Abstract
Background:
The purpose of this descriptive phenomenological study was to gain an in-depth understanding of cancer patients’ experiences and perspectives on self-reporting their symptoms. Patients with cancer experience a wide variety of symptoms from both their disease and treatment, yet clinicians are often unaware of their patients’ symptoms due to poor reporting methods. Poorly documented symptoms are more likely to go untreated, causing increased symptom distress and decreased quality of life for patients. Effective, real-time communication between patients and health-care practitioners is key to symptom assessment and management. Moreover, it is important for patients’ communication preferences to be taken into account when developing symptom management plans.
Methods:
This qualitative study focused on the symptom reporting experiences of 13 adults in the United States with advanced or metastatic cancer who were undergoing systemic cancer treatment. Data were collected via interviews.
Results:
The findings revealed that a personalized symptom management plan, prompt reporting, and timely communication with health-care practitioners improved patients’ physical and emotional wellbeing.
Conclusions:
A better understanding of cancer patients’ experiences self-reporting their symptoms may lead to improved communication methods and more effective reporting systems, which ultimately reduce patient burden and enhance patients’ self-advocacy. Ensuring that patients’ preferences for reporting their symptoms are met may positively influence the likelihood and timeliness of symptom self-reporting. Developing new and improved ways for health-care teams to manage symptoms is vital to improving patients’ quality of life.
Patients with cancer experience symptoms from both their disease and treatment, yet clinicians are unaware of 50% to 80% of their patients’ symptoms (Epstein & Street, 2007; Farrell et al., 2001; Ryan et al., 2005). For most cancer patients, symptoms are poorly documented and their impacts are often underestimated and undertreated (McIntyre, 2015). This can lead to increased symptom distress and decreased quality of life (Cella, 1997; Lee, 2008). Communication of symptoms to health-care practitioners is key to symptom management. Developing new ways for patients to self-report symptoms and for advanced practitioners to manage patient symptoms will help improve cancer patients’ quality of life (National Institute of Nursing Research, 2016). It is crucial for patients to report their symptoms as they are experienced so that assessment and management can occur in real time.
A literature review that was conducted included studies where patients used an electronic method to report their symptoms (Carrasco & Symes, 2018). The studies used a vast array of electronic methods for patients to self-report their symptoms (Basch et al., 2016; Berry et al., 2014; Blum et al., 2014; Cella, et al., 2014; Fromme et al., 2004). Some electronic methods feature an interactive component that allows for patient–clinician communication. This literature review uncovered the lack of understanding of the patients’ lived experience of self-reporting their symptoms and their preferences to report their symptoms. Therefore, a qualitative study was conducted to improve the understanding of how patients prefer to report their symptoms, as this may influence the likelihood that patients will report their symptoms in a timely fashion.
Qualitative studies allow participants to thoroughly express their experiences and perspectives, and increase understanding of the subjective nature of patient self-reporting of symptoms. Qualitative methods more adequately capture the totality of patients’ experiences than one measure alone. The qualitative method used in this study was Husserl’s descriptive phenomenology. Thus, the purpose of this descriptive phenomenological study was to gain an in-depth understanding of cancer patients’ experiences with and perspectives on self-reporting their symptoms, which could then lead to improved symptom management.
One of the holistic frameworks for symptom management in advanced nursing practice has been the symptom management theory (SMT; Figure 1), which was the underlying model for this study. The SMT is a deductive, process-focused model that addresses three interactive components of symptom management: (1) symptom experience, (2) symptom management strategies, and (3) outcomes. All three components are essential for effective symptom management (Dodd et al., 2001). The SMT model indicates simultaneous interactions among all three concepts. In the case of common symptoms (e.g., upset stomach, rash, cough), these interactions can take place quickly and be self-managed. However, when symptoms are complex and/or distressing, as is the case for the symptoms of many advanced cancer patients, reporting the symptom experience is vital so that effective symptom management strategies are pursued and outcomes are assessed in a formal, timely fashion.
Figure 1.
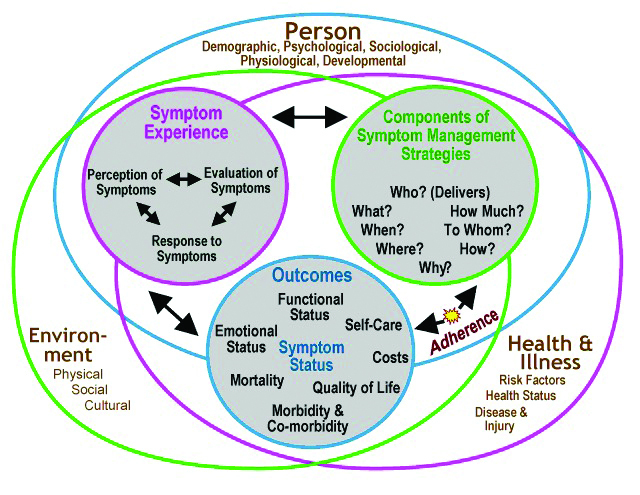
Symptom management model. Reproduced with permission from Dodd et al. (2001).
Newcomb (2010) realized that communication is an important part of symptom management and suggested a modification to the SMT model. In Newcomb’s (2010) updated SMT model, communication and feedback are explicitly described as conceptual links among the components. Humphreys and colleagues (2014) agreed that providers should establish and maintain good patient-provider communication in order to understand their patients’ symptom perceptions and experiences and to implement appropriate management strategies for symptoms. The SMT model was incorporated into this study in order to understand the completeness of the model and if the findings from this study influence the need for further updates to the SMT model. This could further advance the theoretical understanding of symptom management as well as lead to the emergence of clinical implications.
Design and Research Approach
Edmund Husserl’s (1960) descriptive phenomenology formed the theoretical framework for this qualitative study. This existential philosophical school of thought is congruent with the purpose of the study as it seeks to understand the human condition as it is experienced by participants. The main methodological consideration is to explore, analyze, and describe the phenomenon while maintaining a near-real picture of the lived experience (Streubert & Carpenter, 2011). This requires the researcher to review the content devoid of any preconceived notions (Giorgi, 2008). As an oncology advanced practice nurse, it was important for the researcher to separate her own ideas from the study. Bracketing is a practice that involves recognizing and temporarily sustaining the preconceived notions of the phenomenon being studied (Polit & Beck, 2017). The researcher used bracketing to identify her perspectives and allow the phenomenon to be uncovered without distortion by her own preconceptions (Husserl, 1965).
Phenomenology is a method of inquiry with the objective of exploring the phenomenon from the perspective of those who experience it firsthand to uncover the essential meaning of the lived experience of the phenomenon that is not well understood (Grbich, 2012; Polit & Beck, 2012). Phenomenology is also a science that describes textures and structures of things in peoples’ minds (Streubert & Carpenter, 2011). The phenomenological method allows the researcher to critically examine these experiences to reveal their hidden meanings instead of taking them for granted.
Setting and Sample Information
The Institutional Review Board at Texas Woman’s University granted approval for the study. A total of 13 patients were enrolled in the study; all individuals had cancer and direct, first-hand experience of reporting their symptoms. The sample size for qualitative studies should follow the concept of saturation (Morse, 1994); therefore, participants were enrolled until data saturation was reached. Data saturation is achieved when there is redundancy of information or when no new data emerges with further data collection efforts (Polit & Beck, 2017).
Enrollment took place from October 2017 to January 2019, and a total of 13 participants, including the three participants from the pilot study, were enrolled and are part of this final data analysis. Data saturation was reached when there was no new information that emerged in the interviews with the last few participants. Also, qualitative studies that were published in the past 5 years enrolled seven to fifteen participants, with one study enrolling 26 participants.
The patients were English speaking, female and male adults who were 18 years or older and resided in the United States. The study’s patients (N = 13) ranged in age from 34 to 85 years, and all were Caucasian. Four of the patients were male and nine were female. Ten of the patients had more than 17 years of education, while three patients had 13 to 16 years of education. All patients had intact mental statuses and were receiving systemic cancer treatment for unresectable or metastatic disease at the time of the interviews.
Methods
Data were collected through individual interviews. Three interviews were conducted in-person, and the other ten interviews were conducted via Skype, FaceTime, or Google Hangouts. Interviews ranged in length from 20 to 60 minutes and were digitally recorded. The interviews were transcribed verbatim by a professional transcriptionist after obtaining a nondisclosure agreement. The interviewer asked patients to describe their experiences with self-reporting their symptoms. Interviews began with an open-ended prompt: "Let’s start by talking about a time when you reported your symptoms. Tell me a story about how you reported your symptoms." Then, prompts and follow-up questions were used to help patients elaborate on specific experiences reporting symptoms, feelings while reporting, use of electronic methods to report, and individual preferences regarding reporting symptoms. Six patients agreed to review the findings from their respective interviews; these follow-up conversations were digitally recorded and transcribed. Validation of study findings with these six patients verified the accuracy of interpretation (Colaizzi, 1978).
Analysis of Data
Using Colaizzi’s (1978) method of analyzing qualitative data, the transcribed interviews were read and reread by the researcher. The researcher extracted significant statements from each individual transcript and organized these statements into clusters to identify themes. The themes were then organized and synthesized into an exhaustive description of the phenomenon. The exhaustive description was then reduced to a descriptive identification of the patients’ experiences of self-reporting their symptoms.
Study Limitations
One limitation of this study was that the data were dependent on the patients’ abilities to recall their experiences. Other limitations were that the sample was recruited from the researcher’s community and social media websites for cancer patients, and lacks inclusion of individuals with lower educational status or with diverse ethnic and racial backgrounds, which limit the generalizability of the findings. The use of snowball sampling was a third limitation. Snowball sampling allows studies to be conducted with hard-to-reach populations, but it does not select the sample based on random selection, unlike probability sampling techniques. Therefore, it is impossible to determine the sampling error and make statistical inferences from the sample to the larger population. As such, snowball samples should not be considered representative of the population being studied (Faugier & Sargeant, 1997).
Findings
The findings from the categorized interview data of the 13 patients revealed four main themes: (1) inability to recall symptoms, (2) communication expectations (subthemes: timeliness, direct communication, accuracy), (3) self-advocacy, and (4) emotional relief with communication.
Theme 1: Inability to Recall Symptoms
Cancer patients’ inability to recall symptoms can make it difficult to manage and prevent the recurrence of symptoms. The patients in this study reported a wide range of symptoms that included shortness of breath, fatigue, nausea, and sleep disturbances. Some also described changes in cognitive and emotional functioning. Two major factors may contribute to patients’ inability to recall symptoms: timing and frequency of reporting, and cognitive impairment caused by the cancer treatment itself. It is well established that chemotherapy can induce cognitive impairment (Moore, 2014). To mitigate these factors, consistent and detailed self-reporting is essential.
The timing and frequency of patients’ self-reporting of symptoms can greatly influence the information received from the patient and the ways that caregivers can respond. Recall bias, which occurs when people are asked to recall past experiences, may limit accurate reporting of symptoms, especially for patients experiencing multiple symptoms (Yarbro et al., 2011). Experiences that have recently occurred can be recalled more clearly, so it is important that patients have a way to record their symptoms as they occur. The patients reported that they had difficulty recalling their symptoms during the weekly visit with health-care practitioners; recall became even more difficult when patients only met with their practitioner every few weeks. They could not recall the symptoms that had occurred 2 to 7 days after their treatment and could only recall symptoms from the past 1 or 2 days. To remedy the problem of recall bias, some patients routinely logged their symptoms at home and shared these notes with practitioners during their clinic visits.
Theme 2: Communication Expectations
All patients discussed their expectations of communication; their comments were grouped into three subthemes: timeliness, direct communication with the provider, and accuracy of symptoms reported. The patients verbalized that when symptoms were bothersome and/or interfered with activities of daily living, they always reported their symptoms; patients did not want to wait until their next follow-up clinic visit unless it was the next day. Real-time reporting helped patients manage their symptoms at home and avoid extra trips to the clinic. More importantly, real-time reporting and quick feedback from practitioners helped patients avoid emergency room visits to seek relief from symptoms. In addition to communication, feedback was another concept that Newcomb (2010) added to the original SMT model. This study confirmed the importance of timely feedback, as patients talked about the difficulty of waiting for feedback, specifically their health-care team’s responses on how to manage symptoms. It was important to all the patients to get a response about symptom management in a timely manner (within 24 hours).
Direct communication is defined as a patient communicating directly to a health-care practitioner who has knowledge about them. Most patients discussed the importance of talking directly to practitioners who were knowledgeable about them and their situation. In addition to talking directly to their practitioner, most of the patients talked about their expectations for a symptom management plan or, at the very least, acknowledgement of their symptoms by their practitioners. Accurate symptom reporting is related to the importance of direct communication. Some patients framed this issue as being about their individual voices being heard. They wanted their symptoms to be reported accurately, and, if possible, they wanted to speak directly to their practitioners about their symptoms, because they did not want their symptoms to be lost in translation or limited by a standardized checklist.
Increasingly, patients with cancer are being recognized as members of the care team. Building effective communication between the patient and the health-care team can have positive effects during cancer treatments. The expectations regarding patient-clinician communication are changing as more emphasis is placed on the quality of communication between patients and clinicians. To communicate better, patients need easier access to information about their medical condition and their options for patient-centered care. On the other hand, whole-person care requires that practitioners know their patients, what is important to them, and how they derive meaning in their lives. National cancer-related organizations have increasingly recognized communication as crucial and a component of standard cancer care. In 2018, the American Society of Clinical Oncology issued its first patient-clinician communication guideline to help achieve this (Gilligan et al., 2018). Enhanced communication can empower patients to monitor and record their symptoms and provide them with immediate feedback, ultimately leading to more effective management of their symptoms.
Theme 3: Self-Advocacy
Self-advocacy as part of symptom management means that patients are equipped with the necessary tools and skills to assert themselves and clearly communicate their needs during cancer care. In this study, some patients discussed the need to be one’s own advocate: to keep track of symptoms and treatments, to seek knowledge independently, to persist in finding ways to manage symptoms, and to find support outside of the caregiving team. Self-advocacy is not specifically referenced as an aspect of the SMT model, but it could be covered by the feedback aspect in the modified version of the model (Newcomb, 2010).
Self-advocacy can lead patients to more effective symptom management because it can empower them to take more responsibility for their care. Patients who are proactive and educated can positively impact their quality of life and the care they receive (Newcomb, 2010). Stovall and Johns Clark have identified several important reasons for self-advocacy, one of which is a commitment to shared responsibility with the medical team, which can lead to improved physical, emotional, and mental health (National Coalition for Cancer Survivorship, n.d.).
Theme 4: Emotional Relief With Communication
Most patients discussed the fact that communication with their health-care team led to stress relief. Even if communication did not result in any changes to patients’ care, it was important to merely have the ability to report the symptoms as they were occurring. The emotions patients expressed prior to communicating their symptoms included increased anxiety, concern, annoyance, or urgency. Some patients noted that their stress increased when they were not able to talk to their health-care team about their symptoms. After speaking with practitioners, however, patients reported that they felt more relieved, calm, and relaxed. In other words, while patients hoped that communication would lead to management plans for the symptoms they were reporting, the simple acknowledgement of their symptoms made them feel heard and emotionally supported.
Addressing and managing symptoms requires great time and effort from nurses and providers. It may be encouraging to know that all the patients reported that they had experienced anxiety, fear, or concern as a result of their symptoms, but after talking to someone on their health-care team, every participant experienced emotional relief.
Discussion
Research to improve ways for symptom reporting in oncology is ever evolving. Reeve and colleagues (2014) gathered a panel of experts that included patient representatives and identified a core set of 12 symptoms. They recommended that these core symptoms be assessed in all clinical and observation trials, but there was no discussion regarding the use of this core set of symptoms in standard clinical practice. Brant and colleagues (2019) reported on the use of electronic patient-reported outcome assessment that would generate a personalized care plan tailored to the symptoms that patients reported. One finding related to communication was that patients perceived improved team communication with the use of the electronic care plan, yet this was not further explored in the qualitative part of their study.
The modified SMT model (Newcomb, 2010) includes communication and can be used as a model for patient-centered care and as a theoretical framework in symptom research. Patient-centered care includes fostering good communication between patients and their cancer care team. Moreover, patient-centered communication is critical to good patient care (McCabe, 2004). Patient-centered communication guides treatment planning through direct transmission of information and provides a therapeutic and supportive environment for the patient (Jangland et al., 2009; Moira, 2001; Thorsteinsson, 2002).
Understanding each patient’s experiences, perspectives, and preferences is vital to quality care. The two themes that emerged in all the interviews were the importance of real-time reporting for bothersome symptoms and the desire to communicate directly with the practitioner who provided the symptom management plan. Health-care practitioners need to understand patients’ communication preferences. Approaches that allow for real-time reporting and direct communication with the practitioner may better enable patients to accurately report their symptoms, which in turn can benefit their physical and emotional wellbeing.
When the patients discussed their preferred communication methods, they mentioned communication that was simple, easy, accessible, and reliable. Some mentioned they liked call methods with video capabilities, such as Skype, FaceTime, or Google Hangouts. This could be an approach to consider especially during the time of the COVID-19 pandemic. Some of the patients appreciated the ability to send images of their symptoms because photographs helped doctors manage patients’ symptoms more effectively. Some patients noted that their reporting methods needed to be individualized because prepopulated symptom checklists did not always contain the symptoms they were experiencing. Indeed, some thought that the checklist was only helpful during the initial clinic visit.
Several initiatives are under way to improve patients’ abilities to report their symptoms. Basch and colleagues (2016) found a 5-month improvement in overall survival among patients who reported their symptoms routinely using the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) during cancer treatment. The NCI-CTCAE was filled out at each appointment and between appointments using an online, web-based version through which patients’ symptoms were monitored.
In 2015, the Center for Medicare and Medicaid Innovation launched the Oncology Care Model (OCM). The first iteration of the OCM required patient-reported, outcome-based quality metrics. In 2016, this requirement was removed and the 21st Century Cures Act was signed into law. The hope is that the 21st Century Cures Act will offer a structured way to collect information from patients about the burden of their disease and what matters to them in order to improve patient outcomes (Congress.gov. 2016).
Another initiative, known as the Symptom Management Implementation of Patient Reported Outcomes in Oncology (SIMPRO) Research Center, is conducting a study that will integrate the use of patient-reported outcomes into the routine practice of oncology providers with the goal of improving symptom management while decreasing emergency room visits and hospital admissions (SIMPRO Research Center, 2018). SIMPRO will allow patients to use their smartphones or personal computers for real-time reporting. The symptom reports will be integrated in the patient’s electronic health record so that providers can easily access them and reply to the patient.
For patients with cancer, routinely self-reporting symptoms improves detection of symptoms, improves management and quality of care, and enhances patient satisfaction (Basch, 2014). It is crucial that hospitals and researchers continue developing effective ways for oncology patients to communicate with their health-care practitioners.
Conclusion
Understanding cancer patients’ communication-related experiences, preferences, and perspectives can lead to improved reporting of symptoms and improved care. Quality communication between patients and practitioners ultimately reduces patient burden and enhances patient engagement. This research revealed several conclusions and implications for practice.
First, it concurs with Newcomb (2010) that communication is needed in managing symptoms in oncology patients, which leads to decreased stress related to improved communication with, and feedback from, patients’ health-care teams.
Second, real-time reporting and direct communication with health-care practitioners could lead to improved symptom management that would allow patients to more quickly return to their daily lives after experiencing symptoms.
Third, the results of this study could lead health-care teams in the discussion of understanding each of their patients’ preferred methods for reporting their symptoms. These personalized communication methods may lead to better care for oncology patients, greater physical and emotional wellbeing, and better outcomes. This is of greater relevance during the time of the COVID-19 pandemic with the increased use of telemedicine.
Acknowledgment
The author would like to thank Blog for a Cure, Beauty through the Beast, Fight CRC, Dee Sparacio (Women of Teal), Male Breast Cancer Coalition, Tex Us Too, and Outshine with Karen Ingalls for their support and help in recruiting patients for this study.
Footnotes
Dr. Carrasco is an employee of Array BioPharma Inc.
Reference
- Basch E. M., Deal A. M., Kris M. G., Scher H. I., Hudis C. A., Sabbatini P., … Schrag D. (2016).Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. Journal of Clinical Oncology, 34(6), 557–565. 10.1200/JCO.2015.63.0830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry D. L., Hong F., Halpenny B., Partridge A. H., Fann J. R., Wolpin S., … Ford R. (2014).Electronic self-report assessment for cancer and self-care support: Results of a multicenter randomized trial. Journal of Clinical Oncology, 32(3), 199–205. 10.1200/jco.2013.48.6662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blum D., Koeberle D., Omlin A., Walker J., Von Moos R., Mingrone W., … Ribi K. (2014).Feasibility and acceptance of electronic monitoring of symptoms and syndromes using a handheld computer in patients with advanced cancer in daily oncology practice. Supportive Care in Cancer, 22(9), 2425–2434. 10.1007/s00520-014-2201-8 [DOI] [PubMed] [Google Scholar]
- Brant J. M., Hirschman K. B., Keckler S. L., Dudley W. N., & Stricker C. (2019).Patient and provider use of electronic care plans generated from patient-reported outcomes. Oncology Nursing Forum, 46(6), 715–726. 10.1188/19.ONF.715-726 [DOI] [PubMed] [Google Scholar]
- Carrasco S., & Symes L. (2018). Patient use of electronic methods to self-report symptoms: An integrative literature review. Oncology Nursing Forum, 45(3), 399–416. 10.1188/18.ONF.399-416 [DOI] [PubMed] [Google Scholar]
- Cella D. (1997).The functional assessment of cancer therapy-anemia (FACT-An) scale: A new tool for the assessment of outcomes in cancer anemia and fatigue. Seminars in Hematology, 34(3 Suppl 2),13–19.https://pubmed.ncbi.nlm.nih.gov/9253779/ [PubMed] [Google Scholar]
- Cella D., Choi S., Garcia S., Cook K. F., Rosenbloom S., Lai J. S., … Gershon R. (2014).Setting standards for severity of common symptoms in oncology using the PROMIS item banks and expert judgement. Quality of Life Research, 23,2651–2661. 10.1007/s11136-014-0732-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colaizzi P. F. (1978).Psychological research as the phenomenologist views it. In Valle R. S. & King M. (Eds.), Existential phenomenological alternatives for psychologyp.48-71.New York, NY: Plenum. [Google Scholar]
- Congress.gov. (2016).21st Century Cures Act, H.R. 34, 114th Congress. https://www.congress.gov/bill/114th-congress/house-bill/34
- Dodd M., Janson S., Facione N., Faucett J., Froelicher E. S., Humphreys J., … Taylor D. (2001).Advancing the science of symptom management. Journal of Advanced Nursing, 33(5), 668–676. 10.1046/j.1365-2648.2001.01697.x [DOI] [PubMed] [Google Scholar]
- Epstein R. M., & Street R. L. (2007).Patient-centered communication in cancer care: Promoting healing and reducing suffering. NIH Publication No. 07-6225. Bethesda, MD: National Cancer Institute.https://cancercontrol.cancer.gov/brp/docs/pcc_monograph.pdf [Google Scholar]
- Farrell C., Beaver K., Heaven P., & Maguire P. (2001).Identifying the concerns of women undergoing chemotherapy treatment for cancer. European Journal of Cancer, 37(Suppl. 6),S390. 10.1016/S0959-8049(01)81894-3 [DOI] [Google Scholar]
- Faugier J., & Sargeant M. (1997).Sampling hard to reach populations. Journal of Advanced Nursing, 26,790–797. 10.1046/j.1365-2648.1997.00371.x [DOI] [PubMed] [Google Scholar]
- Fromme E. K., Eilers K. M., Mori M., Hsieh Y. C., & Beer T. M. (2004).How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the Quality-of-Life Questionnaire C30. Journal of Clinical Oncology, 22(17), 3485–3490. 10.1200/JCO.2004.03.025 [DOI] [PubMed] [Google Scholar]
- Gilligan T., Bohlke K., & Baile W. F. (2018).Patient-clinician communication: American Society of Clinical Oncology consensus summary. Journal of Oncology Practice, 14(1), 42–46. 10.1200/JOP.2017.027144 [DOI] [PubMed] [Google Scholar]
- Giorgi A. (2008).Concerning a serious misunderstanding of the essence of the phenomenological method in psychology. Journal of Phenomenological Psychology, 39(1), 33–58. 10.1163/156916208x311610 [DOI] [Google Scholar]
- Grbich C. (2012).Qualitative data analysis: An introduction. London, UK: Sage Publications. [Google Scholar]
- Humphreys J., Janson S., Donesky D. A., Dracup K., Lee K. A., Puntillo K., … Kennedy C. (2014).Theory of symptom management. In Smith M. J. & Liehr P. R. (Eds.),Middle range theory for nursing (3rd ed.,p.141-164.New York, NY: Springer. [Google Scholar]
- Husserl E. (1960).Cartesian meditations: An introduction to phenomenology. The Hague: Nijhoff. (Original work published 1931). [Google Scholar]
- Husserl E. (1965).Philosophy as a rigorous science (Q. Lauer, Trans.). In Husserl E. (Ed.), Phenomenology and the crisis of philosophy. New York, NY: Harper & Row. [Google Scholar]
- Jangland E., Gunningberg L., & Carlsson M. (2009).Patients’ and relatives’ complaints about encounters and communication in health care: Evidence for quality improvement. Patient Education and Counseling, 75(2), 199–204. 10.1136/qshc.2003.008490 [DOI] [PubMed] [Google Scholar]
- Lee J. (2008).Exploring chemotherapy-induced nausea and vomiting: The symptoms, interventions, and relationship to functional status (Doctoral dissertation).Retrieved from ProQuest Dissertations and Theses Global. (UMI No. 3311334) [Google Scholar]
- McCabe C. (2004).Nurse–patient communication: An exploration of patients’ experiences. Journal of Clinical Nursing, 13(1), 41–49. 10.1111/j.1365-2702.2004.00817.x [DOI] [PubMed] [Google Scholar]
- McIntyre P. (2015).Side effects of targeted treatments: Clinicians’ perceptions, patients’ realities. Cancer World, 65,20–25.http://www.cancerworld.org/Articles/Issues/65/March-April-2015/Patient-Voice/707/Side-effects-of-targeted-treatments-clinicians-perceptions-patients-realities.html [Google Scholar]
- Moira A. (2001).Patients’ and relatives’ experiences and perspectives of ‘good’ and ‘not so good’ quality care. Journal of Advanced Nursing, 33(4), 456–466. 10.1046/j.1365-2648.2001.01689.x [DOI] [PubMed] [Google Scholar]
- Moore H. (2014).An overview of chemotherapy-related cognitive dysfunction, or "chemobrain.". Oncology, 28(9), 797–804.https://www.cancernetwork.com/oncology-journal/overview-chemotherapy-related-cognitive-dysfunction-or-chemobrain [PubMed] [Google Scholar]
- Morse J. M. (1994).Designing funded qualitative research. In Denizin N. K., & Lincoln Y. S., Handbook of qualitative research (2nd ed.).Thousand Oaks, CA: Sage [Google Scholar]
- National Coalition for Cancer Survivorship. (n.d.).Becoming a self-advocate. Retrieved from https://www.canceradvocacy.org/becoming-a-self-advocate/
- National Institute of Nursing Research. (2016).The NINR strategic plan: Advancing science, improving lives. A vision for nursing science. https://bit.ly/2vlMVdi
- Newcomb P. (2010).Using symptom management theory to explain how nurse practitioners care for children with asthma. Journal of Theory Construction & Testing, 14(2), 40–44. [Google Scholar]
- Polit D. F., & Beck C. T. (2012).Generalization in quantitative and qualitative research: Myths and strategies. International Journal of Nursing Studies, 47(11), 1451–1458. 10.1016/j.ijnurstu.2010.06.004 [DOI] [PubMed] [Google Scholar]
- Polit D. F., & Beck C. T. (2017).Nursing research: Generating and assessing evidence for nursing practice. (10th ed.).Philadelphia, PA: Lippincott, Williams & Wilkins. [Google Scholar]
- Reeve B. B., Mitchell S. A., Dueck A. C., Basch E., Cella D., Reilly C. M., … Bruner D. W. (2014).Recommended patient-reported core set of symptoms to measure in adult cancer treatment trials. Journal of National Cancer Institute, 106(7), 1–8. 10.1093/jnci/dju129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan H., Schofield P., Cockburn J., Butow P., Tattersall M., Turner J., … Bowman D. (2005).How to recognize and manage psychological distress in cancer patients. European Journal of Cancer, 14(1), 7–15. 10.1111/j.1365-2354.2005.00482.x [DOI] [PubMed] [Google Scholar]
- SIMPRO Research Center. (2018).Electronic symptom management (eSyM). https://www.esymcancermoonshot.org/
- Streubert H. J., & Carpenter D. R. (2011).Qualitative research in nursing: Advancing the humanistic imperative. (5th ed.).Philadelphia, PA: Lippincott, Williams and Wilkins. [Google Scholar]
- Thorsteinsson L. S. (2002).The quality of nursing care as perceived by individuals with chronic illnesses: The magical touch of nursing. Journal of Clinical Nursing, 11(1), 32–40. 10.1046/j.1365-2702.2002.00575.x [DOI] [PubMed] [Google Scholar]
- Yarbro C. H.Wujcik, D. & Gobel, B. H. (Eds.).(2011).Cancer nursing: Principles and practice. (7th ed.).Sudbury, MA: Jones and Bartlett Publishers. [Google Scholar]


