Abstract
Facial nerve identification is considered to be a crucial step in parotid surgery as inadvertent injury to the nerve will lead to facial paralysis. Multiple landmarks are described in literature to identify the facial nerve during parotid surgery but controversies remain as the consistency and accuracy of these landmarks vary. Numerous studies exist in literature but they fail to address a single landmark that is most reliable to identify the facial nerve during parotid surgery. The purpose of this study is to find reliable landmarks for identification of the main trunk of facial nerve during parotid surgery by evidence gathered by cadaveric dissection and intraoperative study during parotid surgery and develop a systematic approach to identify the facial nerve trunk. This prospective study included 41 cadavers (82 parotid regions) and 20 patients with parotid pathology who underwent parotidectomy. We evaluated the feasibility of our C-M-S technique to identify the main trunk of facial nerve in both anatomical and surgical study. The relationship of landmarks (tragal pointer, tympanomastoid suture, superior border of posterior belly of digastric muscle) to the facial nerve trunk was assessed and the shortest distance between them from the facial trunk was measured using a slide caliper. The measurements were compared between the anatomical and surgical study. The main trunk of facial nerve was successfully identified in all cases using C-M-S technique in both anatomical and surgical study. Distance of facial nerve trunk to tragal pointer was more in the cadaveric sample (13.04 ± 5.238 mm) compared to live patients (9.95 ± 3.967 mm) with statistically significant difference (p = 0.036). The mean distance of tympanomastoid suture and posterior belly of digastric muscle to the facial nerve trunk was similar in anatomical and surgical study with p value of 0.877 and 0.083 respectively. The tympanomastoid suture, posterior belly of digastric muscle and tragal pointer are the most useful landmarks for facial nerve identification during parotid surgery. In our study we found that the tympanomastoid suture line is the most consistent landmark present in all our cases and being closest to the facial nerve trunk in both anatomical and surgical study. Further we recommend using the “C-M-S technique” in order to locate the main trunk of the facial nerve.
Keywords: Facial nerve, Parotid surgery, Tympanomastoid suture, Tragal pointer, Posterior belly of digastric, Anatomical study, Surgical study
Introduction
Facial nerve identification is considered to be a crucial step in parotid surgery as inadvertent injury to the nerve will lead to facial paralysis. Facial nerve injury can severely affect speech, swallowing, eye closure, facial expressions and social life of the person [1]. Multiple landmarks are described in literature to identify the facial nerve during parotid surgery but controversies remain as the consistency and accuracy of these landmarks vary [2]. The various landmarks described in literature are tragal pointer, posterior belly of digastric muscle, tympanomastoid suture, stylomastoid artery, styloid process, ramus of mandible and transverse process of axis. The use of many landmarks to identify the facial nerve trunk itself points to the fact that there is less evidence about the safety and reliability of these landmarks in terms of consistency. Multiple studies exist in literature but they fail to address a single landmark that is most reliable to identify the facial nerve during parotid surgery. The purpose of this study is to find reliable landmarks for identification of the main trunk of facial nerve during parotid surgery by evidence gathered by cadaveric dissection and intraoperative study during parotid surgery and develop a systematic approach to identify the facial nerve trunk.
Materials and Methods
This prospective study was conducted over a period of 2 years (2018–2020) with anatomical study conducted as a part of Head and Neck cadaveric dissection workshop at M S Ramaiah Advanced Learning Center, Bangalore and surgical study conducted at Apollo Hospitals, Bangalore. The institutional ethical committee clearance was obtained and our study included 41 cadavers (82 parotid regions) and 20 patients with parotid pathology who underwent parotidectomy. We evaluated the feasibility of our C-M-S technique to identify the main trunk of facial nerve in both anatomical and surgical study. The relationship of landmarks (tragal pointer, tympanomastoid suture, superior border of posterior belly of digastric muscle) to the facial nerve trunk was assessed and the shortest distance between them from the facial trunk was measured using a slide caliper. The measurements were compared between the anatomical and surgical study and p value of < 0.05 was considered significant.
Dissection Technique
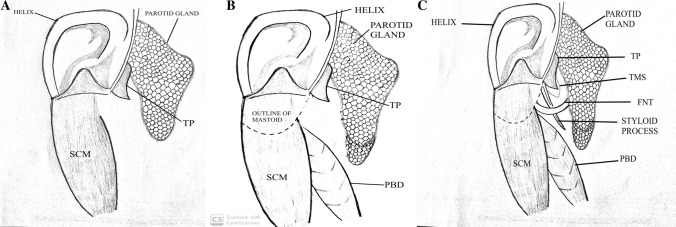
A standard Incision (Modified Blair’s incision) was used in both cadaveric (anatomical study) and live surgery (surgical study). This was followed by elevation of skin flaps. We used a 3 step- “C-M-S” technique to identify the main trunk of the facial nerve (Fig. 1).
Step I: Dissection was carried out in the gutter between the pinna and the parotid gland and the tragal pointer (cartilage) is the most superficial marker. Tragal pointer is identified and exposed completely.
Step II: The tail of the parotid is dissected from the superior portion of sternocleidomastoid muscle, to expose the superior border of posterior belly of digastric muscle. Dissection at this depth between the tragal pointer and posterior belly of digastric muscle can be safely performed as the facial nerve trunk is always deeper to this plane.
Step III: In between the tragal pointer and superior border of posterior belly of digastric, deeper to the level of these landmarks, the tympanomastoid suture is palpable. The facial nerve trunk was found a few millimeters inferiorly at this level in all our cases, the branches can then be traced by careful dissection. The distance between these landmarks and the main trunk of facial nerve were measured using a slide caliper.
Fig. 1.
Diagramatic representation of dissection technique to identify the main trunk of facial nerve (C-M-S TECHNIQUE). a STEP I: Tragal pointer is exposed completely. b STEP II: Superior border of posterior belly of digastric muscle is exposed. c STEP III: Palpation for the tympanomastoid suture line. FNT will be found inferior to this landmark. (FNT- Facial nerve trunk, PBD- Posterior belly of digastric, SCM- Sternocleidomastoid muscle, TP- Tragal pointer, TMS- Tympanomastoid suture.)
This technique involves systematic identification of “Cartilage-Muscle-Suture” (C-M-S) to reach the facial nerve trunk.
Results
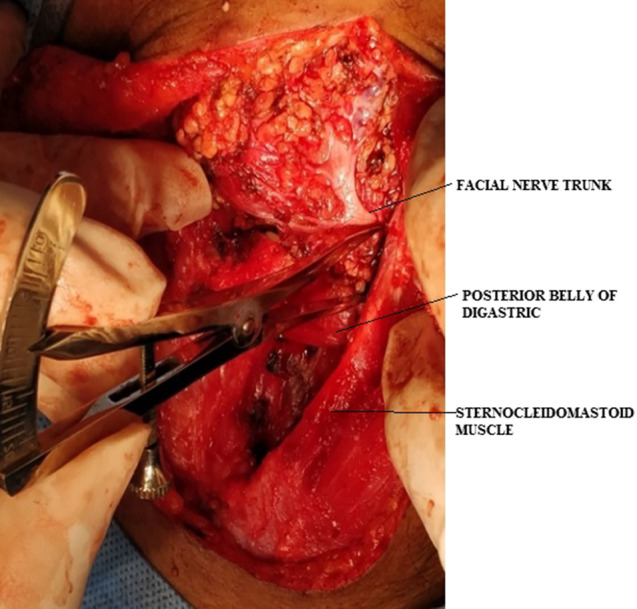
The 3 step “C-M-S” technique was successfully applied to all 82 parotid regions in cadavers as well as 20 in live patients. We found that in 100% of cases we could identify the main trunk of facial nerve without much difficulty (Figs. 2, 3). The age of subjects in the surgical group ranged from 23 to 74 years with a mean of 43.40 years. The mean distance between the tragal pointer (TP) and the facial nerve trunk was 9.95 mm (8.093–11.807 mm) in surgical study and 13.04 mm (10.828–15.252 mm) in the anatomical study (Fig. 4). The mean distance between the tympanomastoid suture (TMS) and the facial nerve trunk in the surgical study and anatomical study was 6.35 mm (5.252–7.448 mm) and 6.50 mm (4.915–8.085 mm) respectively. The mean distance between the posterior belly of digastric (PBD) and the facial nerve trunk in the surgical study was 8.50 mm (7.163–9.837 mm) and in anatomical study was 6.92 mm (5.645–8.195 mm) (Fig. 5). Distance to tragal pointer was more in the cadaveric sample (13.04 ± 5.238 mm) compared to live patients (9.95 ± 3.967 mm) with statistically significant difference (p = 0.036). The mean distance of TMS and posterior belly of digastric muscle to the facial nerve trunk was similar in anatomical and surgical study with p value of 0.877 and 0.083 respectively.
Fig. 2.
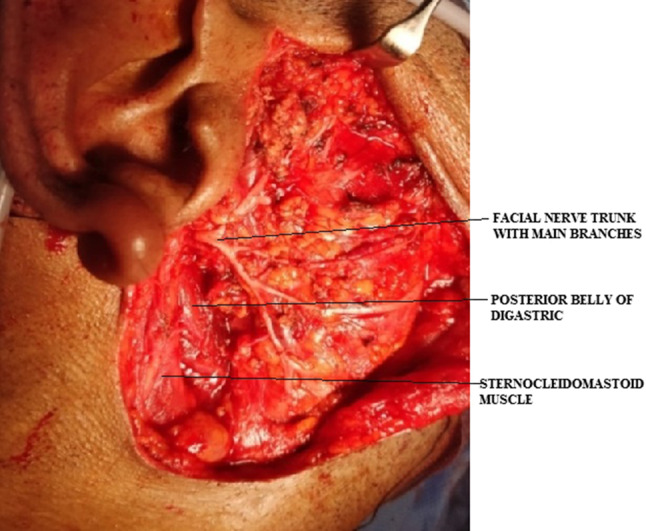
Exposure of facial nerve in surgical study
Fig. 3.
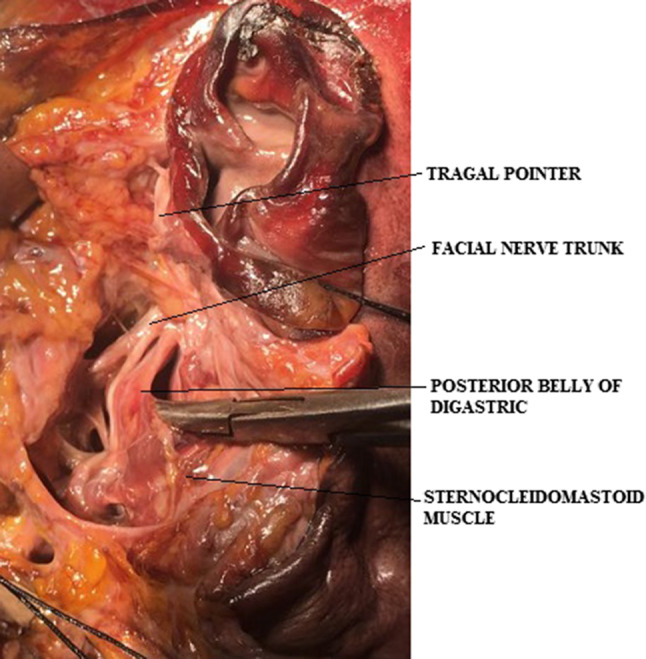
Exposure of facial nerve in anatomical study
Fig. 4.

Measurement of distance between tragal pointer and facial nerve trunk in anatomical study
Fig. 5.
Measurement of distance between superior border of posterior belly of digastric and facial nerve trunk in asurgical study
Discussion
Tragal Pointer as advocated by Conley is the most frequently used landmark for intraoperative identification of Facial nerve trunk [3]. The facial nerve lies around 1 cm deep and inferior to the pointer. A statistically significant difference was noted between the distances to tragal pointer in the cadaveric sample compared to live patients in our study. This may be due to the cartilaginous nature of this landmark and effects of retraction and preservation in the anatomical study. The mean of differences in measurements between tragal pointer and facial nerve trunk ranged from 13.6 ± 11.0 mm [4]. This wide difference in linear distance makes it more time consuming and complex. It was observed that the direction of the cartilaginous tip lacks uniform interpretations. It is cartilaginous, mobile and blunt with irregular tip. If the pointer was involved by the pathology, the next landmark was used instead.
Facial nerve trunk was found to lie within a distance of 4.8–12.8 mm of posterior belly of digastric with a mean distance of 8.79 ± 3.99 mm in literature [4]. In our study, the mean distance of PBD was similar in live patients and cadavers, and the difference was not statistically significant. Its advantages include, being easily identifiable by the virtue of it lying superficial to facial nerve trunk, but being a mobile tissue it is vulnerable to variable degree of retraction. The tragal pointer and the posterior belly of digastric muscle lie at a similar plane. The facial nerve trunk was always found below this plane and hence dissection at this plane can be carried out without much hesitation.
The mean distance of TMS to the main trunk of facial nerve was similar in live patients and cadavers without any statistically significant difference in our study. This may be owing to the bony nature of the landmark which made it less variable than the other landmarks. The TMS which is said to lead to the stylomastoid foramen is the next commonly used landmark, either solely or along with tragal pointer in literature. The facial nerve trunk from TMS was measured in the mean range of 3.79 ± 2.92 mm in various studies [4]. It is easy to locate, because of its constant position and the tragal pointer and tympanomastoid suture seem to be the most preferred landmarks of locating the main trunk of the facial nerve in the literature [5].
Attempts were made to identify and study the other landmarks described in literature. We found that landmarks like the stylomastoid artery and styloid process were more feasible in our cadaveric (Anatomical) study. Due to its inconsistent presence and anatomical variations the stylomastoid artery can only be used when supplemented by the other more commonly known landmarks. It is also known that the artery spirals closely around the facial nerve trunk which could result in iatrogenic nerve injury during surgical exposure of the artery [6]. The styloid process is another landmark described but one may injure the facial nerve while exposing this landmark as it lies medial to the facial nerve trunk. Further abnormally shaped (or absent) styloid process or calcification of stylohyoid tendon may render this landmark unusable [7]. The use of landmarks like the transverse process of axis and ramus of mandible is practically not feasible intra-operatively as it is not encountered during parotid surgery and no specific procedural technique is described to find the facial nerve trunk starting from tip of C1 transverse process. These landmarks are purely of anatomical interest and their clinical utility is questionable [8].
In our study the landmarks were used systematically one after the other to identify the main trunk of facial nerve in a series of 3 steps. We found the facial nerve trunk using this technique in all our cases. C-M-S technique can be used in most cases of benign parotid pathology. In malignant pathology or gross benign pathology the tympanomastoid suture would be the most consistent landmark for the identification of facial nerve trunk, followed by the posterior belly of digastric muscle. In our study we were able to successfully implement this technique and identify the main trunk of facial nerve. Most of the delegates attending our workshops were trainee surgeons and faced no difficulty in following this 3 step technique. This in turn reduces the unwanted dissection and therefore the total operating time. We strongly recommend the use of this technique for identification of facial nerve trunk during parotid surgery.
Conclusion
The tympanomastoid suture, posterior belly of digastric muscle and tragal pointer are the most useful landmarks for facial nerve identification during parotid surgery. In our study we found that the tympanomastoid suture line is the most consistent landmark present in all our cases and being closest to the facial nerve trunk in both anatomical and surgical study. The next most consistent landmark was the posterior belly of digastric muscle followed by the tragal pointer. Further we recommend using the “C-M-S technique” in order to locate the main trunk of the facial nerve.
Authors’ Contributions
Satish Nair: Substantial contributions to the conception or design of the work, revising it critically for important intellectual content, analysis and interpretation of data for the work and drafting the work and final approval of the version to be published. Ashish S Shah: Substantial contributions to the acquisition of data for the work, revising it critically for important intellectual content and final approval of the version to be published. Pavithra V, J G Aishwarya, Brijith KVR, Deeksha Thakur: Substantial contributions to the acquisition of data for the work.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gasser RF. The early development of the parotid gland around the facial nerve and its branches in man. Anat Rec. 1970;167(1):63–77. doi: 10.1002/ar.1091670107. [DOI] [PubMed] [Google Scholar]
- 2.de Ru JA, van Benthem P, Bleys RL, Lubsen H, Hordijk GJ. Landmarks for parotid gland surgery. J Laryngol Otol. 2001;115(2):122–125. doi: 10.1258/0022215011907721. [DOI] [PubMed] [Google Scholar]
- 3.Conley J, Clairmont A. Facial nerve in the recurrent benign pleomorphic adenoma. Arch Otolaryngol. 1979;105(5):247–251. doi: 10.1001/archotol.1979.00790170017004. [DOI] [PubMed] [Google Scholar]
- 4.Ji YD, Donoff RB, Peacock ZS, et al. Surgical landmarks to locating the main trunk of the facial nerve in parotid surgery: a systematic review. J Oral Maxillofac Surg. 2018;76(2):438–443. doi: 10.1016/j.joms.2017.06.039. [DOI] [PubMed] [Google Scholar]
- 5.Tabb HG, Scalco AN, Fraser SF. Exposure of the facial nerve in parotid surgery (use of the tympanomastoid fissure as a guide) Laryngoscope. 1970;80(4):559–577. doi: 10.1288/00005537-197004000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Upile T, Jerjes W, Nouraei SA, et al. The stylomastoid artery as an anatomical landmark to the facial nerve during parotid surgery: a clinico-anatomic study. World J Surg Oncol. 2009;7(1):71. doi: 10.1186/1477-7819-7-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kent DT, Rath TJ, Snyderman C. Conventional and 3-dimensional computerized tomography in eagle’s syndrome, glossopharyngeal neuralgia, and asymptomatic controls. Otolaryngol Head Neck Surg. 2015;153(1):41–47. doi: 10.1177/0194599815583047. [DOI] [PubMed] [Google Scholar]
- 8.Keefe MA, Castro JR, Keefe MS. Identification of the facial nerve main trunk by retrograde dissection of the postauricular branch. Otolaryngol Head Neck Surg. 2009;140(1):126–127. doi: 10.1016/j.otohns.2008.10.014. [DOI] [PubMed] [Google Scholar]