Abstract
PURPOSE
Lung cancer is a global health problem, with more than 220,000 new cases and 150,000 deaths per year in the United States. Likewise, in Brazil, lung cancer is the most lethal cancer with 30,200 new cases expected in 2020. Regarding treatment types, radiation therapy (RT) represents an important approach, since 60%-70% of the patients will receive this modality of treatment during the course of their disease. However, access to RT remains challenging because of the socioeconomic inequalities in the Brazilian population, where approximately 100,000 patients/year die without access to RT. This work provides an overview on the availability of high technology RT in Brazil.
METHODS
A retrospective study was performed using the Brazilian Radiotherapy Census, local public and private databases, and the current literature published in 2019.
RESULTS
The Brazilian radiotherapy network relies on approximately 363 linear accelerators and 20 cobalt machines that remain operational. Most of these machines are installed at public health facilities. Regarding high technology, intensity-modulated RT is available in 53.7% (n = 130) and volumetric modulated arc therapy in 28.5% (n = 69) of the institutions, although only 19.8% (n = 48) of those facilities are capable of performing image-guided RT using cone beam computed tomography. Considering only the public health care system, the scenario is more restricted, with 40.1% (n = 65) of the institutions offering intensity-modulated RT, 21% (n = 34) volumetric modulated arc therapy, and 14.8% (n = 24) using cone beam computed tomography. Because of these scare resources, only 16% of Radiation Departments offer stereotactic body RT.
CONCLUSION
Brazil still needs to improve and provide high and safer RT technologies to patients with lung cancer across all Brazilian regions to attend the population needs and obtain better patient outcomes.
INTRODUCTION
Brazil is a country of continental dimensions with a high diversity of epidemiologic, socioeconomic, and infrastructural differences that deeply interfere with its health system. The high contrast between developed and undeveloped areas in a single country creates a challenge for providing good quality health services. Not only the socioeconomic factors impose a challenge, but also the territory itself where some areas are hard to access, such as certain regions in the Amazon.
CONTEXT
Key Objective
What is the current scenario of access for patients with lung cancer to high-quality radiation therapy in Brazil?
Knowledge Generated
The present study draws attention to the current Brazilian situation that faces a relevant heterogeneous distribution of radiotherapy machines and technology. Only a few departments deliver stereotactic body radiation therapy, leaving most of the patients with stage I lung cancer without access to this treatment option.
Relevance
The findings could be used to support new public projects to expand global access to a better radiotherapy treatment quality. In addition, the data may stimulate existing departments to invest in upgrades and implement new treatment modalities.
The Brazilian health system is composed of a private and a public sector mainly divided into three different categories: the Unified Health System (Sistema Único de Saúde [SUS]), where the assistance is publicly given by the state (federal and municipal levels); the private sector, where private resources or public-private partnership (nonprofit institutions) provides services for both the SUS and patients with private insurance; and the private health insurance sector (offers private health plans and insurance).1 The access to health care is a challenge that needs to be overcome, since uncovered populations may be susceptible to worse health outcomes and greater mortality rates.
Implementing new interventions in health is important to develop a better and more efficient health system. Brazil has been undergoing a demographic transition where the population is aging and the birth rate is decreasing. The current life expectancy is 76.6 years.2 Therefore, interventions to improve the health services quality should also take into account these changes in addition to the countries' diversity in socioeconomic terms.
Several diseases have a profound economic impact in the public health sector. In this article, we will concentrate on cancer, since it represents a major challenge worldwide, especially with aging populations, and it is considered an emerging and critical issue for low- and middle-income countries.3 Most South American countries present difficulties in treating high numbers of patients with cancer, especially because of a lack of appropriate equipment and human resources.
LUNG CANCER EPIDEMIOLOGY IN BRAZIL
The Brazilian National Cancer Institute estimates for the 2020-2022 triennium, 625,000 new cases of cancer (450,000, excluding cases of nonmelanoma skin cancer). Lung cancer represents the third most incident among men and fourth among women, where the age-standardized 5-year survival rate is 18% in Brazil, similar to other countries.4 Surgery is considered the gold standard treatment for primary lung tumors. Patients who are not eligible for surgery, or do not wish to undergo surgery, can receive radiotherapy as the main treatment option.5,6 Besides surgical treatment, stereotactic body radiation therapy (SBRT) is a noninvasive method that uses many precisely focused radiation beams to treat tumors. It has emerged as an alternative treatment for initial staging of lung malignancies in older patients, medically inoperable patients, and patients who refused surgery. Recent data showed better survival outcomes with those techniques in oligometastatic patients,7-10 suggesting that patient treatment can be influenced by availability of the services, equipment quality, and surveillance methods.
RADIOTHERAPY ACCESS IN BRAZIL AND PATIENT OUTCOMES
Radiation therapy (RT) has been fundamental in cancer treatment over the years. The development of safer and precise RT technologies improved radiotherapy techniques, resulting in more effective treatments and becoming one of the most cost-effective modalities in cancer therapy.11 Nevertheless, Brazil still faces difficulties in the access to RT, especially because of a lack of well-trained personnel, fair reimbursement, and enough treatment units.12
According to the Brazilian National Commission of Nuclear Energy, RT facilities are unequally distributed across the country (2 of the 26 states lack RT facilities). The WHO recommends a megavoltage machine for every 500,000 inhabitants to provide an adequate support, and therefore, Brazil would need approximately 425 megavoltage machines, which is not the reality of the country.13 In addition, there are different technologies associated with RT and most of the RT machines belong to public health facilities (SUS), a factor that demands government investments.
The prevalence of modern technologies that are essential for sophisticated treatments such as intensity-modulated RT (IMRT), volumetric modulated arc therapy (VMAT), and lung SBRT was investigated in the present study. We provide an overview of the actual numbers of RT facilities in the country, the current availability status of high technology RT, and the overall magnitude of the negative impact of the lack of modern RT technology in the Brazilian lung cancer patient health care.
METHODS
This study evaluates retrospective data published in the first edition of the Brazil Radiotherapy Census conducted by the Brazilian Radiotherapy Society published in 2019.14 Data on the number of existent RT machines in each Brazilian state with their respective technologies, and whether they are used and offered to public or private services, were obtained from the census. The census data were collected through telephone calls, by the Ministry of Health staff from all Brazilian radiation departments. The questionnaire aimed at evaluating several characteristics of the machines, which included types and prevalence of delivery techniques available, image-guided RT (IGRT) modalities, and if care to SUS patients was provided. For data analysis, departments were classified as private or public health care, regardless if they provided mixed care (public and private). The census opted to classify mixed care providers as public institutions. In addition, data regarding the percentage of the population using the public health care system (SUS) or private health providers were obtained from the National Health Agency (Agência Nacional de Saúde),15 and data concerning the machines status were obtained from the Ministry of Health—Brazilian Federal Government.16
RESULTS
Prevalence of RT Facilities
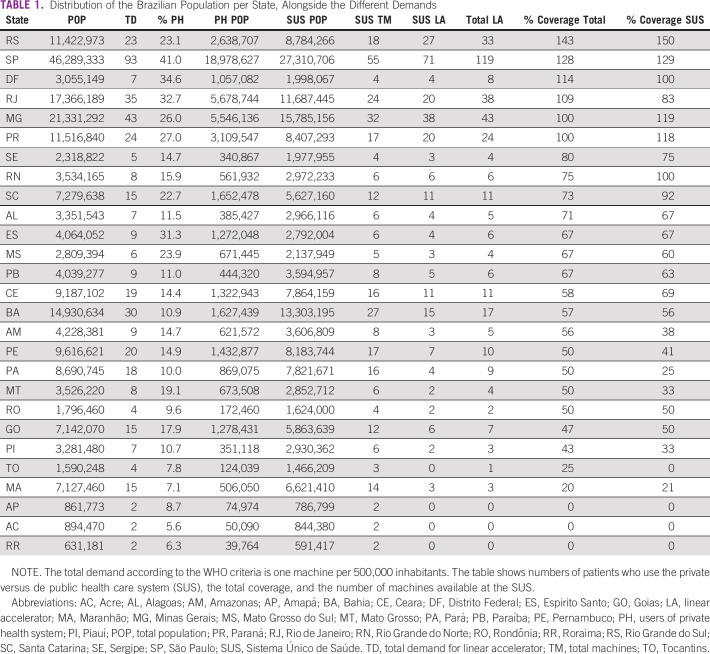
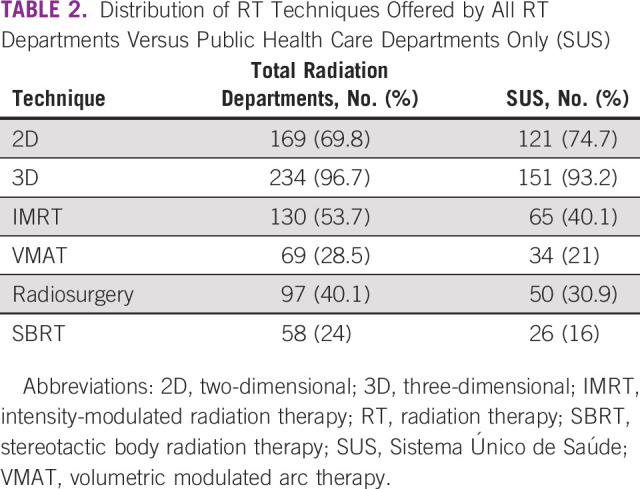
The Brazilian Radiotherapy Census, published for the first time in 2019 by the Ministry of Health, provides different information on the status of RT services in Brazil. The RT machines distribution over Brazilian states according to coverage is shown in Figure 1. In addition, Table 1 shows the Brazilian coverage concerning the population that uses public and private health.
FIG 1.
Distribution of machines' coverage in different Brazilian states. WHO recommends one machine per 500,000 inhabitants.14 AC, Acre; AL, Alagoas; AM, Amazonas; AP, Amapá; BA, Bahia; CE, Ceara; DF, Distrito Federal; ES, Espirito Santo; GO, Goias; MA, Maranhão; MG, Minas Gerais; MS, Mato Grosso do Sul; MT, Mato Grosso; PA, Pará; PB, Paraíba; PE, Pernambuco; PI, Piauí; PR, Paraná; RJ, Rio de Janeiro; RN, Rio Grande do Norte; RO, Rondônia; RR, Roraima; RS, Rio Grande do Sul; SC, Santa Catarina; SE, Sergipe; SP, São Paulo; TO, Tocantins.
TABLE 1.
Distribution of the Brazilian Population per State, Alongside the Different Demands
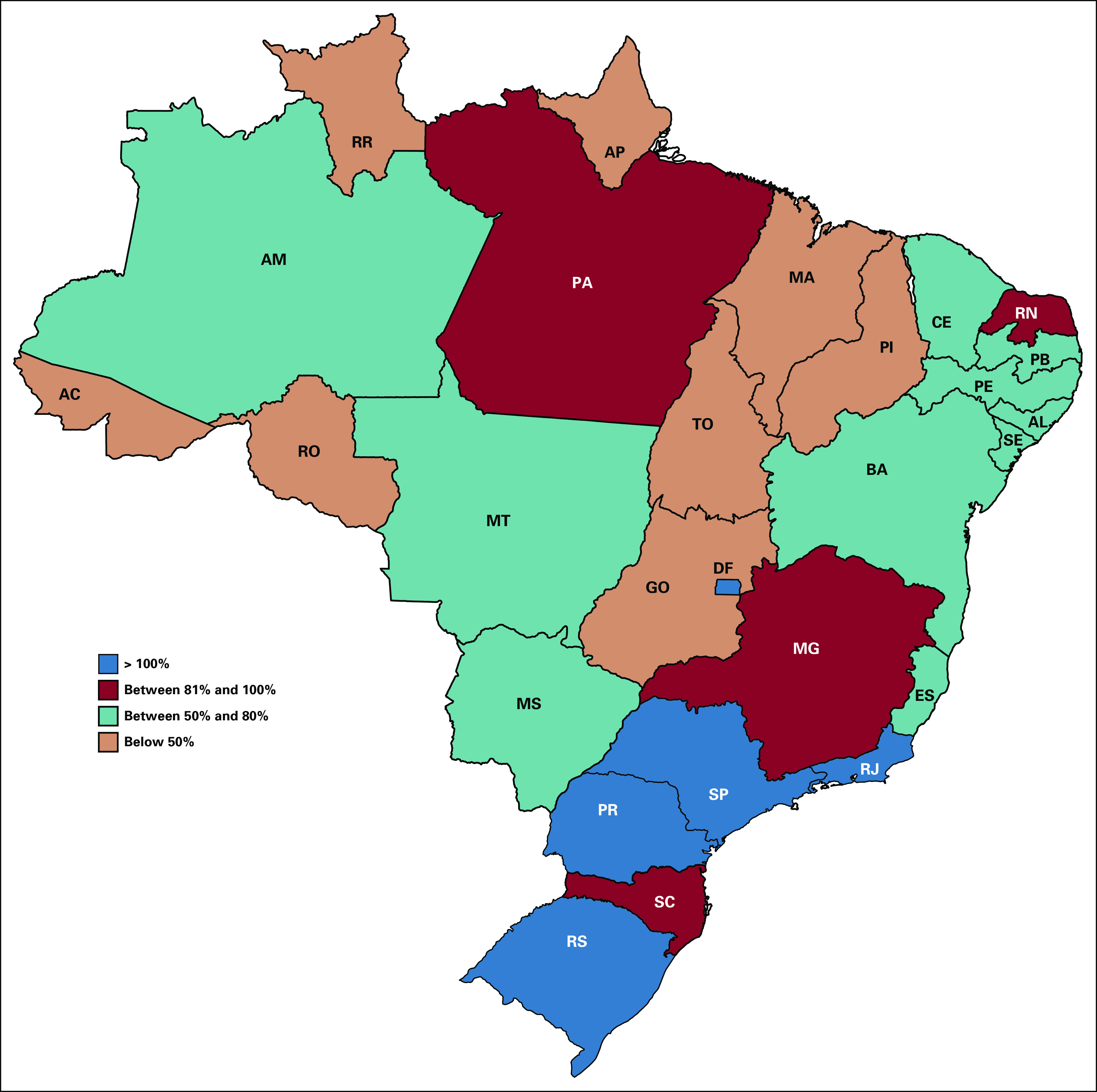
The census objective was to identify and characterize all teletherapy and brachytherapy equipment used in Brazil, which included information about the expected useful life of the equipment in operation, and also to map obsolete models to be potentially replaced in the coming years. The census indicated that Brazil faces a problem regarding obsolete equipment. Brazil has 242 RT departments composed of 20 active cobalt machines and 363 linear accelerators. However, 34% (n = 123) of the linear accelerators are considered obsolete by their manufactures, thus they will not be updated, and the maintenance should be performed by third-party specialized companies other than the original manufacturer. Regarding SUS, there are 162 departments with 251 devices currently being used, but 38% (n = 95) were considered obsolete. The census further indicated that in 2022, it is expected that certain newer models will also go into obsolescence. If the equipment is not replaced soon, there will be 44.6% (n = 162) obsolete equipment in Brazil, where 51% (n = 127) are part of SUS network,14 as shown in Figures 2A and 2B.
FIG 2.
(A) Total obsolete equipment and (B) SUS obsolete equipment for the years 2018 and 2022. SUS, Sistema Único de Saúde.
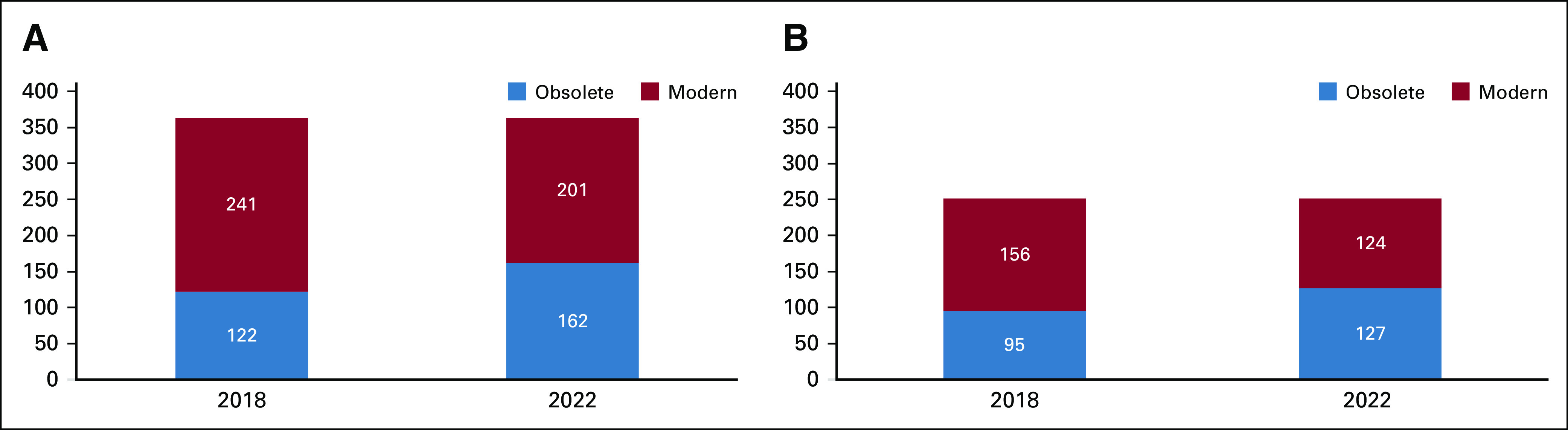
Prevalence of High-Level RT Technologies
Regarding the high technology coverage in Brazil, the results show that IMRT is available in 53.7% (n = 130) of the RT departments and VMAT in 28.5% (n = 69) and only 13.2% (n = 48) of the machines are capable of performing IGRT using cone beam computed tomography (CBCT). In the public network, these numbers are scarcer, with 40.1% (n = 65) offering IMRT, 21% (n = 34) VMAT, and 14.8% (n = 24) having CBCT. In addition, only 16% (n = 26) of the departments offer SBRT. Most RT services in Brazil use conformational or three-dimensional technology in the treatment of lung cancer. This occurs because insurances and the SUS do not include the payment of high technology or daily image diagnosis for these patients, nor is the SBRT technique contemplated. The data are summarized in Table 2.
TABLE 2.
Distribution of RT Techniques Offered by All RT Departments Versus Public Health Care Departments Only (SUS)
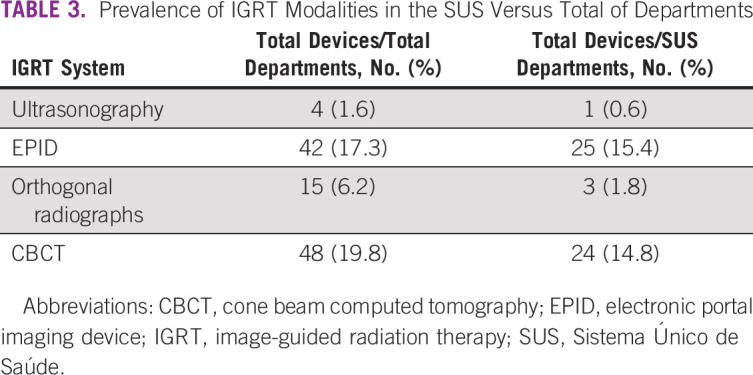
Prevalence of IGRT
IGRT consists of daily position verification guided by images before treatment. Among the devices that have a position verification system, 48 are capable of acquiring CBCTs, which is an indispensable modality considering the treatment of patients with lung cancer. Only 24 CBCT capable machines are part of the SUS coverage network (Table 3). CBCT is a variant of computed tomography (CT), built on the radiation device with an inferior image quality as compared with a diagnosis CT, but it allows patient position verification and basic visualization of the internal anatomy of the area to be treated, such as shape and volume of structures. The implant of fiducials for the use of orthogonal radiographs is also an option, nevertheless this brings greater technical difficulties, in addition to its cost since the technique is not covered by the SUS nor private insurance. Other options are ultrasonography (used for prostate treatments) and electronic portal imaging devices, which operate digital high-energy x-ray system, an adequate tool for bone positioning. Interestingly, there is an issue regarding the lack of use of the already existent technology, which is related to centers that lack equipment maintenance and trained personnel.
TABLE 3.
Prevalence of IGRT Modalities in the SUS Versus Total of Departments
The RT Cost
Until 2017, payment for radiation treatment in Brazil was made based on the number of treatment days and fields delivered. The relationship between the number of treatment days and the payment received had a negative impact on the implementation of hypofractionated schemes for years and consequently on the stimulus for high technology implementation. Treatment packages (per tumor site) have recently been adopted, and the delivery technique and treatment duration are not taken into consideration. For insurers’ payments, there is a guide approved by the Ministry of Health, which regulates prices in all country regions based on the technique used. For SUS, prices are regulated by site, not by technique employed, and any patient with lung cancer, independently if will receive conventional treatment or SBRT, will cost Reais (R$) 3,563 Brazilian reais (∼$792 US dollars [USD]) to the SUS, whereas in the private sector, the average treatment cost is R$15,000.00 Brazilian reais (∼$3,334.00 USD).17 The cost of the linear accelerator itself is approximately 1.5 million USD.18 In addition to the linear accelerator price, import taxes reach up to 40% over the equipment cost in Brazil plus all the implementation costs, and the total value to install and operate a new machine takes up to 60% over the free on board cost and up to 180 days to get operation permit.
DISCUSSION
Cancer management comprises a broad range of treatment types based on distinct techniques, and approximately 60% of all cancer types require RT.19 For lung cancer, this number is even higher reaching approximately 77%.7 Nevertheless, this percentage could be underestimated after recent publications suggested that oligometastatic patients show an increased overall survival benefit when irradiated.8-10,20 Thus, we can estimate that each year, there will be approximately 21,890 new patients with lung cancer requiring RT. In 2016, 823 million USD were spent on lung cancer in Brazil, with mortality rates of approximately 80%21 and 64,000 lung cancer–related deaths in Latin America each year.22 In addition to problems related to treatment, there are problems concerning diagnosis. The Oncoguia Institute, in an online survey, showed that 40.4% of patients with lung cancer were seen by at least three doctors before being diagnosed.23. This increases the costs and difficulties in measuring the real disease's costs. If we expand the analysis to the number of positron emission tomography-CT devices (mandatory examination for patients with lung cancer), Brazil has approximately 135 machines, which represents only 50% of the ideal number according to WHO recommendations.
In 2015, 80 linear accelerators were purchased by the Brazilian Federal Government to be installed throughout the country. Five years later, only 35 installations18 have been carried out and eight are being built, suggesting that if no measures are taken, by 2022, Brazil will have only 244 machines in operation (excluding obsolete machines that will be out of operation). WHO recommends one machine for every 500,000 inhabitants, which means that for 212 million Brazilians, there will have a deficit of at least 180 machines. It is important to point out that in this analysis, the use of the current technology to treat initial or oligometastatic tumors was not taken into consideration. If we analyze the numbers of machines with IMRT/VMAT, SBRT, and IGRT capability, the results would be even more alarming.
In 2018, Mendez et al have estimated the number of preventable oncological deaths in the public health system concerning RT, and they identified that thousands of patients with cancer in need of RT do not have access to this treatment in the SUS (more than 100,000 patients each year). This fact was shown to have a significant impact on cancer survival, since more than 5,000 deaths would have been prevented if RT access was universal.24 To improve the availability of equipment and RT in all Brazilian regions, some measures should be undertaken: an increase in funding, forming new human resources, and a proper training of qualified personnel.12 If all patients with lung cancer who need SBRT would have access to adequate technologies, approximately 1,689 deaths could be prevented. As previously mentioned, of the total number of machines, 34% are considered obsolete by manufactures, and by the year of 2022, these numbers will rise. Therefore, there is a need for urgent actions to improve the future scenario. For example, the machines cost can be an important challenge in developing countries, and in Brazil, the costs comprehend 80% of the total investment, whereas the other 20% is associated with the machines' development and staff salaries (operational costs).7 In contrast, in developed countries, the proportion is the opposite, with the machines cost representing only 30% of the total costs.7 There are still other costs that are difficult to plan ahead, such as training of high-qualified personnel. Training of new specialist doctors adds additional expenses for both training and travel into a project of a new modern facility. Furthermore, economic instability of developing countries leads to the devaluation of the national currency in comparison with foreign currencies, such as the Dollar and Euro, hence increasing the challenge of proposing and executing the implementation of new projects.
With regard to SBRT, if only 16% of services perform this treatment modality,14 it can be estimated that 84% of the population will not have access to this treatment option or will be directly referred to surgery. Interestingly, studies analyzing cost effectiveness comparing SBRT with lobectomy surgery or segmental resection showed superiority of SBRT mainly in patients over 75 years of age,25,26 and thus, the lack of SBRT for younger patients may not interfere with their outcomes.
In the Brazilian SUS, when treatment costs are evaluated without considering installation costs, the payment for Lobectomy surgeries in Brazilian currency (R$) are pulmonary lobectomy in oncology (R$749.97), Mediastinal lymphadenectomy in oncology (R$892.95), and Thoracostomy with closed pleural drainage (R$404.28), which gives a sum of R$2,047.20 reais.26,27 In addition, the patient remains, on average, hospitalized for 7.6 days, with an approximate daily cost of R$2,432.35, totalizing R$18,485.86 for hospitalization plus R$2,047.20 for surgery, giving a total cost of treatment of R$20,533.06 (approximately 3,693.00 USD). This value is 72% higher than the costs of the same patient treated with SRBT. In the private sector, the cost of a video-assisted lobectomy surgery, including all hospitalization costs, is approximately R$6,322.15, and a robotic surgery is R$7,642.94, which is 48% and 57% higher than the cost of a SBRT treatment for the same patient, respectively.28
Although public institutions may take longer to pay for the equipment, as the payments received from SUS are inferior to private insurance payments, new and modern machines are able to treat almost 40% more patients per month than obsolete devices because of the ability to deliver hypofractionated treatments. For this reason, even with the unfavorable monetary scenario, the high demand for radiotherapy along with greater treatment capacity of modern equipment results in a better financial viability for equipment equipped with CBCT. This is due to the fact that the CBCT represents an average of 20% increase in the value of the equipment, but 40% on its capacity. There are many secondary benefits, since patients undergoing modern and high-quality radiotherapy have fewer complications related to treatment toxicity, spend fewer days in hospital, consume less medication to relieve symptoms, and travel less days for treatment.
Limitations of the present study concern the challenge of verifying if an available technique or equipment is fully implemented and operational and if it is being used for all patients. As mentioned in methodology, this study was not able to precisely measure the overlap between private departments also delivering public health care. Older devices are expected to require maintenance more frequently, and the Ministry of Health and the census do not report the uptime (ratio between the real operated hours and the total expected operation hours) after maintenance hours of these devices. Thus, we could not obtain the exact information regarding machine daily activity. This can explain the divergence between the number of machines reported and the existing queues for treatment. An interesting example is the state of Rio de Janeiro, where the demand should be met by the number of installed machines. However, there is currently a waiting time of approximately 8 months for receiving RT treatment offered by the SUS.
The public health system and most of the health insurance companies do not subsidize the use of daily imaging for position verification through differentiated payment, which could potentially improve patient care quality. In addition, the treatment ticket in many cases does not take into account the type of dose delivery technique, which does not support the implementation of newer and more modern schemes of treatment. Although many of the technological improvements have only the installation cost, many institutions understand that the daily use is not economically justifiable.
The main problem in installing a radiotherapy service is the cost of the machine, which can be negatively affected by the devaluation of the country currency and the high import tax rate. An interesting solution for this issue could be to provide tax exceptions, or reductions, on the equipment acquired by private institutions. For example, private departments could be tax exempt in exchange for offering a certain percentage of coverage for public health patients. This measure could help the implementation of new technologies. However, public institutions do not have import tax rate costs, yet administrative problems frequently affect equipment installation and maintenance, plus the process of sustaining an adequate team of human resources.
Despite all problems addressed, in the last few years, we observed a considerable improvement concerning high technology, with some departments capable of offering treatments with similar quality to those offered in developed countries, which was very unlikely to occur a decade ago.
In conclusion, the delivery of contemporary radiotherapy to patients with lung cancer requires the use of state-of-the-art technology to obtain optimal clinical outcomes and minimize side effects. Brazil has approximately 383 treatment units; nevertheless, a significant fraction of the machines is obsolete. Estimates based on the country's population and WHO criteria indicate that 425 treatment units would be necessary for optimal care delivery. Only 16% of departments provide SBRT, resulting in the lack of access by a large part of the lung cancer population, especially stage I inoperable patients. Although improvements took place in the last decade with the acquisition of new equipment, challenges regarding their implementation still need to be overcome. The data gathered in this work suggest that, if no measures are taken, by the year 2022, Brazil will have a deficit of 180 machines, resulting in low quality or even no treatment for some patients (approximately 100,000/year).
Arthur Accioly Rosa
Employment: Grupo Oncoclinicas
Honoraria: Roche
Consulting or Advisory Role: AstraZeneca
Travel, Accommodations, Expenses: Roche
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented at the IALSC World Conference on Lung Cancer 2020, Singapore, January, 28-31, 2021.
AUTHOR CONTRIBUTIONS
Conception and design: Lilian Dantonino Faroni, Veronica Aran, Carlos Gil Ferreira
Administrative support: Lilian Dantonino Faroni, Carlos Gil Ferreira
Provision of study materials or patients: Renan Serrano Ramos
Collection and assembly of data: Lilian Dantonino Faroni, Arthur Accioly Rosa, Renan Serrano Ramos
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by the authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Arthur Accioly Rosa
Employment: Grupo Oncoclinicas
Honoraria: Roche
Consulting or Advisory Role: AstraZeneca
Travel, Accommodations, Expenses: Roche
No other potential conflicts of interest were reported.
REFERENCES
- 1.Paim J, Travassos C, Almeida C, et al. The Brazilian health system: History, advances, and challenges Lancet 3771778–17972011 [DOI] [PubMed] [Google Scholar]
- 2.United Nations World Population Prospects 2019 2019. https://population.un.org/wpp/ [Google Scholar]
- 3.Amendola B, Quarneti A, Rosa AA, et al. Perspectives on patient Access to radiation oncology services in South America Semin Radiat Oncol 27169–1752017 [DOI] [PubMed] [Google Scholar]
- 4.Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries Lancet 3911023–10752018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szklo AS, Yuan Z, Levy D. Update and extension of the Brazil SimSmoke model to estimate the health impact of cigarette smoking by pregnant women in Brazil. Cad Saude Publica. 2017;33:e00207416. doi: 10.1590/0102-311X00207416. [DOI] [PubMed] [Google Scholar]
- 6.Abreu CECV, Ferreira PPR, de Moraes FY, et al. Stereotactic body radiotherapy in lung cancer: An update TT J Bras Pneumol 41376–3872015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atun R, Jaffray DA, Barton MB, et al. Expanding global access to radiotherapy Lancet Oncol 161153–11862015 [DOI] [PubMed] [Google Scholar]
- 8.Gomez DR, Blumenschein GR, Lee JJ, et al. Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer without progression after first-line systemic therapy: A multicentre, randomised, controlled, phase 2 study Lancet Oncol 171672–16822016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palma DA, Olson R, Harrow S, et al. Stereotactic ablative radiotherapy for the comprehensive treatment of oligometastatic cancers: Long-term results of the SABR-COMET phase II randomized trial J Clin Oncol 382830–28382020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitchell KG, Farooqi A, Ludmir EB, et al. Improved overall survival with comprehensive local consolidative therapy in synchronous oligometastatic non–small-cell lung cancer Clin Lung Cancer 2137–46.e72020 [DOI] [PubMed] [Google Scholar]
- 11.Poortmans P, Valentini V, Lievens Y.Expanding global access to radiotherapy: The European Society for Radiotherapy and Oncology perspective Lancet Oncol 161148–11492015 [DOI] [PubMed] [Google Scholar]
- 12.de Moraes FY, Marta GN, Hanna SA, et al. Brazil's challenges and opportunities Int J Radiat Oncol Biol Phys 92707–7122015 [DOI] [PubMed] [Google Scholar]
- 13.Araujo LH, Baldotto C, de Castro G, Jr, et al. Lung cancer in Brazil J Bras Pneumol 4455–642018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ministerio da Saude, Secretaria de Atenção Especializada á Saúde; Departamento de Atenção Especializada e Temática. Censo Radioterapia 2019.; https://portalarquivos.saude.gov.br/images/pdf/2019/julho/26/paper-radioterapia-ALT3.pdf [Google Scholar]
- 15.Agência Nacional de Saúde www.ans.gov.br
- 16.Ministry of Health, Brazil https://portalarquivos.saude.gov.br/images/pdf/2019/julho/26/paper-radioterapia-ALT3.pdf
- 17. https://www.conab.gov.br/institucional/conab-corporativa/assistencia-a-saude
- 18.Portal Arquivos saúde.gov. https://portalarquivos.saude.gov.br/images/pdf/2020/September/29/Situacao-dos-Projetos--PB-e-PE-SETEMBRO-2020---2.pdf
- 19.Mohan G, Ayisha Hamna TP, Jijo AJ, et al. Recent advances in radiotherapy and its associated side effects in cancer—A review. J Basic Appl Zool. 2019;80:14. [Google Scholar]
- 20.Pasalic D, Lu Y, Betancourt-Cuellar SL, et al. Stereotactic ablative radiation therapy for pulmonary metastases: Improving overall survival and identifying subgroups at high risk of local failure Radiother Oncol 145178–1852020 [DOI] [PubMed] [Google Scholar]
- 21.Estimate/2020—Cancer incidence in Brazil. https://www.inca.gov.br/sites/ufu.sti.inca.local/files/media/document/estimativa-2020-incidencia-de-cancer-no-brasil.pdf
- 22.Carioli G, Bertuccio P, Malvezzi M, et al. Cancer mortality predictions for 2019 in Latin America Int J Cancer 147619–6322020 [DOI] [PubMed] [Google Scholar]
- 23.Oncoguia.org: Guia Detalhado do Câncer de Pulmão. http://www.oncoguia.org.br/conteudo/guia-detalhado/2934/150/
- 24.Mendez LC, Moraes FY, Fernandes GDS, et al. Cancer deaths due to lack of universal access to radiotherapy in the Brazilian Public Health System Clin Oncol (R Coll Radiol) 30e29–e362018 [DOI] [PubMed] [Google Scholar]
- 25.Smith BD, Jiang J, Chang JY, et al. Cost-effectiveness of stereotactic radiation, sublobar resection, and lobectomy for early non-small cell lung cancers in older adults J Geriatr Oncol 6324–3312015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paix A, Noel G, Falcoz PE, et al. Cost-effectiveness analysis of stereotactic body radiotherapy and surgery for medically operable early stage non small cell lung cancer Radiother Oncol 128534–5402018 [DOI] [PubMed] [Google Scholar]
- 27.AUDITASUS Custo médio de uma diária em UTI, por especialidade (uf). https://auditasus.com.br/internacoes-sus/custo/custo-medio-diaria-uti/custo-medio-diaria-uti-por-especialidade
- 28.Nassar A, Lucas MO, Pereira J, et al. Robotic thoracic surgery: Cost analysis. J Vis Surg. 2018;4:207. [Google Scholar]