Abstract
PURPOSE
The COVID-19 pandemic has placed unprecedented demands on the health system. This led to delays in the initiation and completion of cancer treatment. We assessed the long-term health consequences because of the delay in diagnosis and treatment for cervical cancer due to COVID-19 in India.
METHODS
We used a Markov-model–based analysis assessing the lifetime health outcomes of the cohort of women population at risk from cervical cancer in India. The decrease in survival for those with the treatment interruption was calculated based on the number of days the treatment was extended beyond the standard duration. Furthermore, to model the impact of late diagnosis and delayed treatment initiation, the patients were assumed to have upstaged during the delay period, as per natural progression of disease.
RESULTS
We estimate 2.52% (n = 795) to 3.80% (n = 2,160) lifetime increase in the deaths caused by cervical cancer with treatment restrictions ranging from 9 weeks to 6 months, respectively, as compared to no delay. On the contrary, 88-238 deaths because of COVID-19 disease are estimated to be saved during this restriction period among the patients with cervical cancer. Overall, the excess mortality because of cervical cancer led to 18,159-53,626 life-years being lost and an increase of 16,808-50,035 disability-adjusted life-years.
CONCLUSION
Delays in diagnosis and treatment are likely to lead to more cervical cancer deaths as compared to COVID-19 mortality averted among the patients with cervical cancer. Health systems must reorganize in terms of priority setting for provision of care, starting with prioritizing the treatment of patients with early-stage cervical cancer, increasing use of teleconsultation, and strengthening the role of primary care physicians in provision of cancer care.
INTRODUCTION
The emergence of the COVID-19 pandemic has led to the disruption in the accessibility to treatment and care for non–COVID-19 health conditions.1,2 Physical containment along with travel restrictions and reduction in the public transport facilities (including roadways, railways, and airways) has posed difficulties for patients in visiting the hospitals for treatment.3-6 Second, fear of contracting the COVID-19 in health facilities, as well as financial issues faced by the poor strata, especially for those coming from far off places, further deterred patients from accessing care.7 Furthermore, most of the hospitals have also become selective in offering elective procedures and prioritizing essential procedures while deferring some nonessential services.8,9 These have led to substantial delays in the initiation and completion of treatment for various non–COVID-19 health conditions.
CONTEXT
Key Objective
To predict the extent of excess cervical cancer deaths caused as a result of COVID-19 in India.
Knowledge Generated
This study estimates that the excess lifetime cervical cancer deaths, because of delay in diagnosis and treatment, are estimated to be higher than the COVID-19 deaths averted among cervical cancer patients.
Relevance
Clinical care pathways would need to be evolved such that the treatment for cancer continues unabated with proper COVID-19 protocols.
The pandemic had significantly affected the patients accessing services from regional cancer centers across India in view of the COVID-19 restrictions. Nearly 60%-70% decline in the attendance of patients with cancer was reported from different parts of the country. The diagnosis of new cancer cases was also delayed because of nonavailability of diagnostic services as well as suspension of population-based screening programs.7-9 Furthermore, ongoing treatment, whether radiotherapy, chemotherapy, or surgery, were replanned or deferred.7-9 Evidence suggests that duration from diagnosis to initiation of cancer treatment and its timely completion affect both treatment efficacy and survival.10-13 Specifically, studies on cervical cancer have shown reduction in survival when the recommended overall treatment duration gets prolonged or when there is delay from diagnosis to treatment.13-18
In light of the global WHO commitment to eradicate cervical cancer, this holds particular significance. It is the third most prevalent cancer (second most prevalent among women) both in the South East Asia region and India.19 It is estimated that around 97,000 cases of cervical cancer are diagnosed and 60,000 deaths are reported each year.20 Considering the high burden of this cancer, and no previous evidence from India, we estimated the long-term health consequences, that is, mortality and disability-adjusted life-years (DALY) because of the treatment interruptions and delay, as well as late diagnosis for cervical cancer because of COVID-19 in India. We present the estimates assuming treatment delays of various durations, that is, 9 weeks, 12 weeks, and 6 months.
METHODS
We used a Markov-model–based analysis for assessing the lifetime health outcomes in a cohort of women population at risk from cervical cancer because of the treatment delay of 9 weeks, 12 weeks, and 6 months, compared with the routine scenario of no-delay in India. In addition, mortality because of COVID-19 infection among these patients with cervical cancer both during with and without treatment restrictions was also assessed. The health outcomes were measured in terms of mortality and DALYs among the patients with cervical cancer.
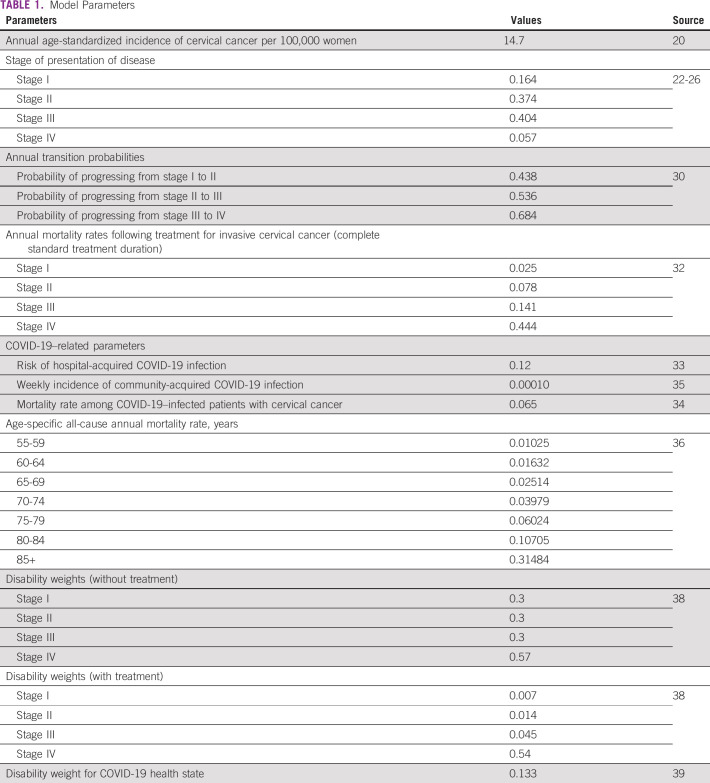
Model Overview
The model structure is divided into two arms as shown in Figure 1. The first arm captures the health impact on those cervical cancer cases that were diagnosed before the onset of the COVID-19 restrictions in the country and were either not able to complete the treatment or there was delay in the initiation of treatment. The interruption in continuation of treatment or delay in the start of treatment was assumed till the COVID-19 restrictions eased out, after which the treatment was immediately resumed and continued till completion. Any treatment given to the patient before the onset of the COVID-19 restrictions was accounted for in the management of the disease, subsequently. So, whatever radiation or chemotherapy dose was delivered before the treatment interruption, the treatment given at the later stage was assumed to be adjusted in light of previous treatment.
FIG 1.
Markov model.
In the second arm, the model captures the health impact of those new incident cancer cases that were ideally supposed to be diagnosed in the absence of COVID-19 restrictions, but were not detected and were thus assumed to have progressed and upstaged during the delay period. These patients were assumed to be finally diagnosed after the COVID-19 restrictions eased out and patients were put on standard treatment regimen based on their final upgraded stage. Finally, in the control scenario of no restrictions, incident cancer cases were assumed to get diagnosis and standard treatment based on current (pre-COVID-19) stage at diagnosis and treatment practices.21 Patients in both the arms were assumed to die both from cervical cancer as well as age-specific mortality from causes other than cervical cancer. Those with treatment interruptions beyond the standard duration were assumed to have lower survival rates as compared to the similar-stage patients who completed the treatment in the standard duration.14-16 Furthermore, patients who were not diagnosed timely during the COVID-19 period were assumed to have progressed as per natural progression. Subsequently, once detected after COVID-19 restrictions eased, progression and survival rates of the respective upgraded stage in which they were diagnosed were applied. The present model also assessed the impact of the developing COVID-19 disease among the incident cervical cancer patients both during with and without COVID-19 restrictions. In the control scenario of no restrictions, where all the patients with cancer were assumed to have access to the cancer care, the model assumed a risk of contracting hospital-acquired COVID-19 infection during the time of hospital stay or treatment regimen and subsequent mortality (because of the infection) among the patients with cancer. Similarly, during the restriction period, those patients with cancer who were not able to access the treatment facilities were also assumed to be at risk of getting infected with COVID-19 disease based on the community-acquired incidence rate. The mortality because of the infection among both community-acquired and hospital-acquired COVID-19 was assumed to be the same.
The management of the cervical cancer was based on the national standard treatment guidelines as recommended by Indian Council of Medical Research.21 The standard treatment for patients with locally advanced cervical cancer (stage IB2, IIA2, IIB, and III) consists of a combination of external-beam radiotherapy and concomitant weekly chemotherapy, which is followed by brachytherapy. The ideal duration for completion of this treatment is 8 weeks.21 Patients in stage IA, IB1, and IIA1 may undergo surgery alone or in combination with adjuvant radiotherapy or chemoradiotherapy or brachytherapy based on the postoperative findings.
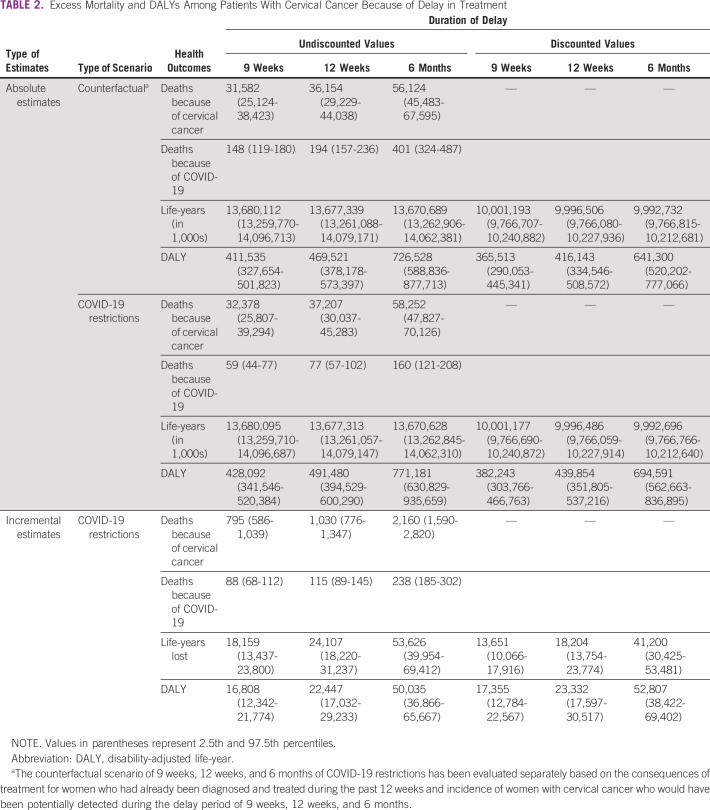
Based on the duration of treatment modalities, the model was assumed to start from 12 weeks before the onset of COVID-19 restrictions, so as to fully capture the impact of treatment interruption or delay on those patients (first arm of the model) diagnosed before the start of COVID-19 restrictions, as shown in Figure 2. Considering the standard duration of radiotherapy or chemoradiotherapy (with brachytherapy) as 8 weeks (or 56 days), the treatment regimen of those patients (requiring radiotherapy or chemoradiotherapy or brachytherapy) diagnosed in the 8 weeks before the COVID-19 restrictions was assumed to be interrupted and postponed till the COVID-19 restrictions eased out. Furthermore, based on the expert opinion that the average waiting time for surgery in India is 4 weeks, it was expected that patients requiring surgery had to be diagnosed before the 4 weeks of the COVID-19 restrictions to successfully undergo the surgical procedure. Considering this, the treatment comprising surgery alone or in combination with radiotherapy or chemoradiotherapy or brachytherapy of those patients diagnosed in the 4 weeks before COVID-19 restrictions was assumed to be delayed, and the disease was presumed to have progressed and upstaged during the delay period. Finally, the radiotherapy or chemoradiotherapy or brachytherapy need of those postoperative cases operated in the time frames A and B, that is, 5-12 weeks before COVID-19 restrictions (Fig 2), was assumed to be interrupted till the restrictions eased down. Based on the data from various oncology centers in India that reported around 60%-70% decrease in the patients with cancer visiting these centers during the onset of COVID-19 restrictions, it was assumed that around 40% of the patients during the treatment interruption period were diagnosed timely and completed the total treatment schedule without any interruption during this period and also had a risk of contracting hospital-acquired COVID-19 disease.
FIG 2.
Pattern of treatment interruption of patients diagnosed with cervical cancer at different time frames before the onset of COVID-19 restrictions.
The model starts with the total susceptible cohort of Indian women population and reported age-standardized weekly incidence rate of the invasive cancer.20 The incident cases were assumed to get diagnosed in the different stages of the cancer based on the stage-specific presentation of the disease.22-26 It was further assumed that model starts at an age of 57 years, considered to be the average age at diagnosis for cervical cancer in India.27 The cycle length of the Markov model was considered weekly for the first year, followed by annual life cycles till lifetime of the cohort. Following infection with COVID-19 disease, infected patients with cancer were either assumed to return back to COVID-19–free state or die from the infection in the third week after diagnosis.28,29 The counterfactual scenario for each of the 9-week, 12-week, and 6-month delay scenario was evaluated separately based on the consequences of treatment for women who had already been diagnosed and treated during the past 12 weeks and those women with cervical cancer who would have been potentially detected during the delay period of 9 weeks, 12 weeks, and 6 months.
Model Parameters
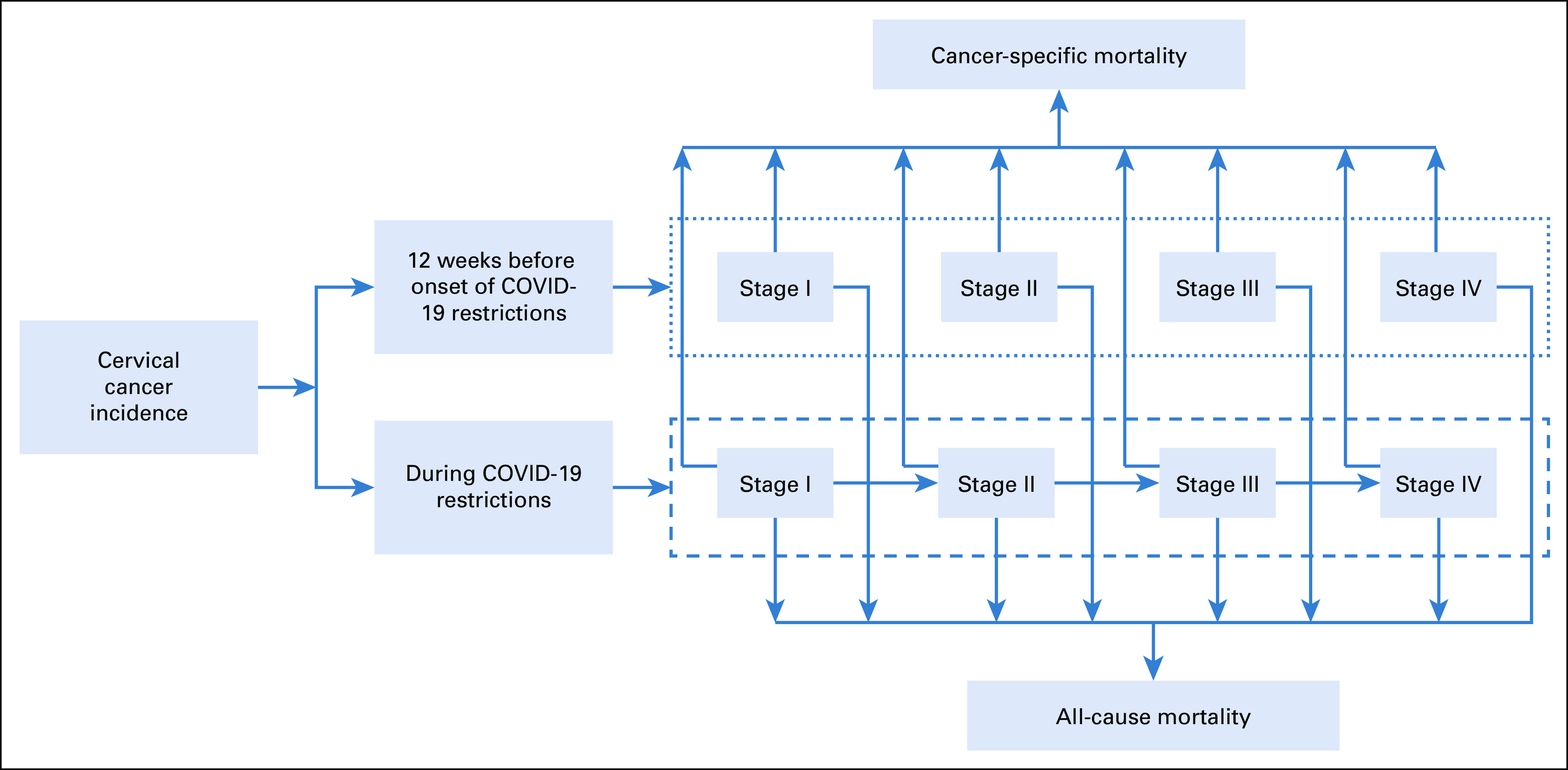
We used the age-standardized incidence rate of 14.7 per 100,000 women for cervical cancer, based on the recent report of the International Agency for Research on Cancer for India.20 Stage-specific presentation of the cervical cancer was based on the pooled estimate derived from the data on the stage of diagnosis for cervical cancer available from various hospital-based registries across India, as shown in Table 1.22-26 Transition probabilities of progressing from a stage of the cancer to higher advanced stage were based on the mathematical model on the natural history of human papillomavirus infection and cervical cancer,30 which has also been used in a recently completed health technology report on cervical cancer screening in India.31
TABLE 1.
Model Parameters
Stage-specific mortality rates (for those with uninterrupted treatment) were based on the stage-specific survival data from an Indian randomized control trial in which patients were followed up to 14 years.32 The decrease in survival for those with the treatment interruption (for patients in the first arm) was calculated based on the number of days the treatment was extended beyond the standard duration.14-16 A decrease in survival of 0.6% was considered per each additional day of treatment interruption among patients treated with radiotherapy or chemoradiotherapy and brachytherapy for stages I-III of the invasive cancer.16 Based on a study that reported a nonsignificant decrease in survival because of treatment interruption in advanced stages of disease, the survival rate for stage IVA patients was assumed to be similar to those who completed the treatment in the standard duration.17 The risk of hospital-acquired COVID-19 disease was assessed from a recently undertaken systemic review.33 Weekly incidence of community-acquired COVID-19 infection was based on the actual number of reported COVID-19 infections in India.34 Furthermore, the mortality rate among the COVID-19–infected patients with cervical cancer was deduced from an observational study on patients with active cancer as well as COVID-19 disease undertaken in a tertiary care hospital from India.35
The probability of dying from causes other than cervical cancer was obtained from age-specific all-cause mortality rate as available from the Census of India Sample Registration System life tables for the female population.36 Standard methods were used for estimating DALY.37 Disability weights separately for those treated and untreated cervical cancer were drawn from a previous WHO-CHOICE study.38 As no specific disability weight was available for COVID-19 health state, the disability weight of 0.133 for lower respiratory tract infection was used.39 Furthermore, for deriving a disability weight for the health condition combining two health states of active cancer (treated or untreated) and COVID-19 disease, we assumed to use a worse (or higher) disability weight among the two health states. We estimated both the undiscounted and discounted health outcomes. A discount rate of 3% was used for discounting future health consequences. Ethical approval for this study was obtained from the Institute Ethics Committee of the Post Graduate Institute of Medical Education and Research, Chandigarh, India.
Sensitivity Analysis
A probabilistic sensitivity analysis was undertaken to test the uncertainty in parameter values.40 All the input parameters were varied by 20% on either side of the base value. A median value of the outcome along with 2.5th and 97.5th percentiles was computed using 999 Monte Carlo simulations. Furthermore, a univariate sensitivity analysis was carried out to assess the change in mortality with variation in the proportion of patients with cancer having accessibility to treatment during the COVID-19 restrictions.
RESULTS
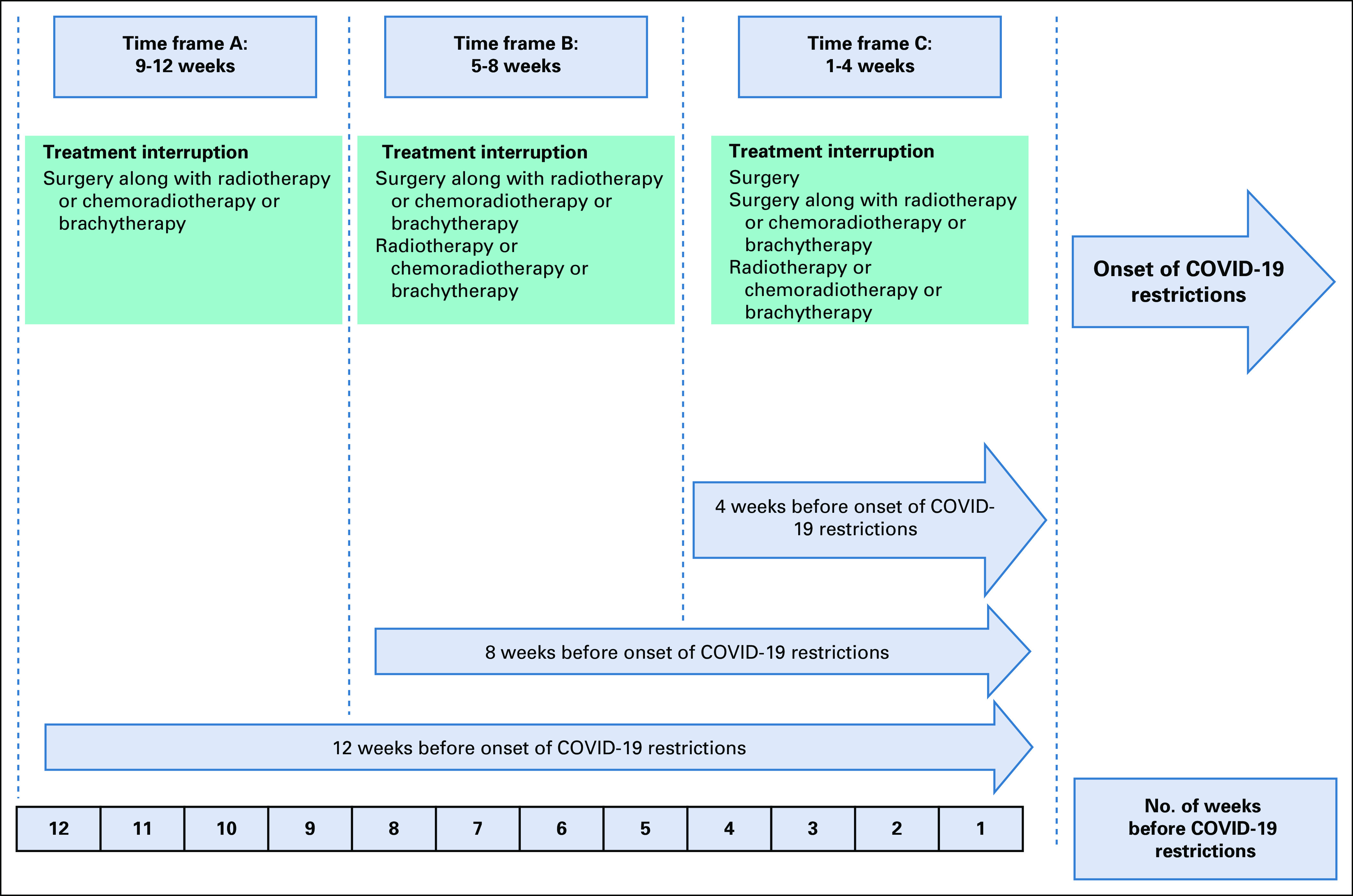
Over the lifetime of the cohort, we estimated an excess of cervical cancer deaths ranging from 795 (2.52%) to 2,160 (3.80%), with the delay period ranging from 9 weeks to 6 months, respectively, as compared to the scenario of no-delay (Table 2). On the contrary, 88, 115, and 238 deaths because of COVID-19 disease are estimated to be saved because of restriction period of 9 weeks, 12 weeks, and 6 months, respectively, among the patients with cervical cancer. Overall, the excess mortality because of cervical cancer are estimated to lead to 18,159-53,626 life-years (undiscounted) being lost and an increase of 16,808-50,035 DALYs (undiscounted). The patients diagnosed in stage I and II of cervical cancer contribute to nearly 68%-77% of these life-years lost, because of delay of 9 weeks to 6 months, respectively.
TABLE 2.
Excess Mortality and DALYs Among Patients With Cervical Cancer Because of Delay in Treatment
If the access to cervical cancer treatment declines to 20% as a result of COVID-19 restrictions, excess mortality because of cervical cancer would increase by a factor of 3.2%-4.97% and deaths saved from COVID-19 would increase to 119-321. By contrast, by increasing the proportion of patients who have access to treatment to 60%, the excess cervical cancer deaths would decrease by 1.74%-2.63% and mortality averted from COVID-19 would decrease to 59-160 deaths.
DISCUSSION
Various COVID-19 restrictions placed to enforce physical space distancing led to difficulty in accessing the specialist services at the regional cancer centers.1,2 Our analysis was undertaken to estimate the health impact on patients with cervical cancer because of a delay in the diagnosis and treatment caused by COVID-19 restrictions in India. It was estimated that delay in diagnoses and treatment due to COVID-19 is likely to lead to more cervical cancer deaths (because of treatment delay and interruption) than the deaths as a result of COVID-19 averted among the patients with cervical cancer. Overall, women in India are estimated to experience between 18,159-53,626 years of life lost, and 16,808-50,035 excess DALYs because of excess cervical cancer mortality during the period of strict COVID-19 restrictions in the country.
The increased mortality because of cervical cancer, as predicted by the present analysis, is actually a very small proportion of the total negative externality on non–COVID-19 conditions. The COVID-19 pandemic has created serious problems for patients suffering from many other health conditions such as other cancers, tuberculosis, maternity and child health care, heart and kidney disorders, and other infectious diseases that need timely and frequent medical care. A study from India had predicted a 5.7%-19.3% increase in deaths because of tuberculosis depending upon the delay in management.41 Likewise, another study found that a 10% decline in service coverage of essential pregnancy-related and newborn care services because of COVID-19 restrictions would lead to 0.03 million additional maternal deaths and 1.7 million additional newborn deaths in India.42 Furthermore, as per data, 69% reduction in the coverage of measles, mumps, and rubella vaccination in India during the strict COVID-19 restriction period had increased the risk of children being infected from infectious diseases.2 There was also a 50% reduction in clinic attendance for acute cardiac events and a 32% fall in inpatient care for pulmonary conditions.2
Policymakers need to carefully understand and comprehensively evaluate the negative effect of nonpharmaceutical interventions such as stringent physical space distancing and reallocation of the health system resources for the management of COVID-19 on the non–COVID-19 health conditions. While on one hand public health experts are promoting physical space distancing, on the other hand, there is also an opinion on ensuring continuous access to routine care for non–COVID-19 ailments. During the 2014-2016 Ebola epidemic, the deaths caused by other endemic diseases, that is, measles, malaria, HIV/AIDS, and tuberculosis, were higher than the morality caused by Ebola itself.43,44 This study also depicts similar results, wherein excess cervical cancer deaths are far more than COVID-19 deaths averted because of the restrictions in the country. Despite the fear and impact of the COVID-19 pandemic, one needs to ensure that these pandemic control measures do not lead to even greater indirect mortality and morbidity. Although we believe that imposition of some form of movement control might be necessary for controlling the spread of COVID-19 infection, the health system should not completely assign itself in containing COVID-19, but it should also restructure itself in such a way that it simultaneously keeps on providing health care and necessary treatment to those with immediate need of it. Thus, the health systems should consider approaches that involve balancing the current pandemic and providing continuous health care to non-COVID conditions.
Cervical cancer is one of the rapidly proliferating tumors where treatment interruption during radiation leads to accelerated tumor proliferation. A combination of chemoradiation and brachytherapy should be ideally completed in the time span of 8 weeks.17,45 It has been reported from various studies that pelvic control decreases by 0.7%-1% per day and overall survival by 0.6%-0.8% per day for each additional day of radiotherapy treatment interruption beyond the standard 56 days, specifically for early stages of disease.14-17 While providing care, measures could be undertaken in individual departments to ensure compliance to nonsurgical (chemoradiotherapy or radiotherapy or brachytherapy) treatment for cervical cancer.46
In view of COVID-19 crisis, many cancer hospitals were converted to COVID-19 care centers or their personnel were under quarantine or under compulsory rotation as per the advisory issued.8 To continue to provide care to the patients with cancer, the oncology departments need to reorganize themselves to simultaneously preserve the medical resources for COVID-19 management and safeguard the health care workers involved in providing the oncology services.8 While treating patients based on equity principles, a first served may be relevant in business as usual. However, maximization of health benefits to save most life and save most life-years would receive highest priority in a pandemic situation.47,48 Thus, those with possible curable disease, where a substantial benefit from the treatment is possible, should be given priority. We found that around 68%-77% of the total loss in life-years during the COVID-19 restrictions was because of the inaccessibility of treatment for patients with early stage of disease (stage I and II). This is because the treatment interruption has a nonsignificant impact on survival in the advanced stages of the disease. Hence, priority should be given to these early-stage patients. In view of the ongoing COVID-19 crisis, elective surgeries also had taken a backseat.8,9 Life-years lost because of delay in surgeries of early-stage patients can be avoided if patients with early-stage cervical cancer are shifted from surgery to definitive radiation, in view of equivalent survival results with both modalities.
Furthermore, to prevent the loss of life-years because of delay in diagnosis of incident cases, the primary care physicians can be a great help. Through teleconferencing with regional cancer centers, primary physicians can be involved to do the basic staging and diagnostic workup including biopsy, hematology, biochemistry, and diagnostic radiology. This can help in starting the treatment upfront when the patient reaches the regional oncology center without further delay.
In conclusion, our study gives an overall model-based estimation of the impact of COVID-19–related restrictions on the health outcomes of patients with cervical cancer in India. The study concludes that COVID-19 restrictions led to more cervical cancer deaths as compared to COVID-19 mortality averted among the patients with cervical cancer. Considering that cervical cancer contributes 0.76% of total disease burden, overall negative health consequences of delay in management are likely to be much greater.49 Health systems must reorganize in terms of priority setting for provision of care, improving the referral pathways, increasing use of teleconsultation, and strengthening the role of primary care physicians in provision of cancer and general health care.
Nidhi Gupta
Employment: Grecian Multispeciality Hospital, Mohali, Punjab, India
No other potential conflicts of interest were reported.
AUTHOR CONTRIBUTIONS
Conception and design: Nidhi Gupta, Shankar Prinja, Awadhesh Kumar Pandey
Collection and assembly of data: Nidhi Gupta, Akashdeep Singh Chauhan, Shankar Prinja
Data analysis and interpretation: Nidhi Gupta, Akashdeep Singh Chauhan, Shankar Prinja
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by the authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Nidhi Gupta
Employment: Grecian Multispeciality Hospital, Mohali, Punjab, India
No other potential conflicts of interest were reported.
REFERENCES
- 1.The Lancet India under COVID-19 lockdown. Lancet. 2020;395:1315. doi: 10.1016/S0140-6736(20)30938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cash R, Patel V.Has COVID-19 subverted global health? Lancet 3951687–16882020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Press Information Bureau, Government of India PM calls for complete lockdown of entire nation for 21 days. https://pib.gov.in/PressReleseDetail.aspx?PRID=1608009
- 4.Press Information Bureau, Government of India PM addresses the nation for 4th time in 4 weeks in India's fight against COVID-19 and announces extension of lockdown till 3rd May. https://pib.gov.in/PressReleseDetail.aspx?PRID=1614255
- 5.Press Information Bureau, Government of India Extension of lockdown for a further period of two weeks with effect from May 4, 2020. https://pib.gov.in/PressReleasePage.aspx?PRID=1620095
- 6.Press Information Bureau, Government of India Extension of lockdown up to May 31, 2020. https://pib.gov.in/PressReleasePage.aspx?PRID=1624763
- 7.Kumar D, Dey T. Treatment delays in oncology patients during COVID-19 pandemic: A perspective. J Glob Health. 2020;10:010367. doi: 10.7189/jogh.10.010367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pramesh CS, Badwe RA. Cancer management in India during Covid-19. N Engl J Med. 2020;382:e61. doi: 10.1056/NEJMc2011595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Lancet Oncology COVID-19: Global consequences for oncology. Lancet Oncol. 2020;21:467. doi: 10.1016/S1470-2045(20)30175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caplan L. Delay in breast cancer: Implications for stage at diagnosis and survival. Front Public Health. 2014;2:87. doi: 10.3389/fpubh.2014.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGee SA, Durham DD, Tse CK, et al. Determinants of breast cancer treatment delay differ for African American and White women Cancer Epidemiol Biomarkers Prev 221227–12382013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diaconescu R, Lafond C, Whittom R.Treatment delays in non-small cell lung cancer and their prognostic implications J Thorac Oncol 61254–12592011 [DOI] [PubMed] [Google Scholar]
- 13.Chen CP, Kung PT, Wang YH, et al. Effect of time interval from diagnosis to treatment for cervical cancer on survival: A nationwide cohort study. PLoS One. 2019;14:e0221946. doi: 10.1371/journal.pone.0221946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Girinsky T, Rey A, Roche B, et al. Overall treatment time in advanced cervical carcinomas: A critical parameter in treatment outcome Int J Radiat Oncol Biol Phys 271051–10561993 [DOI] [PubMed] [Google Scholar]
- 15.Perez CA, Grigsby PW, Castro-Vita H, et al. Carcinoma of the uterine cervix. I. Impact of prolongation of overall treatment time and timing of brachytherapy on outcome of radiation therapy Int J Radiat Oncol Biol Phys 321275–12881995 [DOI] [PubMed] [Google Scholar]
- 16.Petereit DG, Sarkaria JN, Chappell R, et al. The adverse effect of treatment prolongation in cervical carcinoma Int J Radiat Oncol Biol Phys 321301–13071995 [DOI] [PubMed] [Google Scholar]
- 17.Lin SM, Ku HY, Chang TC, et al. The prognostic impact of overall treatment time on disease outcome in uterine cervical cancer patients treated primarily with concomitant chemoradiotherapy: A nationwide Taiwanese cohort study Oncotarget 885203–852132017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krusun S, Pesee M, Supakalin N, et al. Treatment interruption during concurrent chemoradiotherapy of uterine cervical cancer; analysis of factors and outcomes Asian Pac J Cancer Prev 155653–56572014 [DOI] [PubMed] [Google Scholar]
- 19.Global Cancer Observatory, International Agency for Research in Cancer, World Health Organization Estimated number of new cases in 2018, WHO South-East Asia region (SEARO) and India, females, all ages. https://gco.iarc.fr/today/online-analysis-table
- 20.Bruni L, Albero G, Serrano B, et al. Human Papillomavirus and Related Diseases in India: Summary Report 17. ICO/IARC Information Centre on HPV and Cancer. https://hpvcentre.net/statistics/reports/IND.pdf.
- 21.Indian Council of Medical Research Consensus document for management of cancer cervix. https://main.icmr.nic.in/sites/default/files/reports/Cervix%20Cancer.pdf
- 22.Jain A, Ganesh B, Bobdey SC, et al. Sociodemographic and clinical profile of cervical cancer patients visiting in a tertiary care hospital in India Indian J Med Paediatr Oncol 38291–2952017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumari A, Pankaj S, Choudhary V, et al. Retrospective analysis of patients of cervical cancer a tertiary center in Bihar Indian J Cancer 5570–732018 [DOI] [PubMed] [Google Scholar]
- 24.Kataki AC, Sharma JD, Krishnatreya M, et al. A survival study of uterine cervical patients in the North East India: Hospital-cancer registry-based analysis J Cancer Res Ther 141089–10932018 [DOI] [PubMed] [Google Scholar]
- 25.Gupta S, Rastogi K, Bhatnagar AR, et al. Compliance to radiotherapy: A tertiary care center experience Indian J Cancer 55166–1692018 [DOI] [PubMed] [Google Scholar]
- 26.Rajaram S, Bhaskaran S, Sinha S, et al. Role of hospital-based cancer registries: A decade of experience of cancer cervix from a tertiary care centre, India Indian J Community Med 39241–2442014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sreedevi A, Javed R, Dinesh A.Epidemiology of cervical cancer with special focus on India Int J Womens Health 7405–4142015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organisation Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) World Health Organisation; 2020, pp 40.https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf [Google Scholar]
- 29.15 Days between diagnosis and death for Covid patients in India, fatality data shows. The Print. 2020 https://theprint.in/health/15-days-between-diagnosis-and-death-for-covid-patients-in-india-fatality-data-shows/473935/ [Google Scholar]
- 30.Myers ER, McCrory DC, Nanda K, et al. Mathematical model for the natural history of human papillomavirus infection and cervical carcinogenesis Am J Epidemiol 1511158–11712000 [DOI] [PubMed] [Google Scholar]
- 31.Chauhan AS, Prinja S, Srinivasan R, et al. Cost effectiveness of strategies for cervical cancer prevention in India. PLoS One. 2020;15:e0238291. doi: 10.1371/journal.pone.0238291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jayant K, Sankaranarayanan R, Thorat RV, et al. Improved survival of cervical cancer patients in a screened population in rural India Asian Pac J Cancer Prev 174837–48442016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barranco R, Vallega Bernucci Du Tremoul L, Ventura F. Hospital-acquired SARS-Cov-2 infections in patients: Inevitable conditions or medical malpractice? Int J Environ Res Public Health. 2021;18:489. doi: 10.3390/ijerph18020489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jain VK, Iyengar K, Vaish A, et al. Differential mortality in COVID-19 patients from India and western countries Diabetes Metab Syndr 141037–10412020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramaswamy A, Nayak L, Roy Moulik N, et al. COVID-19 in cancer patients on active systemic therapy—Outcomes from LMIC scenario with an emphasis on need for active treatment Cancer Med 98747–87532020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Registrar General & Census Commissioner of India SRS based abridges life tables 2013-17. http://censusindia.gov.in/Vital_Statistics/SRS_Life_Table/SRS%20based%20Abridged%20Life%20Tables%202013-17.pdf
- 37.Fox-Rushby JA, Hanson K.Calculating and presenting disability adjusted life years (DALYs) in cost-effectiveness analysis Health Policy Plan 16326–3312001 [DOI] [PubMed] [Google Scholar]
- 38.Ralaidovy AH, Gopalappa C, Ilbawi A, et al. Cost-effective interventions for breast cancer, cervical cancer, and colorectal cancer: New results from WHO-CHOICE. Cost Eff Resour Alloc. 2018;16:38. doi: 10.1186/s12962-018-0157-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nurchis MC, Pascucci D, Sapienza M, et al. Impact of the burden of COVID-19 in Italy: Results of disability-adjusted life years (DALYs) and productivity loss. Int J Environ Res Public Health. 2020;17:4233. doi: 10.3390/ijerph17124233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doubilet P, Begg CB, Weinstein MC, et al. Probabilistic sensitivity analysis using Monte Carlo simulation. A practical approach Med Decis Making 5157–1771985 [DOI] [PubMed] [Google Scholar]
- 41.Stop TB Partnership The potential impact of the COVID-19 response on tuberculosis in high-burden countries: A modelling analysis. 2020 http://www.stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf
- 42.Riley T, Sully E, Ahmed Z, et al. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low- and middle-income countries Int Perspect Sex Reprod Health 4673–762020 [DOI] [PubMed] [Google Scholar]
- 43.Parpia AS, Ndeffo-Mbah ML, Wenzel NS, et al. Effects of response to 2014-2015 Ebola outbreak on deaths from malaria, HIV/AIDS, and tuberculosis, West Africa Emerg Infect Dis 22433–4412016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brolin Ribacke KJ, Saulnier DD, Eriksson A, et al. Effects of the West Africa Ebola virus disease on health-care utilization—A systematic review. Front Public Health. 2016;4:222. doi: 10.3389/fpubh.2016.00222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nag S, Erickson B, Thomadsen B, et al. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix Int J Radiat Oncol Biol Phys 48201–2112000 [DOI] [PubMed] [Google Scholar]
- 46.Miriyala R, Mahanthsetty U.Cervical cancer radiotherapy with emphasis on brachytherapy and COVID-19 pandemic crisis: Problems and prospects! J Contemp Brachytheraphy 12290–2932020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Prinja S, Pandav CS.Economics of COVID-19 pandemic: Challenges and the way forward for health policy during and after the pandemic Indian J Public Health 64S231–S2332020suppl [DOI] [PubMed] [Google Scholar]
- 48.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19 N Engl J Med 3822049–20552020 [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization Disease burden and mortality estimates, Cuse Specific Mortality, 2000-2016. https://www.who.int/healthinfo/global_burden_disease/estimates/en/