Abstract
Cancer of the tongue forms more than 50% of oral cavity cancers. Generally, patients come with locally advanced tongue cancer. The treatment for this cancer is multi-modality. For resectable cancer, multiple surgical approaches are described in the literature. Mandibulotomy for resection of the middle and posterior third oral cancer is a well-established technique but it has its attended morbidity. We present our results of a new surgical technique, called the Peroral and submandibular cervical surgical approach wherein tongue cancer of middle third and posterior third is resected without mandibulotomy. The advantages of this technique are that the complications of malunion or non-union of bone are avoided, no chances of osteoradionecrosis or osteomyelitis, no need of periosteal elevation or damage, the malignancy is removed with wide margin with minimal blood loss, there is no scar on face or chin, morbidity of surgery is minimal. Also, the technique is easily reproducible.
Keywords: Tongue cancer, Glossectomy, Mandibular sparing approach, Mandibulotomy
Introduction
Cancer of the tongue forms more than 50% of oral cavity cancers [1, 2]. 51% cases involve the lateral margin of the middle third of the tongue, 25% occur in the posterior third, while 20% in the anterior third [3]. Multiple surgical approaches are described in the literature for management of middle and posterior third tongue cancer. These are the mandibular sparing approaches—Transoral approach [4, 5], Transoral Robotic surgery (TORS) [6], Transoral Laser Microsurgery (TLM) [7], the Mandibular Lingual Release approach (MLRA) [8] and the mandible non-sparing approaches—Mandibulotomy (Mandibular Swing approach) [5] and Compartment Excision [9]. Every surgical technique has its own indications and limitations. In this paper, we describe a new surgical approach for easy access and wide excision of middle and posterior third tongue cancer—the Peroral Submandibular Cervical technique, abbreviated as the POSC approach, whereby mandibulotomy can be avoided.
Materials and Methods
In our case series, 13 cases of middle third tongue cancer were included, ranging from 29 to 60 years in age. 12 patients were male while one was female. The squamous cell carcinoma was located on left side in 6 cases, right side in 6 cases and middle of tongue in one case. In all of these cases, the posterior border of the ulcer was located at the junction of the anterior and posterior third of the tongue. T1–T3 lesions of middle and posterior third tongue cancer were included in the study. Cases involving extension of lesion across midline were also included. A complete staging work-up and standard pre-operative assessment was performed with risk stratification for surgery.
The Surgical Steps to be followed in the Same Sequence as Written
Examination is done under anaesthesia (EUA) for extent of lesion. A safe margin is marked on tongue around the lesion (Fig. 1).
From the submandibular approach, the mylohyoid muscle is cut at safe margin and the alveolar mucosa and if needed mandibular periosteum is elevated for oncologically safe margin.
Perorally, the tongue and floor of mouth is incised at a safe margin.
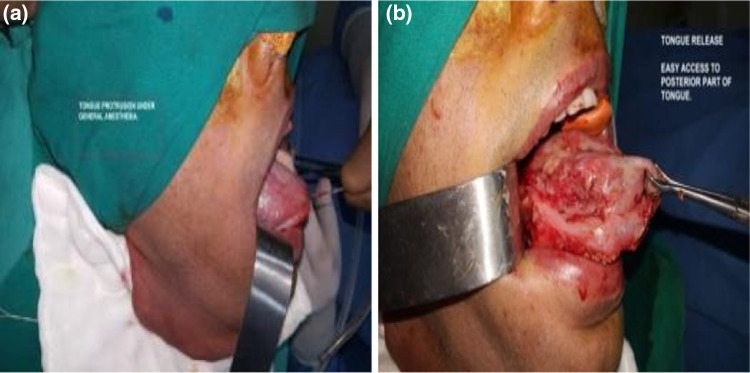
Genioglossus and hyoglossus muscles are cut at safe margin through the submandibular approach. This is known as tongue release (Fig. 2a, b). By this tongue release technique, the posterior part of the tongue can be almost pulled out in the anterior oral cavity and the posterior and medial cut is made with a safe margin, under direct vision.
-
The posterior part of tongue is incised and specimen is delivered out.
In following conditions, it is not possible to see the posterior margin—(a) trismus (b) bulky tongue (c) obese patient. In these situations, after tongue release, the tongue is pulled out through the neck and cut through both per oral and cervical approaches.
Fig. 1.
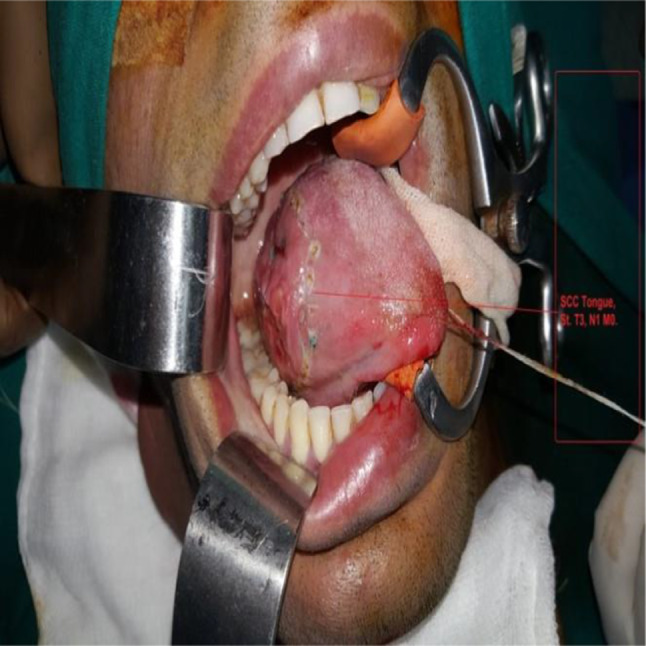
Middle third tongue cancer
Fig. 2.
a Exposure of carcinoma before tongue release, b exposure of carcinoma after tongue release
Results
Hereby, we present our results of the POSC approach in 13 cases of middle third tongue cancer, who were followed-up for an adequate period of 1 year, closely observing for complications (Table 1). In our case series, the age range was from 29 to 60 years, while 12 patients were male and one female. The size of the lesion ranged from 0.8 to 4.5 cm. On histopathological examination, none of the margins in any of the patients were close or positive, such that posterior margin was > 0.8 cm, medial margin was > 1.0 cm, lateral margin > 0.5 cm and the base > 0.5 cm. Reconstruction of the defect was done with either Radial artery forearm free flap or Pectoralis major myocutaneous flap. The complication rate was minimal. None of the cases developed oro-cutaneous fistula or osteoradionecrosis during follow-up. There was no case of local recurrence and the mortality rate was zero percent on 1 year follow-up.
Table 1.
Study of 13 cases carcinoma of middle and/posterior tongue. February 2016–2017. POSC approach
| No | Age | Sex | Location of cancer | Clinical stage | Size of primary HPR (cm) | Posterior margin (cm) | Medial margin | Lateral margin |
|---|---|---|---|---|---|---|---|---|
| 1 | 36 | M | Middle | T1N0M0 | 0.8 × 0.8 × 0.2 | 1 | 1 | 0.7 |
| 2 | 42 | M | Lt lateral | T2N1M0 | 3 × 2 × 1 | 2 | 2 | 1 |
| 3 | 42 | M | Rt lateral | T2N0M0 | 2.5 × 1.5 × 1 | 2 | 2.5 | 0.5 |
| 4 | 64 | M | Lt. Lateral | T1N2M0 | 1 × 1 × 1 | 1 | 2 | 1 |
| 5 | 55 | M | Rt lateral | T2N0M0 | 3 × 2 × 0.5 | 0.8 | 1.8 | 0.5 |
| 6 | 29 | M | Lt lateral | T2N1M0 | 3.5 × 1 × 1 | 2.5 | 2 | 1.5 |
| 7 | 29 | M | Rt lateral | T3N0M0 | 3.5 × 2.5 × 1.2 | 2 | 2.5 | 1 |
| 8 | 35 | M | Lt lateral | T2N0M0 | 3.8 × 1.5 × 1 | 3 | 3 | 1 |
| 9 | 58 | F | Lt lateral | T2N2M0 | 0.8 × 0.5×0.5 | 1 | 2.5 | 1 |
| 10 | 40 | M | Rt lateral | T1N0M0 | 1.5 × 1.5 × 0.5 | 0.8 | 2 | 0.5 |
| 11 | 69 | M | Lt lateral | T2N0M0 | 2.2 × 1 × 0.5 | 3 | 2 | 1 |
| 12 | 57 | M | Rt lateral | T3N0M0 | 4.5 × 3 × 3 | 3 | 2 | 2 |
| 13 | 57 | M | Rt lateral | T2N0M0 | 3 × 1.5 × 0.8 | 4.5 | 3.5 | 2 |
The advantages of the POSC approach could be enumerated as following:
Very good access at middle third and deep part of tongue.
Tongue and floor of mouth cancer is removed with wide margin all around.
No mental nerve damage, hence no chin or labial anaesthesia.
Minimal blood loss.
No need of periosteal elevation, hence no compromise of mandibular vascularity.
As mandibulotomy is not done, the associated morbidity like malunion, non-union, osteomyelitis and osteoradionecrosis of mandible is not seen.
No scarring or labial asymmetry on face due to absence of labial split.
Minimal morbidity of surgery.
This technique is easily reproducible.
Thus, the POSC approach has shown excellent oncological results along with ease of manoeuvrability, which can be achieved at any centre without special instruments and infrastructure.
Discussion
The surgical approaches for tongue cancer are defined by the site of the lesion. Most of the anterior lesions can be resected by per oral approach, without the need for mandibulotomy, if the mouth opening is adequate and there is no involvement of mandibular bone. However, for middle and posterior third tongue cancer, without invasion of the mandibular periosteum or bone, a plethora of surgical approaches have been described in the literature (Table 2), viz—the Transoral approach, cheek flap approach, the lip split mandibulotomy technique (mandibular swing) and the mandibular lingual releasing approach (MLRA).
Table 2.
Comparison of surgical approaches for middle and posterior third tongue
| Per oral rescection | Mandibulotomy. mandibular swing | Pull through | MLRA | |
|---|---|---|---|---|
| Access to lesion | Difficult | Easy | Difficult | Easy |
| Lip split, facial scarring and labial asymmetry | No | Yes | No | No |
| Mental nerve damage and labial anesthesia | No | May be | No | No |
| Access to posterior margin and deep tongue | Very difficult | Easy | Very difficult | Good |
| Damage to inner mucoperiosteum | No | No | No | Yes |
| Blood loss during surgery | More | More | More | More |
| Fistulae rate | More | More | More | Less |
| Malunion or non-union of the osteotomy site | No | Yes | No | No |
| Chances of mandibular osteo radionecrosis | Less | More | Less | More |
| Flap suturing | Very difficult | Very easy | Very difficult | Easy |
Transoral resection [4, 5] for middle and posterior tongue cancer is a difficult approach due to inadequate access for examination and manoeuvrability at middle and posterior part of tongue. Besides, there are increased chances of close or positive medial and posterior margin. As such this approach is more appropriate for T1 lesions. Also, this approach becomes even more difficult in individuals with associated submucous fibrosis, trismus, ankyloglossia, a short neck or obese patients. Most of the patients in our part of the country come with trismus of different grades. In our series of 13 cases, all patients had trismus. Hence, the Transoral approach was not applicable.
The cheek flap approach [5]—this classical technique involves raising of ipsilateral cheek flap (lower) for adequate access and resection of lesions located in anterior part of the tongue. The access for tongue cancer located in middle and posterior third is inadequate and as such these lesions cannot be excised under direct vision. The technique is difficult in cases of attending trismus, ankyloglossia and obesity. Another disadvantage is the sectioning of mental nerve, leading to consequent anaesthesia of chin. This technique can be practiced in edentulous patients but difficult in dentulous cases.
Lip split mandibulotomy or mandibular swing approach [5]—is a well-established approach. It provides adequate exposure of middle and posterior third tongue [4]. This technique involves splitting of lower lip, which is associated with increased morbidity of facial scarring and labial asymmetry [8, 10, 11]. Also, a paramedian or lateral mandibulotomy is done. Hence, a malunion or non-union may occur in 9–13% of cases [12, 13]. Besides, lateral mandibulotomy or elevation of cheek flap leads to sacrifice of mental nerve, resulting in anaesthesia of chin. Closure of the paralingual incision used with mandibular swing is often strenuous. Mandibulotomy can increase the risk of osteoradionecrosis [12], especially when adjuvant radiotherapy is chosen. In contrast, there is no lip split or mandibulotomy done in POSC approach. Hence, all the above mentioned complications are avoided.
Mandibular lingual release approach was first reported by Stanley in 1984 [14]. In this approach, a lingual floor of mouth flap is created and tongue is pulled out in neck. Under direct vision, wide local excision of tongue cancer can be done. This approach gives good access to posterior part of tongue. In Stanley’s series, the fistula rate was 25% and none of the patients had permanent tracheostomy. It was described as a good choice for patients who underwent preoperative radiation or where radiation therapy had failed [14]. In this approach, the inner mandibular periosteum is raised with lingual floor of mouth flap, which compromises the vascularity of the mandible. Since most of the patients are candidates for adjuvant chemoradiation, the resulting morbidity is high due to consequent complications such as osteoradionecrosis, osteomyelitis or pathological fracture. In POSC approach, there is no tempering with mandibular periosteum, until and unless there is a need to take safe margin for cancer.
Conclusion
Our initial results with a follow-up period of 1 year, have shown excellent outcomes for the POSC approach, apart from the many advantages over other surgical techniques. The morbidity of this surgical technique is negligible and the rate of complications is extremely low. Both aesthetics and function are preserved due to avoidance of lip split and mandibulotomy. It is an easily reproducible technique which does not require any special instruments or infrastructure.
Bullet Points
Surgical approaches for radical surgery of middle third tongue cancer, as described in the literature, have attendant morbidities.
Techniques described in the literature for surgery lead to facial asymmetry, poor sphincter mechanism of the lips, damage to the mandible and other healing complications.
With the POSC technique for middle third tongue cancer, all the above mentioned complications are avoided or are minimal and the technique is easily reproducible.
With this technique, oncologically sound resections can be done with a good safe margin all around the tongue lesion, especially posterior and medial margins.
The reconstruction is also accomplished easily (free flap reconstruction / pedicled flap reconstruction) with faster healing, good cosmetic and functional outcome, minimal chances of postoperative fistula.
The adjuvant protocol of treatment in form of radiotherapy is started earliest and completed with good disease free survival and overall survival in these patients.
Author Contributions
NK: Devised a new technique of surgery for middle third tongue cancer, participated in the conception and design of the manuscript, drafting of manuscript and literature search, final editing of the manuscript, PK: Participated in the drafting of manuscript and literature search, JSB: Participated in the drafting of manuscript and literature search, TO: Participated in the conception and design of manuscript.
Funding
The authors declare that there was no financial aid obtained from any source for the preparation of this manuscript.
Data Availability
Data is available on request from authors.
Declarations
Conflict of interest
Nitin Khunteta, Prakhar Katta, Jaspreet Badwal, Tarun Ojha declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nitin Khunteta, Email: onconitin@yahoo.co.in.
Prakhar Katta, Email: drprakharkatta06@gmail.com.
Jaspreet Singh Badwal, Email: winterghosts98@gmail.com.
Tarun Ojha, Email: drtarunojha_ent@yahoo.com.
References
- 1.Moore SR, Johnson NW, Pierce AM, Wilson DF. The epidemiology of mouth cancer: a review of global incidence. Oral Dis. 2000;6:65–74. doi: 10.1111/j.1601-0825.2000.tb00104.x. [DOI] [PubMed] [Google Scholar]
- 2.Marur S, Forastiere AA. Head and neck squamous cell carcinoma: update on epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2016;91(3):386–396. doi: 10.1016/j.mayocp.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 3.Bailey H, McN Love, editors. Short practice of surgery. 24. London: Hodder Arnold; 2004. pp. 702–717. [Google Scholar]
- 4.Shah JP, Patel SG, editors. Head and neck surgery and oncology. New York: Elsevier; 2003. pp. 195–199. [Google Scholar]
- 5.Shah JP. Surgical approaches to the oral cavity primary and neck. Int J Radiat Oncol Biol Phys. 2007;69(2 Suppl):S15–S18. doi: 10.1016/j.ijrobp.2007.03.069. [DOI] [PubMed] [Google Scholar]
- 6.Mercante G, Ruscito P, Pellini R, Cristalli G, Spriano G. Transoral robotic surgery (TORS) for tongue base tumours. Acta Otorhinolaryngol Ital. 2013;33(4):230–235. [PMC free article] [PubMed] [Google Scholar]
- 7.Sinha P, Hackman T, Nussenbaum B, Wu N, Lewis JS, Jr, Haughey BH. Transoral laser microsurgery for oral squamous cell carcinoma: oncologic outcomes and prognostic factors. Head Neck. 2014;36(3):340–351. doi: 10.1002/hed.23293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stringer SP, Jordan JR, Mendenhall WM, Parsons JT, Cassisi NJ, Million RR. Mandibular lingual releasing approach. Otolaryngol Head Neck Surg. 1992;107(3):395–398. doi: 10.1177/019459989210700309. [DOI] [PubMed] [Google Scholar]
- 9.Calabrese L, Giugliano G, Bruschini R, Ansarin M, Navach V, Grosso E, Gibelli B, Ostuni A, Chiesa F. Compartmental surgery in tongue tumours: description of a new surgical technique. Acta Otorhinolaryngol Ital. 2009;29(5):259–264. [PMC free article] [PubMed] [Google Scholar]
- 10.Brown J, Chatterjee R, Lowe D, Lewis-Jones H, Rogers S, Vaughan D. A new guide to mandibular resection for oral squamous cell carcinoma based on the Cawood and Howell classification of the mandible. Int J Oral Maxillofac Surg. 2005;34(8):834–839. doi: 10.1016/j.ijom.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 11.Cilento BW, Izzard M, Weymuller EA, Futran N. Comparison of approaches for oral cavity cancer resection: lip-split versus visor flap. Otolaryngol Head Neck Surg. 2007;137(3):428–432. doi: 10.1016/j.otohns.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Davidson J, Freeman J, Birt D. Mandibulotomy in the irradiated patient. Arch Otolaryngol Head Neck Surg. 1989;115(4):497–499. doi: 10.1001/archotol.1989.01860280095024. [DOI] [PubMed] [Google Scholar]
- 13.DeSanto LW, Whicker JH, Devine KD. Mandibular osteotomy and lingual flaps: use in patients with cancer of the tonsil area and tongue base. Arch Otolaryngol. 1975;101(11):652–655. doi: 10.1001/archotol.1975.00780400010003. [DOI] [PubMed] [Google Scholar]
- 14.Stanley RB. Mandibular lingual releasing approach to oral and oropharyngeal carcinomas. Laryngoscope. 1984;94(5):596–600. doi: 10.1288/00005537-198405000-00002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available on request from authors.