kamila A. Alexander, PhD, MPH, RN is an Assistant Professor at Johns Hopkins School of Nursing. Her research focuses on prevention of sexual health outcome disparities and the complex roles that structural determinants such as intimate partner violence, societal gender expectations, and limited economic opportunities play in the experience of intimate human relationships.
Jacquelyn Campbell, PhD, RN, FAAN, is Professor and Anna D. Wolf Chair at Johns Hopkins University School of Nursing in Baltimore, MD.
Elizabeth Miller, MD, PhD, is Director of the Division of Adolescent and Young Adult Medicine at UPMC Children’s Hospital of Pittsburgh and Professor of Pediatrics at University of Pittsburgh School of Medicine. She has over 15 years of experience with developing and testing clinic and community-based prevention interventions for partner and sexual violence.
Nancy Perrin, PhD, is Professor and Director of the Biostatistics and Methods Core at Johns Hopkins University School of Nursing in Baltimore, MD.
Nancy Glass, PhD, MPH, RN, is Professor and Independence Chair in Nursing Education at Johns Hopkins University School of Nursing in Baltimore, MD, and Associate Director of the Johns Hopkins Center for Global Health.
Footnotes
Conflict of interest: The authors have no conflicts of interest to disclose.
References
- Abbey A, Wegner R, Woerner J, Pegram SE, & Pierce J (2014). Review of Survey and Experimental Research That Examines the Relationship Between Alcohol Consumption and Men’s Sexual Aggression Perpetration. Trauma, Violence, and Abuse, 15(4), 265–282. 10.1177/1524838014521031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I, & Klobas J (2013). Fertility intentions: An approach based on the theory of planned behavior. Demographic Research, 29(8), 203–232. 10.4054/DemRes.2013.29.8 [DOI] [Google Scholar]
- Alexander KA, Sanders RA, Grace KT, Thorpe RJ, Doro E, & Bowleg L (2019). “Having a Child Meant I Had a Real Life”: Reproductive Coercion and Childbearing Motivations among Young Black Men Living in Baltimore. Journal of Interpersonal Violence, 1–29. 10.1177/0886260519853400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander KA, Volpe EM, Abboud S, & Campbell JC (2016). Reproductive coercion, sexual risk behaviours and mental health symptoms among young low-income behaviourally bisexual women: implications for nursing practice. Journal of Clinical Nursing, 25(23–24), 3533–3544. 10.1111/jocn.13238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allsworth JE, Secura GM, Zhao Q, Madden T, & Peipert JF (2013). The impact of emotional, physical, and sexual abuse on contraceptive method selection and discontinuation. American Journal of Public Health, 103(10), 1857–1864. 10.2105/AJPH.2013.301371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Obstetricians & Gynecologists. (2013). Reproductive and sexual coercion. Committee opinion no. 554. Obstetrics & Gynecology, 121(2), 411–415. 10.1097/01.AOG.0000426427.79586.3b [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians & Gynecologists (ACOG). (2018). Early Pregnancy Loss. ACOG Practice Bulletin No. 200. Obstetrics & Gynecology, 132, e197–207. [DOI] [PubMed] [Google Scholar]
- Anderson JC, Grace KT, & Miller E (2017). Reproductive coercion among women living with HIV: An unexplored risk factor for negative sexual and mental health outcomes. AIDS, 31(16), 2261–2265. 10.1097/QAD.0000000000001620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett G, Smith SC, & Wellings K (2004). Conceptualisation, development, and evaluation of a measure of unplanned pregnancy. Journal of Epidemiology and Community Health, 58(5), 426–433. 10.1136/jech.2003.014787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JC (2002). Health consequences of intimate partner violence. Lancet, 359(9314), 1331–1336. 10.1016/S0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- Campbell JC, Anderson JC, McFadgion A, Gill J, Zink E, Patch M, Callwood G, & Campbell D (2018). The Effects of Intimate Partner Violence and Probable Traumatic Brain Injury on Central Nervous System Symptoms. Journal of Women’s Health, 27(6), 761–767. 10.1089/jwh.2016.6311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter M, Kraft JM, Hock-Long L, & Hatfield-Timajchy K (2013). Relationship characteristics and feelings about pregnancy among black and puerto rican young adults. Perspectives on Sexual and Reproductive Health, 45(3), 148–156. 10.1363/4514813 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Impact Research. (2000). Domestic Violence and Birth Control Sabotage: A Report from the Teen Parent Project (Issue February). https://www.issuelab.org/resource/domestic-violence-and-birth-control-sabotage-a-report-from-the-teen-parent-project.html
- Centers for Disease Control & Prevention (CDC). (2018). Alcohol and Public Health, Frequently Asked Questions. https://www.cdc.gov/alcohol/faqs.htm#excessivealcohol
- Cha S, Chapman DA, Wan W, Burton CW, Woolf SH, & Macho SW (2016). Couple Pregnancy Intentions and Induced Abortions in the United States. International Journal of Women’s Health and Reproduction Sciences, 4(4), 2–8. 10.15296/ijwhr.2016.36 [DOI] [Google Scholar]
- Chamberlain L, & Levenson RR (2012). Addressing Intimate Partner Violence, Reproductive and Sexual Coercion: A Guide for Obstetric, Gynecologic and Reproductive Health Care Settings, 2nd Edition. Futures Without Violence. [Google Scholar]
- Chartier K, & Caetano R (2010). Ethnicity and Health Disparities in Alcohol Research. Alcohol Research & Health, 33(1 and 2), 152–160. [PMC free article] [PubMed] [Google Scholar]
- Clark LE, Allen RH, Goyal V, Raker C, & Gottlieb AS (2014). Reproductive coercion and co-occurring intimate partner violence in obstetrics and gynecology patients. American Journal of Obstetrics & Gynecology, 210(1), 42.e1–8. 10.1016/j.ajog.2013.09.019 [DOI] [PubMed] [Google Scholar]
- Coggins M, & Bullock LF (2003). The wavering line in the sand: The effects of domestic violence and sexual coercion. Issues in Mental Health Nursing, 24(6–7), 723–738. 10.1080/01612840305322 [DOI] [PubMed] [Google Scholar]
- Dasari M, Borrero S, Akers AY, Sucato GS, Dick R, Hicks A, & Miller E (2015). Barriers to Long-Acting Reversible Contraceptive Uptake Among Homeless Young Women. Journal of Pediatric and Adolescent Gynecology, 29(2), 104–110. 10.1016/j.jpag.2015.07.003 [DOI] [PubMed] [Google Scholar]
- Decker MR, Flessa S, Pillai RV, Dick RN, Quam J, Cheng D, McDonald-Mosley R, Alexander KA, Holliday CN, & Miller E (2017). Implementing Trauma-Informed Partner Violence Assessment in Family Planning Clinics. Journal of Women’s Health, 26(9), 1–9. 10.1089/jwh.2016.6093 [DOI] [PubMed] [Google Scholar]
- Dick RN, McCauley HL, Jones K, Tancredi DJ, Goldstein S, Blackburn S, Monasterio E, James L, Silverman JG, & Miller E (2014). Cyber dating abuse among teens using school-based health centers. Pediatrics, 134(6), e1560–e1567. [DOI] [PubMed] [Google Scholar]
- Fasula AM, Gray SC, Vereen RN, Carry M, Sales JM, Abad N, Brown JL, Swartzendruber A, & Gelaude DJ (2018). Multiple psychosocial health problems and sexual risk among African American females in juvenile detention: A cross-sectional study. Children & Youth Services Review, 88(February), 74–80. 10.1016/j.childyouth.2018.02.041 [DOI] [Google Scholar]
- Fay K, & Yee L (2018). Reproductive Coercion and Women’s Health. Journal of Midwifery & Women’s Health, 1–8. 10.1111/jmwh.12885 [DOI] [PubMed] [Google Scholar]
- Finer LB, & Zolna MR (2011). Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception, 84(5), 478–485. 10.1016/j.contraception.2011.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, & Zolna MR (2016). Declines in Unintended Pregnancy in the United States, 2008–2011. The New England Journal of Medicine, 374(9), 843–852. 10.1056/NEJMsa1506575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass NE, Clough A, Case J, Hanson G, Barnes-Hoyt J, Waterbury A, Alhusen J, Ehrensaft M, Grace KT, & Perrin N (2015). A safety app to respond to dating violence for college women and their friends: the MyPlan study randomized controlled trial protocol. BMC Public Health, 15(1), 1–13. 10.1186/s12889-015-2191-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace KT, Alexander KA, Jeffers NK, Miller E, Decker MR, Campbell J, & Glass NE (2020). Experiences of reproductive coercion among Latina women and strategies for minimizing harm: “The path makes us strong.” Journal of Midwifery and Women’s Health, e-pub ahea, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JA, Benton L, Copas A, & Stephenson J (2017). Pregnancy Intention and Pregnancy Outcome: Systematic Review and Meta-Analysis. Maternal and Child Health Journal, 0(0), 35. 10.1007/s10995-016-2237-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hathaway JE, Willis G, Zimmer B, & Silverman JG (2005). Impact of partner abuse on women’s reproductive lives. J Am Med Womens Assoc, 60(1), 42–45. [PubMed] [Google Scholar]
- Hazen AL, & Soriano FI (2007). Experiences with intimate partner violence among Latina women. Violence against Women, 13(6), 562–582. 10.1177/1077801207301558 [DOI] [PubMed] [Google Scholar]
- Hess C, & Del Rosario A (2018). Dreams Deferred: A Survey on the Impact of Intimate Partner Violence on Survivors’ Education, Careers, and Economic Security. https://iwpr.org/publications/dreams-deferred-domestic-violence-survey-2018/
- Hill AL, Jones KA, McCauley HL, Tancredi DJ, Silverman JG, & Miller E (2019). Reproductive Coercion and Relationship Abuse Among Adolescents and Young Women Seeking Care at School Health Centers. Obstetrics & Gynecology, 00(00), 1. 10.1097/AOG.0000000000003374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holliday CN, McCauley HL, Silverman JG, Ricci E, Decker MR, Tancredi DJ, Burke JG, Documét P, Borrero S, & Miller E (2017). Racial/Ethnic Differences in Women’s Experiences of Reproductive Coercion, Intimate Partner Violence, and Unintended Pregnancy. Journal of Women’s Health, 26(8), 1–8. 10.1089/jwh.2016.5996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. (2017). IBM SPSS Statistics for Macintosh, version 25 (No. 25). IBM Corp. [Google Scholar]
- Jones KA, Cornelius MD, Silverman JG, Tancredi DJ, Decker MR, Haggerty CL, De Genna NM, & Miller E (2016). Abusive Experiences and Young Women’s Sexual Health Outcomes: Is Condom Negotiation Self-Efficacy a Mediator? Perspectives on Sexual and Reproductive Health, 48(2), 57–64. 10.1363/48e8616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J, Poleshuck EL, Beach B, & Olin R (2017). Reproductive Coercion by Male Sexual Partners: Associations With Partner Violence and College Women’s Sexual Health. Journal of Interpersonal Violence, 32(21), 3301–3320. 10.1177/0886260515597441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J, & Sutherland MA (2017). College Women’s Experiences of Male Partner Contraceptive Interference: Associations With Intimate Partner Violence and Contraceptive Outcomes. Journal of Interpersonal Violence, 1–25. 10.1177/0886260517715600 [DOI] [PubMed] [Google Scholar]
- Kazmerski T, McCauley HL, Jones K, Borrero S, Silverman JG, Decker MR, Tancredi D, & Miller E (2015). Use of reproductive and sexual health services among female family planning clinic clients exposed to partner violence and reproductive coercion. Maternal and Child Health Journal, 19(7), 1490–1496. 10.1007/s10995-014-1653-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim TY, Dagher RK, & Chen J (2016). Racial/Ethnic Differences in Unintended Pregnancy: Evidence From a National Sample of U.S. Women. American Journal of Preventive Medicine, 50(4), 427–435. 10.1016/j.amepre.2015.09.027 [DOI] [PubMed] [Google Scholar]
- Kost K, & Lindberg L (2015). Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography, 52(1), 83–111. 10.1007/s13524-014-0359-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsky S, & Caetano R (2009). Epidemiology of Substance Abuse Among Latinos. 242–260. 10.1080/15332640903110435 [DOI] [PubMed]
- Liu F, Mcfarlane J, Maddoux JA, Cesario S, Gilroy H, & Nava A (2016). Perceived Fertility Control and Pregnancy Outcomes Among Abused Women. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 45(4), 592–600. 10.1016/j.jogn.2016.01.004 [DOI] [PubMed] [Google Scholar]
- Massetti GM, Townsend JS, Thomas CC, Basile KC, & Richardson LC (2018). Healthcare Access and Cancer Screening among Victims of Intimate Partner Violence. Journal of Women’s Health, 27(5), 607–614. 10.1089/jwh.2017.6402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley HL, Bonomi AE, Maas MK, Bogen KW, & O’Malley TL (2018). #MaybeHeDoesntHitYou: Social Media Underscore the Realities of Intimate Partner Violence. Journal of Women’s Health, 27(7), 885–891. 10.1089/jwh.2017.6560 [DOI] [PubMed] [Google Scholar]
- McCauley HL, Dick RN, Tancredi DJ, Goldstein S, Blackburn S, Silverman JG, Monasterio E, James L, & Miller E (2014). Differences by Sexual Minority Status in Relationship Abuse and Sexual and Reproductive Health Among Adolescent Females. Journal of Adolescent Health, 55(5), 652–658. 10.1016/j.jadohealth.2014.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley HL, Falb KL, Streich-Tilles T, Kpebo D, & Gupta J (2014). Mental health impacts of reproductive coercion among women in Cote d’Ivoire. International Journal of Gynecology and Obstetrics, 127(1), 55–59. 10.1016/j.ijgo.2014.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley HL, Silverman JG, Jones KA, Tancredi DJ, Decker MR, McCormick MC, Austin SB, Anderson HA, & Miller E (2017). Psychometric Properties and Refinement of the Reproductive Coercion Scale. Contraception, 95(3), 292–298. 10.1016/j.contraception.2016.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, Schoenwald P, & Silverman JG (2010). Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception, 81(4), 316–322. 10.1016/j.contraception.2009.12.004 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, Schoenwald P, & Silverman JG (2011). A family planning clinic partner violence intervention to reduce risk associated with reproductive coercion. Contraception, 83(3), 274–280. 10.1016/j.contraception.2010.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, Jordan B, Levenson RR, & Silverman JG (2010). Reproductive coercion: connecting the dots between partner violence and unintended pregnancy. Contraception, 81(6), 457–459. 10.1016/j.contraception.2010.02.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, Levenson RR, Herrera L, Kurek L, Stofflet M, & Marin L (2012). Exposure to partner, family, and community violence: gang-affiliated Latina women and risk of unintended pregnancy. Journal of Urban Health, 89(1), 74–86. 10.1007/s11524-011-9631-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, McCauley HL, Tancredi DJ, Decker MR, Anderson H, & Silverman JG (2014). Recent reproductive coercion and unintended pregnancy among female family planning clients. Contraception, 89(2), 122–128. 10.1016/j.contraception.2013.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, & Silverman JG (2010). Reproductive coercion and partner violence: Implications for clinical assessment of unintended pregnancy. Expert Review of Obstetrics and Gynecology, 5(5), 511–515. 10.1586/eog.10.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LS, Robinson JA, & Cibula DA (2016). Healthy Immigrant Effect: Preterm Births Among Immigrants and Refugees in Syracuse, NY. Maternal and Child Health Journal, 20(2), 484–493. 10.1007/s10995-015-1846-3 [DOI] [PubMed] [Google Scholar]
- Moore AM, Frohwirth L, & Miller E (2010). Male reproductive control of women who have experienced intimate partner violence in the United States. Social Science and Medicine, 70(11), 1737–1744. 10.1016/j.socscimed.2010.02.009 [DOI] [PubMed] [Google Scholar]
- Nikolajski C, Miller E, McCauley HL, Akers A, Schwarz EB, Freedman L, Steinberg J, Ibrahim S, & Borrero S (2015). Race and Reproductive Coercion: A Qualitative Assessment. Women’s Health Issues, 25(3), 216–223. https://doi.org/S1049-3867(14)00153-4 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northridge JL, Silver EJ, Talib HJ, & Coupey SM (2017). Reproductive Coercion in High School-Aged Girls: Associations with Reproductive Health Risk and Intimate Partner Violence. Journal of Pediatric and Adolescent Gynecology, 30(6), 603–608. 10.1016/j.jpag.2017.06.007 [DOI] [PubMed] [Google Scholar]
- Paterno MT, Draughon Moret JE, Paskausky A, & Campbell JC (2018). Exploring Reproductive Coercion in Relationship Contexts Among Young Adult, Primarily African American Women at Three Women’s Health Clinics. Journal of Interpersonal Violence, 1–24. 10.1177/0886260518756116 [DOI] [PubMed] [Google Scholar]
- Paterno MT, Hayat MJ, Wenzel J, & Campbell JC (2017). A Mixed Methods Study of Contraceptive Effectiveness in a Relationship Context Among Young Adult, Primarily Low-Income African American Women. Journal of Racial and Ethnic Health Disparities, 4(2), 184–194. 10.1007/s40615-016-0217-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitts KM (2014). Latina immigrants, interpersonal violence, and the decision to report to police. Journal of Interpersonal Violence, 29(9), 1661–1678. 10.1177/0886260513511700 [DOI] [PubMed] [Google Scholar]
- Reina AS, Lohman BJ, & Maldonado MM (2014). “He said they’d deport me”: factors influencing domestic violence help-seeking practices among Latina immigrants. Journal of Interpersonal Violence, 29(4), 593–615. 10.1177/0886260513505214 [DOI] [PubMed] [Google Scholar]
- Rocca CH, Doherty I, Padian NS, Hubbard AE, & Minnis AM (2010). Pregnancy Intentions and Teenage Pregnancy Among Latinas: A Mediation Analysis. Perspectives on Sexual and Reproductive Health, 42(3), 186–196. 10.1363/4218610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocca CH, Wilson MR, Jeon M, & Foster DG (2019). Stability of Retrospective Pregnancy Intention Reporting Among Women with Unwanted Pregnancies in the United States. Maternal and Child Health Journal, 0123456789. 10.1007/s10995-019-02782-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncancio AM, Ward KK, & Berenson AB (2012). The Use of Effective Contraception among Young Hispanic Women: The Role of Acculturation. Journal of Pediatric and Adolescent Gynecology, 25(1), 35–38. 10.1016/j.jpag.2011.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum JE, Zenilman J, Rose E, Wingood G, & DiClemente R (2016). Predicting Unprotected Sex and Unplanned Pregnancy among Urban African-American Adolescent Girls Using the Theory of Gender and Power. Journal of Urban Health, 93(3), 493–510. 10.1007/s11524-016-0047-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfeld EA, Miller E, Zhao X, Sileanu FE, Mor MK, & Borrero S (2017). Male partner reproductive coercion among women veterans. American Journal of Obstetrics and Gynecology, 218(2), 1–8. 10.1016/j.ajog.2017.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santelli JS, Lindberg LD, Orr MG, Finer LB, & Speizer IS (2009). Toward a multidimensional measure of pregnancy intentions: evidence from the United States. Studies in Family Planning, 40(2), 87–100. [DOI] [PubMed] [Google Scholar]
- Sohal H, Eldridge S, & Feder G (2007). The sensitivity and specificity of four questions (HARK) to identify intimate partner violence: a diagnostic accuracy study in general practice. BMC Family Practice, 8(1), 49. 10.1186/1471-2296-8-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland MA, Fantasia HC, & Fontenot H (2015). Reproductive Coercion and Partner Violence among College Women. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 44(2), 218–227. 10.1111/1552-6909.12550 [doi] [DOI] [PubMed] [Google Scholar]
- Tancredi DJ, Silverman JG, Decker MR, McCauley HL, Anderson HA, Jones KA, Ciaravino S, Hicks A, Raible C, Zelazny S, James L, & Miller E (2015). Cluster randomized controlled trial protocol: Addressing reproductive coercion in health settings (ARCHES). BMC Women’s Health, 15(1), 57. 10.1186/s12905-015-0216-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiel de Bocanegra H, Rostovtseva DP, Khera S, & Godhwani N (2010). Birth control sabotage and forced sex: experiences reported by women in domestic violence shelters. Violence Against Women, 16(5), 601–612. 10.1177/1077801210366965 [DOI] [PubMed] [Google Scholar]
- Tsui AO, Casterline J, Singh S, Bankole A, Moore AM, Omideyi AK, Palomino N, Sathar Z, Juarez F, & Shellenberg KM (2011). Managing unplanned pregnancies in five countries: perspectives on contraception and abortion decisions. Global Public Health, 6 Suppl 1(May 2015), S1–S24. 10.1080/17441692.2011.597413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upadhyay UD, Dworkin SL, Weitz TA, & Foster DG (2014). Development and validation of a reproductive autonomy scale. Studies in Family Planning, 45(1), 19–41. 10.1111/j.1728-4465.2014.00374.x [DOI] [PubMed] [Google Scholar]
- Urquia ML, O’Campo PJ, & Heaman MI (2012). Revisiting the immigrant paradox in reproductive health: the roles of duration of residence and ethnicity. Social Science & Medicine (1982), 74(10), 1610–1621. 10.1016/j.socscimed.2012.02.013 [DOI] [PubMed] [Google Scholar]
- Wallenborn JT, Chambers G, Lowery EP, & Masho SW (2018). Discordance in Couples Pregnancy Intentions and Breastfeeding Duration : Results from the National Survey of Family Growth 2011 – 2013. Journal of Pregnancy, 2018, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willie TC, Powell A, Callands T, Sipsma H, Peasant C, Magriples U, Alexander K, & Kershaw T (2019). Investigating intimate partner violence victimization and reproductive coercion victimization among young pregnant and parenting couples: A longitudinal study. Psychology of Violence, 9(3), 278–287. 10.1037/vio0000118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RL, Fawson PR, Siegel E, Jones T, & Stone K (2018). Predictors of Reproductive Autonomy among a Rural University Population. Health & Social Work, 43(4), 235–242. 10.1093/hsw/hly027 [DOI] [PubMed] [Google Scholar]
- Yudko E, Lozhkina O, & Fouts A (2007). A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. Journal of Substance Abuse Treatment, 32(2), 189–198. 10.1016/j.jsat.2006.08.002 [DOI] [PubMed] [Google Scholar]


